72131421b9af6f65ee6cf956c0f2cf7c.ppt
- Количество слайдов: 98
![Presenters Notes [Do not delete this slide] • This slide is an interactive algorithm. Presenters Notes [Do not delete this slide] • This slide is an interactive algorithm.](https://present5.com/presentation/72131421b9af6f65ee6cf956c0f2cf7c/image-1.jpg) Presenters Notes [Do not delete this slide] • This slide is an interactive algorithm. There are hyperlinks to allow you to move through the patient pathway and where appropriate gain further information. • The hyperlinks (green underlined text) only work when the presentation is in ‘slide show mode’. In order to guarantee effective use of the hyperlinks you must ensure you are clicking exactly on the hyperlink (wait for the mouse arrow to turn to a hand). • The presenter should print the whole algorithm in notes format and use this when navigating the slides. When you leave a slide note the slide you have left so that you know which one to return to. • Print the algorithm map and use this to follow your progress. • There is extra information about the contents of the slide in the notes for presenters. Additionally there are instructions for presenters which provide guidance as to what order to navigate the boxes in the slides. Key • Green boxes are the main algorithm. Hyperlinks in these boxes allow the algorithm to flow in order. • Purple boxes contain links to move you on in line with the standardised order of the algorithm. • Yellow boxes contain shortcuts. It is not recommended that you routinely use these unless you would like to skip sections of the algorithm but they can be used if you feel you have missed some slides or you only want to view one algorithm. • Grey back boxes are to be used if you want to go back to the slide you have just come from. In order to use these ensure you know the slide number you have just left. Unless you or one of the people you are presenting to have a query you should not need to use these back buttons. • Where appropriate letters will be placed next to hyperlinks on a slide to indicate the order in which the hyperlinks should be clicked on. Implementing NICE Guidance www. nice. org. uk
Presenters Notes [Do not delete this slide] • This slide is an interactive algorithm. There are hyperlinks to allow you to move through the patient pathway and where appropriate gain further information. • The hyperlinks (green underlined text) only work when the presentation is in ‘slide show mode’. In order to guarantee effective use of the hyperlinks you must ensure you are clicking exactly on the hyperlink (wait for the mouse arrow to turn to a hand). • The presenter should print the whole algorithm in notes format and use this when navigating the slides. When you leave a slide note the slide you have left so that you know which one to return to. • Print the algorithm map and use this to follow your progress. • There is extra information about the contents of the slide in the notes for presenters. Additionally there are instructions for presenters which provide guidance as to what order to navigate the boxes in the slides. Key • Green boxes are the main algorithm. Hyperlinks in these boxes allow the algorithm to flow in order. • Purple boxes contain links to move you on in line with the standardised order of the algorithm. • Yellow boxes contain shortcuts. It is not recommended that you routinely use these unless you would like to skip sections of the algorithm but they can be used if you feel you have missed some slides or you only want to view one algorithm. • Grey back boxes are to be used if you want to go back to the slide you have just come from. In order to use these ensure you know the slide number you have just left. Unless you or one of the people you are presenting to have a query you should not need to use these back buttons. • Where appropriate letters will be placed next to hyperlinks on a slide to indicate the order in which the hyperlinks should be clicked on. Implementing NICE Guidance www. nice. org. uk
 Chest pain algorithm Incorporating the treatment and management algorithms from the NICE guidelines on chest pain of recent onset, unstable angina and NSTEMI, and stable angina Implementing NICE guidance NICE clinical guidelines 94, 95 and 126 3 rd Edition – March 2014
Chest pain algorithm Incorporating the treatment and management algorithms from the NICE guidelines on chest pain of recent onset, unstable angina and NSTEMI, and stable angina Implementing NICE guidance NICE clinical guidelines 94, 95 and 126 3 rd Edition – March 2014
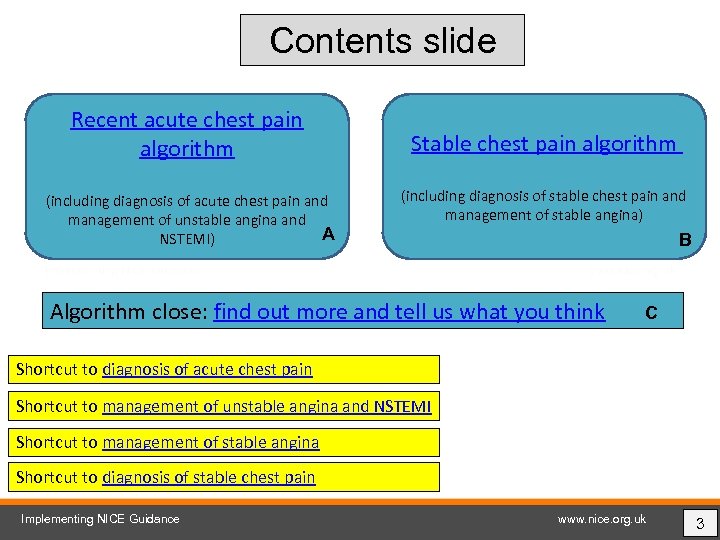 Contents slide Recent acute chest pain algorithm (including diagnosis of acute chest pain and management of unstable angina and A NSTEMI) Stable chest pain algorithm (including diagnosis of stable chest pain and management of stable angina) B Algorithm close: find out more and tell us what you think C Shortcut to diagnosis of acute chest pain Shortcut to management of unstable angina and NSTEMI Shortcut to management of stable angina Shortcut to diagnosis of stable chest pain Implementing NICE Guidance www. nice. org. uk 3
Contents slide Recent acute chest pain algorithm (including diagnosis of acute chest pain and management of unstable angina and A NSTEMI) Stable chest pain algorithm (including diagnosis of stable chest pain and management of stable angina) B Algorithm close: find out more and tell us what you think C Shortcut to diagnosis of acute chest pain Shortcut to management of unstable angina and NSTEMI Shortcut to management of stable angina Shortcut to diagnosis of stable chest pain Implementing NICE Guidance www. nice. org. uk 3
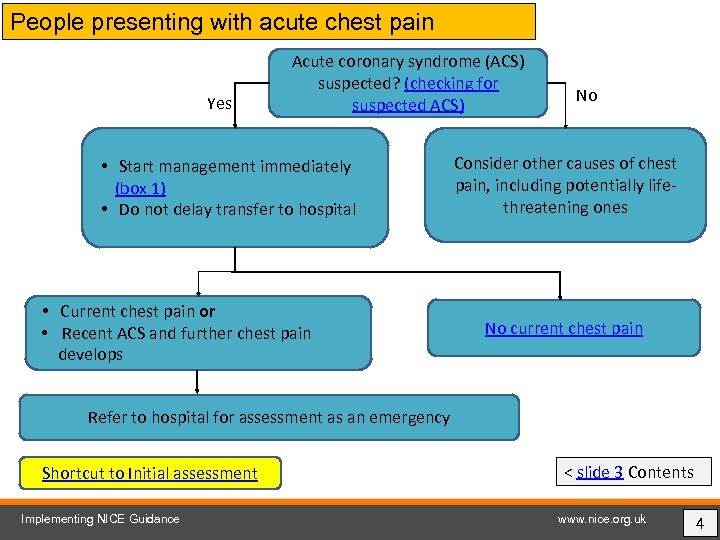 People presenting with acute chest pain Yes Acute coronary syndrome (ACS) suspected? (checking for suspected ACS) • Start management immediately (box 1) • Do not delay transfer to hospital • Current chest pain or • Recent ACS and further chest pain develops No Consider other causes of chest pain, including potentially lifethreatening ones No current chest pain Refer to hospital for assessment as an emergency Shortcut to Initial assessment Implementing NICE Guidance < slide 3 Contents www. nice. org. uk 4
People presenting with acute chest pain Yes Acute coronary syndrome (ACS) suspected? (checking for suspected ACS) • Start management immediately (box 1) • Do not delay transfer to hospital • Current chest pain or • Recent ACS and further chest pain develops No Consider other causes of chest pain, including potentially lifethreatening ones No current chest pain Refer to hospital for assessment as an emergency Shortcut to Initial assessment Implementing NICE Guidance < slide 3 Contents www. nice. org. uk 4
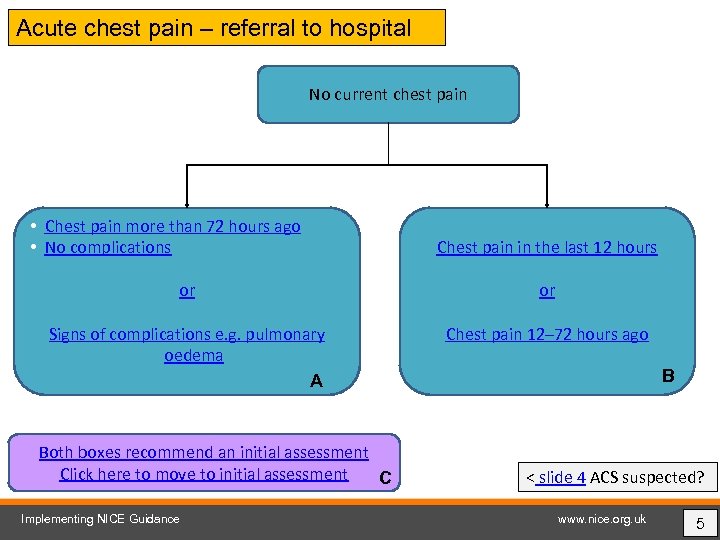 Acute chest pain – referral to hospital No current chest pain • Chest pain more than 72 hours ago • No complications Chest pain in the last 12 hours or or Signs of complications e. g. pulmonary oedema A Chest pain 12– 72 hours ago Both boxes recommend an initial assessment Click here to move to initial assessment C Implementing NICE Guidance B < slide 4 ACS suspected? www. nice. org. uk 5
Acute chest pain – referral to hospital No current chest pain • Chest pain more than 72 hours ago • No complications Chest pain in the last 12 hours or or Signs of complications e. g. pulmonary oedema A Chest pain 12– 72 hours ago Both boxes recommend an initial assessment Click here to move to initial assessment C Implementing NICE Guidance B < slide 4 ACS suspected? www. nice. org. uk 5
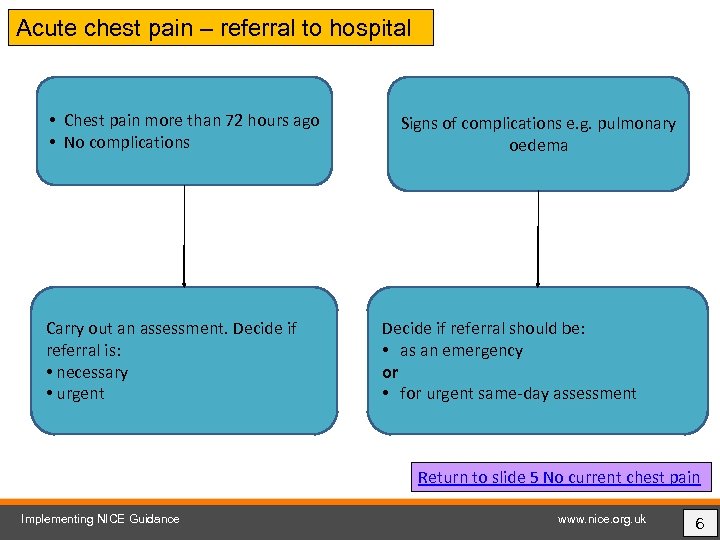 Acute chest pain – referral to hospital • Chest pain more than 72 hours ago • No complications Carry out an assessment. Decide if referral is: • necessary • urgent Signs of complications e. g. pulmonary oedema Decide if referral should be: • as an emergency or • for urgent same-day assessment Return to slide 5 No current chest pain Implementing NICE Guidance www. nice. org. uk 6
Acute chest pain – referral to hospital • Chest pain more than 72 hours ago • No complications Carry out an assessment. Decide if referral is: • necessary • urgent Signs of complications e. g. pulmonary oedema Decide if referral should be: • as an emergency or • for urgent same-day assessment Return to slide 5 No current chest pain Implementing NICE Guidance www. nice. org. uk 6
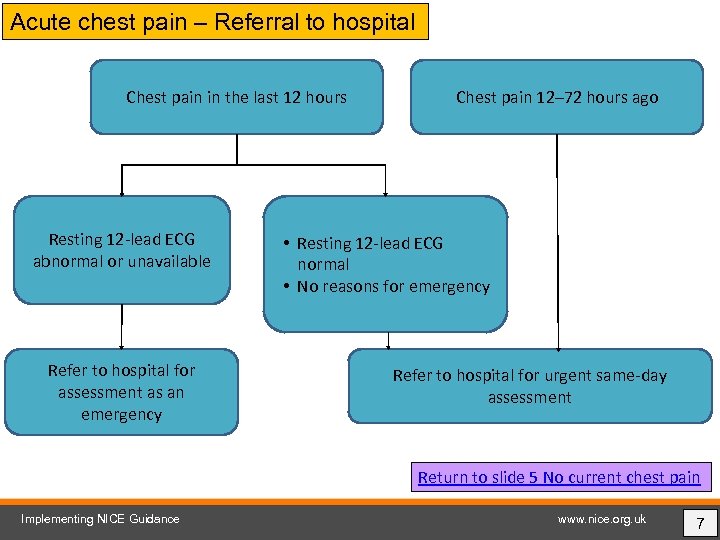 Acute chest pain – Referral to hospital Chest pain in the last 12 hours Resting 12 -lead ECG abnormal or unavailable Refer to hospital for assessment as an emergency Chest pain 12– 72 hours ago • Resting 12 -lead ECG normal • No reasons for emergency Refer to hospital for urgent same-day assessment Return to slide 5 No current chest pain Implementing NICE Guidance www. nice. org. uk 7
Acute chest pain – Referral to hospital Chest pain in the last 12 hours Resting 12 -lead ECG abnormal or unavailable Refer to hospital for assessment as an emergency Chest pain 12– 72 hours ago • Resting 12 -lead ECG normal • No reasons for emergency Refer to hospital for urgent same-day assessment Return to slide 5 No current chest pain Implementing NICE Guidance www. nice. org. uk 7
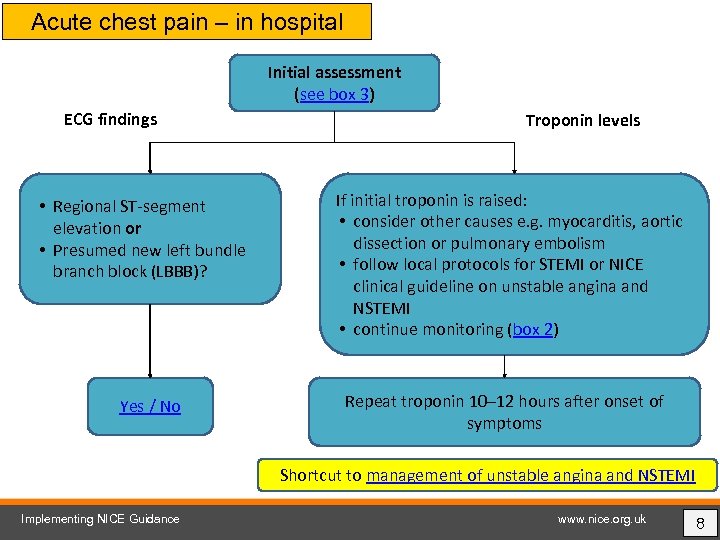 Acute chest pain – in hospital Initial assessment (see box 3) ECG findings • Regional ST-segment elevation or • Presumed new left bundle branch block (LBBB)? Yes / No Troponin levels If initial troponin is raised: • consider other causes e. g. myocarditis, aortic dissection or pulmonary embolism • follow local protocols for STEMI or NICE clinical guideline on unstable angina and NSTEMI • continue monitoring (box 2) Repeat troponin 10– 12 hours after onset of symptoms Shortcut to management of unstable angina and NSTEMI Implementing NICE Guidance www. nice. org. uk 8
Acute chest pain – in hospital Initial assessment (see box 3) ECG findings • Regional ST-segment elevation or • Presumed new left bundle branch block (LBBB)? Yes / No Troponin levels If initial troponin is raised: • consider other causes e. g. myocarditis, aortic dissection or pulmonary embolism • follow local protocols for STEMI or NICE clinical guideline on unstable angina and NSTEMI • continue monitoring (box 2) Repeat troponin 10– 12 hours after onset of symptoms Shortcut to management of unstable angina and NSTEMI Implementing NICE Guidance www. nice. org. uk 8
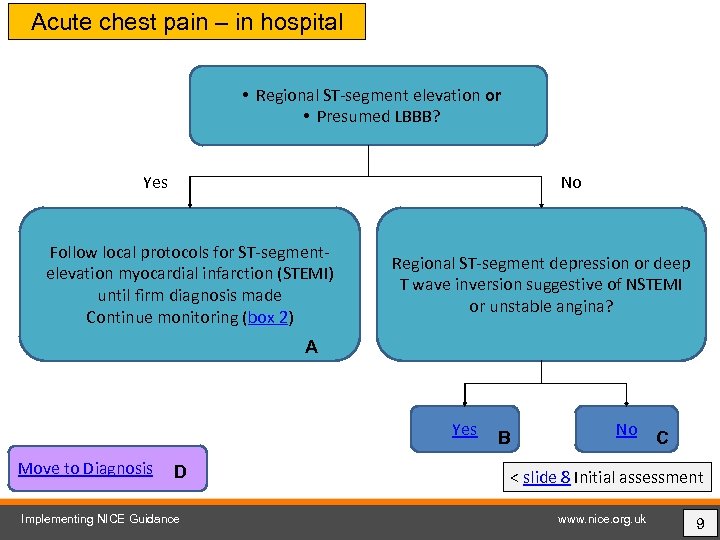 Acute chest pain – in hospital • Regional ST-segment elevation or • Presumed LBBB? Yes No Follow local protocols for ST-segmentelevation myocardial infarction (STEMI) until firm diagnosis made Continue monitoring (box 2) Regional ST-segment depression or deep T wave inversion suggestive of NSTEMI or unstable angina? A Yes Move to Diagnosis D Implementing NICE Guidance B No C < slide 8 Initial assessment www. nice. org. uk 9
Acute chest pain – in hospital • Regional ST-segment elevation or • Presumed LBBB? Yes No Follow local protocols for ST-segmentelevation myocardial infarction (STEMI) until firm diagnosis made Continue monitoring (box 2) Regional ST-segment depression or deep T wave inversion suggestive of NSTEMI or unstable angina? A Yes Move to Diagnosis D Implementing NICE Guidance B No C < slide 8 Initial assessment www. nice. org. uk 9
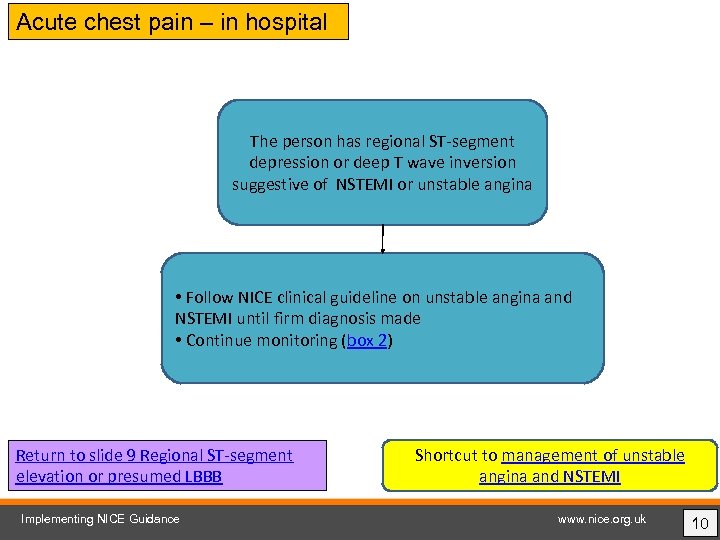 Acute chest pain – in hospital The person has regional ST-segment depression or deep T wave inversion suggestive of NSTEMI or unstable angina • Follow NICE clinical guideline on unstable angina and NSTEMI until firm diagnosis made • Continue monitoring (box 2) Return to slide 9 Regional ST-segment elevation or presumed LBBB Implementing NICE Guidance Shortcut to management of unstable angina and NSTEMI www. nice. org. uk 10
Acute chest pain – in hospital The person has regional ST-segment depression or deep T wave inversion suggestive of NSTEMI or unstable angina • Follow NICE clinical guideline on unstable angina and NSTEMI until firm diagnosis made • Continue monitoring (box 2) Return to slide 9 Regional ST-segment elevation or presumed LBBB Implementing NICE Guidance Shortcut to management of unstable angina and NSTEMI www. nice. org. uk 10
