28ff7c961352e3388873c675387c5fb1.ppt
- Количество слайдов: 40
Preventing Avoidable Hospitalizations: A Primer for Consumer Advocates November 3, 2016 Barbara Frank, B&F Consulting www. bandfconsultinginc. com
Why Reduce Avoidable Hospitalizations? • Because it is better to catch a condition in the early stages before it becomes acute • Because hospitals are not set up to take good care of our frail elders as well as nursing home can • Because when people have an acute condition and a hospitalization, they rarely recover to baseline. ©B&F Consulting 2016 www. bandfconsultinginc. com
OBRA 87 Requires each nursing home to provide care and services to: attain or maintain the highest practicable physical, mental, and psychosocial well-being of each resident ©B&F Consulting 2016 www. bandfconsultinginc. com
Highest Practicable = No “avoidable” decline Unavoidable = natural progression of a resident’s disease or condition ©B&F Consulting 2016 www. bandfconsultinginc. com
Highest Practicable = No “avoidable” decline Avoidable = Iatrogenic = We caused it “Genic” – Beginning/Cause “Iatro” – We ©B&F Consulting 2016 www. bandfconsultinginc. com
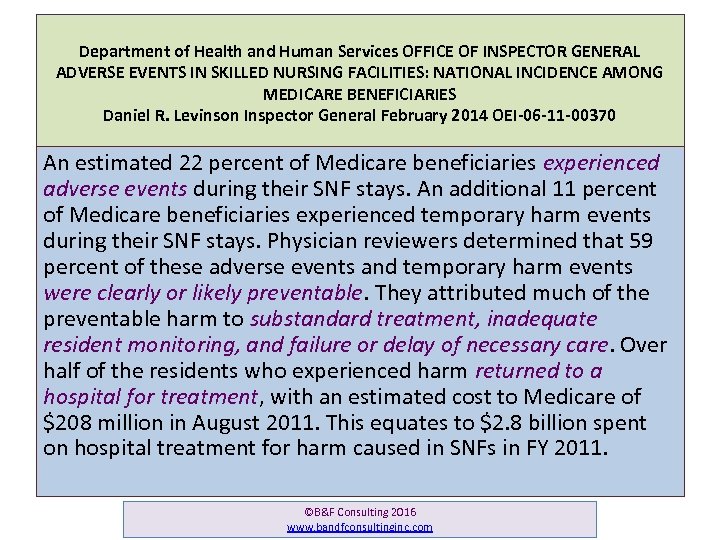
Department of Health and Human Services OFFICE OF INSPECTOR GENERAL ADVERSE EVENTS IN SKILLED NURSING FACILITIES: NATIONAL INCIDENCE AMONG MEDICARE BENEFICIARIES Daniel R. Levinson Inspector General February 2014 OEI-06 -11 -00370 An estimated 22 percent of Medicare beneficiaries experienced adverse events during their SNF stays. An additional 11 percent of Medicare beneficiaries experienced temporary harm events during their SNF stays. Physician reviewers determined that 59 percent of these adverse events and temporary harm events were clearly or likely preventable. They attributed much of the preventable harm to substandard treatment, inadequate resident monitoring, and failure or delay of necessary care. Over half of the residents who experienced harm returned to a hospital for treatment, with an estimated cost to Medicare of $208 million in August 2011. This equates to $2. 