7b6f6bf16bc51af4c312d3bc478b8ccf.ppt
- Количество слайдов: 93
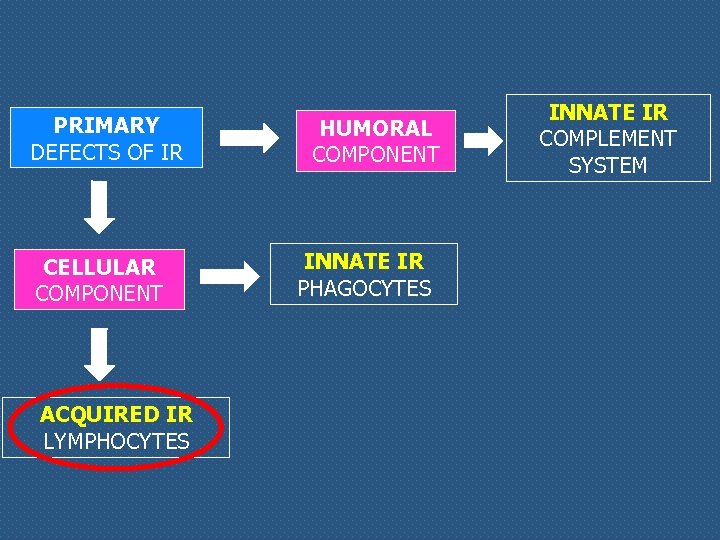 PRIMARY DEFECTS OF IR CELLULAR COMPONENT ACQUIRED IR LYMPHOCYTES HUMORAL COMPONENT INNATE IR PHAGOCYTES INNATE IR COMPLEMENT SYSTEM
PRIMARY DEFECTS OF IR CELLULAR COMPONENT ACQUIRED IR LYMPHOCYTES HUMORAL COMPONENT INNATE IR PHAGOCYTES INNATE IR COMPLEMENT SYSTEM
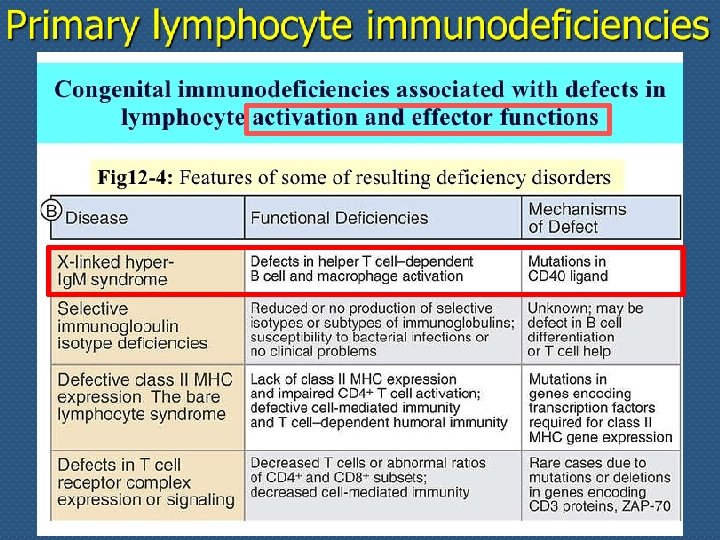
 Primary immune deficiencies: defects in acquired immunity
Primary immune deficiencies: defects in acquired immunity
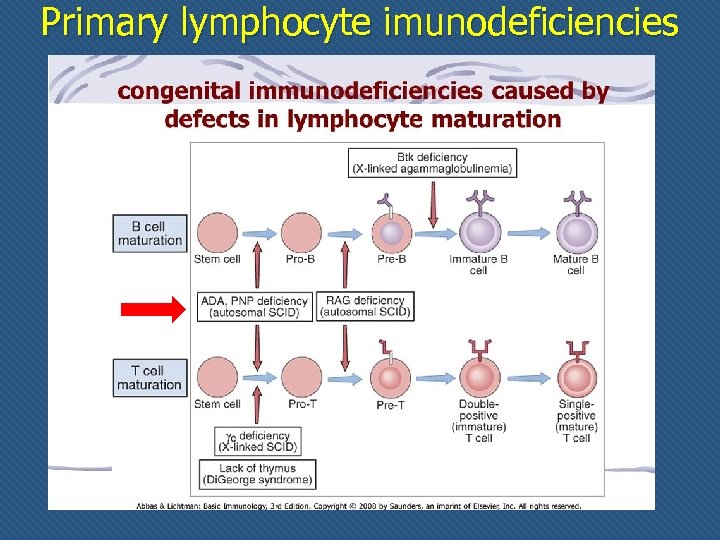
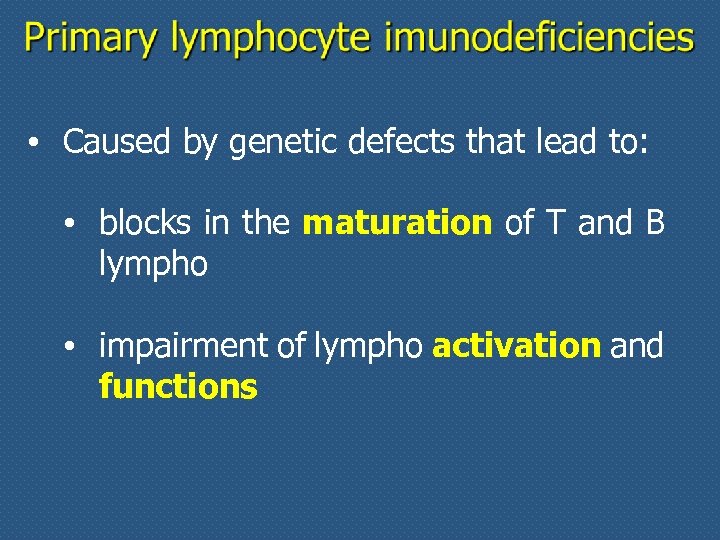 • Caused by genetic defects that lead to: • blocks in the maturation of T and B lympho • impairment of lympho activation and functions
• Caused by genetic defects that lead to: • blocks in the maturation of T and B lympho • impairment of lympho activation and functions
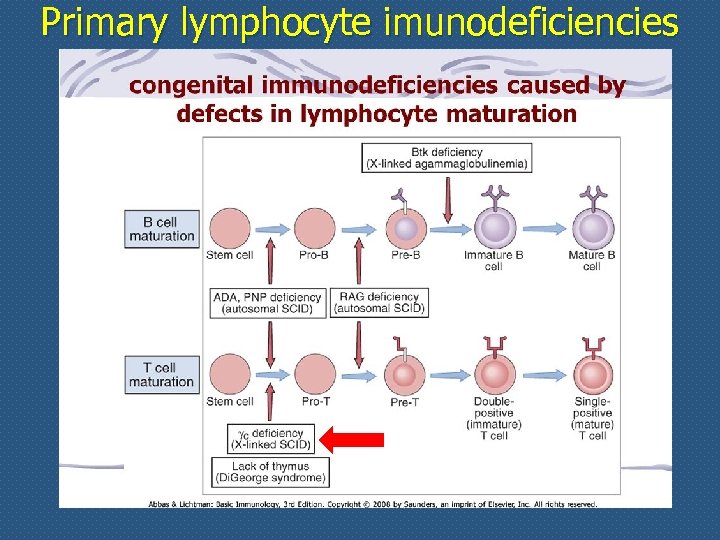
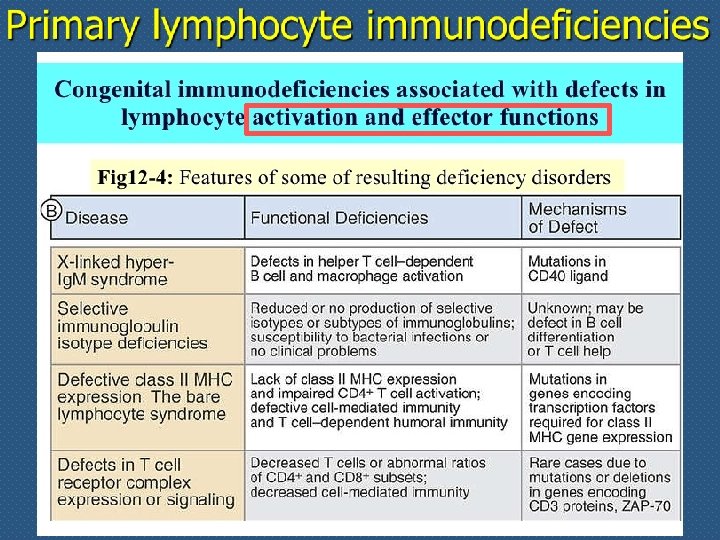
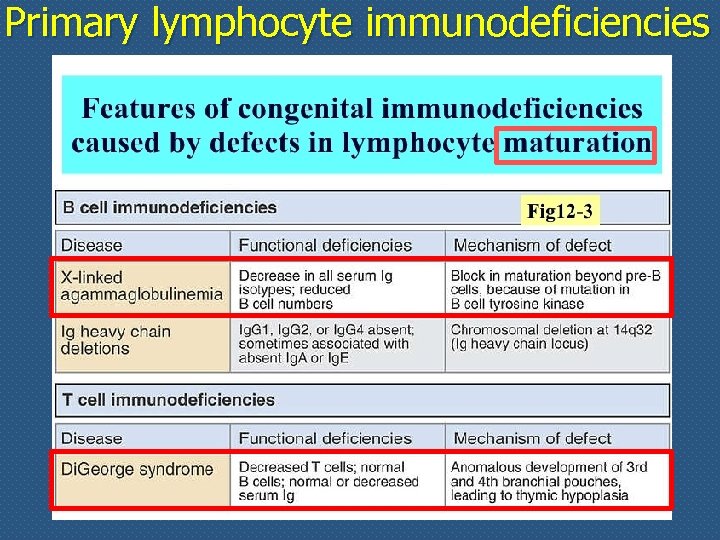 Primary lymphocyte immunodeficiencies
Primary lymphocyte immunodeficiencies
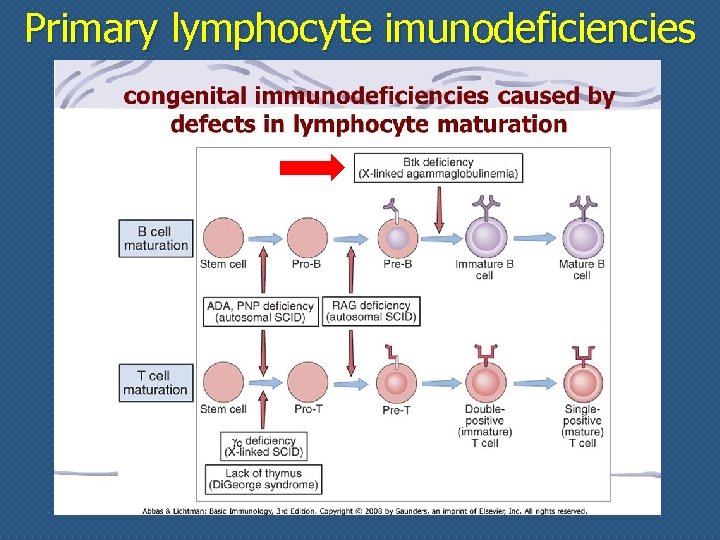 Primary lymphocyte imunodeficiencies
Primary lymphocyte imunodeficiencies
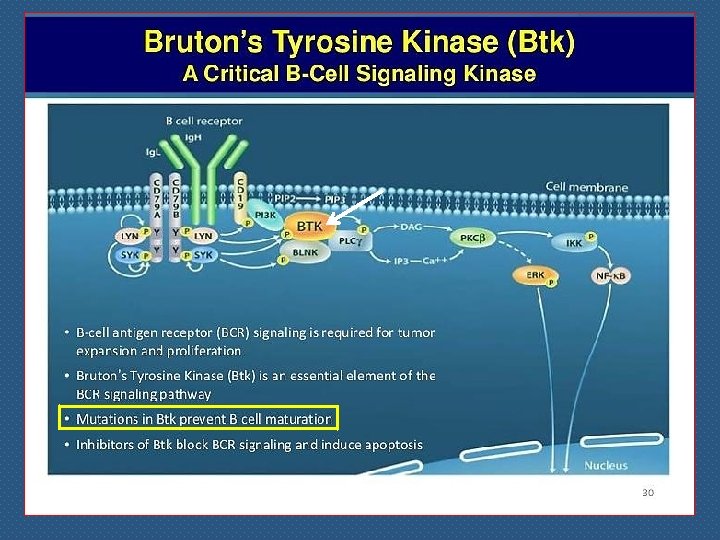
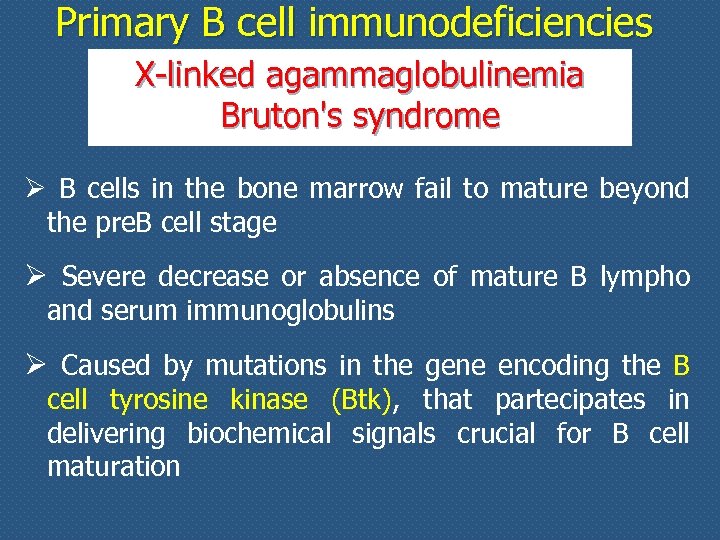 Primary B cell immunodeficiencies X-linked agammaglobulinemia Bruton's syndrome Ø B cells in the bone marrow fail to mature beyond the pre. B cell stage Ø Severe decrease or absence of mature B lympho and serum immunoglobulins Ø Caused by mutations in the gene encoding the B cell tyrosine kinase (Btk), that partecipates in delivering biochemical signals crucial for B cell maturation
Primary B cell immunodeficiencies X-linked agammaglobulinemia Bruton's syndrome Ø B cells in the bone marrow fail to mature beyond the pre. B cell stage Ø Severe decrease or absence of mature B lympho and serum immunoglobulins Ø Caused by mutations in the gene encoding the B cell tyrosine kinase (Btk), that partecipates in delivering biochemical signals crucial for B cell maturation
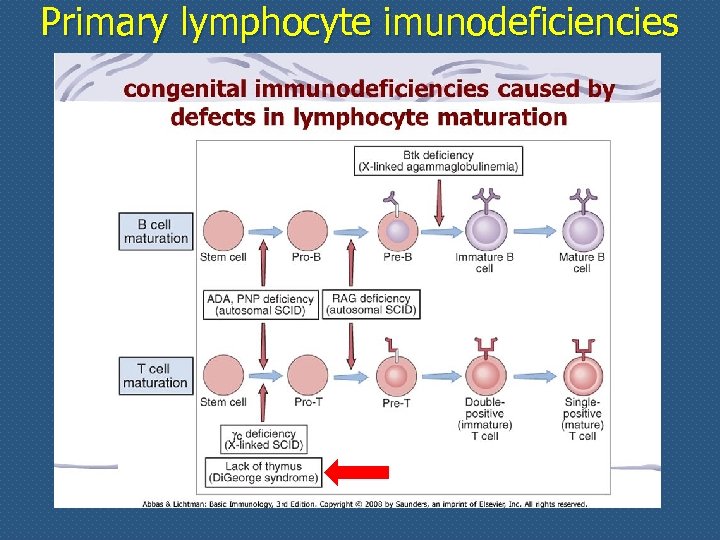 Primary lymphocyte imunodeficiencies
Primary lymphocyte imunodeficiencies
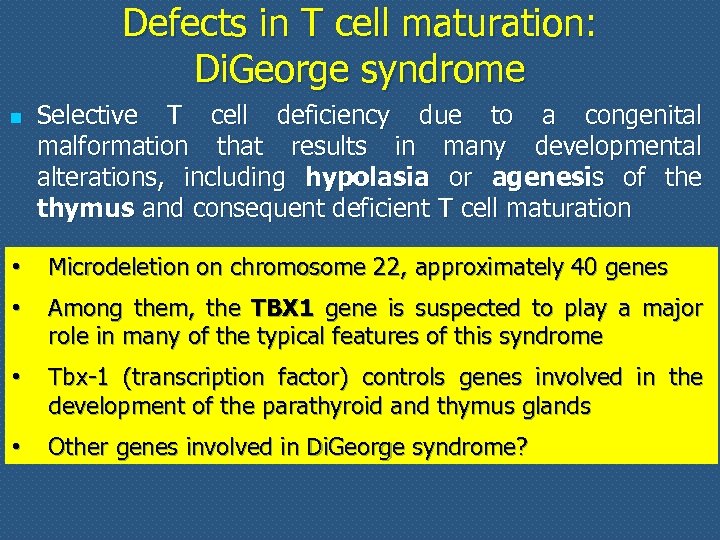 Defects in T cell maturation: Di. George syndrome n n • • Selective T cell deficiency due to a congenital malformation that results in many developmental alterations, including hypolasia or agenesis of the thymus and consequent deficient T cell maturation High susceptibility to mycobacterial, viral and fungal Microdeletion on chromosome 22, approximately 40 genes infection; severely affected patients have low Ig levels Among them, the TBX 1 gene is suspected to play a major role in many of the typical features of this syndrome • Tbx-1 (transcription factor) controls genes involved in the development of the parathyroid and thymus glands • Other genes involved in Di. George syndrome?
