4325d80557399e357b066c1a461ee1d9.ppt
- Количество слайдов: 52
Provider Enrollment and the Affordable Care Act HP Provider Relations May 2012
Agenda – Session Objectives – Provider Enrollment Web Pages – Affordable Care Act (ACA) Impact – Risk Levels – Revalidation – Disclosed Individuals – Profile Updates – Provider Screening – Background Checks – Associated Fees 2 Provider Enrollment and the ACA May 2012
Objectives – Know the screening tasks that apply to your provider type – Understand the impact of your assigned risk level – Understand the revalidation process 3 Provider Enrollment and the ACA May 2012

On the Web Indianamedicaid. com

Affordable Care Act 5 Provider Enrollment and the ACA May 2012
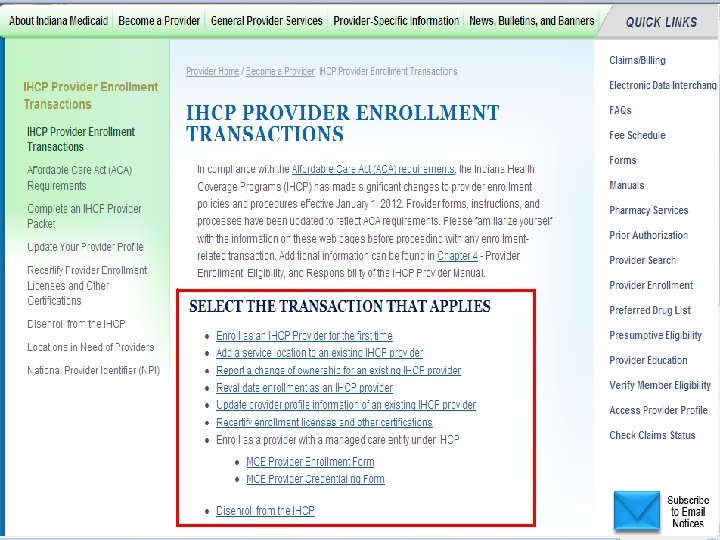
6 Footer Goes Here
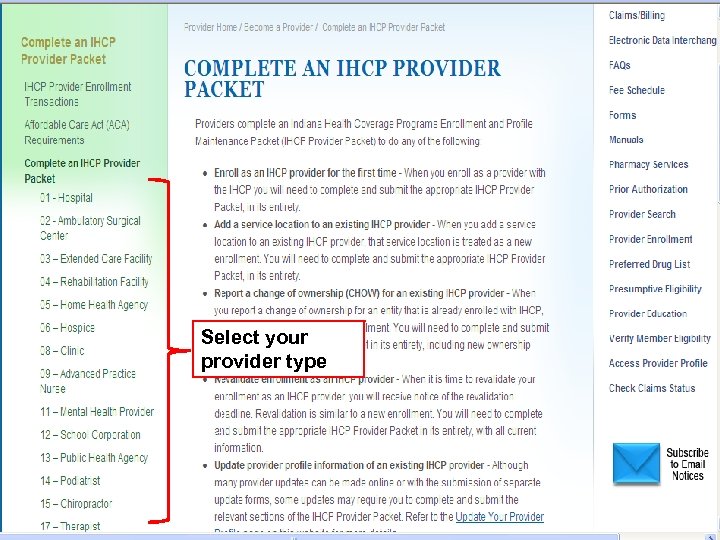
Select your provider type 7 Footer Goes Here
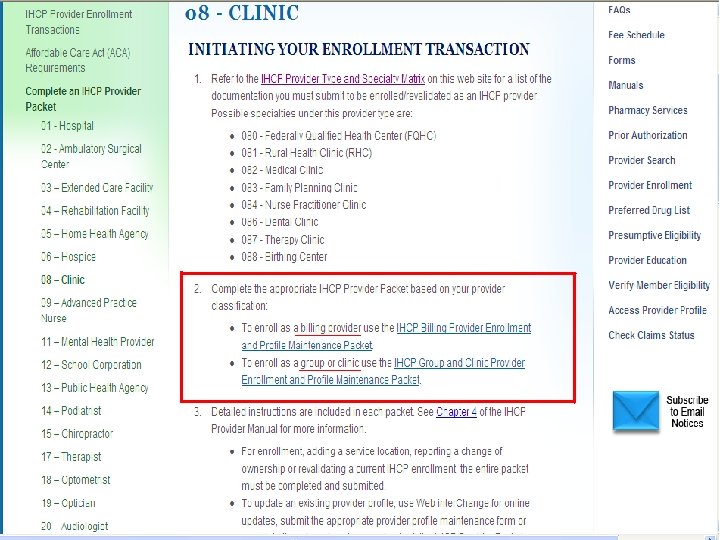
8 Footer Goes Here
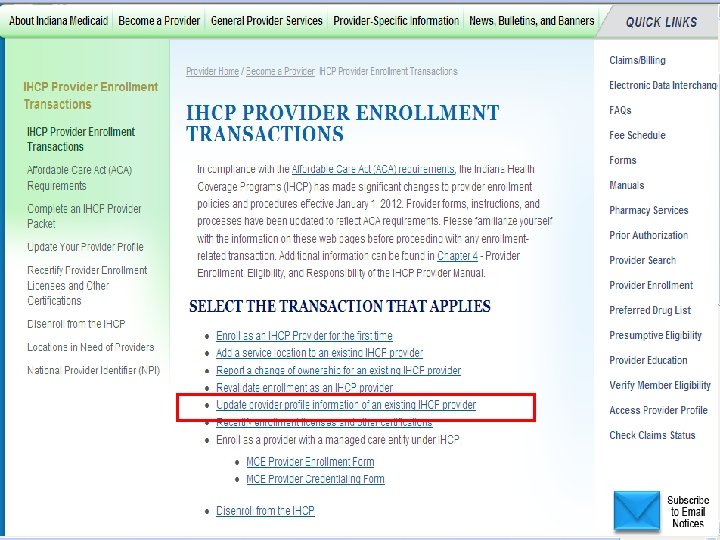
9 Footer Goes Here
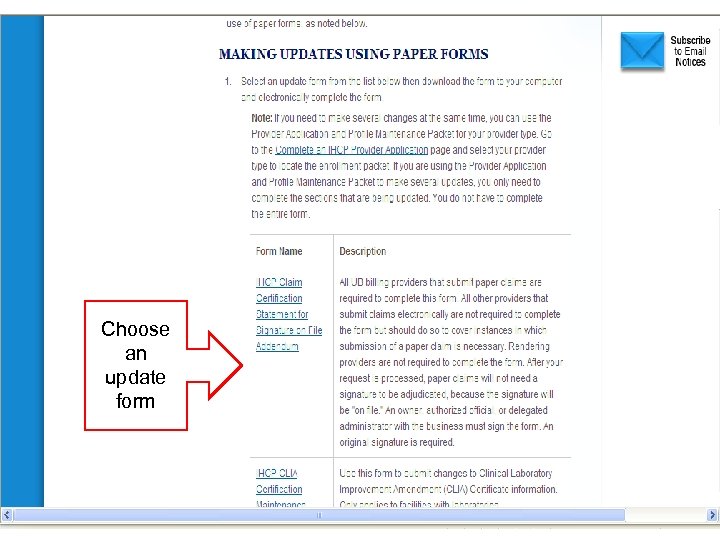
Choose an update form 10 Footer Goes Here

Define What is the ACA?
Affordable Care Act Impact on Provider Enrollment – Centers for Medicare & Medicaid Services (CMS) Rule 6028 -FC of the ACA provides procedures under which screening activities are performed for providers in Medicare and state Medicaid programs. – Screening activities place heightened emphasis on program integrity designed to reduce fraud, waste, and abuse in the Medicare and Medicaid programs. 12 Provider Enrollment and the ACA May 2012
Affordable Care Act Impact on Provider Enrollment – On January 1, 2012, the Indiana Health Coverage Programs (IHCP) adopted and enacted new provider enrollment and screening requirements mandated by the ACA. – Screening and pre-enrollment procedures are applicable to: • • Re-enrollments due to a change of ownership • Existing providers adding new service locations; and, • 13 New providers enrolling for the first time Existing providers revalidating their enrollment. Provider Enrollment and the ACA May 2012