8 billion spent on hospital treatment for harm caused in SNFs in FY 2011. ©B&F Consulting 2016 www. bandfconsultinginc. com 6
Department of Health and Human Services OFFICE OF INSPECTOR GENERAL ADVERSE EVENTS IN SKILLED NURSING FACILITIES: NATIONAL INCIDENCE AMONG MEDICARE BENEFICIARIES Daniel R. Levinson Inspector General February 2014 OEI-06 -11 -00370 E L C Y E C M I T An estimated 22 percent of Medicare beneficiaries experienced adverse events during their SNF stays. An additional 11 percent of Medicare beneficiaries experienced temporary harm events during their SNF stays. Physician reviewers determined that 59 percent of these adverse events and temporary harm events were clearly or likely preventable. They attributed much of the preventable harm to substandard treatment, inadequate resident monitoring, and failure or delay of necessary care. Over half of the residents who experienced harm returned to a hospital for treatment, with an estimated cost to Medicare of $208 million in August 2011. This equates to $2. 8 billion spent on hospital treatment for harm caused in SNFs in FY 2011. ©B&F Consulting 2016 www. bandfconsultinginc. com 7
“Medicare continues its transformation from a passive payer to an effective purchaser of highquality, efficient care. ” Department of Health & Human Services Fiscal Year 2014 Budget in Brief Strengthening Health and Opportunity for All Americans http: //www. hhs. gov/budget ©B&F Consulting 2016 www. bandfconsultinginc. com