Defects in T cell maturation: Di. George syndrome n n • • Selective T cell deficiency due to a congenital malformation that results in many developmental alterations, including hypolasia or agenesis of the thymus and consequent deficient T cell maturation High susceptibility to mycobacterial, viral and fungal Microdeletion on chromosome 22, approximately 40 genes infection; severely affected patients have low Ig levels Among them, the TBX 1 gene is suspected to play a major role in many of the typical features of this syndrome • Tbx-1 (transcription factor) controls genes involved in the development of the parathyroid and thymus glands • Other genes involved in Di. George syndrome?
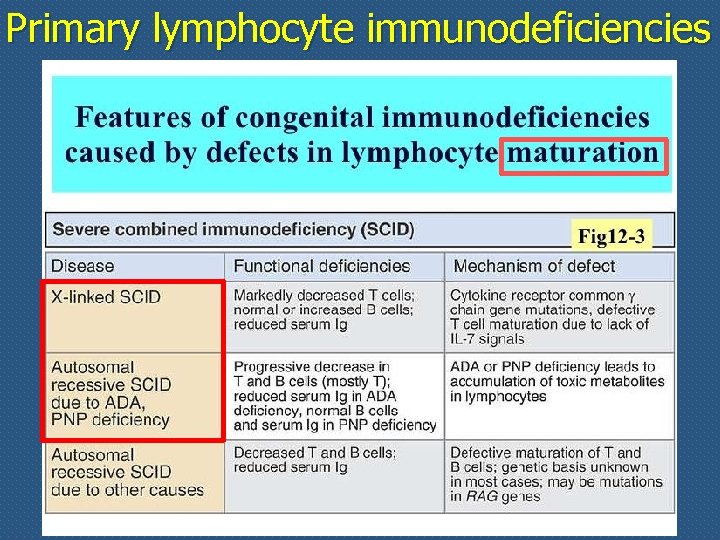 Primary lymphocyte immunodeficiencies
Primary lymphocyte immunodeficiencies
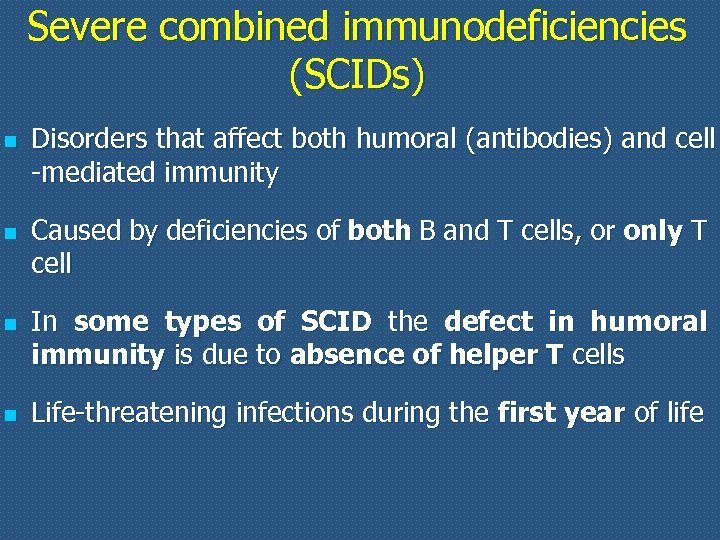 Severe combined immunodeficiencies (SCIDs) n n Disorders that affect both humoral (antibodies) and cell -mediated immunity Caused by deficiencies of both B and T cells, or only T cell In some types of SCID the defect in humoral immunity is due to absence of helper T cells Life-threatening infections during the first year of life
Severe combined immunodeficiencies (SCIDs) n n Disorders that affect both humoral (antibodies) and cell -mediated immunity Caused by deficiencies of both B and T cells, or only T cell In some types of SCID the defect in humoral immunity is due to absence of helper T cells Life-threatening infections during the first year of life
 Primary lymphocyte imunodeficiencies
Primary lymphocyte imunodeficiencies
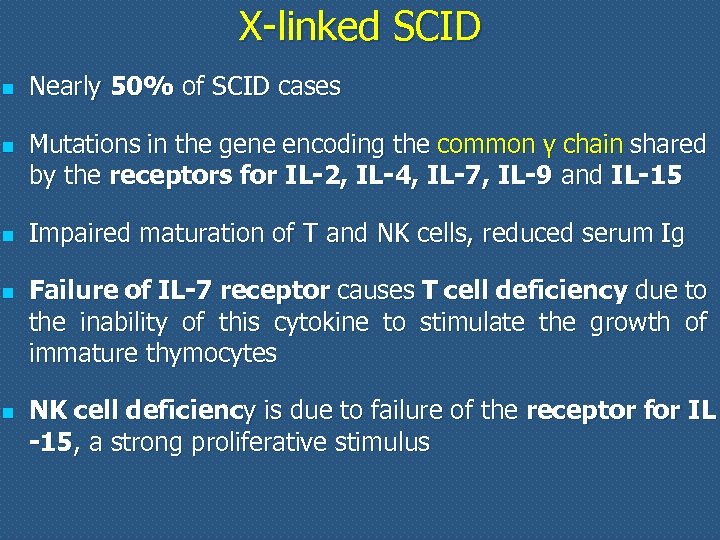 X-linked SCID n n n Nearly 50% of SCID cases Mutations in the gene encoding the common γ chain shared by the receptors for IL-2, IL-4, IL-7, IL-9 and IL-15 Impaired maturation of T and NK cells, reduced serum Ig Failure of IL-7 receptor causes T cell deficiency due to the inability of this cytokine to stimulate the growth of immature thymocytes NK cell deficiency is due to failure of the receptor for IL -15, a strong proliferative stimulus
X-linked SCID n n n Nearly 50% of SCID cases Mutations in the gene encoding the common γ chain shared by the receptors for IL-2, IL-4, IL-7, IL-9 and IL-15 Impaired maturation of T and NK cells, reduced serum Ig Failure of IL-7 receptor causes T cell deficiency due to the inability of this cytokine to stimulate the growth of immature thymocytes NK cell deficiency is due to failure of the receptor for IL -15, a strong proliferative stimulus
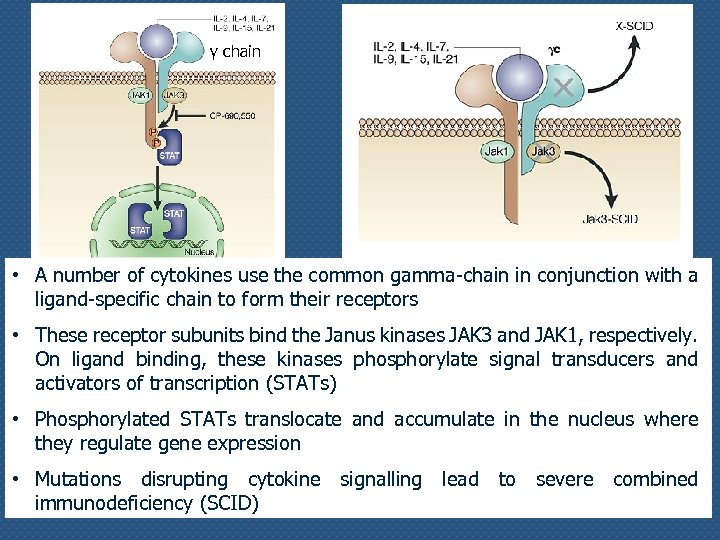 γ chain • A number of cytokines use the common gamma-chain in conjunction with a ligand-specific chain to form their receptors • These receptor subunits bind the Janus kinases JAK 3 and JAK 1, respectively. On ligand binding, these kinases phosphorylate signal transducers and activators of transcription (STATs) • Phosphorylated STATs translocate and accumulate in the nucleus where they regulate gene expression • Mutations disrupting cytokine signalling lead to severe combined immunodeficiency (SCID)
γ chain • A number of cytokines use the common gamma-chain in conjunction with a ligand-specific chain to form their receptors • These receptor subunits bind the Janus kinases JAK 3 and JAK 1, respectively. On ligand binding, these kinases phosphorylate signal transducers and activators of transcription (STATs) • Phosphorylated STATs translocate and accumulate in the nucleus where they regulate gene expression • Mutations disrupting cytokine signalling lead to severe combined immunodeficiency (SCID)
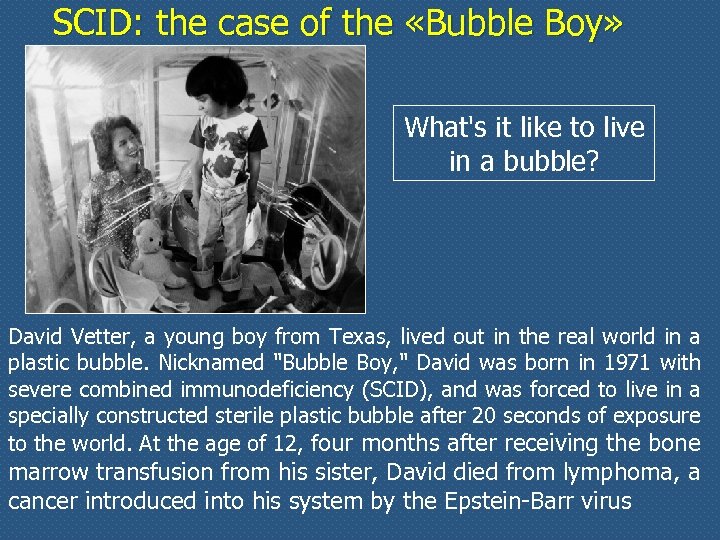 SCID: the case of the «Bubble Boy» What's it like to live in a bubble? David Vetter, a young boy from Texas, lived out in the real world in a plastic bubble. Nicknamed "Bubble Boy, " David was born in 1971 with severe combined immunodeficiency (SCID), and was forced to live in a specially constructed sterile plastic bubble after 20 seconds of exposure to the world. At the age of 12, four months after receiving the bone marrow transfusion from his sister, David died from lymphoma, a cancer introduced into his system by the Epstein-Barr virus
SCID: the case of the «Bubble Boy» What's it like to live in a bubble? David Vetter, a young boy from Texas, lived out in the real world in a plastic bubble. Nicknamed "Bubble Boy, " David was born in 1971 with severe combined immunodeficiency (SCID), and was forced to live in a specially constructed sterile plastic bubble after 20 seconds of exposure to the world. At the age of 12, four months after receiving the bone marrow transfusion from his sister, David died from lymphoma, a cancer introduced into his system by the Epstein-Barr virus
 Primary lymphocyte imunodeficiencies
Primary lymphocyte imunodeficiencies
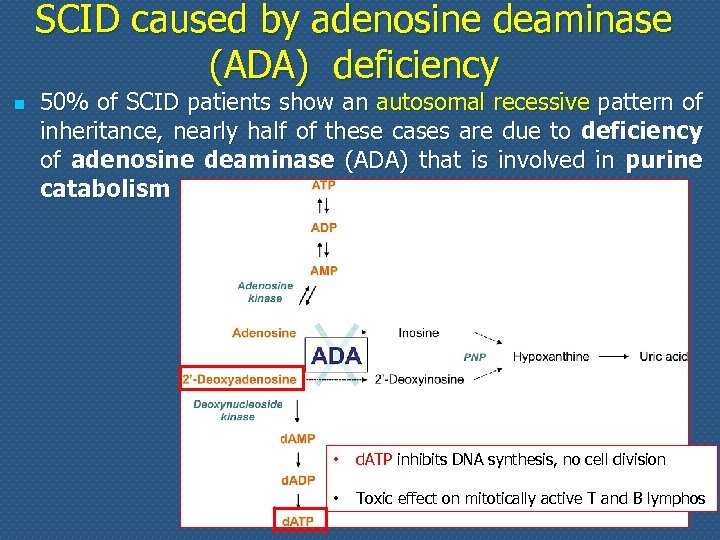 SCID caused by adenosine deaminase (ADA) deficiency n 50% of SCID patients show an autosomal recessive pattern of inheritance, nearly half of these cases are due to deficiency of adenosine deaminase (ADA) that is involved in purine catabolism • d. ATP inhibits DNA synthesis, no cell division • Toxic effect on mitotically active T and B lymphos
SCID caused by adenosine deaminase (ADA) deficiency n 50% of SCID patients show an autosomal recessive pattern of inheritance, nearly half of these cases are due to deficiency of adenosine deaminase (ADA) that is involved in purine catabolism • d. ATP inhibits DNA synthesis, no cell division • Toxic effect on mitotically active T and B lymphos
 ADA-SCID n Occurs in fewer than one in 100, 000 live births n ADA deficiency leads to reduced numbers of T and B cells n n profound lymphopenia and very low immunoglobulin levels of all isotypes resulting in severe and recurrent opportunistic infections Treatments: n n n allogenic hematopoietic stem cell transplantation (HSCT) enzyme replacement therapy with adenosine deaminase enzyme gene therapy by infusion of marrow cells that have been transduced with an ADA-containing vector (18 kids treated, 100% success)
ADA-SCID n Occurs in fewer than one in 100, 000 live births n ADA deficiency leads to reduced numbers of T and B cells n n profound lymphopenia and very low immunoglobulin levels of all isotypes resulting in severe and recurrent opportunistic infections Treatments: n n n allogenic hematopoietic stem cell transplantation (HSCT) enzyme replacement therapy with adenosine deaminase enzyme gene therapy by infusion of marrow cells that have been transduced with an ADA-containing vector (18 kids treated, 100% success)
