aea775f6b6ea9bce1ab9a39c5cc24f91.ppt
- Количество слайдов: 25
Prostate probe with SPECT technique Workshop on endoscospic Imaging – Marseille – 13 -01 -2011 – F. Garibaldi ISS and INFN Roma 1 Ø the medical problem Ø the proposal Ø Ø Compton option Collimation techniques Si. PM/electronics Multimodality Ø summary and outlook 1
Compton Camera Applications to Bio-medical Imaging (Mattinata 5 -7 September 2002) Stem cell workshop – Marseille - December 2008 -Topical Symposium on Advanced molecular intraoperative probes assisting surgical interventions - TOF PET workshop Baia delle Zagare September 2009 next ?
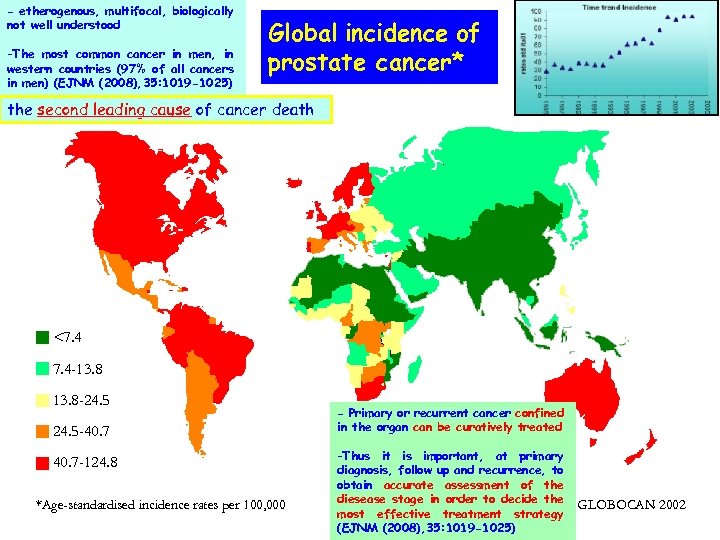
- etherogenous, multifocal, biologically not well understood -The most common cancer in men, in western countries (97% of all cancers in men) (EJNM (2008), 35: 1019 -1025) Global incidence of prostate cancer* the second leading cause of cancer death <7. 