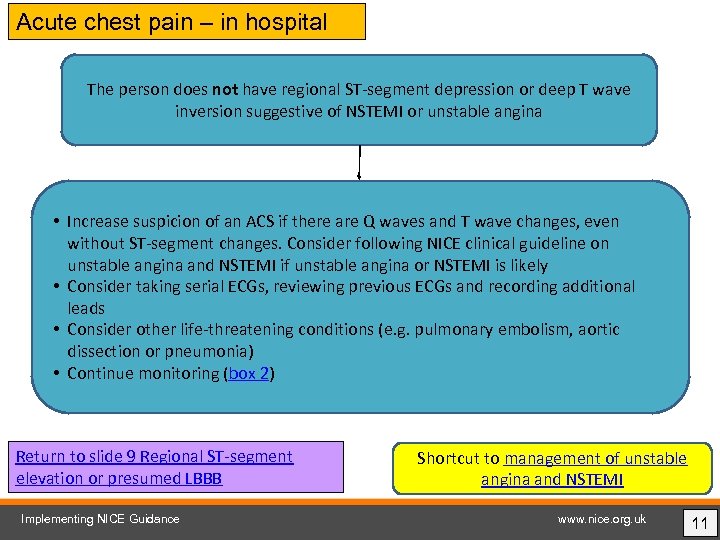 Acute chest pain – in hospital The person does not have regional ST-segment depression or deep T wave inversion suggestive of NSTEMI or unstable angina • Increase suspicion of an ACS if there are Q waves and T wave changes, even without ST-segment changes. Consider following NICE clinical guideline on unstable angina and NSTEMI if unstable angina or NSTEMI is likely • Consider taking serial ECGs, reviewing previous ECGs and recording additional leads • Consider other life-threatening conditions (e. g. pulmonary embolism, aortic dissection or pneumonia) • Continue monitoring (box 2) Return to slide 9 Regional ST-segment elevation or presumed LBBB Implementing NICE Guidance Shortcut to management of unstable angina and NSTEMI www. nice. org. uk 11
Acute chest pain – in hospital The person does not have regional ST-segment depression or deep T wave inversion suggestive of NSTEMI or unstable angina • Increase suspicion of an ACS if there are Q waves and T wave changes, even without ST-segment changes. Consider following NICE clinical guideline on unstable angina and NSTEMI if unstable angina or NSTEMI is likely • Consider taking serial ECGs, reviewing previous ECGs and recording additional leads • Consider other life-threatening conditions (e. g. pulmonary embolism, aortic dissection or pneumonia) • Continue monitoring (box 2) Return to slide 9 Regional ST-segment elevation or presumed LBBB Implementing NICE Guidance Shortcut to management of unstable angina and NSTEMI www. nice. org. uk 11
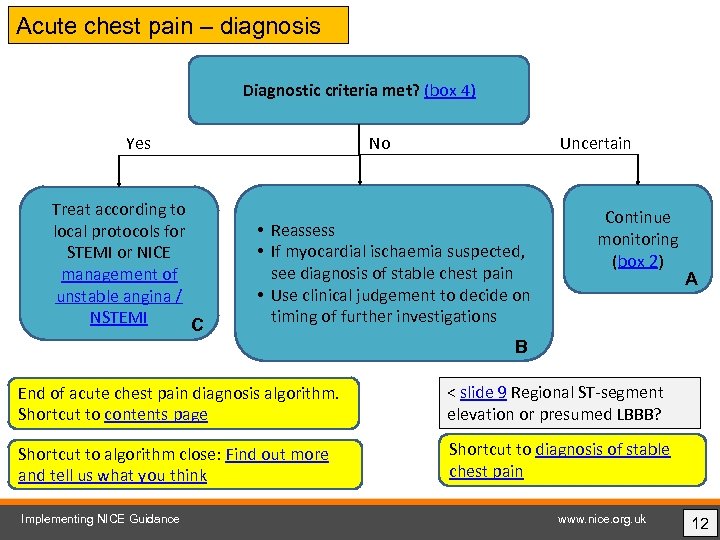 Acute chest pain – diagnosis Diagnostic criteria met? (box 4) No Yes Treat according to local protocols for STEMI or NICE management of unstable angina / NSTEMI C Uncertain • Reassess • If myocardial ischaemia suspected, see diagnosis of stable chest pain • Use clinical judgement to decide on timing of further investigations Continue monitoring (box 2) A B End of acute chest pain diagnosis algorithm. Shortcut to contents page < slide 9 Regional ST-segment elevation or presumed LBBB? Shortcut to algorithm close: Find out more and tell us what you think Shortcut to diagnosis of stable chest pain Implementing NICE Guidance www. nice. org. uk 12
Acute chest pain – diagnosis Diagnostic criteria met? (box 4) No Yes Treat according to local protocols for STEMI or NICE management of unstable angina / NSTEMI C Uncertain • Reassess • If myocardial ischaemia suspected, see diagnosis of stable chest pain • Use clinical judgement to decide on timing of further investigations Continue monitoring (box 2) A B End of acute chest pain diagnosis algorithm. Shortcut to contents page < slide 9 Regional ST-segment elevation or presumed LBBB? Shortcut to algorithm close: Find out more and tell us what you think Shortcut to diagnosis of stable chest pain Implementing NICE Guidance www. nice. org. uk 12
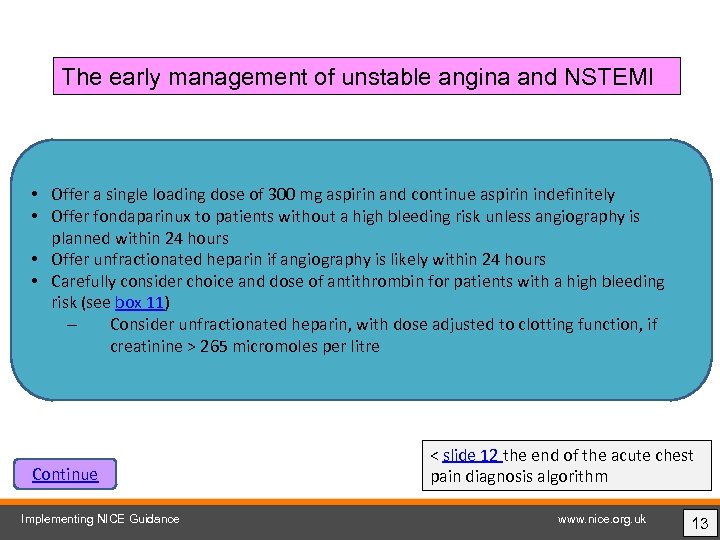 The early management of unstable angina and NSTEMI • Offer a single loading dose of 300 mg aspirin and continue aspirin indefinitely • Offer fondaparinux to patients without a high bleeding risk unless angiography is planned within 24 hours • Offer unfractionated heparin if angiography is likely within 24 hours • Carefully consider choice and dose of antithrombin for patients with a high bleeding risk (see box 11) – Consider unfractionated heparin, with dose adjusted to clotting function, if creatinine > 265 micromoles per litre Continue Implementing NICE Guidance < slide 12 the end of the acute chest pain diagnosis algorithm www. nice. org. uk 13
The early management of unstable angina and NSTEMI • Offer a single loading dose of 300 mg aspirin and continue aspirin indefinitely • Offer fondaparinux to patients without a high bleeding risk unless angiography is planned within 24 hours • Offer unfractionated heparin if angiography is likely within 24 hours • Carefully consider choice and dose of antithrombin for patients with a high bleeding risk (see box 11) – Consider unfractionated heparin, with dose adjusted to clotting function, if creatinine > 265 micromoles per litre Continue Implementing NICE Guidance < slide 12 the end of the acute chest pain diagnosis algorithm www. nice. org. uk 13
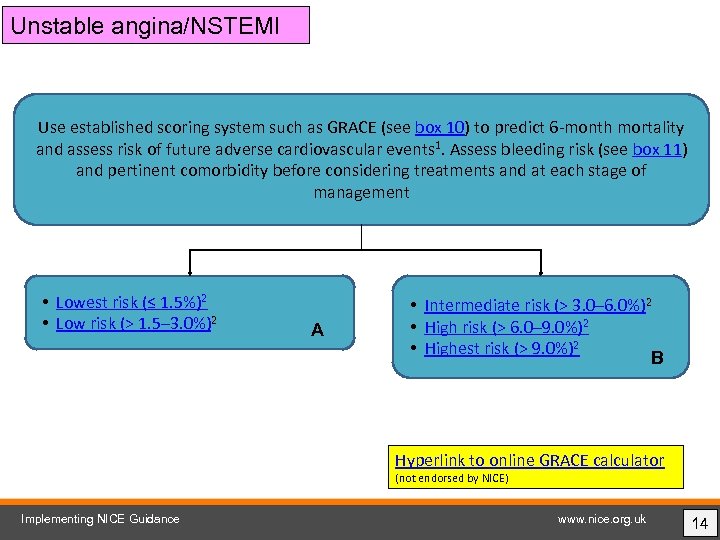 Unstable angina/NSTEMI Use established scoring system such as GRACE (see box 10) to predict 6 -month mortality and assess risk of future adverse cardiovascular events 1. Assess bleeding risk (see box 11) and pertinent comorbidity before considering treatments and at each stage of management • Lowest risk (≤ 1. 5%)2 • Low risk (> 1. 5– 3. 0%)2 A • Intermediate risk (> 3. 0– 6. 0%)2 • High risk (> 6. 0– 9. 0%)2 • Highest risk (> 9. 0%)2 B Hyperlink to online GRACE calculator (not endorsed by NICE) Implementing NICE Guidance www. nice. org. uk 14
Unstable angina/NSTEMI Use established scoring system such as GRACE (see box 10) to predict 6 -month mortality and assess risk of future adverse cardiovascular events 1. Assess bleeding risk (see box 11) and pertinent comorbidity before considering treatments and at each stage of management • Lowest risk (≤ 1. 5%)2 • Low risk (> 1. 5– 3. 0%)2 A • Intermediate risk (> 3. 0– 6. 0%)2 • High risk (> 6. 0– 9. 0%)2 • Highest risk (> 9. 0%)2 B Hyperlink to online GRACE calculator (not endorsed by NICE) Implementing NICE Guidance www. nice. org. uk 14
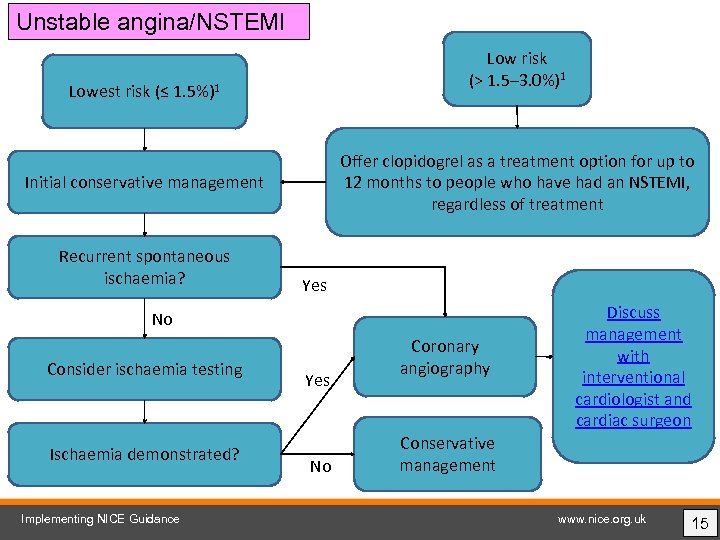 Unstable angina/NSTEMI Low risk (> 1. 5– 3. 0%)1 Lowest risk (≤ 1. 5%)1 Offer clopidogrel as a treatment option for up to 12 months to people who have had an NSTEMI, regardless of treatment Initial conservative management Recurrent spontaneous ischaemia? Yes No Consider ischaemia testing Ischaemia demonstrated? Implementing NICE Guidance Yes No Coronary angiography Discuss management with interventional cardiologist and cardiac surgeon Conservative management www. nice. org. uk 15
Unstable angina/NSTEMI Low risk (> 1. 5– 3. 0%)1 Lowest risk (≤ 1. 5%)1 Offer clopidogrel as a treatment option for up to 12 months to people who have had an NSTEMI, regardless of treatment Initial conservative management Recurrent spontaneous ischaemia? Yes No Consider ischaemia testing Ischaemia demonstrated? Implementing NICE Guidance Yes No Coronary angiography Discuss management with interventional cardiologist and cardiac surgeon Conservative management www. nice. org. uk 15
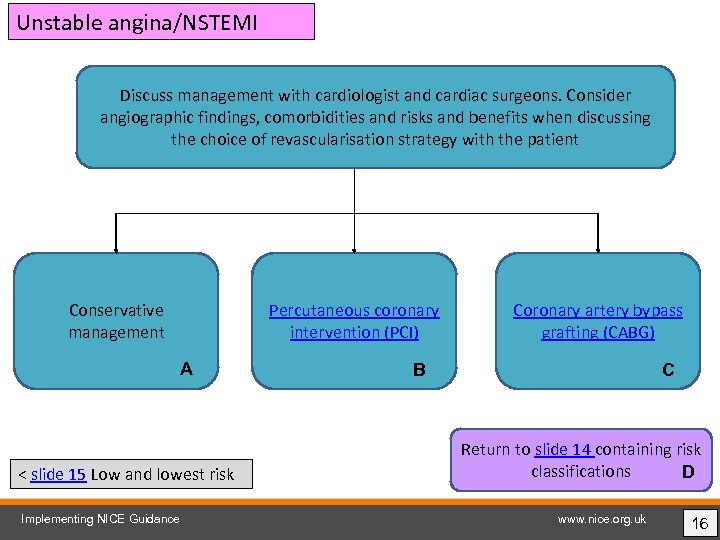 Unstable angina/NSTEMI Discuss management with cardiologist and cardiac surgeons. Consider angiographic findings, comorbidities and risks and benefits when discussing the choice of revascularisation strategy with the patient Conservative management Percutaneous coronary intervention (PCI) A < slide 15 Low and lowest risk Implementing NICE Guidance Coronary artery bypass grafting (CABG) B C Return to slide 14 containing risk classifications D www. nice. org. uk 16
Unstable angina/NSTEMI Discuss management with cardiologist and cardiac surgeons. Consider angiographic findings, comorbidities and risks and benefits when discussing the choice of revascularisation strategy with the patient Conservative management Percutaneous coronary intervention (PCI) A < slide 15 Low and lowest risk Implementing NICE Guidance Coronary artery bypass grafting (CABG) B C Return to slide 14 containing risk classifications D www. nice. org. uk 16
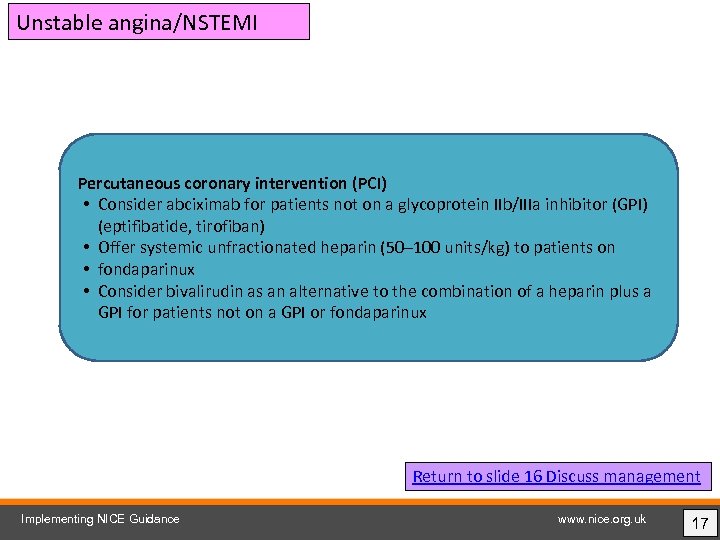 Unstable angina/NSTEMI Percutaneous coronary intervention (PCI) • Consider abciximab for patients not on a glycoprotein IIb/IIIa inhibitor (GPI) (eptifibatide, tirofiban) • Offer systemic unfractionated heparin (50– 100 units/kg) to patients on • fondaparinux • Consider bivalirudin as an alternative to the combination of a heparin plus a GPI for patients not on a GPI or fondaparinux Return to slide 16 Discuss management Implementing NICE Guidance www. nice. org. uk 17
Unstable angina/NSTEMI Percutaneous coronary intervention (PCI) • Consider abciximab for patients not on a glycoprotein IIb/IIIa inhibitor (GPI) (eptifibatide, tirofiban) • Offer systemic unfractionated heparin (50– 100 units/kg) to patients on • fondaparinux • Consider bivalirudin as an alternative to the combination of a heparin plus a GPI for patients not on a GPI or fondaparinux Return to slide 16 Discuss management Implementing NICE Guidance www. nice. org. uk 17
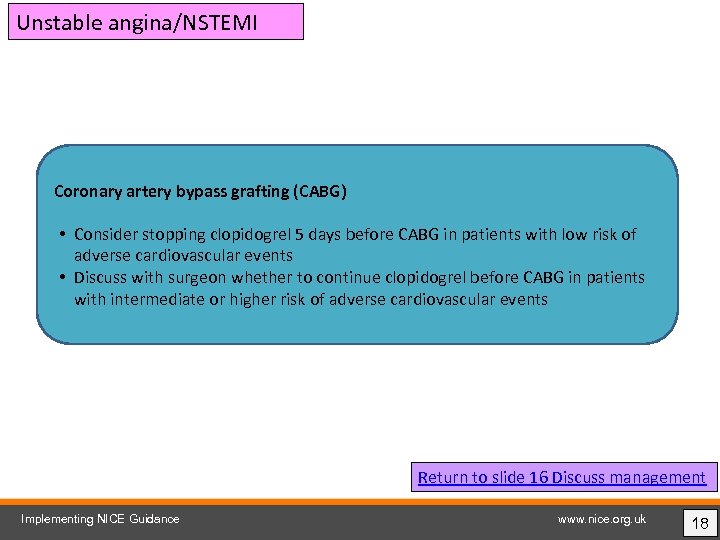 Unstable angina/NSTEMI Coronary artery bypass grafting (CABG) • Consider stopping clopidogrel 5 days before CABG in patients with low risk of adverse cardiovascular events • Discuss with surgeon whether to continue clopidogrel before CABG in patients with intermediate or higher risk of adverse cardiovascular events Return to slide 16 Discuss management Implementing NICE Guidance www. nice. org. uk 18
Unstable angina/NSTEMI Coronary artery bypass grafting (CABG) • Consider stopping clopidogrel 5 days before CABG in patients with low risk of adverse cardiovascular events • Discuss with surgeon whether to continue clopidogrel before CABG in patients with intermediate or higher risk of adverse cardiovascular events Return to slide 16 Discuss management Implementing NICE Guidance www. nice. org. uk 18
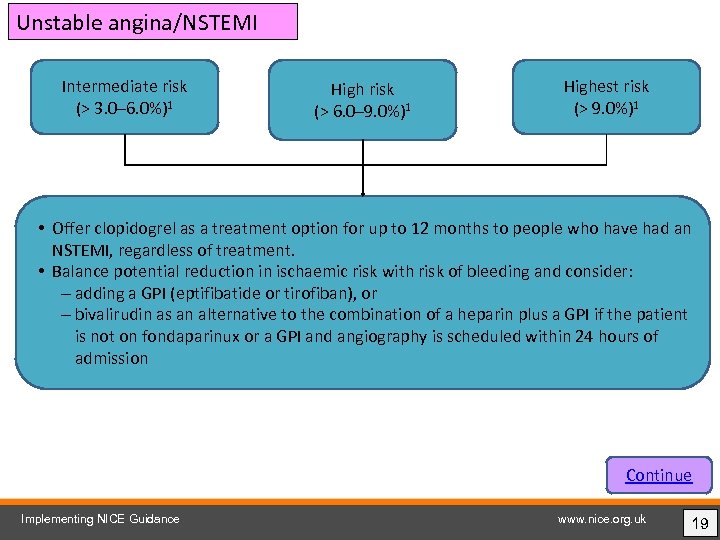 Unstable angina/NSTEMI Intermediate risk (> 3. 0– 6. 0%)1 High risk (> 6. 0– 9. 0%)1 Highest risk (> 9. 0%)1 • Offer clopidogrel as a treatment option for up to 12 months to people who have had an NSTEMI, regardless of treatment. • Balance potential reduction in ischaemic risk with risk of bleeding and consider: – adding a GPI (eptifibatide or tirofiban), or – bivalirudin as an alternative to the combination of a heparin plus a GPI if the patient is not on fondaparinux or a GPI and angiography is scheduled within 24 hours of admission Continue Implementing NICE Guidance www. nice. org. uk 19
Unstable angina/NSTEMI Intermediate risk (> 3. 0– 6. 0%)1 High risk (> 6. 0– 9. 0%)1 Highest risk (> 9. 0%)1 • Offer clopidogrel as a treatment option for up to 12 months to people who have had an NSTEMI, regardless of treatment. • Balance potential reduction in ischaemic risk with risk of bleeding and consider: – adding a GPI (eptifibatide or tirofiban), or – bivalirudin as an alternative to the combination of a heparin plus a GPI if the patient is not on fondaparinux or a GPI and angiography is scheduled within 24 hours of admission Continue Implementing NICE Guidance www. nice. org. uk 19
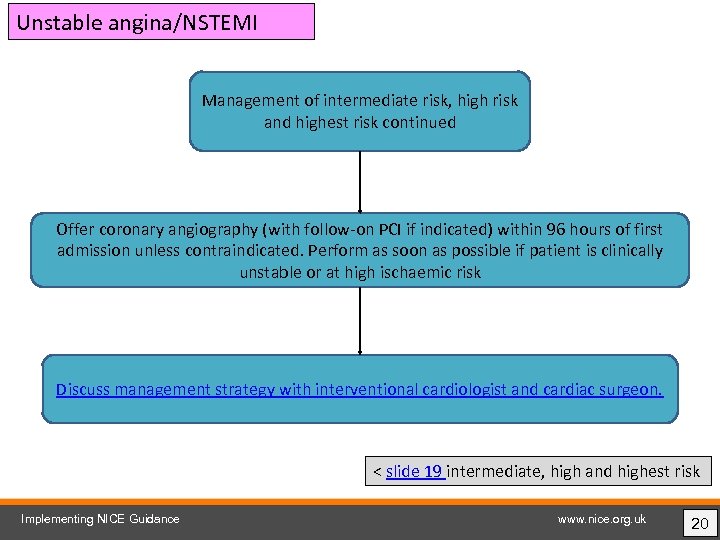 Unstable angina/NSTEMI Management of intermediate risk, high risk and highest risk continued Offer coronary angiography (with follow-on PCI if indicated) within 96 hours of first admission unless contraindicated. Perform as soon as possible if patient is clinically unstable or at high ischaemic risk Discuss management strategy with interventional cardiologist and cardiac surgeon. < slide 19 intermediate, high and highest risk Implementing NICE Guidance www. nice. org. uk 20
Unstable angina/NSTEMI Management of intermediate risk, high risk and highest risk continued Offer coronary angiography (with follow-on PCI if indicated) within 96 hours of first admission unless contraindicated. Perform as soon as possible if patient is clinically unstable or at high ischaemic risk Discuss management strategy with interventional cardiologist and cardiac surgeon. < slide 19 intermediate, high and highest risk Implementing NICE Guidance www. nice. org. uk 20
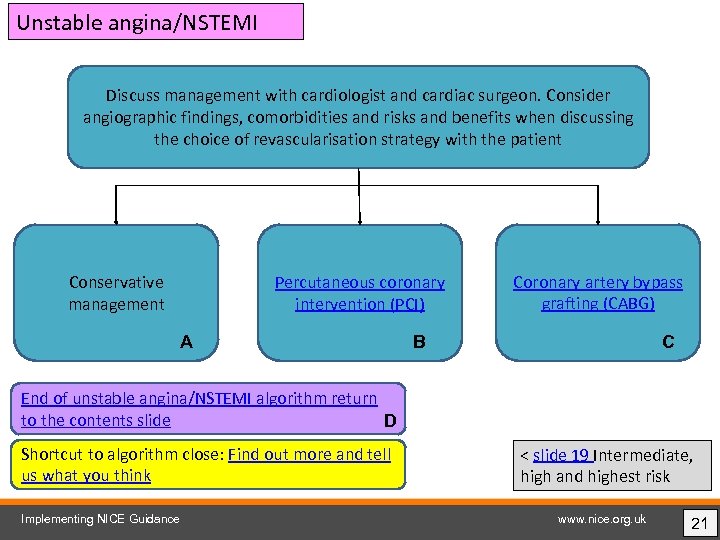 Unstable angina/NSTEMI Discuss management with cardiologist and cardiac surgeon. Consider angiographic findings, comorbidities and risks and benefits when discussing the choice of revascularisation strategy with the patient Conservative management Percutaneous coronary intervention (PCI) A Coronary artery bypass grafting (CABG) B C End of unstable angina/NSTEMI algorithm return to the contents slide D Shortcut to algorithm close: Find out more and tell us what you think Implementing NICE Guidance < slide 19 Intermediate, high and highest risk www. nice. org. uk 21