 Autologous CD 34+ bone marrow stem cells transduced with a retroviral vector containing the ADA gene into 10 children with SCID due to ADA deficiency who lacked an HLA-identical sibling donor
Autologous CD 34+ bone marrow stem cells transduced with a retroviral vector containing the ADA gene into 10 children with SCID due to ADA deficiency who lacked an HLA-identical sibling donor
 Appelli straordinari Patologia molecolare dicembre 2017 Aula D, edificio centrale n n Mercoledì 13 Venerdì 15 Lunedì 18 Mercoledì 20 ore 15: 00 Romano ore 11: 00 Menegazzi ore 15: 00 Romano ore 15: 00 Menegazzi
Appelli straordinari Patologia molecolare dicembre 2017 Aula D, edificio centrale n n Mercoledì 13 Venerdì 15 Lunedì 18 Mercoledì 20 ore 15: 00 Romano ore 11: 00 Menegazzi ore 15: 00 Romano ore 15: 00 Menegazzi
 • Caused by genetic defects that lead to: • blocks in the maturation of T and B lympho • impairment of lympho activation and functions
• Caused by genetic defects that lead to: • blocks in the maturation of T and B lympho • impairment of lympho activation and functions
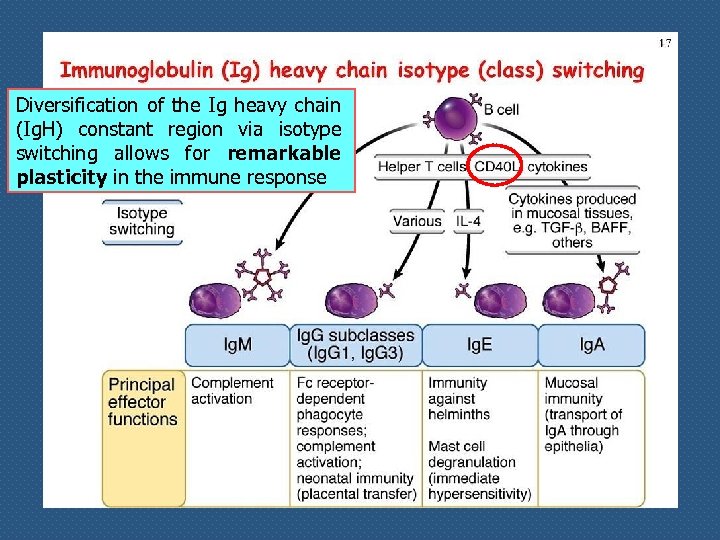 Diversification of the Ig heavy chain (Ig. H) constant region via isotype switching allows for remarkable plasticity in the immune response
Diversification of the Ig heavy chain (Ig. H) constant region via isotype switching allows for remarkable plasticity in the immune response
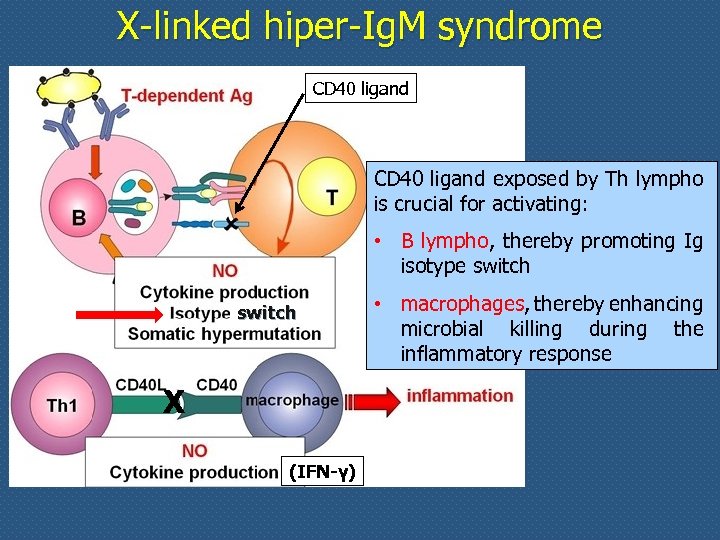 X-linked hiper-Ig. M syndrome CD 40 ligand exposed by Th lympho is crucial for activating: • B lympho, thereby promoting Ig isotype switch X (IFN-γ) • macrophages, thereby enhancing microbial killing during the inflammatory response
X-linked hiper-Ig. M syndrome CD 40 ligand exposed by Th lympho is crucial for activating: • B lympho, thereby promoting Ig isotype switch X (IFN-γ) • macrophages, thereby enhancing microbial killing during the inflammatory response
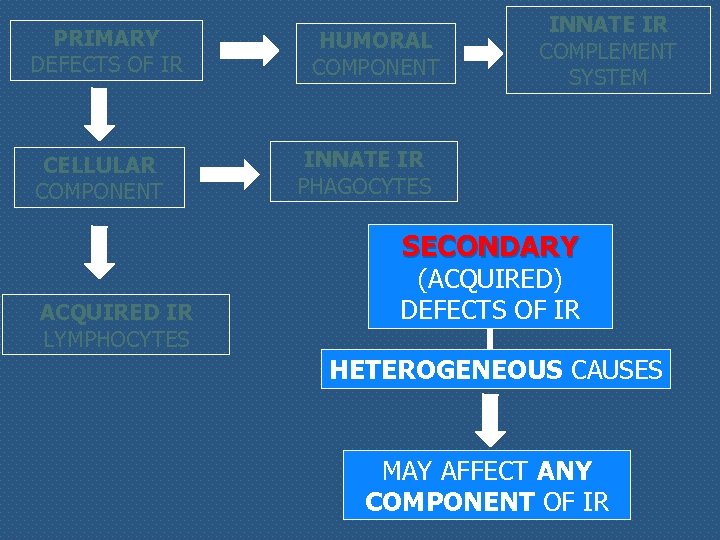 PRIMARY DEFECTS OF IR CELLULAR COMPONENT HUMORAL COMPONENT INNATE IR COMPLEMENT SYSTEM INNATE IR PHAGOCYTES SECONDARY ACQUIRED IR LYMPHOCYTES (ACQUIRED) DEFECTS OF IR HETEROGENEOUS CAUSES MAY AFFECT ANY COMPONENT OF IR
PRIMARY DEFECTS OF IR CELLULAR COMPONENT HUMORAL COMPONENT INNATE IR COMPLEMENT SYSTEM INNATE IR PHAGOCYTES SECONDARY ACQUIRED IR LYMPHOCYTES (ACQUIRED) DEFECTS OF IR HETEROGENEOUS CAUSES MAY AFFECT ANY COMPONENT OF IR
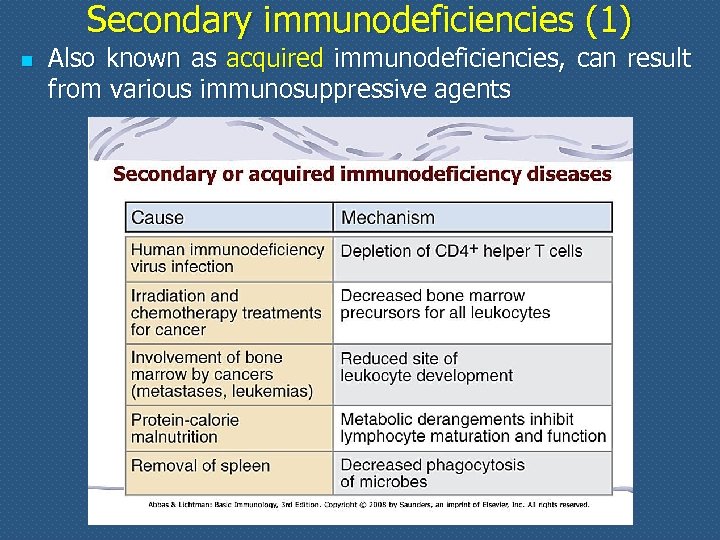 Secondary immunodeficiencies (1) n Also known as acquired immunodeficiencies, can result from various immunosuppressive agents
Secondary immunodeficiencies (1) n Also known as acquired immunodeficiencies, can result from various immunosuppressive agents
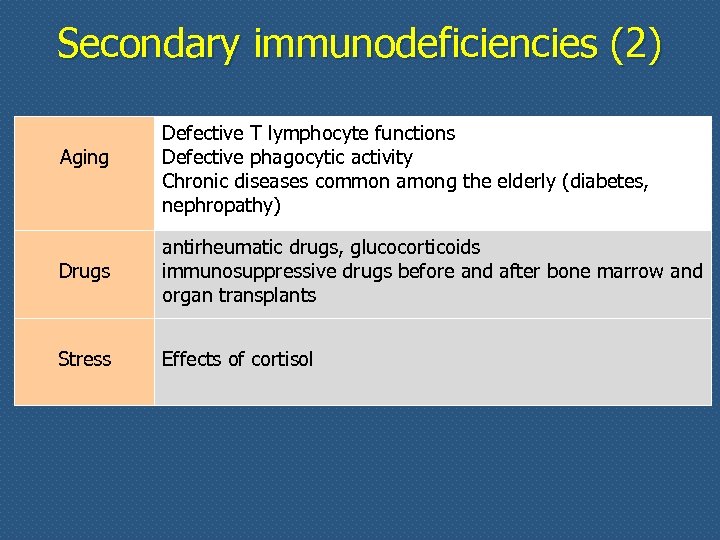 Secondary immunodeficiencies (2) Aging Defective T lymphocyte functions Defective phagocytic activity Chronic diseases common among the elderly (diabetes, nephropathy) Drugs antirheumatic drugs, glucocorticoids immunosuppressive drugs before and after bone marrow and organ transplants Stress Effects of cortisol
Secondary immunodeficiencies (2) Aging Defective T lymphocyte functions Defective phagocytic activity Chronic diseases common among the elderly (diabetes, nephropathy) Drugs antirheumatic drugs, glucocorticoids immunosuppressive drugs before and after bone marrow and organ transplants Stress Effects of cortisol
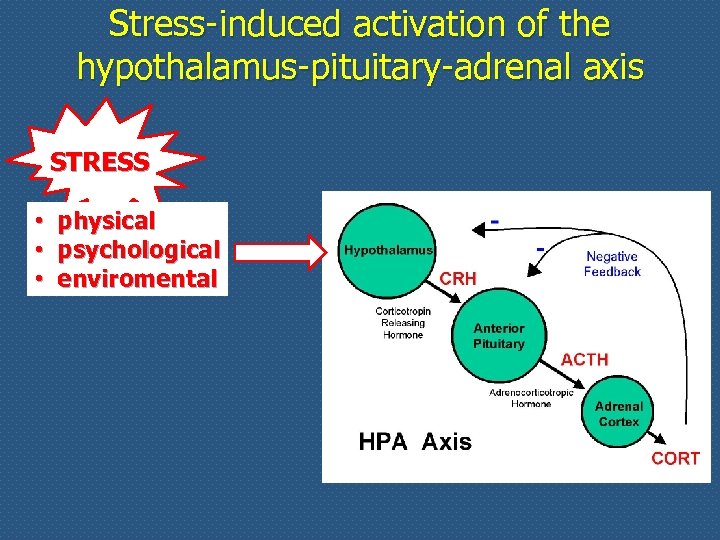 Stress-induced activation of the hypothalamus-pituitary-adrenal axis STRESS • • • physical psychological enviromental
Stress-induced activation of the hypothalamus-pituitary-adrenal axis STRESS • • • physical psychological enviromental
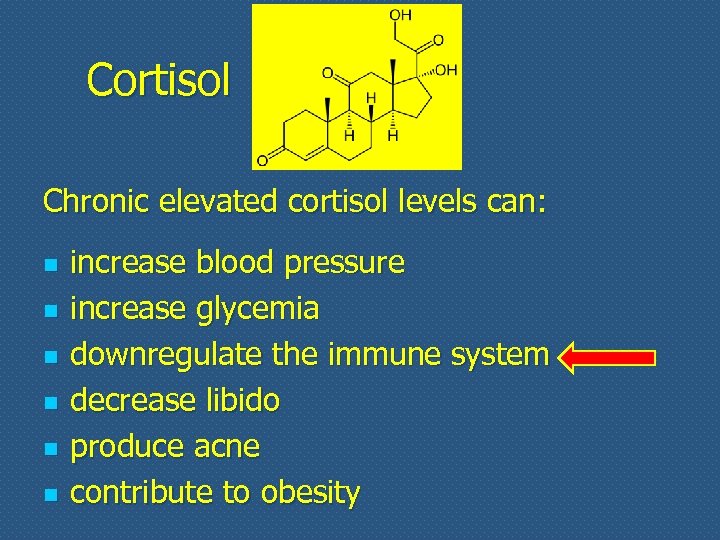 Cortisol Chronic elevated cortisol levels can: n n n increase blood pressure increase glycemia downregulate the immune system decrease libido produce acne contribute to obesity
Cortisol Chronic elevated cortisol levels can: n n n increase blood pressure increase glycemia downregulate the immune system decrease libido produce acne contribute to obesity
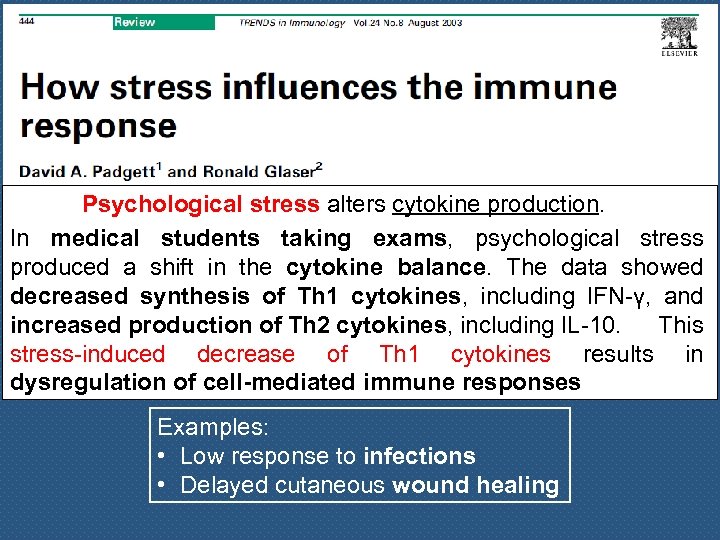 Psychological stress alters cytokine production. In medical students taking exams, psychological stress produced a shift in the cytokine balance. The data showed decreased synthesis of Th 1 cytokines, including IFN-γ, and increased production of Th 2 cytokines, including IL-10. This stress-induced decrease of Th 1 cytokines results in dysregulation of cell-mediated immune responses Examples: • Low response to infections • Delayed cutaneous wound healing
Psychological stress alters cytokine production. In medical students taking exams, psychological stress produced a shift in the cytokine balance. The data showed decreased synthesis of Th 1 cytokines, including IFN-γ, and increased production of Th 2 cytokines, including IL-10. This stress-induced decrease of Th 1 cytokines results in dysregulation of cell-mediated immune responses Examples: • Low response to infections • Delayed cutaneous wound healing
 Immunopathology n n As a branch of Immunology, immunopathology concerns disorders caused by alterations of the immune response 3 main categories of alterations: excessive response reactions v v inappropriate response v defective response hypersensitivity autoimmune diseases immunodeficiencies
Immunopathology n n As a branch of Immunology, immunopathology concerns disorders caused by alterations of the immune response 3 main categories of alterations: excessive response reactions v v inappropriate response v defective response hypersensitivity autoimmune diseases immunodeficiencies
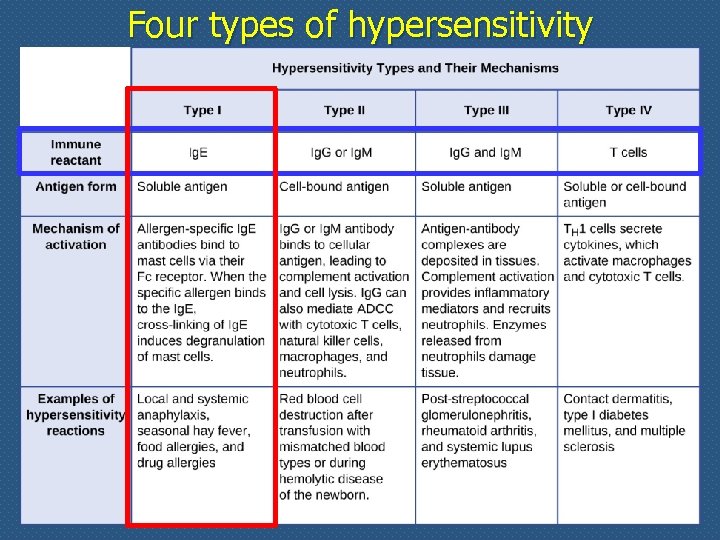 Four types of hypersensitivity
Four types of hypersensitivity
 Hallmarks of type I hypersensitivity reaction n Allergy is the most common disorder of immunity n Exposure to an antigen (allergen) n n Production of Ig. E which bind to Fc receptors on mast cells Basophils and eosinophils also partake in allergic reactions
Hallmarks of type I hypersensitivity reaction n Allergy is the most common disorder of immunity n Exposure to an antigen (allergen) n n Production of Ig. E which bind to Fc receptors on mast cells Basophils and eosinophils also partake in allergic reactions
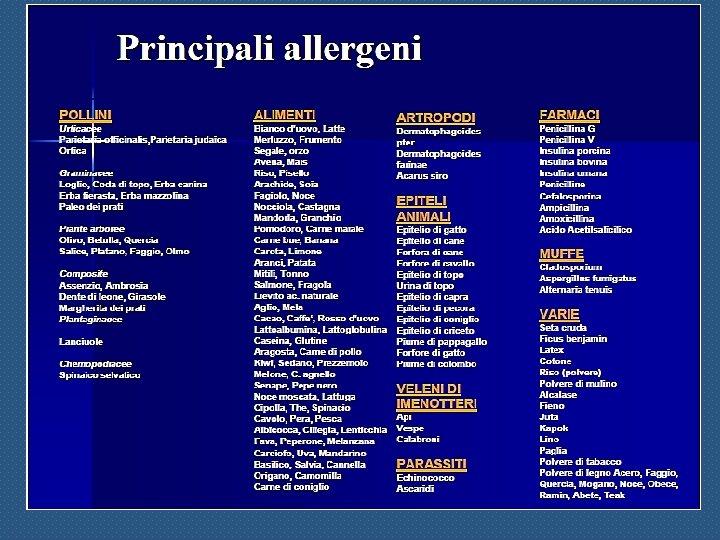