4 -13. 8 -24. 5 -40. 7 -124. 8 *Age-standardised incidence rates per 100, 000 - Primary or recurrent cancer confined in the organ can be curatively treated -Thus it is important, at primary diagnosis, follow up and recurrence, to obtain accurate assessment of the diesease stage in order to decide the most effective treatment strategy (EJNM (2008), 35: 1019 -1025) GLOBOCAN 2002
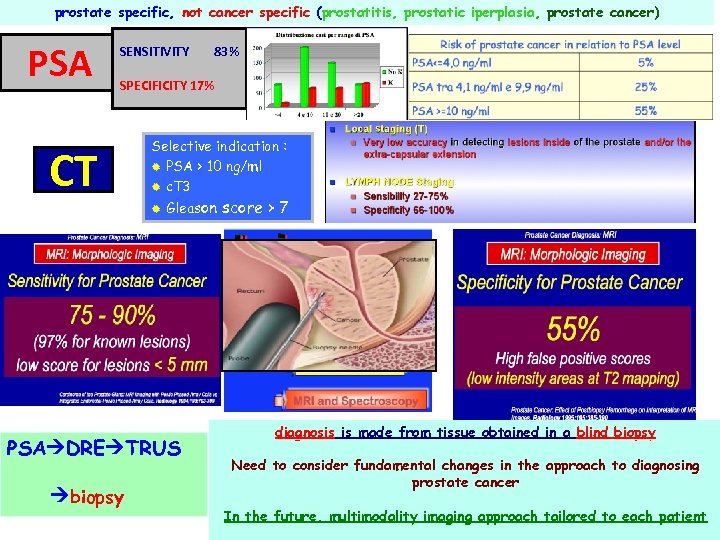
prostate specific, not cancer specific (prostatitis, prostatic iperplasia, prostate cancer) PSA SENSITIVITY 83% SPECIFICITY 17% CT Selective indication : ® PSA > 10 ng/ml ® c. T 3 ® Gleason PSA DRE TRUS biopsy score > 7 diagnosis is made from tissue obtained in a blind biopsy Need to consider fundamental changes in the approach to diagnosing prostate cancer In the future, multimodality imaging approach tailored to each patient
