1f454465b120470b17498fb649316d0c.ppt
- Количество слайдов: 48
 Prevention of Wrong Site Surgery/Procedure Southern Atlantic Healthcare Alliance OR Education Session January 6, 2016
Prevention of Wrong Site Surgery/Procedure Southern Atlantic Healthcare Alliance OR Education Session January 6, 2016
 Jennifer L. Fencl, DNP, RN, CNS-BC, CNOR: Clinical Nurse Specialist, Operative Services Terri Sharpe, MHA, BSN, RN, CNOR: Assistant Director, Short Stay and Pre-Admission Testing Vangela Swofford, BSN, RN, ASQ-CSSBB, CPHQ: Quality Facilitator 2
Jennifer L. Fencl, DNP, RN, CNS-BC, CNOR: Clinical Nurse Specialist, Operative Services Terri Sharpe, MHA, BSN, RN, CNOR: Assistant Director, Short Stay and Pre-Admission Testing Vangela Swofford, BSN, RN, ASQ-CSSBB, CPHQ: Quality Facilitator 2
 Objectives: Describe the background, implications, and risk factors of performing wronged site surgery/procedures Categorize the risk of wrong site surgery in a healthcare facility Illustrate the importance of clear communication and utilization of the C. U. S. model to share patient safety issues Explain how to use Six Sigma and Lean principles to identify areas for opportunity Construct a fish-bone and time-frame diagram to identify areas for improvement 3
Objectives: Describe the background, implications, and risk factors of performing wronged site surgery/procedures Categorize the risk of wrong site surgery in a healthcare facility Illustrate the importance of clear communication and utilization of the C. U. S. model to share patient safety issues Explain how to use Six Sigma and Lean principles to identify areas for opportunity Construct a fish-bone and time-frame diagram to identify areas for improvement 3
 Break Through Project: Wrong Site Surgery/Procedure "Your life today is a result of your thinking yesterday. Your life tomorrow will be determined by what you think today. " John C. Maxwell 4
Break Through Project: Wrong Site Surgery/Procedure "Your life today is a result of your thinking yesterday. Your life tomorrow will be determined by what you think today. " John C. Maxwell 4
 Wrong Site Surgery/Procedure Hospital / Location: System-wide Area of Focus: Continuum of patient care Time procedure is discussed with patient Procedure After Procedure 5
Wrong Site Surgery/Procedure Hospital / Location: System-wide Area of Focus: Continuum of patient care Time procedure is discussed with patient Procedure After Procedure 5
 Wrong Site Surgery is defined as any procedure performed on the wrong site or patient or performance of the wrong procedure. 6
Wrong Site Surgery is defined as any procedure performed on the wrong site or patient or performance of the wrong procedure. 6
 Background 1995 -2005: Wrong Site Surgery ranked #2 frequently reported sentinel event 1997: American Academy of Orthopedic surgeons-- initial operative site 2001: The North American Spine Surgery-- “Sign, Mark and Radiograph” 2002: American College of Surgeons– recommends guidelines for correct patient, correct site, correct procedure 2003: TJC promotes Universal Protocol for preventing wrong site, wrong procedure, wrong person surgery 7
Background 1995 -2005: Wrong Site Surgery ranked #2 frequently reported sentinel event 1997: American Academy of Orthopedic surgeons-- initial operative site 2001: The North American Spine Surgery-- “Sign, Mark and Radiograph” 2002: American College of Surgeons– recommends guidelines for correct patient, correct site, correct procedure 2003: TJC promotes Universal Protocol for preventing wrong site, wrong procedure, wrong person surgery 7
 Implications Patient Family Surgeon Staff Hospital Safety/Medical Emotional Social/Trust Legal Cost 8
Implications Patient Family Surgeon Staff Hospital Safety/Medical Emotional Social/Trust Legal Cost 8
 Incidence of Wrong Site Surgery/Procedures Incidence (varies) 0. 09 to 4. 5 for every 10, 000 procedures 1 for every 27, 686 procedures 40 times a week 9
