598c7a114919eb68cc3a53ed001e1160.ppt
- Количество слайдов: 57
 Prevention Research Centers (PRC)-Healthy Aging Research Network (HAN) Webinar Series Evidence-Based Depression Care Management: Healthy IDEAS October 29, 2008 3: 00 -4: 30 EST Moderated By: Alixe Mc. Neill Nancy L. Wilson, M. A. , LCSW Pat Gleason-Wynn, Ph. D, LCSW, BSN, RN Sharon Foerster, LCSW
Prevention Research Centers (PRC)-Healthy Aging Research Network (HAN) Webinar Series Evidence-Based Depression Care Management: Healthy IDEAS October 29, 2008 3: 00 -4: 30 EST Moderated By: Alixe Mc. Neill Nancy L. Wilson, M. A. , LCSW Pat Gleason-Wynn, Ph. D, LCSW, BSN, RN Sharon Foerster, LCSW
 Sponsors Prevention Research Centers. Healthy Aging Research Network http: //www. prc-han. org/ Retirement Research Foundation http: //www. rrf. org/ National Council on Aging http: //ncoa. org/index. cfm
Sponsors Prevention Research Centers. Healthy Aging Research Network http: //www. prc-han. org/ Retirement Research Foundation http: //www. rrf. org/ National Council on Aging http: //ncoa. org/index. cfm
 Presentation Objectives Describe origins and key components of Healthy IDEAS n Present program outcomes n Discuss steps in implementation process including key partnerships, funding streams, resources needed n Highlight challenges and lessons from program delivery in two states n
Presentation Objectives Describe origins and key components of Healthy IDEAS n Present program outcomes n Discuss steps in implementation process including key partnerships, funding streams, resources needed n Highlight challenges and lessons from program delivery in two states n
 HEALTHY IDEAS Identifying Depression Empowering Activities for Seniors
HEALTHY IDEAS Identifying Depression Empowering Activities for Seniors
 Accomplished through Partnerships n Program Leadership: Care for Elders and Baylor Ø Ø n n n +80 member Houston-based partnership committed to creating solutions to increase access to services, improve quality and enhance life for older adults and caregivers www. careforelders. org Funders: John A. Hartford Foundation, Administration on Aging, Robert Wood Johnson, SAMHSA Policy Leadership: Ao. A , National Council on Aging Academic Expertise: Baylor College of Medicine and Michael E. De. Bakey Veterans Affairs Medical Center Community Aging and Mental Health Providers Elders and family caregivers
Accomplished through Partnerships n Program Leadership: Care for Elders and Baylor Ø Ø n n n +80 member Houston-based partnership committed to creating solutions to increase access to services, improve quality and enhance life for older adults and caregivers www. careforelders. org Funders: John A. Hartford Foundation, Administration on Aging, Robert Wood Johnson, SAMHSA Policy Leadership: Ao. A , National Council on Aging Academic Expertise: Baylor College of Medicine and Michael E. De. Bakey Veterans Affairs Medical Center Community Aging and Mental Health Providers Elders and family caregivers
 Depression is Common, Disabling & Deadly n n n Depression is a recurring, chronic illness Older adults are often under-recognized & under-treated; great disparities Highest rate of successful suicides Identification of depression is not sufficient Effective methods to identify, evaluate, & treat depression and improve quality of life are available
Depression is Common, Disabling & Deadly n n n Depression is a recurring, chronic illness Older adults are often under-recognized & under-treated; great disparities Highest rate of successful suicides Identification of depression is not sufficient Effective methods to identify, evaluate, & treat depression and improve quality of life are available
 Barriers to Addressing Depression in Older Adults n Client Barriers n n n Provider Barriers n n Stigma – “I’m not crazy! I’m not a weak person” Lack of knowledge- “ It’s just my diabetes or being old” “ What will this pill do? ” Lack of knowledge and skills Primary Care faces many competing demands Scarcity of mental health professionals System Barriers n n How can we get care to the person or the person to care? ” Financing of services is limited and in silos
Barriers to Addressing Depression in Older Adults n Client Barriers n n n Provider Barriers n n Stigma – “I’m not crazy! I’m not a weak person” Lack of knowledge- “ It’s just my diabetes or being old” “ What will this pill do? ” Lack of knowledge and skills Primary Care faces many competing demands Scarcity of mental health professionals System Barriers n n How can we get care to the person or the person to care? ” Financing of services is limited and in silos
 What is Healthy IDEAS? Healthy IDEAS (Identifying Depression, Empowering Activities for Seniors) An evidence-based community depression program designed to detect and reduce the severity of depressive symptoms in older adults with chronic health conditions and functional limitations through existing community based case management services.
What is Healthy IDEAS? Healthy IDEAS (Identifying Depression, Empowering Activities for Seniors) An evidence-based community depression program designed to detect and reduce the severity of depressive symptoms in older adults with chronic health conditions and functional limitations through existing community based case management services.
 Program Goals n n To reach the intended population of frail, high-risk, diverse older adults, often overlooked and under-treated. To train agency staff to provide and deliver an evidencebased intervention for depression to older adults To improve the linkage between community aging service providers and health care professionals through appropriate referrals, better communication & effective partnerships. To insure systematic identification of depression and action through attention to depression screening embedded into routine case management services.
Program Goals n n To reach the intended population of frail, high-risk, diverse older adults, often overlooked and under-treated. To train agency staff to provide and deliver an evidencebased intervention for depression to older adults To improve the linkage between community aging service providers and health care professionals through appropriate referrals, better communication & effective partnerships. To insure systematic identification of depression and action through attention to depression screening embedded into routine case management services.
 Evidence for Healthy IDEAS Components n n n IMPACT AND PEARLS offered the “care management road map “ and evidence for in-home approach Screening and Assessment: Early recognition of depression facilitates treatment and can be done by non-professionals using valid tools. (Whooley et al. 1997, Sheikh & Yesavage, 1986, Williams et al. 2002. ) Education, Linkage, and Self-management Support: (Unützer et al. , 2002 and Hunkeler et al. , 2000. ) Behavioral Activation: Helping clients “activate” to increase behaviors that fit with life goals and produce rewards will help decrease depressive symptoms. (Hopko et al. , 2003, , Jacobson et al. , 2000. ) Systematic Follow-up and Assessment of depressive symptoms
Evidence for Healthy IDEAS Components n n n IMPACT AND PEARLS offered the “care management road map “ and evidence for in-home approach Screening and Assessment: Early recognition of depression facilitates treatment and can be done by non-professionals using valid tools. (Whooley et al. 1997, Sheikh & Yesavage, 1986, Williams et al. 2002. ) Education, Linkage, and Self-management Support: (Unützer et al. , 2002 and Hunkeler et al. , 2000. ) Behavioral Activation: Helping clients “activate” to increase behaviors that fit with life goals and produce rewards will help decrease depressive symptoms. (Hopko et al. , 2003, , Jacobson et al. , 2000. ) Systematic Follow-up and Assessment of depressive symptoms
 Target Population Underserved Populations Ethnically diverse and socio-economically diverse populations of older adults who are at high risk for depressive symptoms and living in the community. Inclusion Criteria: n 60+ n Currently enrolled in a care or case management program n Cognitive ability to participate n Able to communicate verbally n
Target Population Underserved Populations Ethnically diverse and socio-economically diverse populations of older adults who are at high risk for depressive symptoms and living in the community. Inclusion Criteria: n 60+ n Currently enrolled in a care or case management program n Cognitive ability to participate n Able to communicate verbally n
 Program Design n n Embedded in case management programs. Conducted in the client’s home on a one-to-one basis by case managers over a 3 -6 month period. Utilizes existing staff with established relationships with targeted participants. A manual outlines the steps and includes written worksheets, client handouts, and forms to support and document the process and client outcomes. Partner with health/mental health care providers to facilitate referral and uses community partnership approach for training, evaluation & fidelity.