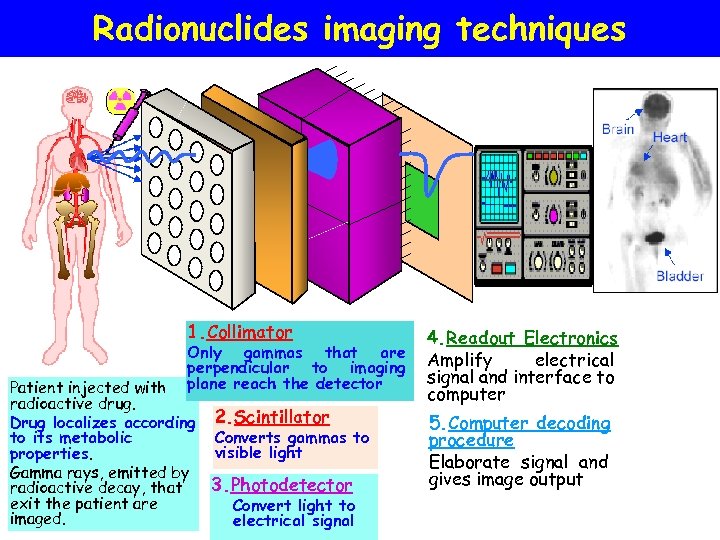
Radionuclides imaging techniques 1. Collimator Only gammas that are perpendicular to imaging plane reach the detector Patient injected with radioactive drug. Drug localizes according 2. Scintillator Converts gammas to to its metabolic visible light properties. Gamma rays, emitted by 3. Photodetector radioactive decay, that exit the patient are Convert light to imaged. electrical signal 4. Readout Electronics Amplify electrical signal and interface to computer 5. Computer decoding procedure Elaborate signal and gives image output
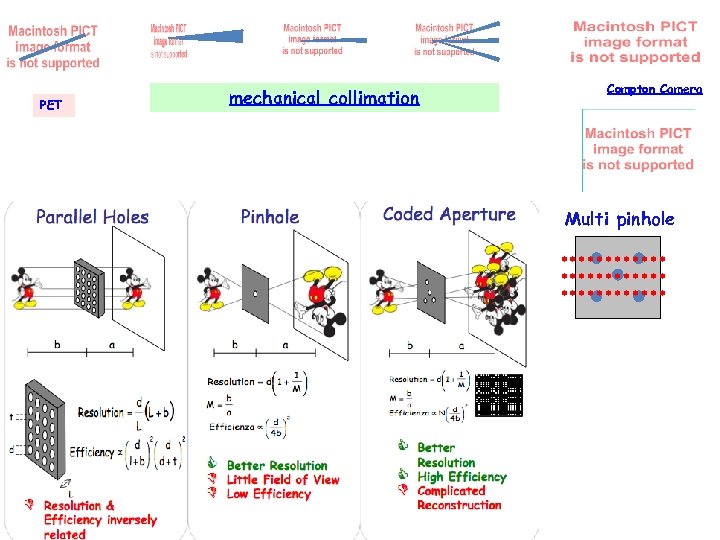
PET mechanical collimation Compton Camera Multi pinhole
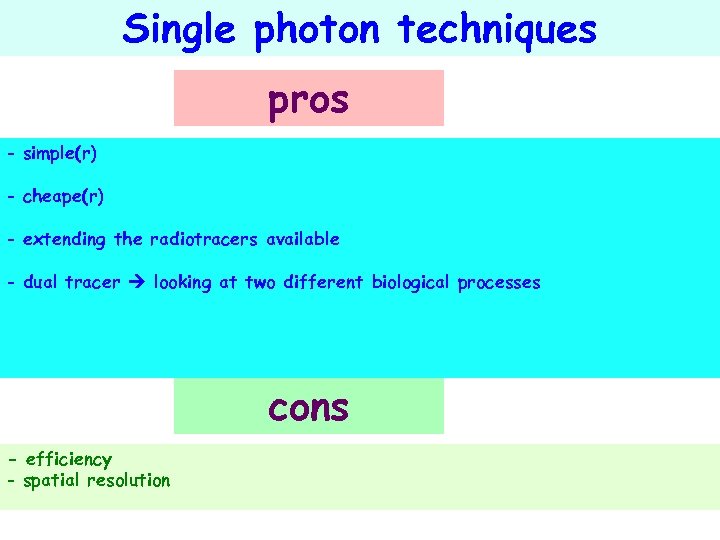
