d267398ba7e482b51333eb0a7be39b4b.ppt
- Количество слайдов: 35
 Pressure support ventilation Dr Vincent Ioos Pulmonologist and Intensivist Medical ICU, PIMS 1 st International Conference Pulmonology and Critical Care Rawalpindi, 9 -11 th March 2007
Pressure support ventilation Dr Vincent Ioos Pulmonologist and Intensivist Medical ICU, PIMS 1 st International Conference Pulmonology and Critical Care Rawalpindi, 9 -11 th March 2007
 Goals of mechanical ventilation But • Put the lung at rest • Restore efficient O 2 delivery • Put the respiratory muscles at rest • Positive pressure ventilation : increased intrathoracic pressure ventilator induced lung injury, hemodynamic impairement • Dysynchrony between patient and ventilator : increased work of breathing
Goals of mechanical ventilation But • Put the lung at rest • Restore efficient O 2 delivery • Put the respiratory muscles at rest • Positive pressure ventilation : increased intrathoracic pressure ventilator induced lung injury, hemodynamic impairement • Dysynchrony between patient and ventilator : increased work of breathing
 Meeting patient’s need and comfort • Neural drive • Avoid unrewarded respiratory efforts • Avoid excessive sedation (hemodynamic consequences, prolonged length of mechanical ventilation)
Meeting patient’s need and comfort • Neural drive • Avoid unrewarded respiratory efforts • Avoid excessive sedation (hemodynamic consequences, prolonged length of mechanical ventilation)
 Flow Preset Modes • Inspiratory flow is preset • Inspiratory time determines the Vt • The variable parameter is the airway peak and plateau pressure
Flow Preset Modes • Inspiratory flow is preset • Inspiratory time determines the Vt • The variable parameter is the airway peak and plateau pressure
 Pressure Preset Modes • Pressure in airway is the preset parameter • Flow is adjusted at every moment to reach the preset pressure • The variable parameter is Vt
Pressure Preset Modes • Pressure in airway is the preset parameter • Flow is adjusted at every moment to reach the preset pressure • The variable parameter is Vt
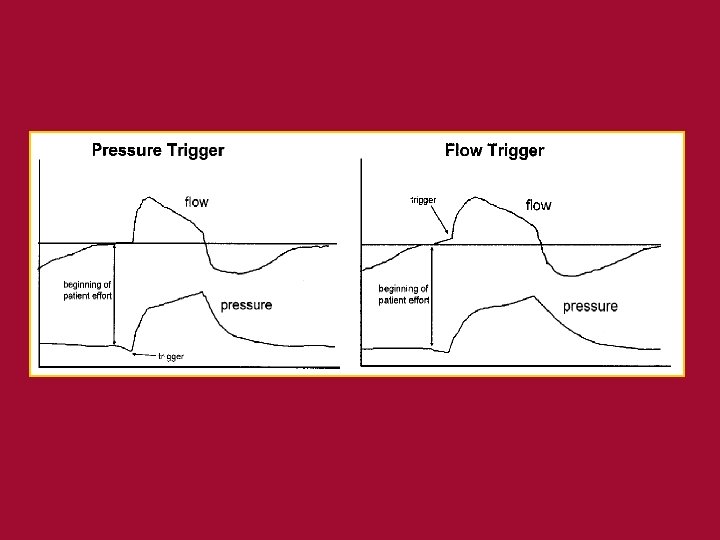
