c76941e9d1793137d88ed0bb11a453c1.ppt
- Количество слайдов: 74
PRETERM LABOR Resident School 8/3/16 Mary Beth Sutter
Learning Objectives Understand importance of preterm birth Identify who is at risk and review prevention options Understand prompt management of initial presentation Review management of preterm premature rupture of membranes
Epidemiology Definition: Contractions causing cervical change before 37 weeks A major public health problem and focus of research 9. 6% of births in 2015 20% increase since 1990, mostly late preterm 34 -36 wk In New Mexico, 9. 2% of births in 2015 35% of all US healthcare dollars spent on infants Sayres W. Preterm Labor American Family Physician 2010; 81: 477 -484. 2012 NM Kids Count Factbook, Preterm Births ACOG Practice Bulletin 127, June 2012. Management of Preterm Labor
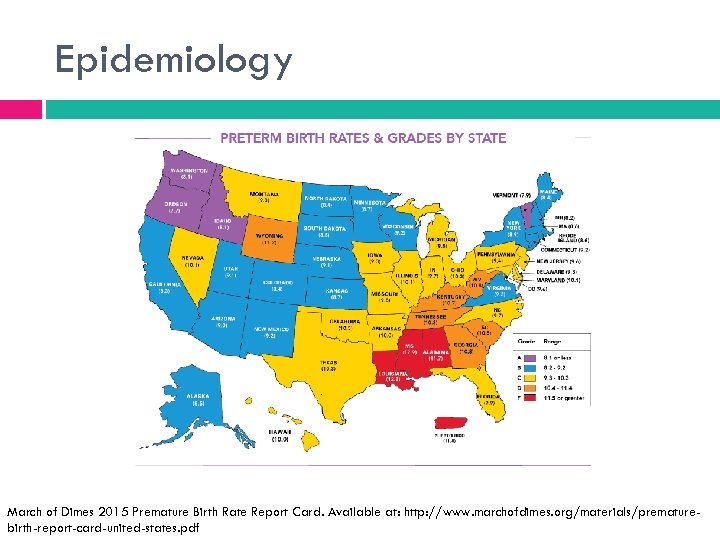
Epidemiology March of Dimes 2015 Premature Birth Rate Report Card. Available at: http: //www. marchofdimes. org/materials/prematurebirth-report-card-united-states. pdf
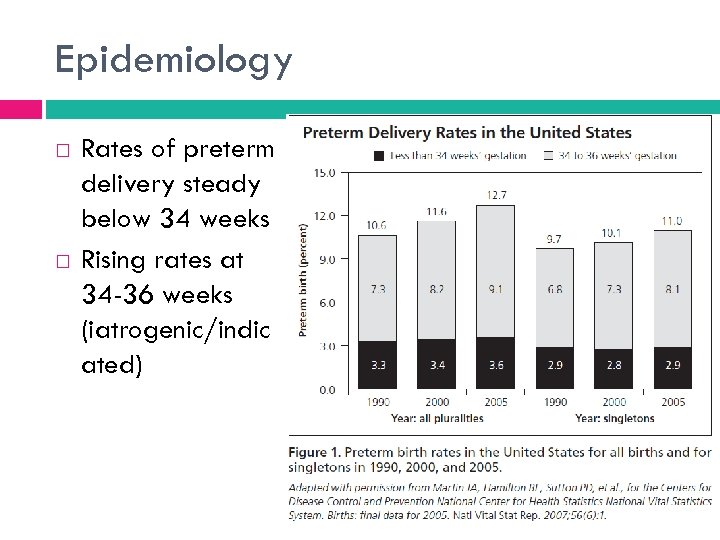
Epidemiology Rates of preterm delivery steady below 34 weeks Rising rates at 34 -36 weeks (iatrogenic/indic ated)
Epidemiology ½ cases are spontaneous labor without ROM ¼ are PPROM ¼ are iatrogenic/ indicated Sayres W. Preterm Labor American Family Physician 2010; 81: 477 -484.
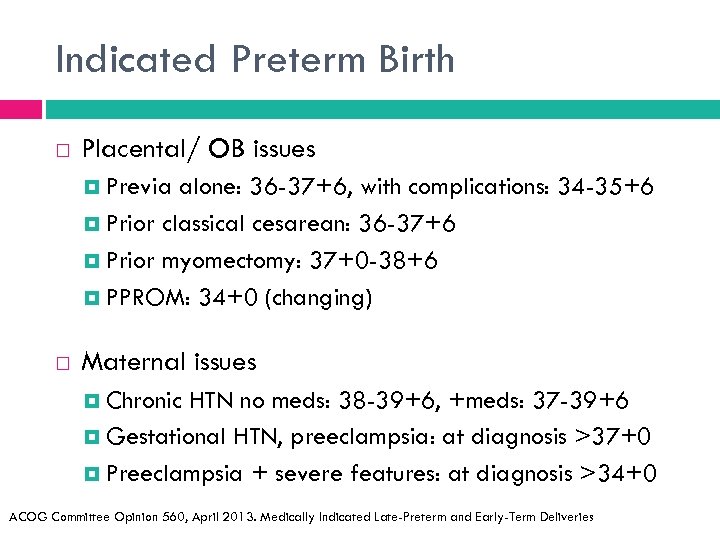
Indicated Preterm Birth Placental/ OB issues Previa alone: 36 -37+6, with complications: 34 -35+6 Prior classical cesarean: 36 -37+6 Prior myomectomy: 37+0 -38+6 PPROM: 34+0 (changing) Maternal issues Chronic HTN no meds: 38 -39+6, +meds: 37 -39+6 Gestational HTN, preeclampsia: at diagnosis >37+0 Preeclampsia + severe features: at diagnosis >34+0 ACOG Committee Opinion 560, April 2013. Medically Indicated Late-Preterm and Early-Term Deliveries
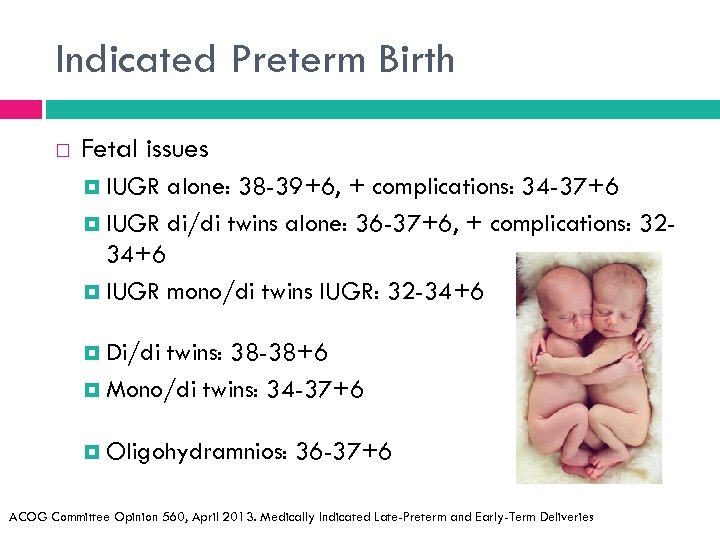
Indicated Preterm Birth Fetal issues IUGR alone: 38 -39+6, + complications: 34 -37+6 IUGR di/di twins alone: 36 -37+6, + complications: 3234+6 IUGR mono/di twins IUGR: 32 -34+6 Di/di twins: 38 -38+6 Mono/di twins: 34 -37+6 Oligohydramnios: 36 -37+6 ACOG Committee Opinion 560, April 2013. Medically Indicated Late-Preterm and Early-Term Deliveries
Risk Factors Maternal Characteristics 1 Race African American > Hispanic > White non-Hispanic Short interpregnancy interval (<6 mo) Physical or mental stress BMI <19 Delayed first pregnancy Use of reproductive assisted technology Previous preterm delivery Sayres W. Preterm Labor American Family Physician 2010; 81: 477 -484.
