PROPHYLAXIS AND TREATMENT FOR ONCO-HEMATOLOGICAL PATIENTS DURING CHEMOTHERAPY-INDUCED

![Neutropenia, particularly severe neutropenia (counts 500 neutrophils/ L [0. 5 x 10 9/L]), increases Neutropenia, particularly severe neutropenia (counts 500 neutrophils/ L [0. 5 x 10 9/L]), increases](http://present5.com/presentforday2/20170213/neytropenii_2017_images/neytropenii_2017_4.jpg)


neytropenii_2017.pptx
- Размер: 9.6 Мб
- Автор:
- Количество слайдов: 38
Описание презентации PROPHYLAXIS AND TREATMENT FOR ONCO-HEMATOLOGICAL PATIENTS DURING CHEMOTHERAPY-INDUCED по слайдам
 PROPHYLAXIS AND TREATMENT FOR ONCO-HEMATOLOGICAL PATIENTS DURING CHEMOTHERAPY-INDUCED NEUTROPENIA Irina Belyavskaya, 2206 The pediatric faculty. Belarusian State Medical University
PROPHYLAXIS AND TREATMENT FOR ONCO-HEMATOLOGICAL PATIENTS DURING CHEMOTHERAPY-INDUCED NEUTROPENIA Irina Belyavskaya, 2206 The pediatric faculty. Belarusian State Medical University
 • To review the publications about the infections in hematological patients during chemotherapy-induced neutropenia. Objectives • We analyzed scientific articles on the topic of the characteristics, hygiene care, isolation of patients, prophylactic use of antibacterial, antifungal and antiviral drugs. Materials and methods
• To review the publications about the infections in hematological patients during chemotherapy-induced neutropenia. Objectives • We analyzed scientific articles on the topic of the characteristics, hygiene care, isolation of patients, prophylactic use of antibacterial, antifungal and antiviral drugs. Materials and methods
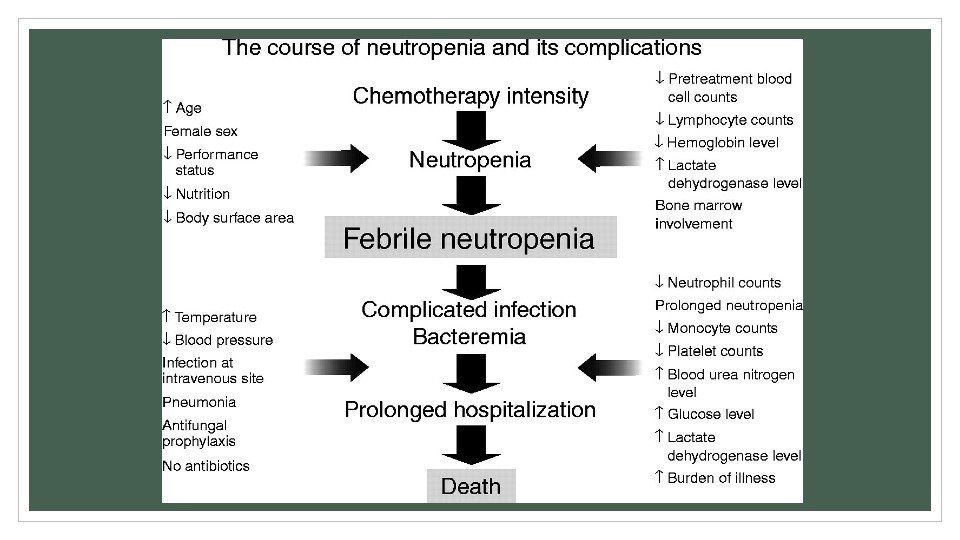
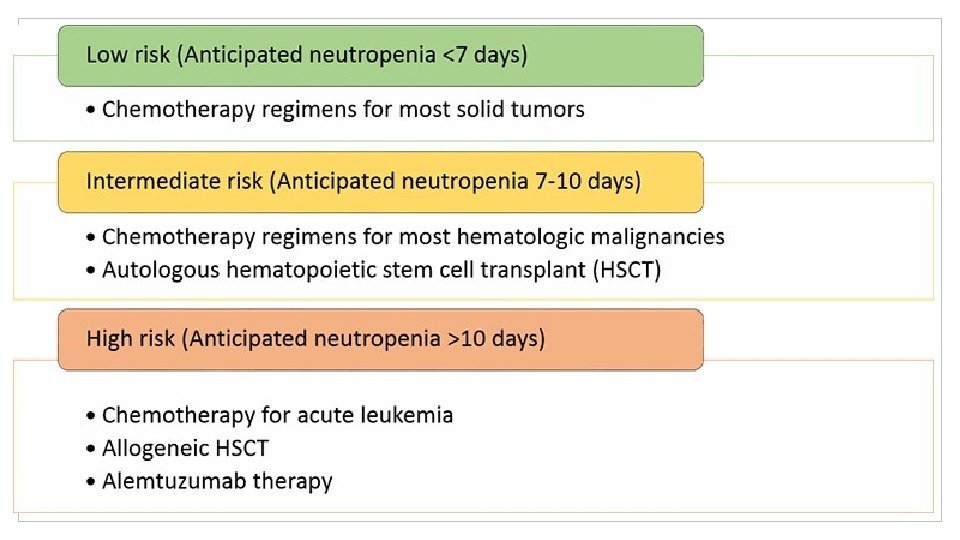
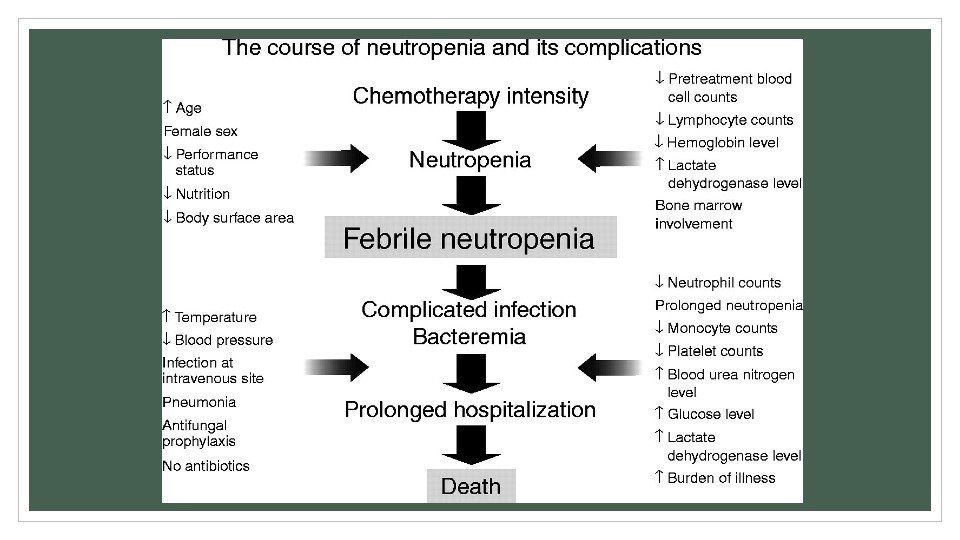
 • Neutropenia is one of the commonest complications of cytotoxic chemotherapy in patients with hematologic malignancies. Patients with hematological and oncological diseases are at increased risk for bacterial infections and pneumonia caused by Pneumocystis jirovecii (PCP) because of their disease-related and therapy-induced immunosuppression. As infections are the leading cause for non-relapse mortality, broad-spectrum antibiotic therapy is introduced as soon as an infectious problem is suspected. Introduction
• Neutropenia is one of the commonest complications of cytotoxic chemotherapy in patients with hematologic malignancies. Patients with hematological and oncological diseases are at increased risk for bacterial infections and pneumonia caused by Pneumocystis jirovecii (PCP) because of their disease-related and therapy-induced immunosuppression. As infections are the leading cause for non-relapse mortality, broad-spectrum antibiotic therapy is introduced as soon as an infectious problem is suspected. Introduction
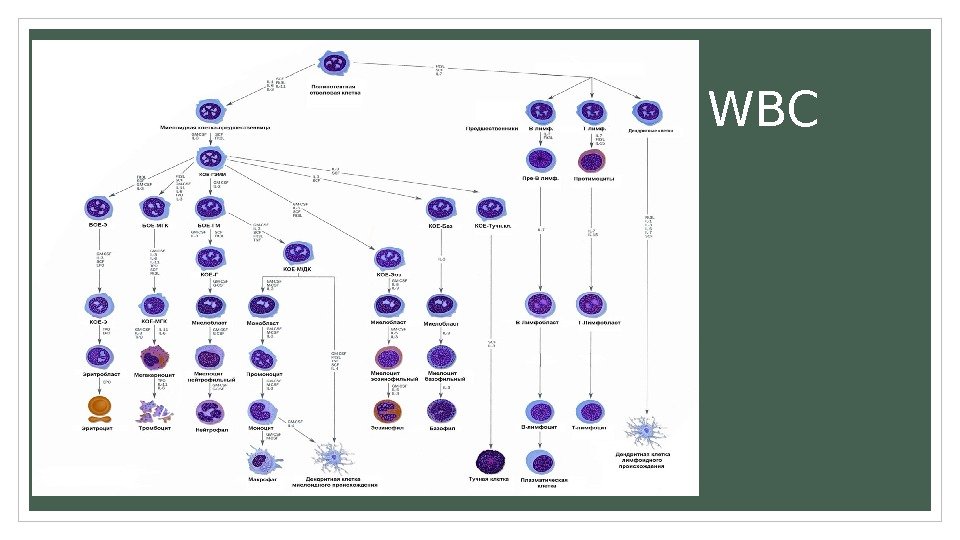
