1289c5b9ebf97516295b050e32ef79d9.ppt
- Количество слайдов: 29
 Project overview (Immersion Call 1) Peter J. Pronovost MD, Ph. D. Johns Hopkins University School of Medicine Quality and Safety Research Group
Project overview (Immersion Call 1) Peter J. Pronovost MD, Ph. D. Johns Hopkins University School of Medicine Quality and Safety Research Group
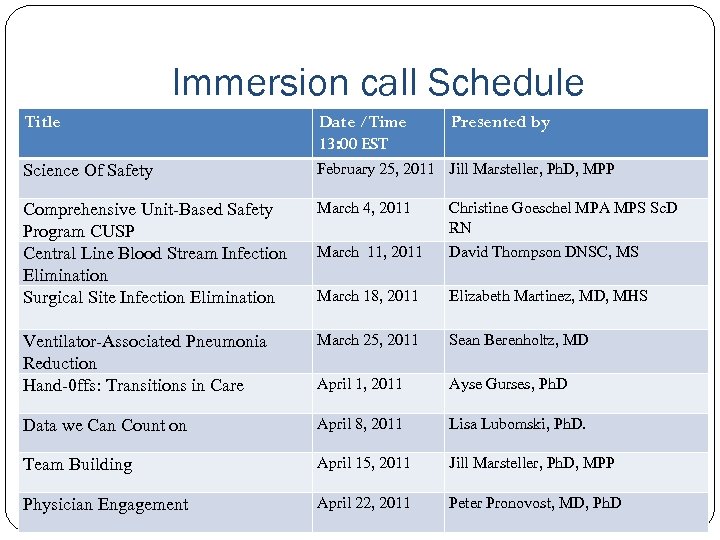 Immersion call Schedule Title Date /Time 13: 00 EST Presented by Science Of Safety February 25, 2011 Jill Marsteller, Ph. D, MPP Comprehensive Unit-Based Safety Program CUSP Central Line Blood Stream Infection Elimination Surgical Site Infection Elimination March 4, 2011 Christine Goeschel MPA MPS Sc. D RN March 11, 2011 David Thompson DNSC, MS March 18, 2011 Elizabeth Martinez, MD, MHS Ventilator-Associated Pneumonia Reduction Hand-0 ffs: Transitions in Care March 25, 2011 Sean Berenholtz, MD April 1, 2011 Ayse Gurses, Ph. D Data we Can Count on April 8, 2011 Lisa Lubomski, Ph. D. Team Building April 15, 2011 Jill Marsteller, Ph. D, MPP Physician Engagement April 22, 2011 Peter Pronovost, MD, Ph. D
Immersion call Schedule Title Date /Time 13: 00 EST Presented by Science Of Safety February 25, 2011 Jill Marsteller, Ph. D, MPP Comprehensive Unit-Based Safety Program CUSP Central Line Blood Stream Infection Elimination Surgical Site Infection Elimination March 4, 2011 Christine Goeschel MPA MPS Sc. D RN March 11, 2011 David Thompson DNSC, MS March 18, 2011 Elizabeth Martinez, MD, MHS Ventilator-Associated Pneumonia Reduction Hand-0 ffs: Transitions in Care March 25, 2011 Sean Berenholtz, MD April 1, 2011 Ayse Gurses, Ph. D Data we Can Count on April 8, 2011 Lisa Lubomski, Ph. D. Team Building April 15, 2011 Jill Marsteller, Ph. D, MPP Physician Engagement April 22, 2011 Peter Pronovost, MD, Ph. D