Single photon techniques pros - simple(r) - cheape(r) - extending the radiotracers available - dual tracer looking at two different biological processes cons - efficiency - spatial resolution
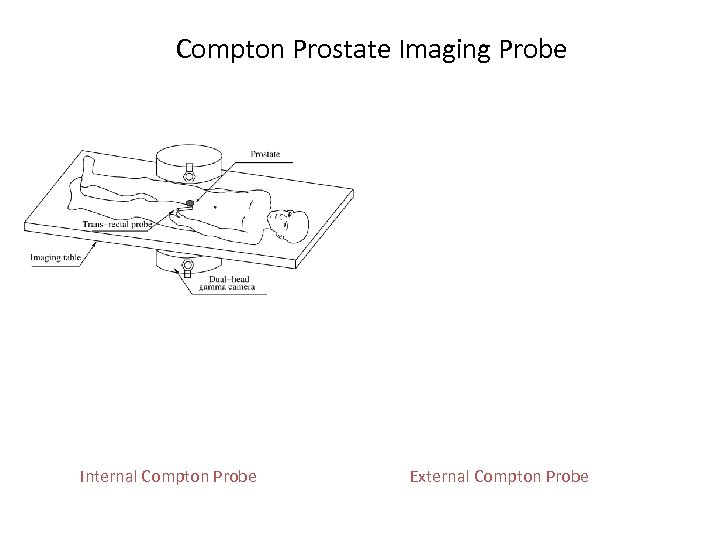
Compton Prostate Imaging Probe Internal Compton Probe External Compton Probe
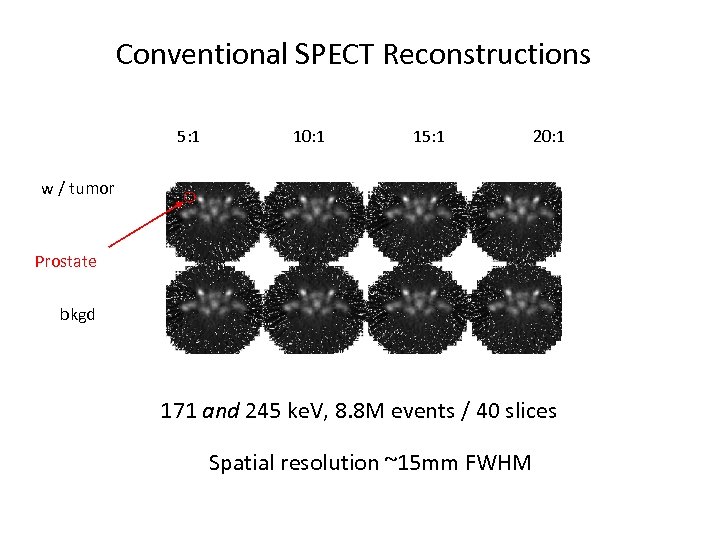
Conventional SPECT Reconstructions 5: 1 10: 1 15: 1 20: 1 w / tumor Prostate bkgd 171 and 245 ke. V, 8. 8 M events / 40 slices Spatial resolution ~15 mm FWHM
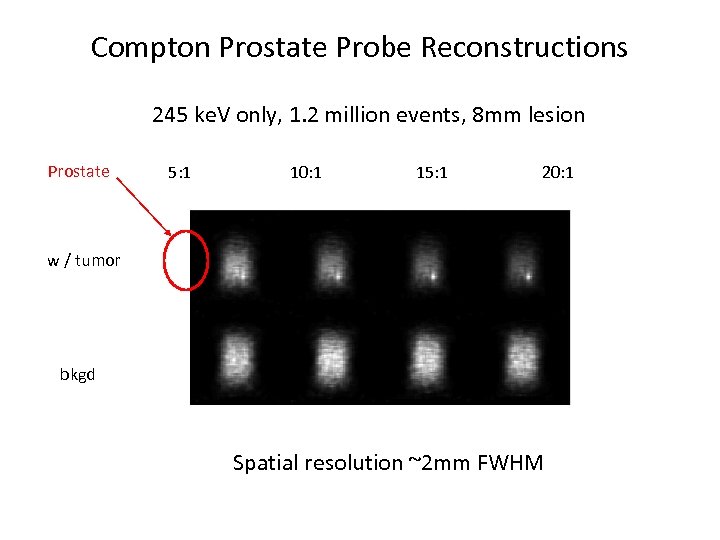
Compton Prostate Probe Reconstructions 245 ke. V only, 1. 2 million events, 8 mm lesion Prostate 5: 1 10: 1 15: 1 20: 1 w / tumor bkgd Spatial resolution ~2 mm FWHM
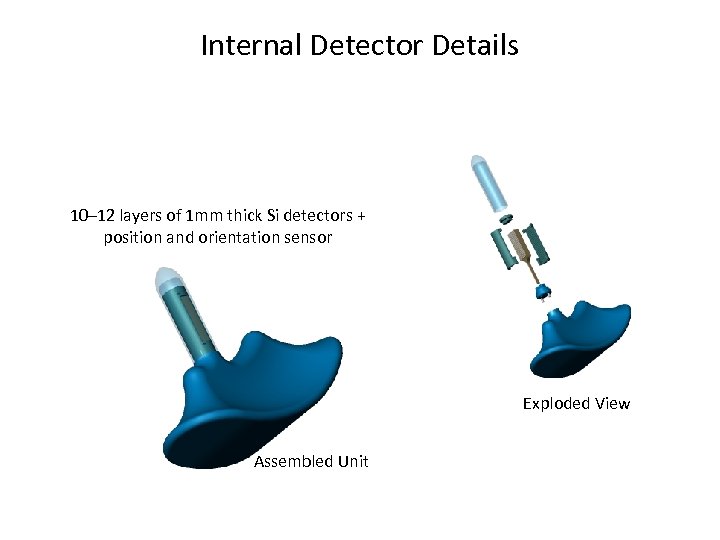
Internal Detector Details 10– 12 layers of 1 mm thick Si detectors + position and orientation sensor Exploded View Assembled Unit