 W
W
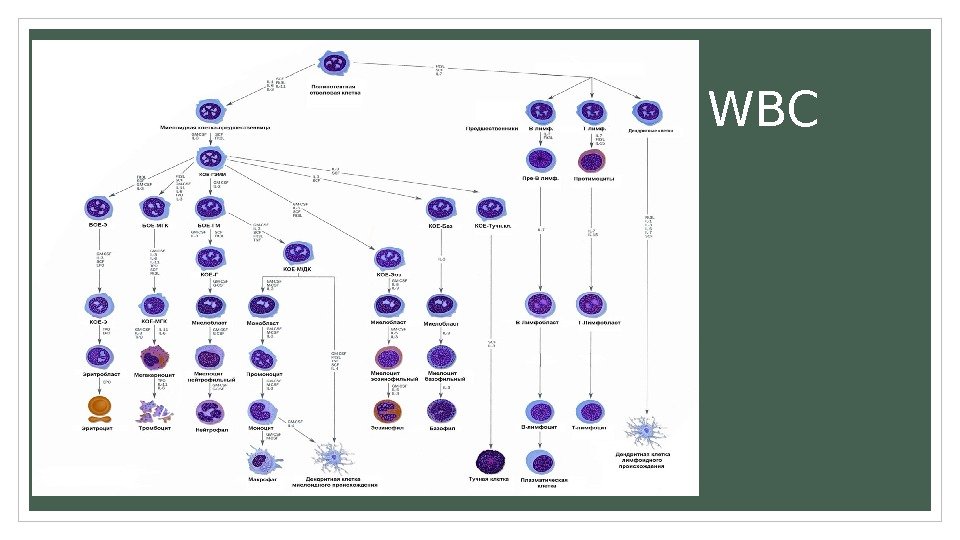
![Neutropenia, particularly severe neutropenia (counts 500 neutrophils/ L [0. 5 x 10 9/L]), increases Neutropenia, particularly severe neutropenia (counts 500 neutrophils/ L [0. 5 x 10 9/L]), increases](http://present5.com/presentforday2/20170213/neytropenii_2017_images/neytropenii_2017_4.jpg) Neutropenia, particularly severe neutropenia (counts <500 neutrophils/ L [0. 5 x 10 9/L]), increases susceptibility to bacterial or fungal infections and impairs the resolution of these infections. For individuals older than age 10 years, neutropenia is defined as a count less than approximately 1. 8 x 10 3 / L(1. 8 x 10 9 /L. Individuals with neutrophil counts of 1. 0 to 1. 8 x 10 3 / L (1. 0– 1. 8 x 10 9 /L) are at little risk of infection. In general, neutrophil counts between 0. 5 x 10 3 / L and 1. 0 x 10 3 / L (0. 5– 1. 0 x 10 9 /L) are associated with only slight risk of infection unless other contributing factors are present. Individuals with neutrophil counts less than 0. 5 x 10 3 / L (0. 5 x 10 9 /L) are at substantially greater risk, but the frequency of infections varies considerably, depending on the cause and duration of neutropenia. Other factors, such as the integrity of the skin and mucous membranes, the vascular supply to tissues, and the nutritional status of the patient, also influence the risk of infections. Neutropenia remains a prevalent problem associated with substantial morbidity, mortality and costs. The degree and duration of the neutropenia determine the risk of infection.
Neutropenia, particularly severe neutropenia (counts <500 neutrophils/ L [0. 5 x 10 9/L]), increases susceptibility to bacterial or fungal infections and impairs the resolution of these infections. For individuals older than age 10 years, neutropenia is defined as a count less than approximately 1. 8 x 10 3 / L(1. 8 x 10 9 /L. Individuals with neutrophil counts of 1. 0 to 1. 8 x 10 3 / L (1. 0– 1. 8 x 10 9 /L) are at little risk of infection. In general, neutrophil counts between 0. 5 x 10 3 / L and 1. 0 x 10 3 / L (0. 5– 1. 0 x 10 9 /L) are associated with only slight risk of infection unless other contributing factors are present. Individuals with neutrophil counts less than 0. 5 x 10 3 / L (0. 5 x 10 9 /L) are at substantially greater risk, but the frequency of infections varies considerably, depending on the cause and duration of neutropenia. Other factors, such as the integrity of the skin and mucous membranes, the vascular supply to tissues, and the nutritional status of the patient, also influence the risk of infections. Neutropenia remains a prevalent problem associated with substantial morbidity, mortality and costs. The degree and duration of the neutropenia determine the risk of infection.
