6ed7427d3fb646bc37f6cef6f9824b17.ppt
- Количество слайдов: 101

Primary Care and Antimicrobial Use: Heroes or Villains? J. Todd Weber, MD Director, Office of Antimicrobial Resistance Centers for Disease Control and Prevention October 16, 2006 Annual Meeting Tucson, Arizona 16 Oct 2006
Disclaimer • The findings and conclusions in this presentation have not been formally disseminated by the Centers for Disease Control and Prevention and should not be construed to represent any agency determination or policy. 16 Oct 2006
Fighting Antimicrobial Resistance: Where do we stand? • New drugs (classes) will not be available in the short term • With a notable exception, vaccines have not been produced that address the problem of resistance • Infection control in healthcare settings remains imperfect • Reducing the discretionary use when possible is helpful, but even if we use these drugs with exquisite precision, resistance will continue to evolve and spread • Adherence to multidrug regimens to prevent emergence of resistance requires uninterrupted drug supplies and is vulnerable to human inconstancy • Improving antimicrobial use in community, healthcare, and agriculture settings, combined with other strategies, is imperative Weber JT, Courvalin P. Emerg Infect Dis. 2005; 11: 791– 3 16 Oct 2006
Drug development, not so much • • • Lack of new drug classes • difficulties in discovery of new compounds • market forces • better markets for other disease treatments in industrialized nations • lower profits in nonindustrialized countries No novel class of antibacterial drug was approved for use in the United States between 1968 and 2000 Most of the new drugs approved since 1968 have been chemical modifications of existing drugs Two new drug classes have been approved by the U. S. Food and Drug Administration since 2000 Several major pharmaceutical companies have withdrawn from antimicrobial research and development 16 Oct 2006
16 Oct 2006
The Questions • • What is the evidence that physicians prescribe antimicrobial drugs too often? What are CDC and its partners doing about over prescribing? What is the evidence that appropriate use education, campaigns and policy interventions have an impact on prescribing? What are currently emerging pathogens that may be promoted by overuse of antimicrobials? • Community-associated MRSA • Streptococcus pneumoniae • Community Clostridium difficile Are there other compelling reasons to reduce antimicrobial prescribing? Are physicians and other prescribers the only ones to blame? What else can be done to improve antimicrobial prescribing? Antimicrobial Resistance and Primary Care Research 16 Oct 2006
• What is the evidence that physicians prescribe antimicrobial drugs too often? 16 Oct 2006
Appropriate Antibiotic Use • Only prescribing antibiotic therapy when beneficial • Using an appropriate (targeted) agent • Using the appropriate dose and duration 16 Oct 2006
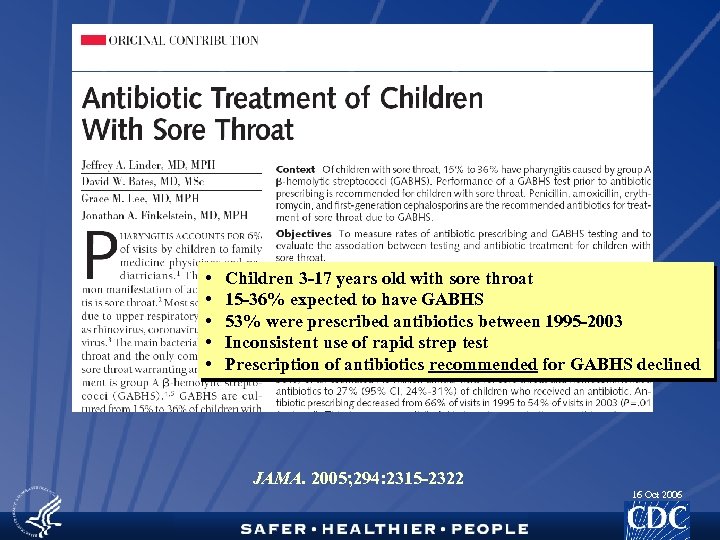
• • • Children 3 -17 years old with sore throat 15 -36% expected to have GABHS 53% were prescribed antibiotics between 1995 -2003 Inconsistent use of rapid strep test Prescription of antibiotics recommended for GABHS declined JAMA. 2005; 294: 2315 -2322 16 Oct 2006
HEDIS: Antibiotic Treatment for Adults with Acute Bronchitis • Assesses if antibiotics were inappropriately prescribed for otherwise healthy adults with acute bronchitis. • A lower rate represents better performance. • First year analysis • Commercial plans: inappropriate antibiotic prescribing for acute bronchitis with an average rate of 66% • Medicaid plans: average rate of 70% • Complements existing HEDIS measures targeting children: • Appropriate Treatment of Children with URI - Inverted rate of inappropriate prescribing for URI • Appropriate Testing for Children with Pharyngitis - Rate of strep testing for children with pharyngitis who had an antibiotic prescribed 16 Oct 2006
• • • Many northern European countries have adopted delayed prescribing for AOM given evidence 48 -72 hour delay, fill Rx if no improvement or worsening symptoms Wait-and-see-prescription: 38% used antibiotics Standard prescription: 87% used antibiotics Children considered toxic were excluded Standard prescription reduced duration of otalgia approximately 10 hours (CI 1. 7 -19 hours) JAMA. 2006; 296: 1235 -1241 16 Oct 2006