 Initiation of inspiration • At a given time, determined by RR setting (Tini) • Pressure triggering (Pini) : decrease in airway pressure from the end-expiratory level to a threshold setting • Flow trigerring (V’ini) : flow change in the breathing in the ventilator circuit beyond a determined threshold • Both Pini / V’ini (the first parameter reached initiate inhalation)
Initiation of inspiration • At a given time, determined by RR setting (Tini) • Pressure triggering (Pini) : decrease in airway pressure from the end-expiratory level to a threshold setting • Flow trigerring (V’ini) : flow change in the breathing in the ventilator circuit beyond a determined threshold • Both Pini / V’ini (the first parameter reached initiate inhalation)
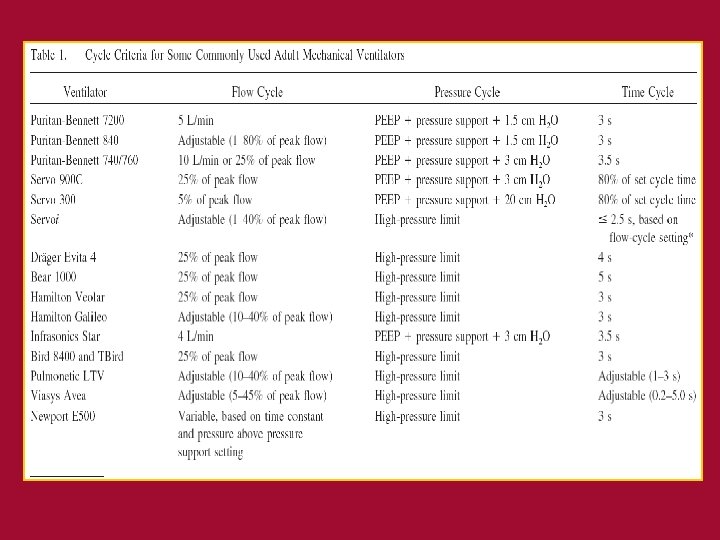
 Cycling from inspiration to expiration • At a given time : Tcyc • Flow cycling : V’cyc – Fixed absolute value – % of peak inspiratory flow (usually 25%) • Positive pressure between Paw and baseline pressure : Pcyc
Cycling from inspiration to expiration • At a given time : Tcyc • Flow cycling : V’cyc – Fixed absolute value – % of peak inspiratory flow (usually 25%) • Positive pressure between Paw and baseline pressure : Pcyc
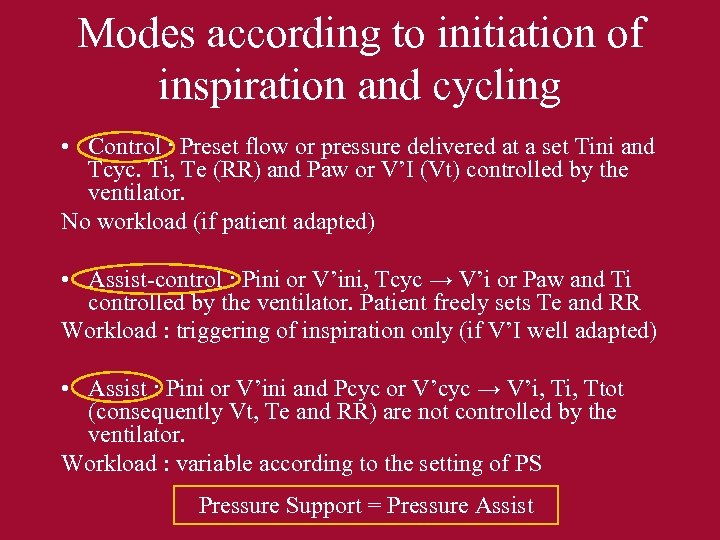 Modes according to initiation of inspiration and cycling • Control : Preset flow or pressure delivered at a set Tini and Tcyc. Ti, Te (RR) and Paw or V’I (Vt) controlled by the ventilator. No workload (if patient adapted) • Assist-control : Pini or V’ini, Tcyc → V’i or Paw and Ti controlled by the ventilator. Patient freely sets Te and RR Workload : triggering of inspiration only (if V’I well adapted) • Assist : Pini or V’ini and Pcyc or V’cyc → V’i, Ttot (consequently Vt, Te and RR) are not controlled by the ventilator. Workload : variable according to the setting of PS Pressure Support = Pressure Assist
Modes according to initiation of inspiration and cycling • Control : Preset flow or pressure delivered at a set Tini and Tcyc. Ti, Te (RR) and Paw or V’I (Vt) controlled by the ventilator. No workload (if patient adapted) • Assist-control : Pini or V’ini, Tcyc → V’i or Paw and Ti controlled by the ventilator. Patient freely sets Te and RR Workload : triggering of inspiration only (if V’I well adapted) • Assist : Pini or V’ini and Pcyc or V’cyc → V’i, Ttot (consequently Vt, Te and RR) are not controlled by the ventilator. Workload : variable according to the setting of PS Pressure Support = Pressure Assist