 Signs and symptoms Common presenting symptoms of neutropenia include the following: Low-grade fever Sore mouth Odynophagia Gingival pain and swelling Skin abscesses Recurrent sinusitis and otitis Symptoms of pneumonia (eg, cough, dyspnea) Perirectal pain and irritation
Signs and symptoms Common presenting symptoms of neutropenia include the following: Low-grade fever Sore mouth Odynophagia Gingival pain and swelling Skin abscesses Recurrent sinusitis and otitis Symptoms of pneumonia (eg, cough, dyspnea) Perirectal pain and irritation
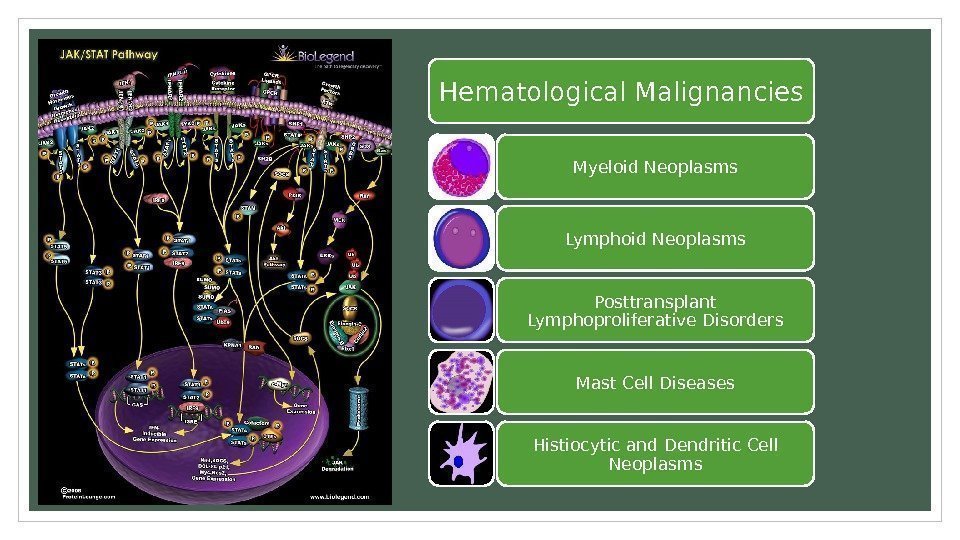 Hematological Malignancies Myeloid Neoplasms Lymphoid Neoplasms Posttransplant Lymphoproliferative Disorders Mast Cell Diseases Histiocytic and Dendritic Cell Neoplasms
Hematological Malignancies Myeloid Neoplasms Lymphoid Neoplasms Posttransplant Lymphoproliferative Disorders Mast Cell Diseases Histiocytic and Dendritic Cell Neoplasms
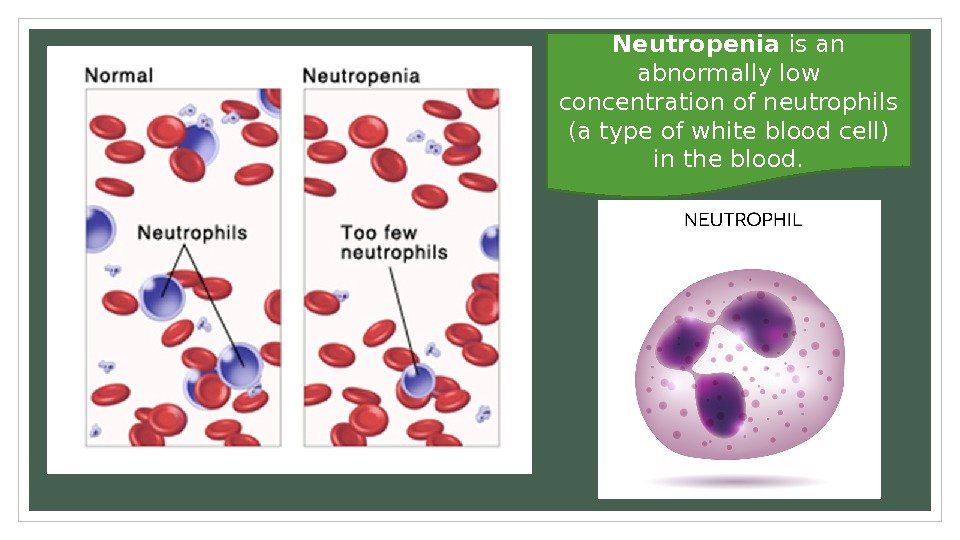
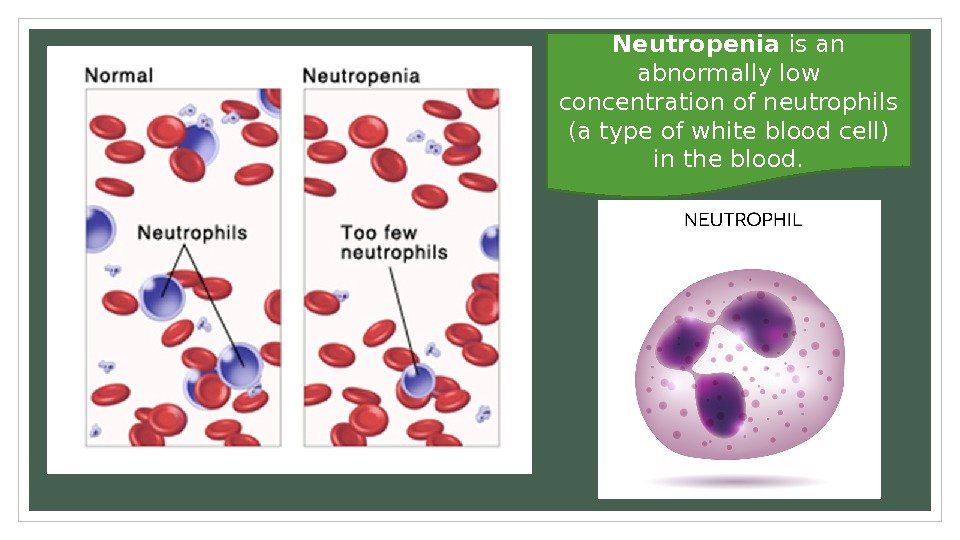 Neutropenia is an abnormally low concentration of neutrophils (a type of white blood cell) in the blood.
Neutropenia is an abnormally low concentration of neutrophils (a type of white blood cell) in the blood.