Unstable angina/NSTEMI Discuss management with cardiologist and cardiac surgeon. Consider angiographic findings, comorbidities and risks and benefits when discussing the choice of revascularisation strategy with the patient Conservative management Percutaneous coronary intervention (PCI) A Coronary artery bypass grafting (CABG) B C End of unstable angina/NSTEMI algorithm return to the contents slide D Shortcut to algorithm close: Find out more and tell us what you think Implementing NICE Guidance < slide 19 Intermediate, high and highest risk www. nice. org. uk 21
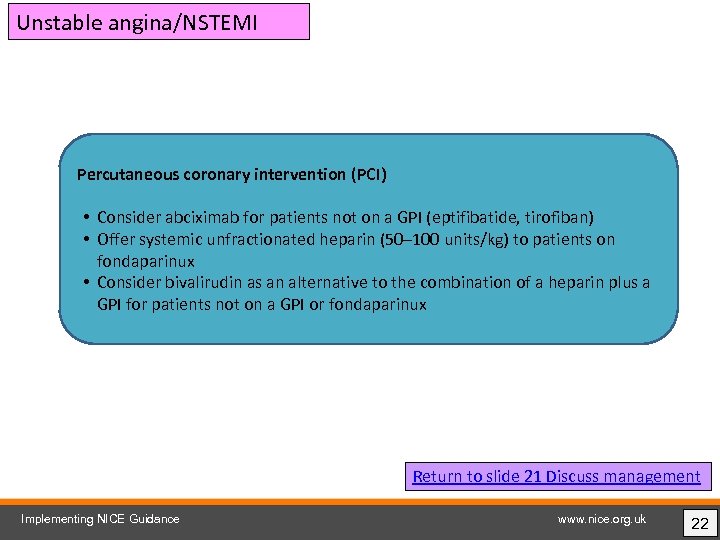 Unstable angina/NSTEMI Percutaneous coronary intervention (PCI) • Consider abciximab for patients not on a GPI (eptifibatide, tirofiban) • Offer systemic unfractionated heparin (50– 100 units/kg) to patients on fondaparinux • Consider bivalirudin as an alternative to the combination of a heparin plus a GPI for patients not on a GPI or fondaparinux Return to slide 21 Discuss management Implementing NICE Guidance www. nice. org. uk 22
Unstable angina/NSTEMI Percutaneous coronary intervention (PCI) • Consider abciximab for patients not on a GPI (eptifibatide, tirofiban) • Offer systemic unfractionated heparin (50– 100 units/kg) to patients on fondaparinux • Consider bivalirudin as an alternative to the combination of a heparin plus a GPI for patients not on a GPI or fondaparinux Return to slide 21 Discuss management Implementing NICE Guidance www. nice. org. uk 22
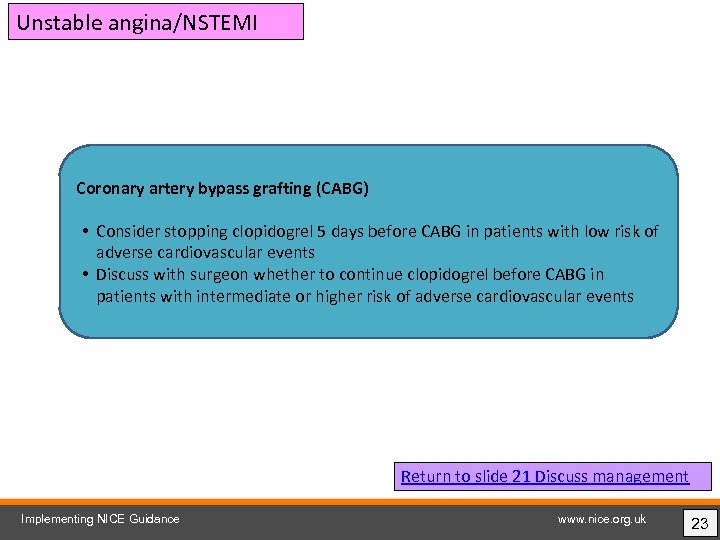 Unstable angina/NSTEMI Coronary artery bypass grafting (CABG) • Consider stopping clopidogrel 5 days before CABG in patients with low risk of adverse cardiovascular events • Discuss with surgeon whether to continue clopidogrel before CABG in patients with intermediate or higher risk of adverse cardiovascular events Return to slide 21 Discuss management Implementing NICE Guidance www. nice. org. uk 23
Unstable angina/NSTEMI Coronary artery bypass grafting (CABG) • Consider stopping clopidogrel 5 days before CABG in patients with low risk of adverse cardiovascular events • Discuss with surgeon whether to continue clopidogrel before CABG in patients with intermediate or higher risk of adverse cardiovascular events Return to slide 21 Discuss management Implementing NICE Guidance www. nice. org. uk 23
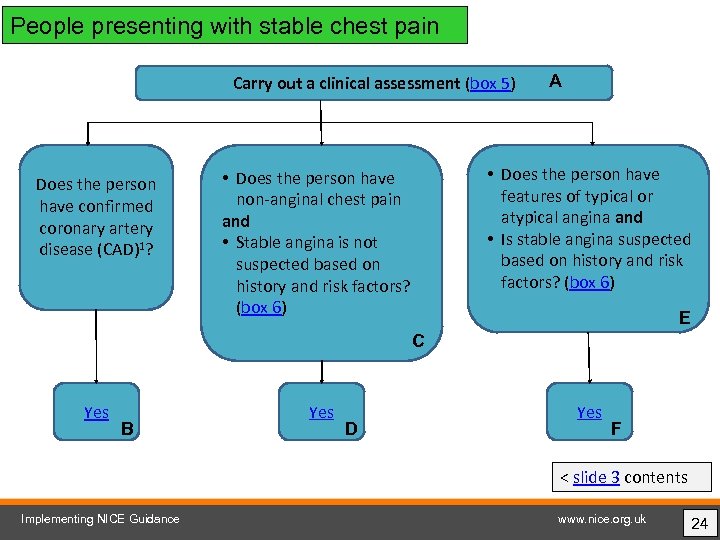 People presenting with stable chest pain Carry out a clinical assessment (box 5) Does the person have confirmed coronary artery disease (CAD)1? A • Does the person have features of typical or atypical angina and • Is stable angina suspected based on history and risk factors? (box 6) • Does the person have non-anginal chest pain and • Stable angina is not suspected based on history and risk factors? (box 6) E C Yes B Yes D Yes F < slide 3 contents Implementing NICE Guidance www. nice. org. uk 24
People presenting with stable chest pain Carry out a clinical assessment (box 5) Does the person have confirmed coronary artery disease (CAD)1? A • Does the person have features of typical or atypical angina and • Is stable angina suspected based on history and risk factors? (box 6) • Does the person have non-anginal chest pain and • Stable angina is not suspected based on history and risk factors? (box 6) E C Yes B Yes D Yes F < slide 3 contents Implementing NICE Guidance www. nice. org. uk 24
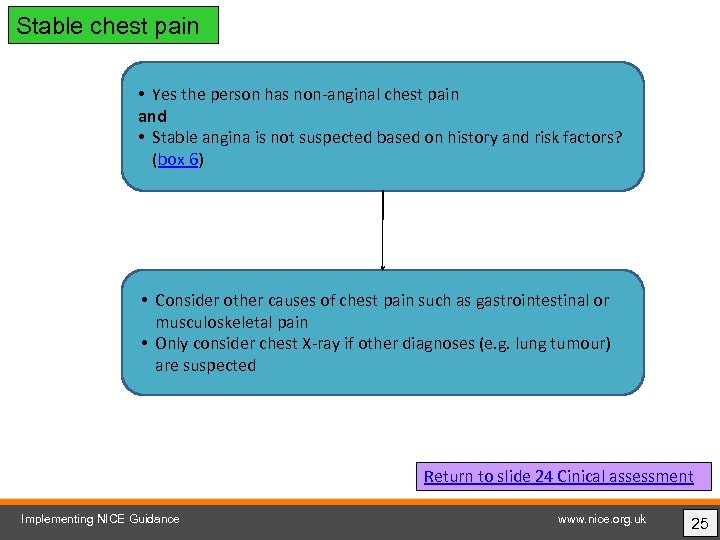 Stable chest pain • Yes the person has non-anginal chest pain and • Stable angina is not suspected based on history and risk factors? (box 6) • Consider other causes of chest pain such as gastrointestinal or musculoskeletal pain • Only consider chest X-ray if other diagnoses (e. g. lung tumour) are suspected Return to slide 24 Cinical assessment Implementing NICE Guidance www. nice. org. uk 25
Stable chest pain • Yes the person has non-anginal chest pain and • Stable angina is not suspected based on history and risk factors? (box 6) • Consider other causes of chest pain such as gastrointestinal or musculoskeletal pain • Only consider chest X-ray if other diagnoses (e. g. lung tumour) are suspected Return to slide 24 Cinical assessment Implementing NICE Guidance www. nice. org. uk 25
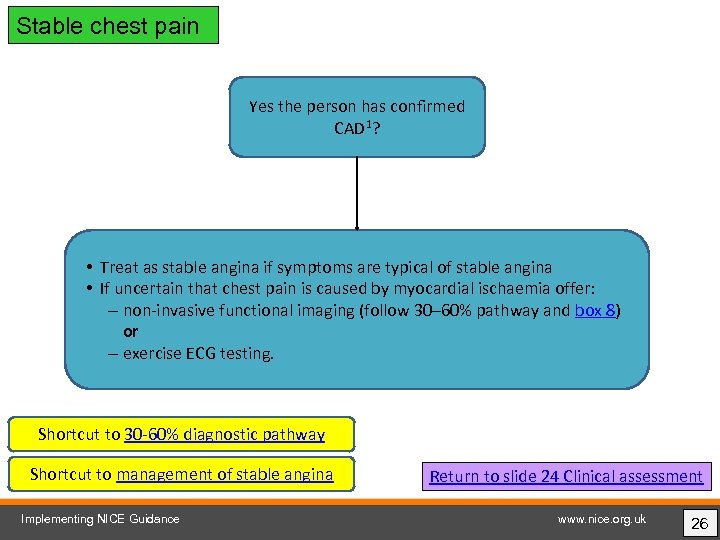 Stable chest pain Yes the person has confirmed CAD 1? • Treat as stable angina if symptoms are typical of stable angina • If uncertain that chest pain is caused by myocardial ischaemia offer: – non-invasive functional imaging (follow 30– 60% pathway and box 8) or – exercise ECG testing. Shortcut to 30 -60% diagnostic pathway Shortcut to management of stable angina Implementing NICE Guidance Return to slide 24 Clinical assessment www. nice. org. uk 26
Stable chest pain Yes the person has confirmed CAD 1? • Treat as stable angina if symptoms are typical of stable angina • If uncertain that chest pain is caused by myocardial ischaemia offer: – non-invasive functional imaging (follow 30– 60% pathway and box 8) or – exercise ECG testing. Shortcut to 30 -60% diagnostic pathway Shortcut to management of stable angina Implementing NICE Guidance Return to slide 24 Clinical assessment www. nice. org. uk 26
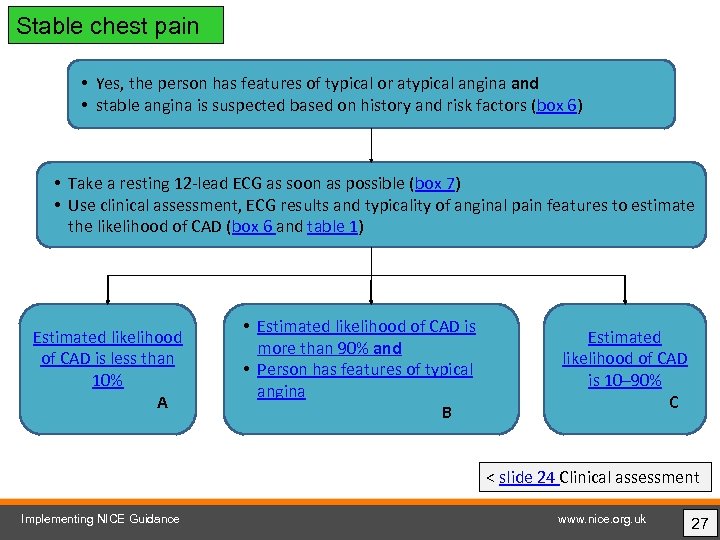 Stable chest pain • Yes, the person has features of typical or atypical angina and • stable angina is suspected based on history and risk factors (box 6) • Take a resting 12 -lead ECG as soon as possible (box 7) • Use clinical assessment, ECG results and typicality of anginal pain features to estimate the likelihood of CAD (box 6 and table 1) Estimated likelihood of CAD is less than 10% A • Estimated likelihood of CAD is more than 90% and • Person has features of typical angina B Estimated likelihood of CAD is 10– 90% C < slide 24 Clinical assessment Implementing NICE Guidance www. nice. org. uk 27
Stable chest pain • Yes, the person has features of typical or atypical angina and • stable angina is suspected based on history and risk factors (box 6) • Take a resting 12 -lead ECG as soon as possible (box 7) • Use clinical assessment, ECG results and typicality of anginal pain features to estimate the likelihood of CAD (box 6 and table 1) Estimated likelihood of CAD is less than 10% A • Estimated likelihood of CAD is more than 90% and • Person has features of typical angina B Estimated likelihood of CAD is 10– 90% C < slide 24 Clinical assessment Implementing NICE Guidance www. nice. org. uk 27
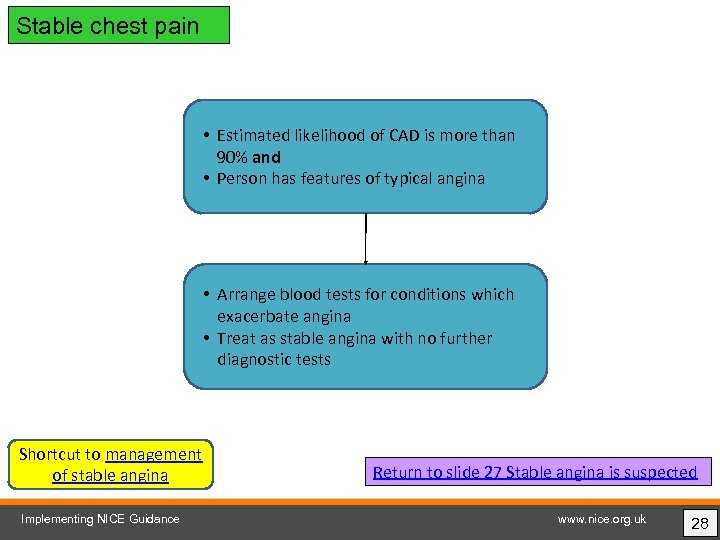 Stable chest pain • Estimated likelihood of CAD is more than 90% and • Person has features of typical angina • Arrange blood tests for conditions which exacerbate angina • Treat as stable angina with no further diagnostic tests Shortcut to management of stable angina Implementing NICE Guidance Return to slide 27 Stable angina is suspected www. nice. org. uk 28
Stable chest pain • Estimated likelihood of CAD is more than 90% and • Person has features of typical angina • Arrange blood tests for conditions which exacerbate angina • Treat as stable angina with no further diagnostic tests Shortcut to management of stable angina Implementing NICE Guidance Return to slide 27 Stable angina is suspected www. nice. org. uk 28
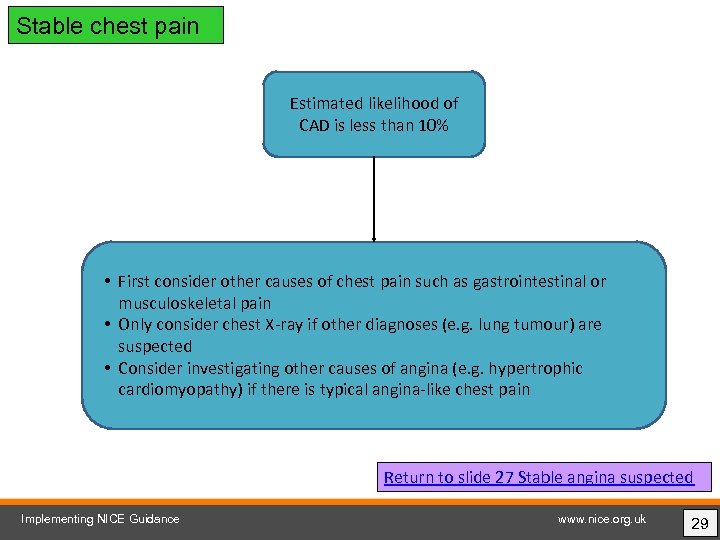 Stable chest pain Estimated likelihood of CAD is less than 10% • First consider other causes of chest pain such as gastrointestinal or musculoskeletal pain • Only consider chest X-ray if other diagnoses (e. g. lung tumour) are suspected • Consider investigating other causes of angina (e. g. hypertrophic cardiomyopathy) if there is typical angina-like chest pain Return to slide 27 Stable angina suspected Implementing NICE Guidance www. nice. org. uk 29
Stable chest pain Estimated likelihood of CAD is less than 10% • First consider other causes of chest pain such as gastrointestinal or musculoskeletal pain • Only consider chest X-ray if other diagnoses (e. g. lung tumour) are suspected • Consider investigating other causes of angina (e. g. hypertrophic cardiomyopathy) if there is typical angina-like chest pain Return to slide 27 Stable angina suspected Implementing NICE Guidance www. nice. org. uk 29
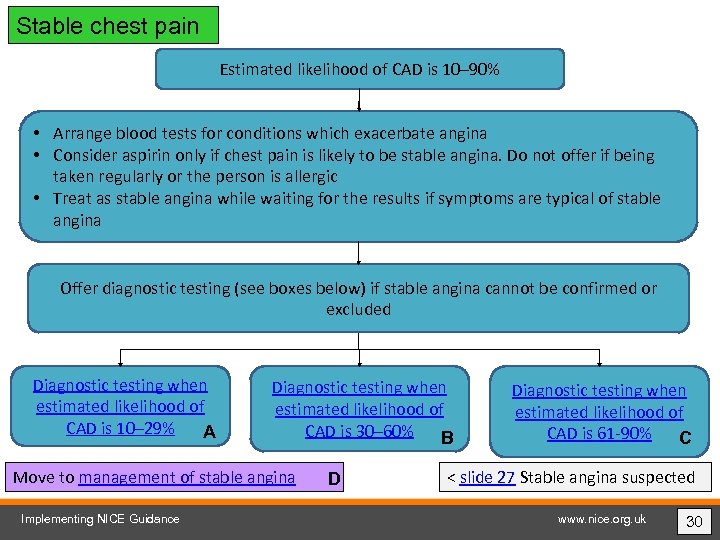 Stable chest pain Estimated likelihood of CAD is 10– 90% • Arrange blood tests for conditions which exacerbate angina • Consider aspirin only if chest pain is likely to be stable angina. Do not offer if being taken regularly or the person is allergic • Treat as stable angina while waiting for the results if symptoms are typical of stable angina Offer diagnostic testing (see boxes below) if stable angina cannot be confirmed or excluded Diagnostic testing when estimated likelihood of CAD is 10– 29% A Diagnostic testing when estimated likelihood of CAD is 30– 60% B Move to management of stable angina Implementing NICE Guidance D Diagnostic testing when estimated likelihood of CAD is 61 -90% C < slide 27 Stable angina suspected www. nice. org. uk 30
Stable chest pain Estimated likelihood of CAD is 10– 90% • Arrange blood tests for conditions which exacerbate angina • Consider aspirin only if chest pain is likely to be stable angina. Do not offer if being taken regularly or the person is allergic • Treat as stable angina while waiting for the results if symptoms are typical of stable angina Offer diagnostic testing (see boxes below) if stable angina cannot be confirmed or excluded Diagnostic testing when estimated likelihood of CAD is 10– 29% A Diagnostic testing when estimated likelihood of CAD is 30– 60% B Move to management of stable angina Implementing NICE Guidance D Diagnostic testing when estimated likelihood of CAD is 61 -90% C < slide 27 Stable angina suspected www. nice. org. uk 30
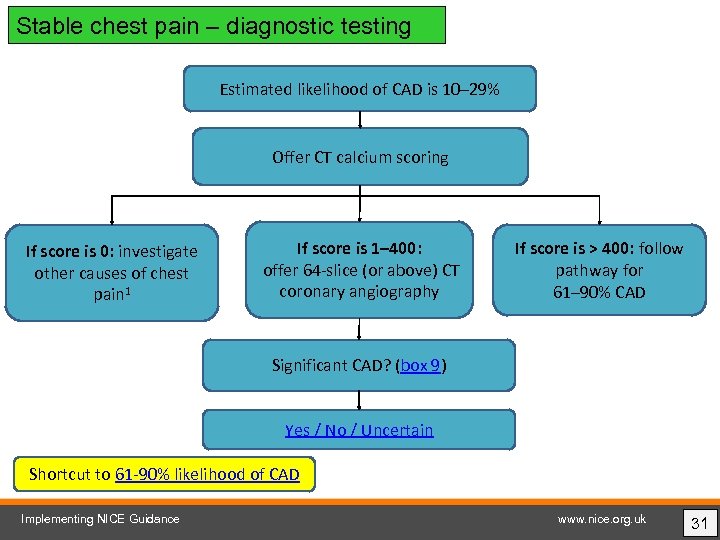 Stable chest pain – diagnostic testing Estimated likelihood of CAD is 10– 29% Offer CT calcium scoring If score is 0: investigate other causes of chest pain 1 If score is 1– 400: offer 64 -slice (or above) CT coronary angiography If score is > 400: follow pathway for 61– 90% CAD Significant CAD? (box 9) Yes / No / Uncertain Shortcut to 61 -90% likelihood of CAD Implementing NICE Guidance www. nice. org. uk 31
Stable chest pain – diagnostic testing Estimated likelihood of CAD is 10– 29% Offer CT calcium scoring If score is 0: investigate other causes of chest pain 1 If score is 1– 400: offer 64 -slice (or above) CT coronary angiography If score is > 400: follow pathway for 61– 90% CAD Significant CAD? (box 9) Yes / No / Uncertain Shortcut to 61 -90% likelihood of CAD Implementing NICE Guidance www. nice. org. uk 31
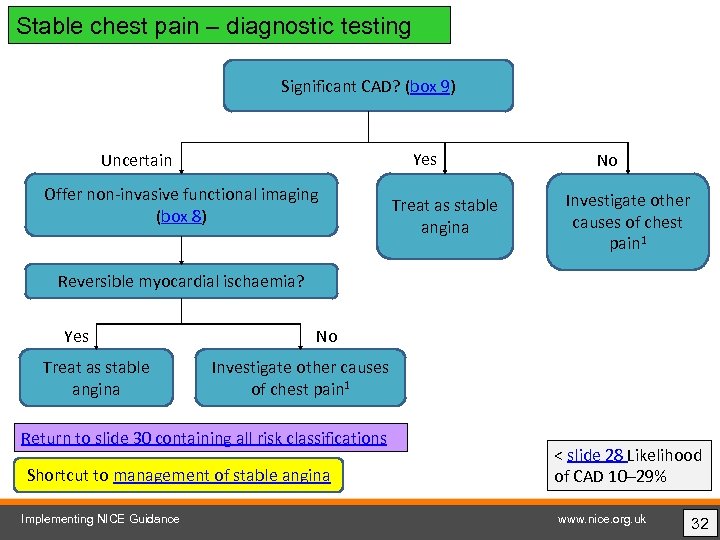 Stable chest pain – diagnostic testing Significant CAD? (box 9) Yes Uncertain Offer non-invasive functional imaging (box 8) Treat as stable angina No Investigate other causes of chest pain 1 Reversible myocardial ischaemia? Yes Treat as stable angina No Investigate other causes of chest pain 1 Return to slide 30 containing all risk classifications Shortcut to management of stable angina Implementing NICE Guidance < slide 28 Likelihood of CAD 10– 29% www. nice. org. uk 32
Stable chest pain – diagnostic testing Significant CAD? (box 9) Yes Uncertain Offer non-invasive functional imaging (box 8) Treat as stable angina No Investigate other causes of chest pain 1 Reversible myocardial ischaemia? Yes Treat as stable angina No Investigate other causes of chest pain 1 Return to slide 30 containing all risk classifications Shortcut to management of stable angina Implementing NICE Guidance < slide 28 Likelihood of CAD 10– 29% www. nice. org. uk 32
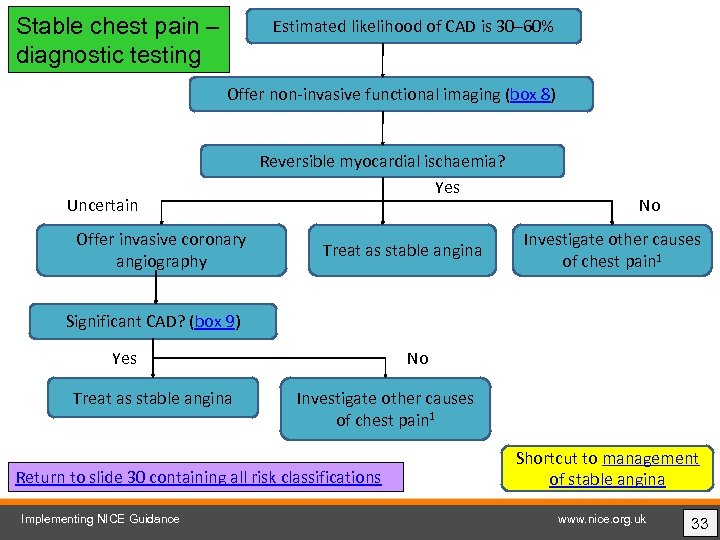 Stable chest pain – diagnostic testing Estimated likelihood of CAD is 30– 60% Offer non-invasive functional imaging (box 8) Uncertain Offer invasive coronary angiography Reversible myocardial ischaemia? Yes Treat as stable angina No Investigate other causes of chest pain 1 Significant CAD? (box 9) Yes Treat as stable angina No Investigate other causes of chest pain 1 Return to slide 30 containing all risk classifications Implementing NICE Guidance Shortcut to management of stable angina www. nice. org. uk 33