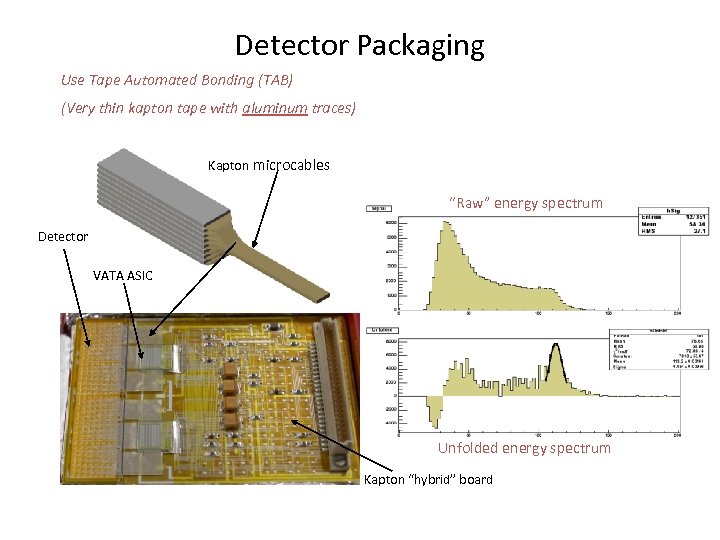
Detector Packaging Use Tape Automated Bonding (TAB) (Very thin kapton tape with aluminum traces) Kapton microcables “Raw” energy spectrum Detector VATA ASIC Unfolded energy spectrum Kapton “hybrid” board
Demise of the Compton Prostate Probe • Decreasing interest in imaging single photon agents • “Coincidence” PET cameras not reimbursed by HCFA • Technology ultimately was a bit far off
Single photon Compton camera ( N. Clinthorne. Michigan )
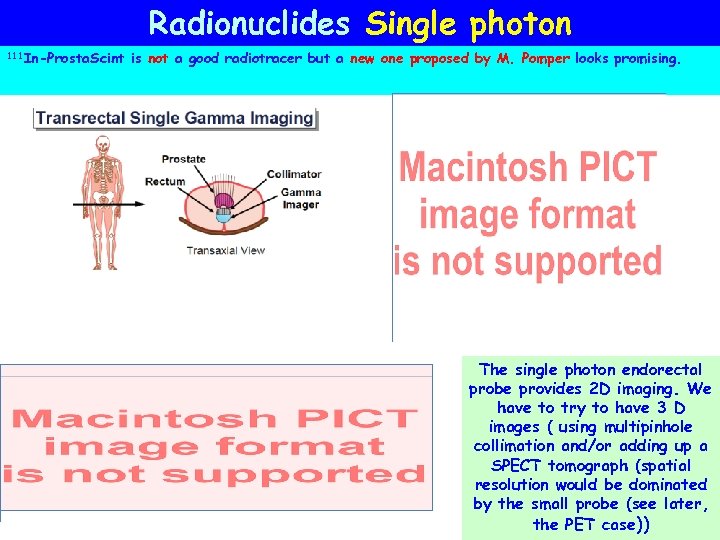
Radionuclides Single photon 111 In-Prosta. Scint is not a good radiotracer but a new one proposed by M. Pomper looks promising. The single photon endorectal probe provides 2 D imaging. We have to try to have 3 D images ( using multipinhole collimation and/or adding up a SPECT tomograph (spatial resolution would be dominated by the small probe (see later, the PET case))