Risk Factors Pregnancy Characteristics 1 BV or chlamydia infection Other intrauterine infection Other systemic infection (pyelo, appendicitis, PNA) Cocaine, heroin, tobacco use Hx of cervical cone biopsy or LEEP Short cervix (<2. 5 cm) Maternal medical problems (DM, thyroid, HTN disorders) Multiple gestation Uterine anomalies Placental abruption or placenta previa Sayres W. Preterm Labor American Family Physician 2010; 81: 477 -484.
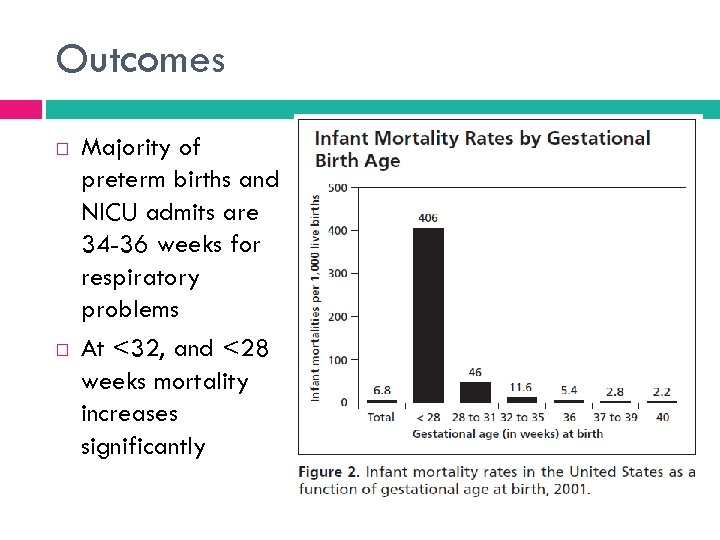
Outcomes Majority of preterm births and NICU admits are 34 -36 weeks for respiratory problems At <32, and <28 weeks mortality increases significantly
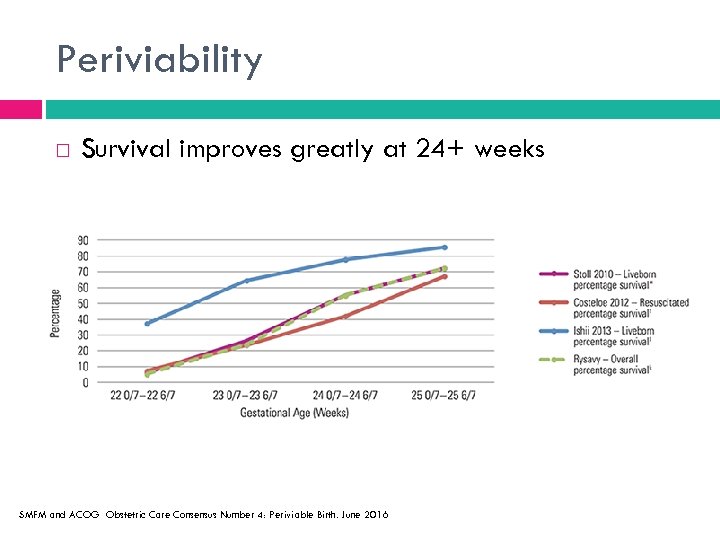
Periviability Survival improves greatly at 24+ weeks SMFM and ACOG Obstetric Care Consensus Number 4: Periviable Birth. June 2016
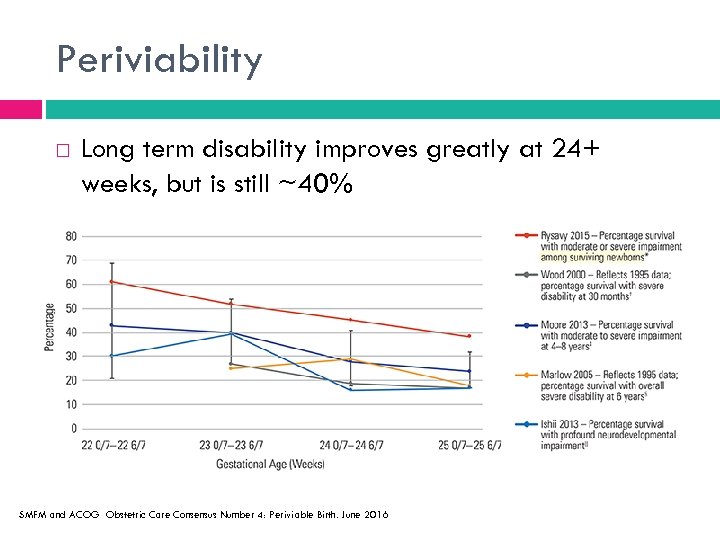
Periviability Long term disability improves greatly at 24+ weeks, but is still ~40% SMFM and ACOG Obstetric Care Consensus Number 4: Periviable Birth. June 2016
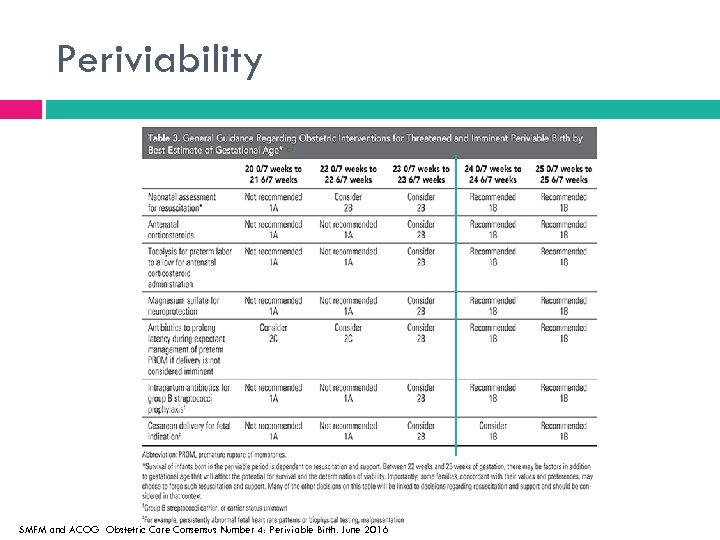
Periviability SMFM and ACOG Obstetric Care Consensus Number 4: Periviable Birth. June 2016
Prevention So many causes- difficult to prevent Smoking cessation programs successful Tx for asymptomatic bacteruria successful Screening and treatment for BV controversial USPSTF- Insufficient evidence to screen or treat If someone has symptomatic BV, oral clinda or metronidazole should be used to tx Sayres W. Preterm Labor American Family Physician 2010; 81: 477 -484.
Prevention Progesterone! Evidence became overwhelming necessitating position statements by ACOG and SMFM in 2012
Prevention Prior spontaneous preterm birth (<37 weeks) Weekly IM 17 -hydroxy progesterone Initiated between 16 -24 weeks, until 36 weeks Cervical length q 2 weeks from 18 -24 wks CL <25 mm, consider cerclage Iams J. Identification of candidates for progesterone. Obstet Gynecol 2014; 123: 1317 -1326
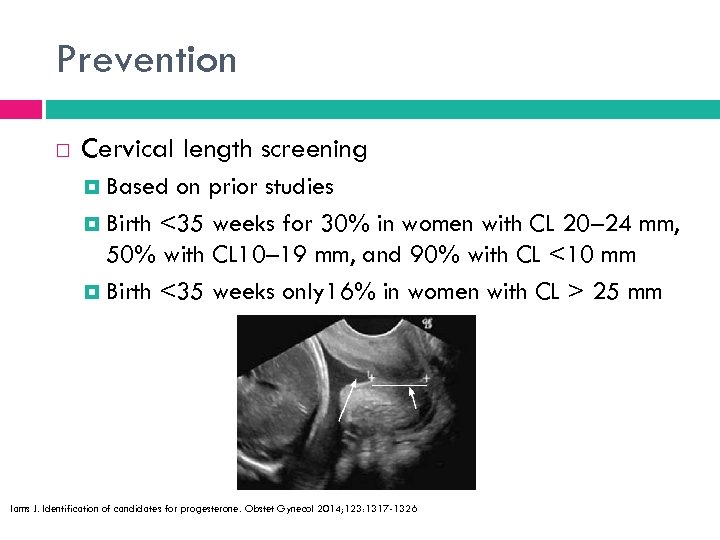