• What is CDC and its partners doing about over prescribing? 16 Oct 2006
16 Oct 2006
National Campaign to Promote Appropriate Antibiotic Use • Objectives: • Decrease unnecessary antimicrobial use • Reduce the spread of resistance • Approach: • Establishing partnerships • Developing materials to educate physicians & the public • Developing and implementing interventions • Assessing impact on antibiotic use, resistance, and physician/patient satisfaction • Serving as a resource to groups undertaking campaigns 16 Oct 2006
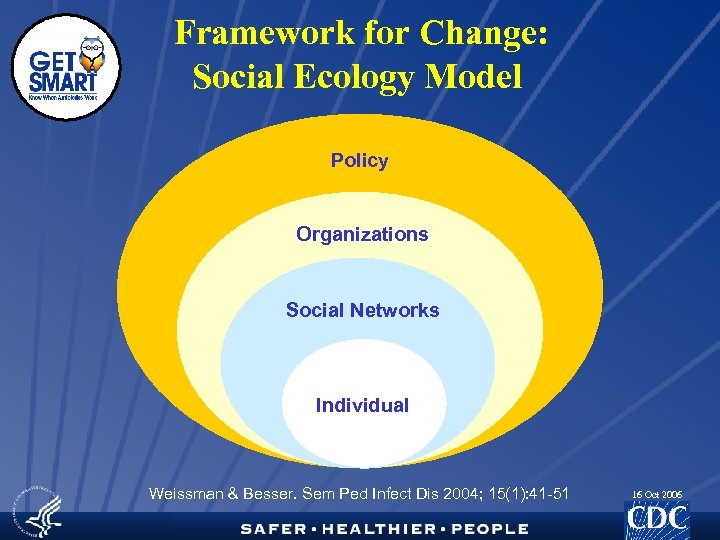
Framework for Change: Social Ecology Model Policy Organizations Social Networks Individual Weissman & Besser. Sem Ped Infect Dis 2004; 15(1): 41 -51 16 Oct 2006
Get Smart activities • Intervening with providers • Medical school curriculum • Residency education • Otitis media curriculum • Pharmacy initiative 16 Oct 2006
Get Smart activities • Intervening with the public • Marketing • Paid advertising • Educational materials • Multidimensional local interventions 16 Oct 2006
16 Oct 2006
• What is the evidence that appropriate use education, campaigns and policy interventions have an impact on prescribing? 16 Oct 2006
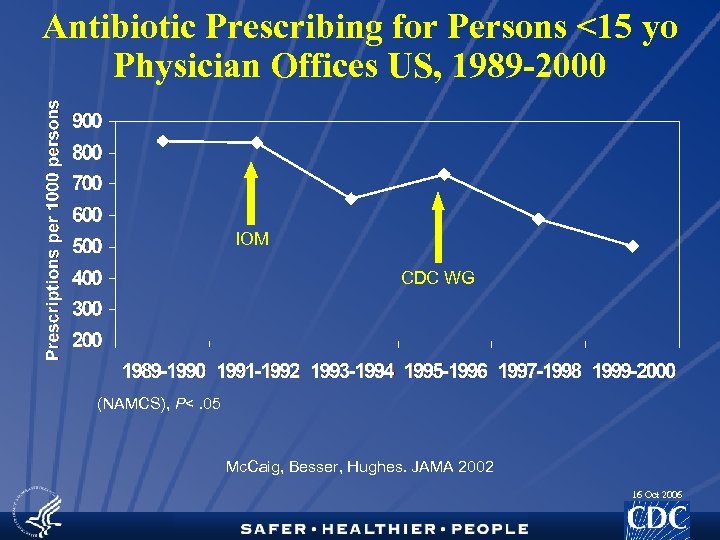
Antibiotic Prescribing for Persons <15 yo Physician Offices US, 1989 -2000 IOM CDC WG (NAMCS), P<. 05 Mc. Caig, Besser, Hughes. JAMA 2002 16 Oct 2006
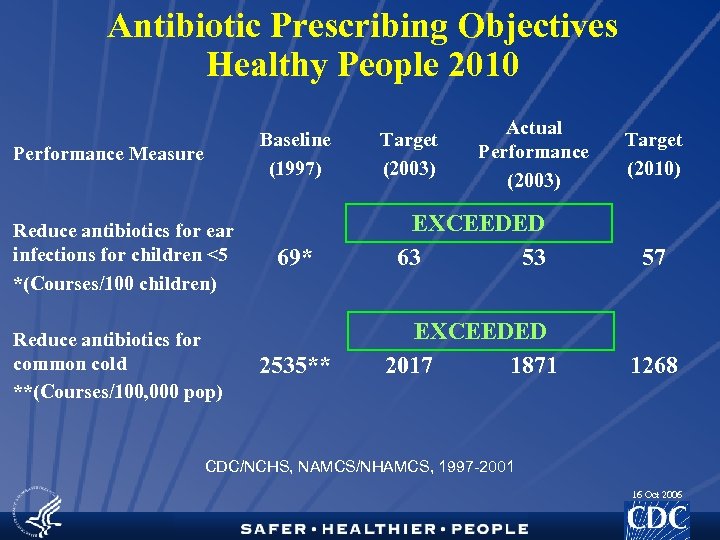
Antibiotic Prescribing Objectives Healthy People 2010 Baseline (1997) Performance Measure Reduce antibiotics for ear infections for children <5 *(Courses/100 children) Reduce antibiotics for common cold **(Courses/100, 000 pop) Target (2003) Actual Performance (2003) Target (2010) 69* EXCEEDED 63 53 57 2535** EXCEEDED 2017 1871 1268 CDC/NCHS, NAMCS/NHAMCS, 1997 -2001 16 Oct 2006
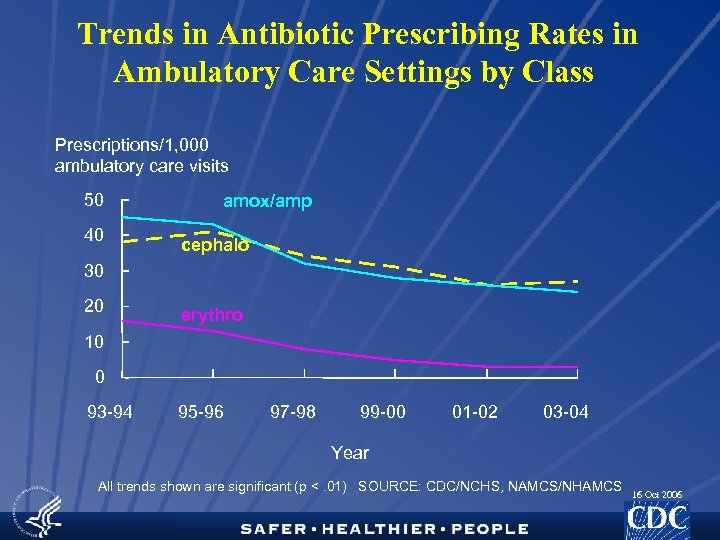
Trends in Antibiotic Prescribing Rates in Ambulatory Care Settings by Class Prescriptions/1, 000 ambulatory care visits 50 40 amox/amp cephalo 30 20 erythro 10 0 93 -94 95 -96 97 -98 99 -00 01 -02 03 -04 Year All trends shown are significant (p <. 01) SOURCE: CDC/NCHS, NAMCS/NHAMCS 16 Oct 2006
Summary • Public health campaigns can modify antimicrobial prescribing by addressing the factors promoting inappropriate prescribing in the community • Get Smart campaign • represents an effective example of a public health program that has been built on strong epidemiologic and behavioral science • represents an effective collaboration within CDC and with external partners • demonstrates how limited resources can be used to leverage significant support through effective partnerships. 16 Oct 2006
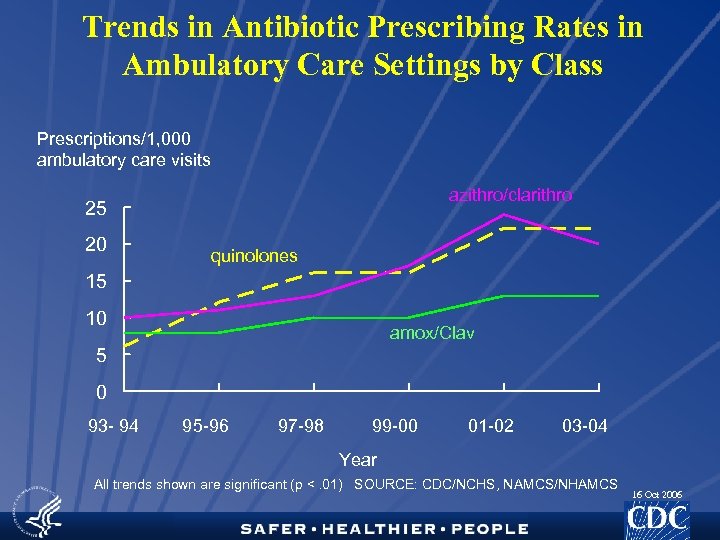
Trends in Antibiotic Prescribing Rates in Ambulatory Care Settings by Class Prescriptions/1, 000 ambulatory care visits azithro/clarithro 25 20 quinolones 15 10 amox/Clav 5 0 93 - 94 95 -96 97 -98 99 -00 01 -02 03 -04 Year All trends shown are significant (p <. 01) SOURCE: CDC/NCHS, NAMCS/NHAMCS 16 Oct 2006
• What are currently emerging pathogens that may be promoted by overuse of antimicrobials? 16 Oct 2006
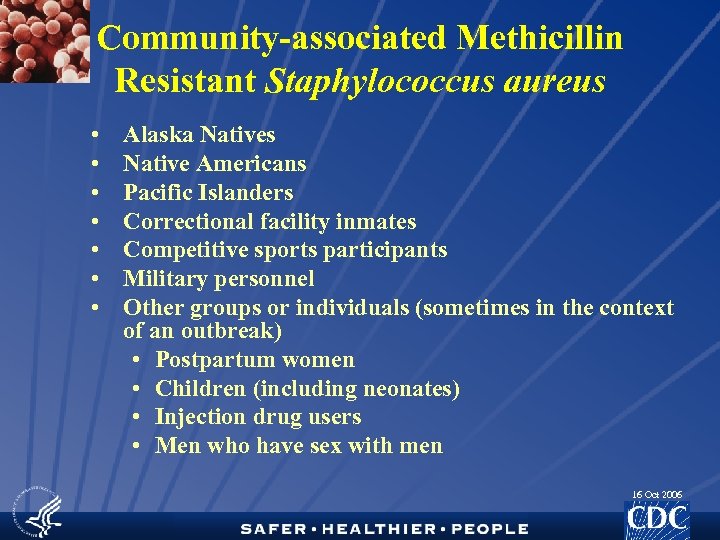
Community-associated Methicillin Resistant Staphylococcus aureus • • Alaska Natives Native Americans Pacific Islanders Correctional facility inmates Competitive sports participants Military personnel Other groups or individuals (sometimes in the context of an outbreak) • Postpartum women • Children (including neonates) • Injection drug users • Men who have sex with men 16 Oct 2006
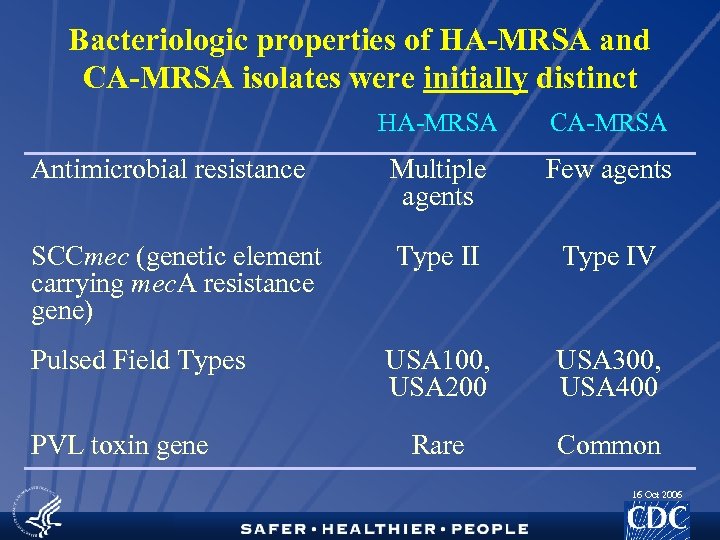
Bacteriologic properties of HA-MRSA and CA-MRSA isolates were initially distinct HA-MRSA CA-MRSA Antimicrobial resistance Multiple agents Few agents SCCmec (genetic element carrying mec. A resistance gene) Type II Type IV USA 100, USA 200 USA 300, USA 400 Rare Common Pulsed Field Types PVL toxin gene 16 Oct 2006
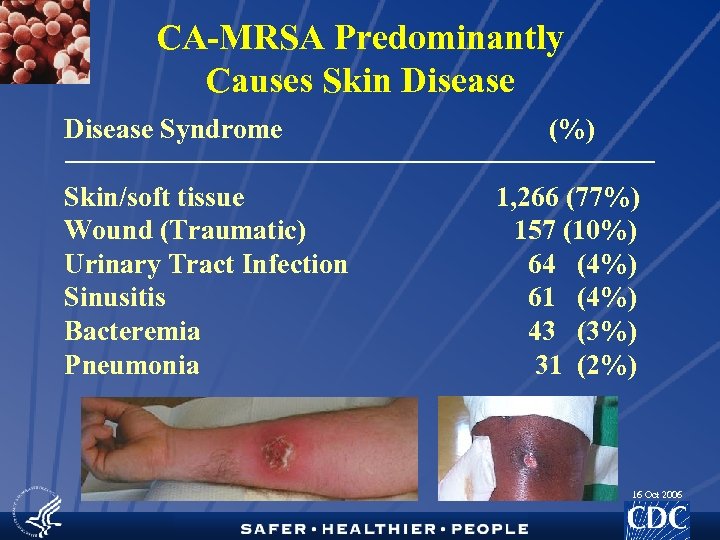
CA-MRSA Predominantly Causes Skin Disease Syndrome Skin/soft tissue Wound (Traumatic) Urinary Tract Infection Sinusitis Bacteremia Pneumonia (%) 1, 266 (77%) 157 (10%) 64 (4%) 61 (4%) 43 (3%) 31 (2%) 16 Oct 2006
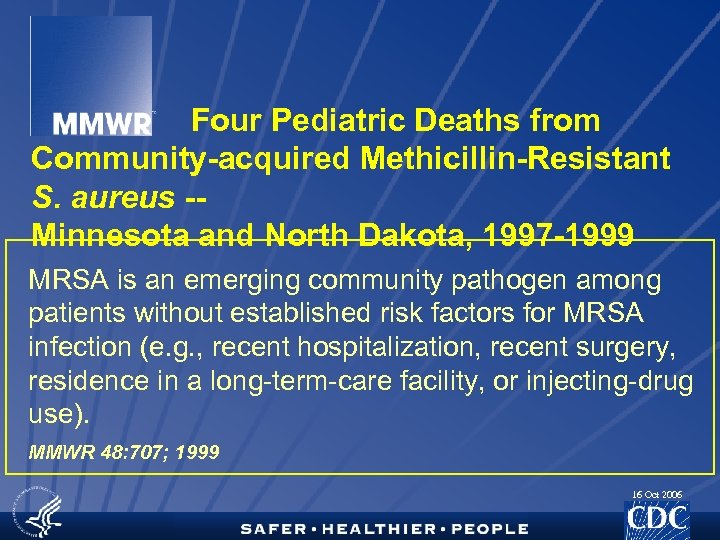