Identify Risk Levels
Risk Levels – All provider types and specialties are assigned to one of the following risk levels. Waiver providers are assigned risk levels at the subspecialty level. • High • Moderate • Limited – Providers are subject to screening tasks based on their assigned risk level – The risk level categorization is established by the CMS, based on an assessment of potential for fraud, waste, and abuse for each provider type/specialty – The risk level assignment may be increased at any time at the discretion of the State. In these instances, the provider will be notified by the State, and the new risk level will apply to processing enrollment-related transactions. – The Provider Type Application Fee and Risk Assignment Matrix (for Non. Waiver and Waiver providers) provides a full list of provider types and their assigned risk level. NOTE: Review this document before revalidating to review current requirements 15 Provider Enrollment and the ACA May 2012
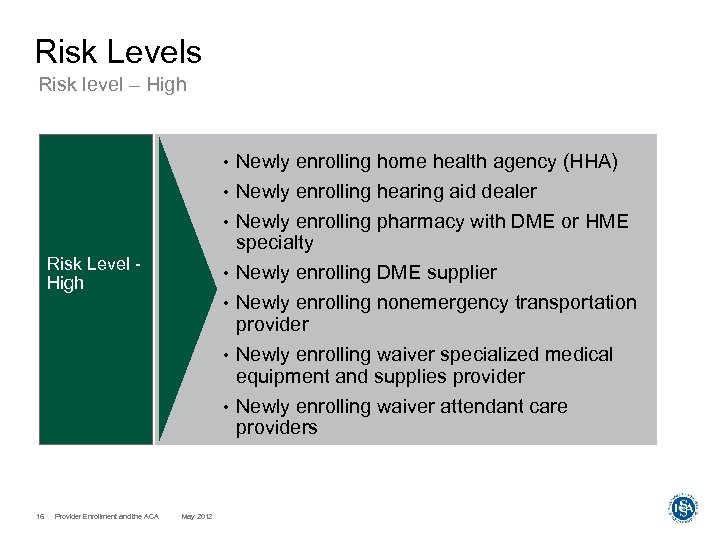
Risk Levels Risk level – High • • Newly enrolling hearing aid dealer • Risk Level High Newly enrolling home health agency (HHA) Newly enrolling pharmacy with DME or HME specialty Newly enrolling DME supplier Newly enrolling nonemergency transportation provider Newly enrolling waiver specialized medical equipment and supplies provider Newly enrolling waiver attendant care providers • • 16 Provider Enrollment and the ACA May 2012
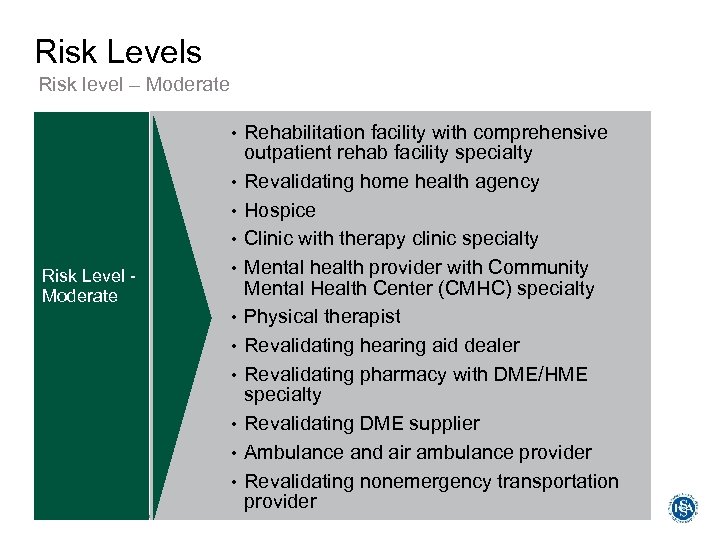