Prevention Cervical length screening Based on prior studies Birth <35 weeks for 30% in women with CL 20– 24 mm, 50% with CL 10– 19 mm, and 90% with CL <10 mm Birth <35 weeks only 16% in women with CL > 25 mm Iams J. Identification of candidates for progesterone. Obstet Gynecol 2014; 123: 1317 -1326
Prevention Routine cervical length screening, no hx preterm birth Site specific Selective based on risk factors Universal transabdominal at 18 -24 wks Universal transvaginal at 18 -24 wks Iams J. Identification of candidates for progesterone. Obstet Gynecol 2014; 123: 1317 -1326 ★
Prevention Vaginal progesterone For short cervix <20 mm with no prior preterm birth 200 mg suppositories, tabs, or gel (compounded by Highland, Prometrium, Crinone) After identification until 36 weeks Iams J. Identification of candidates for progesterone. Obstet Gynecol 2014; 123: 1317 -1326
Prevention OPPTIMUM Recent multicenter randomized double-blind trial 1197 women Vaginal progesterone nightly at 18 -22 weeks No benefit for prevention of preterm birth <34 weeks No benefit for neonatal composite outcome (death, brain injury, bronchopulmonary dysplasia) No difference in childhood cognitive score at 2 years Included both women with prior PTB or short cervix Norman et al. Vaginal progesterone prophylaxis for preterm birth (the OPPTIMUM stydy): a multicentre, randomised, double-blind trial. Lnacet 2016; 387: 2106 -16.
Prevention FOR Progesterone deficiency does not make scientific sense Many issues with quality of past studies This is the first high quality large study to go to 2 years old Time to study something else for preterm birth prevention AGAINST Randomization at 18 -22 weeks- too late? Reduced neonatal death Reduced neonatal brain injury Only 256 women in short cervix subset (>400 in other RCT’s) Prior M, and Thornton JG. Progesterone has no place in the prevention of preterm delivery: FOR: it is time to study something else. BJOG. 2016; 123. Eichelberger KY and Manuck TA. Progesterone has no place in the prevention of preterm delivery: AGAINST: A call for a measured response to the OPPTIMUM trial. BJOG. 2016; 123.
