ee55976f793f444dc5d4ec77554a73b0.ppt
- Количество слайдов: 69
Prof Mohammad Salah Abduljabbar CEREBROVASCULAR ACCIDENT “BRAIN ATTACK”
Objectives Define cerebrovascular accident and associated terminology Discuss related pathophysiology and presentation of various types of stroke Discuss etiology, risk factors, diagnostics, management, and outcomes of stroke Review case studies and nursing diagnoses, interventions, and goals
Definition Stroke or “brain attack” is an acute CNS injury that results in neurologic Symptoms and signs brought on by a reduction or absence of perfusion to a territory of the brain. The disruption in flow is from either an occlusion (ischemic) or rupture (hemorrhagic) of the blood vessel.
Incidence & Prevalence Third leading cause of death in the USA 750, 000+ people/year 175, 000 die within one year (25%) Leading cause of long-term disabilities 5. 5 million survivors (USA) 15 to 30 % live with permanent disability
Stroke Statistics 15% of adults > age 50 cannot name a single symptom of stroke 13 hours after onset of symptoms is the median time to presentation 58% of stroke patients don’t present during the first 24 hours after onset 52% of stroke patients in the ED are unaware that they are experiencing a stroke
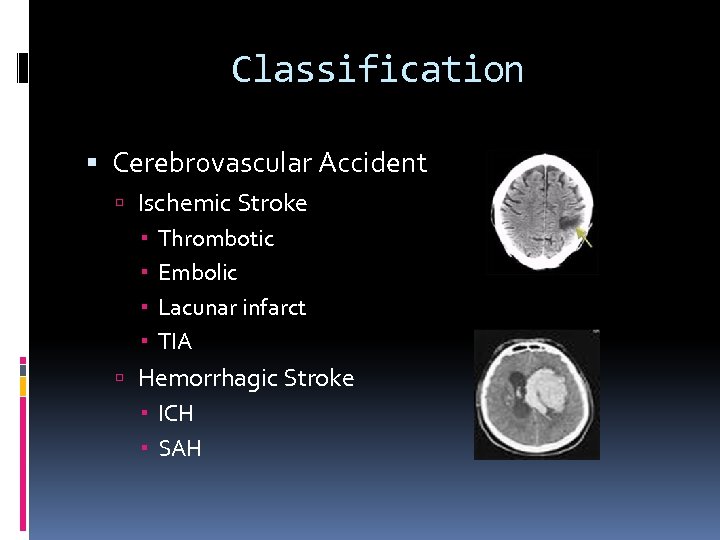
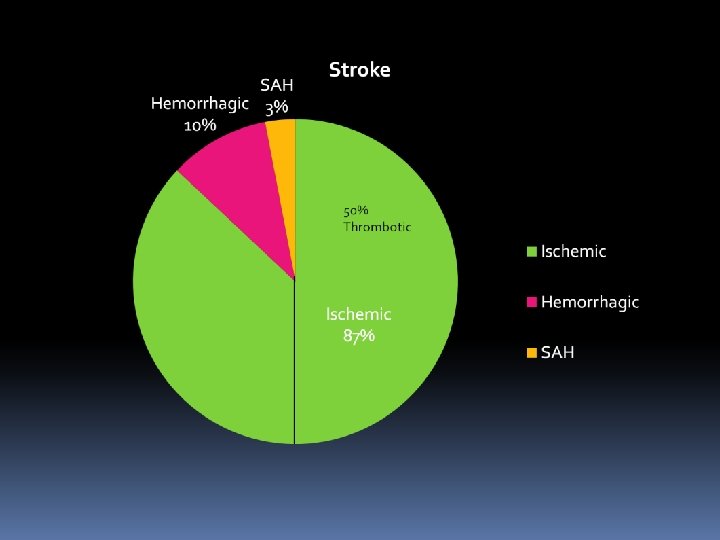
Classification Cerebrovascular Accident Ischemic Stroke Thrombotic Embolic Lacunar infarct TIA Hemorrhagic Stroke ICH SAH
Stroke Knowledge MYTHS FACTS Can’t prevent stroke Stroke is preventable Can’t treat stroke Stroke is treatable Stroke affects the heart Stroke is a brain attack Stroke affects the elderly Stroke affects anyone Recovery happens for a Stroke recovery occurs few months after stroke throughout life
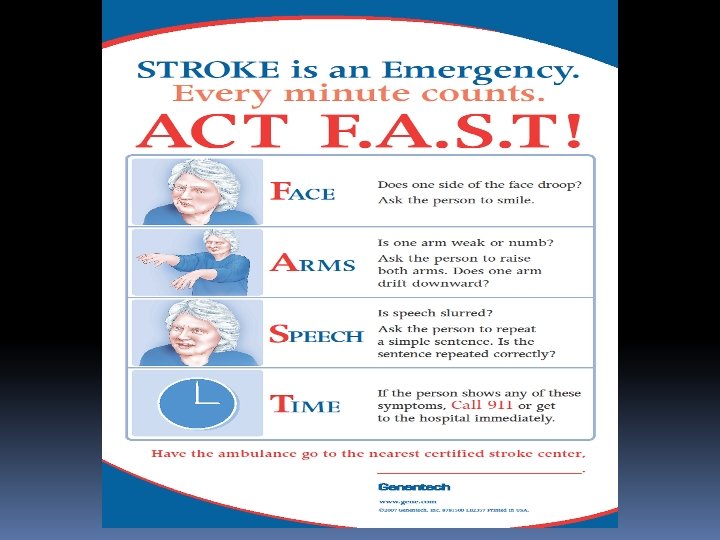
Stroke: Emergency Care