Stable chest pain – diagnostic testing Estimated likelihood of CAD is 30– 60% Offer non-invasive functional imaging (box 8) Uncertain Offer invasive coronary angiography Reversible myocardial ischaemia? Yes Treat as stable angina No Investigate other causes of chest pain 1 Significant CAD? (box 9) Yes Treat as stable angina No Investigate other causes of chest pain 1 Return to slide 30 containing all risk classifications Implementing NICE Guidance Shortcut to management of stable angina www. nice. org. uk 33
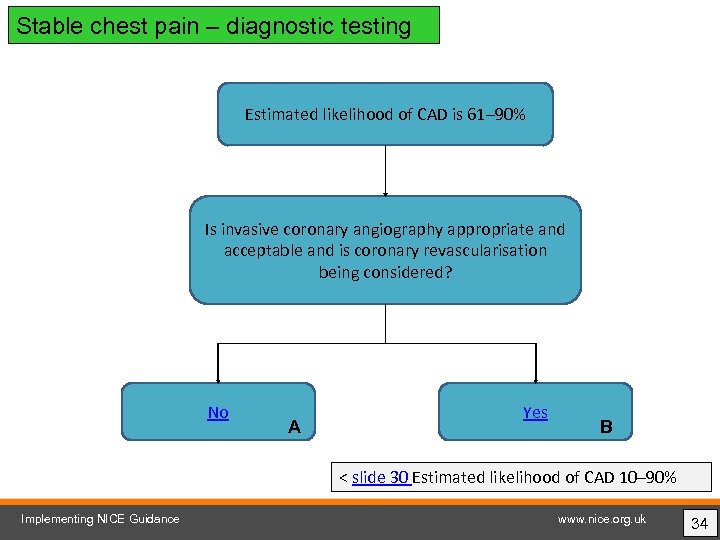 Stable chest pain – diagnostic testing Estimated likelihood of CAD is 61– 90% Is invasive coronary angiography appropriate and acceptable and is coronary revascularisation being considered? No A Yes B < slide 30 Estimated likelihood of CAD 10– 90% Implementing NICE Guidance www. nice. org. uk 34
Stable chest pain – diagnostic testing Estimated likelihood of CAD is 61– 90% Is invasive coronary angiography appropriate and acceptable and is coronary revascularisation being considered? No A Yes B < slide 30 Estimated likelihood of CAD 10– 90% Implementing NICE Guidance www. nice. org. uk 34
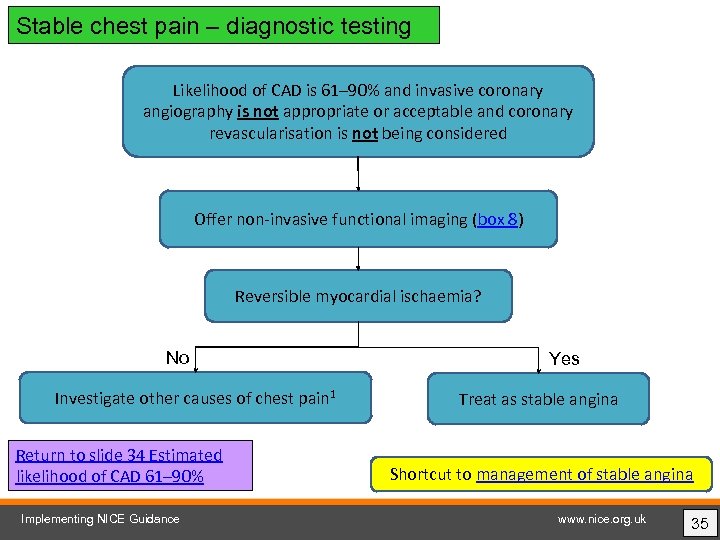 Stable chest pain – diagnostic testing Likelihood of CAD is 61– 90% and invasive coronary angiography is not appropriate or acceptable and coronary revascularisation is not being considered Offer non-invasive functional imaging (box 8) Reversible myocardial ischaemia? No Investigate other causes of chest pain 1 Return to slide 34 Estimated likelihood of CAD 61– 90% Implementing NICE Guidance Yes Treat as stable angina Shortcut to management of stable angina www. nice. org. uk 35
Stable chest pain – diagnostic testing Likelihood of CAD is 61– 90% and invasive coronary angiography is not appropriate or acceptable and coronary revascularisation is not being considered Offer non-invasive functional imaging (box 8) Reversible myocardial ischaemia? No Investigate other causes of chest pain 1 Return to slide 34 Estimated likelihood of CAD 61– 90% Implementing NICE Guidance Yes Treat as stable angina Shortcut to management of stable angina www. nice. org. uk 35
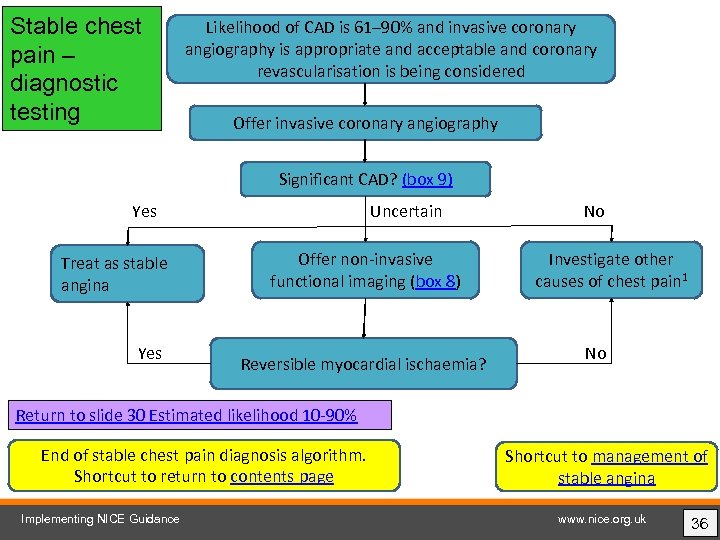 Stable chest pain – diagnostic testing Likelihood of CAD is 61– 90% and invasive coronary angiography is appropriate and acceptable and coronary revascularisation is being considered Offer invasive coronary angiography Significant CAD? (box 9) Yes Treat as stable angina Yes Uncertain Offer non-invasive functional imaging (box 8) Reversible myocardial ischaemia? No Investigate other causes of chest pain 1 No Return to slide 30 Estimated likelihood 10 -90% End of stable chest pain diagnosis algorithm. Shortcut to return to contents page Implementing NICE Guidance Shortcut to management of stable angina www. nice. org. uk 36
Stable chest pain – diagnostic testing Likelihood of CAD is 61– 90% and invasive coronary angiography is appropriate and acceptable and coronary revascularisation is being considered Offer invasive coronary angiography Significant CAD? (box 9) Yes Treat as stable angina Yes Uncertain Offer non-invasive functional imaging (box 8) Reversible myocardial ischaemia? No Investigate other causes of chest pain 1 No Return to slide 30 Estimated likelihood 10 -90% End of stable chest pain diagnosis algorithm. Shortcut to return to contents page Implementing NICE Guidance Shortcut to management of stable angina www. nice. org. uk 36
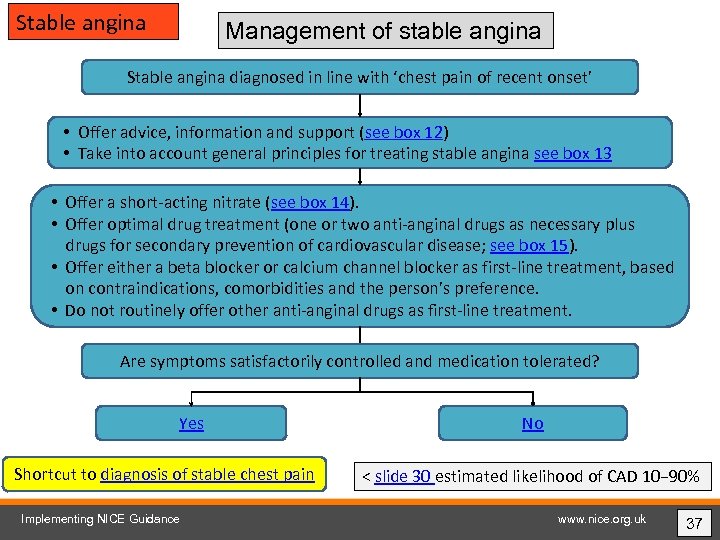 Stable angina Management of stable angina Stable angina diagnosed in line with ‘chest pain of recent onset’ • Offer advice, information and support (see box 12) • Take into account general principles for treating stable angina see box 13 • Offer a short-acting nitrate (see box 14). • Offer optimal drug treatment (one or two anti-anginal drugs as necessary plus drugs for secondary prevention of cardiovascular disease; see box 15). • Offer either a beta blocker or calcium channel blocker as first-line treatment, based on contraindications, comorbidities and the person’s preference. • Do not routinely offer other anti-anginal drugs as first-line treatment. Are symptoms satisfactorily controlled and medication tolerated? Yes Shortcut to diagnosis of stable chest pain Implementing NICE Guidance No < slide 30 estimated likelihood of CAD 10− 90% www. nice. org. uk 37
Stable angina Management of stable angina Stable angina diagnosed in line with ‘chest pain of recent onset’ • Offer advice, information and support (see box 12) • Take into account general principles for treating stable angina see box 13 • Offer a short-acting nitrate (see box 14). • Offer optimal drug treatment (one or two anti-anginal drugs as necessary plus drugs for secondary prevention of cardiovascular disease; see box 15). • Offer either a beta blocker or calcium channel blocker as first-line treatment, based on contraindications, comorbidities and the person’s preference. • Do not routinely offer other anti-anginal drugs as first-line treatment. Are symptoms satisfactorily controlled and medication tolerated? Yes Shortcut to diagnosis of stable chest pain Implementing NICE Guidance No < slide 30 estimated likelihood of CAD 10− 90% www. nice. org. uk 37
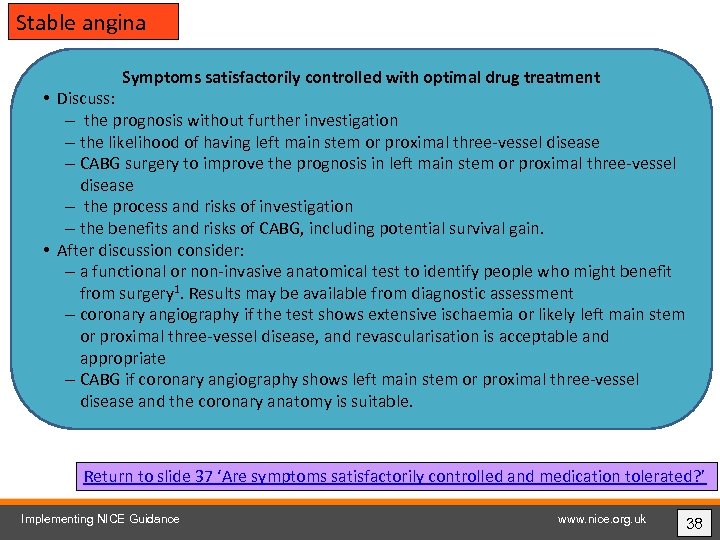 Stable angina Symptoms satisfactorily controlled with optimal drug treatment • Discuss: – the prognosis without further investigation – the likelihood of having left main stem or proximal three-vessel disease – CABG surgery to improve the prognosis in left main stem or proximal three-vessel disease – the process and risks of investigation – the benefits and risks of CABG, including potential survival gain. • After discussion consider: – a functional or non-invasive anatomical test to identify people who might benefit from surgery 1. Results may be available from diagnostic assessment – coronary angiography if the test shows extensive ischaemia or likely left main stem or proximal three-vessel disease, and revascularisation is acceptable and appropriate – CABG if coronary angiography shows left main stem or proximal three-vessel disease and the coronary anatomy is suitable. Return to slide 37 ‘Are symptoms satisfactorily controlled and medication tolerated? ’ Implementing NICE Guidance www. nice. org. uk 38
Stable angina Symptoms satisfactorily controlled with optimal drug treatment • Discuss: – the prognosis without further investigation – the likelihood of having left main stem or proximal three-vessel disease – CABG surgery to improve the prognosis in left main stem or proximal three-vessel disease – the process and risks of investigation – the benefits and risks of CABG, including potential survival gain. • After discussion consider: – a functional or non-invasive anatomical test to identify people who might benefit from surgery 1. Results may be available from diagnostic assessment – coronary angiography if the test shows extensive ischaemia or likely left main stem or proximal three-vessel disease, and revascularisation is acceptable and appropriate – CABG if coronary angiography shows left main stem or proximal three-vessel disease and the coronary anatomy is suitable. Return to slide 37 ‘Are symptoms satisfactorily controlled and medication tolerated? ’ Implementing NICE Guidance www. nice. org. uk 38
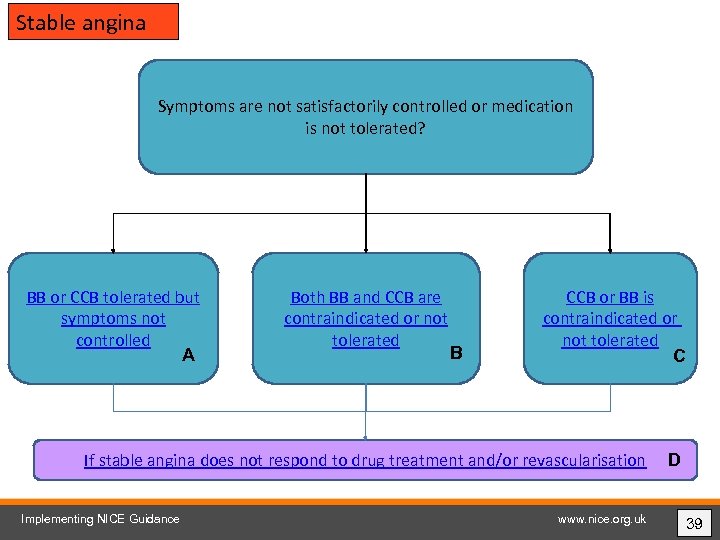 Stable angina Symptoms are not satisfactorily controlled or medication is not tolerated? BB or CCB tolerated but symptoms not controlled A Both BB and CCB are contraindicated or not tolerated B CCB or BB is contraindicated or not tolerated C If stable angina does not respond to drug treatment and/or revascularisation Implementing NICE Guidance www. nice. org. uk D 39
Stable angina Symptoms are not satisfactorily controlled or medication is not tolerated? BB or CCB tolerated but symptoms not controlled A Both BB and CCB are contraindicated or not tolerated B CCB or BB is contraindicated or not tolerated C If stable angina does not respond to drug treatment and/or revascularisation Implementing NICE Guidance www. nice. org. uk D 39
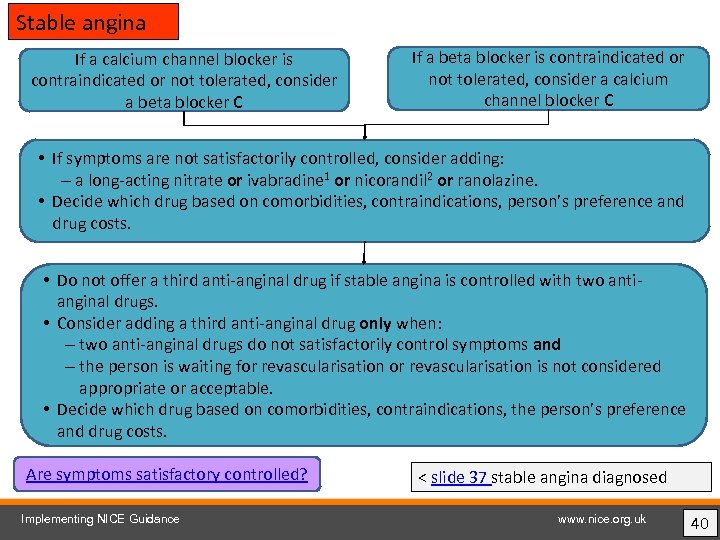 Stable angina If a calcium channel blocker is contraindicated or not tolerated, consider a beta blocker C If a beta blocker is contraindicated or not tolerated, consider a calcium channel blocker C • If symptoms are not satisfactorily controlled, consider adding: – a long-acting nitrate or ivabradine 1 or nicorandil 2 or ranolazine. • Decide which drug based on comorbidities, contraindications, person’s preference and drug costs. • Do not offer a third anti-anginal drug if stable angina is controlled with two antianginal drugs. • Consider adding a third anti-anginal drug only when: – two anti-anginal drugs do not satisfactorily control symptoms and – the person is waiting for revascularisation is not considered appropriate or acceptable. • Decide which drug based on comorbidities, contraindications, the person’s preference and drug costs. Are symptoms satisfactory controlled? Implementing NICE Guidance < slide 37 stable angina diagnosed www. nice. org. uk 40
Stable angina If a calcium channel blocker is contraindicated or not tolerated, consider a beta blocker C If a beta blocker is contraindicated or not tolerated, consider a calcium channel blocker C • If symptoms are not satisfactorily controlled, consider adding: – a long-acting nitrate or ivabradine 1 or nicorandil 2 or ranolazine. • Decide which drug based on comorbidities, contraindications, person’s preference and drug costs. • Do not offer a third anti-anginal drug if stable angina is controlled with two antianginal drugs. • Consider adding a third anti-anginal drug only when: – two anti-anginal drugs do not satisfactorily control symptoms and – the person is waiting for revascularisation is not considered appropriate or acceptable. • Decide which drug based on comorbidities, contraindications, the person’s preference and drug costs. Are symptoms satisfactory controlled? Implementing NICE Guidance < slide 37 stable angina diagnosed www. nice. org. uk 40
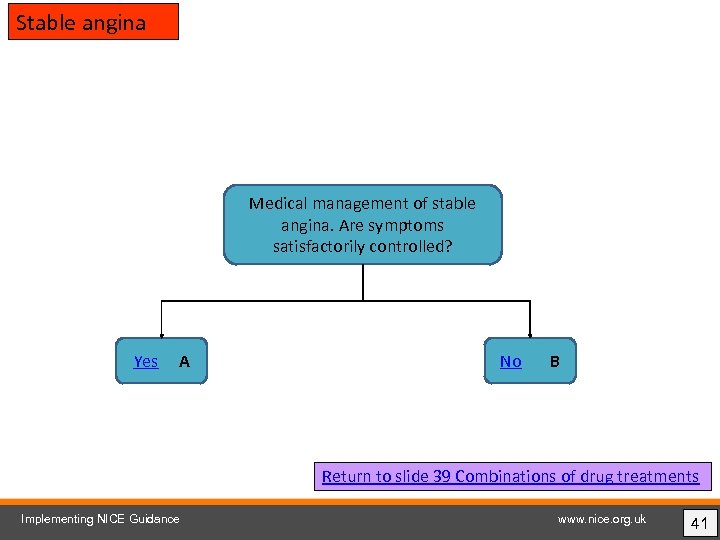 Stable angina Medical management of stable angina. Are symptoms satisfactorily controlled? Yes A No B Return to slide 39 Combinations of drug treatments Implementing NICE Guidance www. nice. org. uk 41
Stable angina Medical management of stable angina. Are symptoms satisfactorily controlled? Yes A No B Return to slide 39 Combinations of drug treatments Implementing NICE Guidance www. nice. org. uk 41
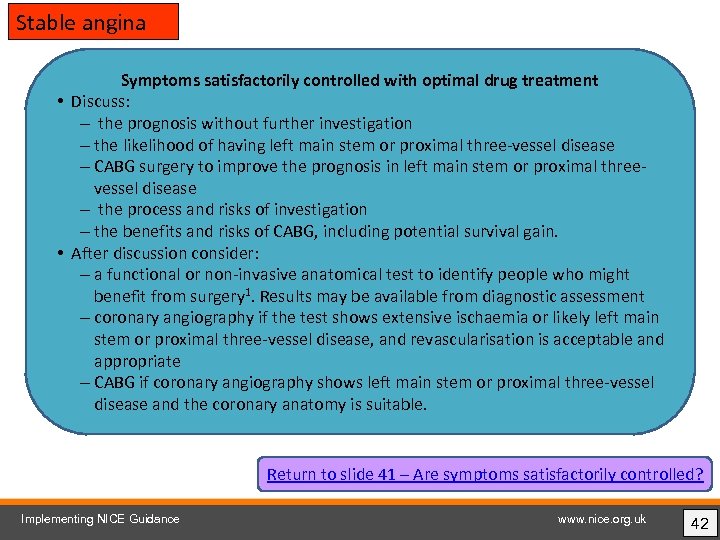 Stable angina Symptoms satisfactorily controlled with optimal drug treatment • Discuss: – the prognosis without further investigation – the likelihood of having left main stem or proximal three-vessel disease – CABG surgery to improve the prognosis in left main stem or proximal threevessel disease – the process and risks of investigation – the benefits and risks of CABG, including potential survival gain. • After discussion consider: – a functional or non-invasive anatomical test to identify people who might benefit from surgery 1. Results may be available from diagnostic assessment – coronary angiography if the test shows extensive ischaemia or likely left main stem or proximal three-vessel disease, and revascularisation is acceptable and appropriate – CABG if coronary angiography shows left main stem or proximal three-vessel disease and the coronary anatomy is suitable. Return to slide 41 – Are symptoms satisfactorily controlled? Implementing NICE Guidance www. nice. org. uk 42