Risk Levels Risk level – Moderate • • • Risk Level Moderate • • • 17 Provider Enrollment and the ACA May 2012 Rehabilitation facility with comprehensive outpatient rehab facility specialty Revalidating home health agency Hospice Clinic with therapy clinic specialty Mental health provider with Community Mental Health Center (CMHC) specialty Physical therapist Revalidating hearing aid dealer Revalidating pharmacy with DME/HME specialty Revalidating DME supplier Ambulance and air ambulance provider Revalidating nonemergency transportation provider
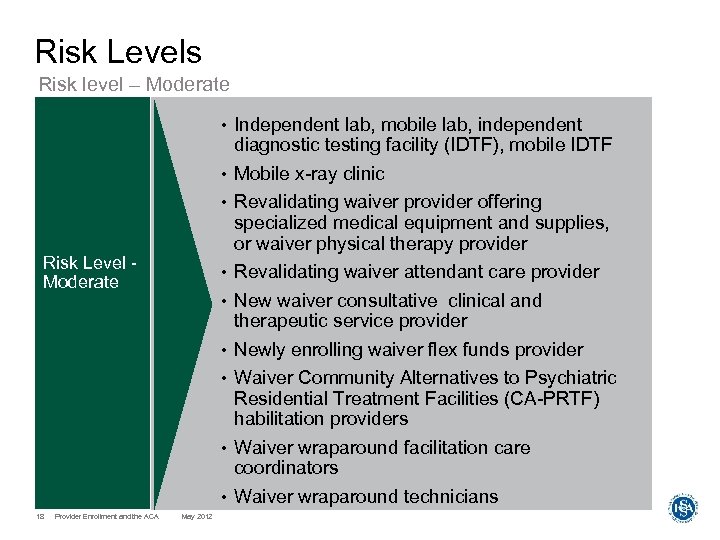
Risk Levels Risk level – Moderate • • • Risk Level Moderate • • • Independent lab, mobile lab, independent diagnostic testing facility (IDTF), mobile IDTF Mobile x-ray clinic Revalidating waiver provider offering specialized medical equipment and supplies, or waiver physical therapy provider Revalidating waiver attendant care provider New waiver consultative clinical and therapeutic service provider Newly enrolling waiver flex funds provider Waiver Community Alternatives to Psychiatric Residential Treatment Facilities (CA-PRTF) habilitation providers • Waiver wraparound facilitation care coordinators • Waiver wraparound technicians • 18 Provider Enrollment and the ACA May 2012
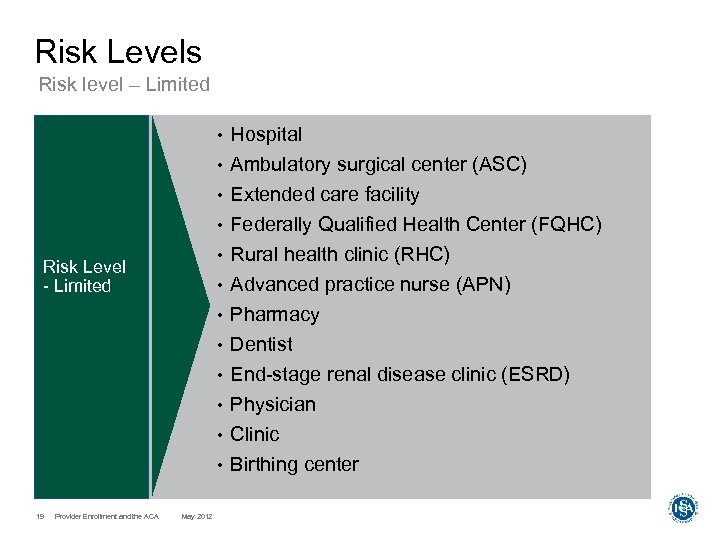
Risk Levels Risk level – Limited • Hospital • Ambulatory surgical center (ASC) • Extended care facility Federally Qualified Health Center (FQHC) Rural health clinic (RHC) Advanced practice nurse (APN) Pharmacy Dentist End-stage renal disease clinic (ESRD) Physician Clinic Birthing center • • Risk Level - Limited • • 19 Provider Enrollment and the ACA May 2012
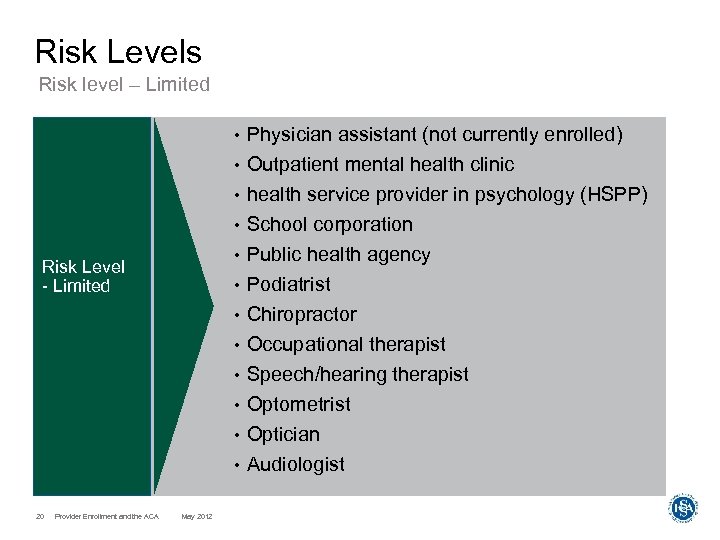
Risk Levels Risk level – Limited • Physician assistant (not currently enrolled) • Outpatient mental health clinic • health service provider in psychology (HSPP) School corporation Public health agency Podiatrist Chiropractor Occupational therapist Speech/hearing therapist Optometrist Optician Audiologist • • Risk Level - Limited • • 20 Provider Enrollment and the ACA May 2012