Stroke Symptoms Sudden numbness or weakness of face, arm or leg, especially on one side of the body Sudden confusion, trouble understanding or speaking Sudden trouble seeing in one or both eyes Sudden trouble walking, dizziness, loss of balance or coordination Sudden severe headache with no known cause
Other Symptoms Sudden nausea, fever and vomiting, distinguished from a viral illness by rapid onset (minutes or hours vs. days) Brief loss of consciousness or period of decreased consciousness (fainting, confusion, convulsions or coma)
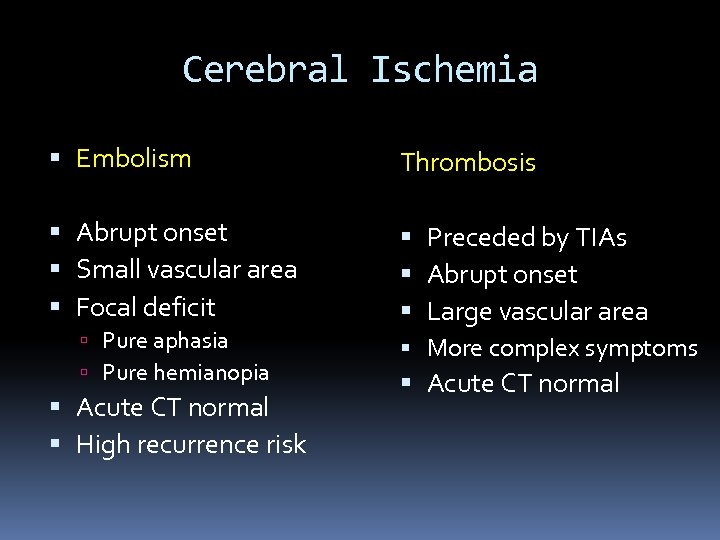
Cerebral Ischemia Embolism Thrombosis Abrupt onset Small vascular area Focal deficit Preceded by TIAs Abrupt onset Large vascular area More complex symptoms Acute CT normal Pure aphasia Pure hemianopia Acute CT normal High recurrence risk
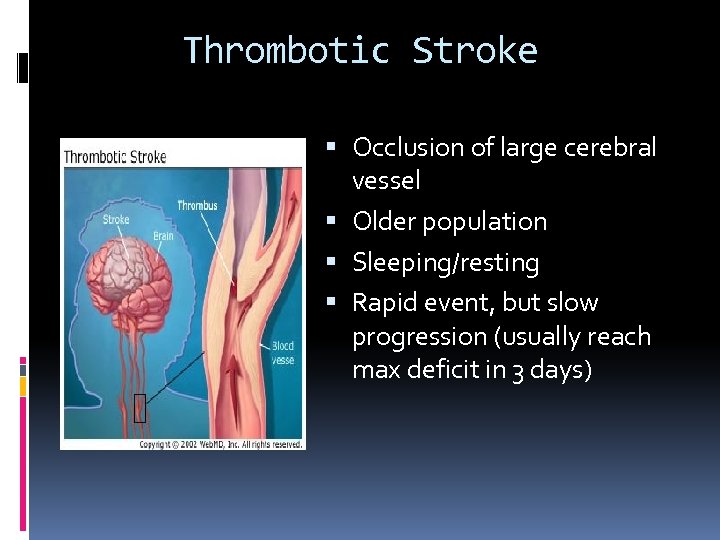
Thrombotic Stroke Occlusion of large cerebral vessel Older population Sleeping/resting Rapid event, but slow progression (usually reach max deficit in 3 days)
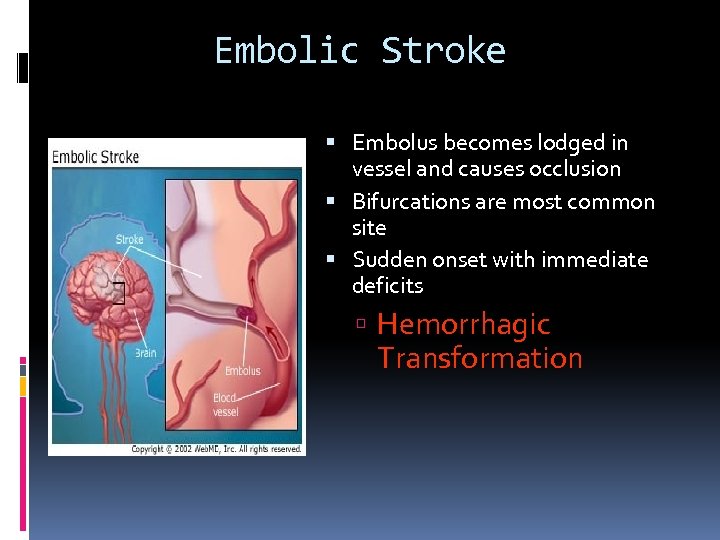
Embolic Stroke Embolus becomes lodged in vessel and causes occlusion Bifurcations are most common site Sudden onset with immediate deficits Hemorrhagic Transformation
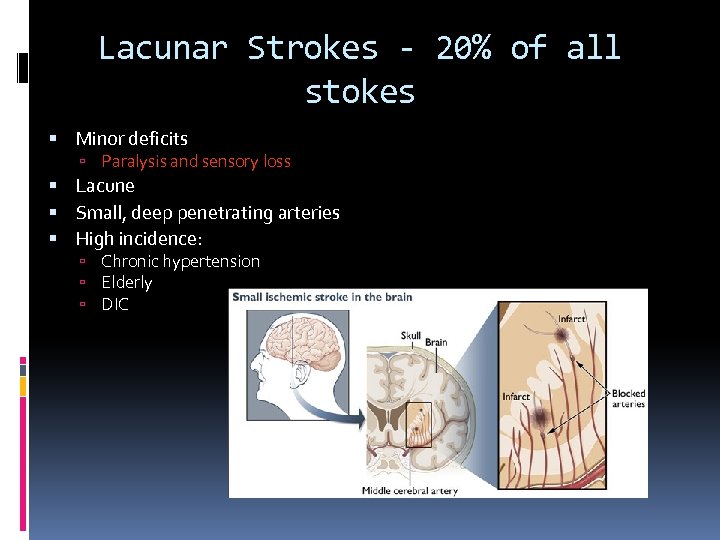
Lacunar Strokes - 20% of all stokes Minor deficits Paralysis and sensory loss Lacune Small, deep penetrating arteries High incidence: Chronic hypertension Elderly DIC
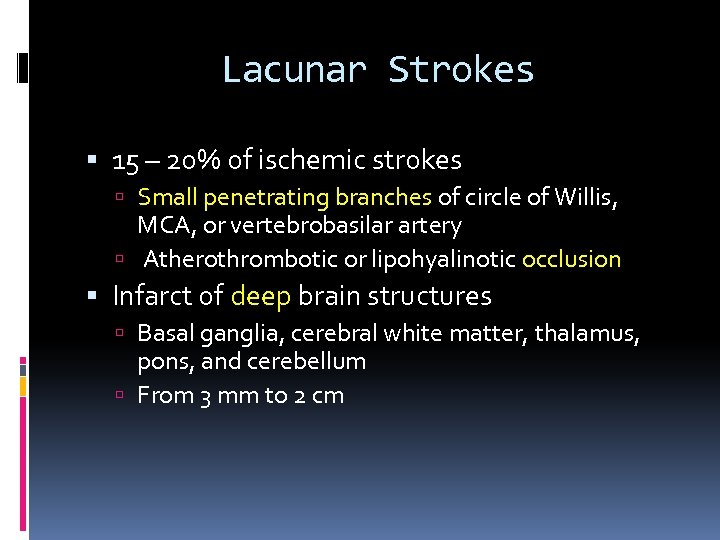
Lacunar Strokes 15 – 20% of ischemic strokes Small penetrating branches of circle of Willis, MCA, or vertebrobasilar artery Atherothrombotic or lipohyalinotic occlusion Infarct of deep brain structures Basal ganglia, cerebral white matter, thalamus, pons, and cerebellum From 3 mm to 2 cm
Lacunar Stroke Syndromes Well-defined syndromes Pure motor hemiparesis (with dysarthria) Pure sensory stroke (loss or paresthesias) Dysarthria-clumsy hand (with contralateral face and tongue weakness) Ataxia-hemiparesis (contralateral face and leg weakness) Isolated motor-sensory stroke