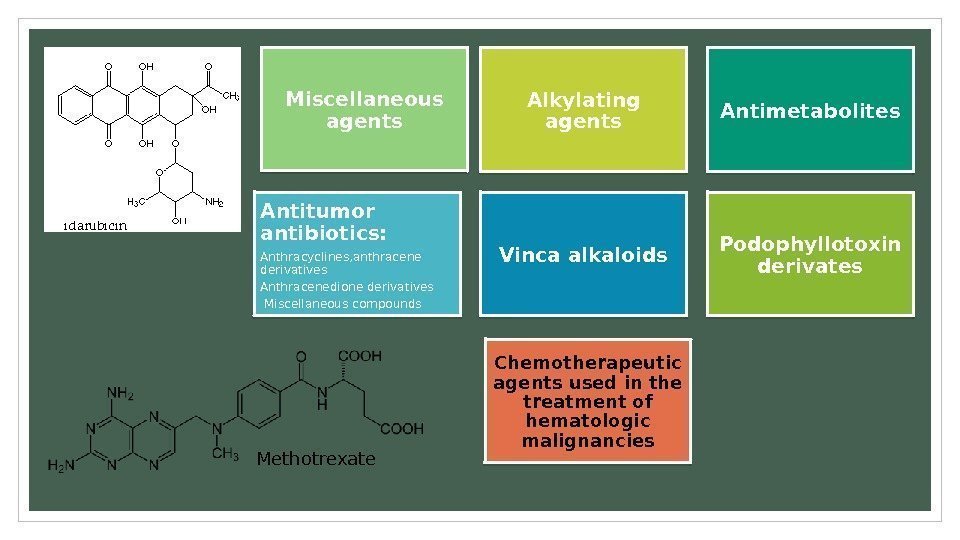
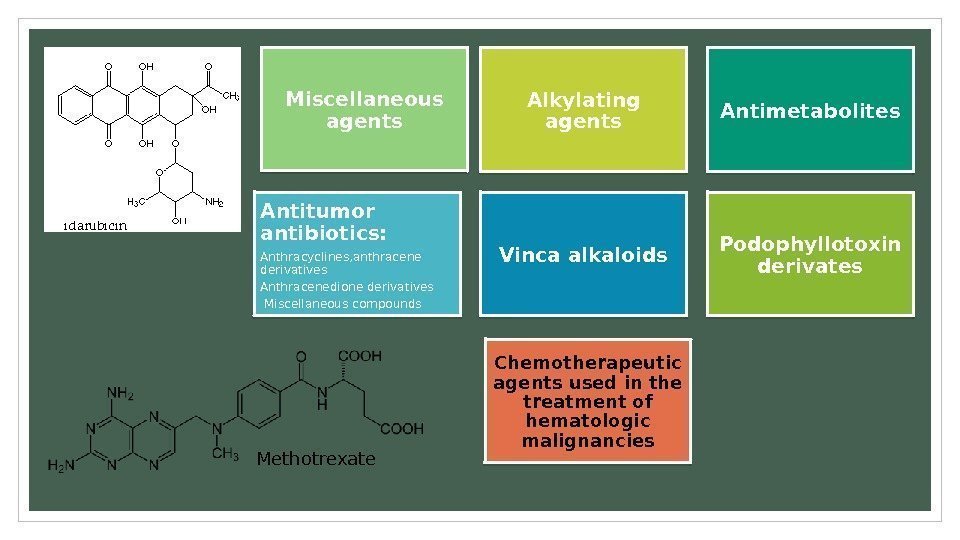 Chemotherapeutic agents used in the treatment of hematologic malignancies Alkylating agents Antimetabolites Antitumor antibiotics: Anthracyclines, anthracene derivatives Anthracenedione derivatives Miscellaneous compounds Vinca alkaloids Podophyllotoxin derivates. Miscellaneous agents Methotrexate
Chemotherapeutic agents used in the treatment of hematologic malignancies Alkylating agents Antimetabolites Antitumor antibiotics: Anthracyclines, anthracene derivatives Anthracenedione derivatives Miscellaneous compounds Vinca alkaloids Podophyllotoxin derivates. Miscellaneous agents Methotrexate
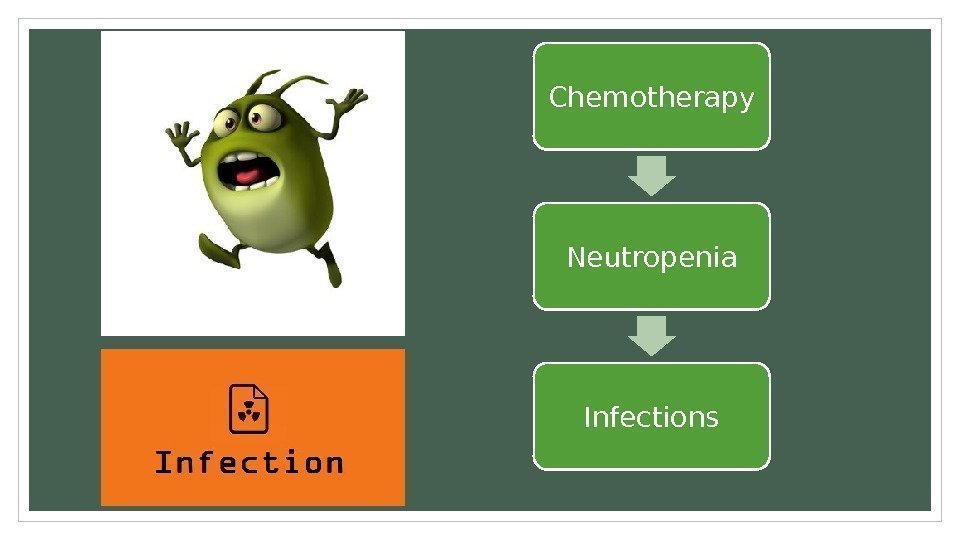
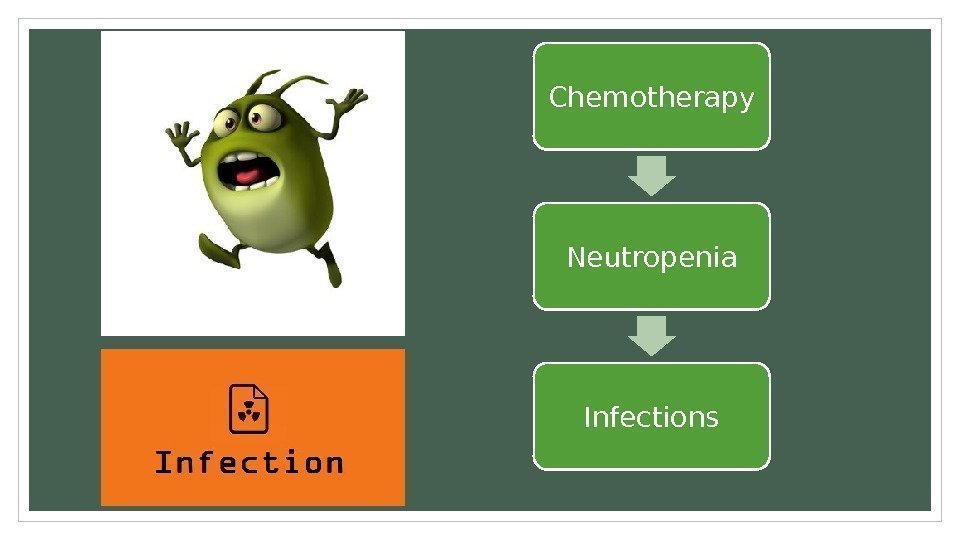 Chemotherapy Neutropenia Infections
Chemotherapy Neutropenia Infections
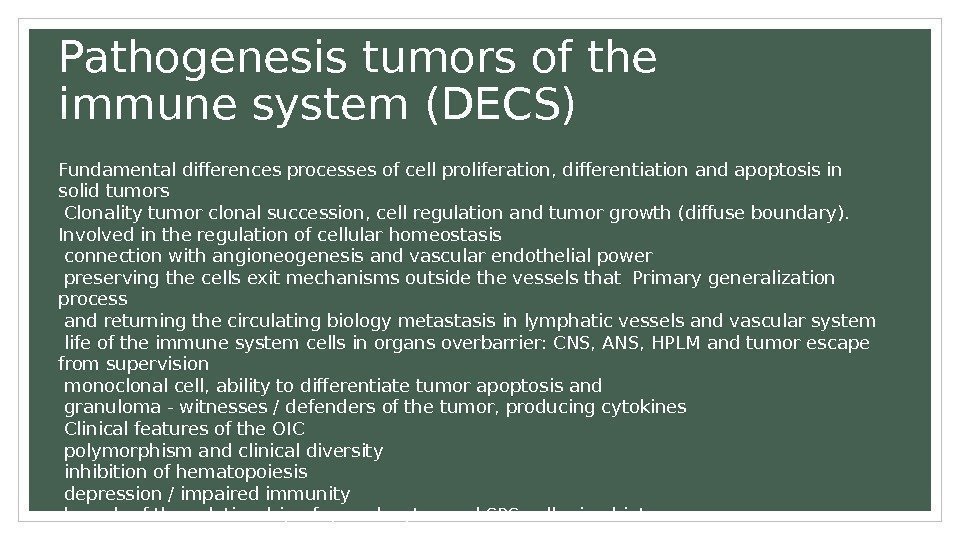 Pathogenesis tumors of the immune system (DECS) Fundamental differences processes of cell proliferation, differentiation and apoptosis in solid tumors Clonality tumor clonal succession, cell regulation and tumor growth (diffuse boundary). Involved in the regulation of cellular homeostasis connection with angioneogenesis and vascular endothelial power preserving the cells exit mechanisms outside the vessels that Primary generalization process and returning the circulating biology metastasis in lymphatic vessels and vascular system life of the immune system cells in organs overbarrier: CNS, ANS, HPLM and tumor escape from supervision monoclonal cell, ability to differentiate tumor apoptosis and granuloma — witnesses / defenders of the tumor, producing cytokines Clinical features of the OIC polymorphism and clinical diversity inhibition of hematopoiesis depression / impaired immunity breach of the relationship of granulocytes and SPS cell microbiota
Pathogenesis tumors of the immune system (DECS) Fundamental differences processes of cell proliferation, differentiation and apoptosis in solid tumors Clonality tumor clonal succession, cell regulation and tumor growth (diffuse boundary). Involved in the regulation of cellular homeostasis connection with angioneogenesis and vascular endothelial power preserving the cells exit mechanisms outside the vessels that Primary generalization process and returning the circulating biology metastasis in lymphatic vessels and vascular system life of the immune system cells in organs overbarrier: CNS, ANS, HPLM and tumor escape from supervision monoclonal cell, ability to differentiate tumor apoptosis and granuloma — witnesses / defenders of the tumor, producing cytokines Clinical features of the OIC polymorphism and clinical diversity inhibition of hematopoiesis depression / impaired immunity breach of the relationship of granulocytes and SPS cell microbiota
 Tumors of the hematopoietic and immune system a unique model of cancer Tumors of the hematopoietic and immune systems (disturbance of cellular homeostasis and transport support UK all organs and tissues) — 50% of children and 10% adults. Tumors of the central and peripheral nervous system — 25% of children and 10% of adults. Mutational incident in utero children development and evolution of tumors on the basis of genetic and biological defects, IDS and bone marrow failure syndromes. Sidney Farber (1947), the evolution of chemotherapy and ideology treatment technologies — molecular biological approach scientifically sound selection targentnoy therapy.