l “Medicare continues its e d payer o transformation from a passive M of highto an effective purchaser s g s n e quality, efficient care. ” i ng s a u. Department of Health & Human Services B ch e s Fiscal Year 2014 Budget in Brief h Strengtheningi. Health and Opportunity for All Americans T http: //www. hhs. gov/budget ©B&F Consulting 2015 www. bandfconsultinginc. com
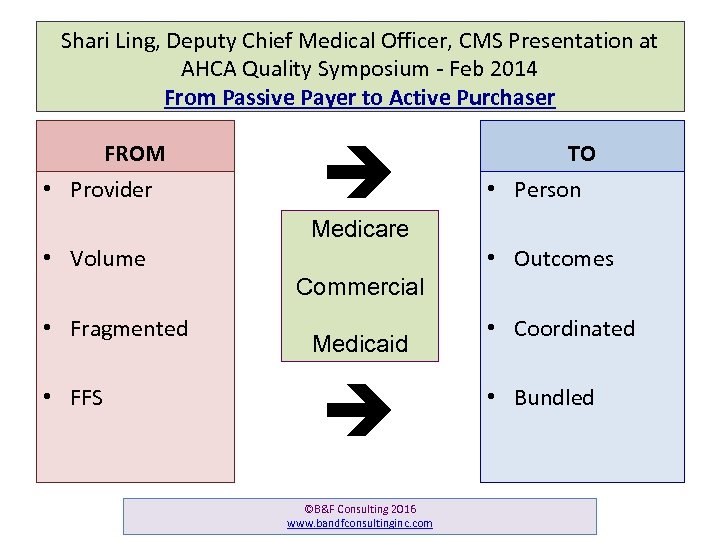
Shari Ling, Deputy Chief Medical Officer, CMS Presentation at AHCA Quality Symposium - Feb 2014 From Passive Payer to Active Purchaser FROM • Provider TO • Person Medicare • Volume • Fragmented • FFS Commercial Medicaid ©B&F Consulting 2016 www. bandfconsultinginc. com • Outcomes • Coordinated • Bundled
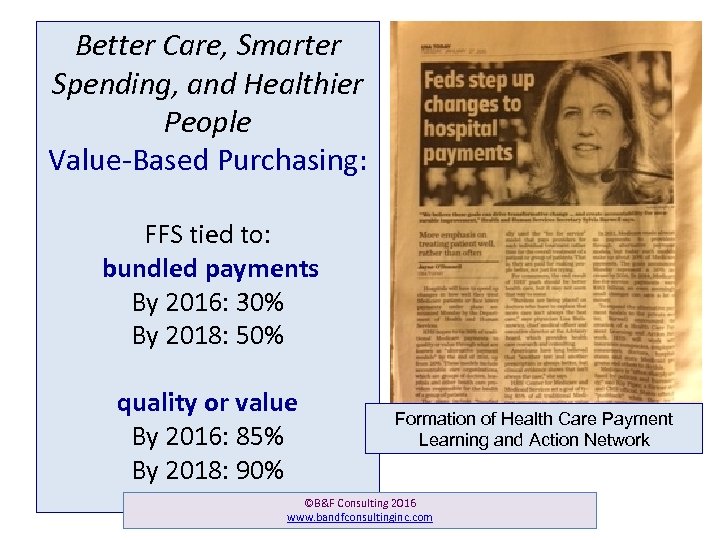
Better Care, Smarter Spending, and Healthier People Value-Based Purchasing: FFS tied to: bundled payments By 2016: 30% By 2018: 50% quality or value By 2016: 85% By 2018: 90% Formation of Health Care Payment Learning and Action Network ©B&F Consulting 2016 www. bandfconsultinginc. com

Using all the government’s levers to drive improvement CMS Nursing Home Convergence Group • • • Payment shift From Volume to Value Financial incentives to get it right for each resident Staffing related to Quality Preventing Avoidable Declines Quality Assurance & Performance Improvement ©B&F Consulting 2016 www. bandfconsultinginc. com
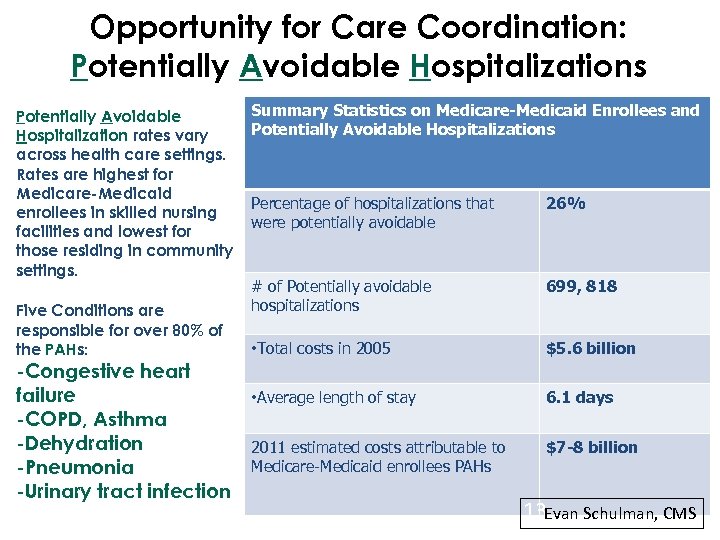
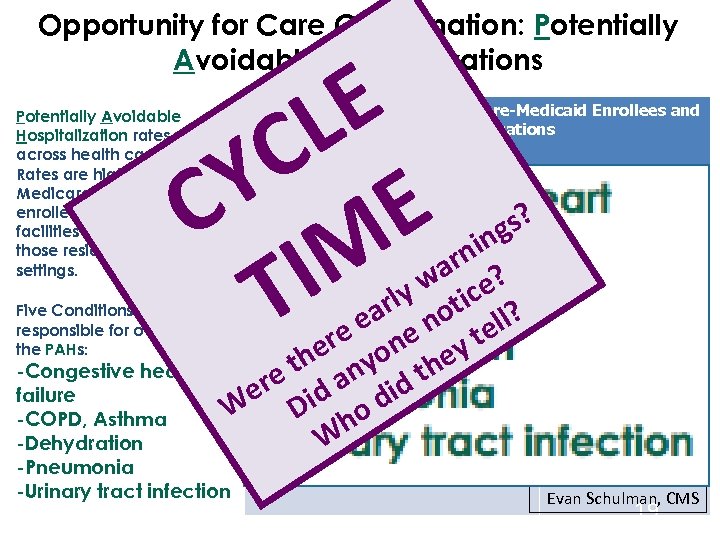
Opportunity for Care Coordination: Potentially Avoidable Hospitalizations Potentially Avoidable Hospitalization rates vary across health care settings. Rates are highest for Medicare-Medicaid enrollees in skilled nursing facilities and lowest for those residing in community settings. Five Conditions are responsible for over 80% of the PAHs: -Congestive heart failure -COPD, Asthma -Dehydration -Pneumonia -Urinary tract infection Summary Statistics on Medicare-Medicaid Enrollees and Potentially Avoidable Hospitalizations Percentage of hospitalizations that were potentially avoidable 26% # of Potentially avoidable hospitalizations 699, 818 • Total costs in 2005 $5. 6 billion • Average length of stay 6. 1 days 2011 estimated costs attributable to Medicare-Medicaid enrollees PAHs $7 -8 billion 13 Evan Schulman, CMS