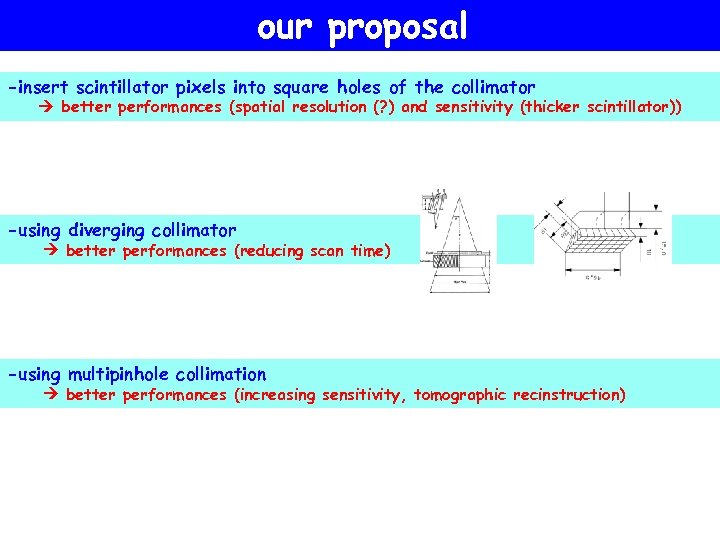
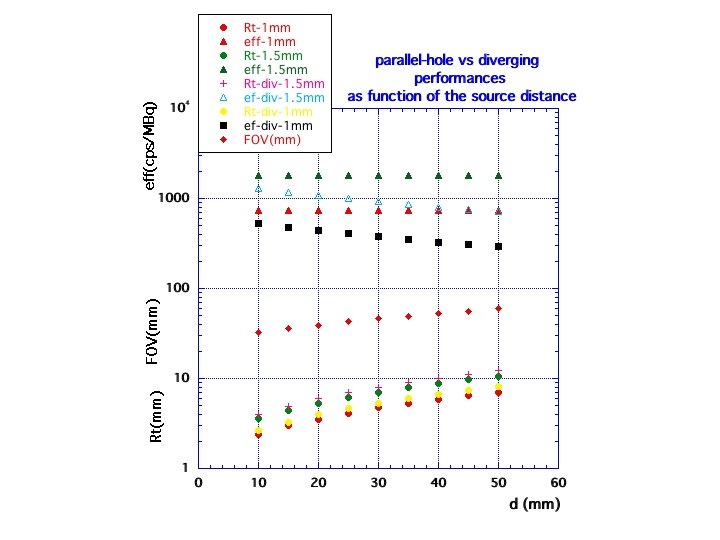
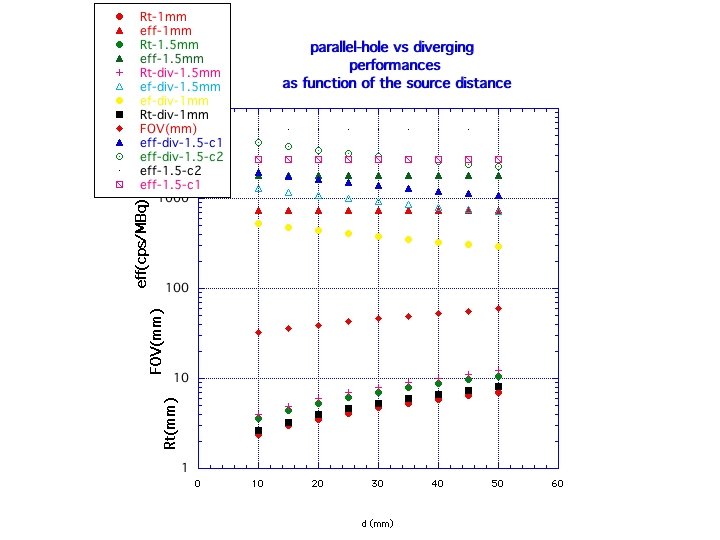
our proposal -insert scintillator pixels into square holes of the collimator better performances (spatial resolution (? ) and sensitivity (thicker scintillator)) -using diverging collimator better performances (reducing scan time) -using multipinhole collimation better performances (increasing sensitivity, tomographic recinstruction)
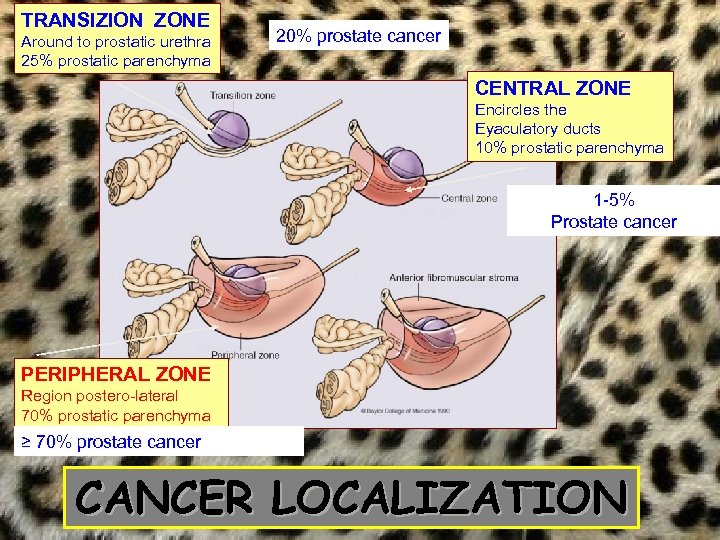
TRANSIZION ZONE Around to prostatic urethra 25% prostatic parenchyma 20% prostate cancer CENTRAL ZONE Encircles the Eyaculatory ducts 10% prostatic parenchyma 1 -5% Prostate cancer PERIPHERAL ZONE Region postero-lateral 70% prostatic parenchyma ≥ 70% prostate cancer CANCER LOCALIZATION