Risk factors Diabetes Hypertension Polycythemia Variable course progressing over days Fluctuating; progressing in steps; or remitting Preceded by TIAs in 25% Without headache or vomiting
Remember Lacunar Strokes
Transient Ischemic Attack “Sudden, focal neurologic deficit lasting less than 24 hours, confined to an area of the brain or eye perfused by a specific artery. ” Based on assumption that TIAs do not cause infarction or other permanent brain injury. Time criterion is arbitrary.
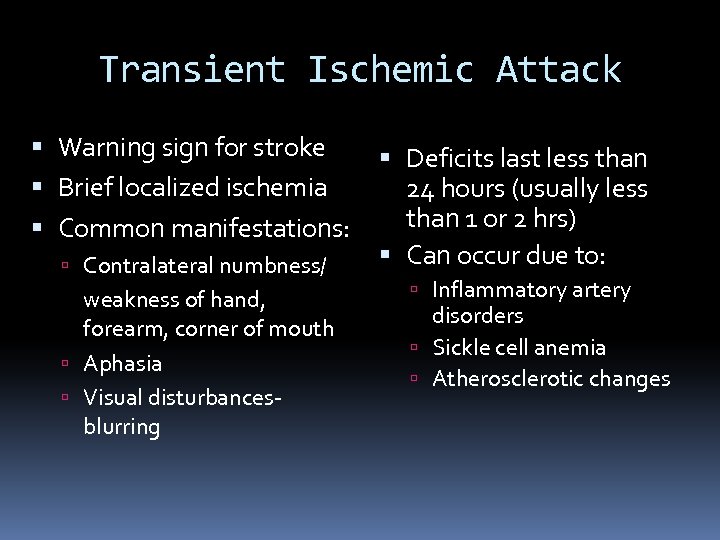
Transient Ischemic Attack Warning sign for stroke Brief localized ischemia Common manifestations: Contralateral numbness/ weakness of hand, forearm, corner of mouth Aphasia Visual disturbancesblurring Deficits last less than 24 hours (usually less than 1 or 2 hrs) Can occur due to: Inflammatory artery disorders Sickle cell anemia Atherosclerotic changes
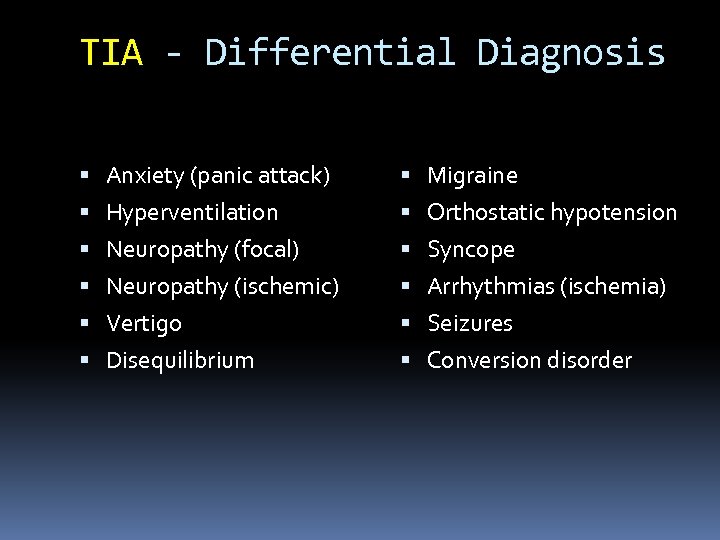
TIA - Differential Diagnosis Anxiety (panic attack) Migraine Hyperventilation Orthostatic hypotension Neuropathy (focal) Syncope Neuropathy (ischemic) Arrhythmias (ischemia) Vertigo Seizures Disequilibrium Conversion disorder
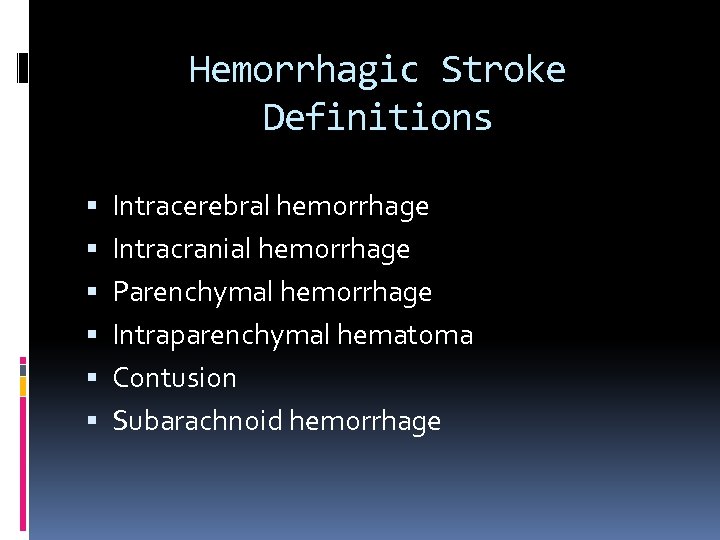
Hemorrhagic Stroke Definitions Intracerebral hemorrhage Intracranial hemorrhage Parenchymal hemorrhage Intraparenchymal hematoma Contusion Subarachnoid hemorrhage
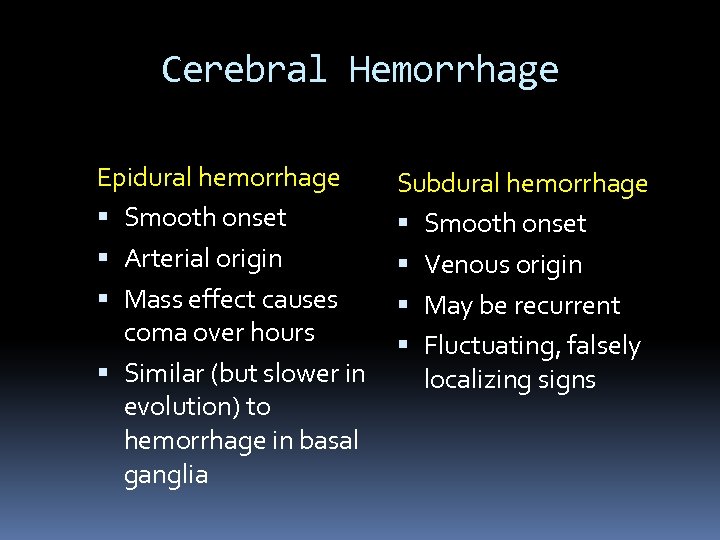
Cerebral Hemorrhage Epidural hemorrhage Smooth onset Arterial origin Mass effect causes coma over hours Similar (but slower in evolution) to hemorrhage in basal ganglia Subdural hemorrhage Smooth onset Venous origin May be recurrent Fluctuating, falsely localizing signs
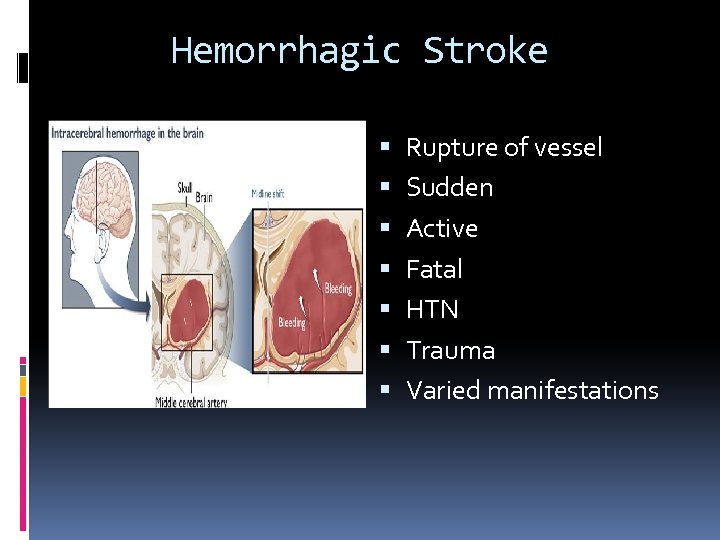
Hemorrhagic Stroke Rupture of vessel Sudden Active Fatal HTN Trauma Varied manifestations