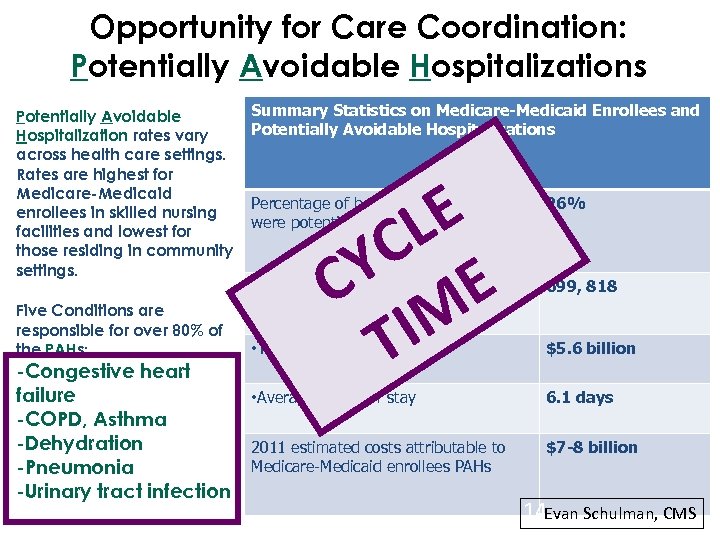
Opportunity for Care Coordination: Potentially Avoidable Hospitalizations Potentially Avoidable Hospitalization rates vary across health care settings. Rates are highest for Medicare-Medicaid enrollees in skilled nursing facilities and lowest for those residing in community settings. Five Conditions are responsible for over 80% of the PAHs: -Congestive heart failure -COPD, Asthma -Dehydration -Pneumonia -Urinary tract infection Summary Statistics on Medicare-Medicaid Enrollees and Potentially Avoidable Hospitalizations E L C Y E C M I T Percentage of hospitalizations that were potentially avoidable 26% # of Potentially avoidable hospitalizations 699, 818 • Total costs in 2005 $5. 6 billion • Average length of stay 6. 1 days 2011 estimated costs attributable to Medicare-Medicaid enrollees PAHs $7 -8 billion 14 Evan Schulman, CMS
For elders, these acute conditions manifest through subtle declines in daily function. Early warning signs need to be assessed and actively addressed right away. ©B&F Consulting 2016 www. bandfconsultinginc. com
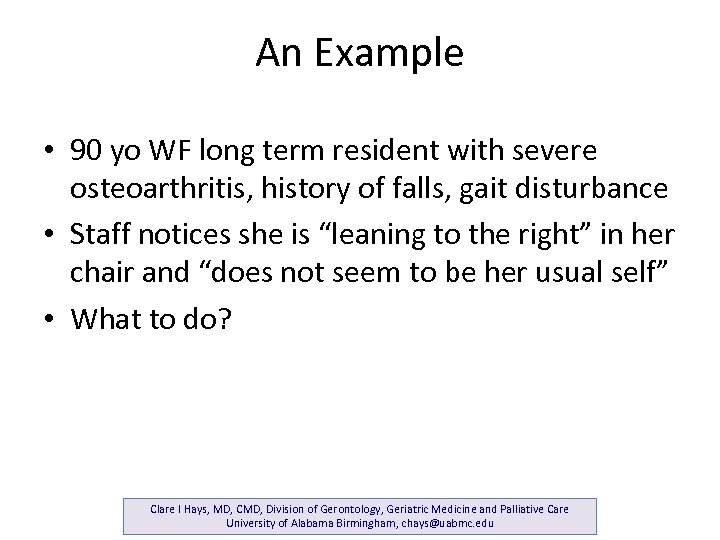
An Example • 90 yo WF long term resident with severe osteoarthritis, history of falls, gait disturbance • Staff notices she is “leaning to the right” in her chair and “does not seem to be her usual self” • What to do? Clare I Hays, MD, CMD, Division of Gerontology, Geriatric Medicine and Palliative Care University of Alabama Birmingham, chays@uabmc. edu
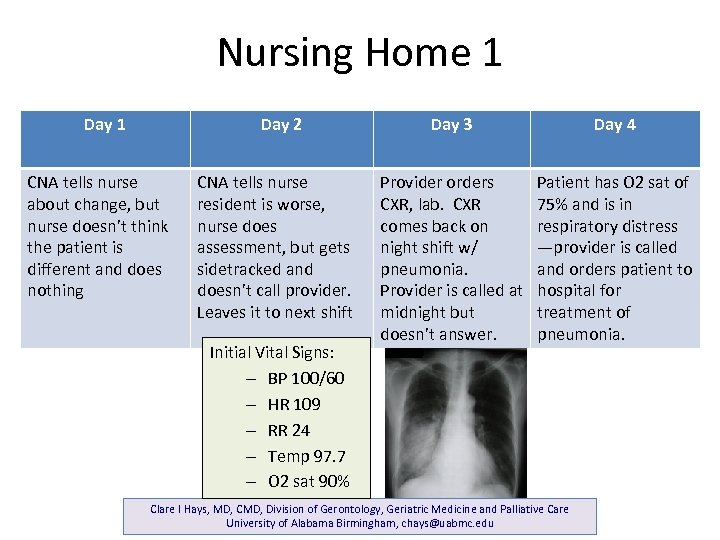