Four Pediatric Deaths from Community-acquired Methicillin-Resistant S. aureus -Minnesota and North Dakota, 1997 -1999 MRSA is an emerging community pathogen among patients without established risk factors for MRSA infection (e. g. , recent hospitalization, recent surgery, residence in a long-term-care facility, or injecting-drug use). MMWR 48: 707; 1999 16 Oct 2006
Severe and Invasive Manifestations of CA-MRSA Infection • Necrotizing pneumonia and empyema • Francis JS, CID, 2005; 40(1): 100 -7 • Sepsis syndrome • Gonzalez BE, Pediatrics, 2005; 115(3): 642 -8 • Disseminated infections with septic emboli • Gonzalez BE, CID, 2005; 41(5): 583 -90 • Musculoskeletal infections (pyomyositis, osteomyelitis) • Martinez-Aguilar G, PIDJ, 2004; 23(8): 701 -6 • Necrotizing fasciitis • Miller LG, NEJM, 2005; 352(14): 1445 -53 • Purpura fulminans • Adem PV, NEJM; 2005; 353(12): 1245 -51 • Toxic shock-like syndrome 16 Oct 2006
Community-associated Methicillin Resistant Staphylococcus aureus • 2003 -2004 influenza season • 17 persons with influenza were reported with severe staphylococcal infection, and 15 of the infections were due to MRSA • All MRSA tested had a community-associated lineage • Among the 5 persons who died, 4 had infections due to MRSA 16 Oct 2006
The 5 C’s of CA-MRSA • Contact • Crowding • Contaminated items • Compromised skin integrity • Lack of Cleanliness 16 Oct 2006
CA-MRSA and prior Antimicrobial Use • • • Religious community located in rural upstate New York 1 • Multivariate analysis • Only sauna use and antimicrobial use within 12 months before infection (OR 11. 7, 95% CI 2. 9– 47. 6) remained significant risk factors CA-MRSA colonization among soldiers 2 • Multivariate analysis • Antibiotic use within the previous 6 months Rural Alaska • Year prior to outbreak • Case patients received a median of 4 antibiotic courses, compared with 2 courses for control subjects • Odds of a skin infection during the outbreak increased with the number of preoutbreak antibiotic courses 1. Coronado, et al. Epidemiol Infect. 2006 Jul 26 2. Ellis, et al. Clinical Infectious Diseases 2004; 39: 971– 9 3. Baggett, et al. Journal of Infectious Diseases 2004; 189: 1565– 73 16 Oct 2006
According to the team pharmacy log for the 2002 football season, maintained at the training facility, a team player on average received 2. 6 antimicrobialdrug prescriptions per year. This rate was greater than 10 times the rate among persons of the same age and sex in the general population…. In their survey responses, approximately 60 percent of players indicated they had taken or received antimicrobials during the 2003 football season. 16 Oct 2006
Risk Factors For CA-MRSA Infections • • 2000 -2003: CA-MRSA cases identified by MN Department of Health at 3 sentinel surveillance hospitals; 1: 1 matched (age group, culture site) with CA methicillin-sensitive S. aureus (MSSA) cases identified by the same hospitals. CA-MRSA cases were more likely to have: • Received an antibiotic in the 0 -6 or 1 -6 months prior to infection. Only risk factor that remained significant after controlling for SE variables. • Shared towels • Lived away from home for ≥ 2 weeks in the year prior to infection • Had a personal history of boils • Household member with a history of boils • Socioeconomic variables: non-white race, household crowding, lower income and less education • Recreational/athletic activities, bathing habits, or exposure to healthcare were not significant. IDSA 2006 Como-Sabetti, et al. 16 Oct 2006
The 5 6? C’s of CA-MRSA • Contact • Crowding • Contaminated items • Compromised skin integrity • Lack of Cleanliness • Antibiotic Capsules 16 Oct 2006
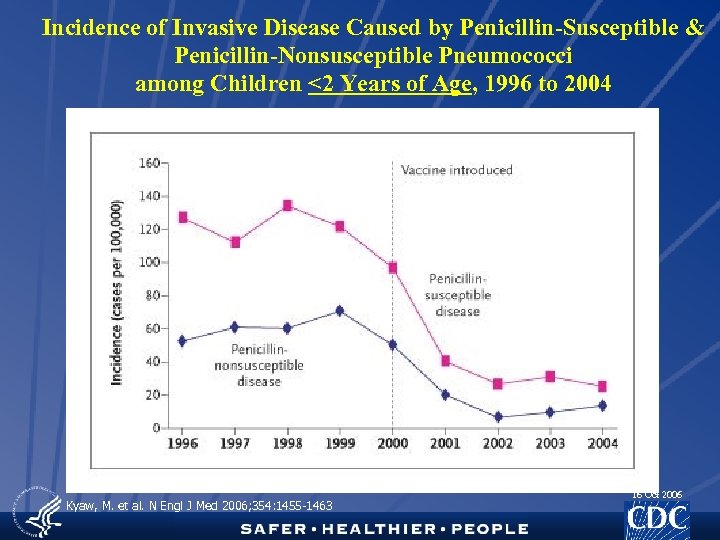
Incidence of Invasive Disease Caused by Penicillin-Susceptible & Penicillin-Nonsusceptible Pneumococci among Children <2 Years of Age, 1996 to 2004 Kyaw, M. et al. N Engl J Med 2006; 354: 1455 -1463 16 Oct 2006
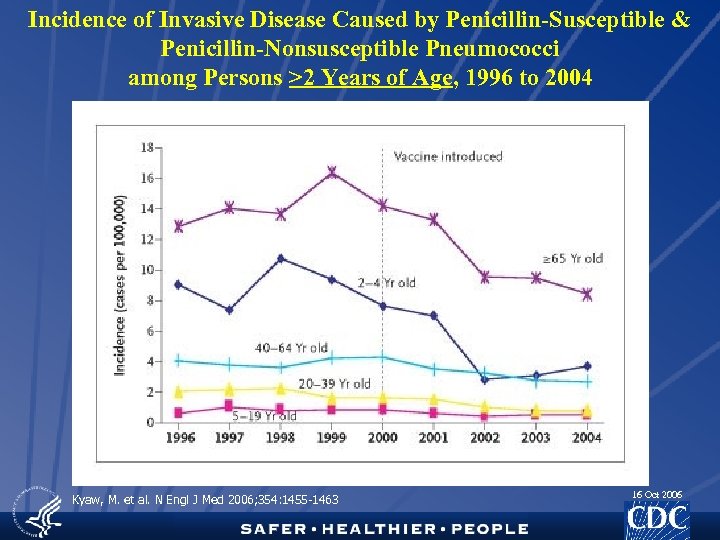
Incidence of Invasive Disease Caused by Penicillin-Susceptible & Penicillin-Nonsusceptible Pneumococci among Persons >2 Years of Age, 1996 to 2004 Kyaw, M. et al. N Engl J Med 2006; 354: 1455 -1463 16 Oct 2006
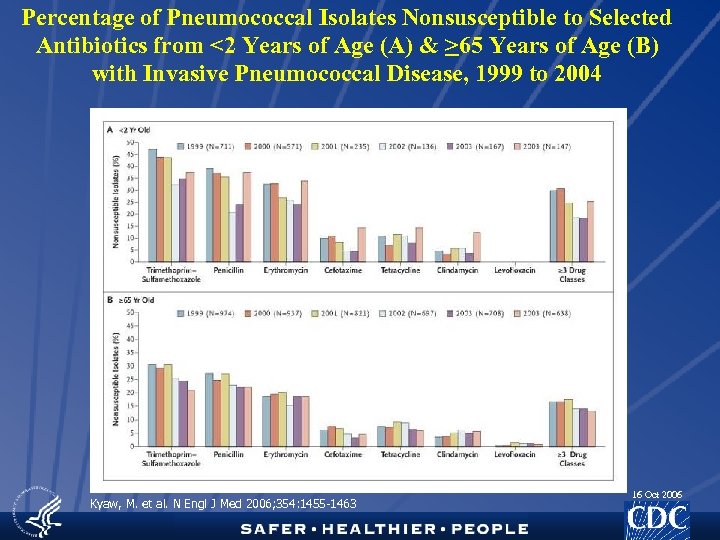