Tumors of the hematopoietic and immune system a unique model of cancer Tumors of the hematopoietic and immune systems (disturbance of cellular homeostasis and transport support UK all organs and tissues) — 50% of children and 10% adults. Tumors of the central and peripheral nervous system — 25% of children and 10% of adults. Mutational incident in utero children development and evolution of tumors on the basis of genetic and biological defects, IDS and bone marrow failure syndromes. Sidney Farber (1947), the evolution of chemotherapy and ideology treatment technologies — molecular biological approach scientifically sound selection targentnoy therapy.
 Concept and a new direction of scientific and practical medicine Interdisciplinary integration of hematology, oncology and immunology in the ontogeny of the human identified a number of general biological processes: Insurance, GSK, differentiation, proliferation (cloning), intercellular communication (autovospalenie), death (apoptosis, necrosis). Cellular homeostasis — the central regulatory system of the organism and its connection with the known regulation systems (. The nervous, endocrine, etc. ) will fundamentally change the pathogenesis and treatment of major human diseases. Genetic defects, infection and tumor cell homeostasis regulators underlie human disease phenotype Advancing the value of production of new knowledge in the field of cellular homeostasis as the scientific basis of cellular technologies (in 2014 included> 2000 qualifier diseases in IDS). The development of new diagnostic techniques and treatment of patients, prevention of genetic, immune, haematological and oncological diseases requires reliable scientific knowledge and methods of evidence-based medicine.
Concept and a new direction of scientific and practical medicine Interdisciplinary integration of hematology, oncology and immunology in the ontogeny of the human identified a number of general biological processes: Insurance, GSK, differentiation, proliferation (cloning), intercellular communication (autovospalenie), death (apoptosis, necrosis). Cellular homeostasis — the central regulatory system of the organism and its connection with the known regulation systems (. The nervous, endocrine, etc. ) will fundamentally change the pathogenesis and treatment of major human diseases. Genetic defects, infection and tumor cell homeostasis regulators underlie human disease phenotype Advancing the value of production of new knowledge in the field of cellular homeostasis as the scientific basis of cellular technologies (in 2014 included> 2000 qualifier diseases in IDS). The development of new diagnostic techniques and treatment of patients, prevention of genetic, immune, haematological and oncological diseases requires reliable scientific knowledge and methods of evidence-based medicine.