Nursing Home 1 Day 2 CNA tells nurse about change, but nurse doesn’t think the patient is different and does nothing CNA tells nurse resident is worse, nurse does assessment, but gets sidetracked and doesn’t call provider. Leaves it to next shift Initial Vital Signs: – BP 100/60 – HR 109 – RR 24 – Temp 97. 7 – O 2 sat 90% Day 3 Day 4 Provider orders CXR, lab. CXR comes back on night shift w/ pneumonia. Provider is called at midnight but doesn’t answer. Patient has O 2 sat of 75% and is in respiratory distress —provider is called and orders patient to hospital for treatment of pneumonia. Clare I Hays, MD, CMD, Division of Gerontology, Geriatric Medicine and Palliative Care University of Alabama Birmingham, chays@uabmc. edu
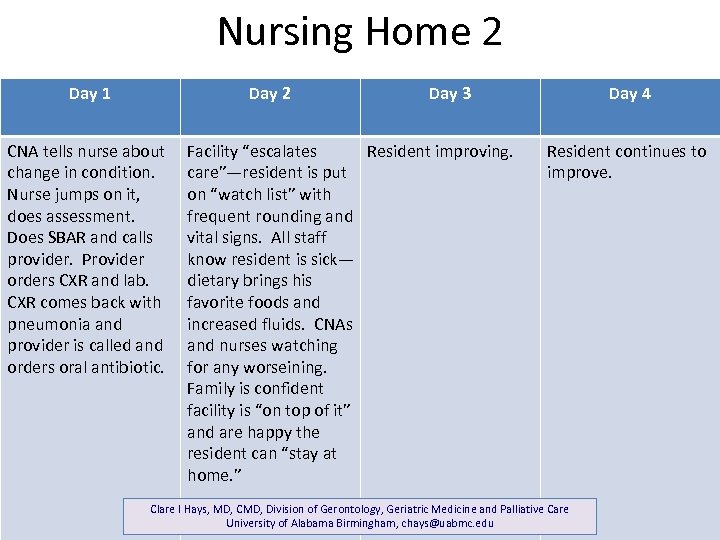
Nursing Home 2 Day 1 Day 2 CNA tells nurse about change in condition. Nurse jumps on it, does assessment. Does SBAR and calls provider. Provider orders CXR and lab. CXR comes back with pneumonia and provider is called and orders oral antibiotic. Day 3 Facility “escalates Resident improving. care”—resident is put on “watch list” with frequent rounding and vital signs. All staff know resident is sick— dietary brings his favorite foods and increased fluids. CNAs and nurses watching for any worseining. Family is confident facility is “on top of it” and are happy the resident can “stay at home. ” Day 4 Resident continues to improve. Clare I Hays, MD, CMD, Division of Gerontology, Geriatric Medicine and Palliative Care University of Alabama Birmingham, chays@uabmc. edu
Opportunity for Care Coordination: Potentially Avoidable Hospitalizations E L C Y E C M I T Potentially Avoidable Hospitalization rates vary across health care settings. Rates are highest for Medicare-Medicaid enrollees in skilled nursing facilities and lowest for those residing in community settings. Summary Statistics on Medicare-Medicaid Enrollees and Potentially Avoidable Hospitalizations Percentage of