Percentage of Pneumococcal Isolates Nonsusceptible to Selected Antibiotics from <2 Years of Age (A) & >65 Years of Age (B) with Invasive Pneumococcal Disease, 1999 to 2004 Kyaw, M. et al. N Engl J Med 2006; 354: 1455 -1463 16 Oct 2006
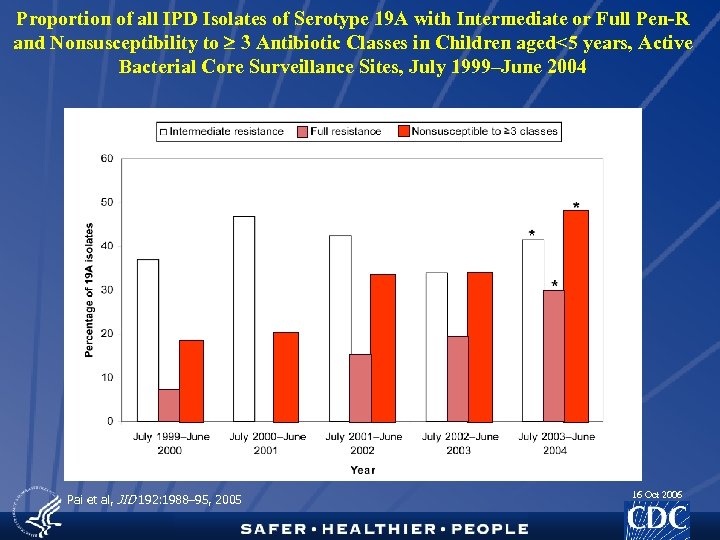
Proportion of all IPD Isolates of Serotype 19 A with Intermediate or Full Pen-R and Nonsusceptibility to 3 Antibiotic Classes in Children aged<5 years, Active Bacterial Core Surveillance Sites, July 1999–June 2004 Pai et al, JID 192: 1988– 95, 2005 16 Oct 2006
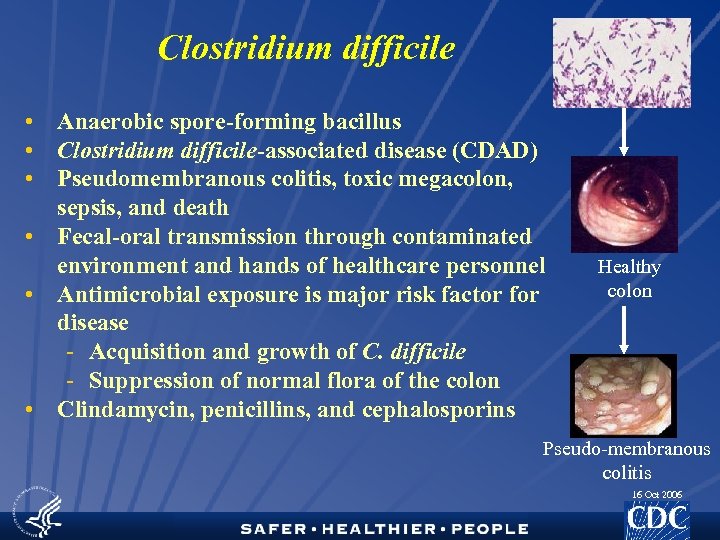
Clostridium difficile • Anaerobic spore-forming bacillus • Clostridium difficile-associated disease (CDAD) • Pseudomembranous colitis, toxic megacolon, sepsis, and death • Fecal-oral transmission through contaminated environment and hands of healthcare personnel • Antimicrobial exposure is major risk factor for disease - Acquisition and growth of C. difficile - Suppression of normal flora of the colon • Clindamycin, penicillins, and cephalosporins Healthy colon Pseudo-membranous colitis 16 Oct 2006
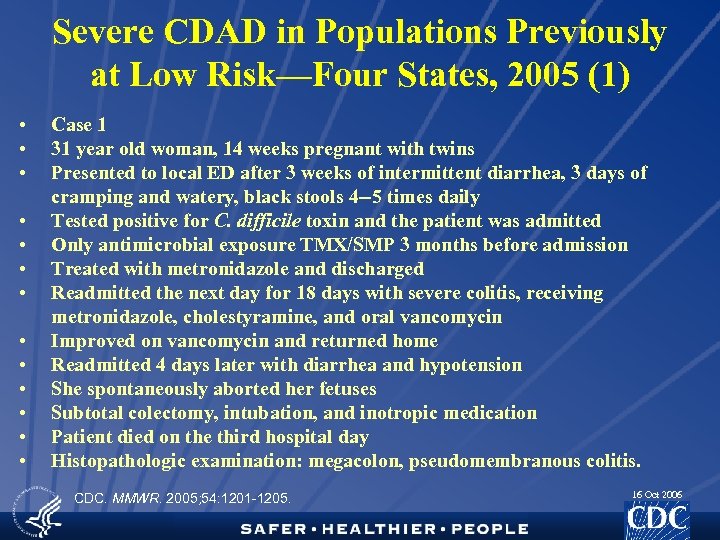
Severe CDAD in Populations Previously at Low Risk—Four States, 2005 (1) • • • • Case 1 31 year old woman, 14 weeks pregnant with twins Presented to local ED after 3 weeks of intermittent diarrhea, 3 days of cramping and watery, black stools 4 --5 times daily Tested positive for C. difficile toxin and the patient was admitted Only antimicrobial exposure TMX/SMP 3 months before admission Treated with metronidazole and discharged Readmitted the next day for 18 days with severe colitis, receiving metronidazole, cholestyramine, and oral vancomycin Improved on vancomycin and returned home Readmitted 4 days later with diarrhea and hypotension She spontaneously aborted her fetuses Subtotal colectomy, intubation, and inotropic medication Patient died on the third hospital day Histopathologic examination: megacolon, pseudomembranous colitis. CDC. MMWR. 2005; 54: 1201 -1205. 16 Oct 2006
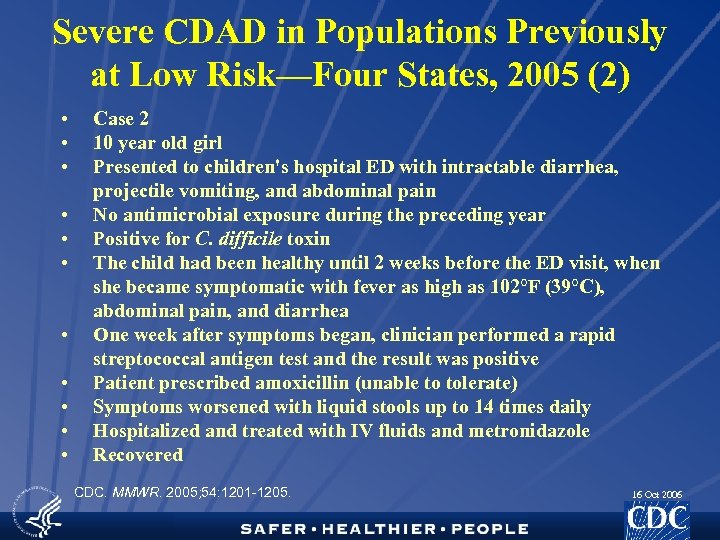
Severe CDAD in Populations Previously at Low Risk—Four States, 2005 (2) • • • Case 2 10 year old girl Presented to children's hospital ED with intractable diarrhea, projectile vomiting, and abdominal pain No antimicrobial exposure during the preceding year Positive for C. difficile toxin The child had been healthy until 2 weeks before the ED visit, when she became symptomatic with fever as high as 102°F (39°C), abdominal pain, and diarrhea One week after symptoms began, clinician performed a rapid streptococcal antigen test and the result was positive Patient prescribed amoxicillin (unable to tolerate) Symptoms worsened with liquid stools up to 14 times daily Hospitalized and treated with IV fluids and metronidazole Recovered CDC. MMWR. 2005; 54: 1201 -1205. 16 Oct 2006
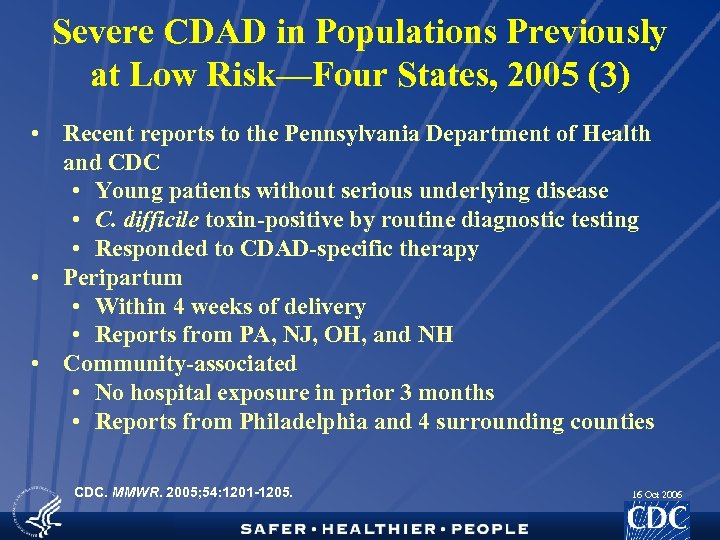
Severe CDAD in Populations Previously at Low Risk—Four States, 2005 (3) • Recent reports to the Pennsylvania Department of Health and CDC • Young patients without serious underlying disease • C. difficile toxin-positive by routine diagnostic testing • Responded to CDAD-specific therapy • Peripartum • Within 4 weeks of delivery • Reports from PA, NJ, OH, and NH • Community-associated • No hospital exposure in prior 3 months • Reports from Philadelphia and 4 surrounding counties CDC. MMWR. 2005; 54: 1201 -1205. 16 Oct 2006
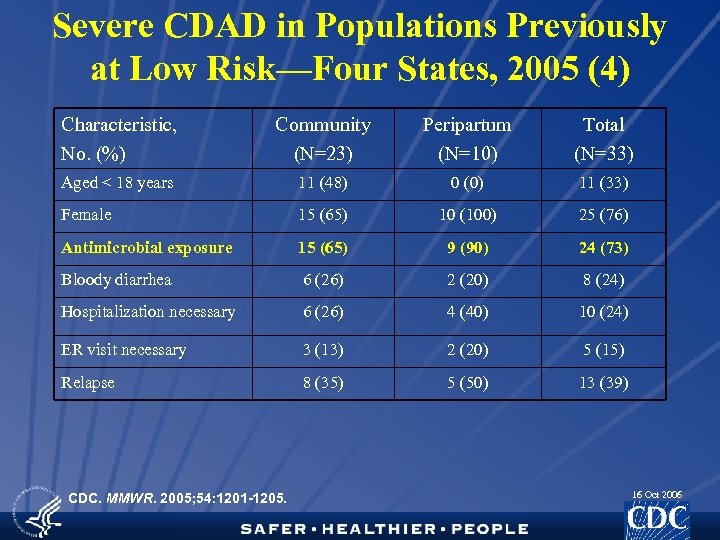
Severe CDAD in Populations Previously at Low Risk—Four States, 2005 (4) Characteristic, No. (%) Community (N=23) Peripartum (N=10) Total (N=33) Aged < 18 years 11 (48) 0 (0) 11 (33) Female 15 (65) 10 (100) 25 (76) Antimicrobial exposure 15 (65) 9 (90) 24 (73) Bloody diarrhea 6 (26) 2 (20) 8 (24) Hospitalization necessary 6 (26) 4 (40) 10 (24) ER visit necessary 3 (13) 2 (20) 5 (15) Relapse 8 (35) 5 (50) 13 (39) CDC. MMWR. 2005; 54: 1201 -1205. 16 Oct 2006
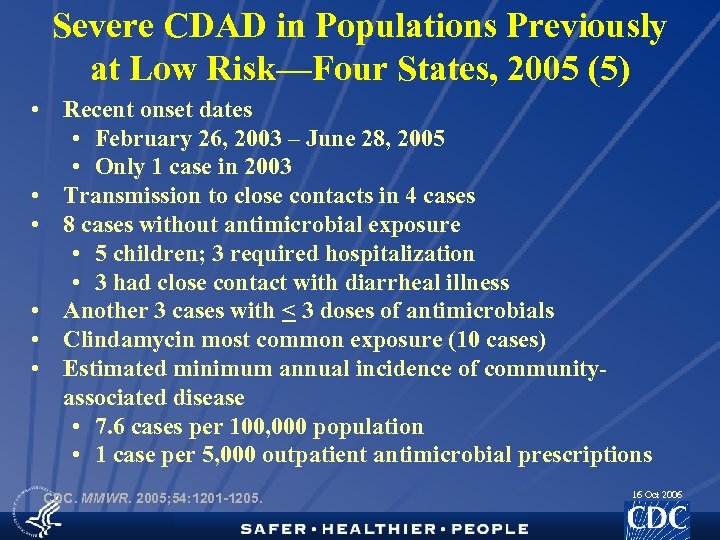
Severe CDAD in Populations Previously at Low Risk—Four States, 2005 (5) • Recent onset dates • February 26, 2003 – June 28, 2005 • Only 1 case in 2003 • Transmission to close contacts in 4 cases • 8 cases without antimicrobial exposure • 5 children; 3 required hospitalization • 3 had close contact with diarrheal illness • Another 3 cases with < 3 doses of antimicrobials • Clindamycin most common exposure (10 cases) • Estimated minimum annual incidence of communityassociated disease • 7. 6 cases per 100, 000 population • 1 case per 5, 000 outpatient antimicrobial prescriptions CDC. MMWR. 2005; 54: 1201 -1205. 16 Oct 2006