Program Design n n Embedded in case management programs. Conducted in the client’s home on a one-to-one basis by case managers over a 3 -6 month period. Utilizes existing staff with established relationships with targeted participants. A manual outlines the steps and includes written worksheets, client handouts, and forms to support and document the process and client outcomes. Partner with health/mental health care providers to facilitate referral and uses community partnership approach for training, evaluation & fidelity.
 Core Program Components § Screening for symptoms of depression & assessing severity Ø 15 item Geriatric Depression Scale (GDS) or PHQ-9 Educating older adults & family caregivers about depression & effective treatment: including self-care & medication. Referral, linkage & follow-up for older adults with untreated depression to health or mental health providers. Behavioral Activation (BA) empowering older adults to manage their depressive symptoms by engaging in meaningful, positive activities. Ø § § § Two-question screen & standardized assessment
Core Program Components § Screening for symptoms of depression & assessing severity Ø 15 item Geriatric Depression Scale (GDS) or PHQ-9 Educating older adults & family caregivers about depression & effective treatment: including self-care & medication. Referral, linkage & follow-up for older adults with untreated depression to health or mental health providers. Behavioral Activation (BA) empowering older adults to manage their depressive symptoms by engaging in meaningful, positive activities. Ø § § § Two-question screen & standardized assessment
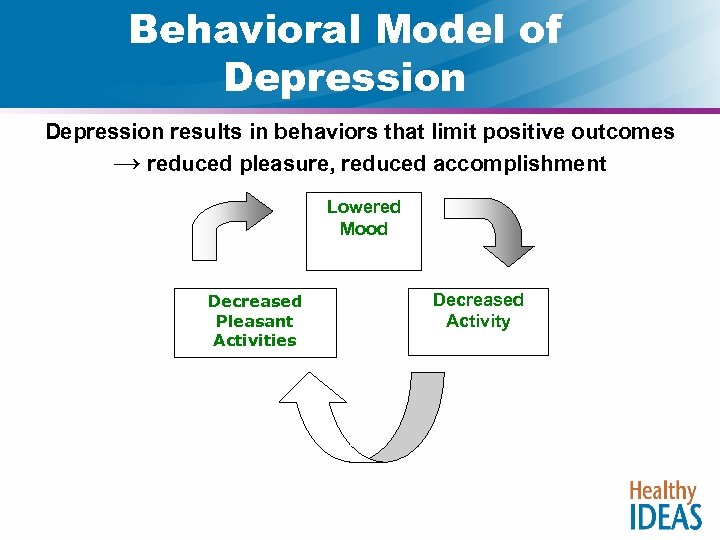 Behavioral Model of Depression results in behaviors that limit positive outcomes → reduced pleasure, reduced accomplishment Lowered Mood Decreased Pleasant Activities Decreased Activity
Behavioral Model of Depression results in behaviors that limit positive outcomes → reduced pleasure, reduced accomplishment Lowered Mood Decreased Pleasant Activities Decreased Activity
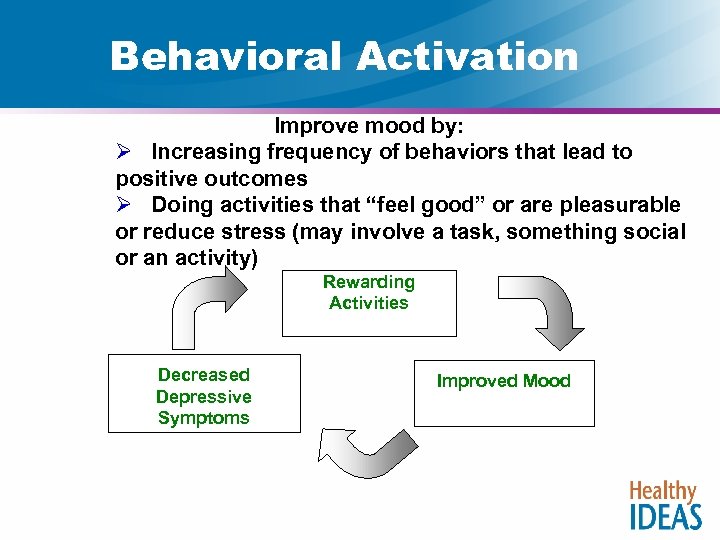 Behavioral Activation Improve mood by: Ø Increasing frequency of behaviors that lead to positive outcomes Ø Doing activities that “feel good” or are pleasurable or reduce stress (may involve a task, something social or an activity) Rewarding Activities Decreased Depressive Symptoms Improved Mood
Behavioral Activation Improve mood by: Ø Increasing frequency of behaviors that lead to positive outcomes Ø Doing activities that “feel good” or are pleasurable or reduce stress (may involve a task, something social or an activity) Rewarding Activities Decreased Depressive Symptoms Improved Mood
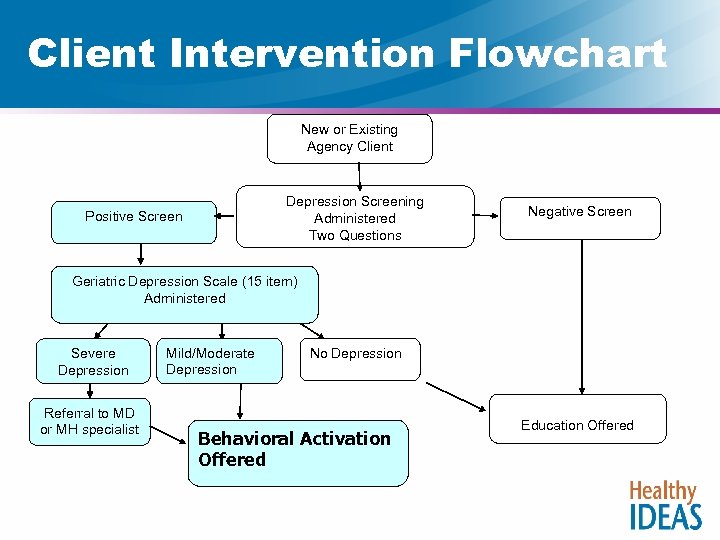 Client Intervention Flowchart New or Existing Agency Client Depression Screening Administered Two Questions Positive Screen Negative Screen Geriatric Depression Scale (15 item) Administered Severe Depression Referral to MD or MH specialist Mild/Moderate Depression No Depression Behavioral Activation Offered Education Offered
Client Intervention Flowchart New or Existing Agency Client Depression Screening Administered Two Questions Positive Screen Negative Screen Geriatric Depression Scale (15 item) Administered Severe Depression Referral to MD or MH specialist Mild/Moderate Depression No Depression Behavioral Activation Offered Education Offered