Prevention Guidelines only apply to singleton pregnancies Some evidence of harm in twins If preterm labor seems likely progesterone should still be continued No role for cerclage in women with very short cervix with no prior preterm birth history Iams J. Identification of candidates for progesterone. Obstet Gynecol 2014; 123: 1317 -1326
Meanwhile in clinic…
Case 1 New OB visit for a 25 yo G 0101 at 16+0 with prior spontaneous preterm birth at 28 weeks What should she be offered and when?
Case 1 IM progesterone to start at 16 weeks until 36 weeks Cervical length screening starting at 18 -20 weeks q 2 weeks until 24 weeks You are paged when she is 20 weeks from New Mexico Sono- cervical length is 1. 8 cm! What do you do?
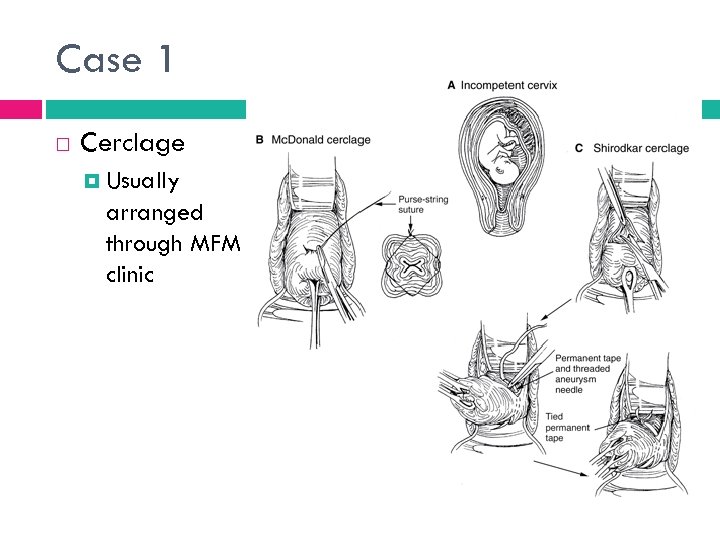
Case 1 Cerclage Usually arranged through MFM clinic
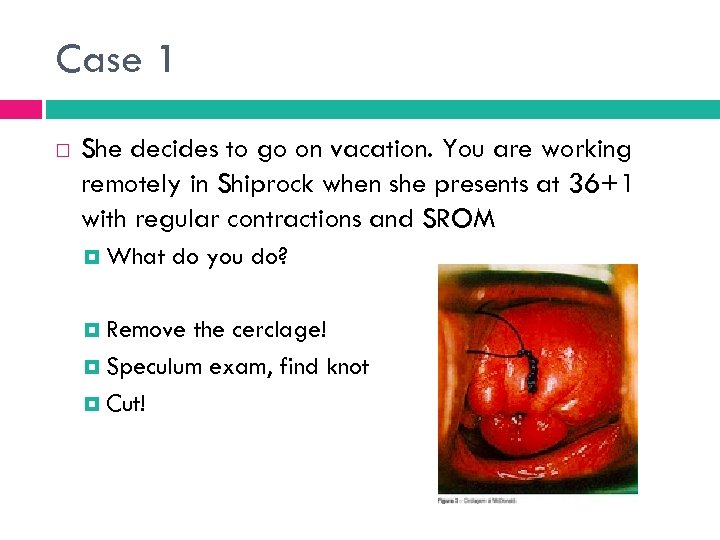
Case 1 She decides to go on vacation. You are working remotely in Shiprock when she presents at 36+1 with regular contractions and SROM What do you do? Remove the cerclage! Speculum exam, find knot Cut!
Case 2 30 yo G 1 P 0 currently at 20 weeks, found to have cervical length of 12 mm on routine screening What should she be offered and when?
Case 2 Vaginal progesterone Rx Eval for signs/symptoms of preterm labor Consider steroids Recheck cervical length in 7 days Is she a candidate for cerclage? Current ACOG consensus is no
Diagnosis Only 30 -60% of women presenting with preterm labor will lead to a preterm birth 4 main areas of concern that make a difference in survival of infant Transfer to hospital with NICU capabilities GBS prophylaxis Administration of steroids Magnesium for neuroprotection Sayres W. Preterm Labor American Family Physician 2010; 81: 477 -484. ACOG Practice Bulletin 127, June 2012. Management of Preterm Labor
Diagnosis Page from OBT: “ 30 weeker contracting” Assess patient as soon as you can Involve attending early Determine dates Earliest US most accurate What are her risk factors? Detailed H+P Sayres W. Preterm Labor American Family Physician 2010; 81: 477 -484.
Diagnosis Are the membranes ruptured? Pooling, ferning, nitrazine US for amniotic fluid index if unsure Is an infection present? GBS, STD amp (gc/c) and wet prep UA and urine culture Is the patient in labor? Regular contractions? Cervical dilation? Sayres W. Preterm Labor American Family Physician 2010; 81: 477 -484.
Diagnosis What is the likelihood she will deliver preterm? Fetal fibronectin (FFN)- 24+0 to 33+6 weeks Negative predictive value 99% for delivery within 14 days Positive predictive value 13 -30% for delivery in 7 -10 days Can only be done if NOTHING in vagina in past 24 hours False positives with amniotic fluid, blood, vaginal infection Collect FIRST on your speculum exam Talk to attending prior to sending test FFN should not replace clinical judgement Sayres W. Preterm Labor American Family Physician 2010; 81: 477 -484. ; 3. ACOG Practice Bulletin 127, June 2012. Management of Preterm Labor
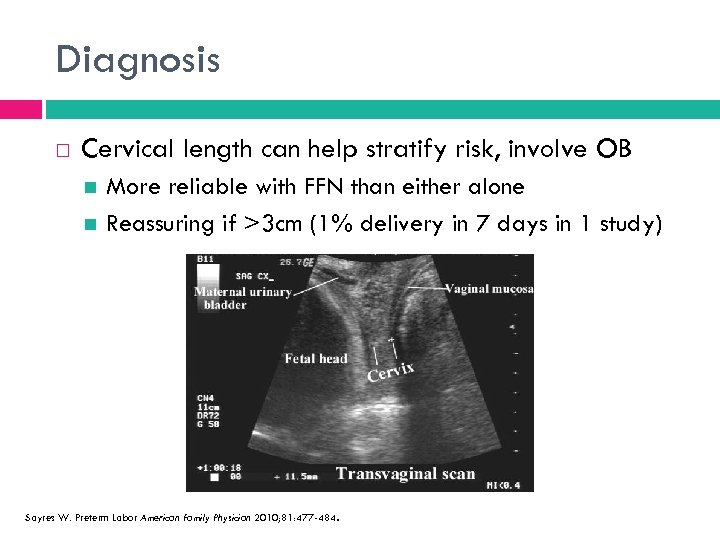
Diagnosis Cervical length can help stratify risk, involve OB More reliable with FFN than either alone Reassuring if >3 cm (1% delivery in 7 days in 1 study) Sayres W. Preterm Labor American Family Physician 2010; 81: 477 -484.