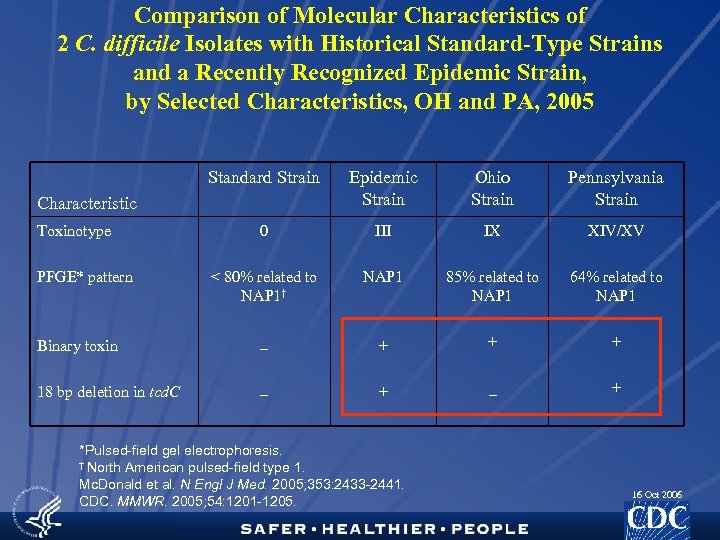
Comparison of Molecular Characteristics of 2 C. difficile Isolates with Historical Standard-Type Strains and a Recently Recognized Epidemic Strain, by Selected Characteristics, OH and PA, 2005 Standard Strain Epidemic Strain Ohio Strain Pennsylvania Strain 0 III IX XIV/XV < 80% related to NAP 1† NAP 1 85% related to NAP 1 64% related to NAP 1 Binary toxin _ + + + 18 bp deletion in tcd. C _ + Characteristic Toxinotype PFGE* pattern *Pulsed-field gel electrophoresis. † North American pulsed-field type 1. Mc. Donald et al. N Engl J Med. 2005; 353: 2433 -2441. CDC. MMWR. 2005; 54: 1201 -1205. 16 Oct 2006
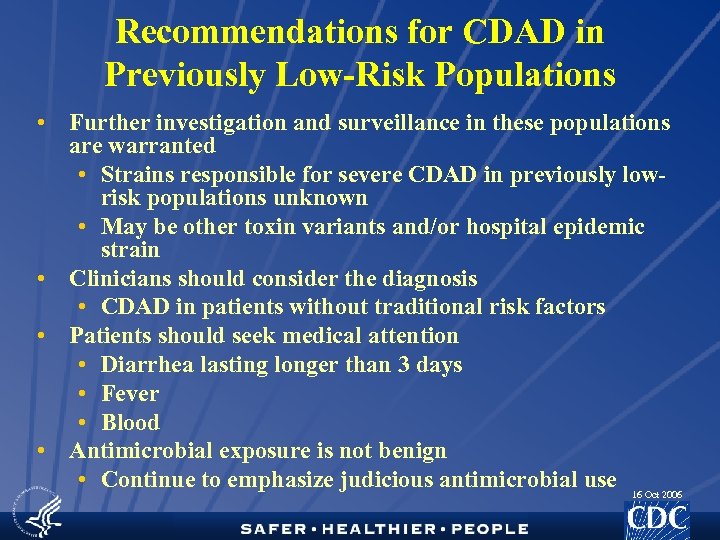
Recommendations for CDAD in Previously Low-Risk Populations • Further investigation and surveillance in these populations are warranted • Strains responsible for severe CDAD in previously lowrisk populations unknown • May be other toxin variants and/or hospital epidemic strain • Clinicians should consider the diagnosis • CDAD in patients without traditional risk factors • Patients should seek medical attention • Diarrhea lasting longer than 3 days • Fever • Blood • Antimicrobial exposure is not benign • Continue to emphasize judicious antimicrobial use 16 Oct 2006
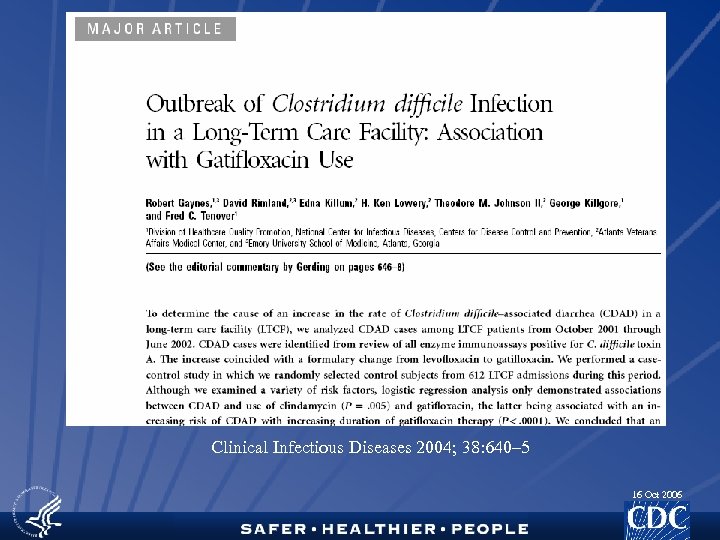
Clinical Infectious Diseases 2004; 38: 640– 5 16 Oct 2006
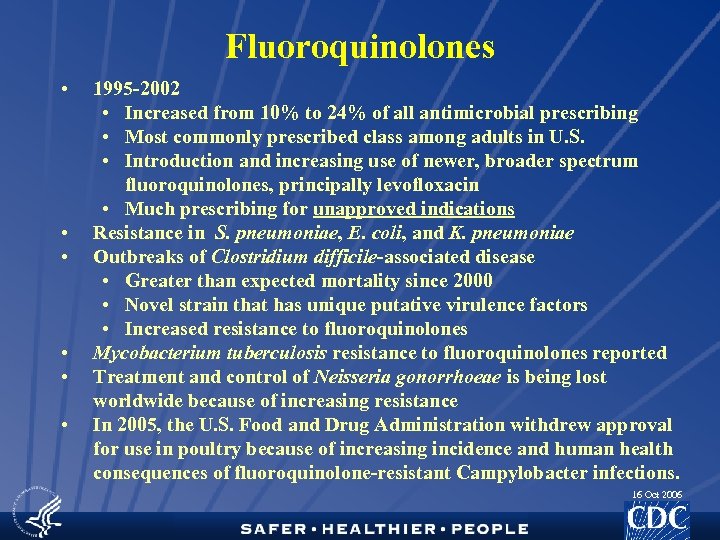
Fluoroquinolones • • • 1995 -2002 • Increased from 10% to 24% of all antimicrobial prescribing • Most commonly prescribed class among adults in U. S. • Introduction and increasing use of newer, broader spectrum fluoroquinolones, principally levofloxacin • Much prescribing for unapproved indications Resistance in S. pneumoniae, E. coli, and K. pneumoniae Outbreaks of Clostridium difficile-associated disease • Greater than expected mortality since 2000 • Novel strain that has unique putative virulence factors • Increased resistance to fluoroquinolones Mycobacterium tuberculosis resistance to fluoroquinolones reported Treatment and control of Neisseria gonorrhoeae is being lost worldwide because of increasing resistance In 2005, the U. S. Food and Drug Administration withdrew approval for use in poultry because of increasing incidence and human health consequences of fluoroquinolone-resistant Campylobacter infections. 16 Oct 2006
• Are there other compelling reasons to reduce antimicrobial prescribing? 16 Oct 2006
16 Oct 2006
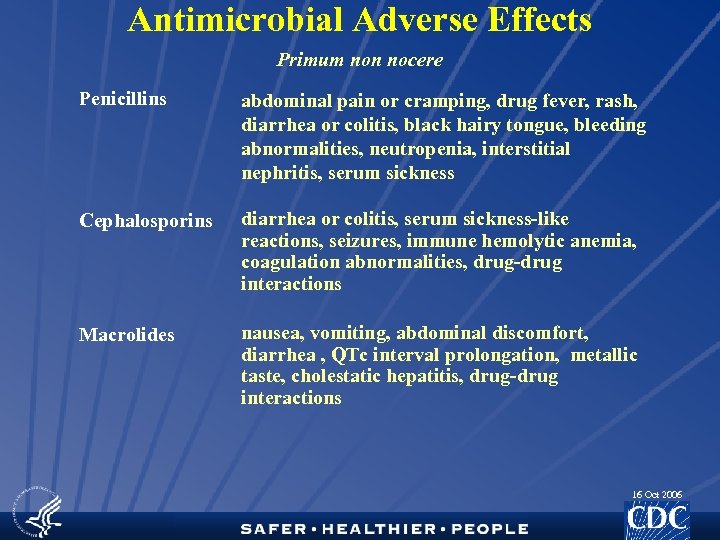
Antimicrobial Adverse Effects Primum non nocere Penicillins abdominal pain or cramping, drug fever, rash, diarrhea or colitis, black hairy tongue, bleeding abnormalities, neutropenia, interstitial nephritis, serum sickness Cephalosporins diarrhea or colitis, serum sickness-like reactions, seizures, immune hemolytic anemia, coagulation abnormalities, drug-drug interactions Macrolides nausea, vomiting, abdominal discomfort, diarrhea , QTc interval prolongation, metallic taste, cholestatic hepatitis, drug-drug interactions 16 Oct 2006
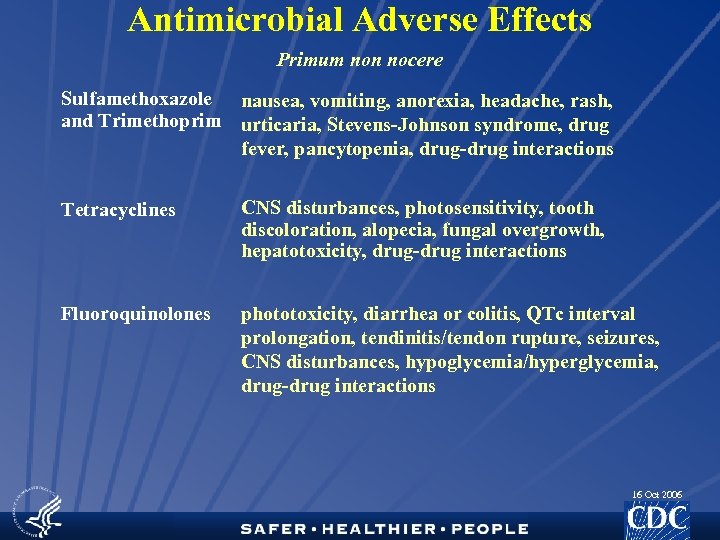
Antimicrobial Adverse Effects Primum non nocere Sulfamethoxazole nausea, vomiting, anorexia, headache, rash, and Trimethoprim urticaria, Stevens-Johnson syndrome, drug fever, pancytopenia, drug-drug interactions Tetracyclines CNS disturbances, photosensitivity, tooth discoloration, alopecia, fungal overgrowth, hepatotoxicity, drug-drug interactions Fluoroquinolones phototoxicity, diarrhea or colitis, QTc interval prolongation, tendinitis/tendon rupture, seizures, CNS disturbances, hypoglycemia/hyperglycemia, drug-drug interactions 16 Oct 2006
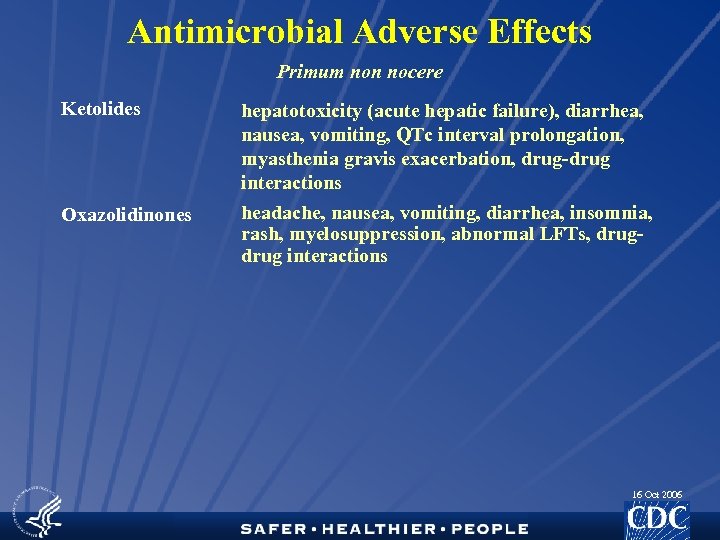
Antimicrobial Adverse Effects Primum non nocere Ketolides hepatotoxicity (acute hepatic failure), diarrhea, nausea, vomiting, QTc interval prolongation, myasthenia gravis exacerbation, drug-drug interactions Oxazolidinones headache, nausea, vomiting, diarrhea, insomnia, rash, myelosuppression, abnormal LFTs, drug interactions 16 Oct 2006
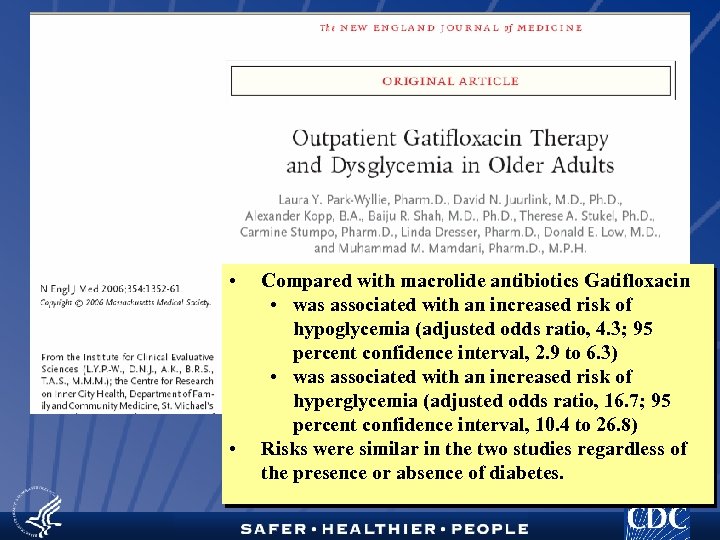