Incidence of Wrong Site Surgery/Procedures Incidence (varies) 0. 09 to 4. 5 for every 10, 000 procedures 1 for every 27, 686 procedures 40 times a week 9
 Specialties at Highest Risk Orthopedics Neurosurgery General Ophthalmology Anesthesia 10
Specialties at Highest Risk Orthopedics Neurosurgery General Ophthalmology Anesthesia 10
 Risk Factors Communication breakdown Inadequate safety checks Technology not utilized Competing demands/distractions Human error Patient characteristics Other 11
Risk Factors Communication breakdown Inadequate safety checks Technology not utilized Competing demands/distractions Human error Patient characteristics Other 11
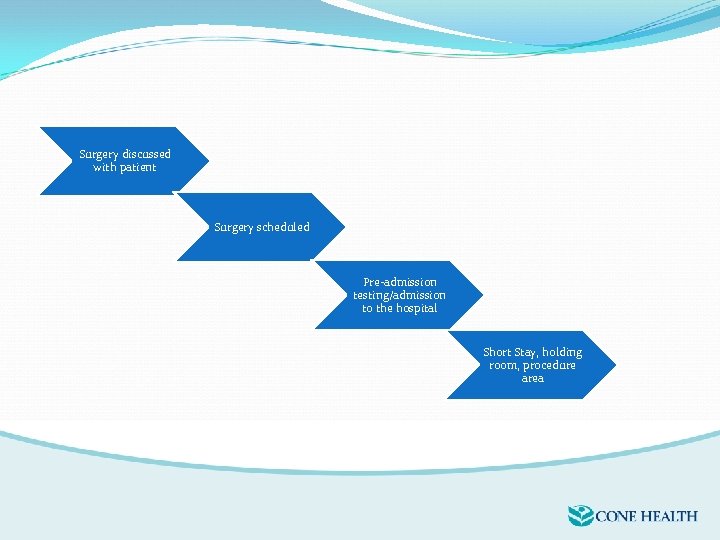 Surgery discussed with patient Surgery scheduled Pre-admission testing/admission to the hospital Short Stay, holding room, procedure area
Surgery discussed with patient Surgery scheduled Pre-admission testing/admission to the hospital Short Stay, holding room, procedure area
 Keys to Success Communication Engagement Standardization Education Mission Statement: We strive to be national leaders in providing exceptional, safe patient care through clear interprofessional communication and collaboration utilizing evidence based practice to standardize processes while maintaining fiscal responsibility. We are committed to providing the correct procedure to the correct patient at the correct site every time. Every patient, every time. 13
Keys to Success Communication Engagement Standardization Education Mission Statement: We strive to be national leaders in providing exceptional, safe patient care through clear interprofessional communication and collaboration utilizing evidence based practice to standardize processes while maintaining fiscal responsibility. We are committed to providing the correct procedure to the correct patient at the correct site every time. Every patient, every time. 13
 Small Group Work Reflecting on the incidence of wrong site procedure/surgery in your organization, what are your organizations risk category? What would be included in your mission statement? 14
Small Group Work Reflecting on the incidence of wrong site procedure/surgery in your organization, what are your organizations risk category? What would be included in your mission statement? 14
 Time to share your work 15
Time to share your work 15
 Cone Health Categories of error Scheduling error Process not followed Human error Communication error 16
Cone Health Categories of error Scheduling error Process not followed Human error Communication error 16
 It’s Okay to C. U. S
It’s Okay to C. U. S
 Objectives Discuss the importance of clear communication Define the acronym C. U. S. Discuss utilization of the C. U. S. model to share patient safety issues
Objectives Discuss the importance of clear communication Define the acronym C. U. S. Discuss utilization of the C. U. S. model to share patient safety issues
 C. U. S. Training “It’s okay to C. U. S” Attended North Carolina and Virginia (NOCVA) Safety Surgery Collaborative Training Utilized resources for staff in-services Created realistic scenarios staff could face
C. U. S. Training “It’s okay to C. U. S” Attended North Carolina and Virginia (NOCVA) Safety Surgery Collaborative Training Utilized resources for staff in-services Created realistic scenarios staff could face
 Importance of Communication Patient Safety! The Joint Commission has found that many times when sentinel events occur in the OR a member of the surgical team knew that the event was about to happen and they didn’t say anything.
Importance of Communication Patient Safety! The Joint Commission has found that many times when sentinel events occur in the OR a member of the surgical team knew that the event was about to happen and they didn’t say anything.