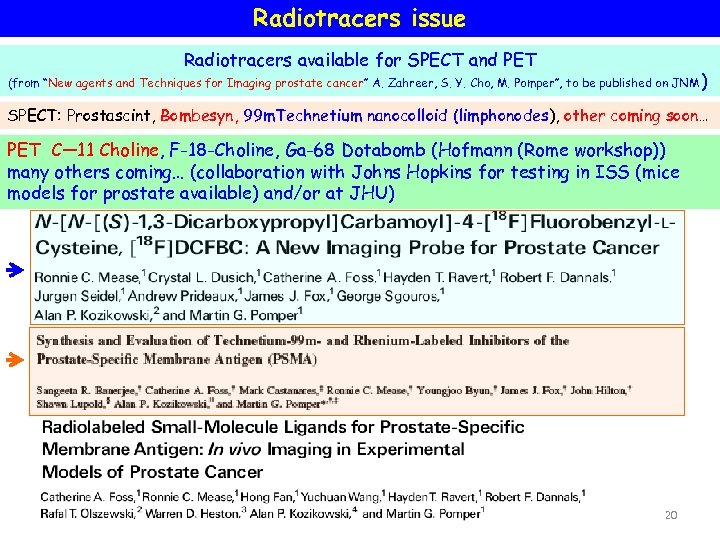
Radiotracers issue Radiotracers available for SPECT and PET (from “New agents and Techniques for Imaging prostate cancer” A. Zahreer, S. Y. Cho, M. Pomper”, to be published on JNM ) SPECT: Prostascint, Bombesyn, 99 m. Technetium nanocolloid (limphonodes), other coming soon… PET C— 11 Choline, F-18 -Choline, Ga-68 Dotabomb (Hofmann (Rome workshop)) many others coming… (collaboration with Johns Hopkins for testing in ISS (mice models for prostate available) and/or at JHU) 20
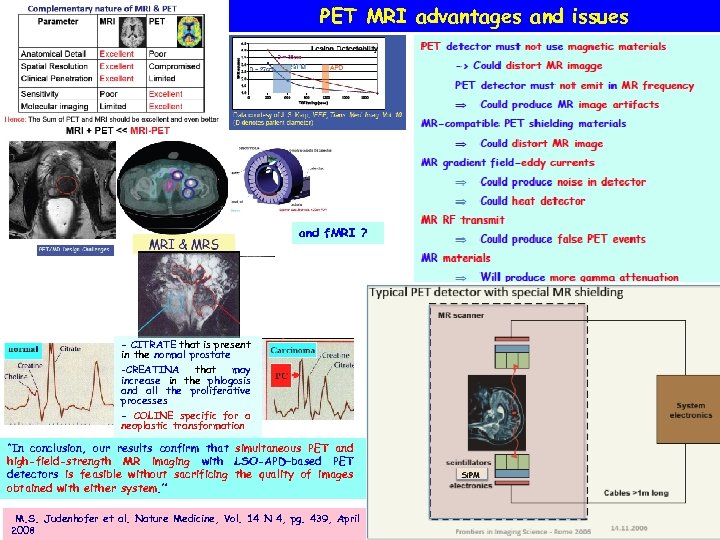
PET MRI advantages and issues and f. MRI ? - CITRATE that is present in the normal prostate -CREATINA that may increase in the phlogosis and all the proliferative processes - COLINE specific for a neoplastic transformation “In conclusion, our results