 Allergens n n Antigens that elicit immediate sensitivity reaction Most individuals who encounter these allergens do not produce specific Ig. E There is a strong genetic predisposition for the development of type I hypersensitivity, known as atopy Typical allergens are common environmental proteins, such as those contained in pollen, house dust mites, animal dander, some foods and chemicals
Allergens n n Antigens that elicit immediate sensitivity reaction Most individuals who encounter these allergens do not produce specific Ig. E There is a strong genetic predisposition for the development of type I hypersensitivity, known as atopy Typical allergens are common environmental proteins, such as those contained in pollen, house dust mites, animal dander, some foods and chemicals
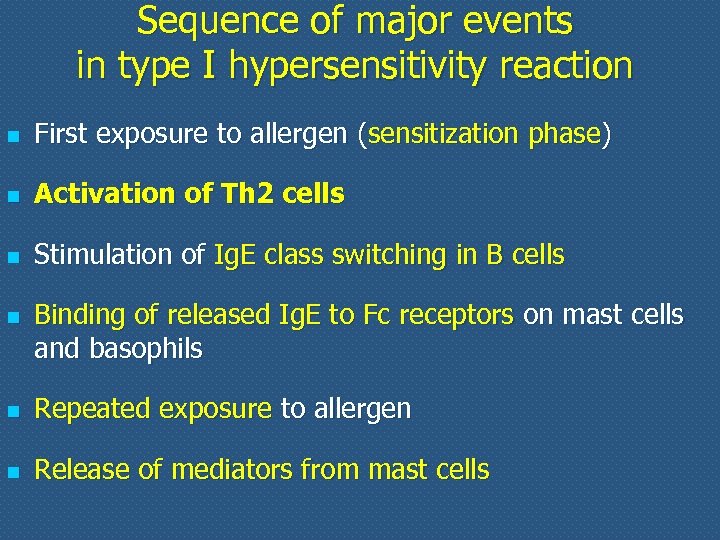 Sequence of major events in type I hypersensitivity reaction n First exposure to allergen (sensitization phase) n Activation of Th 2 cells n Stimulation of Ig. E class switching in B cells n Binding of released Ig. E to Fc receptors on mast cells and basophils n Repeated exposure to allergen n Release of mediators from mast cells
Sequence of major events in type I hypersensitivity reaction n First exposure to allergen (sensitization phase) n Activation of Th 2 cells n Stimulation of Ig. E class switching in B cells n Binding of released Ig. E to Fc receptors on mast cells and basophils n Repeated exposure to allergen n Release of mediators from mast cells
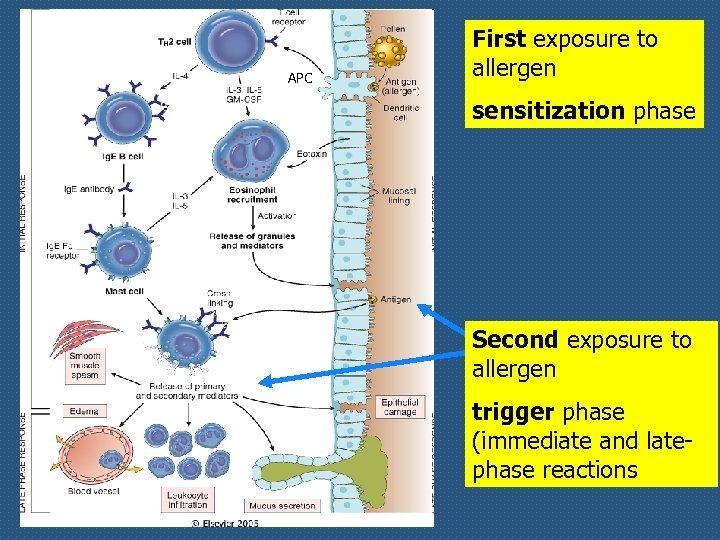 APC First exposure to allergen sensitization phase Second exposure to allergen trigger phase (immediate and latephase reactions
APC First exposure to allergen sensitization phase Second exposure to allergen trigger phase (immediate and latephase reactions
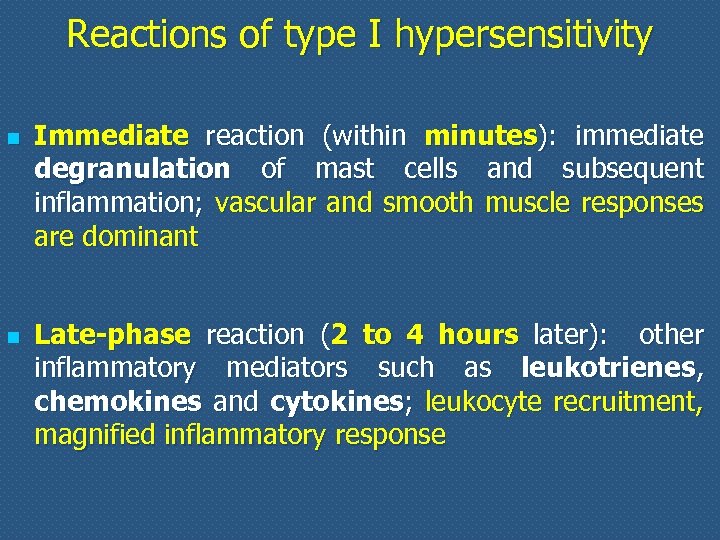 Reactions of type I hypersensitivity n n Immediate reaction (within minutes): immediate degranulation of mast cells and subsequent inflammation; vascular and smooth muscle responses are dominant Late-phase reaction (2 to 4 hours later): other inflammatory mediators such as leukotrienes, chemokines and cytokines; leukocyte recruitment, magnified inflammatory response
Reactions of type I hypersensitivity n n Immediate reaction (within minutes): immediate degranulation of mast cells and subsequent inflammation; vascular and smooth muscle responses are dominant Late-phase reaction (2 to 4 hours later): other inflammatory mediators such as leukotrienes, chemokines and cytokines; leukocyte recruitment, magnified inflammatory response
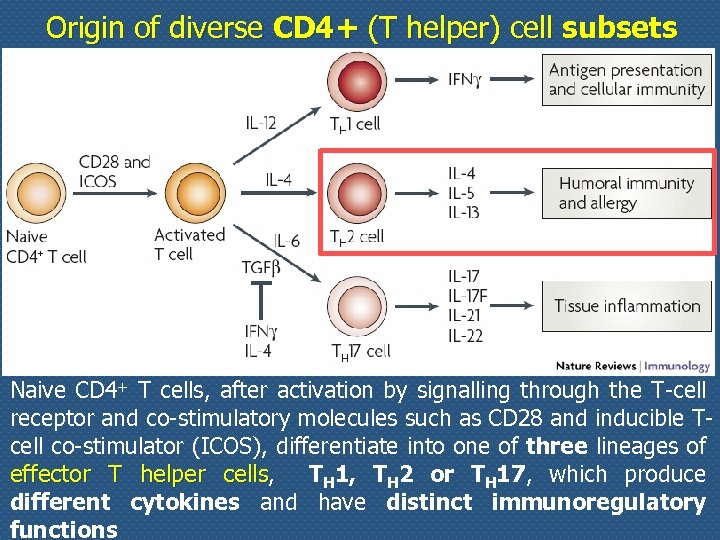 Origin of diverse CD 4+ (T helper) cell subsets Naive CD 4+ T cells, after activation by signalling through the T-cell receptor and co-stimulatory molecules such as CD 28 and inducible Tcell co-stimulator (ICOS), differentiate into one of three lineages of effector T helper cells, TH 1, TH 2 or TH 17, which produce different cytokines and have distinct immunoregulatory functions
Origin of diverse CD 4+ (T helper) cell subsets Naive CD 4+ T cells, after activation by signalling through the T-cell receptor and co-stimulatory molecules such as CD 28 and inducible Tcell co-stimulator (ICOS), differentiate into one of three lineages of effector T helper cells, TH 1, TH 2 or TH 17, which produce different cytokines and have distinct immunoregulatory functions
 Central role of Th 2 cells in allergic reactions n n Ig. E synthesis is dependent on activation of Th 2 cells and their secretion of IL-4 and IL-13 IL-4/IL-13 -stimulated B cells undergo heavy chain isotype switching and secrete Ig. E Th 2 also release IL-5 that recruits and activate eosinophils IL-13 released by Th 2 also stimulates epithelial cells (e. g. in the airways) to secrete increased amount of mucus
Central role of Th 2 cells in allergic reactions n n Ig. E synthesis is dependent on activation of Th 2 cells and their secretion of IL-4 and IL-13 IL-4/IL-13 -stimulated B cells undergo heavy chain isotype switching and secrete Ig. E Th 2 also release IL-5 that recruits and activate eosinophils IL-13 released by Th 2 also stimulates epithelial cells (e. g. in the airways) to secrete increased amount of mucus
 Genetic susceptibility to type I hypersensitivity n n The propensity to produce high levels of Ig. E (atopy) is influenced by a multigenic pattern of inheritance The genes involved code for several proteins which have a role in the regulation of hypersensitivity, such as: modulators of T cell activation n IL-4 and IL-13 (Ig. E class switching) n IL-5 (eosinophil recruitment and activation) n stem cell factor (mast cell maturation) n
Genetic susceptibility to type I hypersensitivity n n The propensity to produce high levels of Ig. E (atopy) is influenced by a multigenic pattern of inheritance The genes involved code for several proteins which have a role in the regulation of hypersensitivity, such as: modulators of T cell activation n IL-4 and IL-13 (Ig. E class switching) n IL-5 (eosinophil recruitment and activation) n stem cell factor (mast cell maturation) n
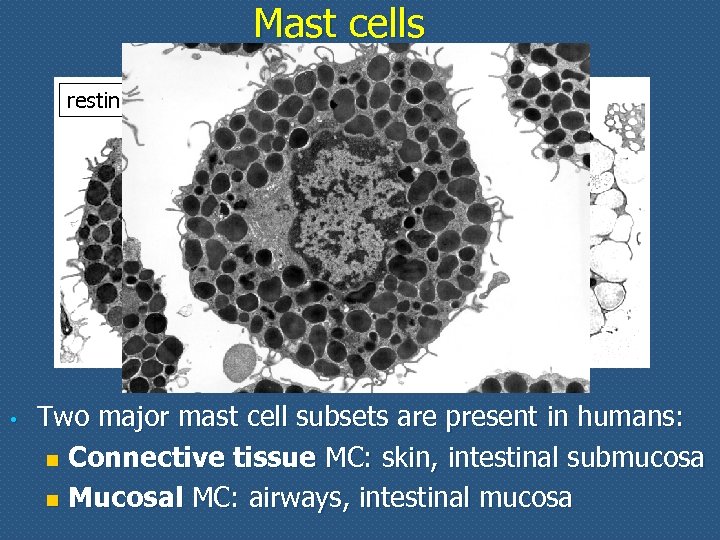 Mast cells resting • activated Two major mast cell subsets are present in humans: n Connective tissue MC: skin, intestinal submucosa n Mucosal MC: airways, intestinal mucosa
Mast cells resting • activated Two major mast cell subsets are present in humans: n Connective tissue MC: skin, intestinal submucosa n Mucosal MC: airways, intestinal mucosa
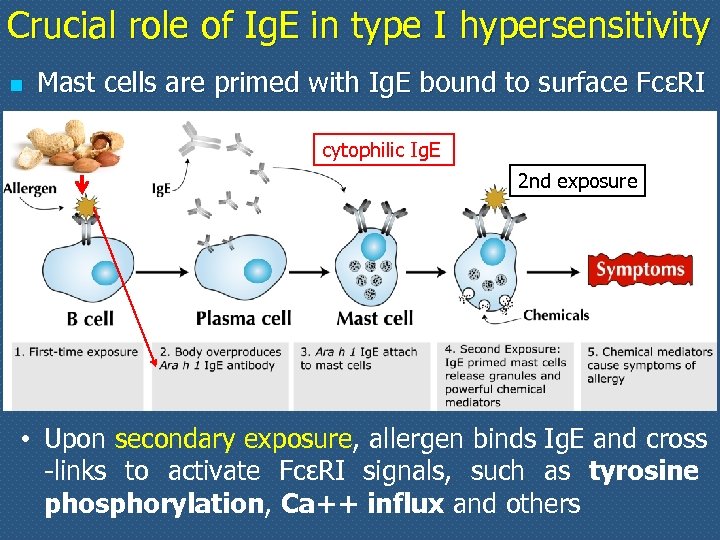 Crucial role of Ig. E in type I hypersensitivity n Mast cells are primed with Ig. E bound to surface FcεRI cytophilic Ig. E 2 nd exposure • Upon secondary exposure, allergen binds Ig. E and cross -links to activate FcεRI signals, such as tyrosine phosphorylation, Ca++ influx and others
Crucial role of Ig. E in type I hypersensitivity n Mast cells are primed with Ig. E bound to surface FcεRI cytophilic Ig. E 2 nd exposure • Upon secondary exposure, allergen binds Ig. E and cross -links to activate FcεRI signals, such as tyrosine phosphorylation, Ca++ influx and others
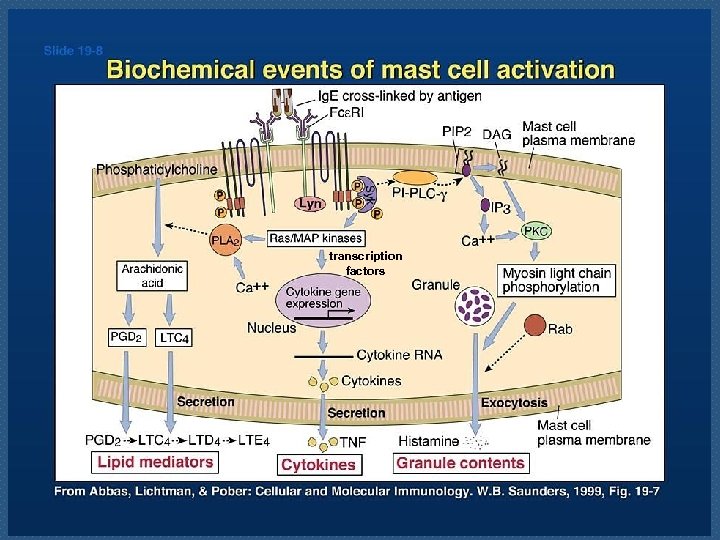 transcription factors
transcription factors
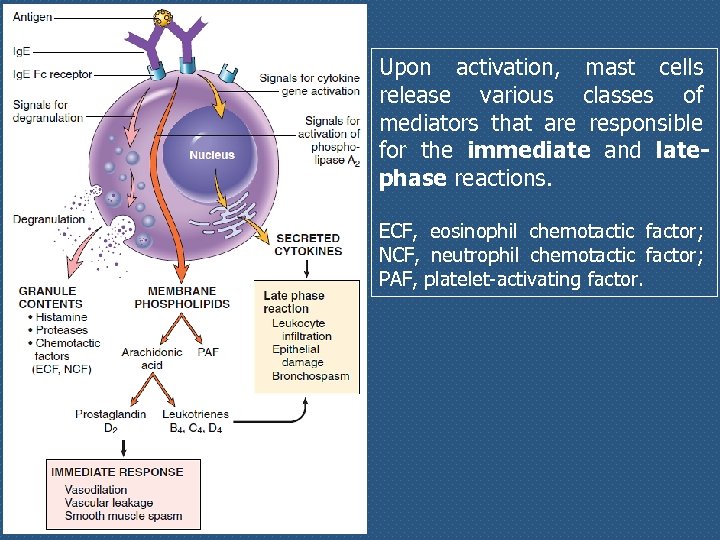 Upon activation, mast cells release various classes of mediators that are responsible for the immediate and latephase reactions. ECF, eosinophil chemotactic factor; NCF, neutrophil chemotactic factor; PAF, platelet-activating factor.
Upon activation, mast cells release various classes of mediators that are responsible for the immediate and latephase reactions. ECF, eosinophil chemotactic factor; NCF, neutrophil chemotactic factor; PAF, platelet-activating factor.