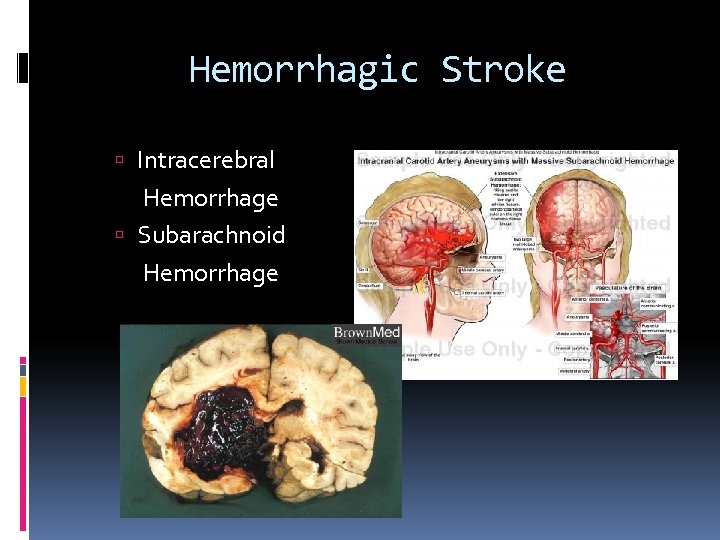
Hemorrhagic Stroke Intracerebral Hemorrhage Subarachnoid Hemorrhage
Pathophysiology Hemorrhagic Stroke Changes in vasculature Tear or rupture Hemorrhage Decreased perfusion Clotting Edema Increased intracranial pressure Cortical irritation
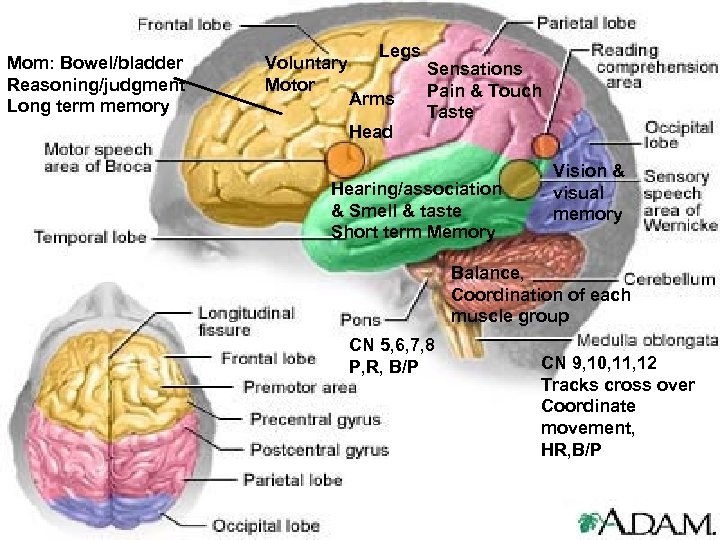
Mom: Bowel/bladder Reasoning/judgment Long term memory Voluntary Motor Legs Arms Head Sensations Pain & Touch Taste Hearing/association & Smell & taste Short term Memory Vision & visual memory Balance, Coordination of each muscle group CN 5, 6, 7, 8 P, R, B/P CN 9, 10, 11, 12 Tracks cross over Coordinate movement, HR, B/P
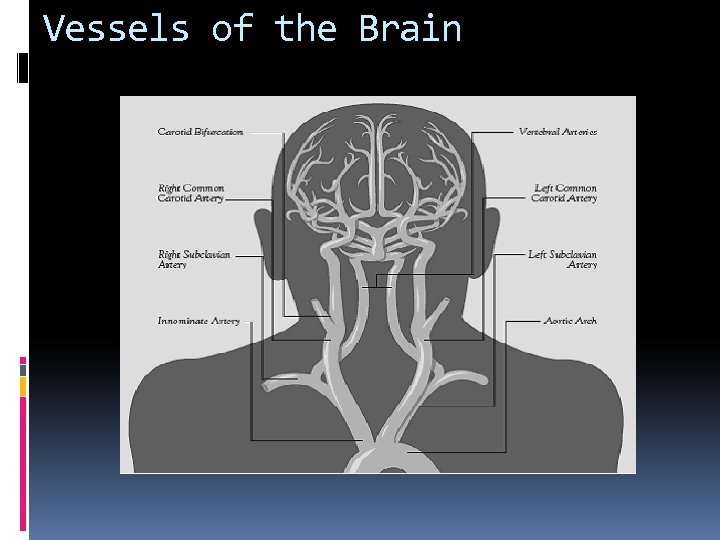
Vessels of the Brain
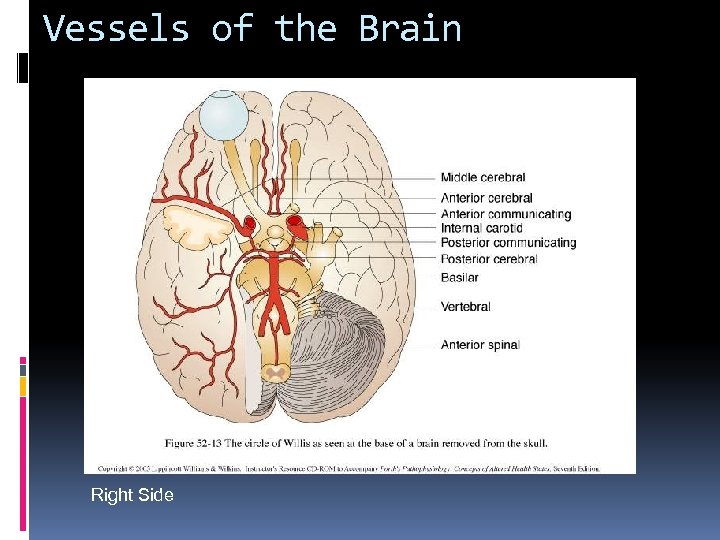
Vessels of the Brain Right Side
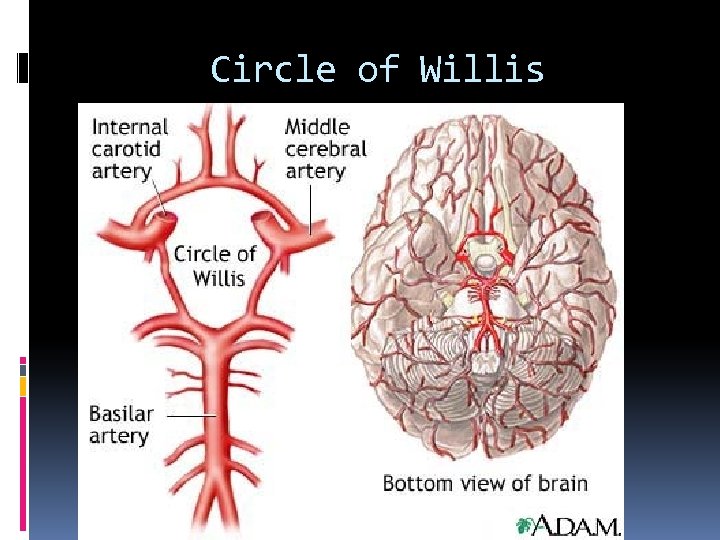
Circle of Willis
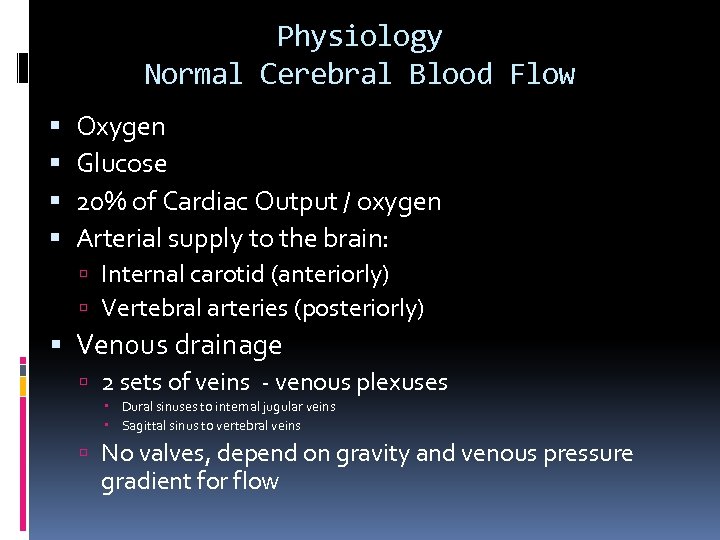
Physiology Normal Cerebral Blood Flow Oxygen Glucose 20% of Cardiac Output / oxygen Arterial supply to the brain: Internal carotid (anteriorly) Vertebral arteries (posteriorly) Venous drainage 2 sets of veins - venous plexuses Dural sinuses to internal jugular veins Sagittal sinus to vertebral veins No valves, depend on gravity and venous pressure gradient for flow
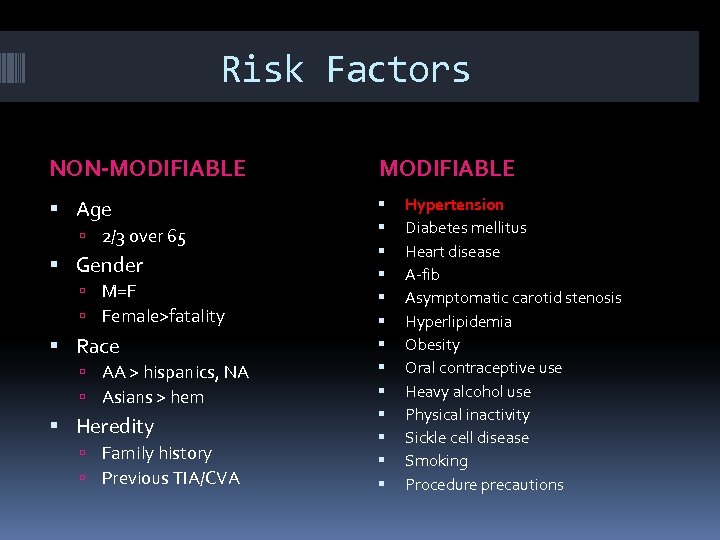
Risk Factors NON-MODIFIABLE Age 2/3 over 65 Gender M=F Female>fatality Race AA > hispanics, NA Asians > hem Heredity Family history Previous TIA/CVA Hypertension Diabetes mellitus Heart disease A-fib Asymptomatic carotid stenosis Hyperlipidemia Obesity Oral contraceptive use Heavy alcohol use Physical inactivity Sickle cell disease Smoking Procedure precautions
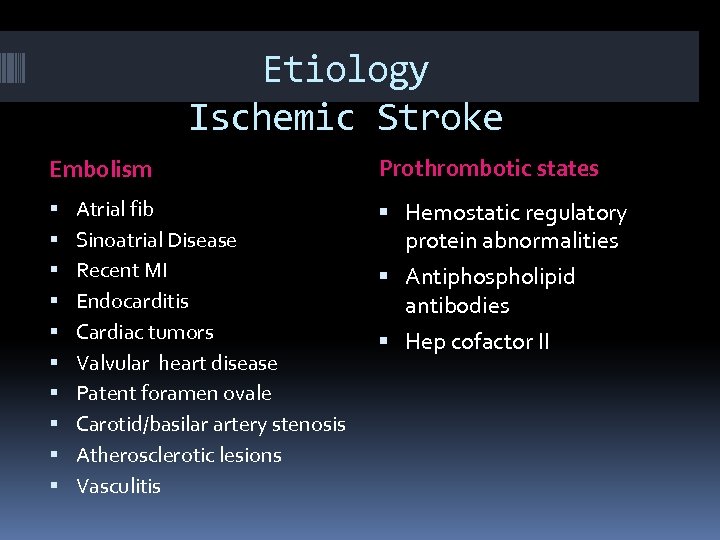
Etiology Ischemic Stroke Embolism Atrial fib Sinoatrial Disease Recent MI Endocarditis Cardiac tumors Valvular heart disease Patent foramen ovale Carotid/basilar artery stenosis Atherosclerotic lesions Vasculitis Prothrombotic states Hemostatic regulatory protein abnormalities Antiphospholipid antibodies Hep cofactor II