 Learning Objectives • To delineate the goals of Cardiac Surgery CER Project • To describe the project organization • To define the interventions • To outline the planned learning sessions • To identify who to call for help
Learning Objectives • To delineate the goals of Cardiac Surgery CER Project • To describe the project organization • To define the interventions • To outline the planned learning sessions • To identify who to call for help

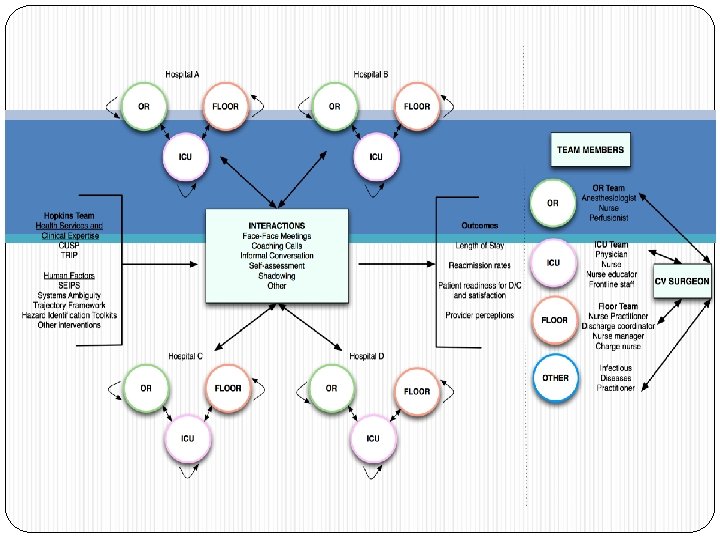
 Project Organization Multi-site Project coordinated by Quality and Safety Research Group with collaboration from SCAF Learning collaborative model (e. g. , multisite participation, 2 face-to-face meetings, monthly calls) Standardized data collection tools and evidence Local unit modification of how to implement interventions
Project Organization Multi-site Project coordinated by Quality and Safety Research Group with collaboration from SCAF Learning collaborative model (e. g. , multisite participation, 2 face-to-face meetings, monthly calls) Standardized data collection tools and evidence Local unit modification of how to implement interventions
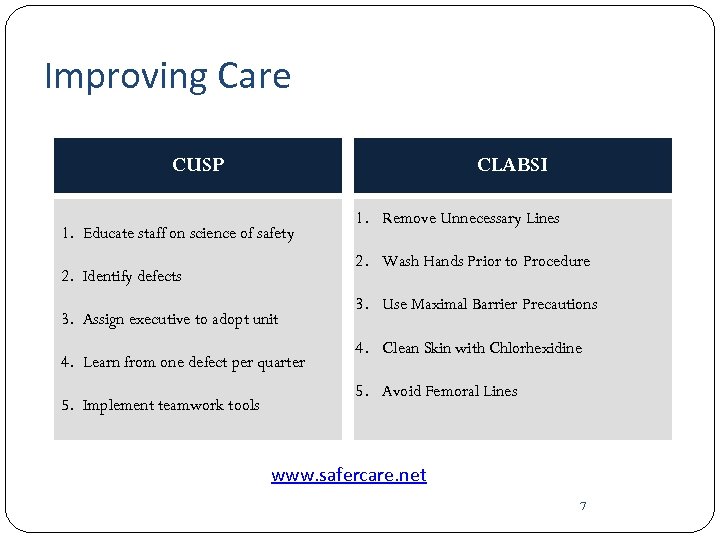 Improving Care CUSP CLABSI 1. Educate staff on science of safety 2. Wash Hands Prior to Procedure 2. Identify defects 3. Assign executive to adopt unit 4. Learn from one defect per quarter 5. Implement teamwork tools 1. Remove Unnecessary Lines 3. Use Maximal Barrier Precautions 4. Clean Skin with Chlorhexidine 5. Avoid Femoral Lines www. safercare. net 7
Improving Care CUSP CLABSI 1. Educate staff on science of safety 2. Wash Hands Prior to Procedure 2. Identify defects 3. Assign executive to adopt unit 4. Learn from one defect per quarter 5. Implement teamwork tools 1. Remove Unnecessary Lines 3. Use Maximal Barrier Precautions 4. Clean Skin with Chlorhexidine 5. Avoid Femoral Lines www. safercare. net 7
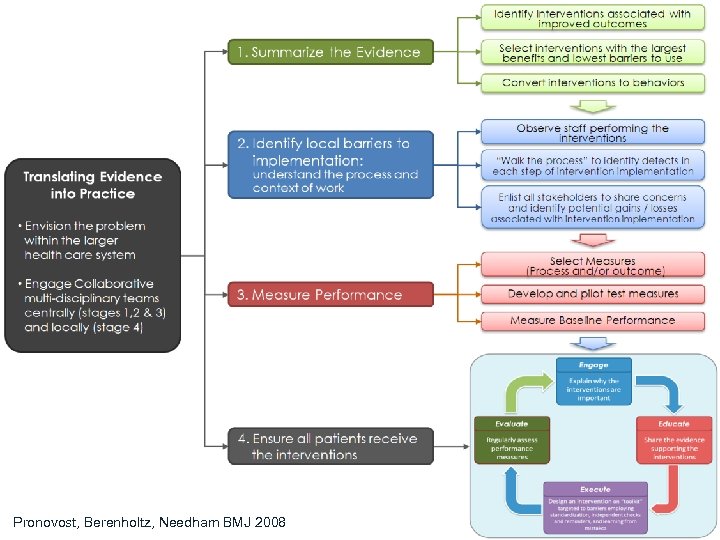 Pronovost, Berenholtz, Needham BMJ 2008