 Equation of insuflated gases in flow assist control ventilation • Describes interactions between the patient and the ventilator • Pressure required to deliver a volume of gas in the lungs is determined by elastic and resistive properties of the lung Paw = Vt/C + Vi’x. R + PEP
Equation of insuflated gases in flow assist control ventilation • Describes interactions between the patient and the ventilator • Pressure required to deliver a volume of gas in the lungs is determined by elastic and resistive properties of the lung Paw = Vt/C + Vi’x. R + PEP
 Pressure Support • Reducing the load on respiratory muscles • Improving synchrony between patient and ventilator without excessive sedation • Easing the weaning process • Non-invasive ventilation
Pressure Support • Reducing the load on respiratory muscles • Improving synchrony between patient and ventilator without excessive sedation • Easing the weaning process • Non-invasive ventilation
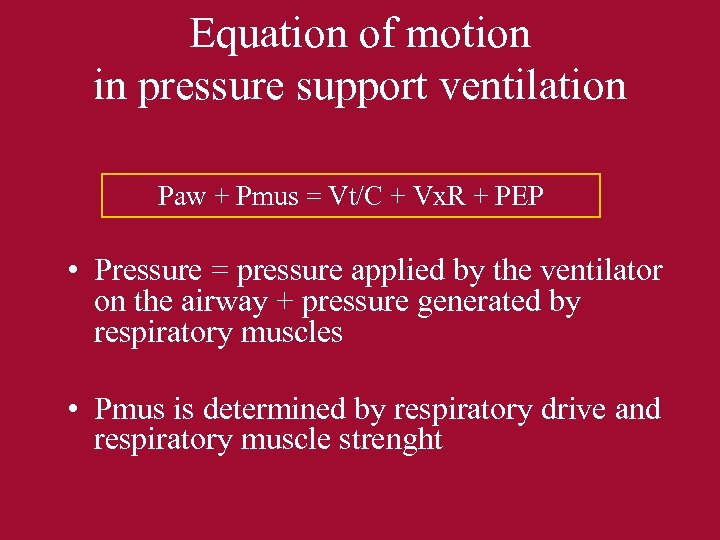 Equation of motion in pressure support ventilation Paw + Pmus = Vt/C + Vx. R + PEP • Pressure = pressure applied by the ventilator on the airway + pressure generated by respiratory muscles • Pmus is determined by respiratory drive and respiratory muscle strenght
Equation of motion in pressure support ventilation Paw + Pmus = Vt/C + Vx. R + PEP • Pressure = pressure applied by the ventilator on the airway + pressure generated by respiratory muscles • Pmus is determined by respiratory drive and respiratory muscle strenght
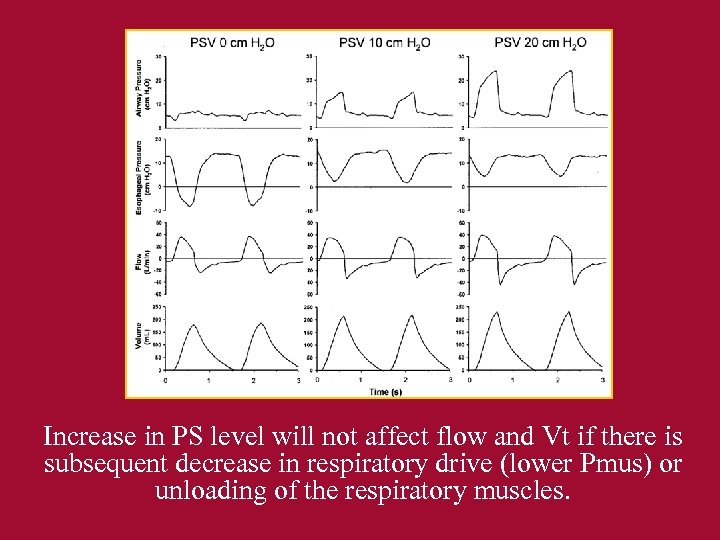 Increase in PS level will not affect flow and Vt if there is subsequent decrease in respiratory drive (lower Pmus) or unloading of the respiratory muscles.
Increase in PS level will not affect flow and Vt if there is subsequent decrease in respiratory drive (lower Pmus) or unloading of the respiratory muscles.