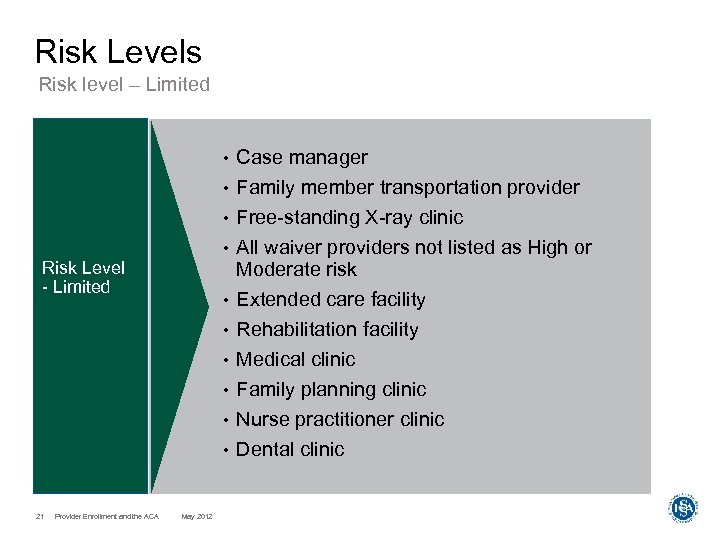
Risk Levels Risk level – Limited Case manager • Family member transportation provider • • • Risk Level - Limited • • • 21 Provider Enrollment and the ACA May 2012 Free-standing X-ray clinic All waiver providers not listed as High or Moderate risk Extended care facility Rehabilitation facility Medical clinic Family planning clinic Nurse practitioner clinic Dental clinic

Revalidation
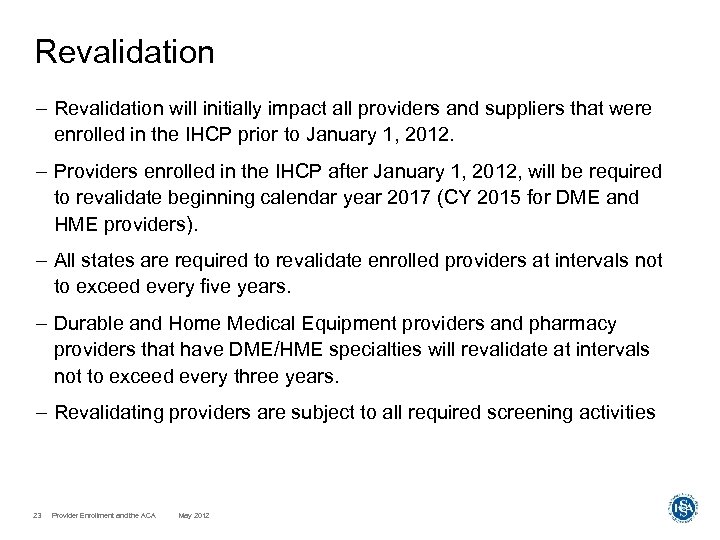
Revalidation – Revalidation will initially impact all providers and suppliers that were enrolled in the IHCP prior to January 1, 2012. – Providers enrolled in the IHCP after January 1, 2012, will be required to revalidate beginning calendar year 2017 (CY 2015 for DME and HME providers). – All states are required to revalidate enrolled providers at intervals not to exceed every five years. – Durable and Home Medical Equipment providers and pharmacy providers that have DME/HME specialties will revalidate at intervals not to exceed every three years. – Revalidating providers are subject to all required screening activities 23 Provider Enrollment and the ACA May 2012
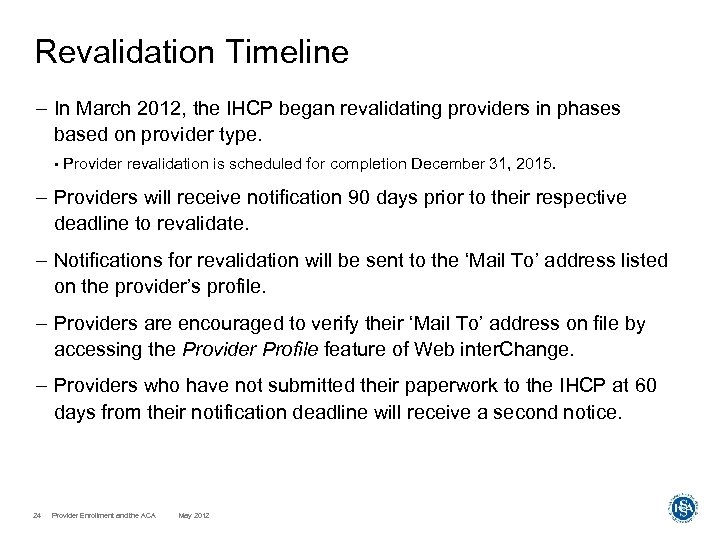
Revalidation Timeline – In March 2012, the IHCP began revalidating providers in phases based on provider type. • Provider revalidation is scheduled for completion December 31, 2015. – Providers will receive notification 90 days prior to their respective deadline to revalidate. – Notifications for revalidation will be sent to the ‘Mail To’ address listed on the provider’s profile. – Providers are encouraged to verify their ‘Mail To’ address on file by accessing the Provider Profile feature of Web inter. Change. – Providers who have not submitted their paperwork to the IHCP at 60 days from their notification deadline will receive a second notice. 24 Provider Enrollment and the ACA May 2012