Pronovost, Berenholtz, Needham BMJ 2008
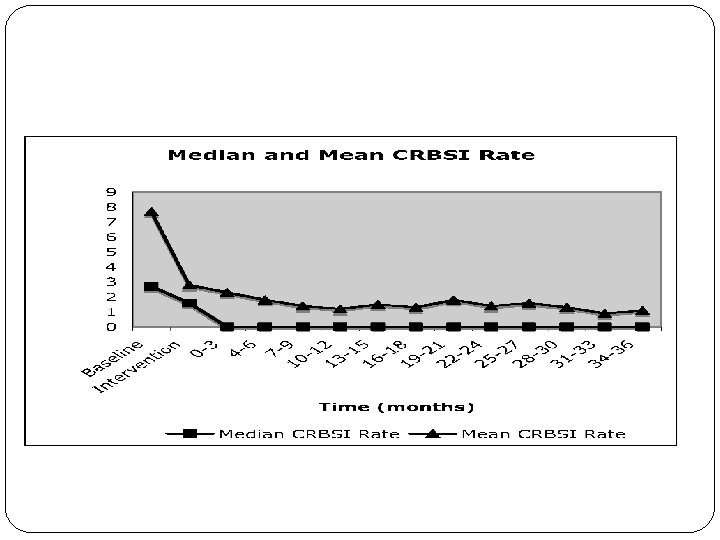 CRBSI Rate Over Time 9
CRBSI Rate Over Time 9
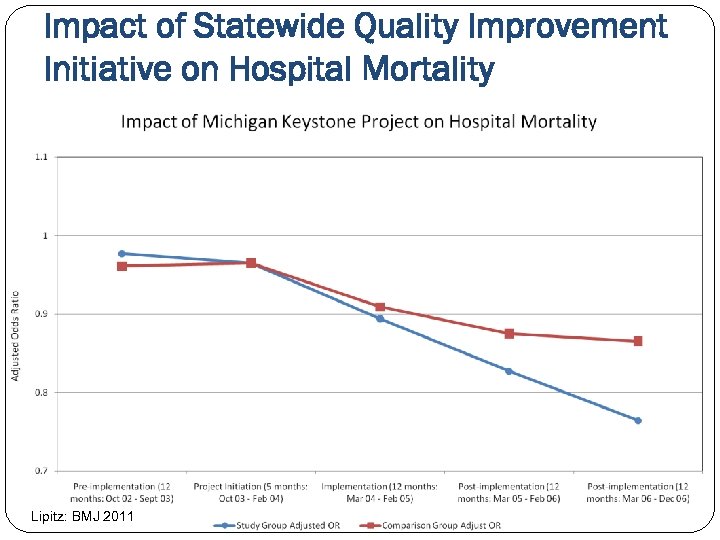 Impact of Statewide Quality Improvement Initiative on Hospital Mortality Lipitz: BMJ 2011
Impact of Statewide Quality Improvement Initiative on Hospital Mortality Lipitz: BMJ 2011
 Michigan ICU Safety Climate Improvement * “Needs Improvement” - Safety Climate Score <60% 11
Michigan ICU Safety Climate Improvement * “Needs Improvement” - Safety Climate Score <60% 11
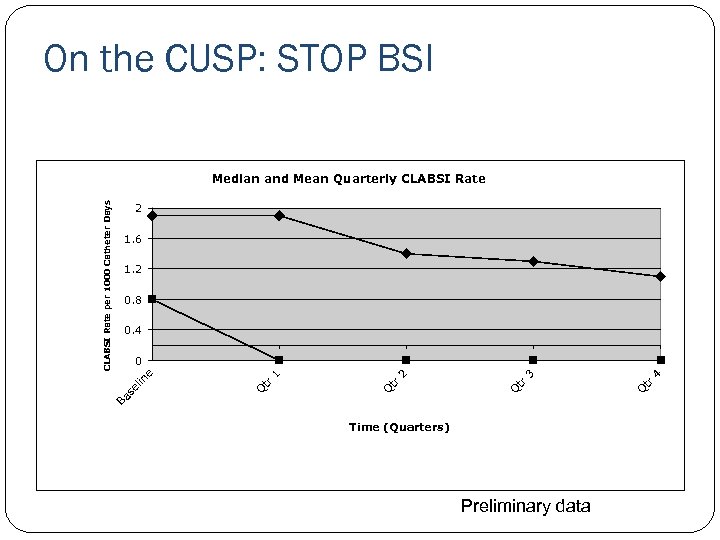 On the CUSP: STOP BSI 2 1. 6 1. 2 0. 8 0. 4 Time (Quarters) Preliminary data Q tr 4 3 tr Q Q tr 1 tr Q lin Ba se 2 0 e CLABSI Rate per 1000 Catheter Days Median and Mean Quarterly CLABSI Rate
On the CUSP: STOP BSI 2 1. 6 1. 2 0. 8 0. 4 Time (Quarters) Preliminary data Q tr 4 3 tr Q Q tr 1 tr Q lin Ba se 2 0 e CLABSI Rate per 1000 Catheter Days Median and Mean Quarterly CLABSI Rate
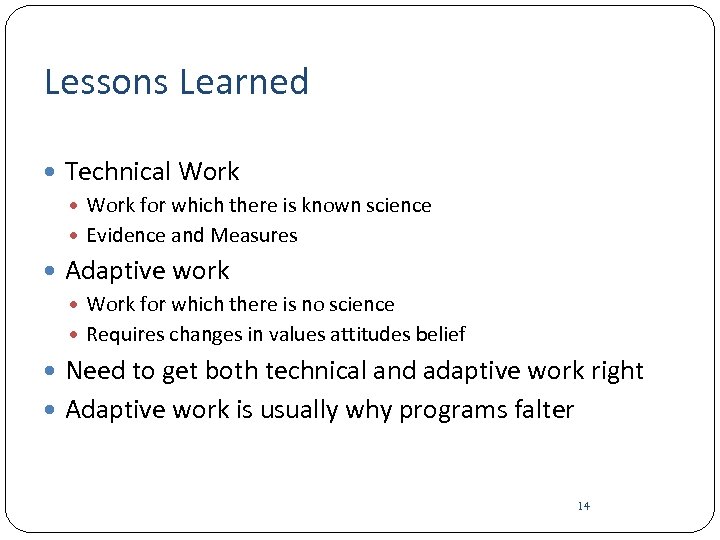 Lessons Learned Technical Work for which there is known science Evidence and Measures Adaptive work Work for which there is no science Requires changes in values attitudes belief Need to get both technical and adaptive work right Adaptive work is usually why programs falter 14
Lessons Learned Technical Work for which there is known science Evidence and Measures Adaptive work Work for which there is no science Requires changes in values attitudes belief Need to get both technical and adaptive work right Adaptive work is usually why programs falter 14
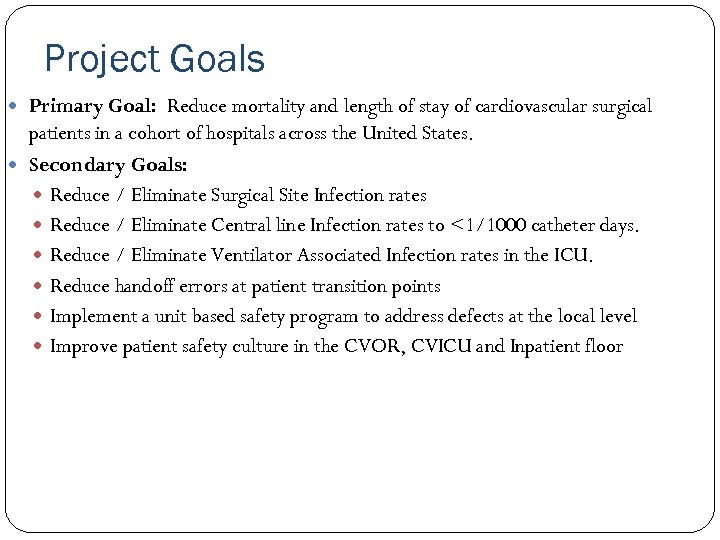 Project Goals Primary Goal: Reduce mortality and length of stay of cardiovascular surgical patients in a cohort of hospitals across the United States. Secondary Goals: Reduce / Eliminate Surgical Site Infection rates Reduce / Eliminate Central line Infection