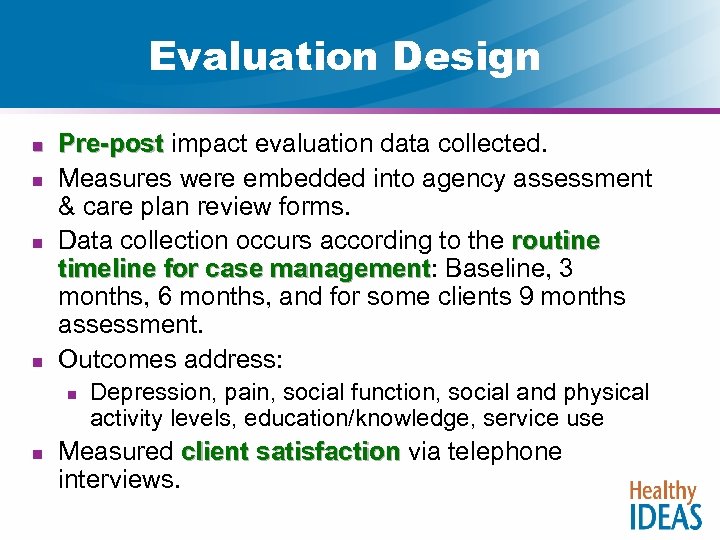 Evaluation Design n n Pre-post impact evaluation data collected. Pre-post Measures were embedded into agency assessment & care plan review forms. Data collection occurs according to the routine timeline for case management: Baseline, 3 timeline for case management months, 6 months, and for some clients 9 months assessment. Outcomes address: n n Depression, pain, social function, social and physical activity levels, education/knowledge, service use Measured client satisfaction via telephone client satisfaction interviews.
Evaluation Design n n Pre-post impact evaluation data collected. Pre-post Measures were embedded into agency assessment & care plan review forms. Data collection occurs according to the routine timeline for case management: Baseline, 3 timeline for case management months, 6 months, and for some clients 9 months assessment. Outcomes address: n n Depression, pain, social function, social and physical activity levels, education/knowledge, service use Measured client satisfaction via telephone client satisfaction interviews.
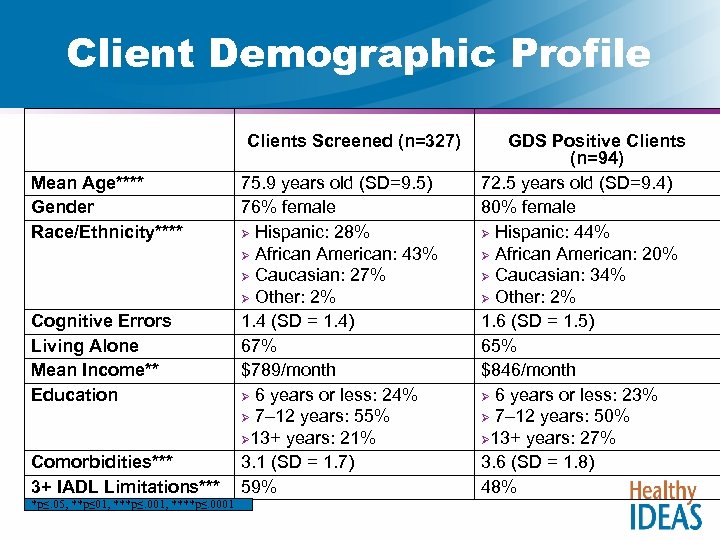 Client Demographic Profile Clients Screened (n=327) Mean Age**** Gender Race/Ethnicity**** Cognitive Errors Living Alone Mean Income** Education Comorbidities*** 3+ IADL Limitations*** *p≤. 05, **p≤ 01, ***p≤. 001, ****p≤. 0001 75. 9 years old (SD=9. 5) 76% female Ø Hispanic: 28% Ø African American: 43% Ø Caucasian: 27% Ø Other: 2% 1. 4 (SD = 1. 4) 67% $789/month Ø 6 years or less: 24% Ø 7– 12 years: 55% Ø 13+ years: 21% 3. 1 (SD = 1. 7) 59% GDS Positive Clients (n=94) 72. 5 years old (SD=9. 4) 80% female Ø Hispanic: 44% Ø African American: 20% Ø Caucasian: 34% Ø Other: 2% 1. 6 (SD = 1. 5) 65% $846/month Ø 6 years or less: 23% Ø 7– 12 years: 50% Ø 13+ years: 27% 3. 6 (SD = 1. 8) 48%
Client Demographic Profile Clients Screened (n=327) Mean Age**** Gender Race/Ethnicity**** Cognitive Errors Living Alone Mean Income** Education Comorbidities*** 3+ IADL Limitations*** *p≤. 05, **p≤ 01, ***p≤. 001, ****p≤. 0001 75. 9 years old (SD=9. 5) 76% female Ø Hispanic: 28% Ø African American: 43% Ø Caucasian: 27% Ø Other: 2% 1. 4 (SD = 1. 4) 67% $789/month Ø 6 years or less: 24% Ø 7– 12 years: 55% Ø 13+ years: 21% 3. 1 (SD = 1. 7) 59% GDS Positive Clients (n=94) 72. 5 years old (SD=9. 4) 80% female Ø Hispanic: 44% Ø African American: 20% Ø Caucasian: 34% Ø Other: 2% 1. 6 (SD = 1. 5) 65% $846/month Ø 6 years or less: 23% Ø 7– 12 years: 50% Ø 13+ years: 27% 3. 6 (SD = 1. 8) 48%
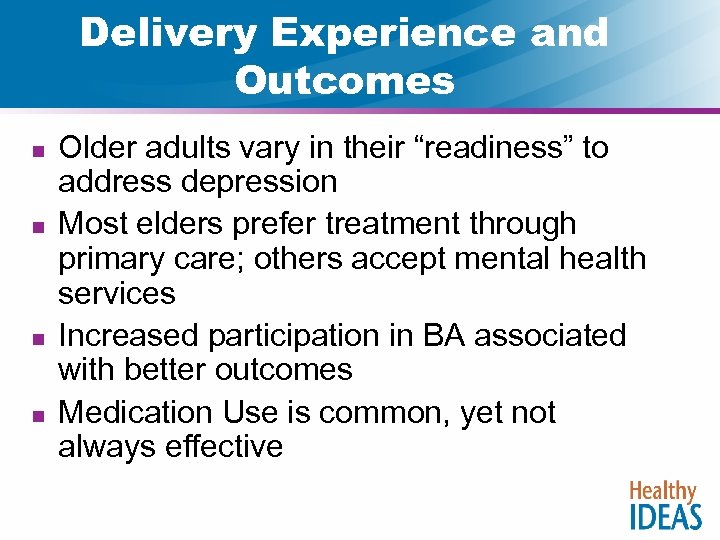 Delivery Experience and Outcomes n n Older adults vary in their “readiness” to address depression Most elders prefer treatment through primary care; others accept mental health services Increased participation in BA associated with better outcomes Medication Use is common, yet not always effective
Delivery Experience and Outcomes n n Older adults vary in their “readiness” to address depression Most elders prefer treatment through primary care; others accept mental health services Increased participation in BA associated with better outcomes Medication Use is common, yet not always effective
 Client Impact n n n Reduction in depression severity Reduction of self-reported pain Increased knowledge of how to get help for depression. Increased level of activity knowledge of how to manage depressive symptoms.