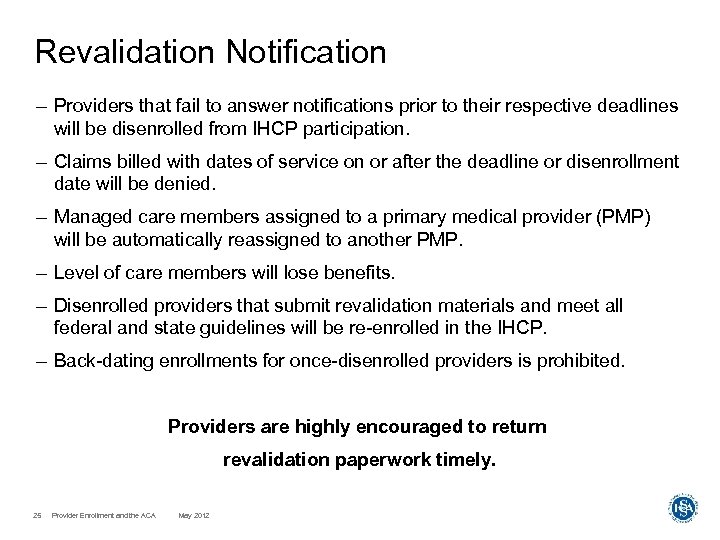
Revalidation Notification – Providers that fail to answer notifications prior to their respective deadlines will be disenrolled from IHCP participation. – Claims billed with dates of service on or after the deadline or disenrollment date will be denied. – Managed care members assigned to a primary medical provider (PMP) will be automatically reassigned to another PMP. – Level of care members will lose benefits. – Disenrolled providers that submit revalidation materials and meet all federal and state guidelines will be re-enrolled in the IHCP. – Back-dating enrollments for once-disenrolled providers is prohibited. Providers are highly encouraged to return revalidation paperwork timely. 25 Provider Enrollment and the ACA May 2012
Revalidation Notification – Web inter. Change users will be able to view the providers’ Service Location name, address, and revalidation deadline for those that are due for revalidation. • • Provider names will be listed under the View Upcoming Providers for Revalidation link under the Provider Profile feature. • 26 Users must have “View” access within Provider Profile to see the list of names. Providers’ names will be removed from the list when the revalidation deadline passes. Provider Enrollment and the ACA May 2012
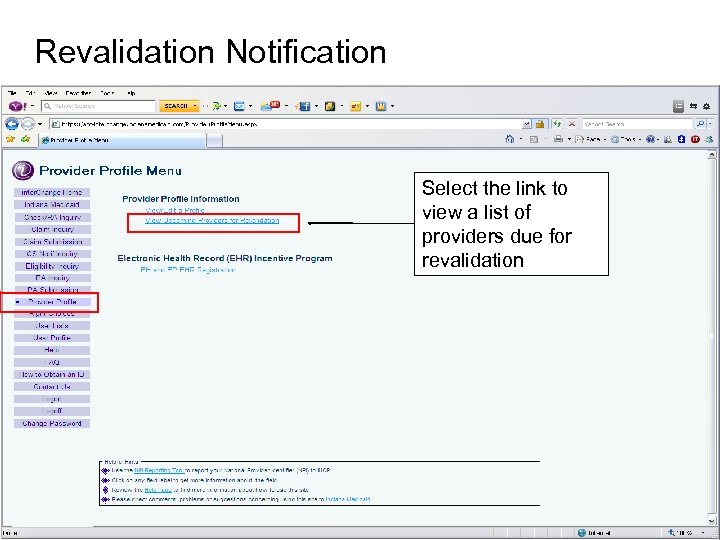
Revalidation Notification Select the link to view a list of providers due for revalidation 27 Provider Enrollment and the ACA May 2012
Revalidation Notification 28 Provider Enrollment and the ACA May 2012
Revalidation vs. Recertification – Revalidation • • Required for all currently enrolled providers at intervals of three or five years • Involves completing a new enrollment application • 29 Required by the Affordable Care Act Requires performance of all risk-appropriate screening activities Provider Enrollment and the ACA May 2012