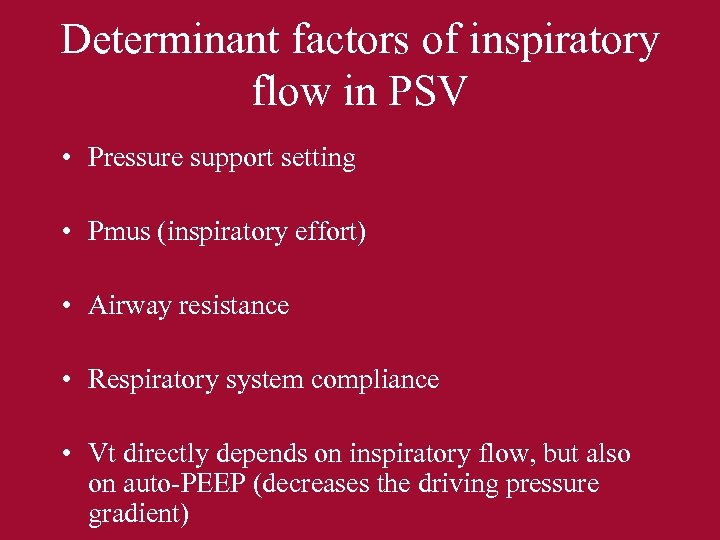 Determinant factors of inspiratory flow in PSV • Pressure support setting • Pmus (inspiratory effort) • Airway resistance • Respiratory system compliance • Vt directly depends on inspiratory flow, but also on auto-PEEP (decreases the driving pressure gradient)
Determinant factors of inspiratory flow in PSV • Pressure support setting • Pmus (inspiratory effort) • Airway resistance • Respiratory system compliance • Vt directly depends on inspiratory flow, but also on auto-PEEP (decreases the driving pressure gradient)
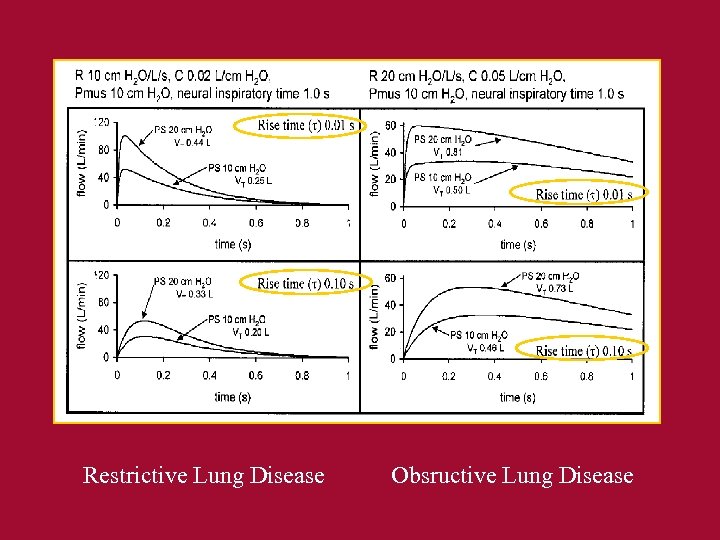 Restrictive Lung Disease Obsructive Lung Disease
Restrictive Lung Disease Obsructive Lung Disease
 Pressure Support initiation • Patient should be able to initiate an inspiratory effort, detected by pressure or flow trigger • Pressure triggering : pressure sensitivity -2 cm H 20 to 0, 5 cm H 20 • Flow triggering : flow sensitivity 1 -5 l/mn
Pressure Support initiation • Patient should be able to initiate an inspiratory effort, detected by pressure or flow trigger • Pressure triggering : pressure sensitivity -2 cm H 20 to 0, 5 cm H 20 • Flow triggering : flow sensitivity 1 -5 l/mn
 Auto-cycling • Leaks • Patient movement • Water in the ventilator circuit • Cardiac signals Signal noise trigerring the vent especially when settings sensitive Respiratory alkalosis, lung hyperinflation