Initial management at UNM Sterile speculum exam Obtain FFN (+/- send it) Check for pool/fern/nitrazine Check for possible infection (wet mount, STDamp, regular GBS cx) Visualize cervical dilation Digital cervical exam by senior or attending if not ruptured UA and UDATR drug screen NST and toco monitoring Consider fluids
Who to treat? 30% of preterm labor resolves spontaneously 50% of patient hospitalized for PTL birth at term Intervention must benefit baby Must be viable, prolonging pregnancy better than not Premature onset of contractions without cervical change “POOC” Only 18% deliver before 37 weeks Only 3% deliver within 2 weeks of triage visit for ctx ACOG Practice Bulletin 127, June 2012. Management of Preterm Labor
Steroids Single course 24 -34 wks at risk for delivery in 7 days Betamethasone 12 mg IM q 24 hrs x 2 doses Dexamethasone 6 mg IM q 12 hrs x 4 doses Improves neonatal outcomes Decreases: Mortality Incidence and severity of RDS Intraventricular hemorrhage Necrotizing enterocolitis Sayres W. Preterm Labor American Family Physician 2010; 81: 477 -484; 3. ACOG Practice Bulletin 127, June 2012. Management of Preterm Labor Roberts D et al. Antenatal corticosteroids for women at risk of preterm birth. Cochrane Database 2006, Issue 3. Mc. Kinlay CJ, et al. Repeat antenatal glucocorticoids for women at risk of preterm birth: a Cochrane Systemic Review. American Journal of Obstetrics and Gynecology. 2012; 187 -194.
Steroids Cochrane Review 2012 - repeat single course >7 days after initial course “Rescue steroids” Further reduces RDS without adverse outcomes Should be reserved for imminent delivery No evidence for multiple repeat courses No evidence for initial “accelerated course” in imminent birth Sayres W. Preterm Labor American Family Physician 2010; 81: 477 -484; 3. ACOG Practice Bulletin 127, June 2012. Management of Preterm Labor Roberts D et al. Antenatal corticosteroids for women at risk of preterm birth. Cochrane Database 2006, Issue 3. Mc. Kinlay CJ, et al. Repeat antenatal glucocorticoids for women at risk of preterm birth: a Cochrane Systemic Review. American Journal of Obstetrics and Gynecology. 2012; 187 -194.
Late Preterm Steroids 2016 multicenter randomized trial 2827 women 34+0 to 36+5 at risk for delivery Primary outcome (neonatal composite of CPAP for 2+ hours, O 2 with Fi. O 2 at least 0. 30 for 4+ hours, ECMO, or mechanical ventilation, stillbirth, neonatal death in first 72 hrs) less in betamethasone group (11. 6% vs 14. 4%) No differences in chorio or neonatal sepsis Hypoglycemia more common in betamethasone group (RR 1. 60) Gyamfi-Bannerman C. et al. Antenatal betamethasone for women at risk for late preterm delivery. NEJM 2016; 374: 1311 -1320.
Late Preterm Steroids UNM protocol ACS for women with indicated preterm delivery 34+036+6 Betamethasone 2 doses, 12 mg IM, 24 hrs apart Indications such as: hypertensive disorders, abnormal placentation, PPROM, IUGR ACS for women with preterm labor (cervical dilation 3 cm, or effacement >75%) up until 35+6 weeks
Late Preterm Steroids UNM protocol continued No tocolytics in late preterm period No ACS until a definitive delivery plan is made Follow standard of care for hypoglycemia in late preterm babies No ACS for unstudied conditions: Any prior steroids Twins reduced to singleton after 14 weeks Known major fetal anomalies Maternal contraindications to betamethasone Pre-gestational diabetes Chorioamnionitis Gyamfi-Bannerman C. et al. Antenatal betamethasone for women at risk for late preterm delivery. NEJM 2016; 374: 1311 -1320.
Magnesium Administer when birth is anticipated <32 weeks Mg. SO 4 reduces severity and risk of cerebral palsy when given for neuroprotection in 3 meta-analyses No evidence for any specific regimen UNM 4 g loading dose, then 1 g/hr infusion No evidence for pregnancy prolongation Serious maternal complications rare Usually reserved for imminent birth Doyle et al. Magnesium sulphate for women at risk of preterm birth for neuroprotection of the fetus. Cochrane Database 2009 Costantine MM et al. Effects of antenatal exposure to magnesium sulfate on neuroprotection and mortality in preterm infants. NICHD MFM Units Network Obstet Gynecol 2009; 114: 354 -364. Magnesium sulfate before anticipated preterm birth for neuroprotection. ACOG Committee Opinon 455. ACOG and SMFM.