rates to <1/1000 catheter days. Reduce / Eliminate Ventilator Associated Infection rates in the ICU. Reduce handoff errors at patient transition points Implement a unit based safety program to address defects at the local level Improve patient safety culture in the CVOR, CVICU and Inpatient floor
Project Goals Primary Goal: Reduce mortality and length of stay of cardiovascular surgical patients in a cohort of hospitals across the United States. Secondary Goals: Reduce / Eliminate Surgical Site Infection rates Reduce / Eliminate Central line Infection rates to <1/1000 catheter days. Reduce / Eliminate Ventilator Associated Infection rates in the ICU. Reduce handoff errors at patient transition points Implement a unit based safety program to address defects at the local level Improve patient safety culture in the CVOR, CVICU and Inpatient floor
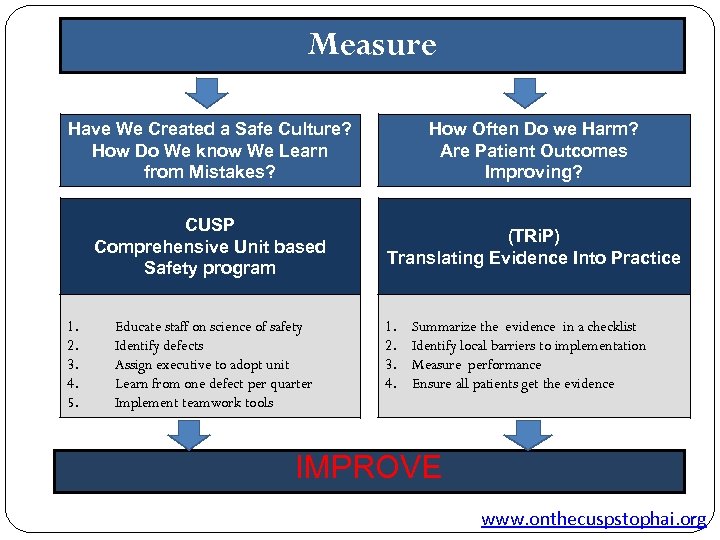 Measure Have We Created a Safe Culture? How Do We know We Learn from Mistakes? How Often Do we Harm? Are Patient Outcomes Improving? CUSP Comprehensive Unit based Safety program (TRi. P) Translating Evidence Into Practice 1. 2. 3. 4. 5. Educate staff on science of safety Identify defects Assign executive to adopt unit Learn from one defect per quarter Implement teamwork tools 1. 2. 3. 4. Summarize the evidence in a checklist Identify local barriers to implementation Measure performance Ensure all patients get the evidence IMPROVE www. onthecuspstophai. org
Measure Have We Created a Safe Culture? How Do We know We Learn from Mistakes? How Often Do we Harm? Are Patient Outcomes Improving? CUSP Comprehensive Unit based Safety program (TRi. P) Translating Evidence Into Practice 1. 2. 3. 4. 5. Educate staff on science of safety Identify defects Assign executive to adopt unit Learn from one defect per quarter Implement teamwork tools 1. 2. 3. 4. Summarize the evidence in a checklist Identify local barriers to implementation Measure performance Ensure all patients get the evidence IMPROVE www. onthecuspstophai. org
