c20c65d394f2b6af586718c6fda0506c.ppt
- Количество слайдов: 1
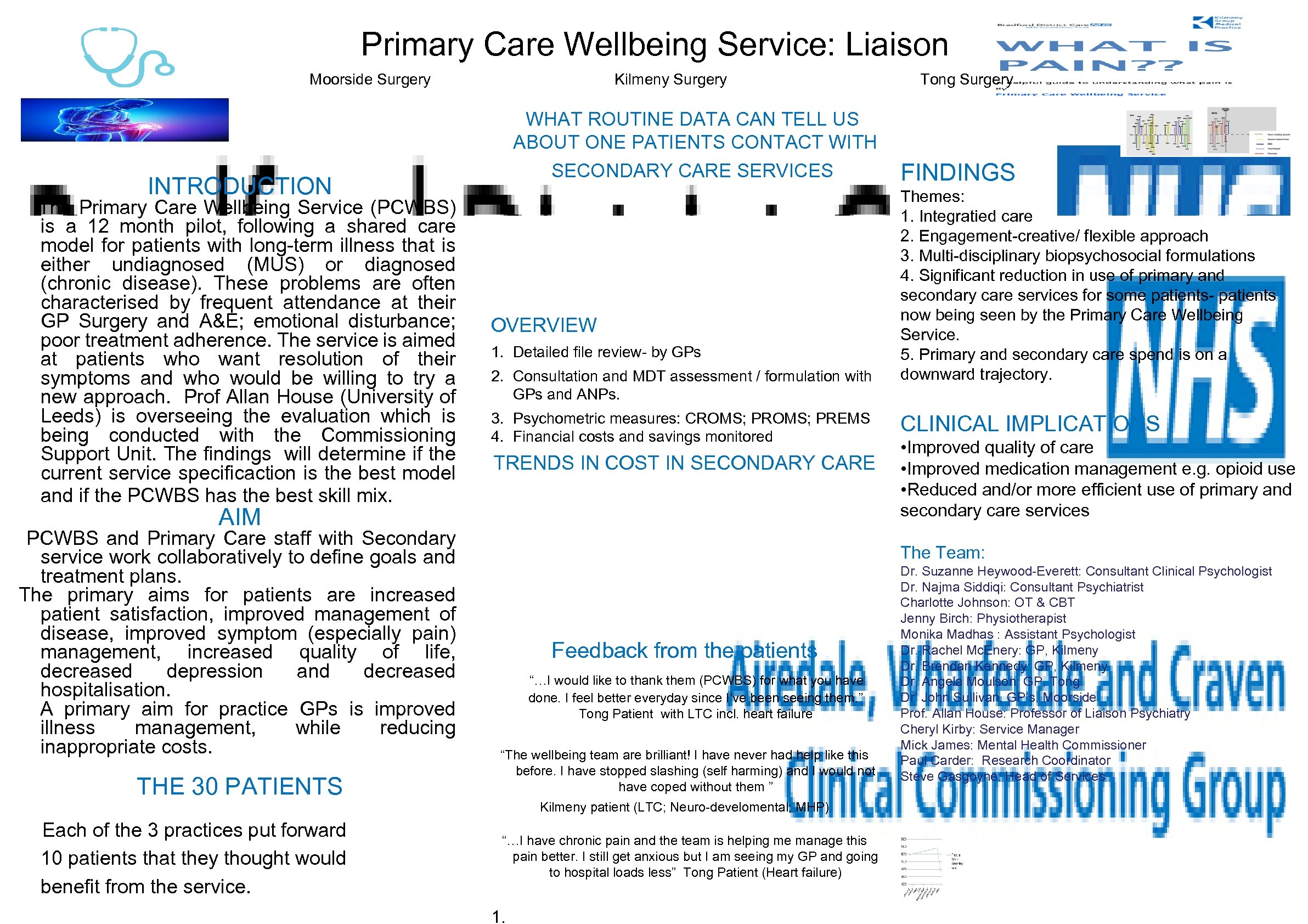
Primary Care Wellbeing Service: Liaison Moorside Surgery Kilmeny Surgery WHAT ROUTINE DATA CAN TELL US ABOUT ONE PATIENTS CONTACT WITH SECONDARY CARE SERVICES INTRODUCTION The Primary Care Wellbeing Service (PCWBS) is a 12 month pilot, following a shared care model for patients with long-term illness that is either undiagnosed (MUS) or diagnosed (chronic disease). These problems are often characterised by frequent attendance at their GP Surgery and A&E; emotional disturbance; poor treatment adherence. The service is aimed at patients who want resolution of their symptoms and who would be willing to try a new approach. Prof Allan House (University of Leeds) is overseeing the evaluation which is being conducted with the Commissioning Support Unit. The findings will determine if the current service specificaction is the best model and if the PCWBS has the best skill mix. OVERVIEW 1. Detailed file review- by GPs 2. Consultation and MDT assessment / formulation with GPs and ANPs. 3. Psychometric measures: CROMS; PREMS 4. Financial costs and savings monitored TRENDS IN COST IN SECONDARY CARE AIM PCWBS and Primary Care staff with Secondary service work collaboratively to define goals and treatment plans. The primary aims for patients are increased patient satisfaction, improved management of disease, improved symptom (especially pain) management, increased quality of life, decreased depression and decreased hospitalisation. A primary aim for practice GPs is improved illness management, while reducing inappropriate costs. THE 30 PATIENTS Each of the 3 practices put forward 10 patients that they thought would benefit from the service. Tong Surgery FINDINGS Themes: 1. Integratied care 2. Engagement-creative/ flexible approach 3. Multi-disciplinary biopsychosocial formulations 4. Significant reduction in use of primary and secondary care services for some patients- patients now being seen by the Primary Care Wellbeing Service. 5. Primary and secondary care spend is on a downward trajectory. CLINICAL IMPLICATIONS • Improved quality of care • Improved medication management e. g. opioid use • Reduced and/or more efficient use of primary and secondary care services The Team: Feedback from the patients “…I would like to thank them (PCWBS) for what you have done. I feel better everyday since I’ve been seeing them. ” Tong Patient with LTC incl. heart failure “The wellbeing team are brilliant! I have never had help like this before. I have stopped slashing (self harming) and I would not have coped without them ” Kilmeny patient (LTC; Neuro-develomental; MHP) “…I have chronic pain and the team is helping me manage this pain better. I still get anxious but I am seeing my GP and going to hospital loads less” Tong Patient (Heart failure) 1. Dr. Suzanne Heywood-Everett: Consultant Clinical Psychologist Dr. Najma Siddiqi: Consultant Psychiatrist Charlotte Johnson: OT & CBT Jenny Birch: Physiotherapist Monika Madhas : Assistant Psychologist Dr. Rachel Mc. Enery: GP, Kilmeny Dr. Brendan Kennedy: GP, Kilmeny Dr. Angela Moulson: GP, Tong Dr’ John Sullivan, GP’s, Moorside Prof. Allan House: Professor of Liaison Psychiatry Cheryl Kirby: Service Manager Mick James: Mental Health Commissioner Paul Carder: Research Coordinator Steve Gasgoyne: Head of Services
c20c65d394f2b6af586718c6fda0506c.ppt