hospitalizations that were potentially avoidable s? g nin ar ? # of Potentially avoidable y w tice hospitalizations rl o Five Conditions are ea e n tell? responsible for over 80% of • Total costsrin 2005 n the PAHs: e e yo ey h n -Congestive heart e t a id th failure er id ofd • Average length stay W D ho -COPD, Asthma W -Dehydration 2011 estimated costs attributable to -Pneumonia -Urinary tract infection Medicare-Medicaid enrollees PAHs 26% 699, 818 $5. 6 billion 6. 1 days $7 -8 billion Evan Schulman, CMS 19
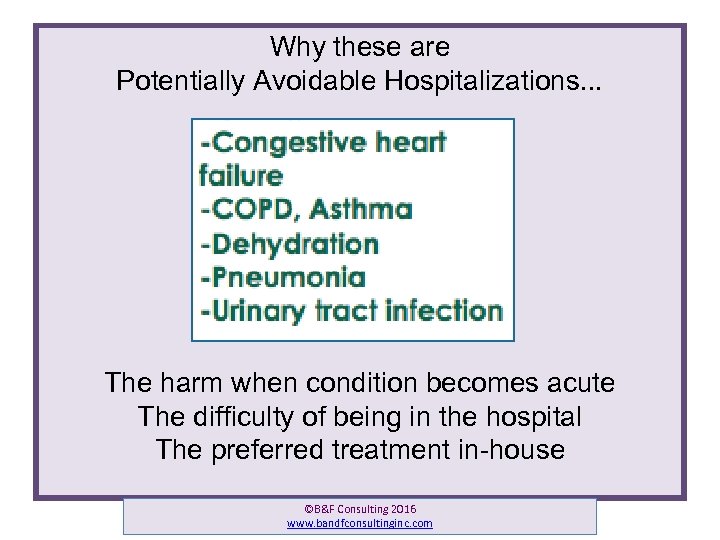
Why these are Potentially Avoidable Hospitalizations. . . The harm when condition becomes acute The difficulty of being in the hospital The preferred treatment in-house ©B&F Consulting 2016 www. bandfconsultinginc. com
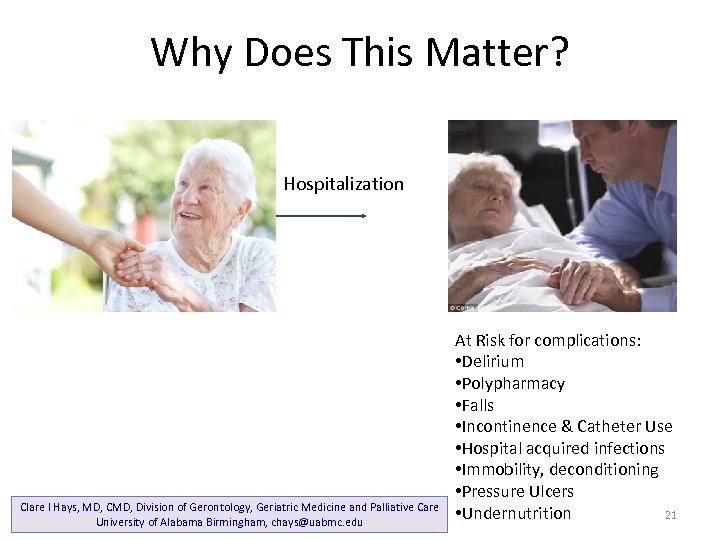
Why Does This Matter? Hospitalization Clare I Hays, MD, CMD, Division of Gerontology, Geriatric Medicine and Palliative Care University of Alabama Birmingham, chays@uabmc. edu At Risk for complications: • Delirium • Polypharmacy • Falls • Incontinence & Catheter Use • Hospital acquired infections • Immobility, deconditioning • Pressure Ulcers • Undernutrition 21
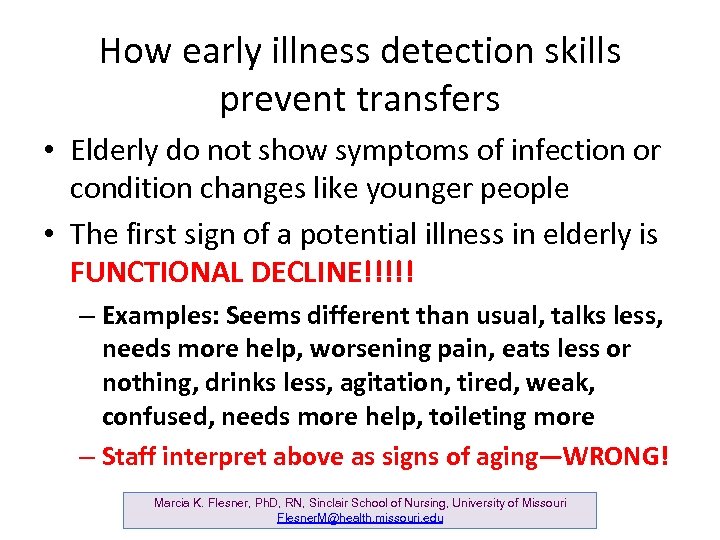
How early illness detection skills prevent transfers • Elderly do not show symptoms of infection or condition changes like younger people • The first sign of a potential illness in elderly is FUNCTIONAL DECLINE!!!!! – Examples: Seems different than usual, talks less, needs more help, worsening pain, eats less or nothing, drinks less, agitation, tired, weak, confused, needs more help, toileting more – Staff interpret above as signs of aging—WRONG! Marcia K. Flesner, Ph. D, RN, Sinclair School of Nursing, University of Missouri Flesner. M@health. missouri. edu
www. interact 2. net Clare I Hays, MD, CMD, Division of Gerontology, Geriatric Medicine and Palliative Care University of Alabama Birmingham, chays@uabmc. edu 23