Tocolytics Used to allow time to give steroids and magnesium, arrange transport if needed Contraindications: Pre-viability IUFD Lethal anomaly Nonreassuring fetal status Chorioamnionitis Sayres W. Preterm Labor American Family Physician 2010; 81: 477 -484. ACOG Practice Bulletin 127, June 2012. Management of Preterm Labor Preeclampsia with severe features, eclampsia Hemodynamic instability of mother PPROM Maternal contraindications
Tocolytics Reduces birth within 48 hours but does not improve neonatal outcomes No evidence for maintenance therapy outside 48 -72 hr while inpatient and many risks Magnesium should no longer be given for tocolysis When using for neuroprotection, watch interactions with tocolytics Sayres W. Preterm Labor American Family Physician 2010; 81: 477 -484. ACOG Practice Bulletin 127, June 2012. Management of Preterm Labor
Tocolytics Nifedipine First line agent at UNM for all 20 mg PO q 6 hours, can increase dosing interval to q 4 hrs if BP tolerates Risk of hypotension; side effects include flushing, nausea, HA, dizziness Contraindicated in hypotension and aortic insufficiency Caution with use with magnesium- higher risk for pulmonary edema No known adverse effects for fetus
Tocolytics Indomethacin Usually used under 32 weeks, after this concern for premature closure of ductus arteriosis Loading dose 50 -100 mg PO, then 25 mg PO q 4 -6 hours Okay to use with magnesium Contraindications cross over with NSAIDS Terbutaline 0. 25 mg SQ q 20 min Risk of maternal and fetal tachycardia, pulmonary edema Use should be limited to short term, ex for tachysystole, one time use in triage “terbutaline trial” Sayres W. Preterm Labor American Family Physician 2010; 81: 477 -484. ACOG Practice Bulletin 127, June 2012. Management of Preterm Labor
Antibiotics Bacterial infection is presumed cause for many preterm births <32 weeks No evidence antibiotic therapy prolongs pregnancy, or reduces neonatal morbidity/ mortality Some evidence of harm King et al. Prophylactic antibiotics for inhibiting preterm labor with intact membranes. Cochrane Database 2002, Issue 4.
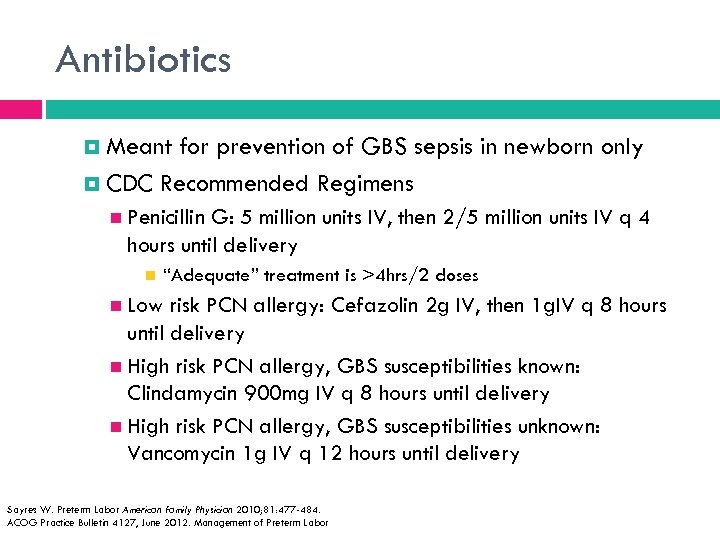
Antibiotics Meant for prevention of GBS sepsis in newborn only CDC Recommended Regimens Penicillin G: 5 million units IV, then 2/5 million units IV q 4 hours until delivery “Adequate” treatment is >4 hrs/2 doses Low risk PCN allergy: Cefazolin 2 g IV, then 1 g. IV q 8 hours until delivery High risk PCN allergy, GBS susceptibilities known: Clindamycin 900 mg IV q 8 hours until delivery High risk PCN allergy, GBS susceptibilities unknown: Vancomycin 1 g IV q 12 hours until delivery Sayres W. Preterm Labor American Family Physician 2010; 81: 477 -484. ACOG Practice Bulletin 4127, June 2012. Management of Preterm Labor
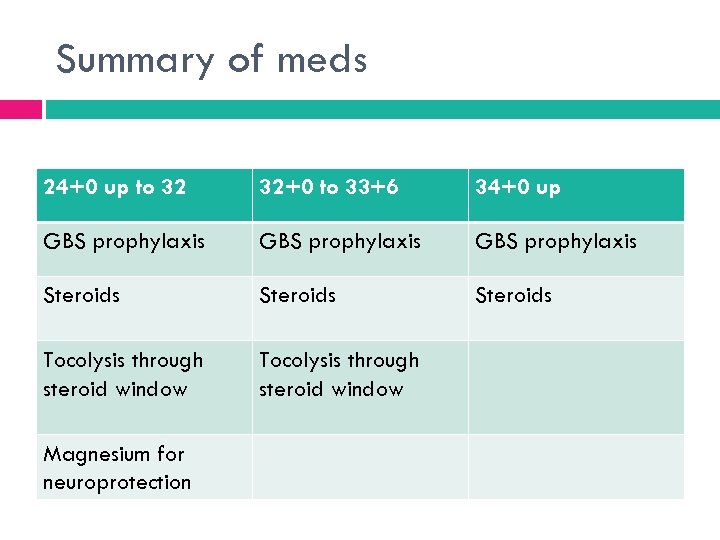
Summary of meds 24+0 up to 32 32+0 to 33+6 34+0 up GBS prophylaxis Steroids Tocolysis through steroid window Magnesium for neuroprotection
Meanwhile in triage…
Case 3 21 yo G 2 P 0101 presents to triage with contractions at 31+6 weeks What is your initial work up?
Case 3 Contact attending Sterile spec with FFN (+/-), GC/C, GBS, eval for SROM Digital exam if no SROM Monitor for ongoing contractions and cervical change She continues to have ongoing contractions q 3 min and cervical change… What do you do?
Case 3 Admit patient to Labor and Delivery Betamethasone Neuroprotection with magnesium GBS prophylaxis Nifedipine vs indomethacin for tocolysis She stops contracting overnight, what are next steps? Finish steroids with tocolysis Observe 24 hrs s/p tocolysis
Case 4 29 yo G 2 P 1001 at 34+5 weeks presents with regular contractions What will be your first steps?
Case 4 Contact attending Sterile spec with FFN (+/-), GC/C, GBS, eval for SROM Digital exam if no SROM Monitor for ongoing contractions and cervical change She continues to have ongoing cervical change, what will you do? Admit to L+D GBS prophylaxis Steroids! NO magnesium, NO tocolysis
Case 4 She progresses to fully dilated in the next 6 hours What should your considerations be when delivering her baby?