Client Impact n n n Reduction in depression severity Reduction of self-reported pain Increased knowledge of how to get help for depression. Increased level of activity knowledge of how to manage depressive symptoms.
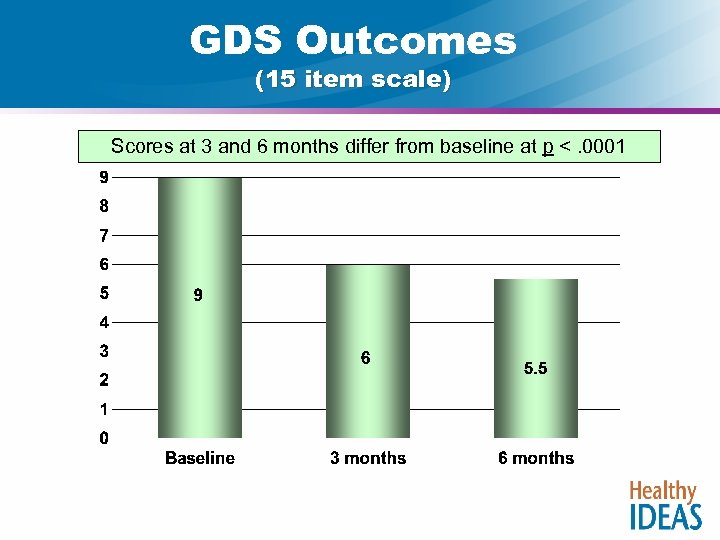 GDS Outcomes (15 item scale) Scores at 3 and 6 months differ from baseline at p <. 0001
GDS Outcomes (15 item scale) Scores at 3 and 6 months differ from baseline at p <. 0001
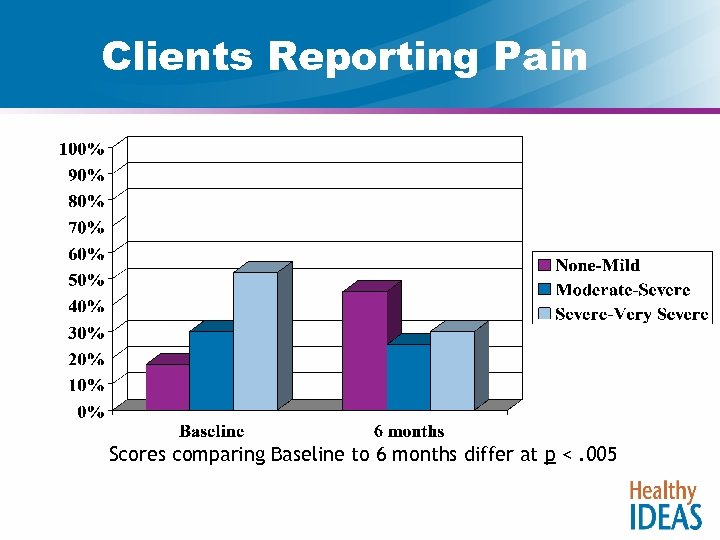 Clients Reporting Pain Scores comparing Baseline to 6 months differ at p <. 005
Clients Reporting Pain Scores comparing Baseline to 6 months differ at p <. 005
 Healthy IDEAS Implementation Process : Activities and Resources Agencies or Community Partnerships need: n Dedicated program leadership n Mental/Behavioral Health Expertise for Training/Coaching n Effective Linkage and Communication systems with Treatment Providers n Practitioners who can incorporate components into their existing case management routine with older adults/caregivers n System for collecting and monitoring depression and other relevant outcome data
Healthy IDEAS Implementation Process : Activities and Resources Agencies or Community Partnerships need: n Dedicated program leadership n Mental/Behavioral Health Expertise for Training/Coaching n Effective Linkage and Communication systems with Treatment Providers n Practitioners who can incorporate components into their existing case management routine with older adults/caregivers n System for collecting and monitoring depression and other relevant outcome data
 Challenges n n n Stigma – among clients and providers Reluctance to change – Clients and staff both have to learn new behaviors Resources - Affordable mental health diagnostic or treatment services Time required for the intervention – in the face of competing demands Commitment – at the agency level to addressing depression and supporting a change process.
Challenges n n n Stigma – among clients and providers Reluctance to change – Clients and staff both have to learn new behaviors Resources - Affordable mental health diagnostic or treatment services Time required for the intervention – in the face of competing demands Commitment – at the agency level to addressing depression and supporting a change process.