 Preparation of cell concentrate to freezing
Preparation of cell concentrate to freezing
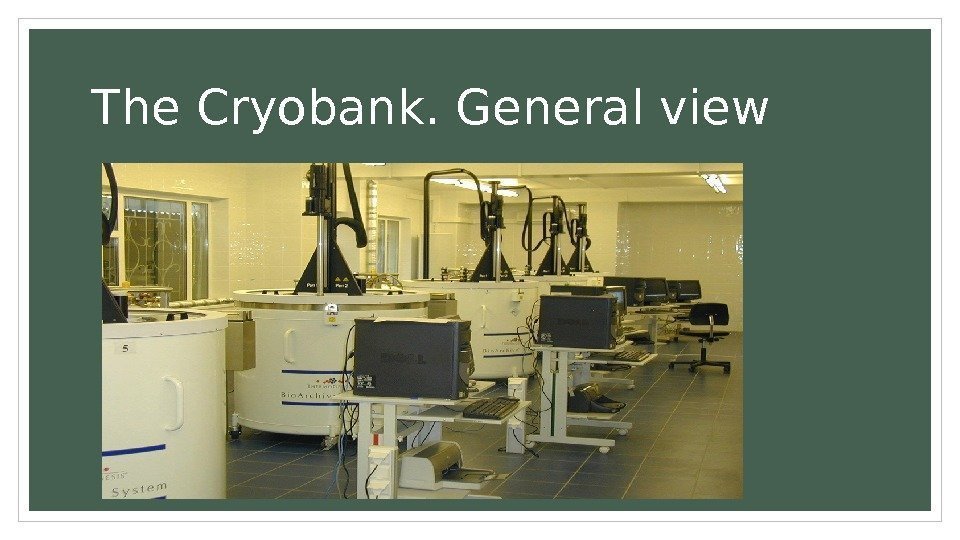
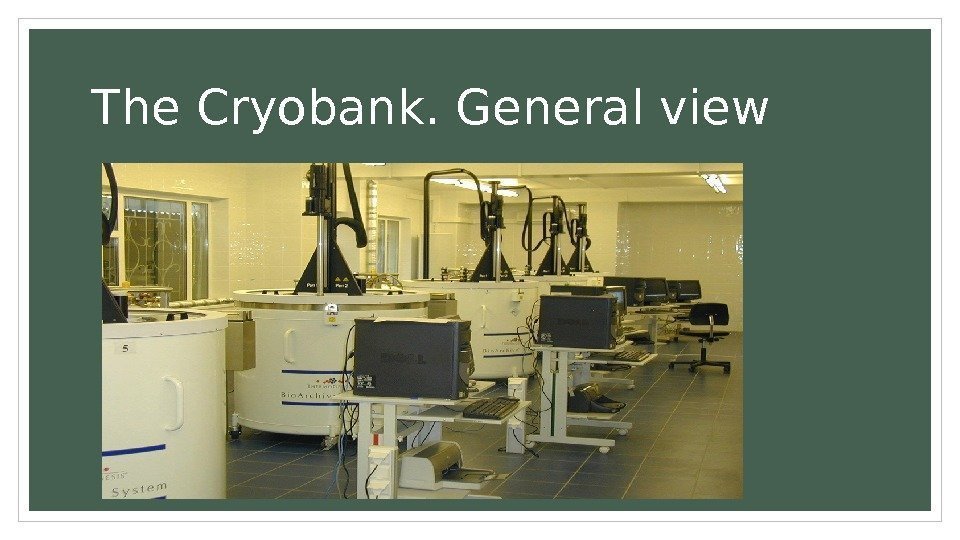 The Cryobank. General view
The Cryobank. General view
 Induction of tumor growth or protective effect? -Increase The frequency of occurrence mikrohimernyh fetal cells in tumor tissues -Tsirkuliruyuschie Mikrohimernye occur in cells 2 -4 times less in comparison with healthy women (48 -56%) (Gadi and Nelson, 2007; Gadi et al, 2008). Breast (11 -26%) of patients with cancer. -Vstrechaemost Mikrohimernyh cells in tumor tissue in melanoma — 62% against 12% in benign nevi Is to prove the effect of «graft-versus-tumor» in the transfusion of stem woman baby cells with fetal microchimerism (Tokita et al. , Gadi et al).
Induction of tumor growth or protective effect? -Increase The frequency of occurrence mikrohimernyh fetal cells in tumor tissues -Tsirkuliruyuschie Mikrohimernye occur in cells 2 -4 times less in comparison with healthy women (48 -56%) (Gadi and Nelson, 2007; Gadi et al, 2008). Breast (11 -26%) of patients with cancer. -Vstrechaemost Mikrohimernyh cells in tumor tissue in melanoma — 62% against 12% in benign nevi Is to prove the effect of «graft-versus-tumor» in the transfusion of stem woman baby cells with fetal microchimerism (Tokita et al. , Gadi et al).
 The possible contribution of microchimerism in oncogenesis POSSIBLE MECHANISMS OF INDUCTION OF TUMORS IN THE FETUS/CHILD Change immune surveillance: Maternal microchimerism is detected in 1/3 of the women in the cells involved in the innate and adaptive immunity (T and b-lymphocytes, NK-cells, macrophages)
The possible contribution of microchimerism in oncogenesis POSSIBLE MECHANISMS OF INDUCTION OF TUMORS IN THE FETUS/CHILD Change immune surveillance: Maternal microchimerism is detected in 1/3 of the women in the cells involved in the innate and adaptive immunity (T and b-lymphocytes, NK-cells, macrophages)
 The influence of maternal illness on the fetus and newborn States that existed before pregnancy SLE. Cage SLE first discovered in 1965 in a newborn to mothers with SLE newborns manifests AIHA, thrombocytopenia and neutropenia. Characteristic signs — congenital heart block, congestive pericarditis, hepatosplenomegaly. Symptomatic therapy. Leukemia. > 400 descriptions and experience Hematology Research Center, no cases of induction in the fetus and child. Crayfish. Described metastases in the fetus in melanoma and breast cancer in mother. The defeat of the fetus never develops without defeat placenta
The influence of maternal illness on the fetus and newborn States that existed before pregnancy SLE. Cage SLE first discovered in 1965 in a newborn to mothers with SLE newborns manifests AIHA, thrombocytopenia and neutropenia. Characteristic signs — congenital heart block, congestive pericarditis, hepatosplenomegaly. Symptomatic therapy. Leukemia. > 400 descriptions and experience Hematology Research Center, no cases of induction in the fetus and child. Crayfish. Described metastases in the fetus in melanoma and breast cancer in mother. The defeat of the fetus never develops without defeat placenta
 Intrauterine infection with hematological manifestations Toxoplasmosis Syphilis Rubella Cytomegalovirus infection Infection caused by the herpes virus I The infection is caused by the VZ virus Enteroviral infections (Coxsackie, echo) Parvovirus infection HIV
Intrauterine infection with hematological manifestations Toxoplasmosis Syphilis Rubella Cytomegalovirus infection Infection caused by the herpes virus I The infection is caused by the VZ virus Enteroviral infections (Coxsackie, echo) Parvovirus infection HIV
 ISOLATION PROCEDURES
ISOLATION PROCEDURES
 Isolation procedures Place in a private room. Limit visitors as indicated. Prohibit live plants or flowers. Coordinate patient care so that leukemic patient doesn’t come in contact with staff who also care for patients with infections or infectious diseases.