Delivery management Important considerations for preterm delivery Contact NICU No vacuums <34 weeks Control head extension Delayed cord clamping Less need for transfusion Less hypotension Less anemia Less intraventricular hemorrhage No difference in death Timing of Umbilical Cord Clamping. ACOG Practice Bulletin 543, December 2012.
Delivery Management Methods for delayed cord clamping Assess stability of baby Older babies with spontaneous cry, wait 1 -2 min at level of perineum vs 3 -4 min on skin-to-skin Milking cord is an alternative if NICU intervention critical Where will the baby go? <36 weeks to ICN 3 vs NICU >36 weeks to MBU Timing of Umbilical Cord Clamping. ACOG Practice Bulletin 543, December 2012.
Meanwhile in Northern NM…
Case 5 You are working remotely in Zuni when a 27 yo G 1 P 0 at 32+2 presents with strong contractions q 3 min While you are assessing a cervical exam, her water breaks and she is found to be 8 cm dilated and vertex by palpation of sutures What do you do?
Case 5 No time for transfer prior to delivery Basics of delivery of a preterm infant Contact NICU transport team Control extension of the head Do NOT use vacuum Delay cord clamping ✕
PPROM Preterm premature rupture of membranes SROM prior to 37 weeks and prior to onset of contractions About 3% of deliveries in US >50% will give birth within 1 week of rupture, 70 -80% in 2 -5 weeks after Intra-amniotic infection in 15 -25%, more likely when more preterm Premature Rupture of Membranes. ACOG Practice Bulletin 139, October 2013.
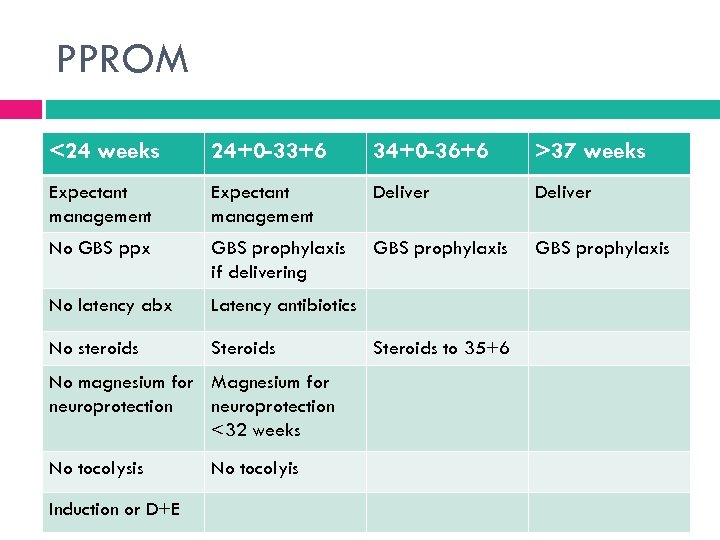
PPROM <24 weeks 24+0 -33+6 34+0 -36+6 >37 weeks Expectant management Deliver No GBS ppx GBS prophylaxis if delivering GBS prophylaxis No latency abx Latency antibiotics No steroids Steroids No magnesium for Magnesium for neuroprotection <32 weeks No tocolysis Induction or D+E No tocolyis Steroids to 35+6
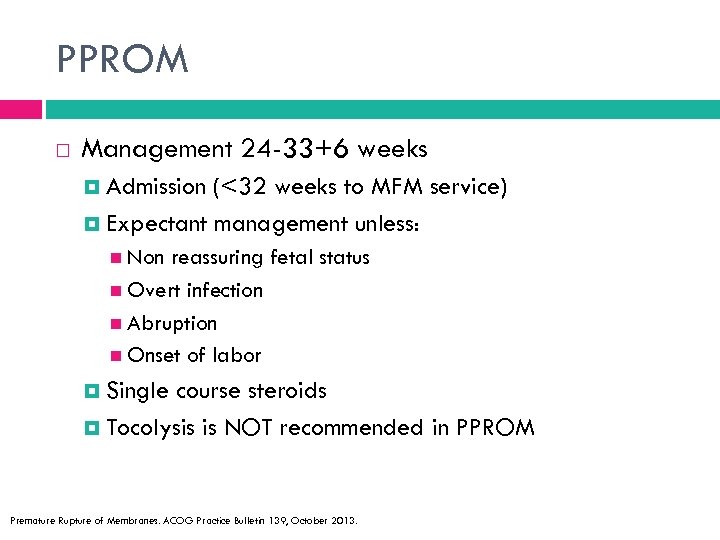
PPROM Management 24 -33+6 weeks Admission (<32 weeks to MFM service) Expectant management unless: Non reassuring fetal status Overt infection Abruption Onset of labor Single course steroids Tocolysis is NOT recommended in PPROM Premature Rupture of Membranes. ACOG Practice Bulletin 139, October 2013.
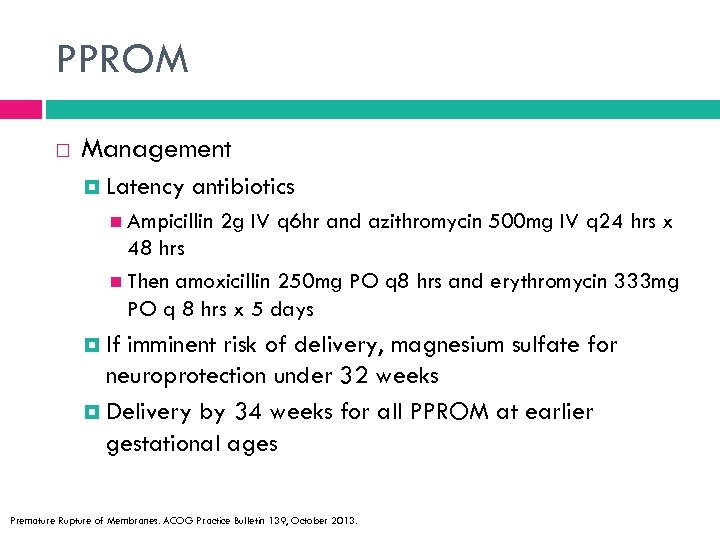
PPROM Management Latency antibiotics Ampicillin 2 g IV q 6 hr and azithromycin 500 mg IV q 24 hrs x 48 hrs Then amoxicillin 250 mg PO q 8 hrs and erythromycin 333 mg PO q 8 hrs x 5 days If imminent risk of delivery, magnesium sulfate for neuroprotection under 32 weeks Delivery by 34 weeks for all PPROM at earlier gestational ages Premature Rupture of Membranes. ACOG Practice Bulletin 139, October 2013.