Auto-cycling • Leaks • Patient movement • Water in the ventilator circuit • Cardiac signals Signal noise trigerring the vent especially when settings sensitive Respiratory alkalosis, lung hyperinflation
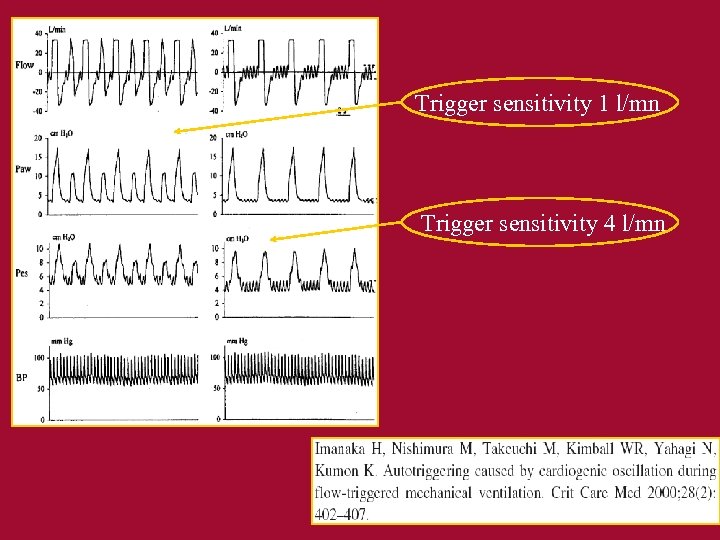 Trigger sensitivity 1 l/mn Trigger sensitivity 4 l/mn
Trigger sensitivity 1 l/mn Trigger sensitivity 4 l/mn
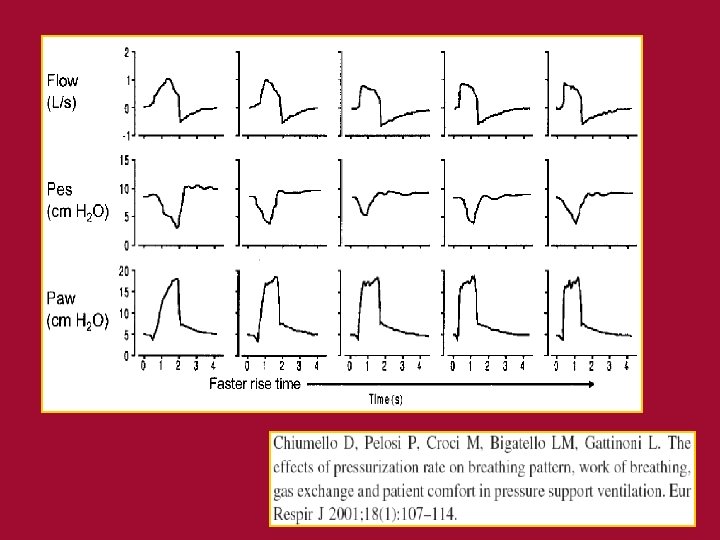
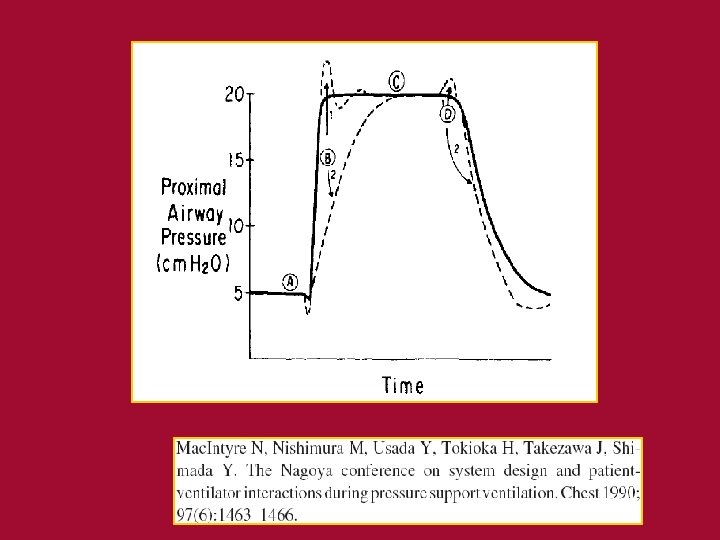
 Rise time • Time required for the ventilator to reach the PS setting at the onset of inspiration • Should be adjusted to patient comfort, to decrease the work of breathing • Allows to adjust the flow at the onset of the inspiratory phase
Rise time • Time required for the ventilator to reach the PS setting at the onset of inspiration • Should be adjusted to patient comfort, to decrease the work of breathing • Allows to adjust the flow at the onset of the inspiratory phase
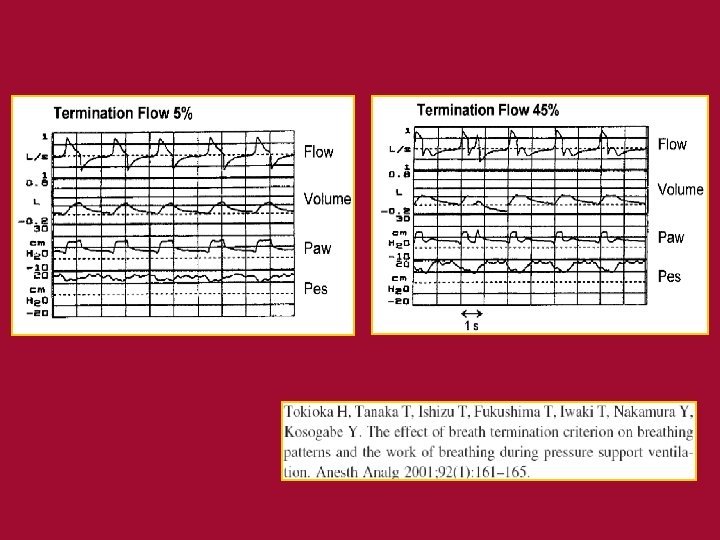
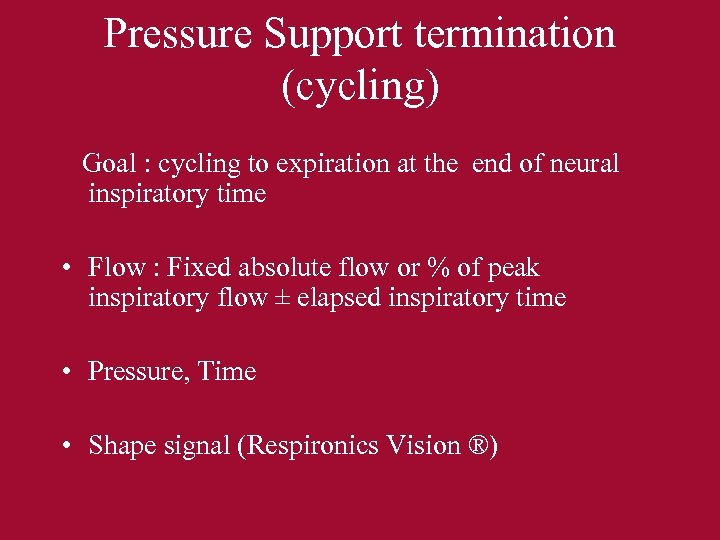 Pressure Support termination (cycling) Goal : cycling to expiration at the end of neural inspiratory time • Flow : Fixed absolute flow or % of peak inspiratory flow ± elapsed inspiratory time • Pressure, Time • Shape signal (Respironics Vision ®)