Revalidation vs. Recertification – Recertification • Required by the State of Indiana • Required for currently enrolled out-of-state providers of certain specialties − Hospital – Upon renewal of license or Joint Commission on the Accreditation of Healthcare Organizations (JCAHO) certification − Some Extended Care Facilities – Annual submission of a newly signed Provider Agreement − Ambulance – Upon issuance of a renewed Emergency Medical Service (EMS) certificate or EMS Air Ambulance certificate − Transportation – Upon issuance of a renewed Motor Carrier Services (MCS) certificate/operating authority or Livery license and insurance policy • • Does not require completion of a new enrollment application • Does not require completion of screening activities • 30 Requires completion of the IHCP Provider Recertification Form Does not require payment of the application fee Provider Enrollment and the ACA May 2012

Define Disclosed Individuals
Disclosed Individuals Paper Enrollment Application – Schedule C, sections C. 1 through C. 3 of the IHCP Provider Enrollment Application collects the names of disclosed individuals. – Disclosure information refers to the identification of: • Business owners • Officers • Managers • Members of the Board of Directors • Managers responsible for day-to-day operations • Subcontractors – The ACA mandates background checks for those with a 5% or more ownership in a High risk provider entity 32 Provider Enrollment and the ACA May 2012
Disclosed Individuals Web inter. Change – Disclosure information is also collected via the Provider Profile feature of Web inter. Change. • Applies to providers assigned to the limited risk category only – A field has been added to Web inter. Change Provider Profile to capture, store, and display the date of birth for all disclosed individuals. – Web inter. Change requires the addition of the date of birth for new entries and updates to existing entries for disclosed individuals and rendering providers. 33 Provider Enrollment and the ACA May 2012