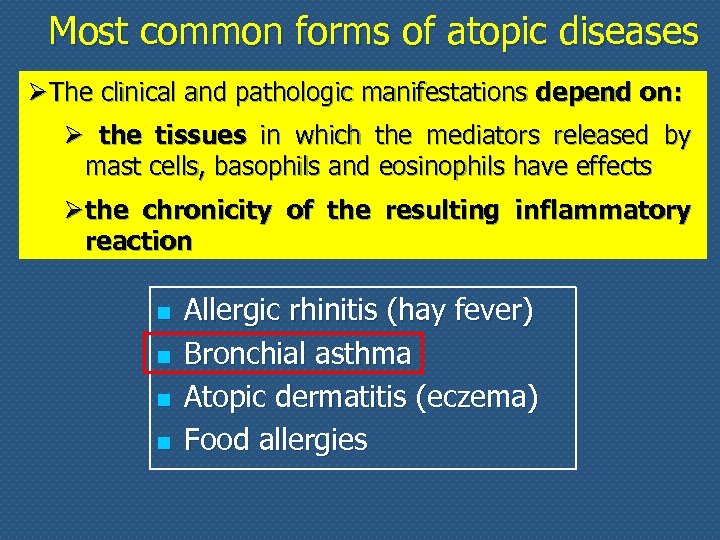 Most common forms of atopic diseases Ø The clinical and pathologic manifestations depend on: Ø the tissues in which the mediators released by mast cells, basophils and eosinophils have effects Ø the chronicity of the resulting inflammatory reaction n n Allergic rhinitis (hay fever) Bronchial asthma Atopic dermatitis (eczema) Food allergies
Most common forms of atopic diseases Ø The clinical and pathologic manifestations depend on: Ø the tissues in which the mediators released by mast cells, basophils and eosinophils have effects Ø the chronicity of the resulting inflammatory reaction n n Allergic rhinitis (hay fever) Bronchial asthma Atopic dermatitis (eczema) Food allergies
 Bronchial asthma n n n Inflammatory disease caused by repeated immediate and late-phase hypersensitivity reactions in the lung Affects 10 to 20% of childs and adults living in industrialized countries Major clinico-pathologic manifestations: n intermittent airway obstruction n chronic bronchial inflammation n n bronchial smooth hyperplasia muscle hypertrophy and hyperreactivity to bronchoconstrictors (products derived from arachidonic a. , LTC 4, LTD 4)
Bronchial asthma n n n Inflammatory disease caused by repeated immediate and late-phase hypersensitivity reactions in the lung Affects 10 to 20% of childs and adults living in industrialized countries Major clinico-pathologic manifestations: n intermittent airway obstruction n chronic bronchial inflammation n n bronchial smooth hyperplasia muscle hypertrophy and hyperreactivity to bronchoconstrictors (products derived from arachidonic a. , LTC 4, LTD 4)
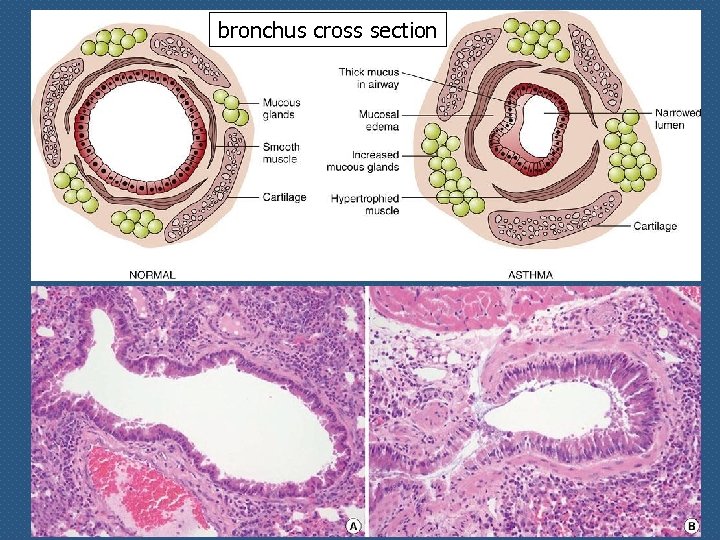 bronchus cross section
bronchus cross section
 Anaphylaxis: acute multiorgan systemic reaction q A variety of sympthoms that may unevenly associate • muco-cutaneous s. (generalized hive, hot flush, oedema of tongue, lips and throath) are almost always present • The diagnosis of anaphylactic reaction is established when at least two of the following sympthoms occur • respiratory s. (dyspnea, bronchospasm) • cardiovascular s. (hypotension) • gastroenteric s. (abdominal pain, vomiting)
Anaphylaxis: acute multiorgan systemic reaction q A variety of sympthoms that may unevenly associate • muco-cutaneous s. (generalized hive, hot flush, oedema of tongue, lips and throath) are almost always present • The diagnosis of anaphylactic reaction is established when at least two of the following sympthoms occur • respiratory s. (dyspnea, bronchospasm) • cardiovascular s. (hypotension) • gastroenteric s. (abdominal pain, vomiting)
 Systemic anaphylaxis: a life-threatening condition • Systemic exposure to protein antigens (e. g. , bee venom) or drugs (e. g. , penicillin) may result in systemic anaphylaxis • Within minutes of the exposure in a sensitized host, itching, urticaria (hives), and skin erythema appear, followed by profound respiratory difficulty caused by pulmonary bronchoconstriction • In addition, laryngeal edema may occur causing upper airway obstruction; the musculature of the entire gastrointestinal tract may be affected, with resultant vomiting, abdominal cramps, and diarrhea • There may be systemic vasodilation with a fall in blood pressure (anaphylactic shock), and the patient may progress to circulatory collapse and death within few minutes
Systemic anaphylaxis: a life-threatening condition • Systemic exposure to protein antigens (e. g. , bee venom) or drugs (e. g. , penicillin) may result in systemic anaphylaxis • Within minutes of the exposure in a sensitized host, itching, urticaria (hives), and skin erythema appear, followed by profound respiratory difficulty caused by pulmonary bronchoconstriction • In addition, laryngeal edema may occur causing upper airway obstruction; the musculature of the entire gastrointestinal tract may be affected, with resultant vomiting, abdominal cramps, and diarrhea • There may be systemic vasodilation with a fall in blood pressure (anaphylactic shock), and the patient may progress to circulatory collapse and death within few minutes
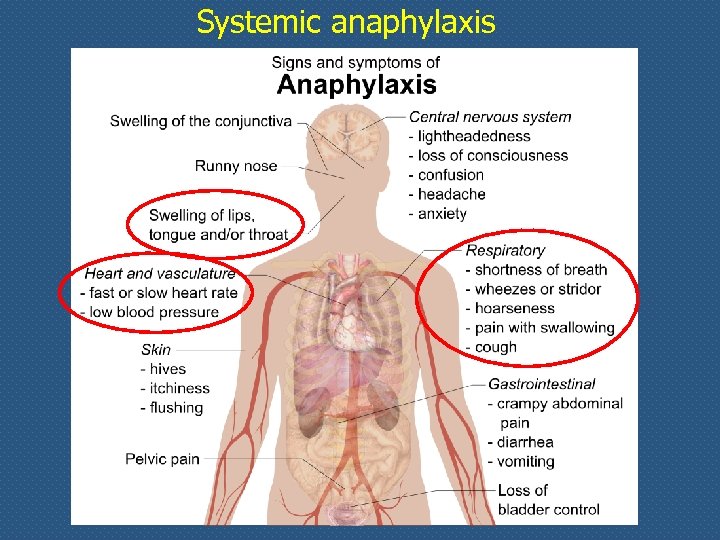 Systemic anaphylaxis
Systemic anaphylaxis
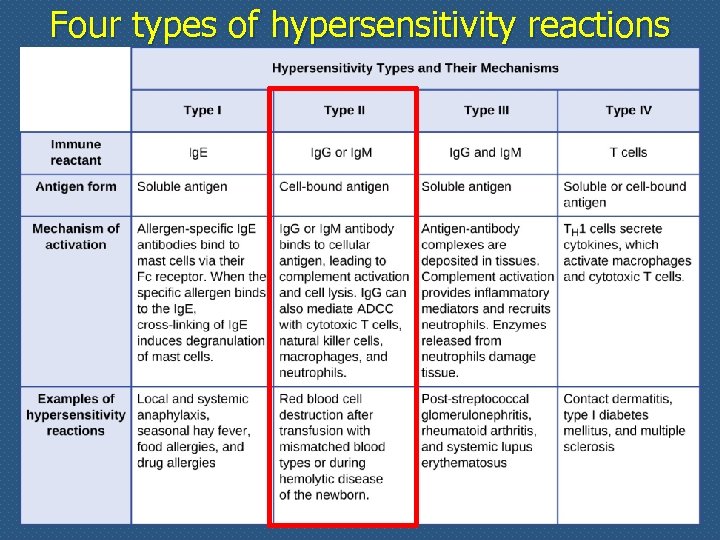 Four types of hypersensitivity reactions
Four types of hypersensitivity reactions
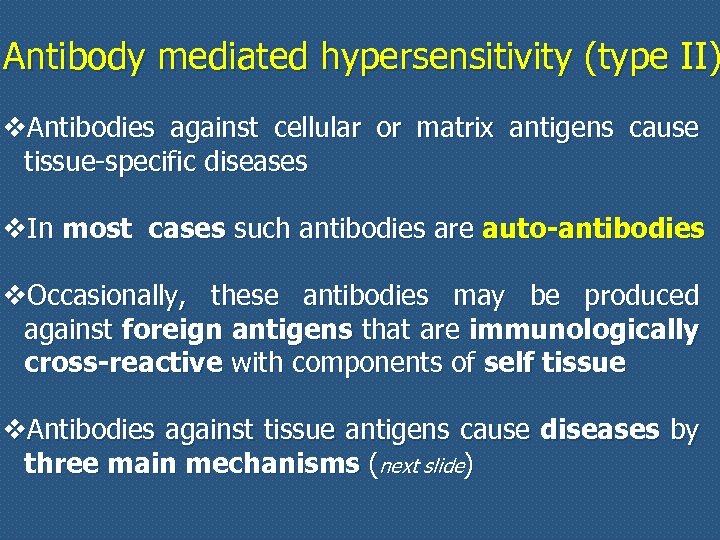 Antibody mediated hypersensitivity (type II) v. Antibodies against cellular or matrix antigens cause tissue-specific diseases v. In most cases such antibodies are auto-antibodies v. Occasionally, these antibodies may be produced against foreign antigens that are immunologically cross-reactive with components of self tissue v. Antibodies against tissue antigens cause diseases by three main mechanisms (next slide)
Antibody mediated hypersensitivity (type II) v. Antibodies against cellular or matrix antigens cause tissue-specific diseases v. In most cases such antibodies are auto-antibodies v. Occasionally, these antibodies may be produced against foreign antigens that are immunologically cross-reactive with components of self tissue v. Antibodies against tissue antigens cause diseases by three main mechanisms (next slide)
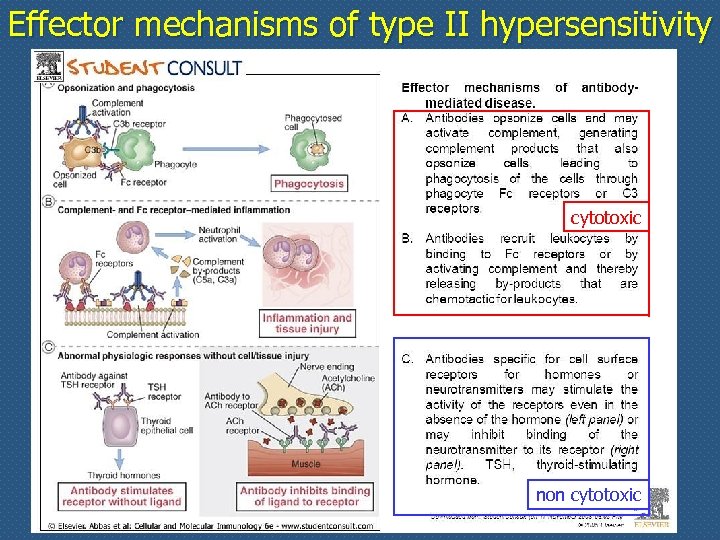 Effector mechanisms of type II hypersensitivity cytotoxic non cytotoxic
Effector mechanisms of type II hypersensitivity cytotoxic non cytotoxic
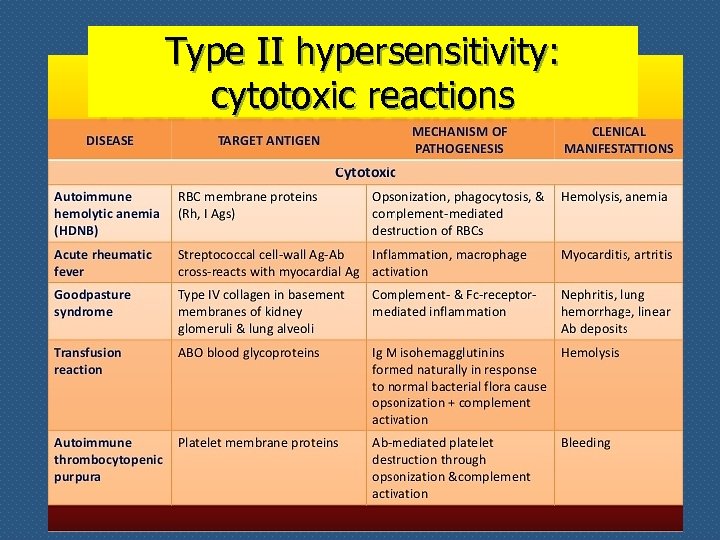 Type II hypersensitivity: cytotoxic reactions
Type II hypersensitivity: cytotoxic reactions
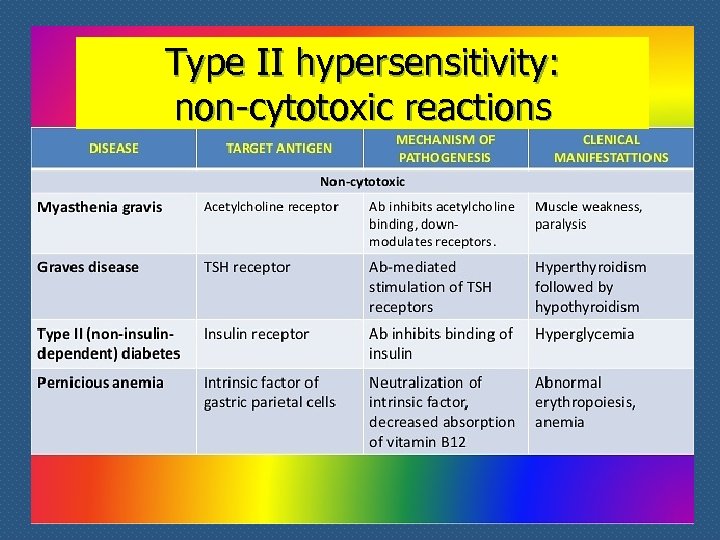 Type II hypersensitivity: non-cytotoxic reactions
Type II hypersensitivity: non-cytotoxic reactions
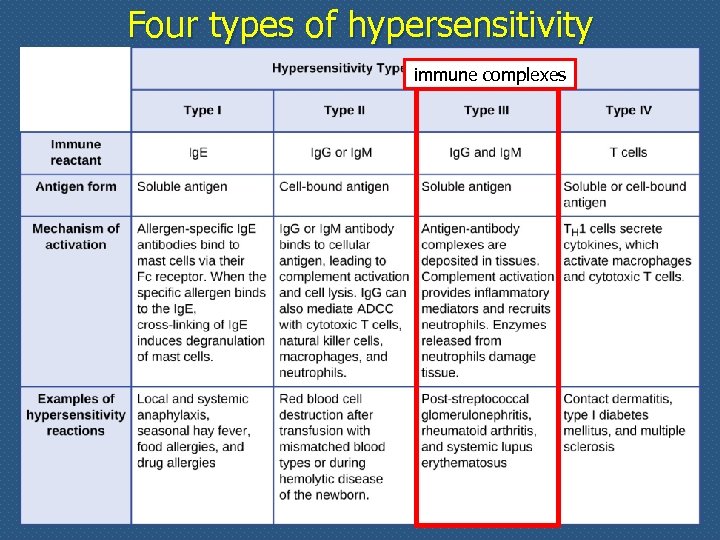 Four types of hypersensitivity immune complexes
Four types of hypersensitivity immune complexes
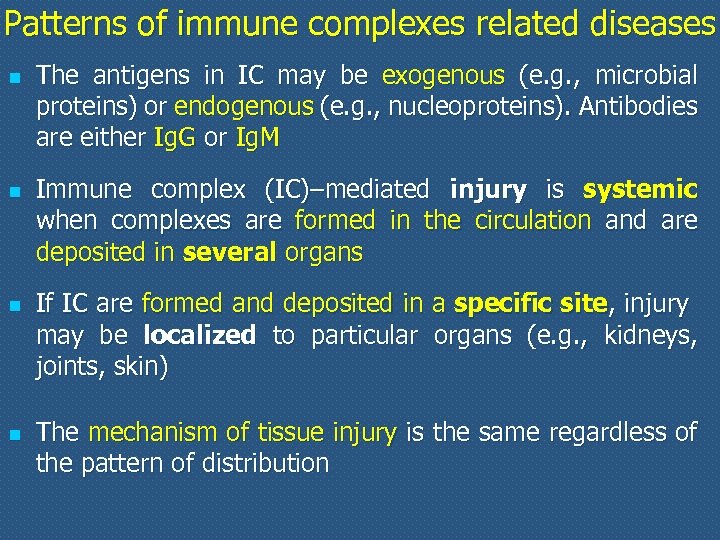 Patterns of immune complexes related diseases n n The antigens in IC may be exogenous (e. g. , microbial proteins) or endogenous (e. g. , nucleoproteins). Antibodies are either Ig. G or Ig. M Immune complex (IC)–mediated injury is systemic when complexes are formed in the circulation and are deposited in several organs If IC are formed and deposited in a specific site, injury may be localized to particular organs (e. g. , kidneys, joints, skin) The mechanism of tissue injury is the same regardless of the pattern of distribution
Patterns of immune complexes related diseases n n The antigens in IC may be exogenous (e. g. , microbial proteins) or endogenous (e. g. , nucleoproteins). Antibodies are either Ig. G or Ig. M Immune complex (IC)–mediated injury is systemic when complexes are formed in the circulation and are deposited in several organs If IC are formed and deposited in a specific site, injury may be localized to particular organs (e. g. , kidneys, joints, skin) The mechanism of tissue injury is the same regardless of the pattern of distribution
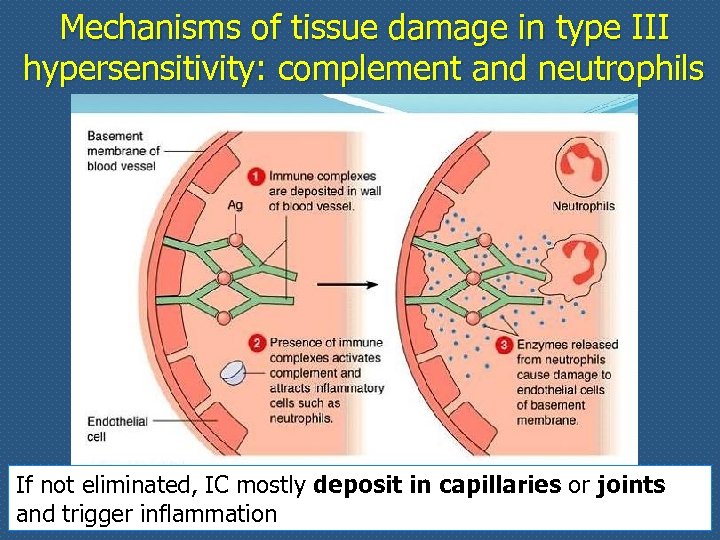 Mechanisms of tissue damage in type III hypersensitivity: complement and neutrophils If not eliminated, IC mostly deposit in capillaries or joints and trigger inflammation
Mechanisms of tissue damage in type III hypersensitivity: complement and neutrophils If not eliminated, IC mostly deposit in capillaries or joints and trigger inflammation