 The Maine Experience Sharon Foerster, LCSW Director, Elder Independence of Maine Webinar – October 29, 2008
The Maine Experience Sharon Foerster, LCSW Director, Elder Independence of Maine Webinar – October 29, 2008
 Why replicate Healthy IDEAS? n Need and Opportunity n n n EIM Home Care Coordination Agency n Case management (telephone and face to face) n Serve consumers throughout the state n Community-based population (HCB Waiver services) – Identify a specific population and specific Care Managers n Significant functional limitations Consumer Need had previously been identified n 60% with mental health diagnosis HI a good match n Depression focus n Case management relationship with home visits/Fidelity
Why replicate Healthy IDEAS? n Need and Opportunity n n n EIM Home Care Coordination Agency n Case management (telephone and face to face) n Serve consumers throughout the state n Community-based population (HCB Waiver services) – Identify a specific population and specific Care Managers n Significant functional limitations Consumer Need had previously been identified n 60% with mental health diagnosis HI a good match n Depression focus n Case management relationship with home visits/Fidelity
 History and Current Status n n n Leadership began exploration and planning in April 2007 Fifteen (18) Staff (case managers, supervisors, managers) trained how to deliver intervention in October 2007 CM Staff (RNs and LSWs) began screenings in November 2007 (pilot first in Oct 07) 343 population of HCB older adult consumers 102 not approached n cognitive level, non-communicative, n GDS not available in primary language (Somali) 191 screened between November 2007 and April 2007 n GDS two question screen n 80 screened in (GDS positive) (42%)
History and Current Status n n n Leadership began exploration and planning in April 2007 Fifteen (18) Staff (case managers, supervisors, managers) trained how to deliver intervention in October 2007 CM Staff (RNs and LSWs) began screenings in November 2007 (pilot first in Oct 07) 343 population of HCB older adult consumers 102 not approached n cognitive level, non-communicative, n GDS not available in primary language (Somali) 191 screened between November 2007 and April 2007 n GDS two question screen n 80 screened in (GDS positive) (42%)
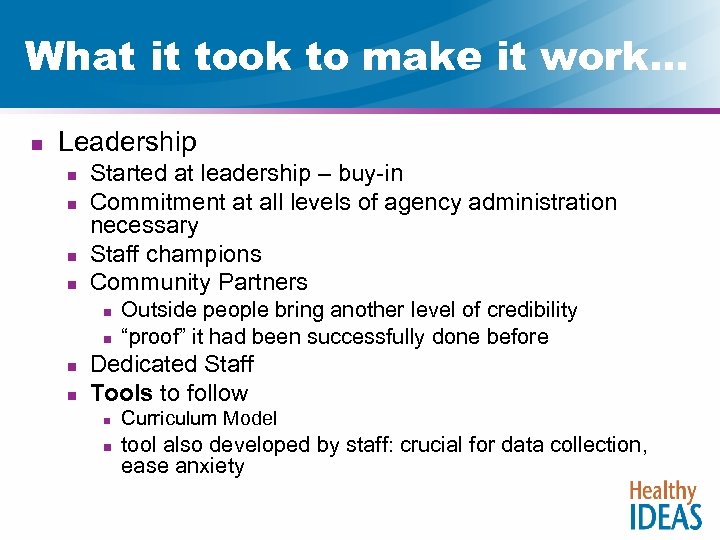 What it took to make it work… n Leadership n n Started at leadership – buy-in Commitment at all levels of agency administration necessary Staff champions Community Partners n n Outside people bring another level of credibility “proof” it had been successfully done before Dedicated Staff Tools to follow n n Curriculum Model tool also developed by staff: crucial for data collection, ease anxiety
What it took to make it work… n Leadership n n Started at leadership – buy-in Commitment at all levels of agency administration necessary Staff champions Community Partners n n Outside people bring another level of credibility “proof” it had been successfully done before Dedicated Staff Tools to follow n n Curriculum Model tool also developed by staff: crucial for data collection, ease anxiety
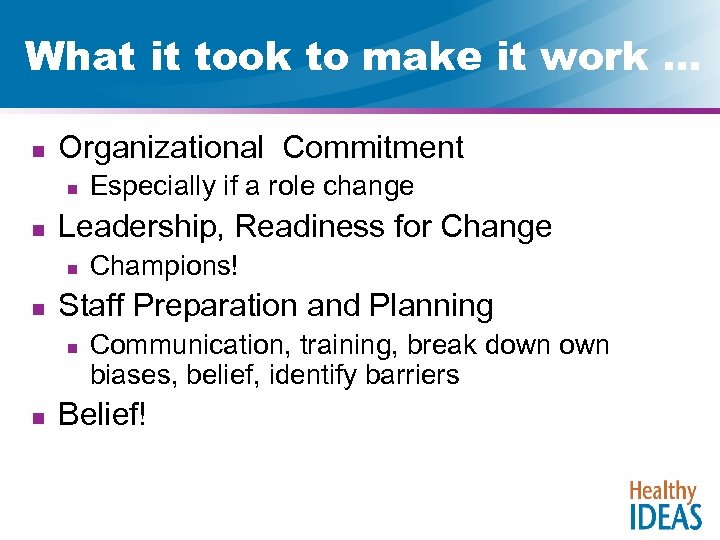 What it took to make it work … n Organizational Commitment n n Leadership, Readiness for Change n n Champions! Staff Preparation and Planning n n Especially if a role change Communication, training, break down biases, belief, identify barriers Belief!
What it took to make it work … n Organizational Commitment n n Leadership, Readiness for Change n n Champions! Staff Preparation and Planning n n Especially if a role change Communication, training, break down biases, belief, identify barriers Belief!
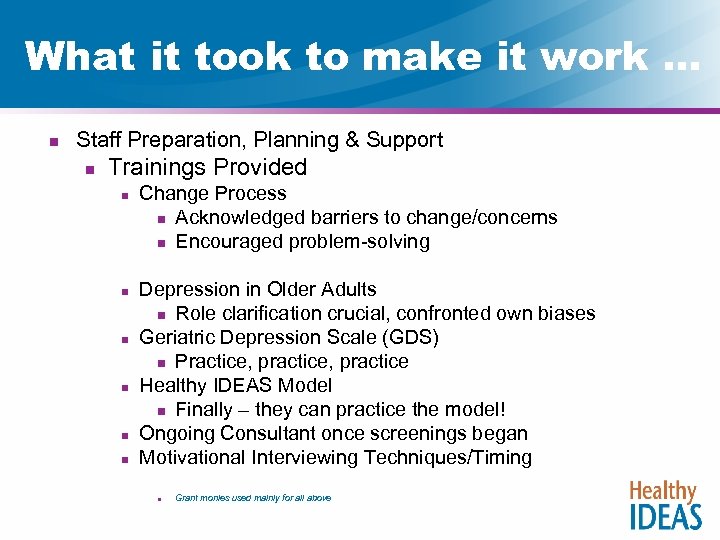 What it took to make it work … n Staff Preparation, Planning & Support n Trainings Provided n n n Change Process n Acknowledged barriers to change/concerns n Encouraged problem-solving Depression in Older Adults n Role clarification crucial, confronted own biases Geriatric Depression Scale (GDS) n Practice, practice Healthy IDEAS Model n Finally – they can practice the model! Ongoing Consultant once screenings began Motivational Interviewing Techniques/Timing n Grant monies used mainly for all above
What it took to make it work … n Staff Preparation, Planning & Support n Trainings Provided n n n Change Process n Acknowledged barriers to change/concerns n Encouraged problem-solving Depression in Older Adults n Role clarification crucial, confronted own biases Geriatric Depression Scale (GDS) n Practice, practice Healthy IDEAS Model n Finally – they can practice the model! Ongoing Consultant once screenings began Motivational Interviewing Techniques/Timing n Grant monies used mainly for all above
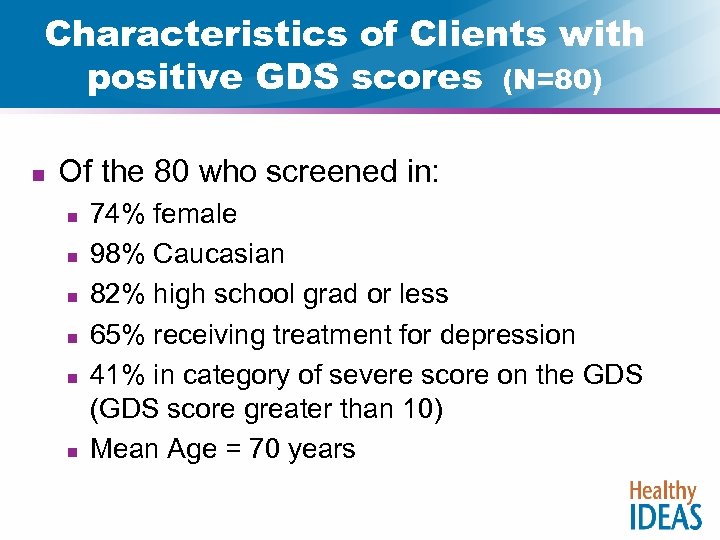 Characteristics of Clients with positive GDS scores (N=80) n Of the 80 who screened in: n n n 74% female 98% Caucasian 82% high school grad or less 65% receiving treatment for depression 41% in category of severe score on the GDS (GDS score greater than 10) Mean Age = 70 years
Characteristics of Clients with positive GDS scores (N=80) n Of the 80 who screened in: n n n 74% female 98% Caucasian 82% high school grad or less 65% receiving treatment for depression 41% in category of severe score on the GDS (GDS score greater than 10) Mean Age = 70 years