• • Compared with macrolide antibiotics Gatifloxacin • was associated with an increased risk of hypoglycemia (adjusted odds ratio, 4. 3; 95 percent confidence interval, 2. 9 to 6. 3) • was associated with an increased risk of hyperglycemia (adjusted odds ratio, 16. 7; 95 percent confidence interval, 10. 4 to 26. 8) Risks were similar in the two studies regardless of the presence or absence of diabetes. 16 Oct 2006
16 Oct 2006
In a pilot study of 10 sites, antimicrobials accounted for 16. 1% of outpatient adverse drug events requiring emergency department visits. Ann Emerg Med. 2005; 45: 197 -206 16 Oct 2006
• Generalists provided ambulatory care to 45% of women prescribed potentially teratogenic medications • 12% of prescriptions were potentially teratogenic antibiotics • Doxycycline, Tetracycline • 1. 4 million annual prescriptions 16 Oct 2006
• • • Case-control study Large, nonprofit health plan Increasing cumulative days of antibiotic use were associated with increased risk Increased risk was observed in all antibiotic classes studied and in a subanalysis having breast cancer fatality as the outcome Cannot determine whether antibiotic use is causally related to breast cancer, or whether indication for use, overall weakened immune function, or other factors are pertinent underlying exposures JAMA. 2004; 291: 827 -835 16 Oct 2006
• Are physicians and other prescribers the only ones to blame? 16 Oct 2006
Non-prescription Use of Antimicrobial Drugs • Latino Community, South Carolina • Clinics serving Latino population • 30. 6% believed antibiotics should be available without Rx • 45. 2% acquired antibiotics without Rx while outside U. S. • Reasons for using antibiotics • Flu • Cough • Ear infections • Sore throat • Colds • Diarrhea • Reasons for importing antibiotics • Avoid going to the doctor • Avoid the language barrier • Prepare for future illness Mainous, et al. EID, 11(6); 2005 16 Oct 2006
Non-prescription Use of Antimicrobial Drugs • Antibiotics without Prescription, New York City • 3 neighborhoods surveyed • Latino (majority from Dominican Republic) • Black, non-Hispanic • White, non-Hispanic • All private, independent pharmacies, grocery stores, delicatessens, bodegas (which sold medicine), and botanical or health food stores within 30 blocks of the major commercial areas surveyed • All stores in Hispanic neighborhood had antibiotics on the shelves or on request • None of the stores in the other neighborhoods had antibiotics Larson and Grullon-Figueroa, Journal of Urban Health, 81(3); 2004 16 Oct 2006
16 Oct 2006
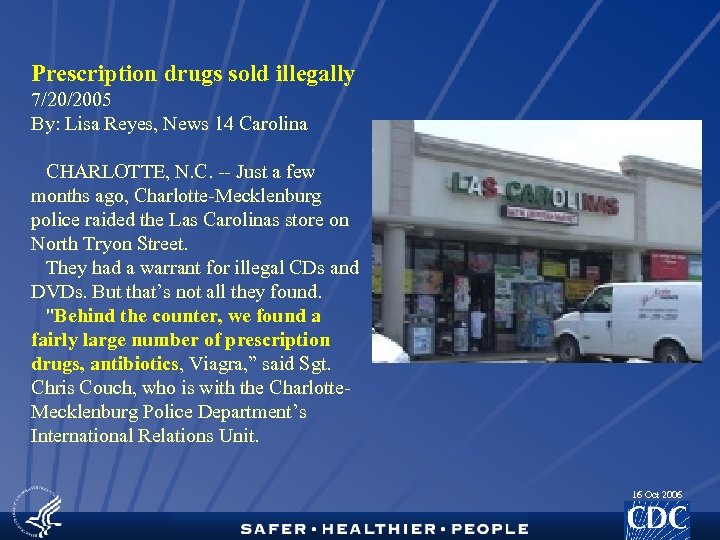
Prescription drugs sold illegally 7/20/2005 By: Lisa Reyes, News 14 Carolina CHARLOTTE, N. C. -- Just a few months ago, Charlotte-Mecklenburg police raided the Las Carolinas store on North Tryon Street. They had a warrant for illegal CDs and DVDs. But that’s not all they found. "Behind the counter, we found a fairly large number of prescription drugs, antibiotics, Viagra, ” said Sgt. Chris Couch, who is with the Charlotte. Mecklenburg Police Department’s International Relations Unit. 16 Oct 2006

16 Oct 2006
16 Oct 2006
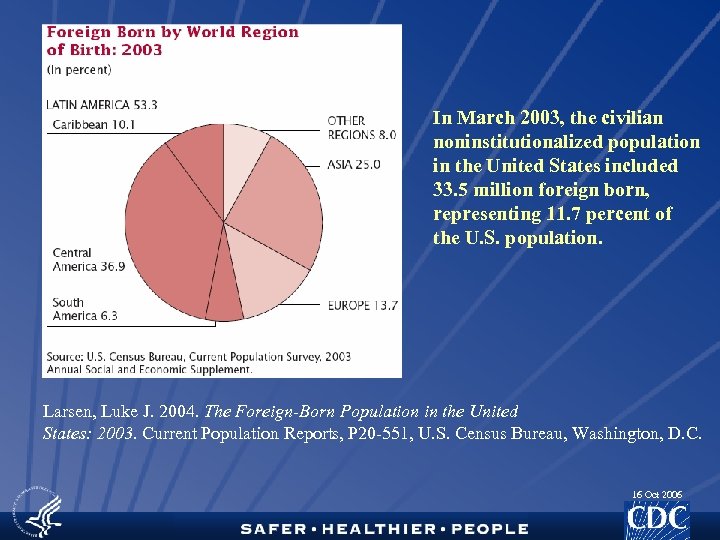
In March 2003, the civilian noninstitutionalized population in the United States included 33. 5 million foreign born, representing 11. 7 percent of the U. S. population. Larsen, Luke J. 2004. The Foreign-Born Population in the United States: 2003. Current Population Reports, P 20 -551, U. S. Census Bureau, Washington, D. C. 16 Oct 2006
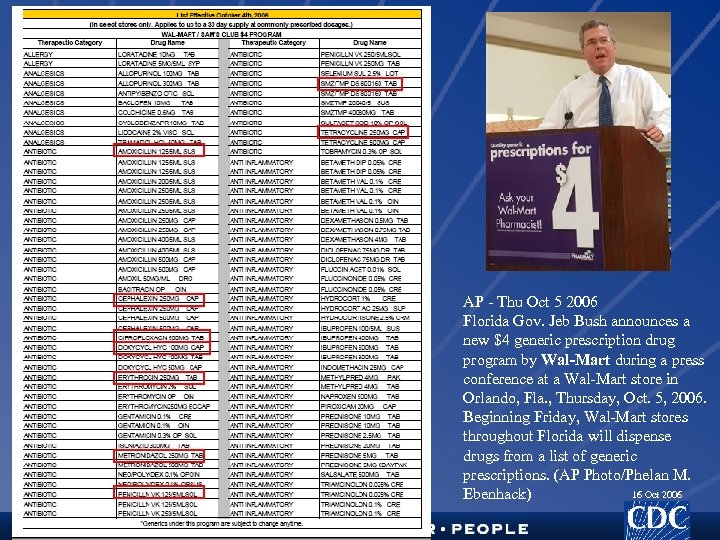
AP - Thu Oct 5 2006 Florida Gov. Jeb Bush announces a new $4 generic prescription drug program by Wal-Mart during a press conference at a Wal-Mart store in Orlando, Fla. , Thursday, Oct. 5, 2006. Beginning Friday, Wal-Mart stores throughout Florida will dispense drugs from a list of generic prescriptions. (AP Photo/Phelan M. 16 Oct 2006 Ebenhack)
The clinic tenants offer essential preventive and routine health services for a standard set of the most common health ailments that can be treated without urgent or emergency care, including allergies, ear aches, sore throat, sinus infections, upper respiratory infections, bladder infections, insect bits & stings, cholesterol screening, blood sugar testing, drug screening and routine physicals. 16 Oct 2006