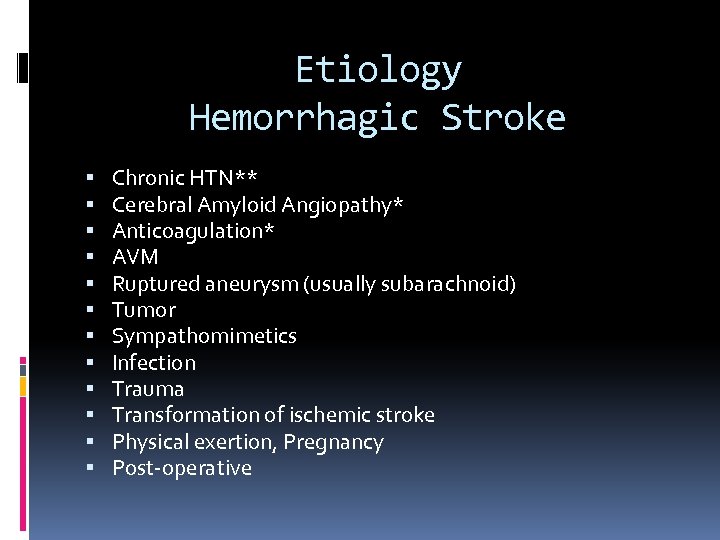
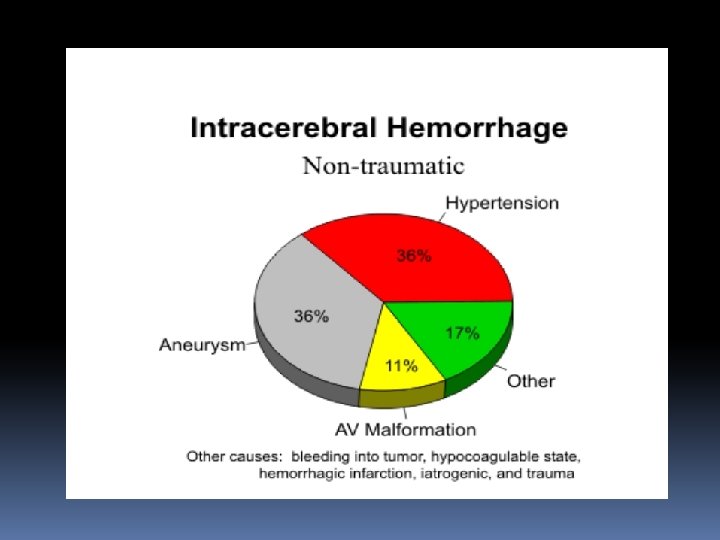
Etiology Hemorrhagic Stroke Chronic HTN** Cerebral Amyloid Angiopathy* Anticoagulation* AVM Ruptured aneurysm (usually subarachnoid) Tumor Sympathomimetics Infection Trauma Transformation of ischemic stroke Physical exertion, Pregnancy Post-operative
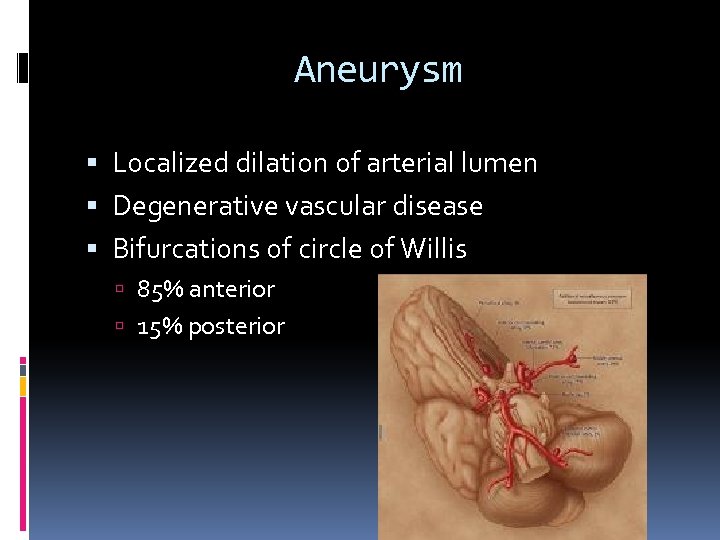
Aneurysm Localized dilation of arterial lumen Degenerative vascular disease Bifurcations of circle of Willis 85% anterior 15% posterior
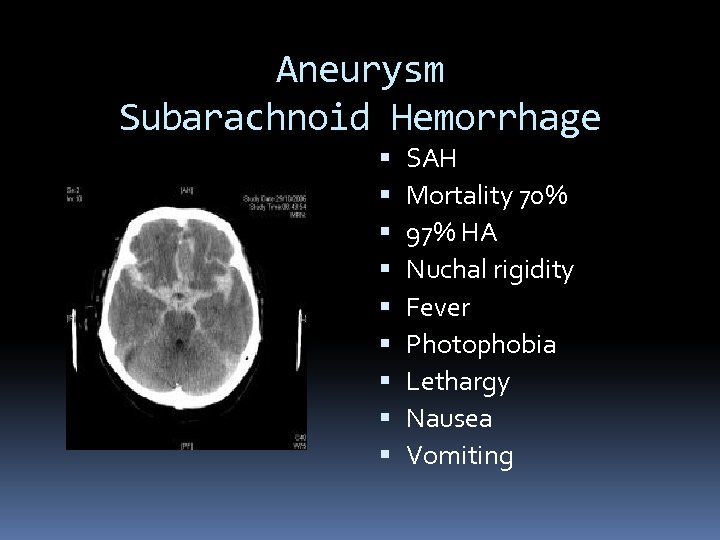
Aneurysm Subarachnoid Hemorrhage SAH Mortality 70% 97% HA Nuchal rigidity Fever Photophobia Lethargy Nausea Vomiting
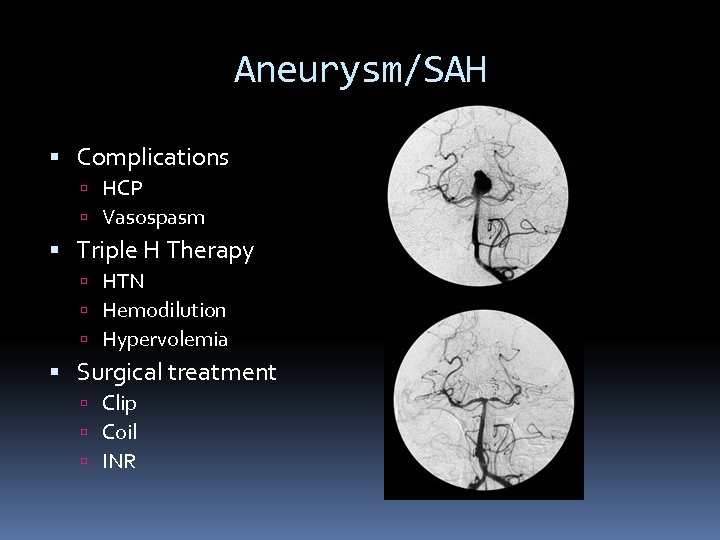
Aneurysm/SAH Complications HCP Vasospasm Triple H Therapy HTN Hemodilution Hypervolemia Surgical treatment Clip Coil INR
Nursing Management Assessment Monitoring BP TCDs CBC Preventing complications Bowel program DVT prophylaxis Seizure prophylaxis Psychological support Discharge planning
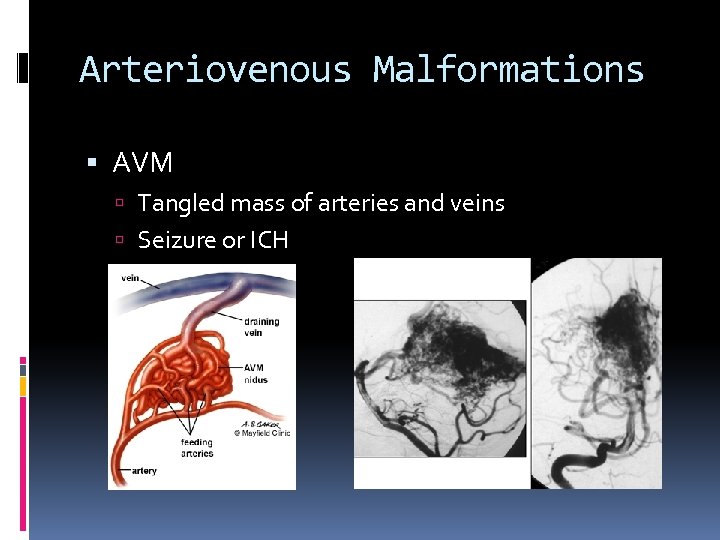
Arteriovenous Malformations AVM Tangled mass of arteries and veins Seizure or ICH
Presentation Sudden onset Focal neurological deficit Progresses over minutes to hours HA, N/V, <<LOC, HTN Depends on location
Treatment of AVM Endovascular Neurosurgery Radiosurgery
Manifestations by Vessel Vertebral Artery Pain in face, nose, or eye Numbness and weakness of face (involved side) Gait disturbances Dysphagia Dysarthria (motor speech)
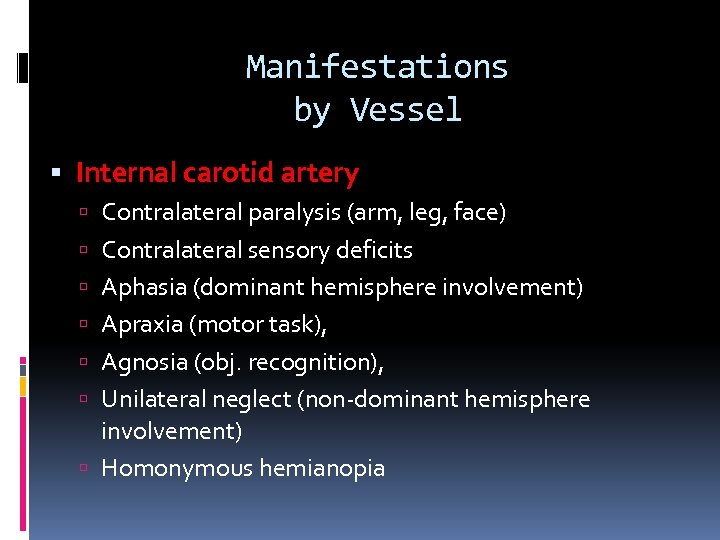
Manifestations by Vessel Internal carotid artery Contralateral paralysis (arm, leg, face) Contralateral sensory deficits Aphasia (dominant hemisphere involvement) Apraxia (motor task), Agnosia (obj. recognition), Unilateral neglect (non-dominant hemisphere involvement) Homonymous hemianopia