 Consumers Who Screened in n Eighty (80) screened in n Forty-three (43), 54%, had GDS Score of 6 or above and eligible for the Behavioral Activation n n 24 (56%) agreed to do the BA intervention 23 (53%) had a referral to physician or mental health counselor
Consumers Who Screened in n Eighty (80) screened in n Forty-three (43), 54%, had GDS Score of 6 or above and eligible for the Behavioral Activation n n 24 (56%) agreed to do the BA intervention 23 (53%) had a referral to physician or mental health counselor
 “Lessons Learned” n Perfection not the Goal n n Learning is the Goal n n n Redefines type of pressure/learning curve demonstration grant/reminders/new skills Communication Adequate Support needed/no additional staff but still need time & resources Motivational Interviewing great addition/timing “Therapy” not always “the” answer n Prevention/health promotion, self-management aspect to depression, connection of mood to activities
“Lessons Learned” n Perfection not the Goal n n Learning is the Goal n n n Redefines type of pressure/learning curve demonstration grant/reminders/new skills Communication Adequate Support needed/no additional staff but still need time & resources Motivational Interviewing great addition/timing “Therapy” not always “the” answer n Prevention/health promotion, self-management aspect to depression, connection of mood to activities
 Consumer Outcomes n n n n 81 yr old female with significant arthritis, anemia, renal insufficiency, and long standing history of depression. Family members report she would “often be snippy” with them. Scored a 12 on GDS (out of 15), moderate to severe cons was willing to do HI Behavioral Activation to improve her mood. Chose activities and work with physician Effects on family dynamics Reported Outcome: She reported that she was doing much better with interactions with family and enjoying more quality time with them. She also was getting out more. 6 month GDS score was 7
Consumer Outcomes n n n n 81 yr old female with significant arthritis, anemia, renal insufficiency, and long standing history of depression. Family members report she would “often be snippy” with them. Scored a 12 on GDS (out of 15), moderate to severe cons was willing to do HI Behavioral Activation to improve her mood. Chose activities and work with physician Effects on family dynamics Reported Outcome: She reported that she was doing much better with interactions with family and enjoying more quality time with them. She also was getting out more. 6 month GDS score was 7
 Consumer Outcomes n n n 77 year old with history of stroke. No use of one side of her body, transfers via hoyer lift. Family reported she was not motivated to do anything. When approached with HI and discussion of mood, consumer feared NF placement. Scored 9 on GDS and after much discussion (use of MI), agreed to participate in HI Behavioral Activation. Family was supportive and helped her to work on her goals. Chose activities enjoyed previous to the stroke, but given up n n Knit caps, puzzles, look at her garden 6 month GDS score was 6
Consumer Outcomes n n n 77 year old with history of stroke. No use of one side of her body, transfers via hoyer lift. Family reported she was not motivated to do anything. When approached with HI and discussion of mood, consumer feared NF placement. Scored 9 on GDS and after much discussion (use of MI), agreed to participate in HI Behavioral Activation. Family was supportive and helped her to work on her goals. Chose activities enjoyed previous to the stroke, but given up n n Knit caps, puzzles, look at her garden 6 month GDS score was 6
 Consumer Outcomes – CM Impact n n n 77 y/o man recent stroke Scored in and chose to try Behavioral Activation Chose goal of wife reading aloud to him Case Manager thought this goal was “too passive” and would not make a true difference Hindsight: understood how goal was meaningful
Consumer Outcomes – CM Impact n n n 77 y/o man recent stroke Scored in and chose to try Behavioral Activation Chose goal of wife reading aloud to him Case Manager thought this goal was “too passive” and would not make a true difference Hindsight: understood how goal was meaningful
 The BIG Success n Staff Role Change n n n Shift to mental health focus Greater awareness of depression in older adults Depression “OK” to talk about, “I think about consumers differently” Staff developed the tool for organizing the work (from the HI training module) Positive Outcomes basis for Policy Change: Need to embed EBP into waiver programs, added value in payment structure for this case management model
The BIG Success n Staff Role Change n n n Shift to mental health focus Greater awareness of depression in older adults Depression “OK” to talk about, “I think about consumers differently” Staff developed the tool for organizing the work (from the HI training module) Positive Outcomes basis for Policy Change: Need to embed EBP into waiver programs, added value in payment structure for this case management model
 Big Success (Cont’d. ) n Consumer depression signs addressed n n n Staff: More than therapy and medication as intervention Consumers: learn self-management along with other resources Family Members grateful “System: ” Prevention is key HI EBP is “marriage” of science and service: staff see improvement