• What else can be done to improve antimicrobial prescribing? 16 Oct 2006
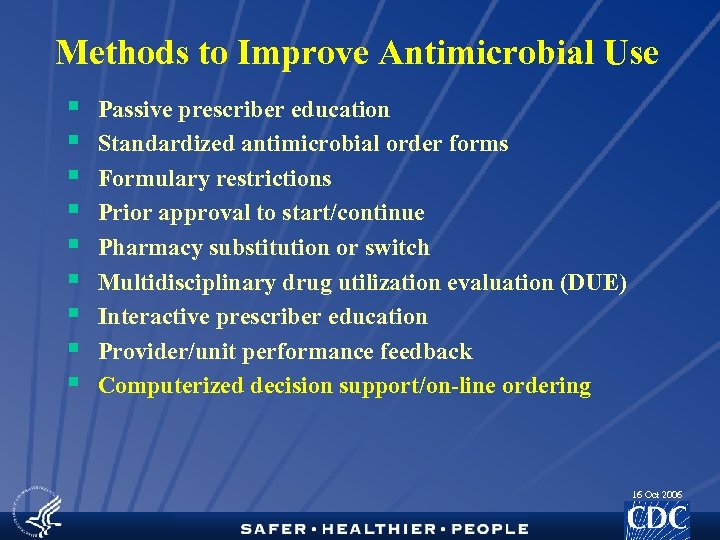
Methods to Improve Antimicrobial Use § § § § § Passive prescriber education Standardized antimicrobial order forms Formulary restrictions Prior approval to start/continue Pharmacy substitution or switch Multidisciplinary drug utilization evaluation (DUE) Interactive prescriber education Provider/unit performance feedback Computerized decision support/on-line ordering 16 Oct 2006
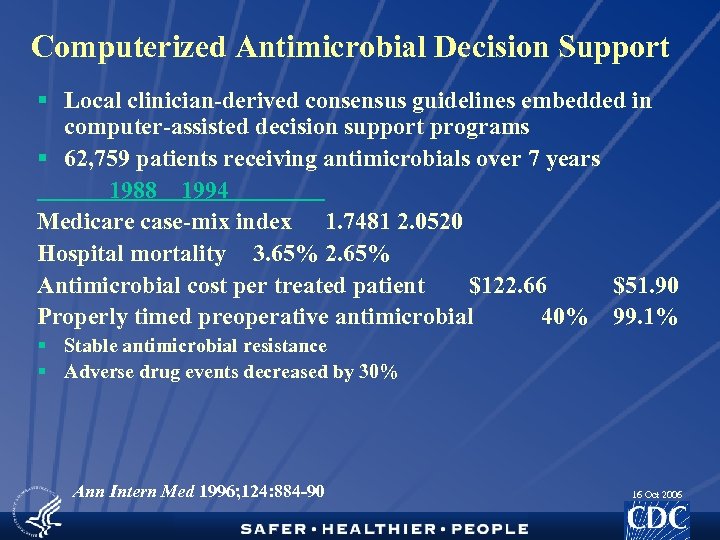
Computerized Antimicrobial Decision Support § Local clinician-derived consensus guidelines embedded in computer-assisted decision support programs § 62, 759 patients receiving antimicrobials over 7 years 1988 1994 Medicare case-mix index 1. 7481 2. 0520 Hospital mortality 3. 65% 2. 65% Antimicrobial cost per treated patient $122. 66 $51. 90 Properly timed preoperative antimicrobial 40% 99. 1% § Stable antimicrobial resistance § Adverse drug events decreased by 30% Ann Intern Med 1996; 124: 884 -90 16 Oct 2006
University of Utah, Salt Lake City, UT Health. Insight, Salt Lake City, UT Qualis Health, Boise, ID. JAMA. 2005; 294: 2305 -2314 16 Oct 2006
Clinical Decision Support and Appropriateness of Antimicrobial Prescribing A Randomized Trial – Samore, et al. • • • Cluster randomized trial involving communities divided into 2 groups Community: • Meetings • news releases • distribution of educational materials • a mailing to parents of young children • news articles about antimicrobial use CDSS: • Same community-level intervention and • Clinical decision support tool given to primary care clinicians • paper or in an electronic version accessible through a personal digital assistant, whichever they preferred • introduced through lectures, meetings, one-on-one interactions with physicians, voluntary CME session. 16 Oct 2006
Clinical Decision Support and Appropriateness of Antimicrobial Prescribing A Randomized Trial – Samore, et al. • • Prescription of antimicrobial drugs declined • by 10% in CDSS communities • by 1% in community intervention communities Prescribing of macrolides (mostly azithromycin) decreased most markedly, with CDSS communities having a 28% reduction. Reductions in prescribing for acute bronchitis and colds, for which antimicrobials are never indicated, with a greater decline in the CDSS communities than in the community intervention communities. However, antimicrobials were still prescribed for more than 24% of these diagnoses. 16 Oct 2006
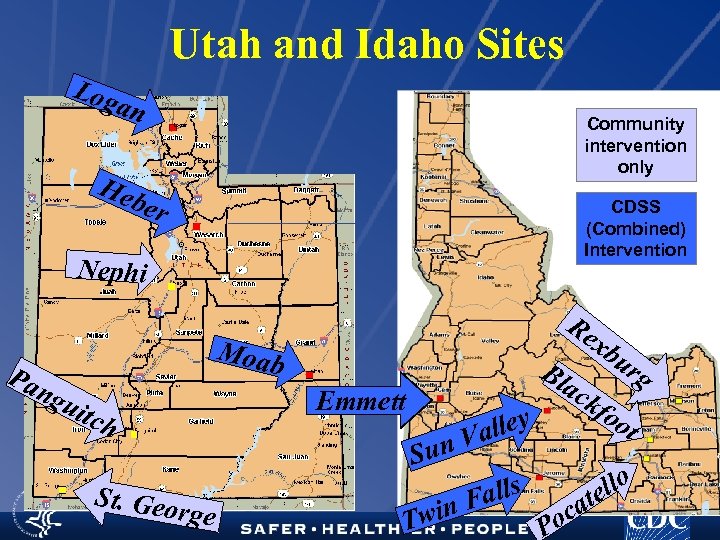
Utah and Idaho Sites Log an Community intervention only Heb er CDSS (Combined) Intervention Nephi Pa ng Re Moab Emmett uit ch St. Geo rg Sun e Twin xb ur Bl g ac kfo ot alley V alls F Po llo ate c 16 Oct 2006
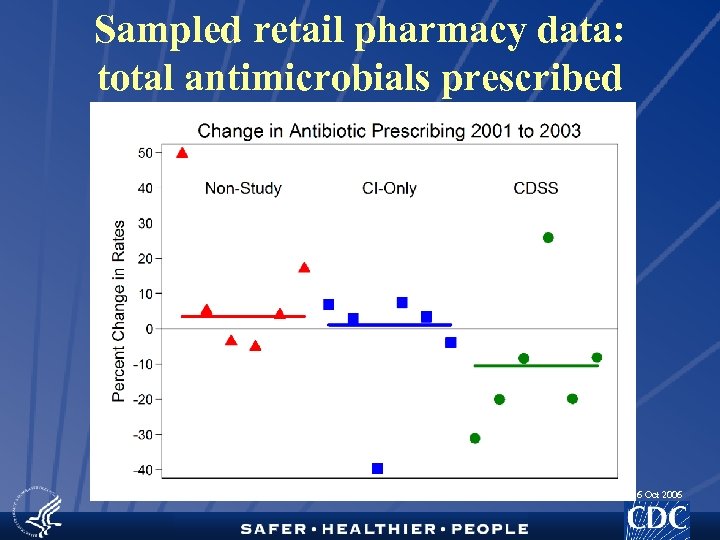
Sampled retail pharmacy data: total antimicrobials prescribed 16 Oct 2006
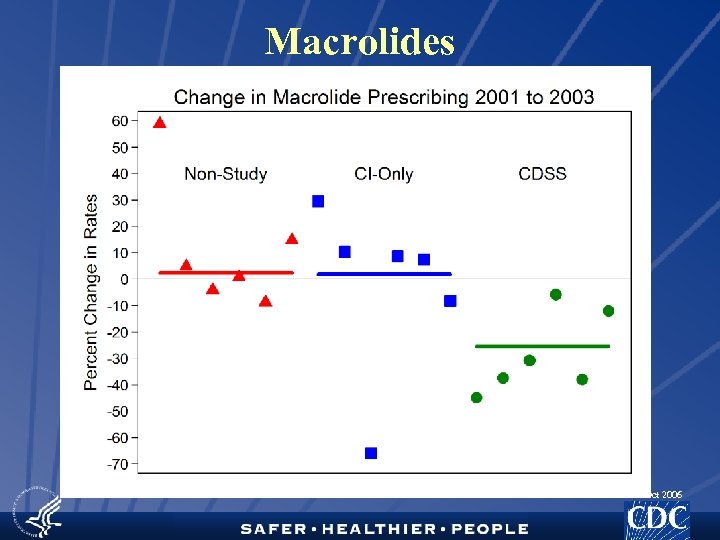
Macrolides 16 Oct 2006
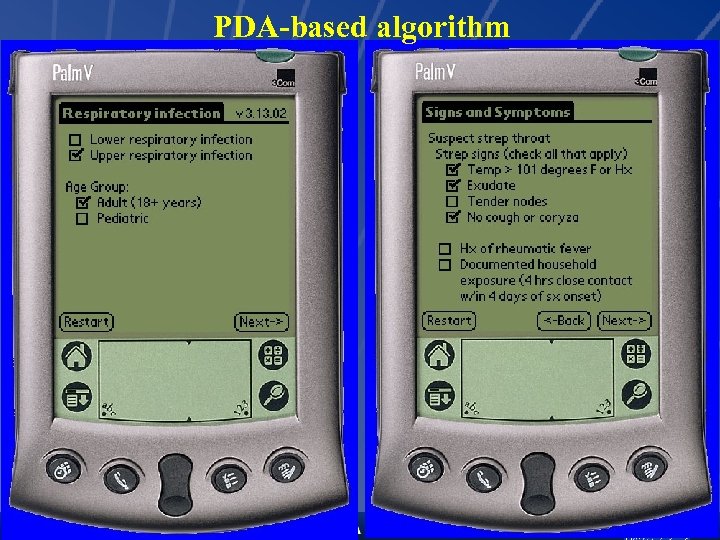
PDA-based algorithm 16 Oct 2006
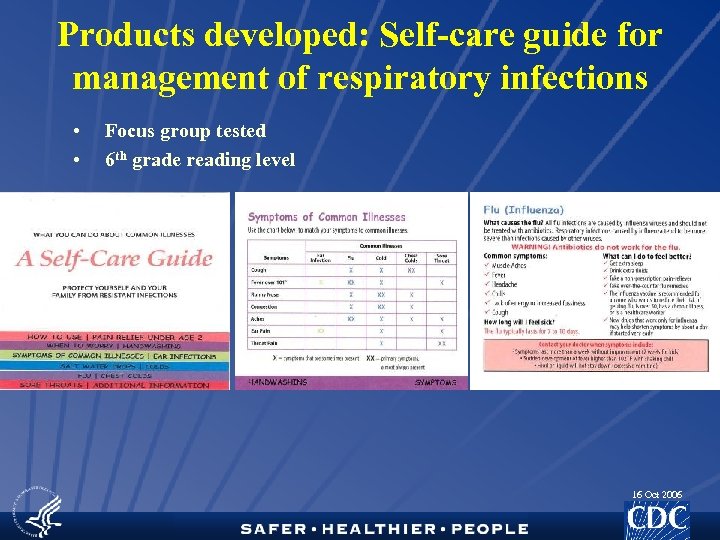
Products developed: Self-care guide for management of respiratory infections • • Focus group tested 6 th grade reading level 16 Oct 2006

Red villain, green prevention, yellow weapon, blue hero cards 16 Oct 2006
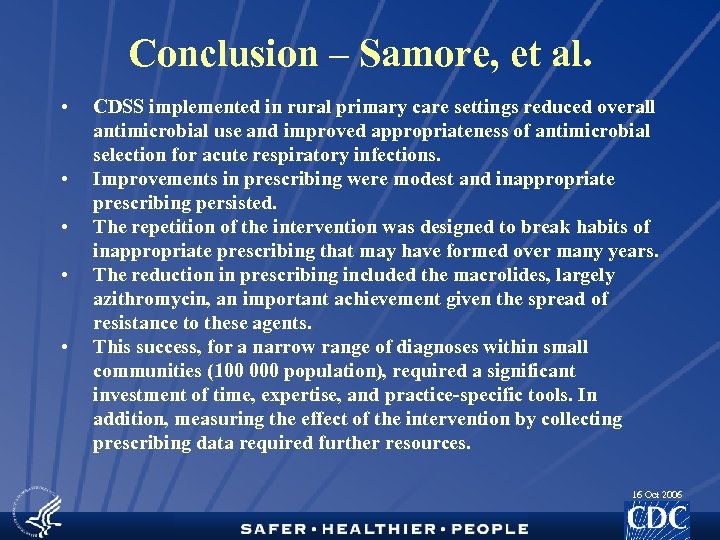
Conclusion – Samore, et al. • • • CDSS implemented in rural primary care settings reduced overall antimicrobial use and improved appropriateness of antimicrobial selection for acute respiratory infections. Improvements in prescribing were modest and inappropriate prescribing persisted. The repetition of the intervention was designed to break habits of inappropriate prescribing that may have formed over many years. The reduction in prescribing included the macrolides, largely azithromycin, an important achievement given the spread of resistance to these agents. This success, for a narrow range of diagnoses within small communities (100 000 population), required a significant investment of time, expertise, and practice-specific tools. In addition, measuring the effect of the intervention by collecting prescribing data required further resources. 16 Oct 2006
Antimicrobial Resistance and Primary Care Research • • Prevention Antimicrobial Use Treatment Epidemiology/Pharmacoepidemiology 16 Oct 2006