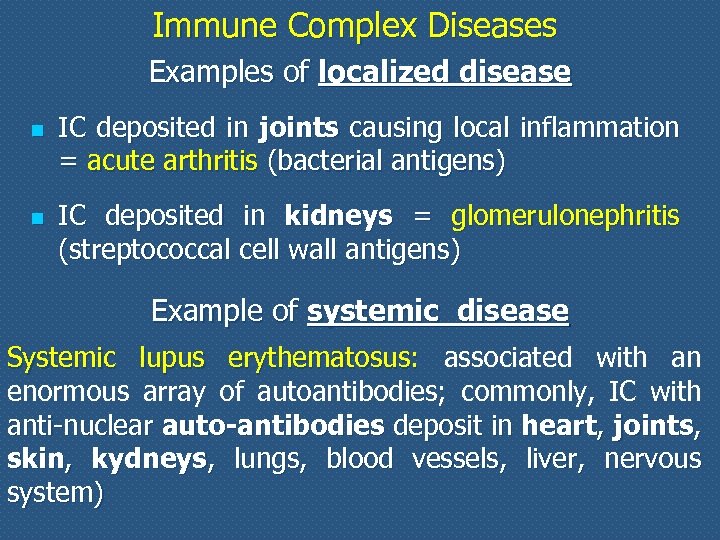 Immune Complex Diseases Examples of localized disease n n IC deposited in joints causing local inflammation = acute arthritis (bacterial antigens) IC deposited in kidneys = glomerulonephritis (streptococcal cell wall antigens) Example of systemic disease Systemic lupus erythematosus: associated with an enormous array of autoantibodies; commonly, IC with anti-nuclear auto-antibodies deposit in heart, joints, skin, kydneys, lungs, blood vessels, liver, nervous system)
Immune Complex Diseases Examples of localized disease n n IC deposited in joints causing local inflammation = acute arthritis (bacterial antigens) IC deposited in kidneys = glomerulonephritis (streptococcal cell wall antigens) Example of systemic disease Systemic lupus erythematosus: associated with an enormous array of autoantibodies; commonly, IC with anti-nuclear auto-antibodies deposit in heart, joints, skin, kydneys, lungs, blood vessels, liver, nervous system)
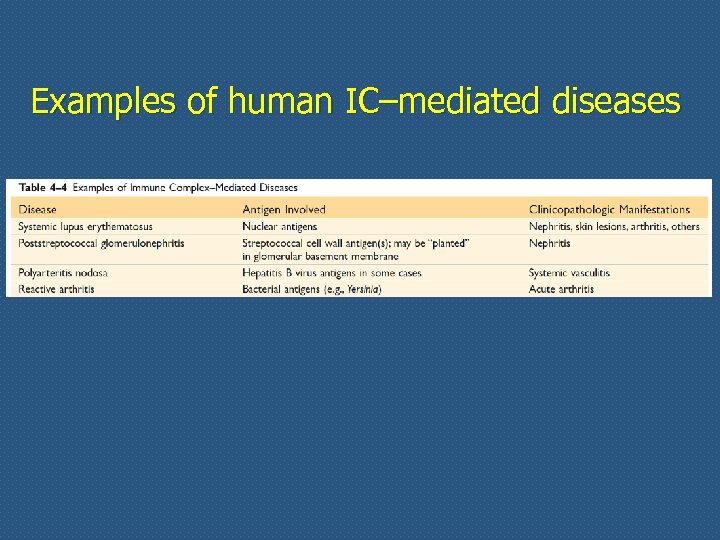 Examples of human IC–mediated diseases
Examples of human IC–mediated diseases
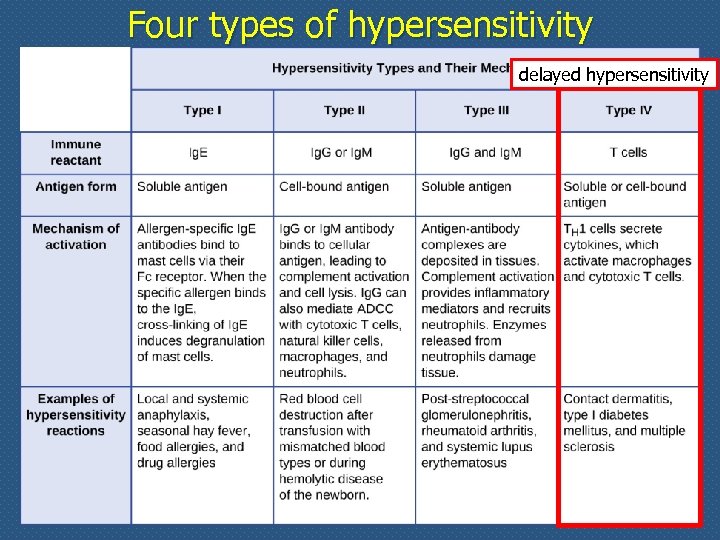 Four types of hypersensitivity delayed hypersensitivity
Four types of hypersensitivity delayed hypersensitivity
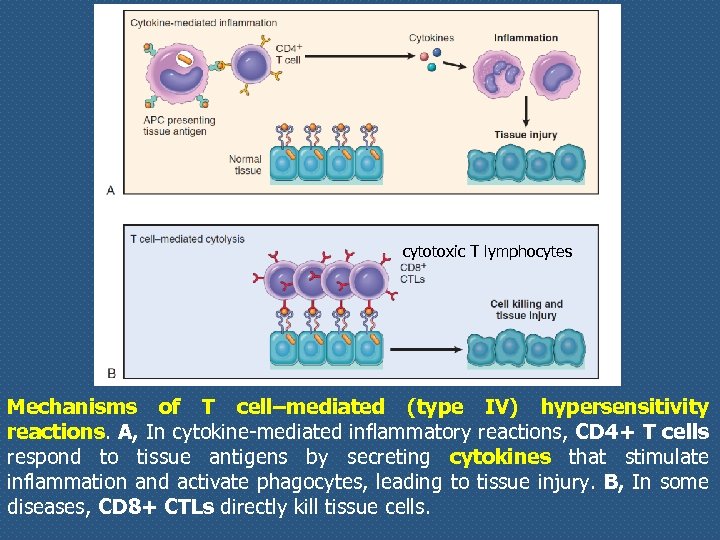 cytotoxic T lymphocytes Mechanisms of T cell–mediated (type IV) hypersensitivity reactions. A, In cytokine-mediated inflammatory reactions, CD 4+ T cells respond to tissue antigens by secreting cytokines that stimulate inflammation and activate phagocytes, leading to tissue injury. B, In some diseases, CD 8+ CTLs directly kill tissue cells.
cytotoxic T lymphocytes Mechanisms of T cell–mediated (type IV) hypersensitivity reactions. A, In cytokine-mediated inflammatory reactions, CD 4+ T cells respond to tissue antigens by secreting cytokines that stimulate inflammation and activate phagocytes, leading to tissue injury. B, In some diseases, CD 8+ CTLs directly kill tissue cells.
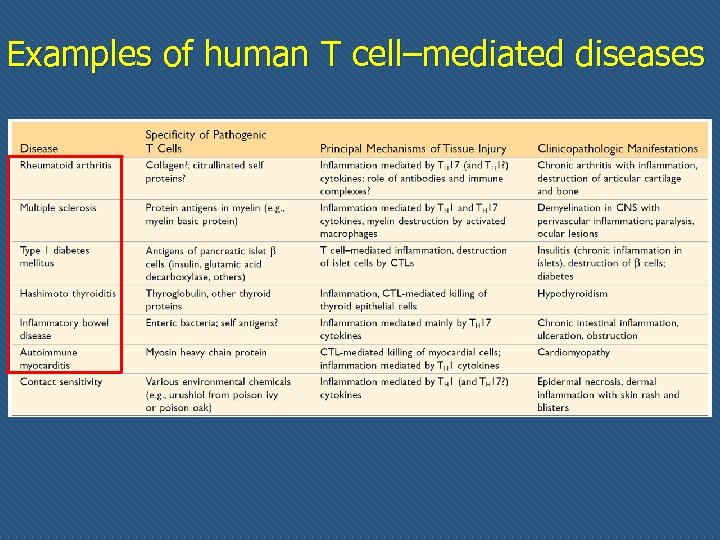 Examples of human T cell–mediated diseases
Examples of human T cell–mediated diseases
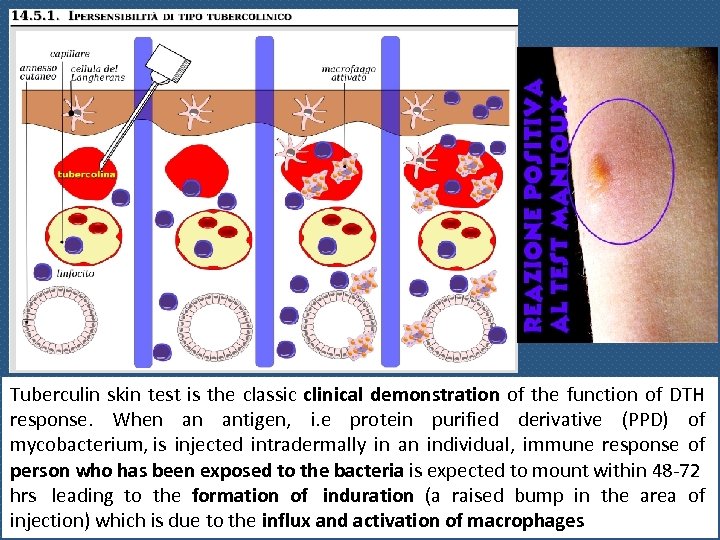 Tuberculin skin test is the classic clinical demonstration of the function of DTH response. When an antigen, i. e protein purified derivative (PPD) of mycobacterium, is injected intradermally in an individual, immune response of person who has been exposed to the bacteria is expected to mount within 48 -72 hrs leading to the formation of induration (a raised bump in the area of injection) which is due to the influx and activation of macrophages
Tuberculin skin test is the classic clinical demonstration of the function of DTH response. When an antigen, i. e protein purified derivative (PPD) of mycobacterium, is injected intradermally in an individual, immune response of person who has been exposed to the bacteria is expected to mount within 48 -72 hrs leading to the formation of induration (a raised bump in the area of injection) which is due to the influx and activation of macrophages
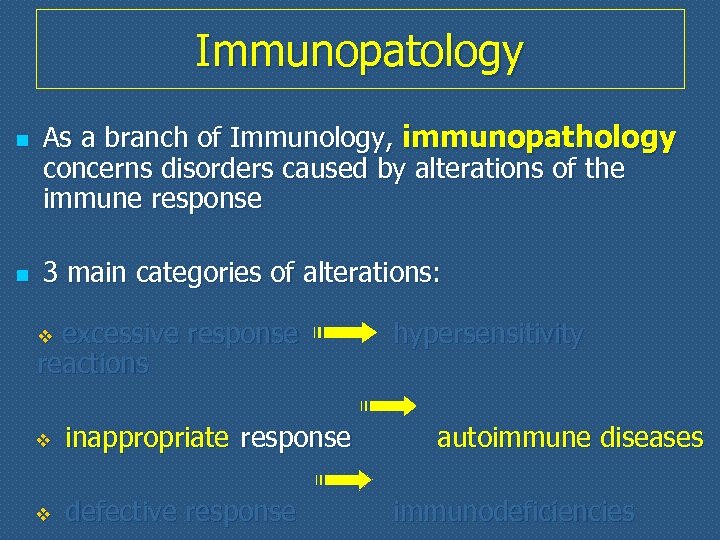 Immunopatology n n As a branch of Immunology, immunopathology concerns disorders caused by alterations of the immune response 3 main categories of alterations: excessive response reactions v v inappropriate response v defective response hypersensitivity autoimmune diseases immunodeficiencies
Immunopatology n n As a branch of Immunology, immunopathology concerns disorders caused by alterations of the immune response 3 main categories of alterations: excessive response reactions v v inappropriate response v defective response hypersensitivity autoimmune diseases immunodeficiencies
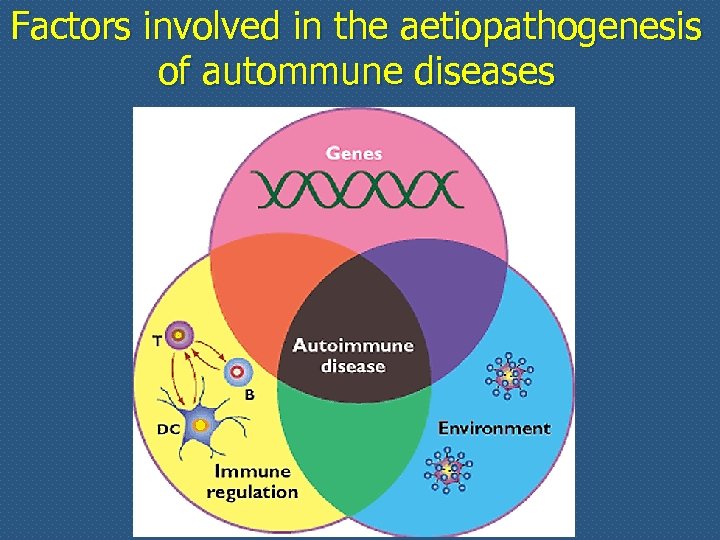 Factors involved in the aetiopathogenesis of autommune diseases
Factors involved in the aetiopathogenesis of autommune diseases
 Autoimmunity n n n Immune reactions to self antigens (i. e. , autoimmunity) are the underlying cause of numerous human diseases Autoimmune diseases are estimated to affect 2% to 5% of the population in developed countries, and appear to be increasing in incidence The evidence that some human diseases are indeed the result of autoimmune reactions is more persuasive for some than for others in which the role of autoimmunity is suspected but not proved
Autoimmunity n n n Immune reactions to self antigens (i. e. , autoimmunity) are the underlying cause of numerous human diseases Autoimmune diseases are estimated to affect 2% to 5% of the population in developed countries, and appear to be increasing in incidence The evidence that some human diseases are indeed the result of autoimmune reactions is more persuasive for some than for others in which the role of autoimmunity is suspected but not proved
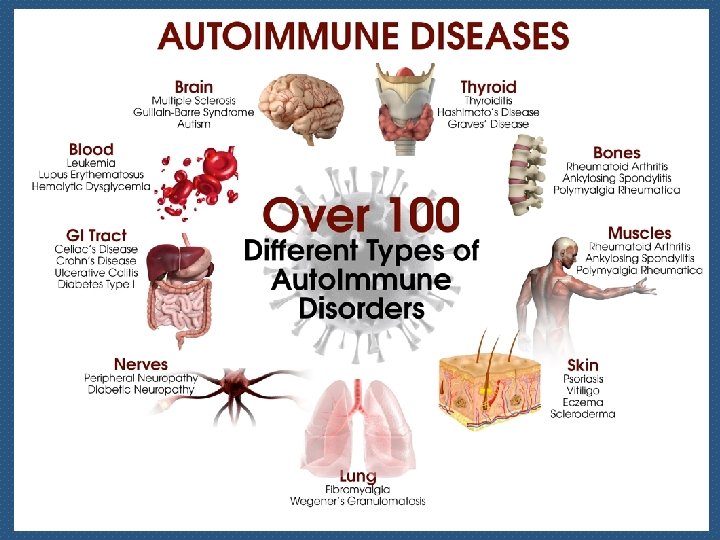
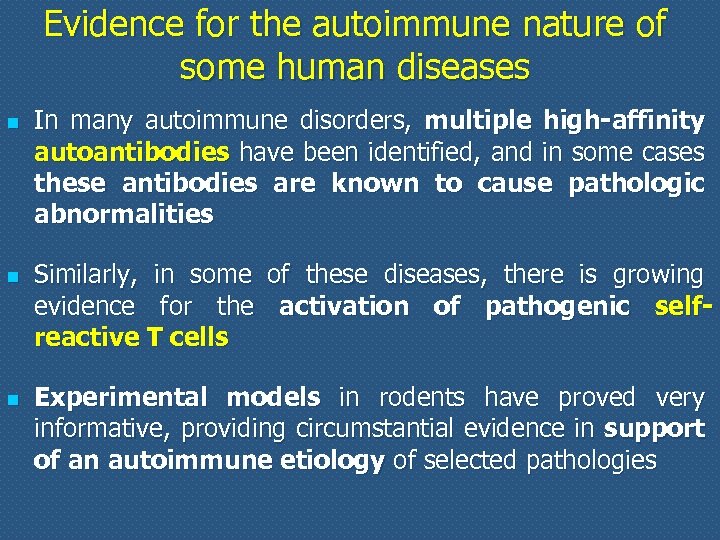 Evidence for the autoimmune nature of some human diseases n n n In many autoimmune disorders, multiple high-affinity autoantibodies have been identified, and in some cases these antibodies are known to cause pathologic abnormalities Similarly, in some of these diseases, there is growing evidence for the activation of pathogenic selfreactive T cells Experimental models in rodents have proved very informative, providing circumstantial evidence in support of an autoimmune etiology of selected pathologies
Evidence for the autoimmune nature of some human diseases n n n In many autoimmune disorders, multiple high-affinity autoantibodies have been identified, and in some cases these antibodies are known to cause pathologic abnormalities Similarly, in some of these diseases, there is growing evidence for the activation of pathogenic selfreactive T cells Experimental models in rodents have proved very informative, providing circumstantial evidence in support of an autoimmune etiology of selected pathologies
 Introducing autoimmunity Basic items underlying unresponsiveness to selfantigens n Immunological tolerance (central and peripheral) n Negative selection n Role of regulatory T cells (Treg)
Introducing autoimmunity Basic items underlying unresponsiveness to selfantigens n Immunological tolerance (central and peripheral) n Negative selection n Role of regulatory T cells (Treg)
 Immunologic tolerance n n n Billions of different antigen receptors are randomly generated in developing T and B lymphocytes It is not surprising that during this process, receptors that recognize self antigens are produced Since these antigens cannot all be concealed from the immune system, there must be means of eliminating or controlling self-reactive lymphocytes [tolerance] The breakdown of tolerance is the basis of autoimmunity
Immunologic tolerance n n n Billions of different antigen receptors are randomly generated in developing T and B lymphocytes It is not surprising that during this process, receptors that recognize self antigens are produced Since these antigens cannot all be concealed from the immune system, there must be means of eliminating or controlling self-reactive lymphocytes [tolerance] The breakdown of tolerance is the basis of autoimmunity
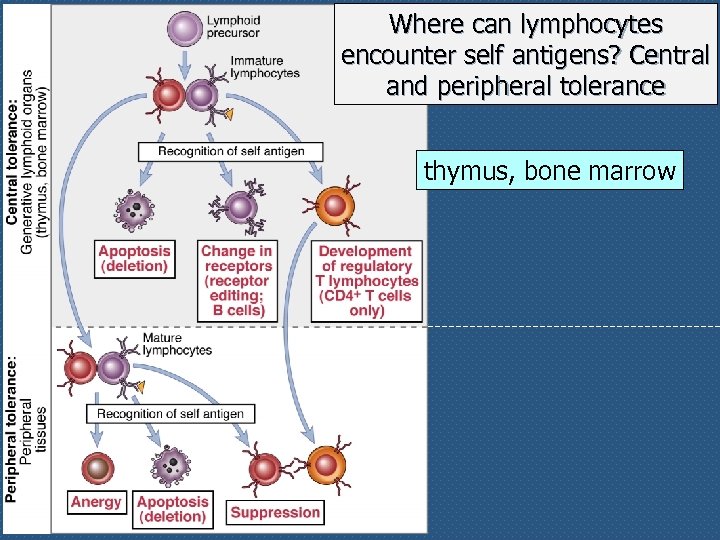 Where can lymphocytes encounter self antigens? Central and peripheral tolerance thymus, bone marrow
Where can lymphocytes encounter self antigens? Central and peripheral tolerance thymus, bone marrow