Big Success (Cont’d. ) n Consumer depression signs addressed n n n Staff: More than therapy and medication as intervention Consumers: learn self-management along with other resources Family Members grateful “System: ” Prevention is key HI EBP is “marriage” of science and service: staff see improvement
 Contact Information n Sharon Foerster, L. C. S. W. n Director, Elder Independence of Maine n n A division of Seniors. Plus, Area Agency on Aging sfoerster@elderindependence. org 207 -795 -7213 P. O. Box 659, Lewiston, ME 04243
Contact Information n Sharon Foerster, L. C. S. W. n Director, Elder Independence of Maine n n A division of Seniors. Plus, Area Agency on Aging sfoerster@elderindependence. org 207 -795 -7213 P. O. Box 659, Lewiston, ME 04243
 Healthy IDEAS In Fort Worth Pat Gleason-Wynn, Ph. D, LCSW, BSN, RN Healthy IDEAS Team Leader Area Agency on Aging of Tarrant County Webinar – October 29, 2008
Healthy IDEAS In Fort Worth Pat Gleason-Wynn, Ph. D, LCSW, BSN, RN Healthy IDEAS Team Leader Area Agency on Aging of Tarrant County Webinar – October 29, 2008
 Healthy IDEAS (HI) n n Initiative of the Area Agency on Aging (AAA) and United Way of Tarrant County, Texas Located in Fort Worth, Texas; Tarrant County; North Central Texas n n n Total County Population: about 1. 7 million Population age 60 and over: over 200, 000 “Great Place to Grow Old”
Healthy IDEAS (HI) n n Initiative of the Area Agency on Aging (AAA) and United Way of Tarrant County, Texas Located in Fort Worth, Texas; Tarrant County; North Central Texas n n n Total County Population: about 1. 7 million Population age 60 and over: over 200, 000 “Great Place to Grow Old”
 Decision to Implement n n n High prevalence of isolated older adults with depressive symptoms HI is an evidence-based program focusing on depression & older adults, with demonstrated effectiveness Infrastructure present in Tarrant County to implement the program among existing case management services; high collaboration
Decision to Implement n n n High prevalence of isolated older adults with depressive symptoms HI is an evidence-based program focusing on depression & older adults, with demonstrated effectiveness Infrastructure present in Tarrant County to implement the program among existing case management services; high collaboration
 Stage 1: Pilot Project n March to September 2008 n Funding Stream: In-kind Contributions (Time & Materials) n Agencies: AAA, Catholic Charities, Meals on Wheels, MHMR, and MHA n My roles: Trainer, Coach, Organizer
Stage 1: Pilot Project n March to September 2008 n Funding Stream: In-kind Contributions (Time & Materials) n Agencies: AAA, Catholic Charities, Meals on Wheels, MHMR, and MHA n My roles: Trainer, Coach, Organizer
 Pilot Project n n Agencies: AAA, Catholic Charities, Meals on Wheels, MHMR, and MHA Training: 12 hours n n 22 professionals including administrators, students from agencies [outcome: 7 active case managers] 2 “booster” meetings – May, September – 2 hours
Pilot Project n n Agencies: AAA, Catholic Charities, Meals on Wheels, MHMR, and MHA Training: 12 hours n n 22 professionals including administrators, students from agencies [outcome: 7 active case managers] 2 “booster” meetings – May, September – 2 hours
 Stage 2: Implementation n October 1, 2008 – Current Stage Agencies: AAA, Catholic Charities, Meals on Wheels, Senior Citizen Service n Funding Stream: Title III B, Older Americans Act n Role Changes – still Trainer, Coach n AAA has assumed role of coordinator/organizer for the 5 agencies n
Stage 2: Implementation n October 1, 2008 – Current Stage Agencies: AAA, Catholic Charities, Meals on Wheels, Senior Citizen Service n Funding Stream: Title III B, Older Americans Act n Role Changes – still Trainer, Coach n AAA has assumed role of coordinator/organizer for the 5 agencies n
 Implementation n n Agencies: AAA, Catholic Charities, Meals on Wheels, Senior Citizen Service Training: 8 hours n n 17 professionals including administrators and students [outcome: 13 active case managers] Booster Meeting scheduled for December
Implementation n n Agencies: AAA, Catholic Charities, Meals on Wheels, Senior Citizen Service Training: 8 hours n n 17 professionals including administrators and students [outcome: 13 active case managers] Booster Meeting scheduled for December
 Implementation: Case Managers n 20 case managers actively involved n n n 50% have social work degrees, remaining have degrees in related fields Wide variance of experience: 3 wks to 16 years 4 different agencies involved with 2 other agencies serving as resources
Implementation: Case Managers n 20 case managers actively involved n n n 50% have social work degrees, remaining have degrees in related fields Wide variance of experience: 3 wks to 16 years 4 different agencies involved with 2 other agencies serving as resources
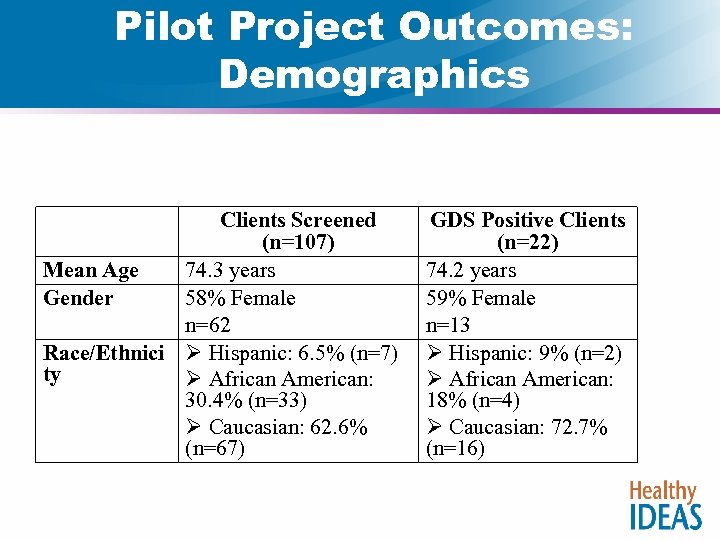 Pilot Project Outcomes: Demographics Clients Screened (n=107) Mean Age 74. 3 years Gender 58% Female n=62 Race/Ethnici Ø Hispanic: 6. 5% (n=7) ty Ø African American: 30. 4% (n=33) Ø Caucasian: 62. 6% (n=67) GDS Positive Clients (n=22) 74. 2 years 59% Female n=13 Ø Hispanic: 9% (n=2) Ø African American: 18% (n=4) Ø Caucasian: 72. 7% (n=16)
Pilot Project Outcomes: Demographics Clients Screened (n=107) Mean Age 74. 3 years Gender 58% Female n=62 Race/Ethnici Ø Hispanic: 6. 5% (n=7) ty Ø African American: 30. 4% (n=33) Ø Caucasian: 62. 6% (n=67) GDS Positive Clients (n=22) 74. 2 years 59% Female n=13 Ø Hispanic: 9% (n=2) Ø African American: 18% (n=4) Ø Caucasian: 72. 7% (n=16)