Stable angina Symptoms satisfactorily controlled with optimal drug treatment • Discuss: – the prognosis without further investigation – the likelihood of having left main stem or proximal three-vessel disease – CABG surgery to improve the prognosis in left main stem or proximal threevessel disease – the process and risks of investigation – the benefits and risks of CABG, including potential survival gain. • After discussion consider: – a functional or non-invasive anatomical test to identify people who might benefit from surgery 1. Results may be available from diagnostic assessment – coronary angiography if the test shows extensive ischaemia or likely left main stem or proximal three-vessel disease, and revascularisation is acceptable and appropriate – CABG if coronary angiography shows left main stem or proximal three-vessel disease and the coronary anatomy is suitable. Return to slide 41 – Are symptoms satisfactorily controlled? Implementing NICE Guidance www. nice. org. uk 42
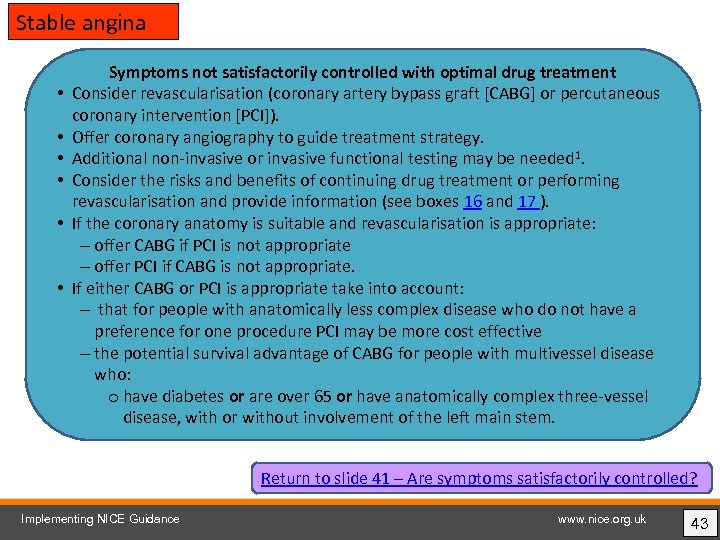 Stable angina • • • Symptoms not satisfactorily controlled with optimal drug treatment Consider revascularisation (coronary artery bypass graft [CABG] or percutaneous coronary intervention [PCI]). Offer coronary angiography to guide treatment strategy. Additional non-invasive or invasive functional testing may be needed 1. Consider the risks and benefits of continuing drug treatment or performing revascularisation and provide information (see boxes 16 and 17 ). If the coronary anatomy is suitable and revascularisation is appropriate: – offer CABG if PCI is not appropriate – offer PCI if CABG is not appropriate. If either CABG or PCI is appropriate take into account: – that for people with anatomically less complex disease who do not have a preference for one procedure PCI may be more cost effective – the potential survival advantage of CABG for people with multivessel disease who: o have diabetes or are over 65 or have anatomically complex three-vessel disease, with or without involvement of the left main stem. Return to slide 41 – Are symptoms satisfactorily controlled? Implementing NICE Guidance www. nice. org. uk 43
Stable angina • • • Symptoms not satisfactorily controlled with optimal drug treatment Consider revascularisation (coronary artery bypass graft [CABG] or percutaneous coronary intervention [PCI]). Offer coronary angiography to guide treatment strategy. Additional non-invasive or invasive functional testing may be needed 1. Consider the risks and benefits of continuing drug treatment or performing revascularisation and provide information (see boxes 16 and 17 ). If the coronary anatomy is suitable and revascularisation is appropriate: – offer CABG if PCI is not appropriate – offer PCI if CABG is not appropriate. If either CABG or PCI is appropriate take into account: – that for people with anatomically less complex disease who do not have a preference for one procedure PCI may be more cost effective – the potential survival advantage of CABG for people with multivessel disease who: o have diabetes or are over 65 or have anatomically complex three-vessel disease, with or without involvement of the left main stem. Return to slide 41 – Are symptoms satisfactorily controlled? Implementing NICE Guidance www. nice. org. uk 43
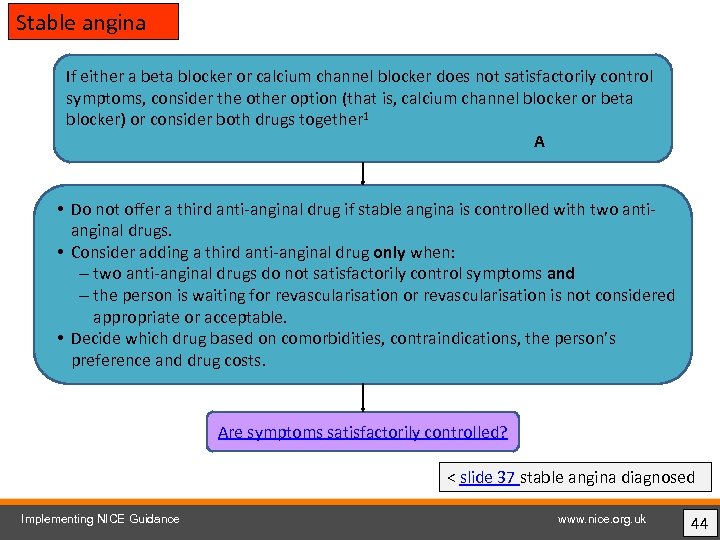 Stable angina If either a beta blocker or calcium channel blocker does not satisfactorily control symptoms, consider the other option (that is, calcium channel blocker or beta blocker) or consider both drugs together 1 A • Do not offer a third anti-anginal drug if stable angina is controlled with two antianginal drugs. • Consider adding a third anti-anginal drug only when: – two anti-anginal drugs do not satisfactorily control symptoms and – the person is waiting for revascularisation is not considered appropriate or acceptable. • Decide which drug based on comorbidities, contraindications, the person’s preference and drug costs. Are symptoms satisfactorily controlled? < slide 37 stable angina diagnosed Implementing NICE Guidance www. nice. org. uk 44
Stable angina If either a beta blocker or calcium channel blocker does not satisfactorily control symptoms, consider the other option (that is, calcium channel blocker or beta blocker) or consider both drugs together 1 A • Do not offer a third anti-anginal drug if stable angina is controlled with two antianginal drugs. • Consider adding a third anti-anginal drug only when: – two anti-anginal drugs do not satisfactorily control symptoms and – the person is waiting for revascularisation is not considered appropriate or acceptable. • Decide which drug based on comorbidities, contraindications, the person’s preference and drug costs. Are symptoms satisfactorily controlled? < slide 37 stable angina diagnosed Implementing NICE Guidance www. nice. org. uk 44
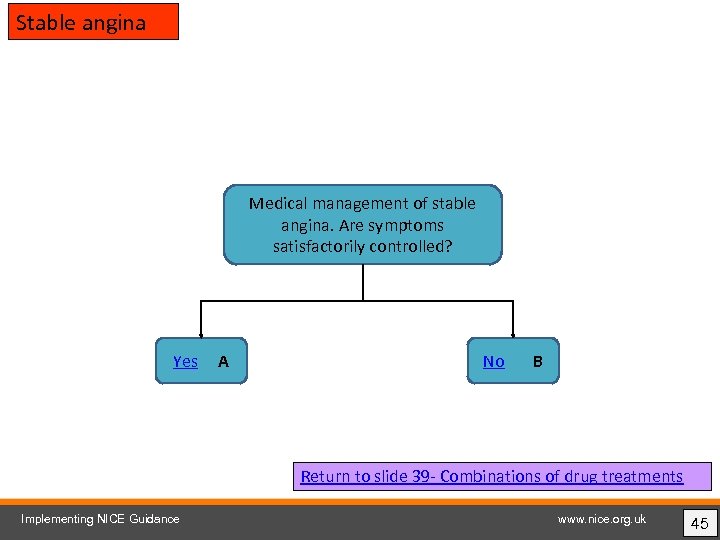 Stable angina Medical management of stable angina. Are symptoms satisfactorily controlled? Yes A No B Return to slide 39 - Combinations of drug treatments Implementing NICE Guidance www. nice. org. uk 45
Stable angina Medical management of stable angina. Are symptoms satisfactorily controlled? Yes A No B Return to slide 39 - Combinations of drug treatments Implementing NICE Guidance www. nice. org. uk 45
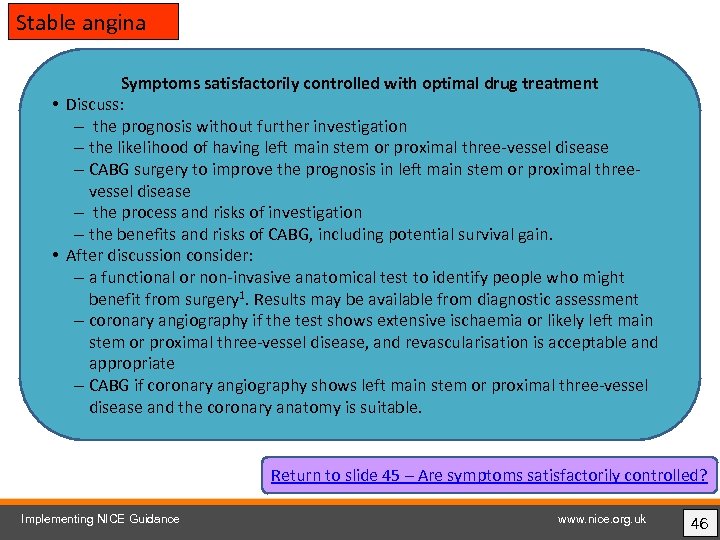 Stable angina Symptoms satisfactorily controlled with optimal drug treatment • Discuss: – the prognosis without further investigation – the likelihood of having left main stem or proximal three-vessel disease – CABG surgery to improve the prognosis in left main stem or proximal threevessel disease – the process and risks of investigation – the benefits and risks of CABG, including potential survival gain. • After discussion consider: – a functional or non-invasive anatomical test to identify people who might benefit from surgery 1. Results may be available from diagnostic assessment – coronary angiography if the test shows extensive ischaemia or likely left main stem or proximal three-vessel disease, and revascularisation is acceptable and appropriate – CABG if coronary angiography shows left main stem or proximal three-vessel disease and the coronary anatomy is suitable. Return to slide 45 – Are symptoms satisfactorily controlled? Implementing NICE Guidance www. nice. org. uk 46
Stable angina Symptoms satisfactorily controlled with optimal drug treatment • Discuss: – the prognosis without further investigation – the likelihood of having left main stem or proximal three-vessel disease – CABG surgery to improve the prognosis in left main stem or proximal threevessel disease – the process and risks of investigation – the benefits and risks of CABG, including potential survival gain. • After discussion consider: – a functional or non-invasive anatomical test to identify people who might benefit from surgery 1. Results may be available from diagnostic assessment – coronary angiography if the test shows extensive ischaemia or likely left main stem or proximal three-vessel disease, and revascularisation is acceptable and appropriate – CABG if coronary angiography shows left main stem or proximal three-vessel disease and the coronary anatomy is suitable. Return to slide 45 – Are symptoms satisfactorily controlled? Implementing NICE Guidance www. nice. org. uk 46
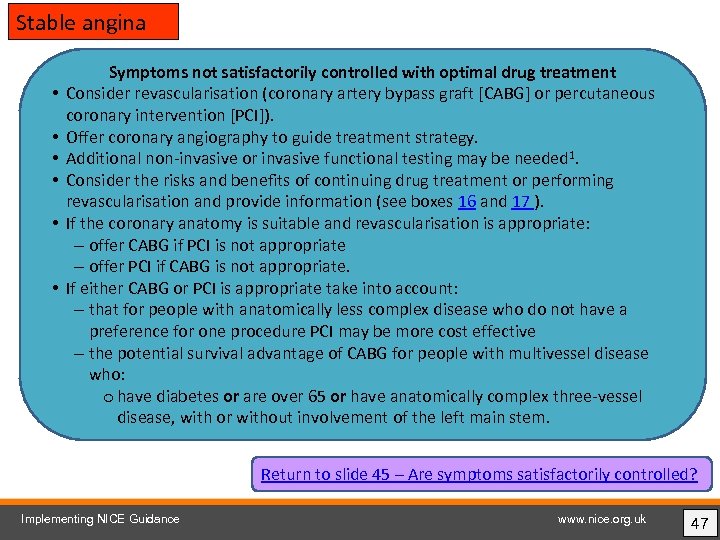 Stable angina • • • Symptoms not satisfactorily controlled with optimal drug treatment Consider revascularisation (coronary artery bypass graft [CABG] or percutaneous coronary intervention [PCI]). Offer coronary angiography to guide treatment strategy. Additional non-invasive or invasive functional testing may be needed 1. Consider the risks and benefits of continuing drug treatment or performing revascularisation and provide information (see boxes 16 and 17 ). If the coronary anatomy is suitable and revascularisation is appropriate: – offer CABG if PCI is not appropriate – offer PCI if CABG is not appropriate. If either CABG or PCI is appropriate take into account: – that for people with anatomically less complex disease who do not have a preference for one procedure PCI may be more cost effective – the potential survival advantage of CABG for people with multivessel disease who: o have diabetes or are over 65 or have anatomically complex three-vessel disease, with or without involvement of the left main stem. Return to slide 45 – Are symptoms satisfactorily controlled? Implementing NICE Guidance www. nice. org. uk 47
Stable angina • • • Symptoms not satisfactorily controlled with optimal drug treatment Consider revascularisation (coronary artery bypass graft [CABG] or percutaneous coronary intervention [PCI]). Offer coronary angiography to guide treatment strategy. Additional non-invasive or invasive functional testing may be needed 1. Consider the risks and benefits of continuing drug treatment or performing revascularisation and provide information (see boxes 16 and 17 ). If the coronary anatomy is suitable and revascularisation is appropriate: – offer CABG if PCI is not appropriate – offer PCI if CABG is not appropriate. If either CABG or PCI is appropriate take into account: – that for people with anatomically less complex disease who do not have a preference for one procedure PCI may be more cost effective – the potential survival advantage of CABG for people with multivessel disease who: o have diabetes or are over 65 or have anatomically complex three-vessel disease, with or without involvement of the left main stem. Return to slide 45 – Are symptoms satisfactorily controlled? Implementing NICE Guidance www. nice. org. uk 47
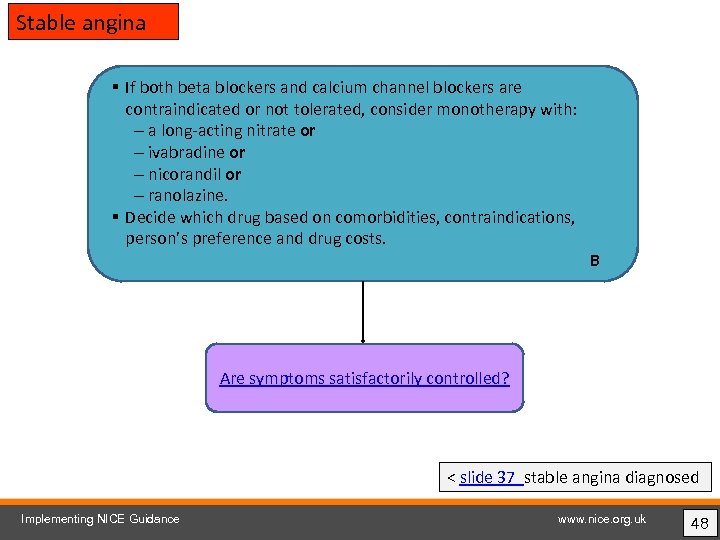 Stable angina § If both beta blockers and calcium channel blockers are contraindicated or not tolerated, consider monotherapy with: – a long-acting nitrate or – ivabradine or – nicorandil or – ranolazine. § Decide which drug based on comorbidities, contraindications, person’s preference and drug costs. B Are symptoms satisfactorily controlled? < slide 37 stable angina diagnosed Implementing NICE Guidance www. nice. org. uk 48
Stable angina § If both beta blockers and calcium channel blockers are contraindicated or not tolerated, consider monotherapy with: – a long-acting nitrate or – ivabradine or – nicorandil or – ranolazine. § Decide which drug based on comorbidities, contraindications, person’s preference and drug costs. B Are symptoms satisfactorily controlled? < slide 37 stable angina diagnosed Implementing NICE Guidance www. nice. org. uk 48
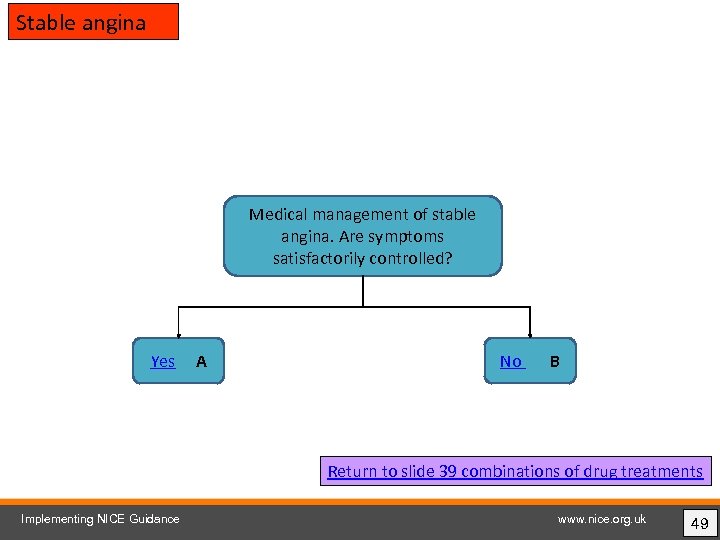 Stable angina Medical management of stable angina. Are symptoms satisfactorily controlled? Yes A No B Return to slide 39 combinations of drug treatments Implementing NICE Guidance www. nice. org. uk 49
Stable angina Medical management of stable angina. Are symptoms satisfactorily controlled? Yes A No B Return to slide 39 combinations of drug treatments Implementing NICE Guidance www. nice. org. uk 49
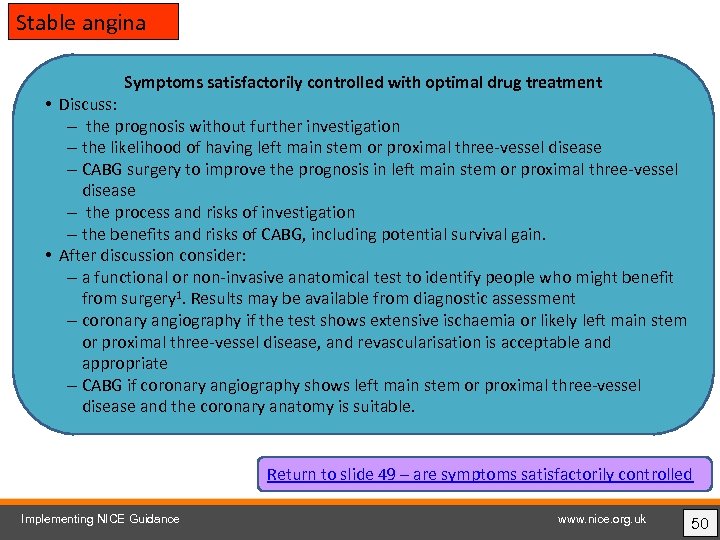 Stable angina Symptoms satisfactorily controlled with optimal drug treatment • Discuss: – the prognosis without further investigation – the likelihood of having left main stem or proximal three-vessel disease – CABG surgery to improve the prognosis in left main stem or proximal three-vessel disease – the process and risks of investigation – the benefits and risks of CABG, including potential survival gain. • After discussion consider: – a functional or non-invasive anatomical test to identify people who might benefit from surgery 1. Results may be available from diagnostic assessment – coronary angiography if the test shows extensive ischaemia or likely left main stem or proximal three-vessel disease, and revascularisation is acceptable and appropriate – CABG if coronary angiography shows left main stem or proximal three-vessel disease and the coronary anatomy is suitable. Return to slide 49 – are symptoms satisfactorily controlled Implementing NICE Guidance www. nice. org. uk 50