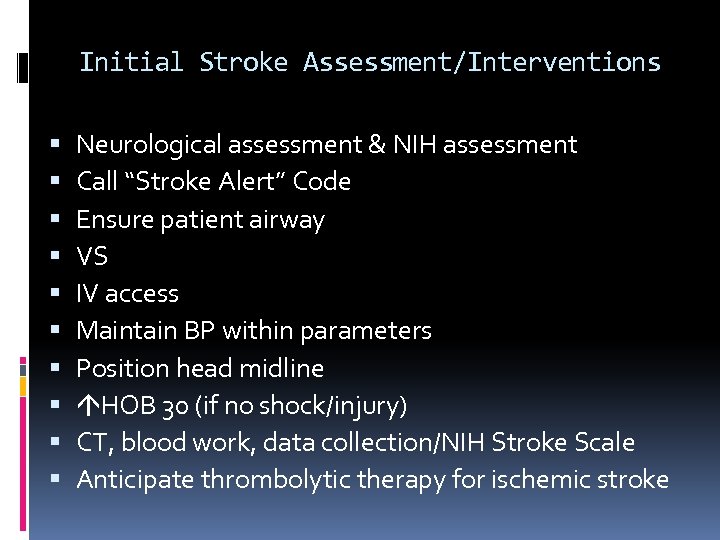
Initial Stroke Assessment/Interventions Neurological assessment & NIH assessment Call “Stroke Alert” Code Ensure patient airway VS IV access Maintain BP within parameters Position head midline HOB 30 (if no shock/injury) CT, blood work, data collection/NIH Stroke Scale Anticipate thrombolytic therapy for ischemic stroke
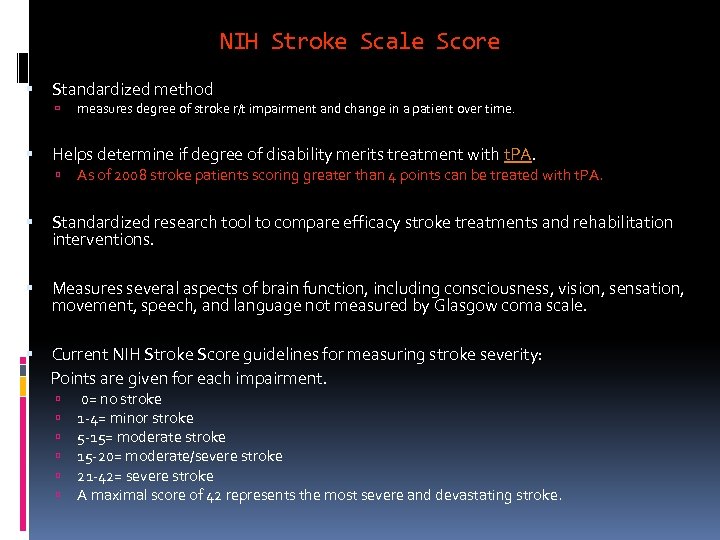
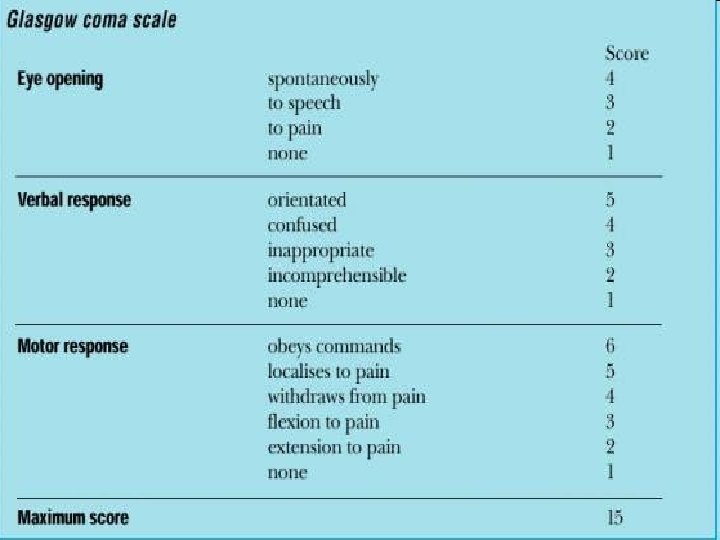
NIH Stroke Scale Score Standardized method measures degree of stroke r/t impairment and change in a patient over time. Helps determine if degree of disability merits treatment with t. PA. As of 2008 stroke patients scoring greater than 4 points can be treated with t. PA. Standardized research tool to compare efficacy stroke treatments and rehabilitation interventions. Measures several aspects of brain function, including consciousness, vision, sensation, movement, speech, and language not measured by Glasgow coma scale. Current NIH Stroke Score guidelines for measuring stroke severity: Points are given for each impairment. 0= no stroke 1 -4= minor stroke 5 -15= moderate stroke 15 -20= moderate/severe stroke 21 -42= severe stroke A maximal score of 42 represents the most severe and devastating stroke.

Comic Relief
Question The neurologic functions that are affected by a stroke are primarily related to A. the amount of tissue area involved. B. the rapidity of the onset of symptoms. C. the brain area perfused by the affected artery. D. the presence or absence of collateral circulation.
Question A patient is admitted to the hospital with a left hemiplegia. To determine the size and location and to ascertain whether a stroke is ischemic or hemorrhagic, the nurse anticipated that the health care provider will request a A. CT scan. B. lumbar puncture. C. cerebral angiogram. D. PET scan.
