fa9dc216988dbccc91a991d25c683a57.ppt
- Количество слайдов: 21
Primary Health Care: international experiences & ‘best practices’ Health Care Neighbourhoods and Integrated Care Implications for the Development of Patient Centred Medical and Health Care Homes Sydney, December 01 2016 Professor Chris van Weel Radboud University Nijmegen, the Netherlands Australian National University 1

International concerns driving health reforms and drive primary health care policy • Access – Equity – ressponsiveness to highest need • Affordability – Financial and Societal Terms – Aging and Chrinic Health Problems • Availability – (Community based) Facilities – Discipline-mixture and their professional Training • Appropriateness – Quality & Safety – Autonomy, self-reliance – Inter-sectorial – socio-economic well-being • Accountability – From reactive to pro-active approach 2
Policy Priorities • Primary Health Care – Since 1941 -1948 NL, UK – WHO Alma Ata 1978 – WHO WHR 2008 ‘primary health care now more than ever’ • Universal Health Coverage – Related UN Sustainable Development Goals – Address financial burden of poor health – WHO: to be realised through PHC – need of ‘PHC-literacy’ • Cost-effectiveness • Avoidance of waste of resources – Co-ordination within health system and with other sectors – Multi-disciplinary teams, community centers, PCMH 3
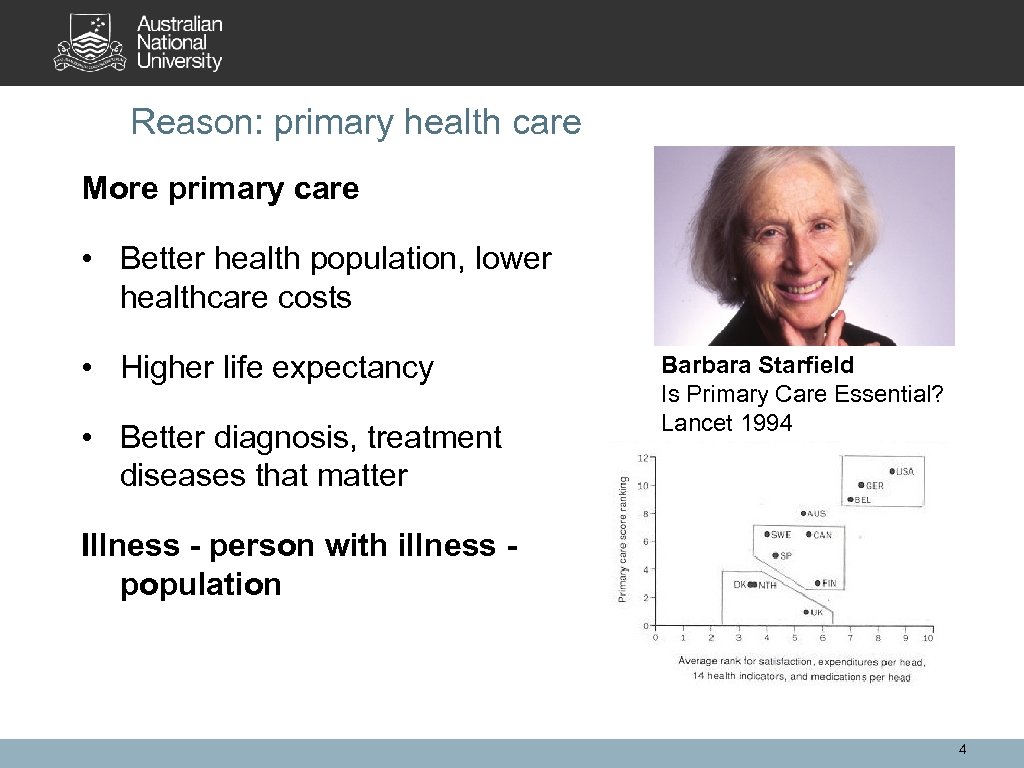
Reason: primary health care More primary care • Better health population, lower healthcare costs • Higher life expectancy • Better diagnosis, treatment diseases that matter Barbara Starfield Is Primary Care Essential? Lancet 1994 Illness - person with illness population 4