Isolation procedures Place in a private room. Limit visitors as indicated. Prohibit live plants or flowers. Coordinate patient care so that leukemic patient doesn’t come in contact with staff who also care for patients with infections or infectious diseases.


 PROPHYLAXIS END TREATMENT
PROPHYLAXIS END TREATMENT
 Cell technologies in Hematology Worked: Allogeneic transplantation from donors genidentity Allogeneic transplantation from an unrelated donor freidenrich Methods infusion of donor lymphocytes Transplantation of unrelated PC Methods of partial T-Deplete T-depleted haploidentical transplantation In development: Induction of tolerance/anergy Virus-specific T cells Vaccination of dendritic cells Transplantation of mesenchymal cells
Cell technologies in Hematology Worked: Allogeneic transplantation from donors genidentity Allogeneic transplantation from an unrelated donor freidenrich Methods infusion of donor lymphocytes Transplantation of unrelated PC Methods of partial T-Deplete T-depleted haploidentical transplantation In development: Induction of tolerance/anergy Virus-specific T cells Vaccination of dendritic cells Transplantation of mesenchymal cells
 Infectiou s agents • Bacteria • Fungi • Viruses Protozoas Helminthes
Infectiou s agents • Bacteria • Fungi • Viruses Protozoas Helminthes
 Maternal microchimerism and neonatal immunity Receipt of maternal cells in the fetus documented 55 years ago (Grenn I. et al, Hodgkin’s disease: a matuernal-to fetal lymphocyte chimegera Lancet, 1960? ) Maternal DNA is determined by the fetus from the moment of development of placental krovoobrazscheniya. The panel for the RT-AKP informative for 90% of couples with a child-mother chuvstvitelnostyu 1 1006 was developed 11 years ago (Lambert NC et al Arthritis Rheum, 2004, 50, 906 -914. ) And tested 47 cell lines Diagnosis / Screening — umbilical cord blood We prove the transfer of breast milk cells Studied the cellular composition MMX macrophages, T cells, B cells, natural killer cells There are descriptions of the transfer of tumor diseases (NHL, melanoma and others. ) Maternal cells are found in children, not only in the form of circulating blood cells, but also as a differentiated tissue of the skin cells of the thymus, heart, lung, pancreas, spleen, kidney, muscle, and bone marrow
Maternal microchimerism and neonatal immunity Receipt of maternal cells in the fetus documented 55 years ago (Grenn I. et al, Hodgkin’s disease: a matuernal-to fetal lymphocyte chimegera Lancet, 1960? ) Maternal DNA is determined by the fetus from the moment of development of placental krovoobrazscheniya. The panel for the RT-AKP informative for 90% of couples with a child-mother chuvstvitelnostyu 1 1006 was developed 11 years ago (Lambert NC et al Arthritis Rheum, 2004, 50, 906 -914. ) And tested 47 cell lines Diagnosis / Screening — umbilical cord blood We prove the transfer of breast milk cells Studied the cellular composition MMX macrophages, T cells, B cells, natural killer cells There are descriptions of the transfer of tumor diseases (NHL, melanoma and others. ) Maternal cells are found in children, not only in the form of circulating blood cells, but also as a differentiated tissue of the skin cells of the thymus, heart, lung, pancreas, spleen, kidney, muscle, and bone marrow
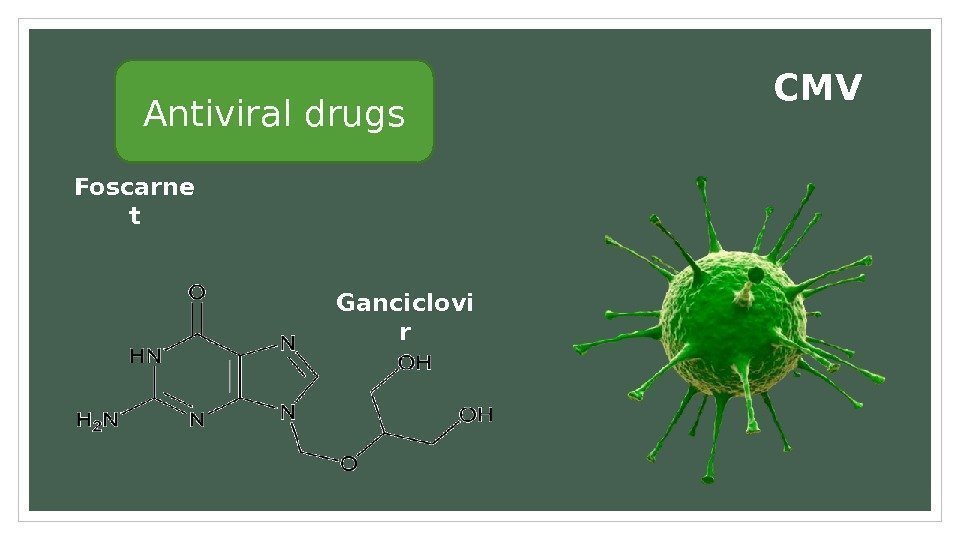
 Drugs There are three groups of drugs can be used in the profylaxis of infections: antibacterial (for example, fluoroquinolones), antiviral (such as acyclovir and ganciclovir) and antifungal ( fluconazole, itraconazole and posaconazole).
Drugs There are three groups of drugs can be used in the profylaxis of infections: antibacterial (for example, fluoroquinolones), antiviral (such as acyclovir and ganciclovir) and antifungal ( fluconazole, itraconazole and posaconazole).