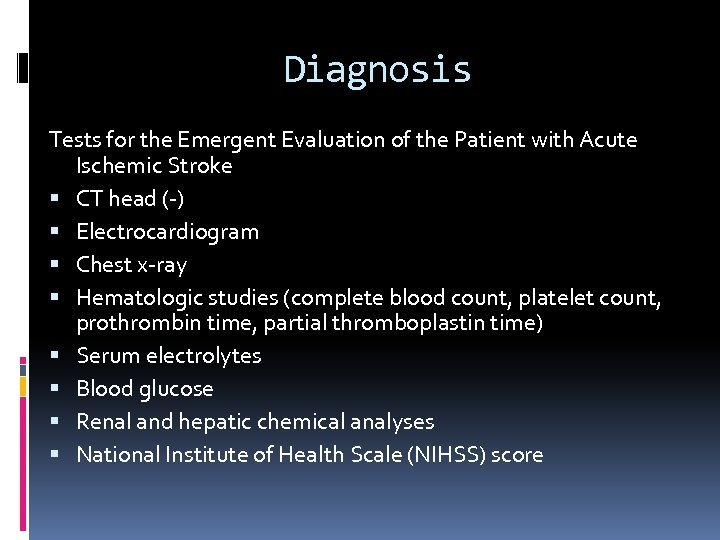
Diagnosis Tests for the Emergent Evaluation of the Patient with Acute Ischemic Stroke CT head (-) Electrocardiogram Chest x-ray Hematologic studies (complete blood count, platelet count, prothrombin time, partial thromboplastin time) Serum electrolytes Blood glucose Renal and hepatic chemical analyses National Institute of Health Scale (NIHSS) score
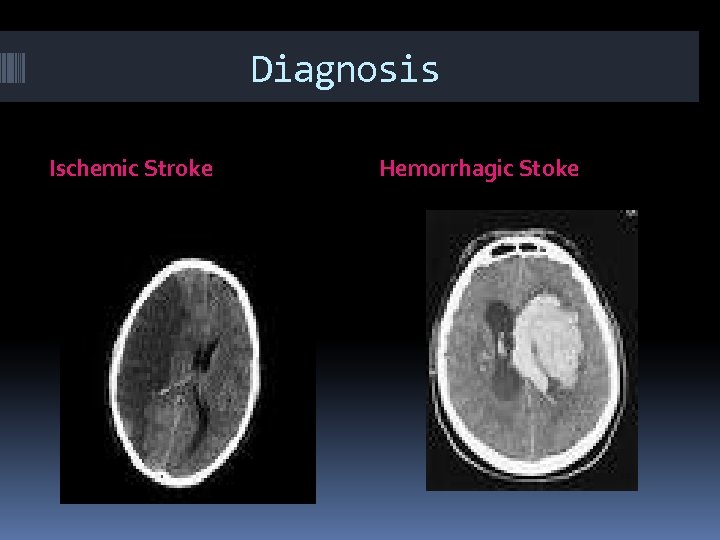
Diagnosis Ischemic Stroke Hemorrhagic Stoke
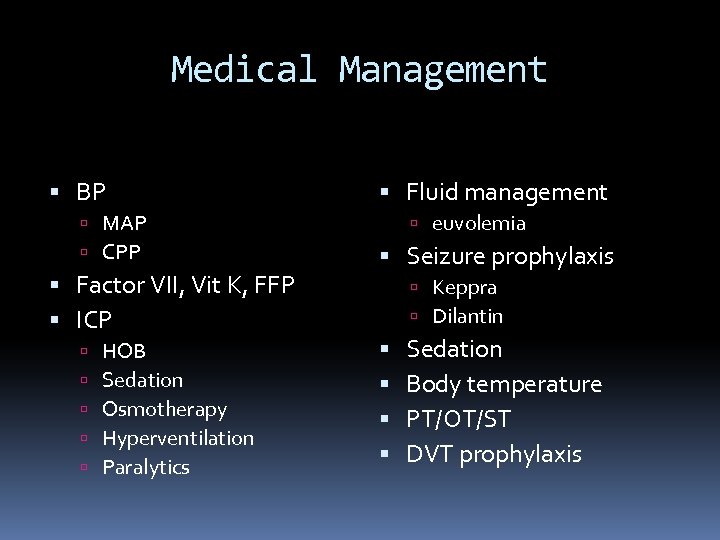
Medical Management BP MAP CPP Factor VII, Vit K, FFP ICP HOB Sedation Osmotherapy Hyperventilation Paralytics Fluid management euvolemia Seizure prophylaxis Keppra Dilantin Sedation Body temperature PT/OT/ST DVT prophylaxis
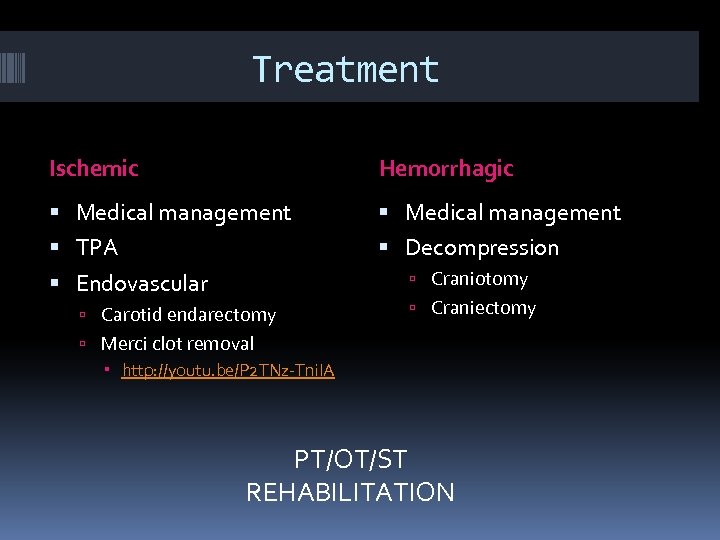
Treatment Ischemic Hemorrhagic Medical management TPA Decompression Craniotomy Endovascular Carotid endarectomy Craniectomy Merci clot removal http: //youtu. be/P 2 TNz-Tni. IA PT/OT/ST REHABILITATION
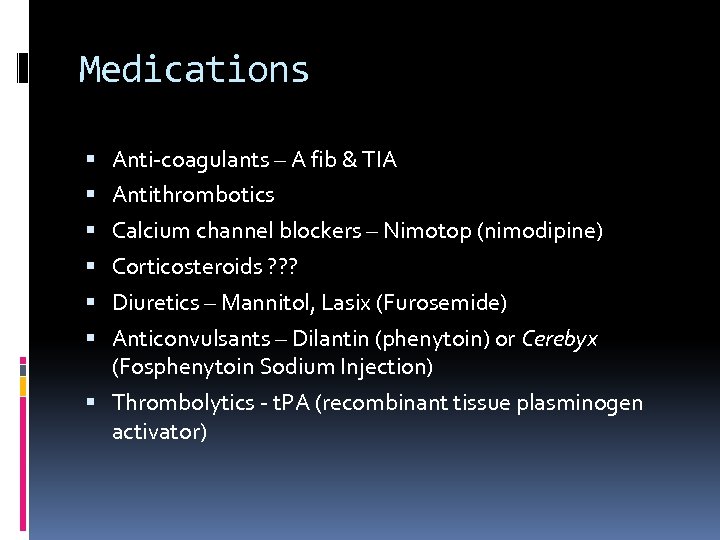
Medications Anti-coagulants – A fib & TIA Antithrombotics Calcium channel blockers – Nimotop (nimodipine) Corticosteroids ? ? ? Diuretics – Mannitol, Lasix (Furosemide) Anticonvulsants – Dilantin (phenytoin) or Cerebyx (Fosphenytoin Sodium Injection) Thrombolytics - t. PA (recombinant tissue plasminogen activator)
Medications Thrombolytics Recombinant Alteplase (rt. PA) Activase, Tissue plasminogen activator Treatment must be initiated promptly after CT to R/O bleed Systemic within 3 hours of onset of symptoms Intra-arterial within 6 hours of symptoms Some exclusions: Seizure at onset Subarachnoid hemorrhage Trauma within 3 months History of prior intracranial hemorrhage AV malformation or aneurysm Surgery 14 days, pregnancy, Cardiac cath. 7 days
Neurosurgical Management Craniotomy Craniectomy EVD placement ICP monitor placement
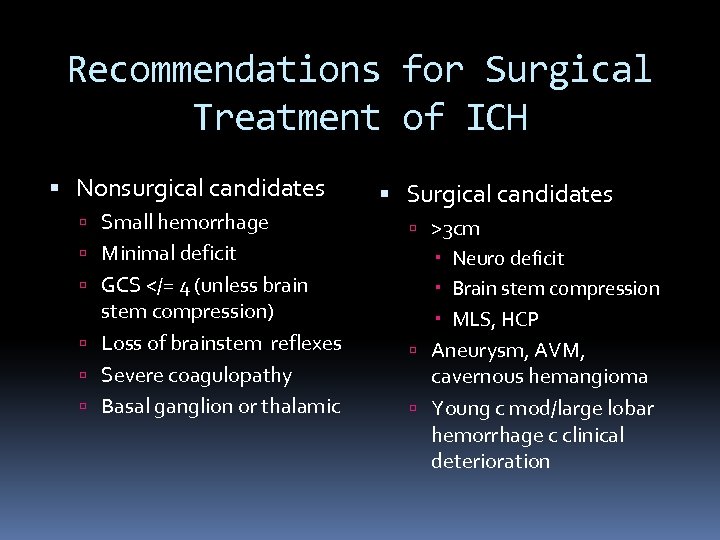
Recommendations for Surgical Treatment of ICH Nonsurgical candidates Small hemorrhage Minimal deficit GCS </= 4 (unless brain stem compression) Loss of brainstem reflexes Severe coagulopathy Basal ganglion or thalamic Surgical candidates >3 cm Neuro deficit Brain stem compression MLS, HCP Aneurysm, AVM, cavernous hemangioma Young c mod/large lobar hemorrhage c clinical deterioration