 Central tolerance: thymus and bone marrow The interaction of lymphoid precursors with self antigens in the central lymphoid organs may have three main outcomes: 1. some immature lymphos (both B and T) are killed by apoptosis (negative selection) 2. in the bone marrow, some self-reactive B lymphos switch to new antigen receptors that are not self-reactive (receptor editing) 3. in the thymus, some T lymphos differentiate into regulatory T cells (Treg)
Central tolerance: thymus and bone marrow The interaction of lymphoid precursors with self antigens in the central lymphoid organs may have three main outcomes: 1. some immature lymphos (both B and T) are killed by apoptosis (negative selection) 2. in the bone marrow, some self-reactive B lymphos switch to new antigen receptors that are not self-reactive (receptor editing) 3. in the thymus, some T lymphos differentiate into regulatory T cells (Treg)
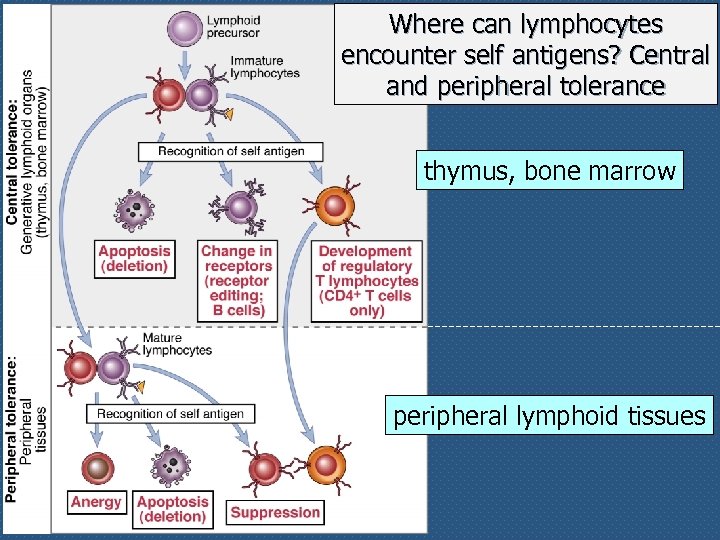 Where can lymphocytes encounter self antigens? Central and peripheral tolerance thymus, bone marrow peripheral lymphoid tissues
Where can lymphocytes encounter self antigens? Central and peripheral tolerance thymus, bone marrow peripheral lymphoid tissues
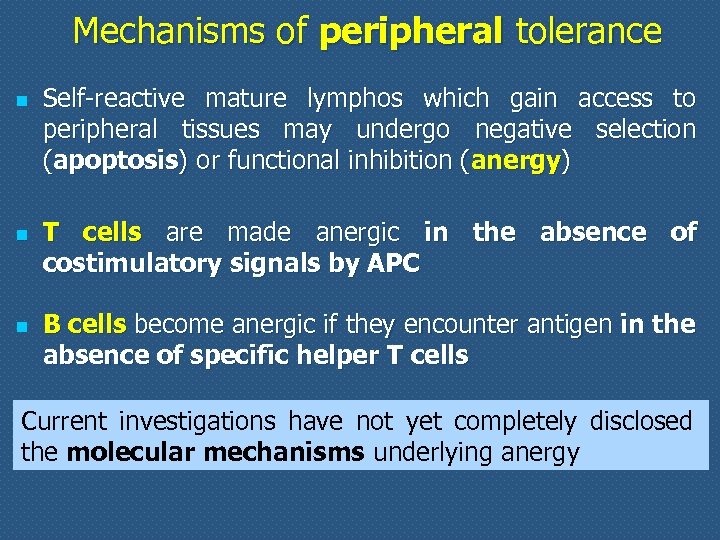 Mechanisms of peripheral tolerance n n n Self-reactive mature lymphos which gain access to peripheral tissues may undergo negative selection (apoptosis) or functional inhibition (anergy) T cells are made anergic in the absence of costimulatory signals by APC B cells become anergic if they encounter antigen in the absence of specific helper T cells Current investigations have not yet completely disclosed the molecular mechanisms underlying anergy
Mechanisms of peripheral tolerance n n n Self-reactive mature lymphos which gain access to peripheral tissues may undergo negative selection (apoptosis) or functional inhibition (anergy) T cells are made anergic in the absence of costimulatory signals by APC B cells become anergic if they encounter antigen in the absence of specific helper T cells Current investigations have not yet completely disclosed the molecular mechanisms underlying anergy
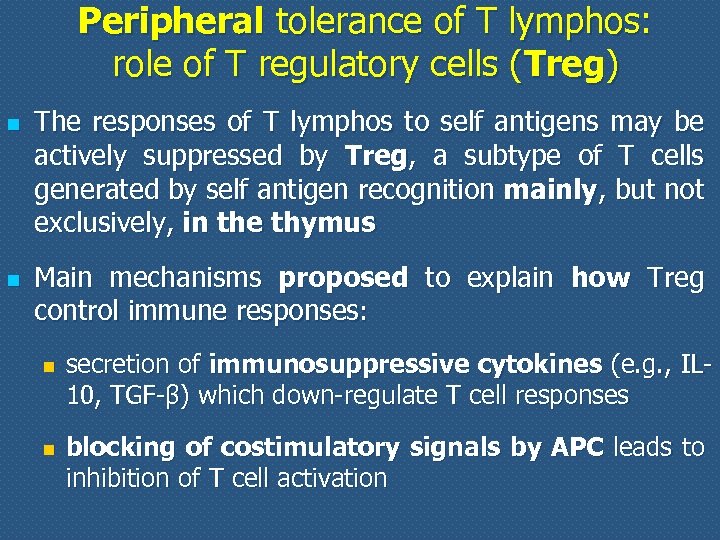 Peripheral tolerance of T lymphos: role of T regulatory cells (Treg) n n The responses of T lymphos to self antigens may be actively suppressed by Treg, a subtype of T cells generated by self antigen recognition mainly, but not exclusively, in the thymus Main mechanisms proposed to explain how Treg control immune responses: n n secretion of immunosuppressive cytokines (e. g. , IL 10, TGF-β) which down-regulate T cell responses blocking of costimulatory signals by APC leads to inhibition of T cell activation
Peripheral tolerance of T lymphos: role of T regulatory cells (Treg) n n The responses of T lymphos to self antigens may be actively suppressed by Treg, a subtype of T cells generated by self antigen recognition mainly, but not exclusively, in the thymus Main mechanisms proposed to explain how Treg control immune responses: n n secretion of immunosuppressive cytokines (e. g. , IL 10, TGF-β) which down-regulate T cell responses blocking of costimulatory signals by APC leads to inhibition of T cell activation
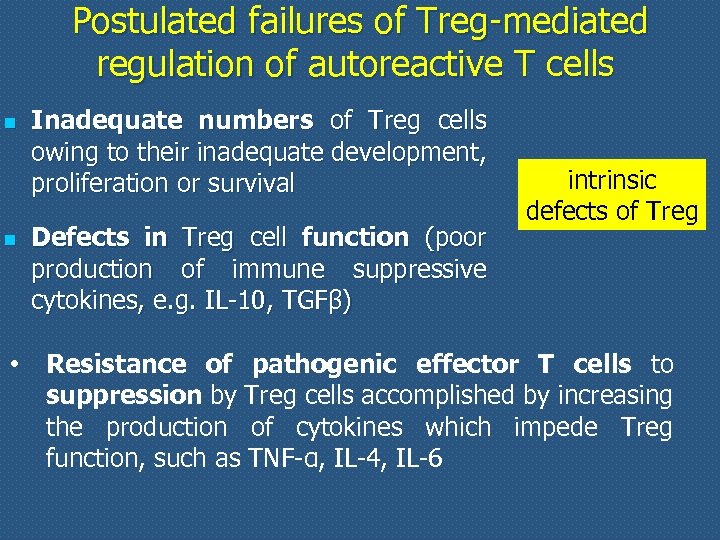 Postulated failures of Treg-mediated regulation of autoreactive T cells n n • Inadequate numbers of Treg cells owing to their inadequate development, proliferation or survival Defects in Treg cell function (poor production of immune suppressive cytokines, e. g. IL-10, TGFβ) intrinsic defects of Treg Resistance of pathogenic effector T cells to suppression by Treg cells accomplished by increasing the production of cytokines which impede Treg function, such as TNF-α, IL-4, IL-6
Postulated failures of Treg-mediated regulation of autoreactive T cells n n • Inadequate numbers of Treg cells owing to their inadequate development, proliferation or survival Defects in Treg cell function (poor production of immune suppressive cytokines, e. g. IL-10, TGFβ) intrinsic defects of Treg Resistance of pathogenic effector T cells to suppression by Treg cells accomplished by increasing the production of cytokines which impede Treg function, such as TNF-α, IL-4, IL-6
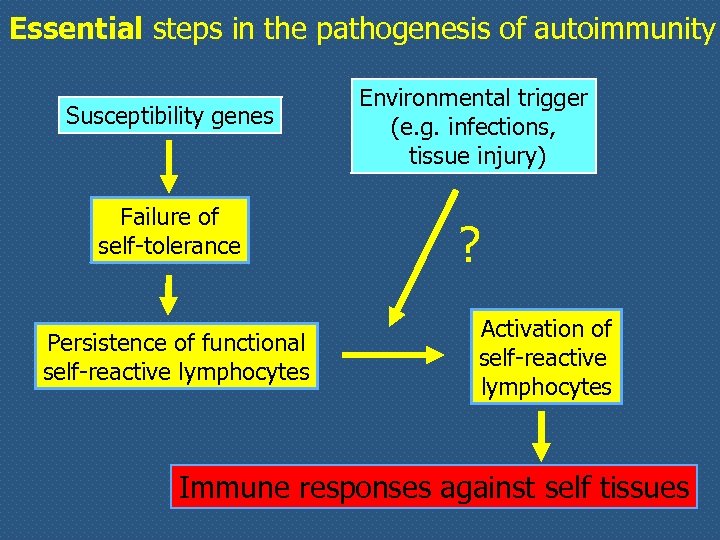 Essential steps in the pathogenesis of autoimmunity Susceptibility genes Failure of self-tolerance Persistence of functional self-reactive lymphocytes Environmental trigger (e. g. infections, tissue injury) ? Activation of self-reactive lymphocytes Immune responses against self tissues
Essential steps in the pathogenesis of autoimmunity Susceptibility genes Failure of self-tolerance Persistence of functional self-reactive lymphocytes Environmental trigger (e. g. infections, tissue injury) ? Activation of self-reactive lymphocytes Immune responses against self tissues
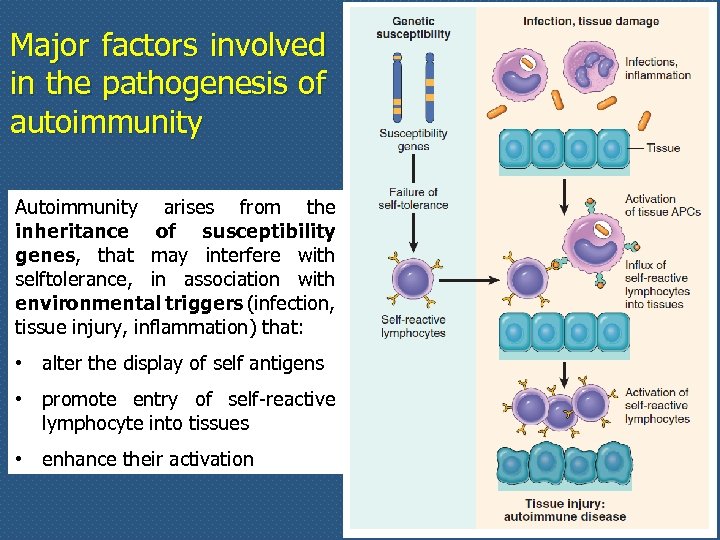 Major factors involved in the pathogenesis of autoimmunity Autoimmunity arises from the inheritance of susceptibility genes, that may interfere with selftolerance, in association with environmental triggers (infection, tissue injury, inflammation) that: • alter the display of self antigens • promote entry of self-reactive lymphocyte into tissues • enhance their activation
Major factors involved in the pathogenesis of autoimmunity Autoimmunity arises from the inheritance of susceptibility genes, that may interfere with selftolerance, in association with environmental triggers (infection, tissue injury, inflammation) that: • alter the display of self antigens • promote entry of self-reactive lymphocyte into tissues • enhance their activation
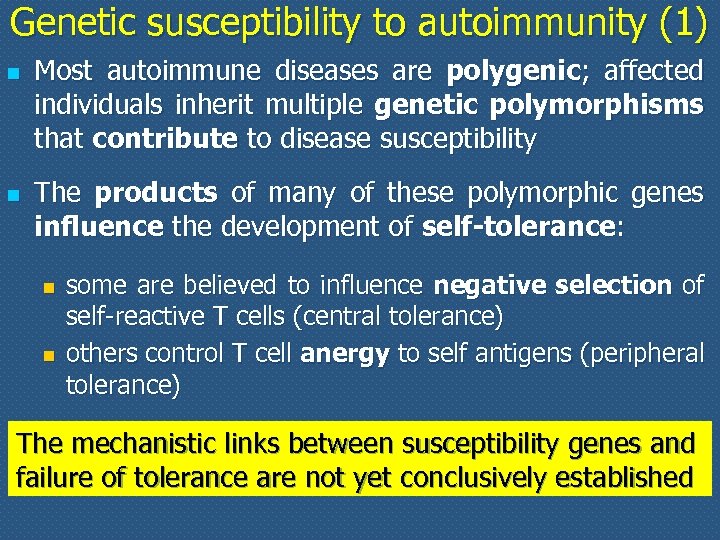 Genetic susceptibility to autoimmunity (1) n n Most autoimmune diseases are polygenic; affected individuals inherit multiple genetic polymorphisms that contribute to disease susceptibility The products of many of these polymorphic genes influence the development of self-tolerance: n n some are believed to influence negative selection of self-reactive T cells (central tolerance) others control T cell anergy to self antigens (peripheral tolerance) The mechanistic links between susceptibility genes and failure of tolerance are not yet conclusively established
Genetic susceptibility to autoimmunity (1) n n Most autoimmune diseases are polygenic; affected individuals inherit multiple genetic polymorphisms that contribute to disease susceptibility The products of many of these polymorphic genes influence the development of self-tolerance: n n some are believed to influence negative selection of self-reactive T cells (central tolerance) others control T cell anergy to self antigens (peripheral tolerance) The mechanistic links between susceptibility genes and failure of tolerance are not yet conclusively established
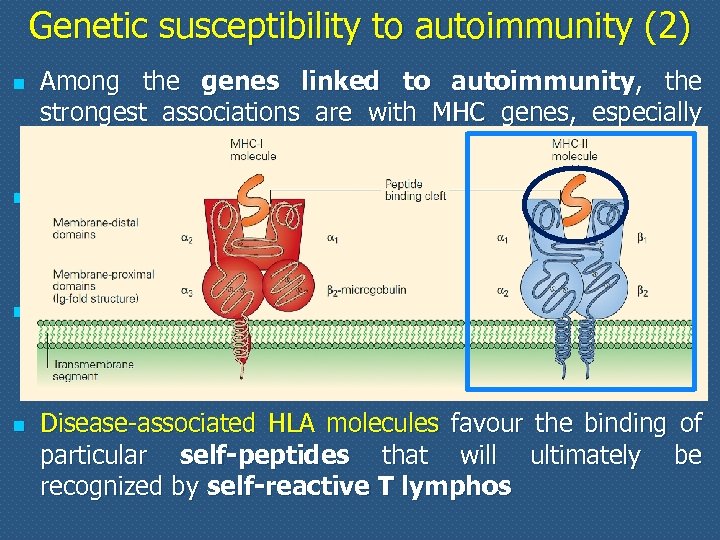 Genetic susceptibility to autoimmunity (2) n n Among the genes linked to autoimmunity, the strongest associations are with MHC genes, especially class II MHC genes Class II MHC genes are involved in the selection and activation of CD 4+ T cells that regulate both humoral and cell-mediated immune response to protein antigens In many autoimmune diseases, the disease-associated HLA molecules differ in their peptide binding cleft from HLA molecules that are not disease-associated Disease-associated HLA molecules favour the binding of particular self-peptides that will ultimately be recognized by self-reactive T lymphos