Pressure Support termination (cycling) Goal : cycling to expiration at the end of neural inspiratory time • Flow : Fixed absolute flow or % of peak inspiratory flow ± elapsed inspiratory time • Pressure, Time • Shape signal (Respironics Vision ®)
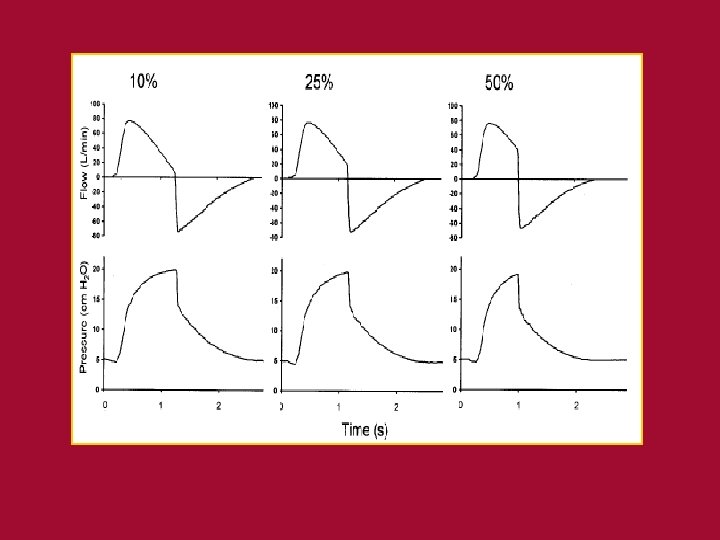
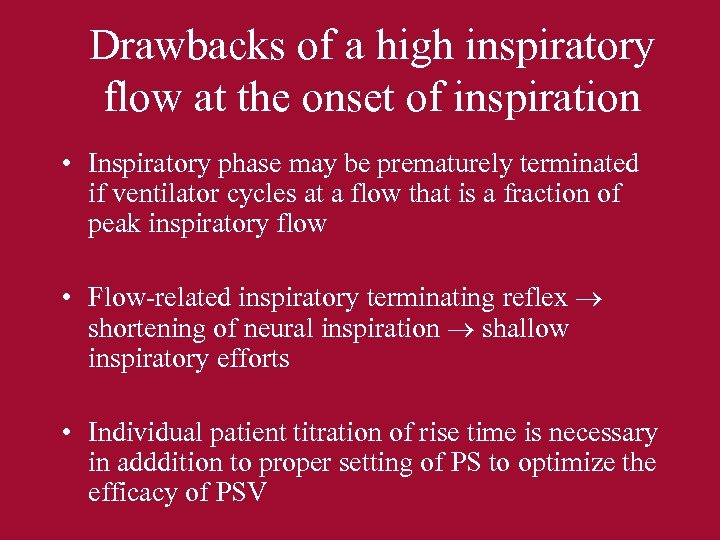 Drawbacks of a high inspiratory flow at the onset of inspiration • Inspiratory phase may be prematurely terminated if ventilator cycles at a flow that is a fraction of peak inspiratory flow • Flow-related inspiratory terminating reflex shortening of neural inspiration shallow inspiratory efforts • Individual patient titration of rise time is necessary in adddition to proper setting of PS to optimize the efficacy of PSV
Drawbacks of a high inspiratory flow at the onset of inspiration • Inspiratory phase may be prematurely terminated if ventilator cycles at a flow that is a fraction of peak inspiratory flow • Flow-related inspiratory terminating reflex shortening of neural inspiration shallow inspiratory efforts • Individual patient titration of rise time is necessary in adddition to proper setting of PS to optimize the efficacy of PSV
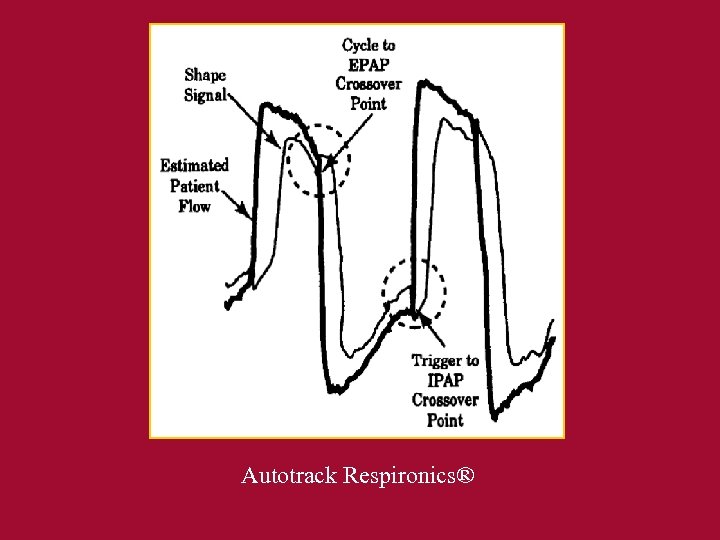 Autotrack Respironics®
Autotrack Respironics®
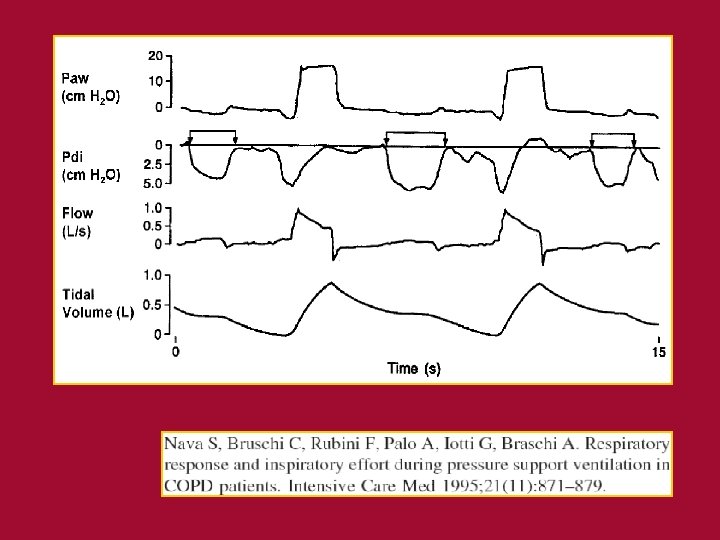
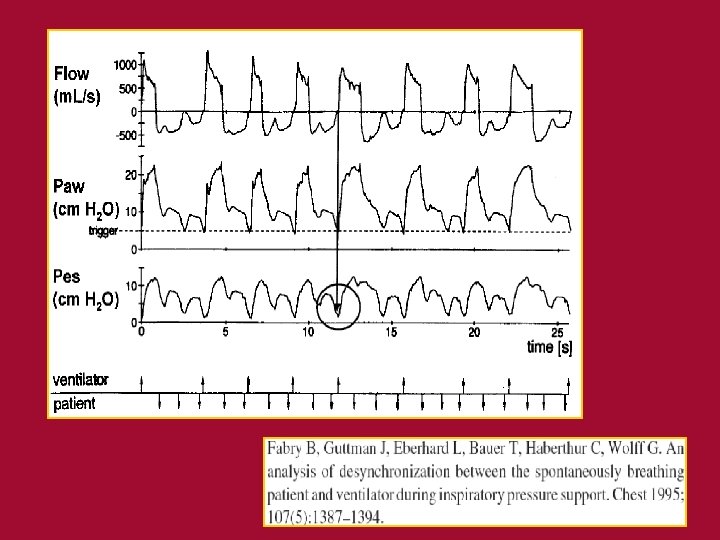