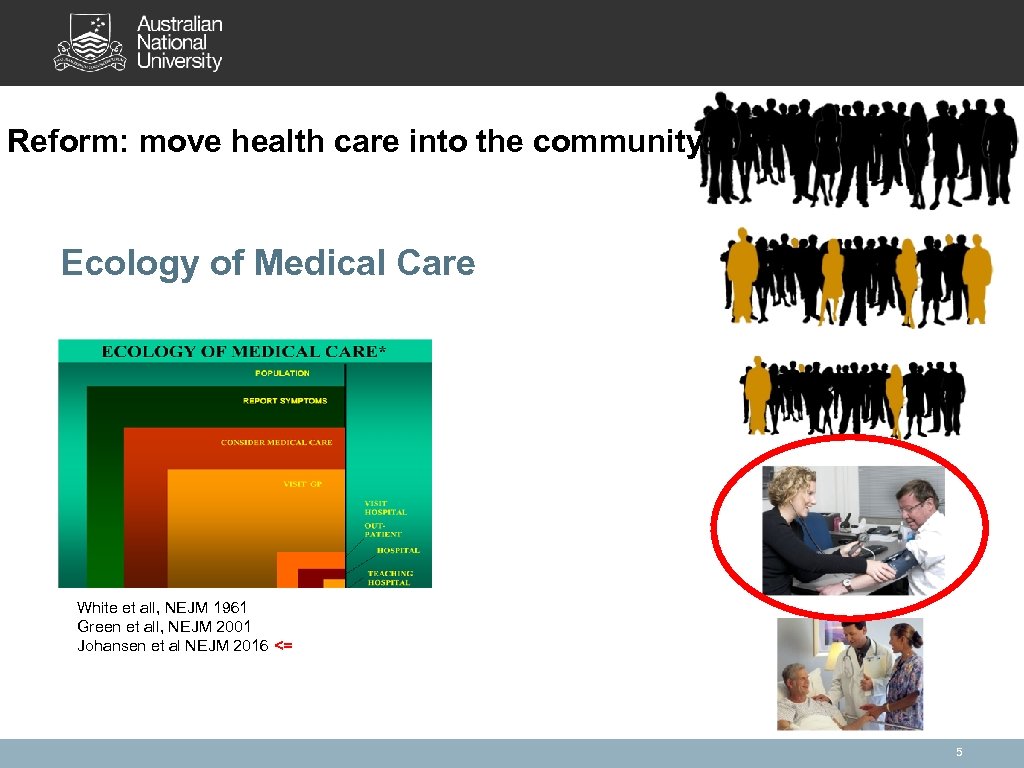
Reform: move health care into the community Ecology of Medical Care White et all, NEJM 1961 Green et all, NEJM 2001 Johansen et al NEJM 2016 <= 5
Community-based PHC Paradigm Shift: • PHC • Person and population (people) centered • Continuity, comprehensiveness, coordination • Social Context, Co-multimorbidity • Evidence-based Health Policy • Health Systems, Education, Research • Disease-specificity in diagnosis treatment and management 6
Role, Function, Values Primary Health Care* ‘First’ contact o All health problems, all individuals, all stages o No pre-selection, undifferentiated o Diagnostic and understanding Selectively used contacts o Reasons for contact as important as the health problem o Needs, expectations, equity o Autonomy and self-efficacy Community – population basis o Community specific, needs, social determinants health Continuity over time o Variety of (health) problems in same individual o Personal understanding determines proceeding o Trust * Wonca Europe. Definition of the general practitioner/family physician. http: //www. woncaeurope. org/sites/default/files/documents/Definition%20 EURACTshort%20 version%20 revised%202011. pdf 7
From general practice to primary health care* From WHO Resolution WHA 62. 12. 2009 Primary health care, including health system strengthening. Professionals: • • Nurses, Midwifes, Family Physicians, Allied Health Professionals The team * WHO: Resolution WHA 62. 12. Primary health care, including health system strengthening. In: Sixty-second World Health Assembly, Geneva, 18– 22 May 2009. Resolutions and decisions, and annexes. Geneva: World Health Organization; 2009: 16– 19 (WHA 62/2009/REC/1). 8