 Importance of Communication Patient Safety! Events that have happened because no one spoke up: Wrong Site Wrong Procedure Wrong Equipment Wrong/Missing Implant Wrong Medication/Allergy
Importance of Communication Patient Safety! Events that have happened because no one spoke up: Wrong Site Wrong Procedure Wrong Equipment Wrong/Missing Implant Wrong Medication/Allergy
 Why We Don’t Speak Up I’m afraid I’m embarrassed I’m stupid They will yell at me I might be wrong The phyisan is mean They won’t listen anyway It’s not that important
Why We Don’t Speak Up I’m afraid I’m embarrassed I’m stupid They will yell at me I might be wrong The phyisan is mean They won’t listen anyway It’s not that important
 C. U. S. Training C = Concern U = Uncomfortable S = Stop, this is a Safety Issue The power of articulating concern for patient safety
C. U. S. Training C = Concern U = Uncomfortable S = Stop, this is a Safety Issue The power of articulating concern for patient safety
 C. U. S. Training Interactive: divided into small groups Time for each group to discuss scenario “Dr. Fencl” enters to the room (remember, it is okay to C. U. S. )
C. U. S. Training Interactive: divided into small groups Time for each group to discuss scenario “Dr. Fencl” enters to the room (remember, it is okay to C. U. S. )
 C. U. S. Training Responses from each group Learning from each other Power of articulating your concern for patient safety
C. U. S. Training Responses from each group Learning from each other Power of articulating your concern for patient safety
 Importance of Clear Concise Communication “I’ll be right there”
Importance of Clear Concise Communication “I’ll be right there”
 Importance of Clear Concise Communication “On my way”
Importance of Clear Concise Communication “On my way”
 Importance of Clear Concise Communication “Give me a minute”
Importance of Clear Concise Communication “Give me a minute”
 Importance of Clear Concise Communication “Right now”
Importance of Clear Concise Communication “Right now”
 Importance of Clear Concise Communication “I’ll be right there” “On my way” “Give me a minute” “Right now”
Importance of Clear Concise Communication “I’ll be right there” “On my way” “Give me a minute” “Right now”
 Closed Loop Communication break-down Commonly lead to patient harm. They derive from: Lack of clarity A noisy and chaotic environment Failure to confirm that information was understood
Closed Loop Communication break-down Commonly lead to patient harm. They derive from: Lack of clarity A noisy and chaotic environment Failure to confirm that information was understood
 History of Closed Loop Communication Early voice radio communication Smoke signals and signal flags didn’t work anymore Every transmission required a reply No reply, you assumed that the message was not received, and you repeated it.
History of Closed Loop Communication Early voice radio communication Smoke signals and signal flags didn’t work anymore Every transmission required a reply No reply, you assumed that the message was not received, and you repeated it.
 Not Closed Loop Communication
Not Closed Loop Communication
 Closed Loop Communication: How It Works The sender initiates a message. 1. The receiver accepts the message, interprets it, and confirms what was communicated. 2. The sender verifies that the message was received. Derived from the Agency for Healthcare Research and Quality, Team. STEPPS
Closed Loop Communication: How It Works The sender initiates a message. 1. The receiver accepts the message, interprets it, and confirms what was communicated. 2. The sender verifies that the message was received. Derived from the Agency for Healthcare Research and Quality, Team. STEPPS
 Closed Loop Communication Who would like to volunteer?
Closed Loop Communication Who would like to volunteer?