 Problems faced during PSV • Apneas • Patient – ventilator dyssynchrony : – COPD patients : – Auto. PEEP : » Increases the effort required to trigger the ventilator » Decreases the delivered Vt – Inspiratory flow decreases slowly flow cycle criteria not reached at the end of neural inspiration active exhalation to pressure cycle the breath – High minute ventilation : insufficient inspiratory flow
Problems faced during PSV • Apneas • Patient – ventilator dyssynchrony : – COPD patients : – Auto. PEEP : » Increases the effort required to trigger the ventilator » Decreases the delivered Vt – Inspiratory flow decreases slowly flow cycle criteria not reached at the end of neural inspiration active exhalation to pressure cycle the breath – High minute ventilation : insufficient inspiratory flow
 Which level of PS ? • PS + PEP 30 cm H 2 O (barotrauma) • Unloading of respiratory muscle : – Should encourage reconditioning and prevention of atrophy – While avoiding fatigue • Objectives : Vt 8 -10 ml / kg, RR < 30 -35/mn and no SCM muscle contractions
Which level of PS ? • PS + PEP 30 cm H 2 O (barotrauma) • Unloading of respiratory muscle : – Should encourage reconditioning and prevention of atrophy – While avoiding fatigue • Objectives : Vt 8 -10 ml / kg, RR < 30 -35/mn and no SCM muscle contractions