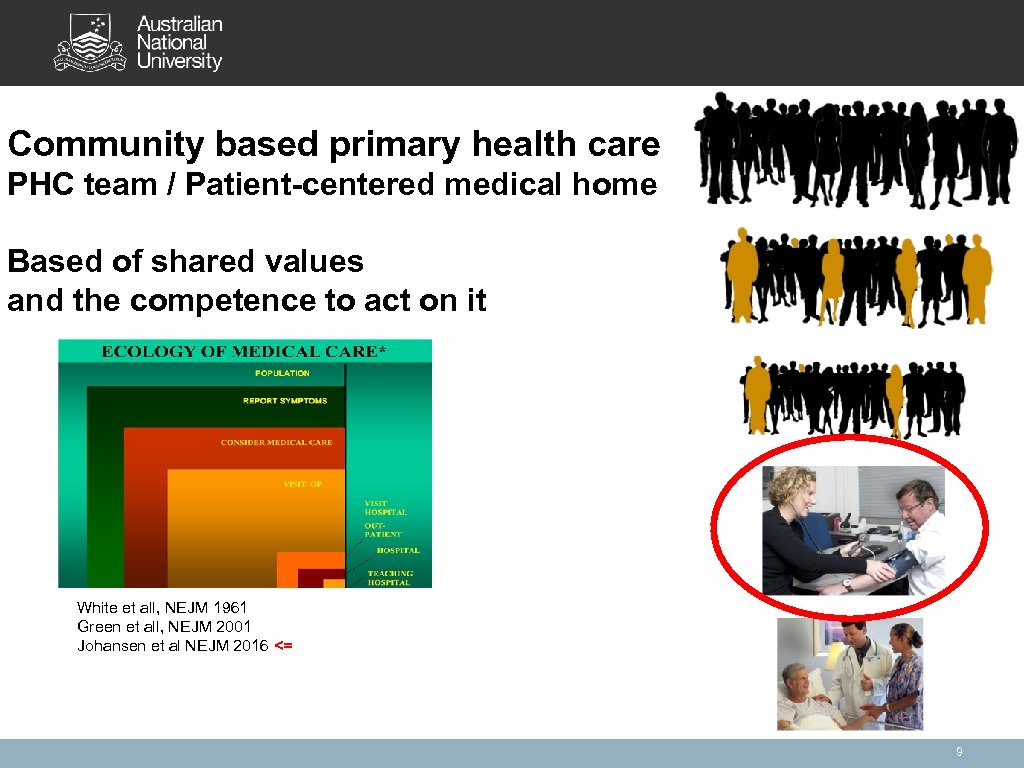
Community based primary health care PHC team / Patient-centered medical home Based of shared values and the competence to act on it White et all, NEJM 1961 Green et all, NEJM 2001 Johansen et al NEJM 2016 <= 9
Determinants of effective Primary Health Care Structure health care • Level 1. Primary Health Care Structure – Access to Health Care through PHC – Specialist, Hospital Care through Referral • Level 2. Personal Relation – Listing of Patients with a GP/FP – Capitation payment as main source financing • Level 3. Community relation – Community Health Centres – Multidisciplinary teams • Level 4. Intersectorial structure – Social determinants of health – Integrating health and welfare 10
Experiences from The Netherlands – 1941 Sick Fund Decree – affordable health care, population needs, equity • ‘Primary health care structure’, with patients listed with a GP, capitation payment – 1956 DCGP – paradigm shift, person centeredness of health care • Start of academic development • 1968 Founding University Departments, chairs general practice, all schools • Teaching, Specialty Training (1973), Research – 1975 White Paper ‘Primary Health Care’ population/community centeredness • Support multidisciplinary health centres • Rewarding of pro-active planning of community health care – 1986 GP Research, DCGP Quality program – EBM, primary-hospital care • Research for practice, guideline program • Individual and practice audit & accreditation – 2006 Introduction mandatory for-profit health insurance – innovative initiatives • • • Support for collaborative partnerships public health – PHC – hospital care Inter-sectorial collaboration – ‘community diagnosis’ – social determinants of health Strong focus on public health – primary health care interaction 11
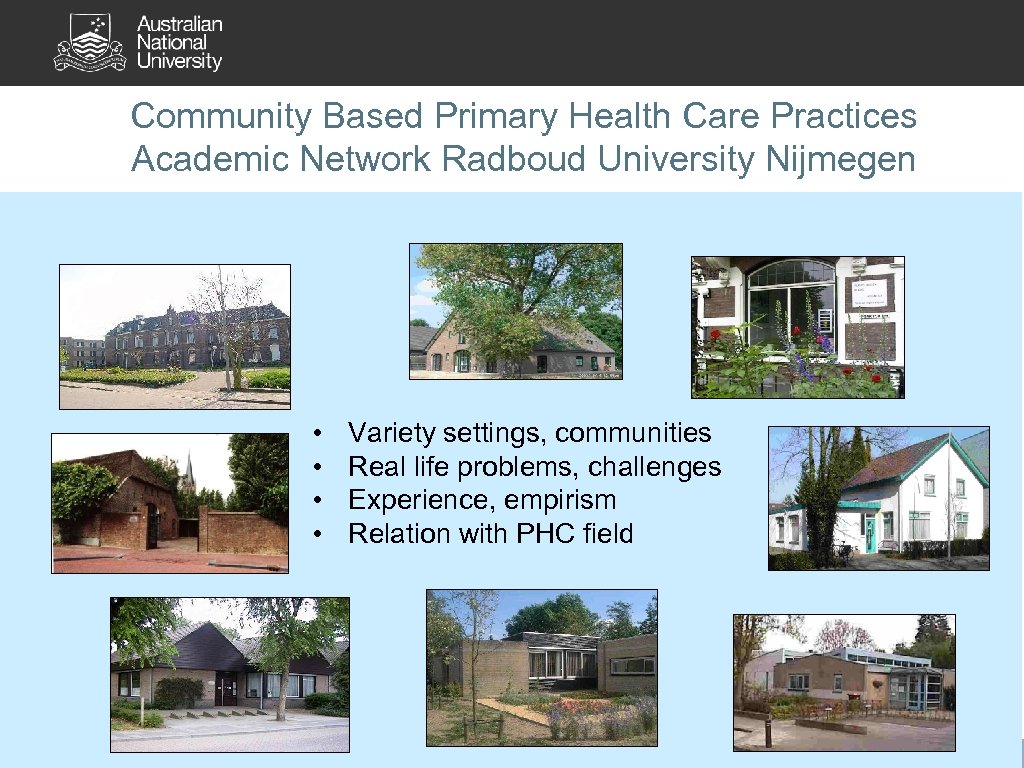
Community Based Primary Health Care Practices Academic Network Radboud University Nijmegen • • Variety settings, communities Real life problems, challenges Experience, empirism Relation with PHC field
Primary health care teams NL: ‘community based’ related to defined ‘practice population’ GP acknowledging primary health care leadership Patient Centered Medical Home US: ‘individual patient’ centered aimed to impose co-ordination of care that was not available directed at the interface hospital – primary health care
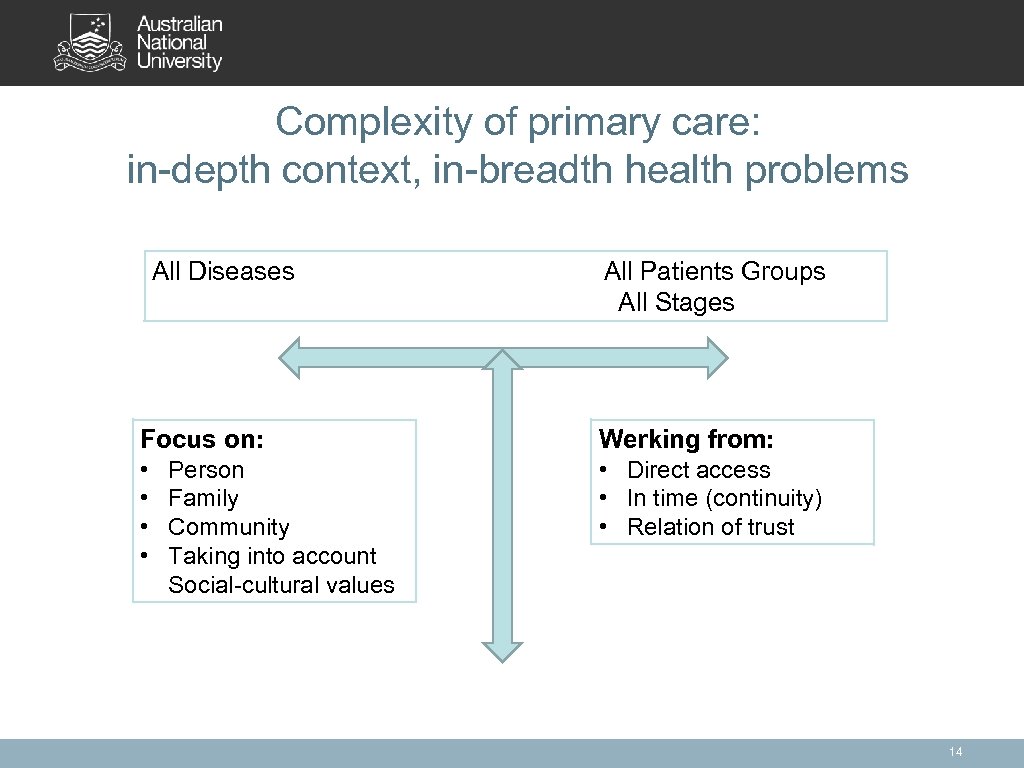
Complexity of primary care: in-depth context, in-breadth health problems All Diseases All Patients Groups All Stages Focus on: Werking from: • • • Direct access • In time (continuity) • Relation of trust Person Family Community Taking into account Social-cultural values 14
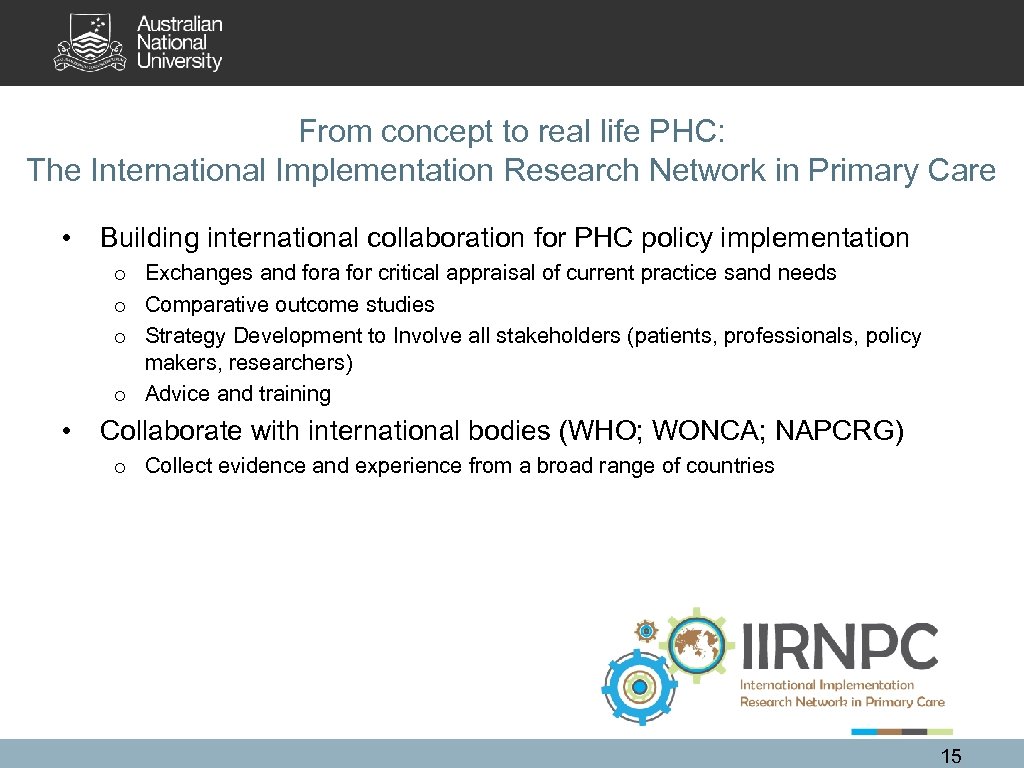
From concept to real life PHC: The International Implementation Research Network in Primary Care • Building international collaboration for PHC policy implementation o Exchanges and fora for critical appraisal of current practice sand needs o Comparative outcome studies o Strategy Development to Involve all stakeholders (patients, professionals, policy makers, researchers) o Advice and training • Collaborate with international bodies (WHO; WONCA; NAPCRG) o Collect evidence and experience from a broad range of countries 15