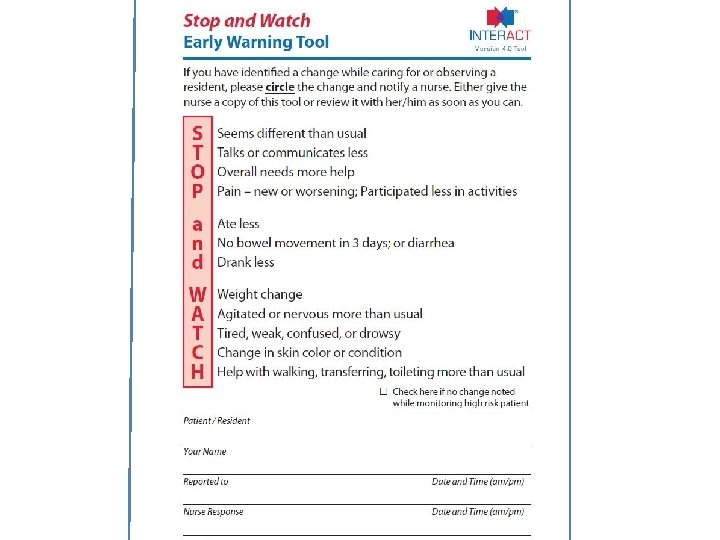
Stop and Watch • To guide direct care staff through a brief review of early changes in resident’s condition. • To improve communication between frontline staff and the nurse in charge about early changes in condition. Clare I Hays, MD, CMD, Division of Gerontology, Geriatric Medicine and Palliative Care University of Alabama Birmingham, chays@uabmc. edu 24
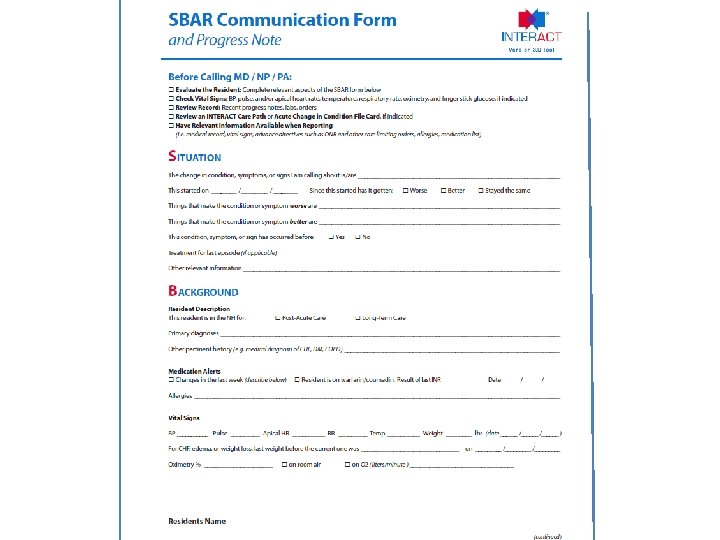
When functional decline occurs • Make the mistake of monitoring resident • Resident needs to be assessed by an RN or APRN using the SBAR tool • A plan needs to be made on what action should take place—lab or x-ray, increased hydration (oral, IV or Sub-Q), increase VS monitoring, notify practitioner • USE THE SBAR TOOL Marcia K. Flesner, Ph. D, RN, Sinclair School of Nursing, University of Missouri Flesner. M@health. missouri. edu
Lessons Learned • Nursing Homes need SYSTEMS for early identification and communication of acute changes in condition (INTERACT or similar) • Requires nursing and administrative leadership • Teamwork essential—we can no longer work in silos • Must have consistent assignment/know the residents Clare I Hays, MD, CMD, Division of Gerontology, Geriatric Medicine and Palliative Care University of Alabama Birmingham, chays@uabmc. edu 28
Focus on New Admissions n High risk in first 24 – 72 hours q q q n Frontload your interventions Individualize – customary routines Risk of readmission declines each day Know who is critically ill q Everyone focus on high risk and new admits David Farrell, LNHA, MSW dfarrell@telecarecorp. com 29