Genetic susceptibility to autoimmunity (2) n n Among the genes linked to autoimmunity, the strongest associations are with MHC genes, especially class II MHC genes Class II MHC genes are involved in the selection and activation of CD 4+ T cells that regulate both humoral and cell-mediated immune response to protein antigens In many autoimmune diseases, the disease-associated HLA molecules differ in their peptide binding cleft from HLA molecules that are not disease-associated Disease-associated HLA molecules favour the binding of particular self-peptides that will ultimately be recognized by self-reactive T lymphos
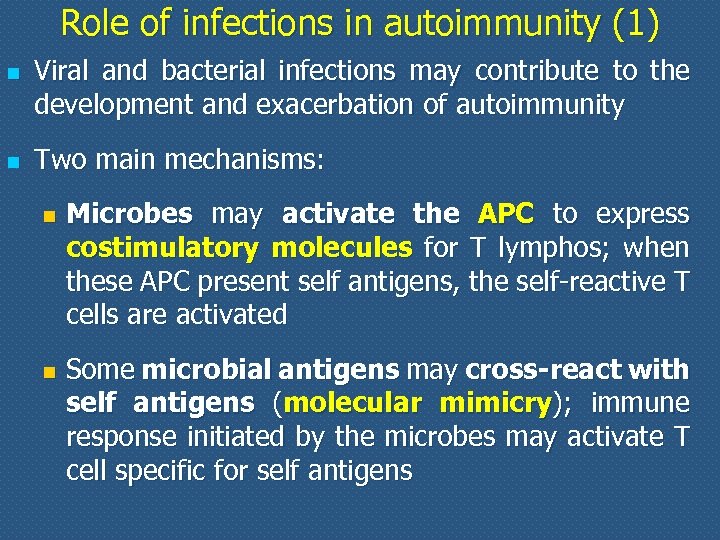 Role of infections in autoimmunity (1) n n Viral and bacterial infections may contribute to the development and exacerbation of autoimmunity Two main mechanisms: n n Microbes may activate the APC to express costimulatory molecules for T lymphos; when these APC present self antigens, the self-reactive T cells are activated Some microbial antigens may cross-react with self antigens (molecular mimicry); immune response initiated by the microbes may activate T cell specific for self antigens
Role of infections in autoimmunity (1) n n Viral and bacterial infections may contribute to the development and exacerbation of autoimmunity Two main mechanisms: n n Microbes may activate the APC to express costimulatory molecules for T lymphos; when these APC present self antigens, the self-reactive T cells are activated Some microbial antigens may cross-react with self antigens (molecular mimicry); immune response initiated by the microbes may activate T cell specific for self antigens
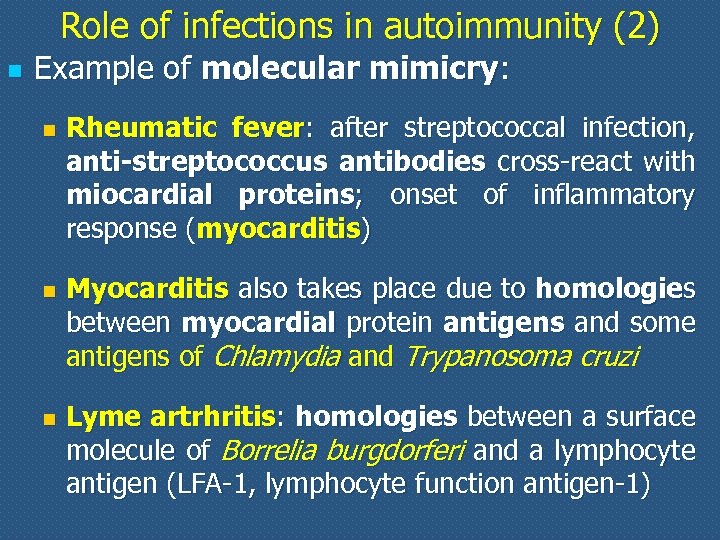 Role of infections in autoimmunity (2) n Example of molecular mimicry: n n n Rheumatic fever: after streptococcal infection, anti-streptococcus antibodies cross-react with miocardial proteins; onset of inflammatory response (myocarditis) Myocarditis also takes place due to homologies between myocardial protein antigens and some antigens of Chlamydia and Trypanosoma cruzi Lyme artrhritis: homologies between a surface molecule of Borrelia burgdorferi and a lymphocyte antigen (LFA-1, lymphocyte function antigen-1)
Role of infections in autoimmunity (2) n Example of molecular mimicry: n n n Rheumatic fever: after streptococcal infection, anti-streptococcus antibodies cross-react with miocardial proteins; onset of inflammatory response (myocarditis) Myocarditis also takes place due to homologies between myocardial protein antigens and some antigens of Chlamydia and Trypanosoma cruzi Lyme artrhritis: homologies between a surface molecule of Borrelia burgdorferi and a lymphocyte antigen (LFA-1, lymphocyte function antigen-1)
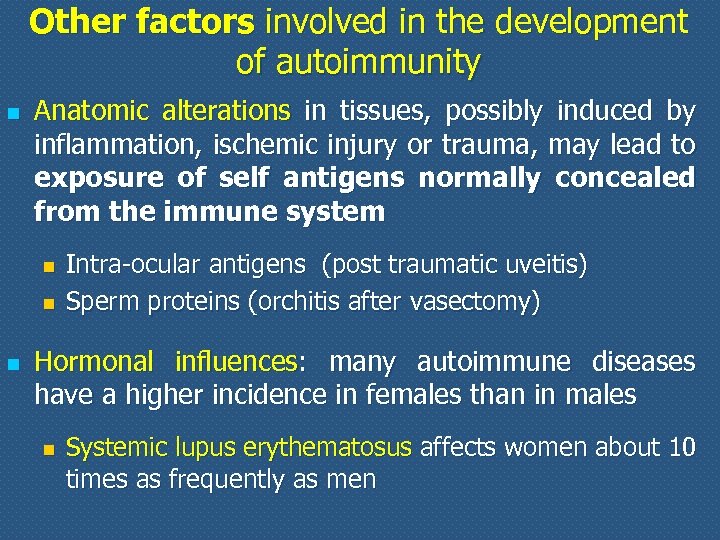 Other factors involved in the development of autoimmunity n Anatomic alterations in tissues, possibly induced by inflammation, ischemic injury or trauma, may lead to exposure of self antigens normally concealed from the immune system n n n Intra-ocular antigens (post traumatic uveitis) Sperm proteins (orchitis after vasectomy) Hormonal influences: many autoimmune diseases have a higher incidence in females than in males n Systemic lupus erythematosus affects women about 10 times as frequently as men
Other factors involved in the development of autoimmunity n Anatomic alterations in tissues, possibly induced by inflammation, ischemic injury or trauma, may lead to exposure of self antigens normally concealed from the immune system n n n Intra-ocular antigens (post traumatic uveitis) Sperm proteins (orchitis after vasectomy) Hormonal influences: many autoimmune diseases have a higher incidence in females than in males n Systemic lupus erythematosus affects women about 10 times as frequently as men
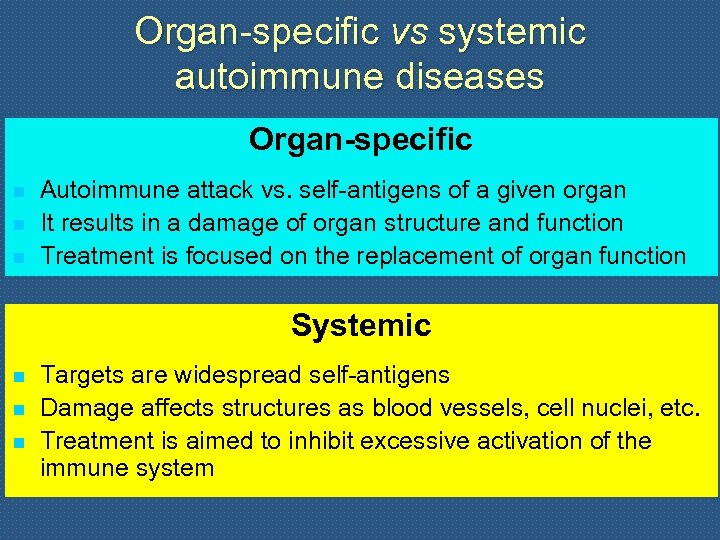 Organ-specific vs systemic autoimmune diseases Organ-specific n n n Autoimmune attack vs. self-antigens of a given organ It results in a damage of organ structure and function Treatment is focused on the replacement of organ function Systemic n n n Targets are widespread self-antigens Damage affects structures as blood vessels, cell nuclei, etc. Treatment is aimed to inhibit excessive activation of the immune system
Organ-specific vs systemic autoimmune diseases Organ-specific n n n Autoimmune attack vs. self-antigens of a given organ It results in a damage of organ structure and function Treatment is focused on the replacement of organ function Systemic n n n Targets are widespread self-antigens Damage affects structures as blood vessels, cell nuclei, etc. Treatment is aimed to inhibit excessive activation of the immune system
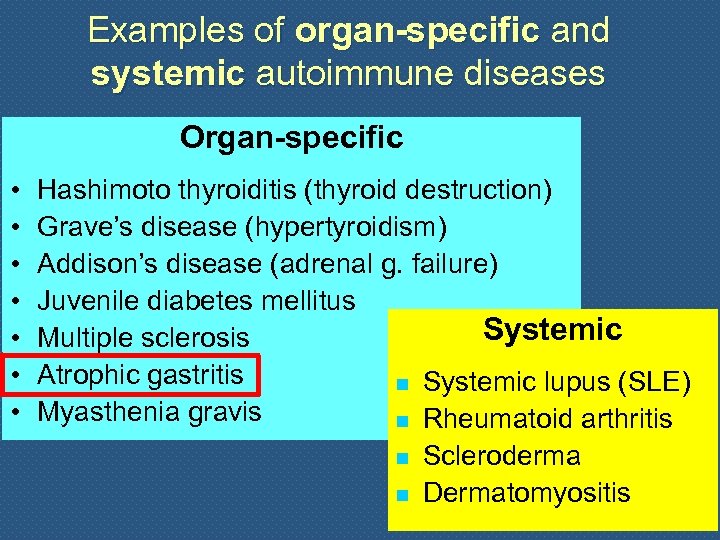 Examples of organ-specific and systemic autoimmune diseases Organ-specific • • Hashimoto thyroiditis (thyroid destruction) Grave’s disease (hypertyroidism) Addison’s disease (adrenal g. failure) Juvenile diabetes mellitus Systemic Multiple sclerosis Atrophic gastritis n Systemic lupus (SLE) Myasthenia gravis n Rheumatoid arthritis n n Scleroderma Dermatomyositis
Examples of organ-specific and systemic autoimmune diseases Organ-specific • • Hashimoto thyroiditis (thyroid destruction) Grave’s disease (hypertyroidism) Addison’s disease (adrenal g. failure) Juvenile diabetes mellitus Systemic Multiple sclerosis Atrophic gastritis n Systemic lupus (SLE) Myasthenia gravis n Rheumatoid arthritis n n Scleroderma Dermatomyositis
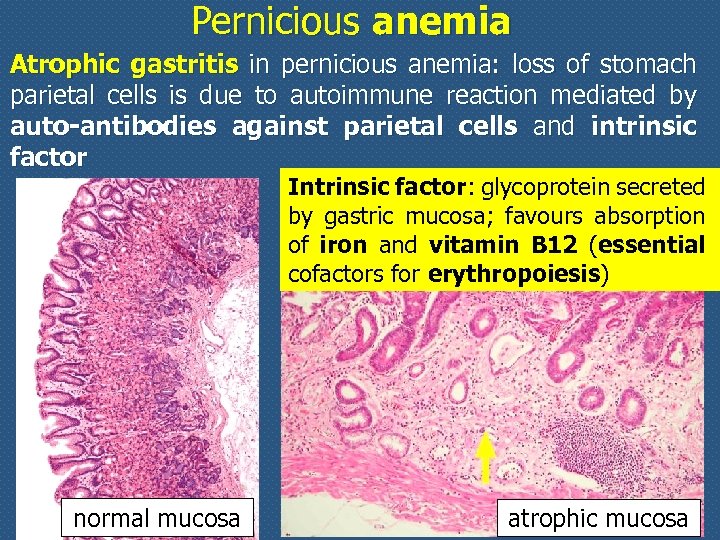 Pernicious anemia Atrophic gastritis in pernicious anemia: loss of stomach parietal cells is due to autoimmune reaction mediated by auto-antibodies against parietal cells and intrinsic factor Intrinsic factor: glycoprotein secreted by gastric mucosa; favours absorption of iron and vitamin B 12 (essential cofactors for erythropoiesis) normal mucosa atrophic mucosa
Pernicious anemia Atrophic gastritis in pernicious anemia: loss of stomach parietal cells is due to autoimmune reaction mediated by auto-antibodies against parietal cells and intrinsic factor Intrinsic factor: glycoprotein secreted by gastric mucosa; favours absorption of iron and vitamin B 12 (essential cofactors for erythropoiesis) normal mucosa atrophic mucosa
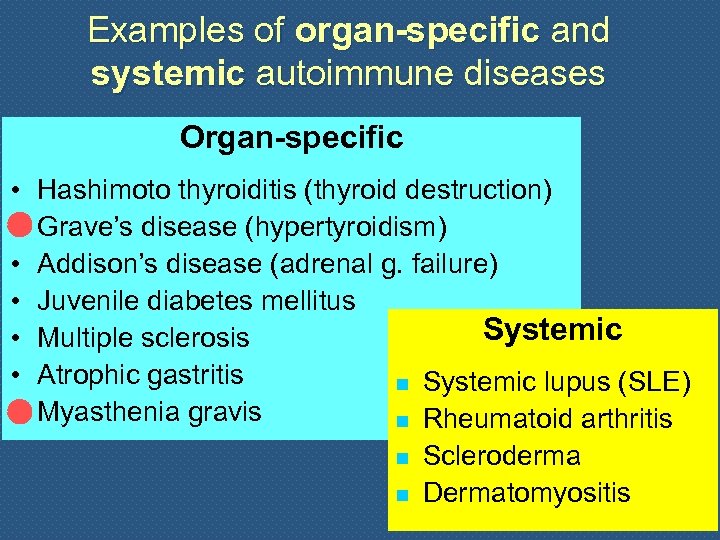 Examples of organ-specific and systemic autoimmune diseases Organ-specific • • Hashimoto thyroiditis (thyroid destruction) Grave’s disease (hypertyroidism) Addison’s disease (adrenal g. failure) Juvenile diabetes mellitus Systemic Multiple sclerosis Atrophic gastritis n Systemic lupus (SLE) Myasthenia gravis n Rheumatoid arthritis n n Scleroderma Dermatomyositis
Examples of organ-specific and systemic autoimmune diseases Organ-specific • • Hashimoto thyroiditis (thyroid destruction) Grave’s disease (hypertyroidism) Addison’s disease (adrenal g. failure) Juvenile diabetes mellitus Systemic Multiple sclerosis Atrophic gastritis n Systemic lupus (SLE) Myasthenia gravis n Rheumatoid arthritis n n Scleroderma Dermatomyositis
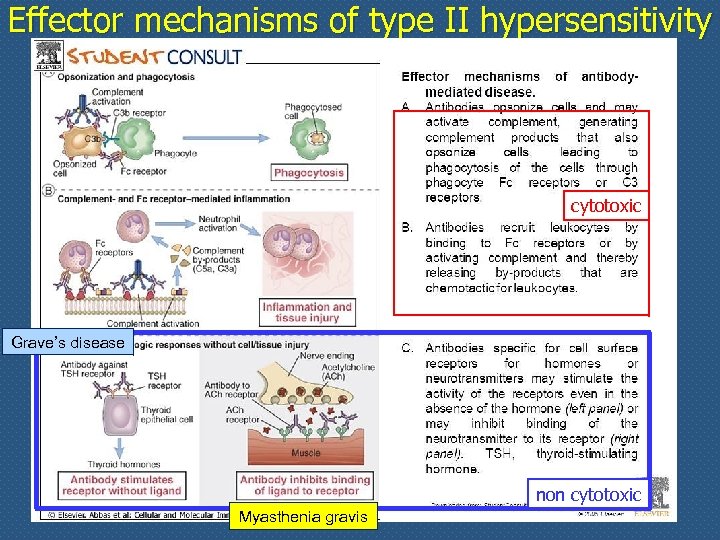 Effector mechanisms of type II hypersensitivity cytotoxic Grave’s disease non cytotoxic Myasthenia gravis
Effector mechanisms of type II hypersensitivity cytotoxic Grave’s disease non cytotoxic Myasthenia gravis