confirm that simultaneous PET and high-field-strength MR imaging with LSO-APD–based PET detectors is feasible without sacrificing the quality of images obtained with either system. ” M. S. Judenhofer et al. Nature Medicine, Vol. 14 N 4, pg. 439, April 2008
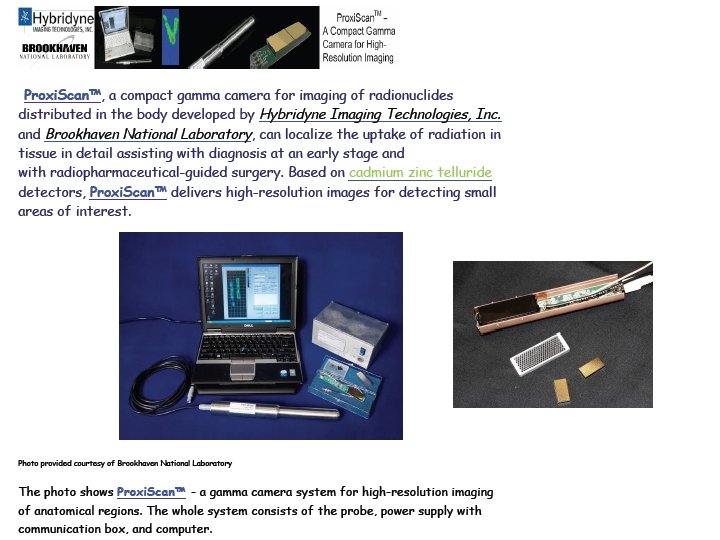
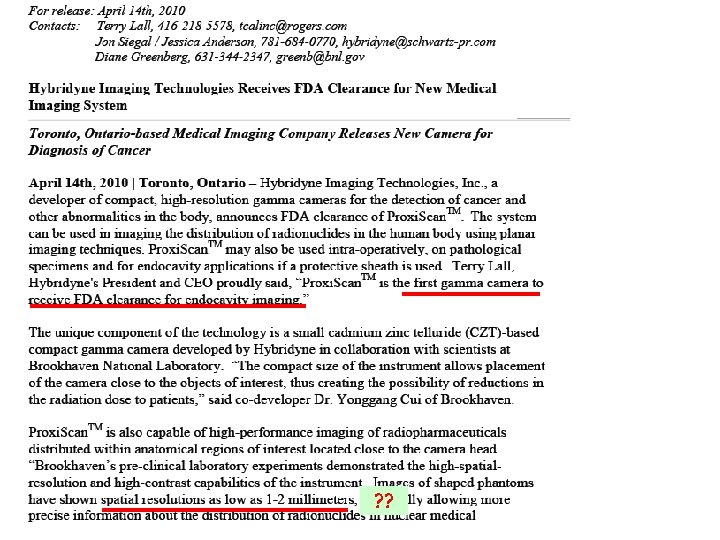
? ?
Summary and Conclusions - prostate cancer detection, diagnosis and staging very difficult - standard imaging systems suffer from VERY low specificity - better radiotracers + multimodality can be the solution - single photon techniques are an option because - simpler and cheaper than PET - dual tracer - multimodality with MRI possible - FDA approved for tests on humans - better radiotarcers coming soon - Using also an external SPECT? - Prospectives: Compton
aea775f6b6ea9bce1ab9a39c5cc24f91.ppt