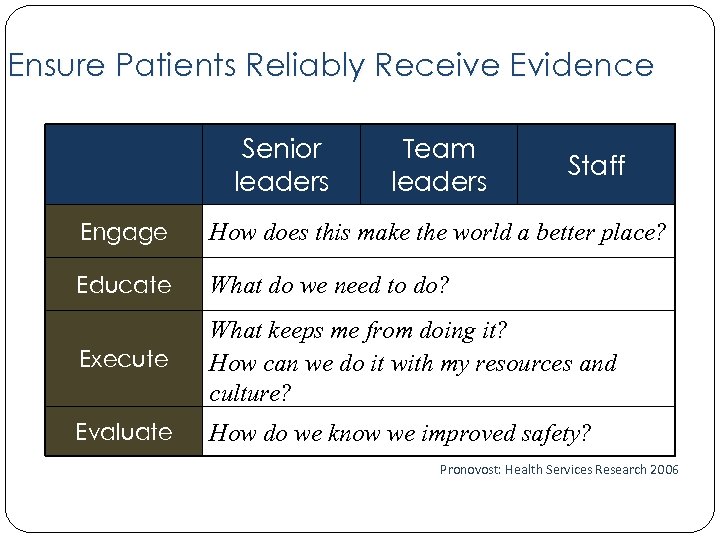 Ensure Patients Reliably Receive Evidence Senior leaders Team leaders Staff Engage How does this make the world a better place? Educate What do we need to do? Execute What keeps me from doing it? How can we do it with my resources and culture? Evaluate How do we know we improved safety? Pronovost: Health Services Research 2006
Ensure Patients Reliably Receive Evidence Senior leaders Team leaders Staff Engage How does this make the world a better place? Educate What do we need to do? Execute What keeps me from doing it? How can we do it with my resources and culture? Evaluate How do we know we improved safety? Pronovost: Health Services Research 2006
 Major Intervention Areas CLABSI VAP SSI CUSP Cross-unit integration (For selected sites) Handoffs and Transitions of care
Major Intervention Areas CLABSI VAP SSI CUSP Cross-unit integration (For selected sites) Handoffs and Transitions of care
 Specific Aims AIM 1: To implement and evaluate the impact of a patient safety program on surgical site infection (SSI) rates and operating room (OR) safety culture in a cohort of cardiac ORs. AIM 2: To implement and evaluate the impact of a patient safety program on rates of central line-associated bloodstream infections (CLABSI), ventilator-associated pneumonia (VAP), and safety culture in a cohort of cardiovascular surgical intensive care units (CVICUs) AIM 3: To improve the safety of transitions of care/hand-offs from the cardiac OR to the cardiovascular ICU (CVICU), from the CVICU to the surgical inpatient floor, and from the surgical inpatient floor to hospital discharge. AIM 4: To facilitate and improve teamwork, communication, and coordination across the three clinical areas/units.