 Other parameters settings • Triggers set at their higher sensitivity, decreased if auto-cycling • Rise time titration • PEEP according to auto-PEEP and gas exchange • Fi. O 2 according to gas exchange
Other parameters settings • Triggers set at their higher sensitivity, decreased if auto-cycling • Rise time titration • PEEP according to auto-PEEP and gas exchange • Fi. O 2 according to gas exchange
 For which patients ? • COPD • ALI • Patient not synchronized with the ventilator on Flow AC MV • Weaning • NIV
For which patients ? • COPD • ALI • Patient not synchronized with the ventilator on Flow AC MV • Weaning • NIV
 Conclusions • Complexe ventilation modality, allows to get close to patient’s physiologic needs, though significant dyssynchrony may occur • Ventilators’ performance for PSV varies • Requires understanding of patient’s interaction with the ventilator • Ventilator waveforms are helpful for appropriate settings, however do not forget to look at the patient
Conclusions • Complexe ventilation modality, allows to get close to patient’s physiologic needs, though significant dyssynchrony may occur • Ventilators’ performance for PSV varies • Requires understanding of patient’s interaction with the ventilator • Ventilator waveforms are helpful for appropriate settings, however do not forget to look at the patient
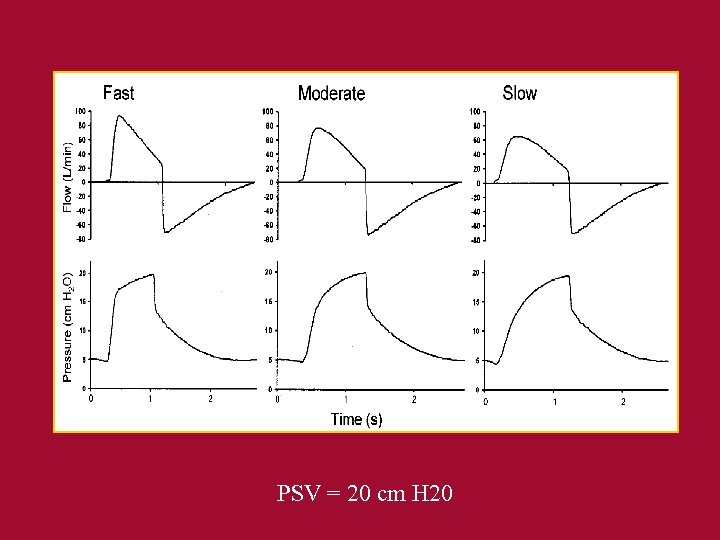 PSV = 20 cm H 20
PSV = 20 cm H 20