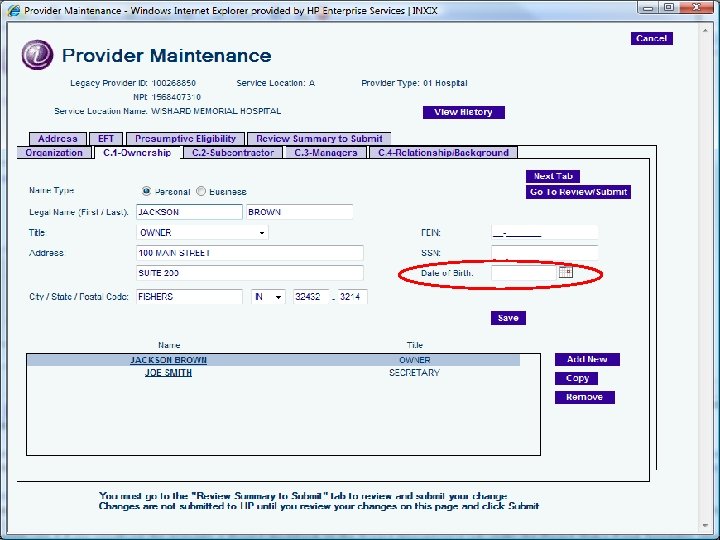
Disclosure Information 34 Provider Enrollment and the ACA May 2012
Profile Updates
Profile Updates – For providers assigned to the high and moderate risk levels, the following Web inter. Change updates are not allowed: • Service Location address change − Unannounced, unscheduled site visits will be conducted before the address change is approved • Addition and removal of names from the disclosure information − Disclosed individuals are subject to screening activities before changes are approved • Addition of Specialty − Those that acquire a higher-risk specialty than previously assigned may not update on Web inter. Change Note: These profile updates must be performed using the paper forms 36 Provider Enrollment and the ACA May 2012
Profile Updates Paper maintenance forms • Providers may continue to use paper update forms to perform maintenance to their profile. • Modifications have been made to the following maintenance forms: − IHCP Name Address Maintenance Form − IHCP Claim Certification Statement for Signature on File Addendum − IHCP CLIA Certification Maintenance Form − IHCP Delegated Administrator Addendum − IHCP Electronic Funds Transfer Addendum − IHCP Medicare Number Maintenance Form − IHCP Recertification Form − IHCP Disenrollment Form − IHCP Specialty Maintenance Form − IHCP Tax Identification Maintenance Form − IHCP Psychiatric Hospital Bed Addendum − IHCP PRTF Attestation Letter Information 37 Provider Enrollment and the ACA May 2012 Modifications include the addition of Social Security Number and date of birth fields, a fee payment form and background/fingerprint check form.