Specific Aims AIM 1: To implement and evaluate the impact of a patient safety program on surgical site infection (SSI) rates and operating room (OR) safety culture in a cohort of cardiac ORs. AIM 2: To implement and evaluate the impact of a patient safety program on rates of central line-associated bloodstream infections (CLABSI), ventilator-associated pneumonia (VAP), and safety culture in a cohort of cardiovascular surgical intensive care units (CVICUs) AIM 3: To improve the safety of transitions of care/hand-offs from the cardiac OR to the cardiovascular ICU (CVICU), from the CVICU to the surgical inpatient floor, and from the surgical inpatient floor to hospital discharge. AIM 4: To facilitate and improve teamwork, communication, and coordination across the three clinical areas/units.
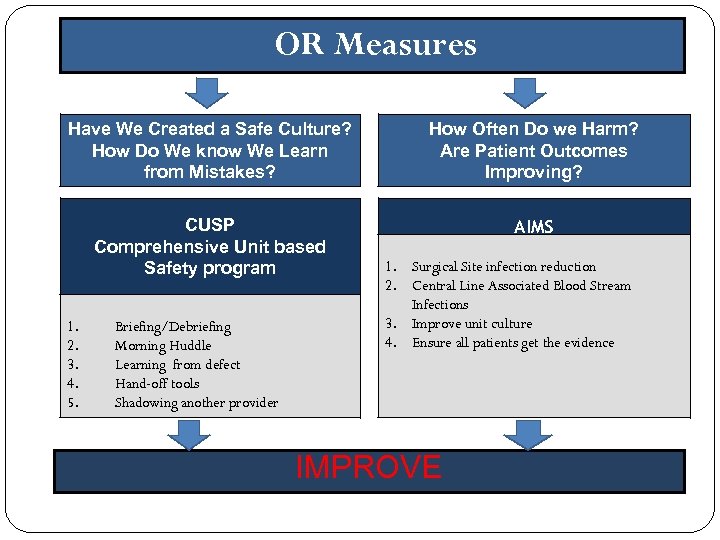 OR Measures Have We Created a Safe Culture? How Do We know We Learn from Mistakes? How Often Do we Harm? Are Patient Outcomes Improving? CUSP Comprehensive Unit based Safety program AIMS 1. 2. 3. 4. 5. Briefing/Debriefing Morning Huddle Learning from defect Hand-off tools Shadowing another provider 1. Surgical Site infection reduction 2. Central Line Associated Blood Stream Infections 3. Improve unit culture 4. Ensure all patients get the evidence IMPROVE
OR Measures Have We Created a Safe Culture? How Do We know We Learn from Mistakes? How Often Do we Harm? Are Patient Outcomes Improving? CUSP Comprehensive Unit based Safety program AIMS 1. 2. 3. 4. 5. Briefing/Debriefing Morning Huddle Learning from defect Hand-off tools Shadowing another provider 1. Surgical Site infection reduction 2. Central Line Associated Blood Stream Infections 3. Improve unit culture 4. Ensure all patients get the evidence IMPROVE
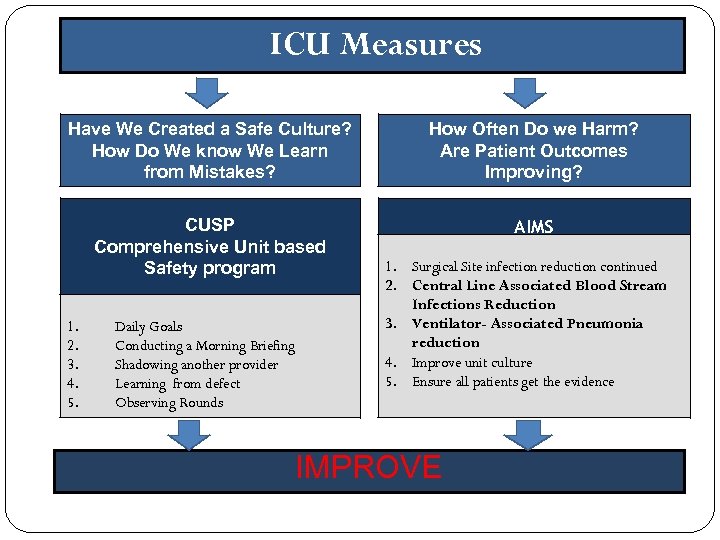 ICU Measures Have We Created a Safe Culture? How Do We know We Learn from Mistakes? How Often Do we Harm? Are Patient Outcomes Improving? CUSP Comprehensive Unit based Safety program AIMS 1. 2. 3. 4. 5. Daily Goals Conducting a Morning Briefing Shadowing another provider Learning from defect Observing Rounds 1. Surgical Site infection reduction continued 2. Central Line Associated Blood Stream Infections Reduction 3. Ventilator- Associated Pneumonia reduction 4. Improve unit culture 5. Ensure all patients get the evidence IMPROVE
ICU Measures Have We Created a Safe Culture? How Do We know We Learn from Mistakes? How Often Do we Harm? Are Patient Outcomes Improving? CUSP Comprehensive Unit based Safety program AIMS 1. 2. 3. 4. 5. Daily Goals Conducting a Morning Briefing Shadowing another provider Learning from defect Observing Rounds 1. Surgical Site infection reduction continued 2. Central Line Associated Blood Stream Infections Reduction 3. Ventilator- Associated Pneumonia reduction 4. Improve unit culture 5. Ensure all patients get the evidence IMPROVE