 Examples-Behavioral Activation n n n n Go outside on scooter, 15 -30 minutes daily Pick one and go with wife: doctor appt, store, restaurant Visit with selected neighbor, 1 x wk Work on puzzles, 3 x wk for 30 minutes Walking with Walking Club, Walk daily Go to Senior Center Compile photo albums Tending to plants Writing in journal
Examples-Behavioral Activation n n n n Go outside on scooter, 15 -30 minutes daily Pick one and go with wife: doctor appt, store, restaurant Visit with selected neighbor, 1 x wk Work on puzzles, 3 x wk for 30 minutes Walking with Walking Club, Walk daily Go to Senior Center Compile photo albums Tending to plants Writing in journal
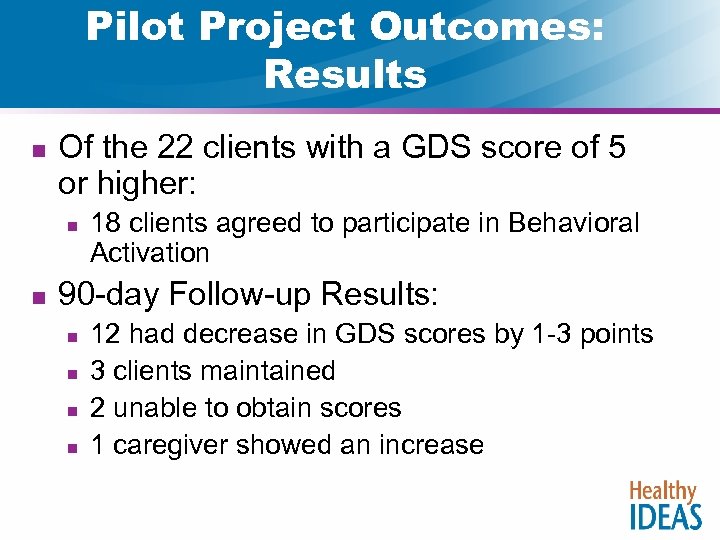 Pilot Project Outcomes: Results n Of the 22 clients with a GDS score of 5 or higher: n n 18 clients agreed to participate in Behavioral Activation 90 -day Follow-up Results: n n 12 had decrease in GDS scores by 1 -3 points 3 clients maintained 2 unable to obtain scores 1 caregiver showed an increase
Pilot Project Outcomes: Results n Of the 22 clients with a GDS score of 5 or higher: n n 18 clients agreed to participate in Behavioral Activation 90 -day Follow-up Results: n n 12 had decrease in GDS scores by 1 -3 points 3 clients maintained 2 unable to obtain scores 1 caregiver showed an increase
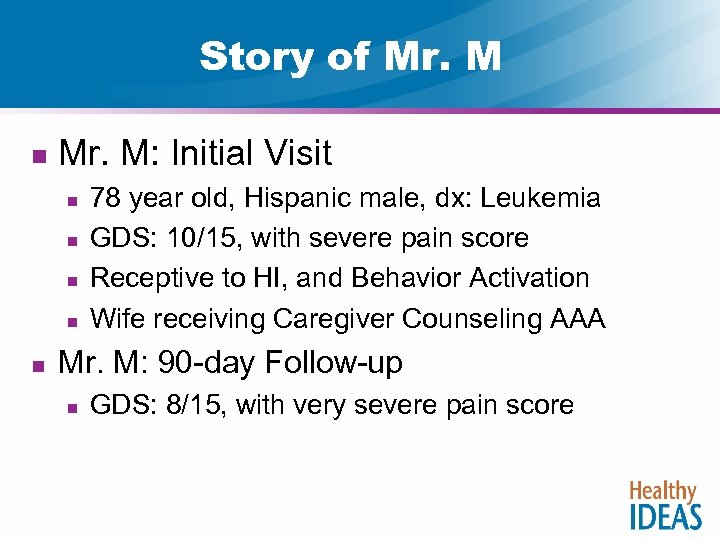 Story of Mr. M n Mr. M: Initial Visit n n n 78 year old, Hispanic male, dx: Leukemia GDS: 10/15, with severe pain score Receptive to HI, and Behavior Activation Wife receiving Caregiver Counseling AAA Mr. M: 90 -day Follow-up n GDS: 8/15, with very severe pain score
Story of Mr. M n Mr. M: Initial Visit n n n 78 year old, Hispanic male, dx: Leukemia GDS: 10/15, with severe pain score Receptive to HI, and Behavior Activation Wife receiving Caregiver Counseling AAA Mr. M: 90 -day Follow-up n GDS: 8/15, with very severe pain score
 Lessons Learned n n n HI is effective modality – it WORKS! Program can be implemented across agencies, unified funding stream Frequent contact (email, phone, booster meetings) between coordinator and case managers important
Lessons Learned n n n HI is effective modality – it WORKS! Program can be implemented across agencies, unified funding stream Frequent contact (email, phone, booster meetings) between coordinator and case managers important
 Future Plans n n n Plan to continue Healthy IDEAS; and, anticipate serving at least 350 clients this fiscal year Implement User Group on Google for discussion and idea sharing among case managers “Booster” meeting is scheduled for December 4 for all active case managers
Future Plans n n n Plan to continue Healthy IDEAS; and, anticipate serving at least 350 clients this fiscal year Implement User Group on Google for discussion and idea sharing among case managers “Booster” meeting is scheduled for December 4 for all active case managers
 For More Information … n n Quijano, L. M. , Stanley, M. A. , Petersen, N. J. , Casado, B. L. , Steinberg, E. H. , Cully, J. A. , Wilson, N. L. Healthy IDEAS: A depression intervention delivered by community-based case managers serving older adults. (2007) Journal of Applied Gerontology 26: 139 -156. Casado, B. L. , Quijano, L. M. , Stanley, M. A. , Cully, J. A. , Steinberg, E. H. , Wilson, N. L Healthy IDEAS: Implementation of A Depression Program Through Community-Based Case Management. (in press) The Gerontologist. Replication report: NCOA-Center for Healthy Aging website http: //www. healthyagingprograms. org Care for Elders: www. careforelders. org/healthyideas
For More Information … n n Quijano, L. M. , Stanley, M. A. , Petersen, N. J. , Casado, B. L. , Steinberg, E. H. , Cully, J. A. , Wilson, N. L. Healthy IDEAS: A depression intervention delivered by community-based case managers serving older adults. (2007) Journal of Applied Gerontology 26: 139 -156. Casado, B. L. , Quijano, L. M. , Stanley, M. A. , Cully, J. A. , Steinberg, E. H. , Wilson, N. L Healthy IDEAS: Implementation of A Depression Program Through Community-Based Case Management. (in press) The Gerontologist. Replication report: NCOA-Center for Healthy Aging website http: //www. healthyagingprograms. org Care for Elders: www. careforelders. org/healthyideas
 Dissemination: www. careforelders. org/healthyideas § Organizations States Ø Area Agency on Ø Arizona Aging case management Ø Georgia programs Ø Maryland Ø Local non-profit Ø Maine social service Ø Michigan agencies Ø New Jersey Ø Behavioral health provider Ø Ohio agencies Ø Texas Ø Caregiver Ø Vermont support programs Contact: esteinberg@shelteringarms. org n
Dissemination: www. careforelders. org/healthyideas § Organizations States Ø Area Agency on Ø Arizona Aging case management Ø Georgia programs Ø Maryland Ø Local non-profit Ø Maine social service Ø Michigan agencies Ø New Jersey Ø Behavioral health provider Ø Ohio agencies Ø Texas Ø Caregiver Ø Vermont support programs Contact: esteinberg@shelteringarms. org n
 Questions & Answers
Questions & Answers
 Future PRC-HAN Webinars All 3: 00 -4: 30 pm EST Relevant to all Evidence-based Programs Thursday, November 13 th Money Matters To Register: http: //ncoa. org/content. cfm? section. ID=64
Future PRC-HAN Webinars All 3: 00 -4: 30 pm EST Relevant to all Evidence-based Programs Thursday, November 13 th Money Matters To Register: http: //ncoa. org/content. cfm? section. ID=64