Screen Due Diligence
Provider Screening tasks – Prior to completing enrollment processing, providers are subject to screening tasks based on their risk category. – High risk category : • Unscheduled, unannounced site visits − Site visits are conducted prior to and after an approved enrollment • • Validation of disclosed individuals with the Office of the Inspector General (OIG) Excluded Individuals database, the Excluded Parties List System (EPLS) and the Social Security Death Master List • License verification • Proof of Medicare enrollment, if Medicare-enrolled with Medicare Provider Enrollment Chain and Ownership System (PECOS) • 39 Fingerprint-based background check of disclosed individuals with a 5% or more ownership interest Validation of the National Provider Identifier (NPI) with the National Plan and Provider Enumeration System (NPPES) Provider Enrollment and the ACA May 2012
Provider Screening tasks – Moderate risk category • Unscheduled, unannounced site visits − Site visits are conducted prior to and after an approved enrollment • Validation of disclosed individuals with the OIG Excluded Individuals database, the EPLS and Social Security Death Master List • License verification • Proof of Medicare enrollment, if Medicare-enrolled – Limited risk category : • Validation of disclosed individuals with the OIG Excluded Individuals database, the EPLS and Social Security Death Master List • License verification • Proof of Medicare enrollment, if Medicare-enrolled – All screening tasks for all risk categories are performed for each service location individually 40 Provider Enrollment and the ACA May 2012
Provider Screening Database checks – The names of disclosed individuals for currently enrolled providers are validated on the EPLS, OIG, Social Security Death Master List, NPPES, PECOS, and MCSIS databases on a monthly basis. – The Excluded Parties List System identifies individuals that are debarred, suspended, excluded, or disqualified from receiving federal contracts, subcontracts, financial, and nonfinancial assistance and benefits. – The OIG Exclusion List identifies individuals that are excluded from participation in Medicare, Medicaid, and Title XX programs. – The Social Security Death Master List is the national repository to validate that an individual is deceased. 41 Provider Enrollment and the ACA May 2012
Provider Screening Database checks – NPPES is a database of NPIs assigned to healthcare providers – PECOS is the provider enrollment system used by Medicare – Medicaid and CHIP State Information Sharing System (MCSIS) database identifies individuals excluded from participation in other State’s Medicaid programs – These providers are not eligible to participate in the IHCP. – Providers that were sanctioned by the OIG are not eligible to enroll in the IHCP. – Bulletin BT 200934 reminds providers of their responsibility to screen disclosed individuals and employees prior to hiring and periodically thereafter. 42 Provider Enrollment and the ACA May 2012

Background Check
Background Check – Disclosed individuals with a 5% or more ownership in a “high risk” provider entity are required to undergo a fingerprint-based background investigation. – The IHCP will utilize Lexis. Nexis to provide fingerprint-based background investigation services. 44 Provider Enrollment and the ACA May 2012
Background Check Process – Disclosed individuals access the links on indianamedicaid. com to make arrangements for fingerprinting. – Disclosed individuals will make an appointment at a nearby collection site using the links on indianamedicaid. com. – Fingerprints are sent electronically to the Federal Bureau of Investigation (FBI) for processing. – The FBI will return the Criminal History Reports to the IHCP. – Each disclosed individual requiring fingerprinting will pay a separate $25. 00 administration fee to the fingerprint collection site. 45 Provider Enrollment and the ACA May 2012

Describe Application Fees
Fees – The CMS sets the application fee amount annually; the fee for 2012 is $523. – A $523 application fee will be collected from providers (as defined by CMS) that have not paid the application fee to Medicare, or who have not paid the fee to another state Medicaid program. – Out of state providers that enroll or revalidate with the IHCP must provide proof of payment of the application fee if paid to their state’s Medicaid program. – The application fee applies to newly enrolling and revalidating providers, entities executing a change of ownership, those adding or changing to a higher-risk specialty, and existing providers adding a new service location. 47 Provider Enrollment and the ACA May 2012
Fees – Application fee • Institutional providers will pay a fee to enroll in the Medicare or Medicaid programs. • Dually enrolled providers will pay the fee only to Medicare. • Medicaid-only providers will pay the fee to Medicaid. • Each service location must pay the fee upon enrolling and revalidating. • Review the Risk Category and Application Fee Matrix at http: //provider. indianamedicaid. com/media/27745/matrix. pdf to determine if an application fee is required for your provider type. • Payment methods include: − Check − Money order − Credit/debit card using HP Convenience Pay − Electronic check including Automated Clearing House (ACH) and electronic funds transfer (EFT) 48 Provider Enrollment and the ACA May 2012
Fees – The IHCP will use HP Convenience Pay to process credit/debit card payments of the application fee. – The Convenience Pay Services Client Access Portal provides authorized users with online, real-time access to ACH/EFT self-service capabilities. – HP Convenience Pay can be accessed via indianamedicaid. com or https: //www. paybill. com/Client. Access. Portal/Login. aspx. 49 Provider Enrollment and the ACA May 2012

Find Help Resources Available
Helpful Tools Avenues of resolution – Provider Enrollment page at indianamedicaid. com – HP Convenience Pay https: //www. paybill. com/Client. Acces s. Portal/Login. aspx – IHCP Provider Manual, Chapter 4 (Web, CD-ROM, or paper) – Provider Bulletin BT 201151 – Provider Enrollment Phone Line • 1 -877 -707 -5750 – Provider field consultant • 51 provider. indianamedicaid. com/contactus/provider-relations-field-consultants. aspx Provider Enrollment and the ACA May 2012
Q&A
4325d80557399e357b066c1a461ee1d9.ppt