Activities until now • Conferences o o o NAPCRG pre-conferences 2013, 2014, 2015 WONCA AP Conference 2015 WONCA SA Conference 2016 WONCA World Conference 2016 NAPCRG Workshop 2016 • Publications – – Annals Family Medicine 2015 http: //www. annfammed. org/content/13/1/86. full. pdf+html Annals Family Medicine 2016 http: //www. annfammed. org/content/14/3/279. full. pdf+html Br J Gen Pract 2016 DOI: 10. 3399/bjgp 16 X 685513 BMJ Global Health 2016; 1: e 000057. doi: 10. 1136/bmjgh-2016000057 16
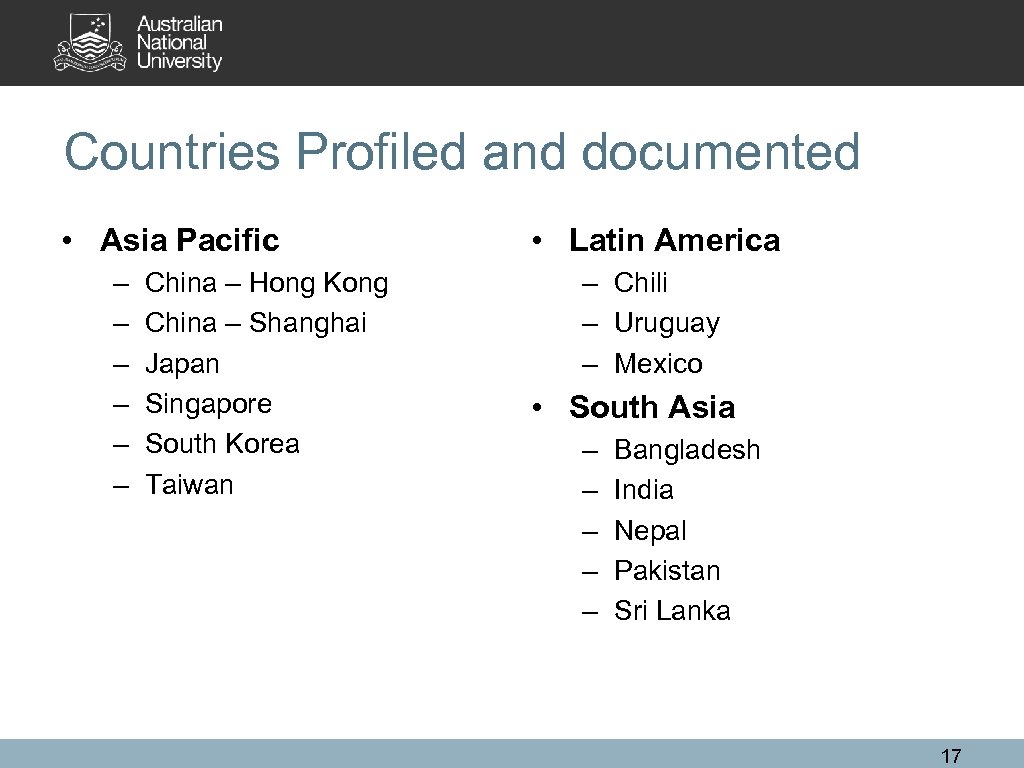
Countries Profiled and documented • Asia Pacific – – – China – Hong Kong China – Shanghai Japan Singapore South Korea Taiwan • Latin America – Chili – Uruguay – Mexico • South Asia – – – Bangladesh India Nepal Pakistan Sri Lanka 17
Summary of Findings Common Themes • • Concerns of equity – Universal Health Coverage Limited understanding of PHC (‘Black Box’), UHC and PHC as separate issues – Monitoring health reforms ignores markers of PHC (f. e. continuity; comprehensiveness) – Continuation of disease-centered care • Reforms: co-ordinated top-down policy and bottom-up implementation action – But are often disconnected • Importance of Leadership from primary health care; but: – Specialty training, and restriction to practice PHC for certified PHC specialists – Community-based teaching, research & development – Turf battles of hospital specialists, academic centers • Context-specific – Resistance to ‘health insurance’ (India) – Restrictions to practice medicine outside hospital setting (South Korea) – Victim of earlier success limited PHC (Sri Lanka) 18
Barriers in implementing PHC • Financing models based on the delivery of (often disease-specific) items of service, creating perverse incentives; • Fragmentation of services of providers working in isolation, disrupting continuity and integration of care; • Dis-balance between community based primary care and centralised hospital facilities with a ‘brain drain’ of professionals towards hospital care; • Insufficient professional training and career opportunities in the community setting; • Poor organisation of communities and service users to engage in and co-design local primary health care development and implementation and perform their role as stakeholders. 19
Importance to monitor PHC Values in health reforms, to secure true change Continuity, co-ordination, comprehensiveness of care, empowerment of individuals and communities, trust Primary health care literacy
Plans coming years Continued Advocacy PHC • • • Core function in any health system Importance of bottom-up implementation of top-down policy Key factor in realising affordable, safe effectiive Universal Health Coverage Comparative countries- studies • Role, function Community based primary health care – From physician practices to multidisciplinary teams – Involvement – participation of patients – community leaders – Focus on Social Determinants of Health, intersectorial – Use of ppt template Workshop 2018 WONCA World Conference Seoul • In collaboration with WHO 21
fa9dc216988dbccc91a991d25c683a57.ppt