Stable angina Symptoms satisfactorily controlled with optimal drug treatment • Discuss: – the prognosis without further investigation – the likelihood of having left main stem or proximal three-vessel disease – CABG surgery to improve the prognosis in left main stem or proximal three-vessel disease – the process and risks of investigation – the benefits and risks of CABG, including potential survival gain. • After discussion consider: – a functional or non-invasive anatomical test to identify people who might benefit from surgery 1. Results may be available from diagnostic assessment – coronary angiography if the test shows extensive ischaemia or likely left main stem or proximal three-vessel disease, and revascularisation is acceptable and appropriate – CABG if coronary angiography shows left main stem or proximal three-vessel disease and the coronary anatomy is suitable. Return to slide 49 – are symptoms satisfactorily controlled Implementing NICE Guidance www. nice. org. uk 50
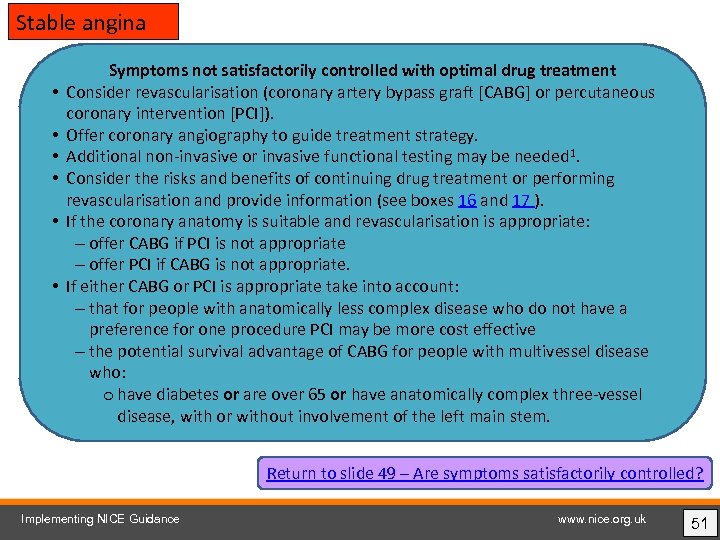 Stable angina • • • Symptoms not satisfactorily controlled with optimal drug treatment Consider revascularisation (coronary artery bypass graft [CABG] or percutaneous coronary intervention [PCI]). Offer coronary angiography to guide treatment strategy. Additional non-invasive or invasive functional testing may be needed 1. Consider the risks and benefits of continuing drug treatment or performing revascularisation and provide information (see boxes 16 and 17 ). If the coronary anatomy is suitable and revascularisation is appropriate: – offer CABG if PCI is not appropriate – offer PCI if CABG is not appropriate. If either CABG or PCI is appropriate take into account: – that for people with anatomically less complex disease who do not have a preference for one procedure PCI may be more cost effective – the potential survival advantage of CABG for people with multivessel disease who: o have diabetes or are over 65 or have anatomically complex three-vessel disease, with or without involvement of the left main stem. Return to slide 49 – Are symptoms satisfactorily controlled? Implementing NICE Guidance www. nice. org. uk 51
Stable angina • • • Symptoms not satisfactorily controlled with optimal drug treatment Consider revascularisation (coronary artery bypass graft [CABG] or percutaneous coronary intervention [PCI]). Offer coronary angiography to guide treatment strategy. Additional non-invasive or invasive functional testing may be needed 1. Consider the risks and benefits of continuing drug treatment or performing revascularisation and provide information (see boxes 16 and 17 ). If the coronary anatomy is suitable and revascularisation is appropriate: – offer CABG if PCI is not appropriate – offer PCI if CABG is not appropriate. If either CABG or PCI is appropriate take into account: – that for people with anatomically less complex disease who do not have a preference for one procedure PCI may be more cost effective – the potential survival advantage of CABG for people with multivessel disease who: o have diabetes or are over 65 or have anatomically complex three-vessel disease, with or without involvement of the left main stem. Return to slide 49 – Are symptoms satisfactorily controlled? Implementing NICE Guidance www. nice. org. uk 51
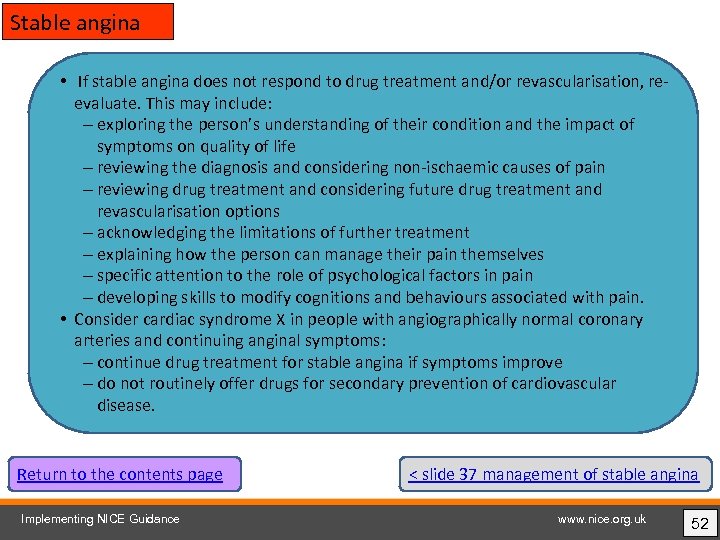 Stable angina • If stable angina does not respond to drug treatment and/or revascularisation, reevaluate. This may include: – exploring the person’s understanding of their condition and the impact of symptoms on quality of life – reviewing the diagnosis and considering non-ischaemic causes of pain – reviewing drug treatment and considering future drug treatment and revascularisation options – acknowledging the limitations of further treatment – explaining how the person can manage their pain themselves – specific attention to the role of psychological factors in pain – developing skills to modify cognitions and behaviours associated with pain. • Consider cardiac syndrome X in people with angiographically normal coronary arteries and continuing anginal symptoms: – continue drug treatment for stable angina if symptoms improve – do not routinely offer drugs for secondary prevention of cardiovascular disease. Return to the contents page Implementing NICE Guidance < slide 37 management of stable angina www. nice. org. uk 52
Stable angina • If stable angina does not respond to drug treatment and/or revascularisation, reevaluate. This may include: – exploring the person’s understanding of their condition and the impact of symptoms on quality of life – reviewing the diagnosis and considering non-ischaemic causes of pain – reviewing drug treatment and considering future drug treatment and revascularisation options – acknowledging the limitations of further treatment – explaining how the person can manage their pain themselves – specific attention to the role of psychological factors in pain – developing skills to modify cognitions and behaviours associated with pain. • Consider cardiac syndrome X in people with angiographically normal coronary arteries and continuing anginal symptoms: – continue drug treatment for stable angina if symptoms improve – do not routinely offer drugs for secondary prevention of cardiovascular disease. Return to the contents page Implementing NICE Guidance < slide 37 management of stable angina www. nice. org. uk 52
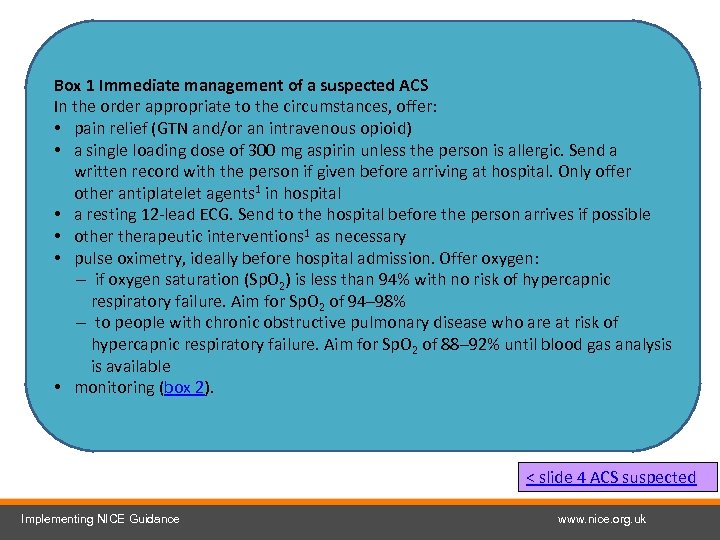 Box 1 Immediate management of a suspected ACS In the order appropriate to the circumstances, offer: • pain relief (GTN and/or an intravenous opioid) • a single loading dose of 300 mg aspirin unless the person is allergic. Send a written record with the person if given before arriving at hospital. Only offer other antiplatelet agents 1 in hospital • a resting 12 -lead ECG. Send to the hospital before the person arrives if possible • otherapeutic interventions 1 as necessary • pulse oximetry, ideally before hospital admission. Offer oxygen: – if oxygen saturation (Sp. O 2) is less than 94% with no risk of hypercapnic respiratory failure. Aim for Sp. O 2 of 94– 98% – to people with chronic obstructive pulmonary disease who are at risk of hypercapnic respiratory failure. Aim for Sp. O 2 of 88– 92% until blood gas analysis is available • monitoring (box 2). < slide 4 ACS suspected Implementing NICE Guidance www. nice. org. uk
Box 1 Immediate management of a suspected ACS In the order appropriate to the circumstances, offer: • pain relief (GTN and/or an intravenous opioid) • a single loading dose of 300 mg aspirin unless the person is allergic. Send a written record with the person if given before arriving at hospital. Only offer other antiplatelet agents 1 in hospital • a resting 12 -lead ECG. Send to the hospital before the person arrives if possible • otherapeutic interventions 1 as necessary • pulse oximetry, ideally before hospital admission. Offer oxygen: – if oxygen saturation (Sp. O 2) is less than 94% with no risk of hypercapnic respiratory failure. Aim for Sp. O 2 of 94– 98% – to people with chronic obstructive pulmonary disease who are at risk of hypercapnic respiratory failure. Aim for Sp. O 2 of 88– 92% until blood gas analysis is available • monitoring (box 2). < slide 4 ACS suspected Implementing NICE Guidance www. nice. org. uk
 Box 2 Monitor until diagnosis • Include: – exacerbations of pain and/or other symptoms – pulse and blood pressure – heart rhythm – oxygen saturation by pulse oximetry – repeated resting 12 -lead ECGs – checking pain relief is effective. • Decide how often this should be done. < box 1 Immediate management Implementing NICE Guidance www. nice. org. uk
Box 2 Monitor until diagnosis • Include: – exacerbations of pain and/or other symptoms – pulse and blood pressure – heart rhythm – oxygen saturation by pulse oximetry – repeated resting 12 -lead ECGs – checking pain relief is effective. • Decide how often this should be done. < box 1 Immediate management Implementing NICE Guidance www. nice. org. uk
 Box 2 Monitor until diagnosis • Include: – exacerbations of pain and/or other symptoms – pulse and blood pressure – heart rhythm – oxygen saturation by pulse oximetry – repeated resting 12 -lead ECGs – checking pain relief is effective. • Decide how often this should be done. < slide 8 Initial assessment Implementing NICE Guidance www. nice. org. uk
Box 2 Monitor until diagnosis • Include: – exacerbations of pain and/or other symptoms – pulse and blood pressure – heart rhythm – oxygen saturation by pulse oximetry – repeated resting 12 -lead ECGs – checking pain relief is effective. • Decide how often this should be done. < slide 8 Initial assessment Implementing NICE Guidance www. nice. org. uk
 Box 2 Monitor until diagnosis • Include: – exacerbations of pain and/or other symptoms – pulse and blood pressure – heart rhythm – oxygen saturation by pulse oximetry – repeated resting 12 -lead ECGs – checking pain relief is effective. • Decide how often this should be done. < slide 9 ST-segment elevation and new LBBB Implementing NICE Guidance www. nice. org. uk
Box 2 Monitor until diagnosis • Include: – exacerbations of pain and/or other symptoms – pulse and blood pressure – heart rhythm – oxygen saturation by pulse oximetry – repeated resting 12 -lead ECGs – checking pain relief is effective. • Decide how often this should be done. < slide 9 ST-segment elevation and new LBBB Implementing NICE Guidance www. nice. org. uk
 Box 2 Monitor until diagnosis • Include: – exacerbations of pain and/or other symptoms – pulse and blood pressure – heart rhythm – oxygen saturation by pulse oximetry – repeated resting 12 -lead ECGs – checking pain relief is effective. • Decide how often this should be done. < slide 10 yes ST-segment depression or T wave inversion Implementing NICE Guidance www. nice. org. uk
Box 2 Monitor until diagnosis • Include: – exacerbations of pain and/or other symptoms – pulse and blood pressure – heart rhythm – oxygen saturation by pulse oximetry – repeated resting 12 -lead ECGs – checking pain relief is effective. • Decide how often this should be done. < slide 10 yes ST-segment depression or T wave inversion Implementing NICE Guidance www. nice. org. uk
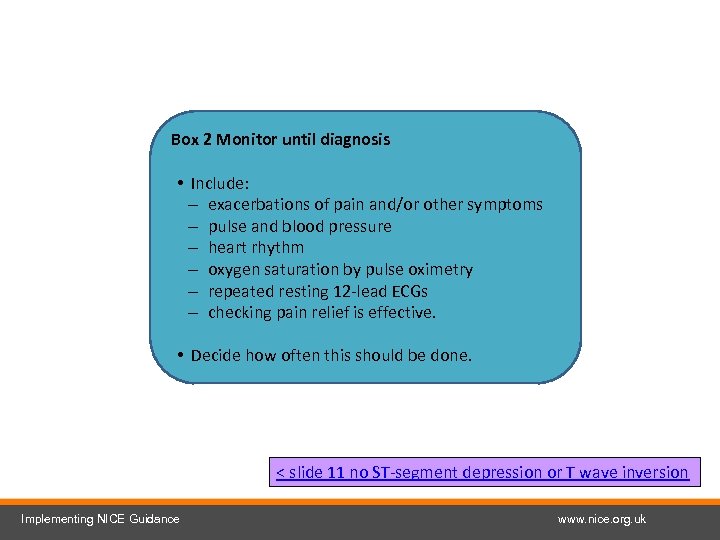 Box 2 Monitor until diagnosis • Include: – exacerbations of pain and/or other symptoms – pulse and blood pressure – heart rhythm – oxygen saturation by pulse oximetry – repeated resting 12 -lead ECGs – checking pain relief is effective. • Decide how often this should be done. < slide 11 no ST-segment depression or T wave inversion Implementing NICE Guidance www. nice. org. uk
Box 2 Monitor until diagnosis • Include: – exacerbations of pain and/or other symptoms – pulse and blood pressure – heart rhythm – oxygen saturation by pulse oximetry – repeated resting 12 -lead ECGs – checking pain relief is effective. • Decide how often this should be done. < slide 11 no ST-segment depression or T wave inversion Implementing NICE Guidance www. nice. org. uk
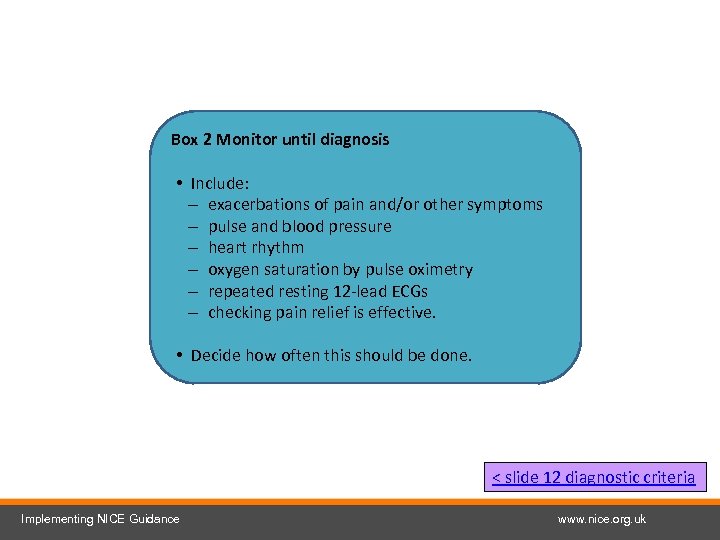 Box 2 Monitor until diagnosis • Include: – exacerbations of pain and/or other symptoms – pulse and blood pressure – heart rhythm – oxygen saturation by pulse oximetry – repeated resting 12 -lead ECGs – checking pain relief is effective. • Decide how often this should be done. < slide 12 diagnostic criteria Implementing NICE Guidance www. nice. org. uk
Box 2 Monitor until diagnosis • Include: – exacerbations of pain and/or other symptoms – pulse and blood pressure – heart rhythm – oxygen saturation by pulse oximetry – repeated resting 12 -lead ECGs – checking pain relief is effective. • Decide how often this should be done. < slide 12 diagnostic criteria Implementing NICE Guidance www. nice. org. uk