Prevention • What is the impact of hygiene and where does it need to be emphasized? • CA-MRSA • Home • Recreation • Institutions • Personal vs. environmental hygiene • Reduction of viral infections would reduce opportunities for inappropriate use • URIs • Seasonal and Pandemic Influenza • Non-Pharmaceutical Public Health Interventions 16 Oct 2006
Antimicrobial Use • How can antimicrobial use be further improved? • Diagnostic • Accurate distinction between viral vs. bacterial infections • Computer-assisted decision support • Evaluation • HEDIS measures • Practice improvement 16 Oct 2006
Treatment • Which skin and soft tissue infections require antimicrobial treatment vs. I&D vs. both? • Trials of existing antimicrobial drugs for resistant infections for which there are no data or FDA-approved indications • What is the role of new antimicrobial drugs as they are approved? • More or less restrictive than FDA-approved indications • [HIV] • [Influenza] • [TB] 16 Oct 2006
Epidemiology/Pharmacoepidemiology • What is the extent of adverse events? • Would improved knowledge of AEs further encourage appropriate use? • How much does non-prescription sale of antimicrobial drugs contribute to inappropriate use? • How can non-prescription antimicrobial use behaviors be changed? • Is this a cultural or access to care issue or both? • Are there social/ethnic groups beyond Latinos for which this is a phenomenon? • Are $4 prescription prices a good or a bad thing? 16 Oct 2006
U. S. Interagency Task Force on Antimicrobial Resistance Agency for Healthcare Research and Quality Health Resources and Services Administration Centers for Medicare and Medicaid Services Agency for International Development Department of Defense Department of Agriculture Environmental Protection Agency Department of Veterans Affairs 16 Oct 2006
Public Health Action Plan to Combat Antimicrobial Resistance • Focus areas • • Surveillance Prevention and Control Research Product Development • Implementation contingent on resources • Annual reports at public meetings: 2002 -2005 • Documents: http: //www. cdc. gov/drugresistance/ 16 Oct 2006
Acknowledgements • • • CA-MRSA: Rachel Gorwitz, Jeff Hageman C. difficile: Cliff Mc. Donald Adverse events: Nadine Shehab, Dan Budnitz S. pneumoniae: Matt Moore, Cyndy Whitney CDSS/Rural: Matthew Samore Get Smart, prescribing data: Allison Patti, Pat Cook, Cindy Friedman, Richard Besser • www. cdc. gov/drugresistance/ 16 Oct 2006
believe it boss you may not believe it boss but it is the solemn truth that sometimes you humans are just as ridiculous to us insects as we insects are to you humans archyology the long lost tales of archy and mehitabel don marquis (1878 -1937) university press of new england 1996 16 Oct 2006
Intervening with Providers: Medical School Appropriate Antibiotic Use Curriculum • Developed by University of California, San Diego • Piloted at 6 medical schools • Updated in 2004 • 25 Schools in 2005 16 Oct 2006
Intervening with Providers: Residency Education • Appropriate antibiotic use curriculum based on med school curriculum • For family practice, pediatric and internal medicine residents • Under development by Oregon Health and Science University 16 Oct 2006
Intervening with Providers: Otitis Media Curriculum • Curriculum to increase residents’ proficiency in the diagnosis of AOM • For pediatric and family practice residents • Methods include • web-based cases • telemedicine technology (video otoscopes) • hands-on skill building activities • Under development by Children’s Hospital of Pittsburgh 16 Oct 2006
16 Oct 2006
Intervening with Providers: Pharmacy Initiative • Pharmacy CE • Hospital based in clearance • Community-based being planned • Adherence tool developed and distributed • Focus tested in July 05 • >2 million tri-folds distributed (Oct-Jan 06) • “How-to” guide 16 Oct 2006
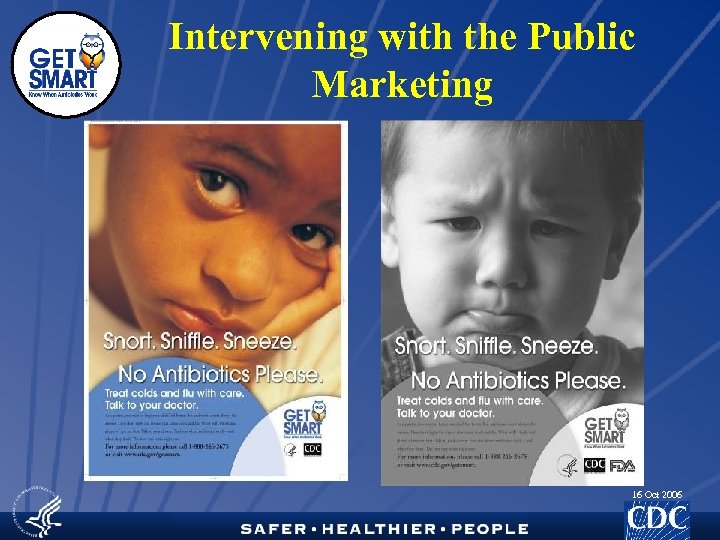
Intervening with the Public Marketing 16 Oct 2006

Paid Advertising 16 Oct 2006
Sample Educational Materials 16 Oct 2006
Multidimensional Local Interventions • Physician prescribing report cards • Public awareness media campaign • Elementary education curriculum • Cold care kits through providers 16 Oct 2006
6ed7427d3fb646bc37f6cef6f9824b17.ppt