Reducing Primary Risk Obstructive sleep apnea Homocysteine folate, B 6, B 12 Hypertension – morning BP surge Smoking 50% risk reduction in 1 yr Hyperlipidemia statins Migraine triptans Drugs – cocaine, ephedra, PPA
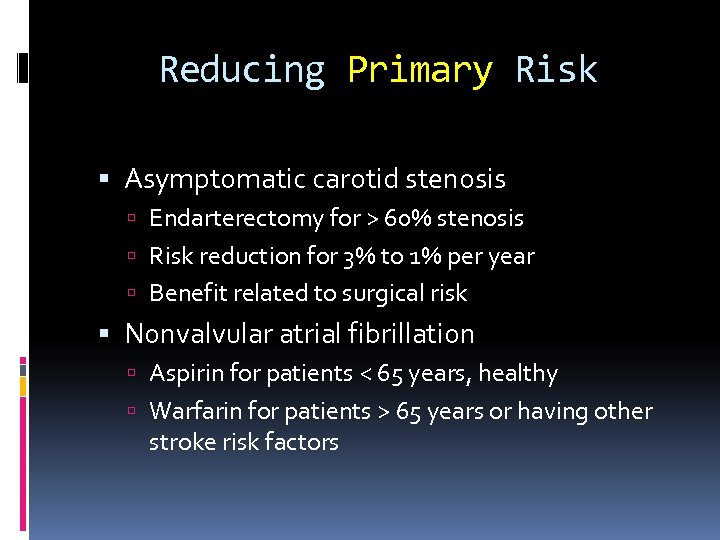
Reducing Primary Risk Asymptomatic carotid stenosis Endarterectomy for > 60% stenosis Risk reduction for 3% to 1% per year Benefit related to surgical risk Nonvalvular atrial fibrillation Aspirin for patients < 65 years, healthy Warfarin for patients > 65 years or having other stroke risk factors
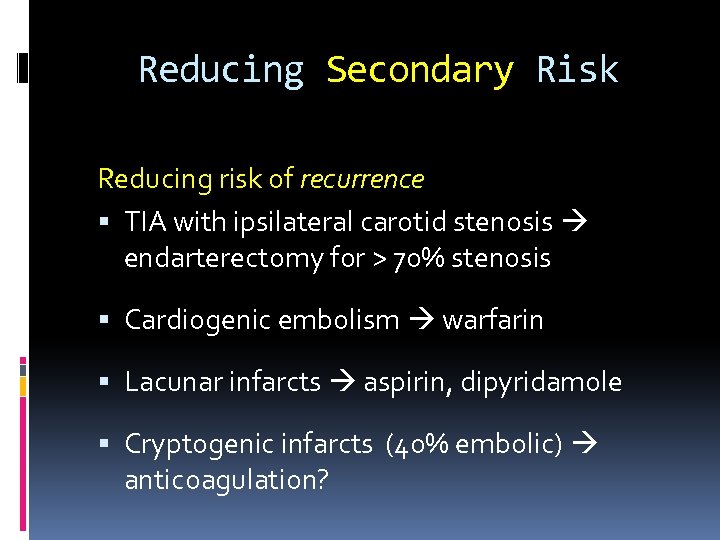
Reducing Secondary Risk Reducing risk of recurrence TIA with ipsilateral carotid stenosis endarterectomy for > 70% stenosis Cardiogenic embolism warfarin Lacunar infarcts aspirin, dipyridamole Cryptogenic infarcts (40% embolic) anticoagulation?
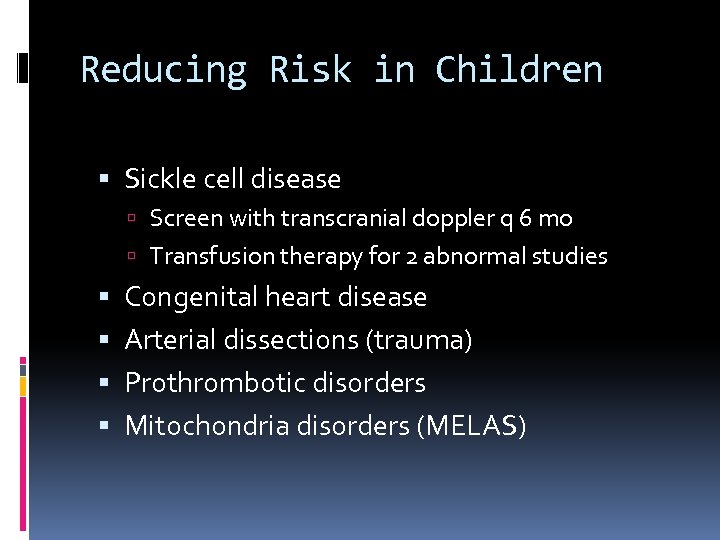
Reducing Risk in Children Sickle cell disease Screen with transcranial doppler q 6 mo Transfusion therapy for 2 abnormal studies Congenital heart disease Arterial dissections (trauma) Prothrombotic disorders Mitochondria disorders (MELAS)
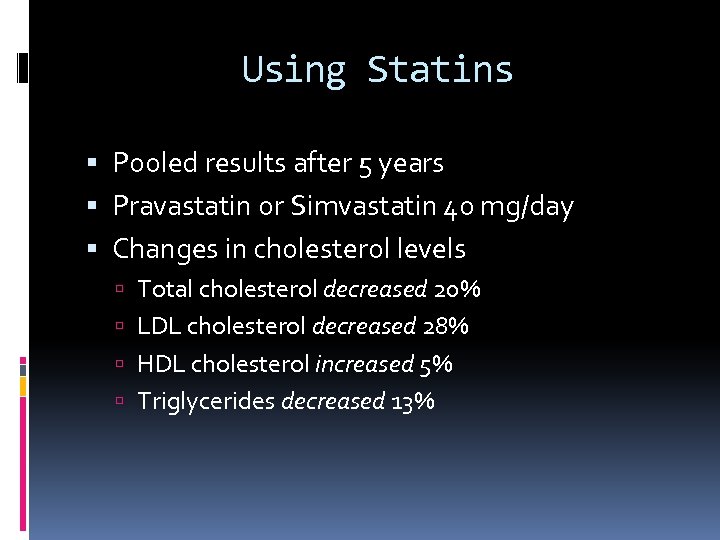
Using Statins Pooled results after 5 years Pravastatin or Simvastatin 40 mg/day Changes in cholesterol levels Total cholesterol decreased 20% LDL cholesterol decreased 28% HDL cholesterol increased 5% Triglycerides decreased 13%
Using Statins Reducing LDL cholesterol by 1 mmol/L 22% stroke reduction in patients with known vascular disease 6% stroke reduction in patients without known vascular disease 28% reduction in thromboembolic stroke
Complications Increased intracranial pressure Rebleeding Vasospasm HCP Death
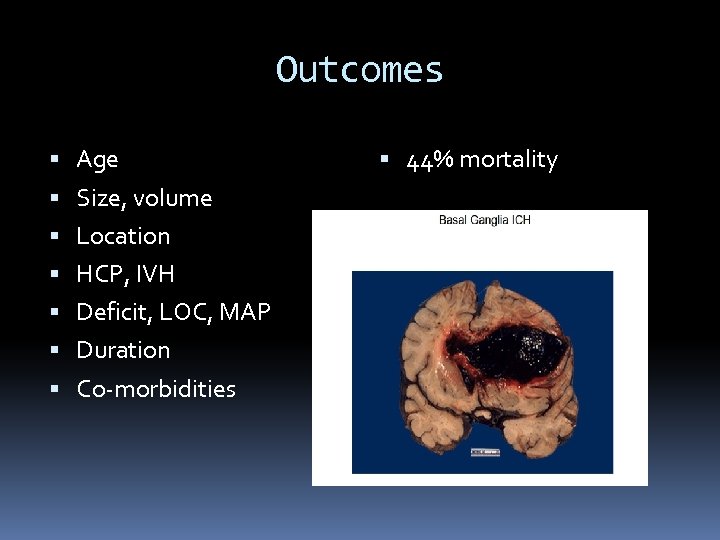
Outcomes Age Size, volume Location HCP, IVH Deficit, LOC, MAP Duration Co-morbidities 44% mortality
References AANN Core Curriculum for Neuroscience Louis, MO. Nursing, 4 th Ed. 2004. Saunders. St. Broderick, J. , et. al. (1999) Guidelines for the management of spontaneous intracerebral hemorrhage. AHA. El-Mitwali, A. , Malkoff, M. (2001) Intracerebral hemorrhage. The Internet Journal of Neurosurgery. 1. 1. Greenberg, Mark. (2006). Handbook of Neurosurgery. Greenberg Graphics, Tampa, Florida.
ee55976f793f444dc5d4ec77554a73b0.ppt