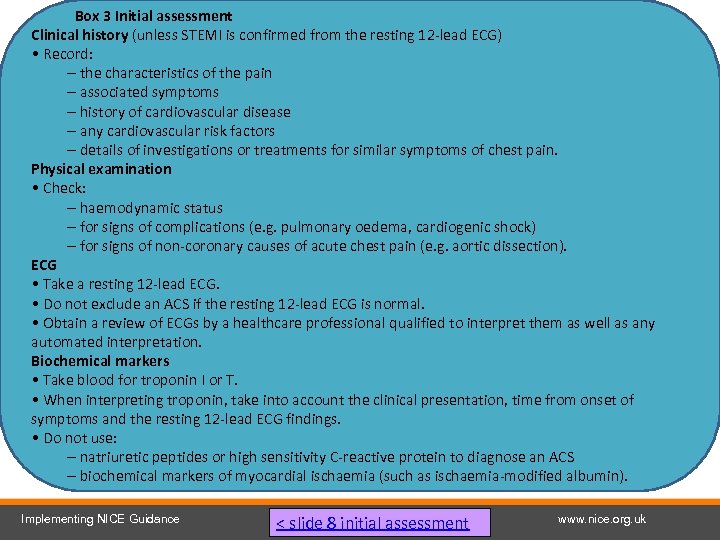 Box 3 Initial assessment Clinical history (unless STEMI is confirmed from the resting 12 -lead ECG) • Record: – the characteristics of the pain – associated symptoms – history of cardiovascular disease – any cardiovascular risk factors – details of investigations or treatments for similar symptoms of chest pain. Physical examination • Check: – haemodynamic status – for signs of complications (e. g. pulmonary oedema, cardiogenic shock) – for signs of non-coronary causes of acute chest pain (e. g. aortic dissection). ECG • Take a resting 12 -lead ECG. • Do not exclude an ACS if the resting 12 -lead ECG is normal. • Obtain a review of ECGs by a healthcare professional qualified to interpret them as well as any automated interpretation. Biochemical markers • Take blood for troponin I or T. • When interpreting troponin, take into account the clinical presentation, time from onset of symptoms and the resting 12 -lead ECG findings. • Do not use: – natriuretic peptides or high sensitivity C-reactive protein to diagnose an ACS – biochemical markers of myocardial ischaemia (such as ischaemia-modified albumin). Implementing NICE Guidance < slide 8 initial assessment www. nice. org. uk
Box 3 Initial assessment Clinical history (unless STEMI is confirmed from the resting 12 -lead ECG) • Record: – the characteristics of the pain – associated symptoms – history of cardiovascular disease – any cardiovascular risk factors – details of investigations or treatments for similar symptoms of chest pain. Physical examination • Check: – haemodynamic status – for signs of complications (e. g. pulmonary oedema, cardiogenic shock) – for signs of non-coronary causes of acute chest pain (e. g. aortic dissection). ECG • Take a resting 12 -lead ECG. • Do not exclude an ACS if the resting 12 -lead ECG is normal. • Obtain a review of ECGs by a healthcare professional qualified to interpret them as well as any automated interpretation. Biochemical markers • Take blood for troponin I or T. • When interpreting troponin, take into account the clinical presentation, time from onset of symptoms and the resting 12 -lead ECG findings. • Do not use: – natriuretic peptides or high sensitivity C-reactive protein to diagnose an ACS – biochemical markers of myocardial ischaemia (such as ischaemia-modified albumin). Implementing NICE Guidance < slide 8 initial assessment www. nice. org. uk
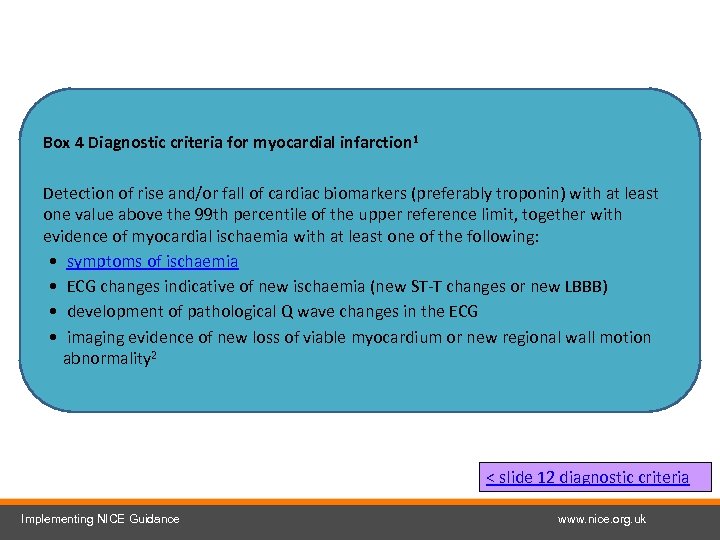 Box 4 Diagnostic criteria for myocardial infarction 1 Detection of rise and/or fall of cardiac biomarkers (preferably troponin) with at least one value above the 99 th percentile of the upper reference limit, together with evidence of myocardial ischaemia with at least one of the following: • symptoms of ischaemia • ECG changes indicative of new ischaemia (new ST-T changes or new LBBB) • development of pathological Q wave changes in the ECG • imaging evidence of new loss of viable myocardium or new regional wall motion abnormality 2 < slide 12 diagnostic criteria Implementing NICE Guidance www. nice. org. uk
Box 4 Diagnostic criteria for myocardial infarction 1 Detection of rise and/or fall of cardiac biomarkers (preferably troponin) with at least one value above the 99 th percentile of the upper reference limit, together with evidence of myocardial ischaemia with at least one of the following: • symptoms of ischaemia • ECG changes indicative of new ischaemia (new ST-T changes or new LBBB) • development of pathological Q wave changes in the ECG • imaging evidence of new loss of viable myocardium or new regional wall motion abnormality 2 < slide 12 diagnostic criteria Implementing NICE Guidance www. nice. org. uk
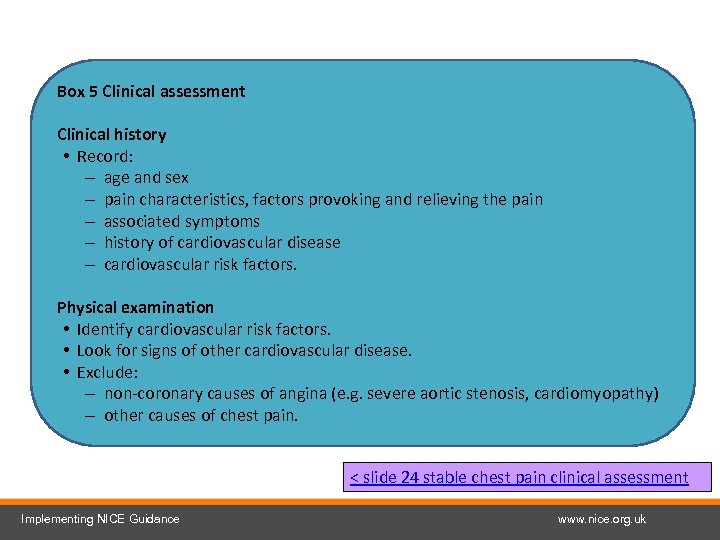 Box 5 Clinical assessment Clinical history • Record: – age and sex – pain characteristics, factors provoking and relieving the pain – associated symptoms – history of cardiovascular disease – cardiovascular risk factors. Physical examination • Identify cardiovascular risk factors. • Look for signs of other cardiovascular disease. • Exclude: – non-coronary causes of angina (e. g. severe aortic stenosis, cardiomyopathy) – other causes of chest pain. < slide 24 stable chest pain clinical assessment Implementing NICE Guidance www. nice. org. uk
Box 5 Clinical assessment Clinical history • Record: – age and sex – pain characteristics, factors provoking and relieving the pain – associated symptoms – history of cardiovascular disease – cardiovascular risk factors. Physical examination • Identify cardiovascular risk factors. • Look for signs of other cardiovascular disease. • Exclude: – non-coronary causes of angina (e. g. severe aortic stenosis, cardiomyopathy) – other causes of chest pain. < slide 24 stable chest pain clinical assessment Implementing NICE Guidance www. nice. org. uk
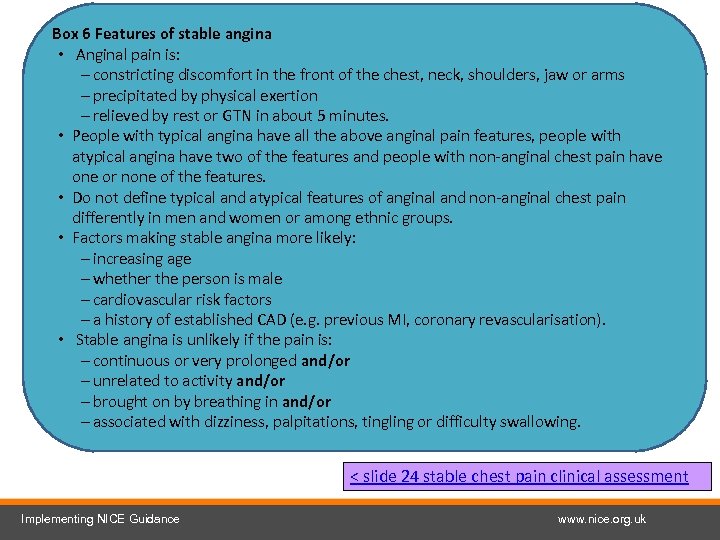 Box 6 Features of stable angina • Anginal pain is: – constricting discomfort in the front of the chest, neck, shoulders, jaw or arms – precipitated by physical exertion – relieved by rest or GTN in about 5 minutes. • People with typical angina have all the above anginal pain features, people with atypical angina have two of the features and people with non-anginal chest pain have one or none of the features. • Do not define typical and atypical features of anginal and non-anginal chest pain differently in men and women or among ethnic groups. • Factors making stable angina more likely: – increasing age – whether the person is male – cardiovascular risk factors – a history of established CAD (e. g. previous MI, coronary revascularisation). • Stable angina is unlikely if the pain is: – continuous or very prolonged and/or – unrelated to activity and/or – brought on by breathing in and/or – associated with dizziness, palpitations, tingling or difficulty swallowing. < slide 24 stable chest pain clinical assessment Implementing NICE Guidance www. nice. org. uk
Box 6 Features of stable angina • Anginal pain is: – constricting discomfort in the front of the chest, neck, shoulders, jaw or arms – precipitated by physical exertion – relieved by rest or GTN in about 5 minutes. • People with typical angina have all the above anginal pain features, people with atypical angina have two of the features and people with non-anginal chest pain have one or none of the features. • Do not define typical and atypical features of anginal and non-anginal chest pain differently in men and women or among ethnic groups. • Factors making stable angina more likely: – increasing age – whether the person is male – cardiovascular risk factors – a history of established CAD (e. g. previous MI, coronary revascularisation). • Stable angina is unlikely if the pain is: – continuous or very prolonged and/or – unrelated to activity and/or – brought on by breathing in and/or – associated with dizziness, palpitations, tingling or difficulty swallowing. < slide 24 stable chest pain clinical assessment Implementing NICE Guidance www. nice. org. uk
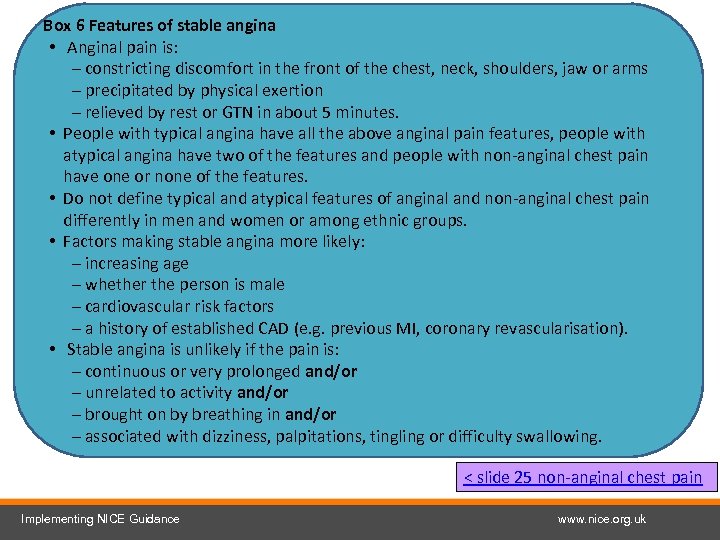 Box 6 Features of stable angina • Anginal pain is: – constricting discomfort in the front of the chest, neck, shoulders, jaw or arms – precipitated by physical exertion – relieved by rest or GTN in about 5 minutes. • People with typical angina have all the above anginal pain features, people with atypical angina have two of the features and people with non-anginal chest pain have one or none of the features. • Do not define typical and atypical features of anginal and non-anginal chest pain differently in men and women or among ethnic groups. • Factors making stable angina more likely: – increasing age – whether the person is male – cardiovascular risk factors – a history of established CAD (e. g. previous MI, coronary revascularisation). • Stable angina is unlikely if the pain is: – continuous or very prolonged and/or – unrelated to activity and/or – brought on by breathing in and/or – associated with dizziness, palpitations, tingling or difficulty swallowing. < slide 25 non-anginal chest pain Implementing NICE Guidance www. nice. org. uk
Box 6 Features of stable angina • Anginal pain is: – constricting discomfort in the front of the chest, neck, shoulders, jaw or arms – precipitated by physical exertion – relieved by rest or GTN in about 5 minutes. • People with typical angina have all the above anginal pain features, people with atypical angina have two of the features and people with non-anginal chest pain have one or none of the features. • Do not define typical and atypical features of anginal and non-anginal chest pain differently in men and women or among ethnic groups. • Factors making stable angina more likely: – increasing age – whether the person is male – cardiovascular risk factors – a history of established CAD (e. g. previous MI, coronary revascularisation). • Stable angina is unlikely if the pain is: – continuous or very prolonged and/or – unrelated to activity and/or – brought on by breathing in and/or – associated with dizziness, palpitations, tingling or difficulty swallowing. < slide 25 non-anginal chest pain Implementing NICE Guidance www. nice. org. uk
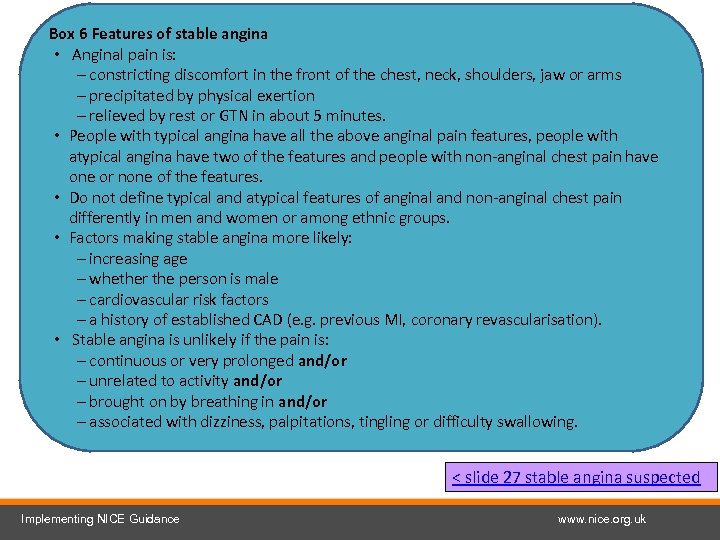 Box 6 Features of stable angina • Anginal pain is: – constricting discomfort in the front of the chest, neck, shoulders, jaw or arms – precipitated by physical exertion – relieved by rest or GTN in about 5 minutes. • People with typical angina have all the above anginal pain features, people with atypical angina have two of the features and people with non-anginal chest pain have one or none of the features. • Do not define typical and atypical features of anginal and non-anginal chest pain differently in men and women or among ethnic groups. • Factors making stable angina more likely: – increasing age – whether the person is male – cardiovascular risk factors – a history of established CAD (e. g. previous MI, coronary revascularisation). • Stable angina is unlikely if the pain is: – continuous or very prolonged and/or – unrelated to activity and/or – brought on by breathing in and/or – associated with dizziness, palpitations, tingling or difficulty swallowing. < slide 27 stable angina suspected Implementing NICE Guidance www. nice. org. uk
Box 6 Features of stable angina • Anginal pain is: – constricting discomfort in the front of the chest, neck, shoulders, jaw or arms – precipitated by physical exertion – relieved by rest or GTN in about 5 minutes. • People with typical angina have all the above anginal pain features, people with atypical angina have two of the features and people with non-anginal chest pain have one or none of the features. • Do not define typical and atypical features of anginal and non-anginal chest pain differently in men and women or among ethnic groups. • Factors making stable angina more likely: – increasing age – whether the person is male – cardiovascular risk factors – a history of established CAD (e. g. previous MI, coronary revascularisation). • Stable angina is unlikely if the pain is: – continuous or very prolonged and/or – unrelated to activity and/or – brought on by breathing in and/or – associated with dizziness, palpitations, tingling or difficulty swallowing. < slide 27 stable angina suspected Implementing NICE Guidance www. nice. org. uk
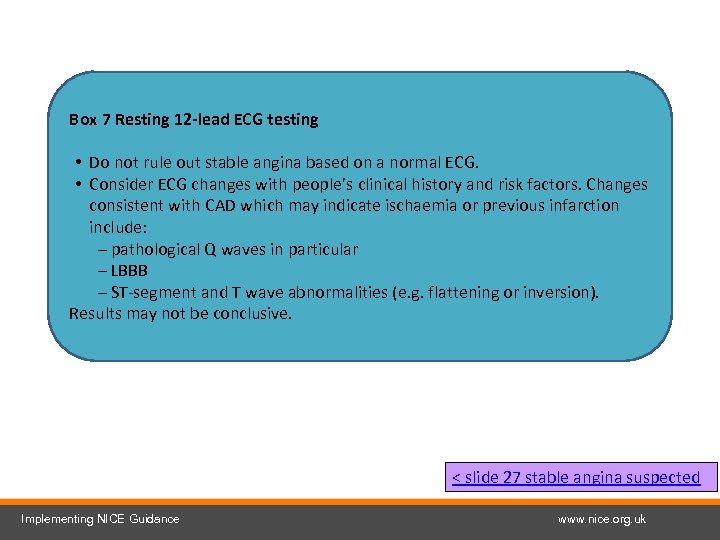 Box 7 Resting 12 -lead ECG testing • Do not rule out stable angina based on a normal ECG. • Consider ECG changes with people’s clinical history and risk factors. Changes consistent with CAD which may indicate ischaemia or previous infarction include: – pathological Q waves in particular – LBBB – ST-segment and T wave abnormalities (e. g. flattening or inversion). Results may not be conclusive. < slide 27 stable angina suspected Implementing NICE Guidance www. nice. org. uk
Box 7 Resting 12 -lead ECG testing • Do not rule out stable angina based on a normal ECG. • Consider ECG changes with people’s clinical history and risk factors. Changes consistent with CAD which may indicate ischaemia or previous infarction include: – pathological Q waves in particular – LBBB – ST-segment and T wave abnormalities (e. g. flattening or inversion). Results may not be conclusive. < slide 27 stable angina suspected Implementing NICE Guidance www. nice. org. uk