 Implications of C. U. S. ing Powerful Communication to share with: OR Nursing Residents OR RN 3 -4 (clinical ladder) OR Shared Governance Endoscopy Outside the OR
Implications of C. U. S. ing Powerful Communication to share with: OR Nursing Residents OR RN 3 -4 (clinical ladder) OR Shared Governance Endoscopy Outside the OR
 Comments/Questions
Comments/Questions
 Six Sigma and Lean Principles 39
Six Sigma and Lean Principles 39
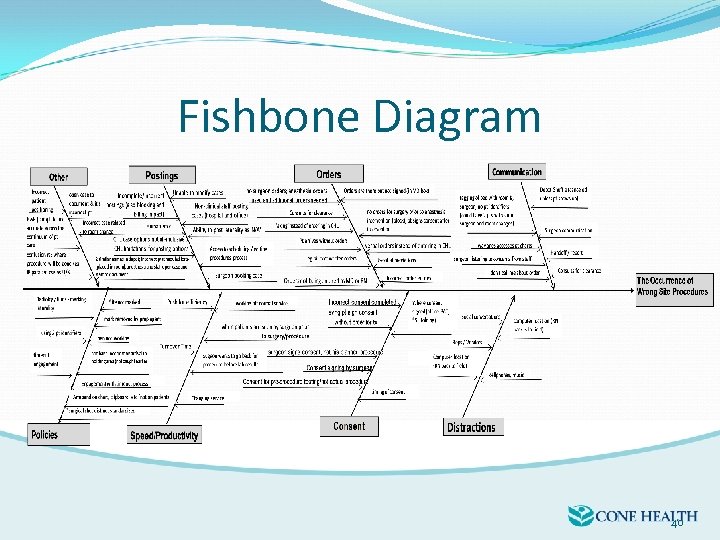 Fishbone Diagram 40
Fishbone Diagram 40
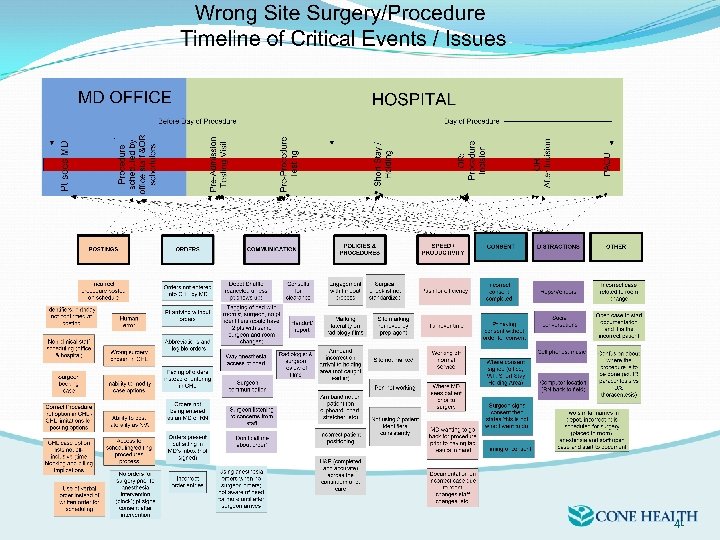 41
41
 Small Group Work Reflecting on the incidence of wrong site procedure/surgery in your organization, start a fishbone and timeline of critical events. 42
Small Group Work Reflecting on the incidence of wrong site procedure/surgery in your organization, start a fishbone and timeline of critical events. 42
 Time to share your work 43
Time to share your work 43
 Key Issues CHL Postings/Scheduling Orders Communication/Standardization Culture Surgical Check-list Policy and Procedures Distractions Competing Demands Pressure for efficiency vs safe patient care 44
Key Issues CHL Postings/Scheduling Orders Communication/Standardization Culture Surgical Check-list Policy and Procedures Distractions Competing Demands Pressure for efficiency vs safe patient care 44
 Outcomes Interprofessional Task Force Defining WSS Addressing Culture Creating Dashboard Standardization Policy and Procedure Time-Out Video Quarterly Newsletter Electronic Health Record Streamlining Orders Sharing Work http: //youtu. be/_e 37 xj. Boa 64 45
Outcomes Interprofessional Task Force Defining WSS Addressing Culture Creating Dashboard Standardization Policy and Procedure Time-Out Video Quarterly Newsletter Electronic Health Record Streamlining Orders Sharing Work http: //youtu. be/_e 37 xj. Boa 64 45
 Final Thoughts Previously stated our keys to success were: Communication Engagement Standardization Education What we learned……this is continuous work that requires a multidisciplinary approach and great effort. The final element is a vision for improvement. 46
Final Thoughts Previously stated our keys to success were: Communication Engagement Standardization Education What we learned……this is continuous work that requires a multidisciplinary approach and great effort. The final element is a vision for improvement. 46
 Executive Support Strategic vision Overcoming objections (surgeon objections) Challenges in community based system with an electronic health record (EMR) Technology/remote support Empowering the staff’s voice Cultural Relevance 47
Executive Support Strategic vision Overcoming objections (surgeon objections) Challenges in community based system with an electronic health record (EMR) Technology/remote support Empowering the staff’s voice Cultural Relevance 47
 Issue Prioritization Review the literature Define wrong site procedures Calculate our rate (over all and per specialty area) Data collection (categorize data) Create timeline of patient care and identify critical elements/competing demands Identify opportunities and action plans Observe timeline of patient care Create tools/risk assessments Implementation/Education 48
Issue Prioritization Review the literature Define wrong site procedures Calculate our rate (over all and per specialty area) Data collection (categorize data) Create timeline of patient care and identify critical elements/competing demands Identify opportunities and action plans Observe timeline of patient care Create tools/risk assessments Implementation/Education 48
 Prevention of Wrong Site Surgery/Procedure Southern Atlantic Healthcare Alliance OR Education Session
Prevention of Wrong Site Surgery/Procedure Southern Atlantic Healthcare Alliance OR Education Session