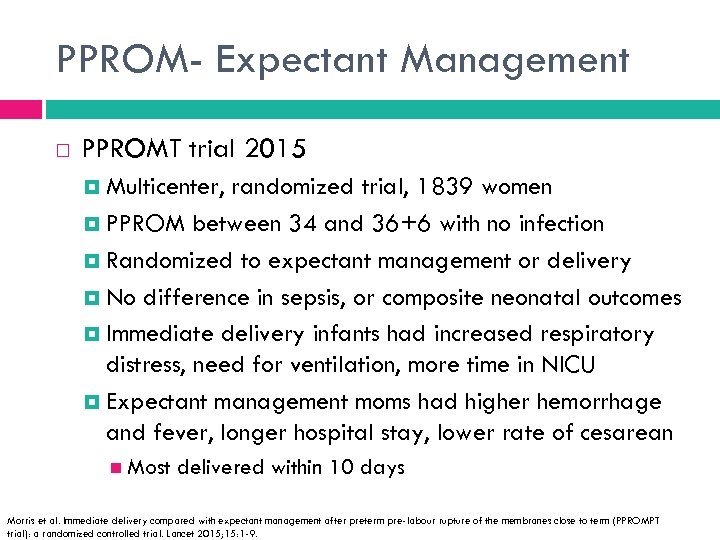
PPROM- Expectant Management PPROMT trial 2015 Multicenter, randomized trial, 1839 women PPROM between 34 and 36+6 with no infection Randomized to expectant management or delivery No difference in sepsis, or composite neonatal outcomes Immediate delivery infants had increased respiratory distress, need for ventilation, more time in NICU Expectant management moms had higher hemorrhage and fever, longer hospital stay, lower rate of cesarean Most delivered within 10 days Morris et al. Immediate delivery compared with expectant management after preterm pre-labour rupture of the membranes close to term (PPROMPT trial): a randomized controlled trial. Lancet 2015; 15: 1 -9.
Back to Albuquerque…
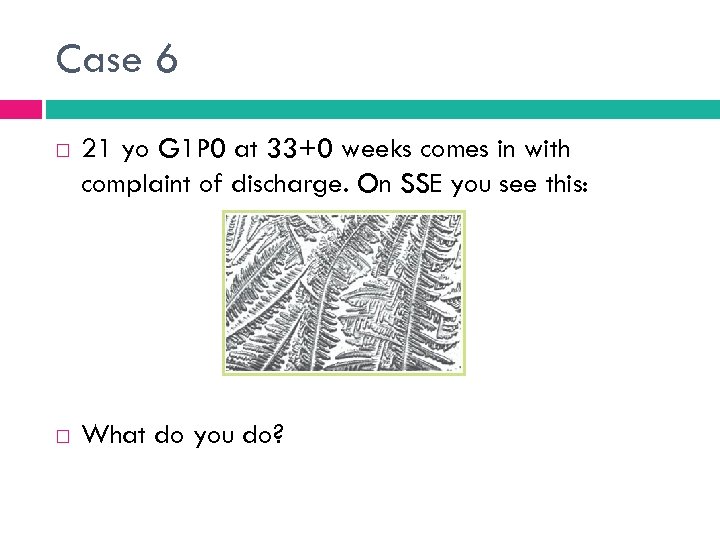
Case 6 21 yo G 1 P 0 at 33+0 weeks comes in with complaint of discharge. On SSE you see this: What do you do?
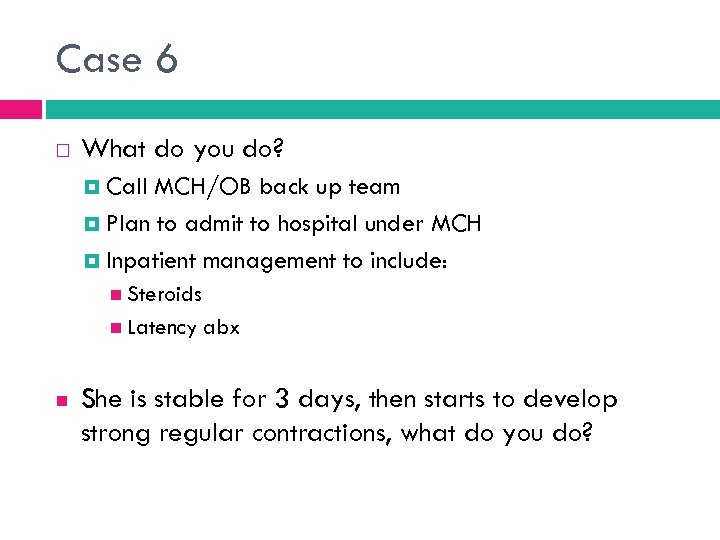
Case 6 What do you do? Call MCH/OB back up team Plan to admit to hospital under MCH Inpatient management to include: Steroids Latency abx She is stable for 3 days, then starts to develop strong regular contractions, what do you do?
Case 6 Prepare for delivery If <32 weeks would give magnesium at this time for neuroprotection She then stops contractions within a few hours and is stable for a few days. When should she be delivered? 34 weeks Any sign of infection or fetal distress
Summary Preterm birth is a serious public health problem On the rise 34 -37 weeks Sometimes indicated Progesterone is effective in preventing preterm birth Prior preterm birth: IM 17 -OHP, cervical lengths, possible cerclage Incidental short cervix: vaginal progesterone
Summary Preterm labor: management with intact membranes Steroids Tocolysis Magnesium for neuroprotection GBS prophylaxis Management of PPROM Steroids Latency antibiotics
Questions?
c76941e9d1793137d88ed0bb11a453c1.ppt