When functional decline occurs • ASSUME RESIDENT IS DEHYDRATED because they probably are. • Research has shown that increased fluids can address developing infection (pneumonia, UTI) without use of antibiotics • Homes need hydration carts, not just an ice cart, and need strong emphasis on helping residents to hydrate Marcia K. Flesner, Ph. D, RN, Sinclair School of Nursing, University of Missouri Flesner. M@health. missouri. edu
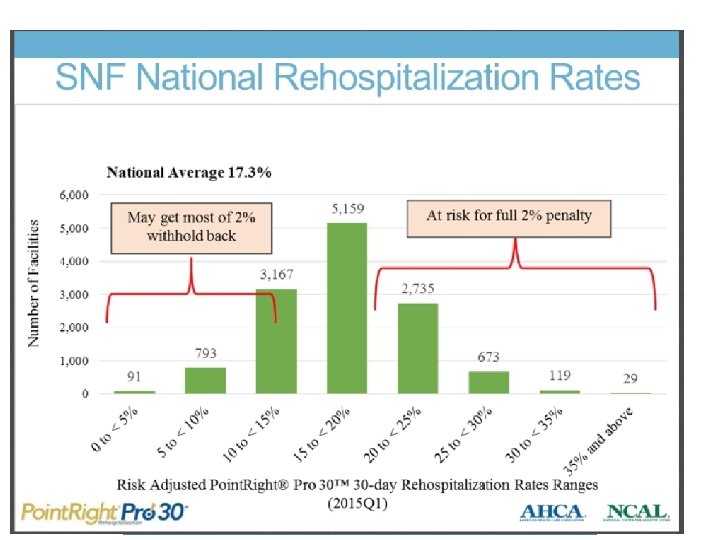
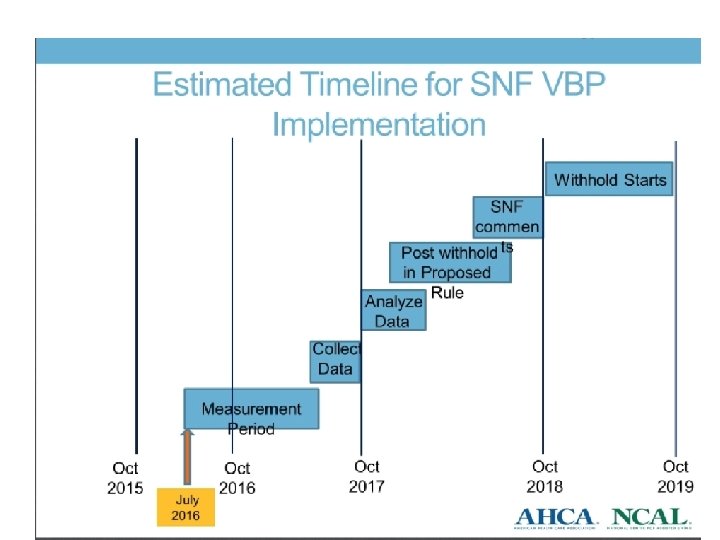
Currently Hospitals are paying a penalty for re-hospitalizations, and evaluating which nursing homes to work with. 5 Star now includes re-hospitalizations. In 2018, nursing homes’ penalty for re-hospitalizations will begin. Eventually This will extend to avoidable hospitalizations of long-stay residents. ©B&F Consulting 2016 www. bandfconsultinginc. com 31
How does this fit with what you are seeing in your nursing homes? ©B&F Consulting 2016 www. bandfconsultinginc. com
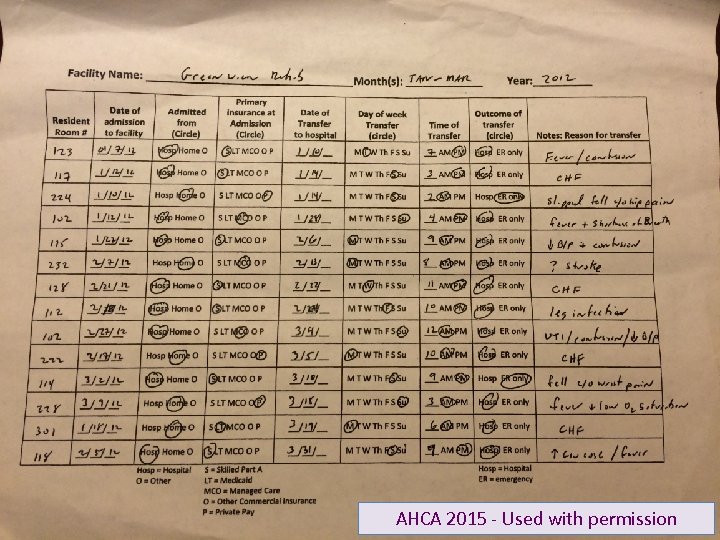
Examining hospital readmissions ©B&F Consulting 2015 www. bandfconsultinginc. com 33 AHCA 2015 - Used with permission
Discuss: 1. 2. 3. 4. 5. Room/Hall Length of Stay Day of Week Time of Day Condition Why step back and look like this? ©B&F Consulting 2016 www. bandfconsultinginc. com 34
©B&F Consulting 2016 www. bandfconsultinginc. com 35
©B&F Consulting 2016 www. bandfconsultinginc. com 36
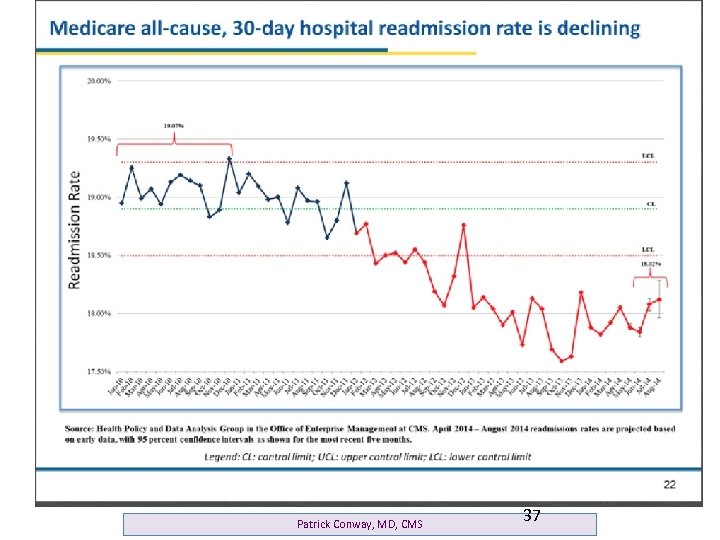
Patrick Conway, MD, CMS 37
Preventing Avoidable Declines What’s your cycle time from the first notice that someone isn’t themselves to effective action? Do this as a QI Exercise with your management team where you Map your current process ©B&F Consulting 2016 www. bandfconsultinginc. com
From 24 Hour Report to Watch List From Conference Room to Rounding ©B&F Consulting 2015 www. bandfconsultinginc. com 39
Contact Information Barbara Frank, B&F Consulting bfrank 1020@aol. com www. bandfconsultinginc. com ©B&F Consulting 2016 www. bandfconsultinginc. com
28ff7c961352e3388873c675387c5fb1.ppt