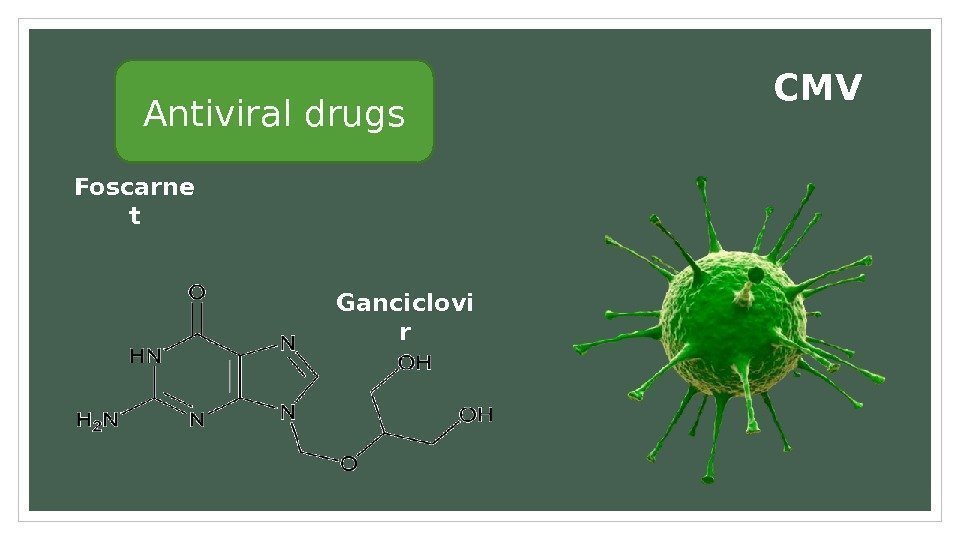 Antiviral drugs CMV Ganciclovi r. Foscarne t
Antiviral drugs CMV Ganciclovi r. Foscarne t
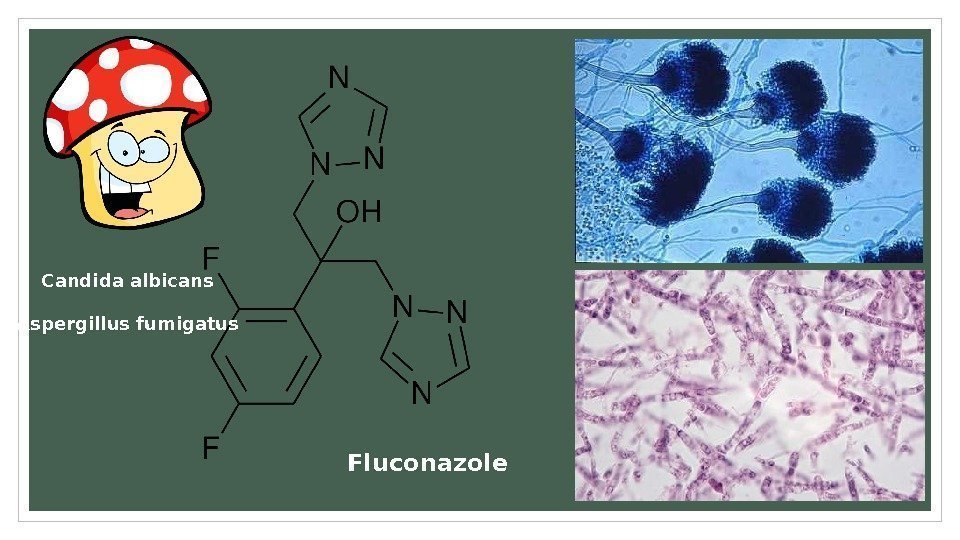 Fluconazole. Candida albicans Aspergillus fumigatus
Fluconazole. Candida albicans Aspergillus fumigatus
 Maternal microchimerism and neonatal immunity Receipt of maternal cells in the fetus documented 55 years ago (Grenn I. et al, Hodgkin’s disease: a matuernal-to fetal lymphocyte chimegera Lancet, 1960? ) Maternal DNA is determined by the fetus from the moment of development of placental krovoobrazscheniya. The panel for the RT-AKP informative for 90% of couples with a child-mother chuvstvitelnostyu 1 1006 was developed 11 years ago (Lambert NC et al Arthritis Rheum, 2004, 50, 906 -914. ) And tested 47 cell lines Diagnosis / Screening — umbilical cord blood We prove the transfer of breast milk cells Studied the cellular composition MMX macrophages, T cells, B cells, natural killer cells There are descriptions of the transfer of tumor diseases (NHL, melanoma and others. ) Maternal cells are found in children, not only in the form of circulating blood cells, but also as a differentiated tissue of the skin cells of the thymus, heart, lung, pancreas, spleen, kidney, muscle, and bone marrow
Maternal microchimerism and neonatal immunity Receipt of maternal cells in the fetus documented 55 years ago (Grenn I. et al, Hodgkin’s disease: a matuernal-to fetal lymphocyte chimegera Lancet, 1960? ) Maternal DNA is determined by the fetus from the moment of development of placental krovoobrazscheniya. The panel for the RT-AKP informative for 90% of couples with a child-mother chuvstvitelnostyu 1 1006 was developed 11 years ago (Lambert NC et al Arthritis Rheum, 2004, 50, 906 -914. ) And tested 47 cell lines Diagnosis / Screening — umbilical cord blood We prove the transfer of breast milk cells Studied the cellular composition MMX macrophages, T cells, B cells, natural killer cells There are descriptions of the transfer of tumor diseases (NHL, melanoma and others. ) Maternal cells are found in children, not only in the form of circulating blood cells, but also as a differentiated tissue of the skin cells of the thymus, heart, lung, pancreas, spleen, kidney, muscle, and bone marrow
 Evidence of intercellular interactions in the system mother-fetus In all pregnancies human fetal cells embedded in the mother’s circulation Fetal cells are detected at 6 weeks of gestation, and the frequency of detection increases with increasing gestational age, reaching 100% at 36 weeks of gestation In normal pregnancy in the second trimester of pregnancy, the number of fetal cells maternal venous blood is 1 -6 cells / ml (i. e. , from 5 to 30 h 103 cells) If abnormalities of the placenta and fetus, eclampsia, tissue compatibility problems, miscarriage, spontaneous abortion in terms of 20 and weeks, the number of circulating fetal cells increases to 20 -1500 cells per ml. After birth, the number of fetal cells in the circulation is reduced drastically, but 50% of fetal cells found in the blood of 4 weeks to 10 weeks postpartum Special studies of postpartum microchimerism find it in 40% of healthy women after pregnancy
Evidence of intercellular interactions in the system mother-fetus In all pregnancies human fetal cells embedded in the mother’s circulation Fetal cells are detected at 6 weeks of gestation, and the frequency of detection increases with increasing gestational age, reaching 100% at 36 weeks of gestation In normal pregnancy in the second trimester of pregnancy, the number of fetal cells maternal venous blood is 1 -6 cells / ml (i. e. , from 5 to 30 h 103 cells) If abnormalities of the placenta and fetus, eclampsia, tissue compatibility problems, miscarriage, spontaneous abortion in terms of 20 and weeks, the number of circulating fetal cells increases to 20 -1500 cells per ml. After birth, the number of fetal cells in the circulation is reduced drastically, but 50% of fetal cells found in the blood of 4 weeks to 10 weeks postpartum Special studies of postpartum microchimerism find it in 40% of healthy women after pregnancy
 Thank you for your attention !
Thank you for your attention !