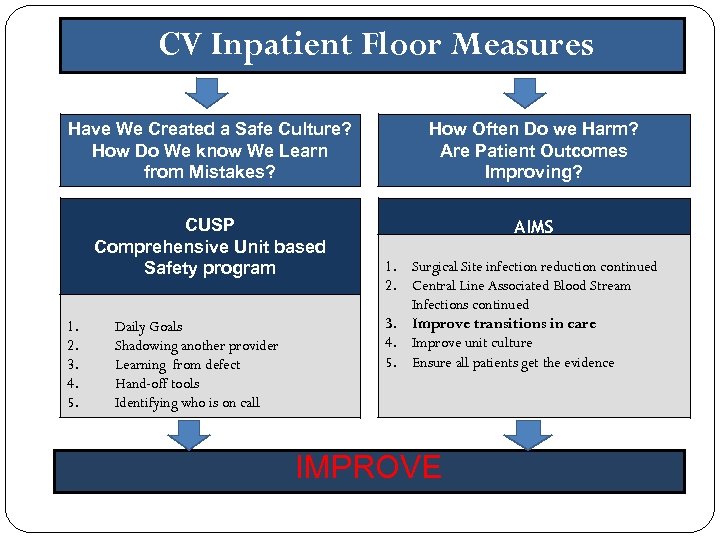 CV Inpatient Floor Measures Have We Created a Safe Culture? How Do We know We Learn from Mistakes? How Often Do we Harm? Are Patient Outcomes Improving? CUSP Comprehensive Unit based Safety program AIMS 1. 2. 3. 4. 5. Daily Goals Shadowing another provider Learning from defect Hand-off tools Identifying who is on call 1. Surgical Site infection reduction continued 2. Central Line Associated Blood Stream Infections continued 3. Improve transitions in care 4. Improve unit culture 5. Ensure all patients get the evidence IMPROVE
CV Inpatient Floor Measures Have We Created a Safe Culture? How Do We know We Learn from Mistakes? How Often Do we Harm? Are Patient Outcomes Improving? CUSP Comprehensive Unit based Safety program AIMS 1. 2. 3. 4. 5. Daily Goals Shadowing another provider Learning from defect Hand-off tools Identifying who is on call 1. Surgical Site infection reduction continued 2. Central Line Associated Blood Stream Infections continued 3. Improve transitions in care 4. Improve unit culture 5. Ensure all patients get the evidence IMPROVE
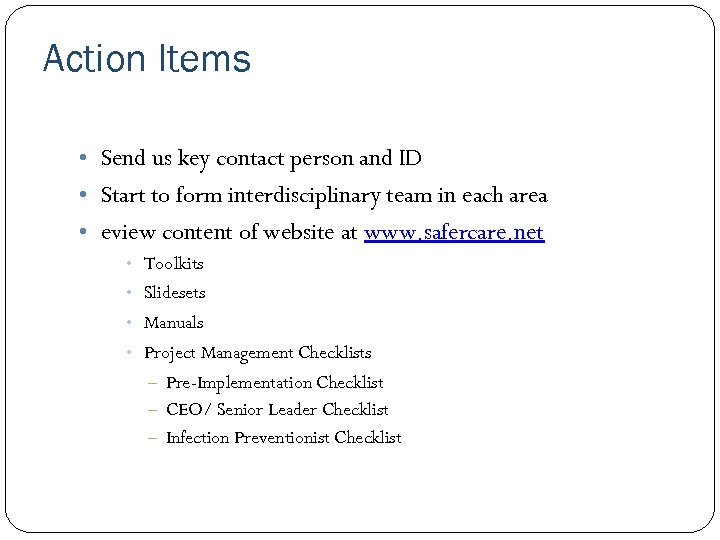 Action Items • Send us key contact person and ID • Start to form interdisciplinary team in each area • eview content of website at www. safercare. net • Toolkits • Slidesets • Manuals • Project Management Checklists Pre-Implementation Checklist – CEO/ Senior Leader Checklist – Infection Preventionist Checklist –
Action Items • Send us key contact person and ID • Start to form interdisciplinary team in each area • eview content of website at www. safercare. net • Toolkits • Slidesets • Manuals • Project Management Checklists Pre-Implementation Checklist – CEO/ Senior Leader Checklist – Infection Preventionist Checklist –
 To Get Help Email David Thompson DNSc, RN for study related questions. dthomps 1@jhmi. edu Talk to your team leader
To Get Help Email David Thompson DNSc, RN for study related questions. dthomps 1@jhmi. edu Talk to your team leader
 References Measuring Safety Pronovost PJ, Goeschel CA, Wachter RM. The wisdom and justice of not paying for "preventable complications". JAMA. 2008; 299(18): 2197 -2199. Pronovost PJ, Miller MR, Wachter RM. Tracking progress in patient safety: An elusive target. JAMA. 2006; 296(6): 696 -699. Pronovost PJ, Sexton JB, Pham JC, Goeschel CA, Winters BD, Miller MR. Measurement of quality and assurance of safety in the critically ill. Clin Chest Med. 2008; in press.
References Measuring Safety Pronovost PJ, Goeschel CA, Wachter RM. The wisdom and justice of not paying for "preventable complications". JAMA. 2008; 299(18): 2197 -2199. Pronovost PJ, Miller MR, Wachter RM. Tracking progress in patient safety: An elusive target. JAMA. 2006; 296(6): 696 -699. Pronovost PJ, Sexton JB, Pham JC, Goeschel CA, Winters BD, Miller MR. Measurement of quality and assurance of safety in the critically ill. Clin Chest Med. 2008; in press.
 References Measuring Safety • Pronovost PJ, Goeschel CA, Wachter RM. The wisdom and justice of not paying for "preventable complications". JAMA. 2008; 299(18): 2197 -2199. • Pronovost PJ, Miller MR, Wachter RM. Tracking progress in patient safety: An elusive target. JAMA. 2006; 296(6): 696 -699. • Pronovost PJ, Sexton JB, Pham JC, Goeschel CA, Winters BD, Miller MR. Measurement of quality and assurance of safety in the critically ill. Clin Chest Med. 2008; in press.
References Measuring Safety • Pronovost PJ, Goeschel CA, Wachter RM. The wisdom and justice of not paying for "preventable complications". JAMA. 2008; 299(18): 2197 -2199. • Pronovost PJ, Miller MR, Wachter RM. Tracking progress in patient safety: An elusive target. JAMA. 2006; 296(6): 696 -699. • Pronovost PJ, Sexton JB, Pham JC, Goeschel CA, Winters BD, Miller MR. Measurement of quality and assurance of safety in the critically ill. Clin Chest Med. 2008; in press.
 References • Pronovost P, Weast B, Rosenstein B, et al. Implementing and validating a comprehensive unit-based safety program. J Pat Safety. 2005; 1(1): 33 -40. • Pronovost P, Berenholtz S, Dorman T, Lipsett PA, Simmonds T, Haraden C. Improving communication in the ICU using daily goals. J Crit Care. 2003; 18(2): 71 -75. • Pronovost PJ, Berenholtz SM, Needham DM. Translating evidence into practice: a model for large scale knowledge translation. BMJ. 2008 Oct 6; 337. • Pronovost PJ, Weast B, Bishop K, et al. Senior executive adopt-a-work unit: A model for safety improvement. Jt Comm J Qual Saf. 2004; 30(2): 59 -68. • Thompson DA, Holzmueller CG, Cafeo CL, Sexton JB, Pronovost PJ. A morning briefing: Setting the stage for a clinically and operationally good day. Jt Comm J Qual and Saf. 2005; 31(8): 476 -479.
References • Pronovost P, Weast B, Rosenstein B, et al. Implementing and validating a comprehensive unit-based safety program. J Pat Safety. 2005; 1(1): 33 -40. • Pronovost P, Berenholtz S, Dorman T, Lipsett PA, Simmonds T, Haraden C. Improving communication in the ICU using daily goals. J Crit Care. 2003; 18(2): 71 -75. • Pronovost PJ, Berenholtz SM, Needham DM. Translating evidence into practice: a model for large scale knowledge translation. BMJ. 2008 Oct 6; 337. • Pronovost PJ, Weast B, Bishop K, et al. Senior executive adopt-a-work unit: A model for safety improvement. Jt Comm J Qual Saf. 2004; 30(2): 59 -68. • Thompson DA, Holzmueller CG, Cafeo CL, Sexton JB, Pronovost PJ. A morning briefing: Setting the stage for a clinically and operationally good day. Jt Comm J Qual and Saf. 2005; 31(8): 476 -479.