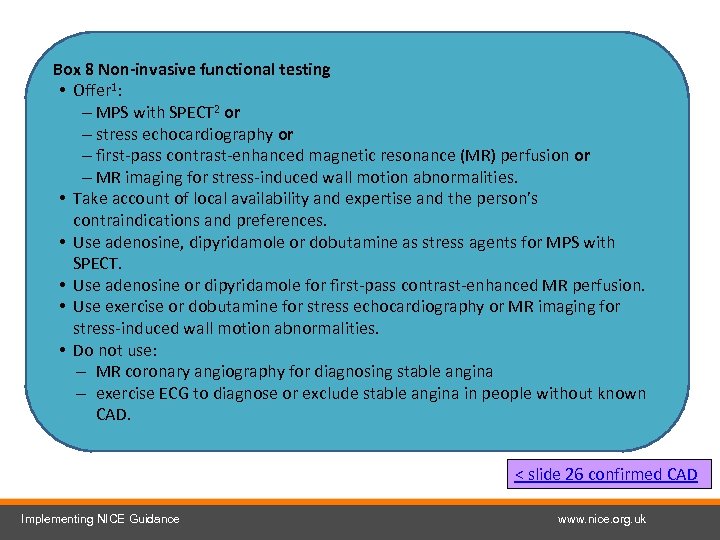 Box 8 Non-invasive functional testing • Offer 1: – MPS with SPECT 2 or – stress echocardiography or – first-pass contrast-enhanced magnetic resonance (MR) perfusion or – MR imaging for stress-induced wall motion abnormalities. • Take account of local availability and expertise and the person’s contraindications and preferences. • Use adenosine, dipyridamole or dobutamine as stress agents for MPS with SPECT. • Use adenosine or dipyridamole for first-pass contrast-enhanced MR perfusion. • Use exercise or dobutamine for stress echocardiography or MR imaging for stress-induced wall motion abnormalities. • Do not use: – MR coronary angiography for diagnosing stable angina – exercise ECG to diagnose or exclude stable angina in people without known CAD. < slide 26 confirmed CAD Implementing NICE Guidance www. nice. org. uk
Box 8 Non-invasive functional testing • Offer 1: – MPS with SPECT 2 or – stress echocardiography or – first-pass contrast-enhanced magnetic resonance (MR) perfusion or – MR imaging for stress-induced wall motion abnormalities. • Take account of local availability and expertise and the person’s contraindications and preferences. • Use adenosine, dipyridamole or dobutamine as stress agents for MPS with SPECT. • Use adenosine or dipyridamole for first-pass contrast-enhanced MR perfusion. • Use exercise or dobutamine for stress echocardiography or MR imaging for stress-induced wall motion abnormalities. • Do not use: – MR coronary angiography for diagnosing stable angina – exercise ECG to diagnose or exclude stable angina in people without known CAD. < slide 26 confirmed CAD Implementing NICE Guidance www. nice. org. uk
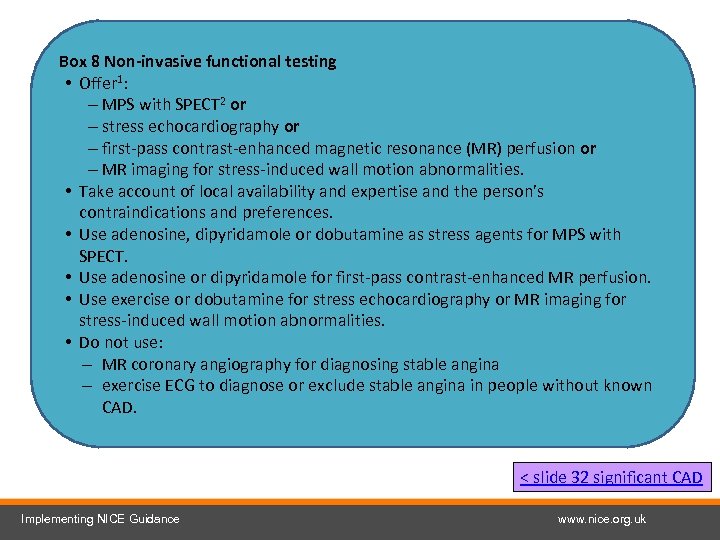 Box 8 Non-invasive functional testing • Offer 1: – MPS with SPECT 2 or – stress echocardiography or – first-pass contrast-enhanced magnetic resonance (MR) perfusion or – MR imaging for stress-induced wall motion abnormalities. • Take account of local availability and expertise and the person’s contraindications and preferences. • Use adenosine, dipyridamole or dobutamine as stress agents for MPS with SPECT. • Use adenosine or dipyridamole for first-pass contrast-enhanced MR perfusion. • Use exercise or dobutamine for stress echocardiography or MR imaging for stress-induced wall motion abnormalities. • Do not use: – MR coronary angiography for diagnosing stable angina – exercise ECG to diagnose or exclude stable angina in people without known CAD. < slide 32 significant CAD Implementing NICE Guidance www. nice. org. uk
Box 8 Non-invasive functional testing • Offer 1: – MPS with SPECT 2 or – stress echocardiography or – first-pass contrast-enhanced magnetic resonance (MR) perfusion or – MR imaging for stress-induced wall motion abnormalities. • Take account of local availability and expertise and the person’s contraindications and preferences. • Use adenosine, dipyridamole or dobutamine as stress agents for MPS with SPECT. • Use adenosine or dipyridamole for first-pass contrast-enhanced MR perfusion. • Use exercise or dobutamine for stress echocardiography or MR imaging for stress-induced wall motion abnormalities. • Do not use: – MR coronary angiography for diagnosing stable angina – exercise ECG to diagnose or exclude stable angina in people without known CAD. < slide 32 significant CAD Implementing NICE Guidance www. nice. org. uk
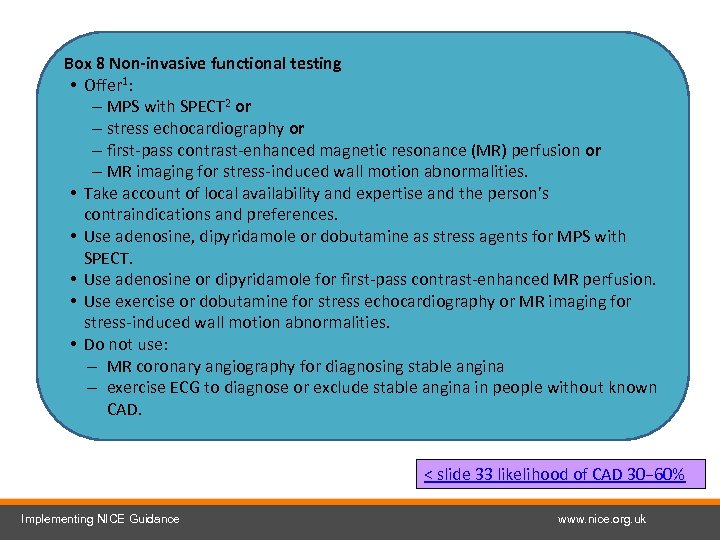 Box 8 Non-invasive functional testing • Offer 1: – MPS with SPECT 2 or – stress echocardiography or – first-pass contrast-enhanced magnetic resonance (MR) perfusion or – MR imaging for stress-induced wall motion abnormalities. • Take account of local availability and expertise and the person’s contraindications and preferences. • Use adenosine, dipyridamole or dobutamine as stress agents for MPS with SPECT. • Use adenosine or dipyridamole for first-pass contrast-enhanced MR perfusion. • Use exercise or dobutamine for stress echocardiography or MR imaging for stress-induced wall motion abnormalities. • Do not use: – MR coronary angiography for diagnosing stable angina – exercise ECG to diagnose or exclude stable angina in people without known CAD. < slide 33 likelihood of CAD 30− 60% Implementing NICE Guidance www. nice. org. uk
Box 8 Non-invasive functional testing • Offer 1: – MPS with SPECT 2 or – stress echocardiography or – first-pass contrast-enhanced magnetic resonance (MR) perfusion or – MR imaging for stress-induced wall motion abnormalities. • Take account of local availability and expertise and the person’s contraindications and preferences. • Use adenosine, dipyridamole or dobutamine as stress agents for MPS with SPECT. • Use adenosine or dipyridamole for first-pass contrast-enhanced MR perfusion. • Use exercise or dobutamine for stress echocardiography or MR imaging for stress-induced wall motion abnormalities. • Do not use: – MR coronary angiography for diagnosing stable angina – exercise ECG to diagnose or exclude stable angina in people without known CAD. < slide 33 likelihood of CAD 30− 60% Implementing NICE Guidance www. nice. org. uk
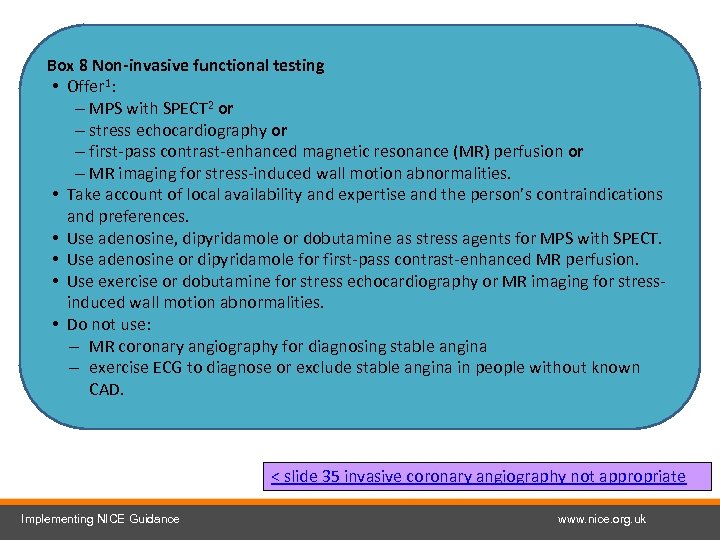 Box 8 Non-invasive functional testing • Offer 1: – MPS with SPECT 2 or – stress echocardiography or – first-pass contrast-enhanced magnetic resonance (MR) perfusion or – MR imaging for stress-induced wall motion abnormalities. • Take account of local availability and expertise and the person’s contraindications and preferences. • Use adenosine, dipyridamole or dobutamine as stress agents for MPS with SPECT. • Use adenosine or dipyridamole for first-pass contrast-enhanced MR perfusion. • Use exercise or dobutamine for stress echocardiography or MR imaging for stressinduced wall motion abnormalities. • Do not use: – MR coronary angiography for diagnosing stable angina – exercise ECG to diagnose or exclude stable angina in people without known CAD. < slide 35 invasive coronary angiography not appropriate Implementing NICE Guidance www. nice. org. uk
Box 8 Non-invasive functional testing • Offer 1: – MPS with SPECT 2 or – stress echocardiography or – first-pass contrast-enhanced magnetic resonance (MR) perfusion or – MR imaging for stress-induced wall motion abnormalities. • Take account of local availability and expertise and the person’s contraindications and preferences. • Use adenosine, dipyridamole or dobutamine as stress agents for MPS with SPECT. • Use adenosine or dipyridamole for first-pass contrast-enhanced MR perfusion. • Use exercise or dobutamine for stress echocardiography or MR imaging for stressinduced wall motion abnormalities. • Do not use: – MR coronary angiography for diagnosing stable angina – exercise ECG to diagnose or exclude stable angina in people without known CAD. < slide 35 invasive coronary angiography not appropriate Implementing NICE Guidance www. nice. org. uk
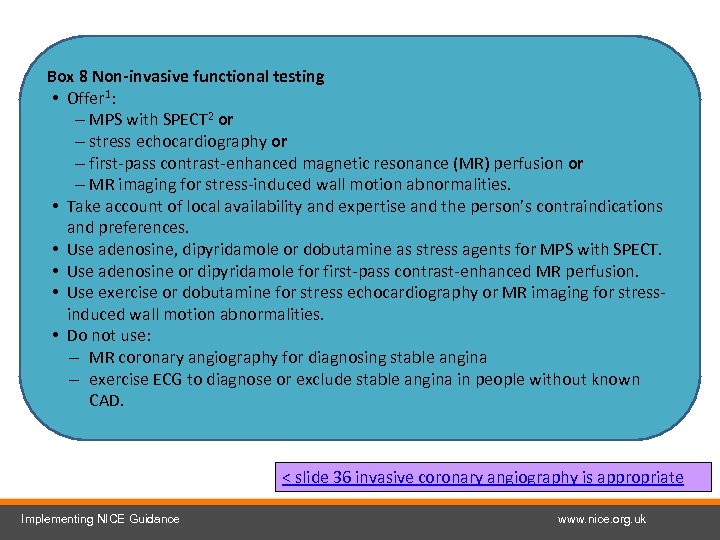 Box 8 Non-invasive functional testing • Offer 1: – MPS with SPECT 2 or – stress echocardiography or – first-pass contrast-enhanced magnetic resonance (MR) perfusion or – MR imaging for stress-induced wall motion abnormalities. • Take account of local availability and expertise and the person’s contraindications and preferences. • Use adenosine, dipyridamole or dobutamine as stress agents for MPS with SPECT. • Use adenosine or dipyridamole for first-pass contrast-enhanced MR perfusion. • Use exercise or dobutamine for stress echocardiography or MR imaging for stressinduced wall motion abnormalities. • Do not use: – MR coronary angiography for diagnosing stable angina – exercise ECG to diagnose or exclude stable angina in people without known CAD. < slide 36 invasive coronary angiography is appropriate Implementing NICE Guidance www. nice. org. uk
Box 8 Non-invasive functional testing • Offer 1: – MPS with SPECT 2 or – stress echocardiography or – first-pass contrast-enhanced magnetic resonance (MR) perfusion or – MR imaging for stress-induced wall motion abnormalities. • Take account of local availability and expertise and the person’s contraindications and preferences. • Use adenosine, dipyridamole or dobutamine as stress agents for MPS with SPECT. • Use adenosine or dipyridamole for first-pass contrast-enhanced MR perfusion. • Use exercise or dobutamine for stress echocardiography or MR imaging for stressinduced wall motion abnormalities. • Do not use: – MR coronary angiography for diagnosing stable angina – exercise ECG to diagnose or exclude stable angina in people without known CAD. < slide 36 invasive coronary angiography is appropriate Implementing NICE Guidance www. nice. org. uk
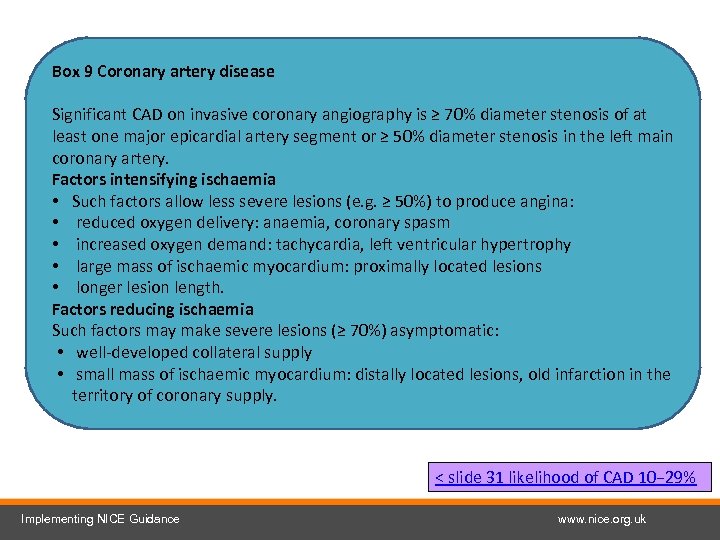 Box 9 Coronary artery disease Significant CAD on invasive coronary angiography is ≥ 70% diameter stenosis of at least one major epicardial artery segment or ≥ 50% diameter stenosis in the left main coronary artery. Factors intensifying ischaemia • Such factors allow less severe lesions (e. g. ≥ 50%) to produce angina: • reduced oxygen delivery: anaemia, coronary spasm • increased oxygen demand: tachycardia, left ventricular hypertrophy • large mass of ischaemic myocardium: proximally located lesions • longer lesion length. Factors reducing ischaemia Such factors may make severe lesions (≥ 70%) asymptomatic: • well-developed collateral supply • small mass of ischaemic myocardium: distally located lesions, old infarction in the territory of coronary supply. < slide 31 likelihood of CAD 10− 29% Implementing NICE Guidance www. nice. org. uk
Box 9 Coronary artery disease Significant CAD on invasive coronary angiography is ≥ 70% diameter stenosis of at least one major epicardial artery segment or ≥ 50% diameter stenosis in the left main coronary artery. Factors intensifying ischaemia • Such factors allow less severe lesions (e. g. ≥ 50%) to produce angina: • reduced oxygen delivery: anaemia, coronary spasm • increased oxygen demand: tachycardia, left ventricular hypertrophy • large mass of ischaemic myocardium: proximally located lesions • longer lesion length. Factors reducing ischaemia Such factors may make severe lesions (≥ 70%) asymptomatic: • well-developed collateral supply • small mass of ischaemic myocardium: distally located lesions, old infarction in the territory of coronary supply. < slide 31 likelihood of CAD 10− 29% Implementing NICE Guidance www. nice. org. uk
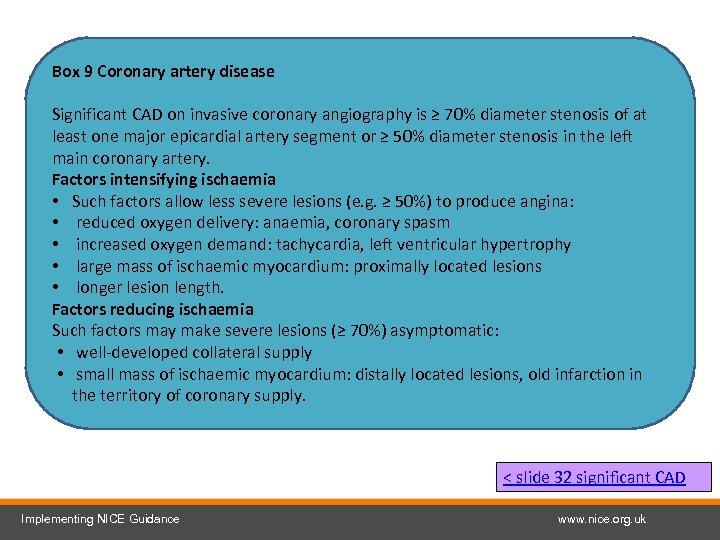 Box 9 Coronary artery disease Significant CAD on invasive coronary angiography is ≥ 70% diameter stenosis of at least one major epicardial artery segment or ≥ 50% diameter stenosis in the left main coronary artery. Factors intensifying ischaemia • Such factors allow less severe lesions (e. g. ≥ 50%) to produce angina: • reduced oxygen delivery: anaemia, coronary spasm • increased oxygen demand: tachycardia, left ventricular hypertrophy • large mass of ischaemic myocardium: proximally located lesions • longer lesion length. Factors reducing ischaemia Such factors may make severe lesions (≥ 70%) asymptomatic: • well-developed collateral supply • small mass of ischaemic myocardium: distally located lesions, old infarction in the territory of coronary supply. < slide 32 significant CAD Implementing NICE Guidance www. nice. org. uk
Box 9 Coronary artery disease Significant CAD on invasive coronary angiography is ≥ 70% diameter stenosis of at least one major epicardial artery segment or ≥ 50% diameter stenosis in the left main coronary artery. Factors intensifying ischaemia • Such factors allow less severe lesions (e. g. ≥ 50%) to produce angina: • reduced oxygen delivery: anaemia, coronary spasm • increased oxygen demand: tachycardia, left ventricular hypertrophy • large mass of ischaemic myocardium: proximally located lesions • longer lesion length. Factors reducing ischaemia Such factors may make severe lesions (≥ 70%) asymptomatic: • well-developed collateral supply • small mass of ischaemic myocardium: distally located lesions, old infarction in the territory of coronary supply. < slide 32 significant CAD Implementing NICE Guidance www. nice. org. uk
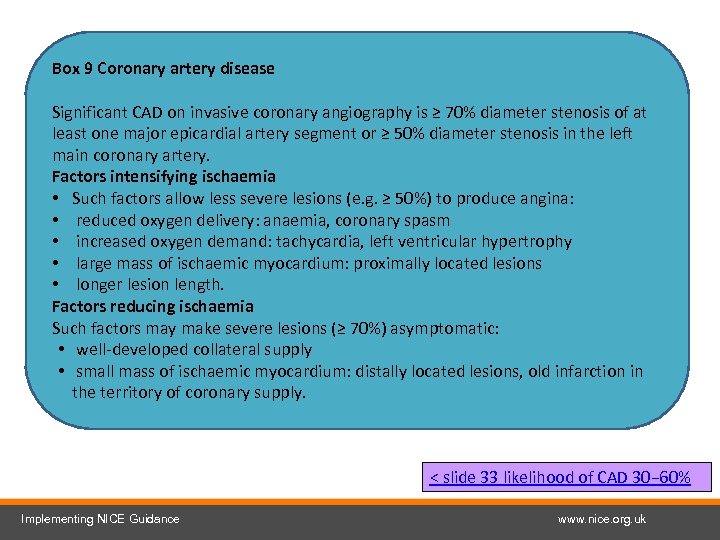 Box 9 Coronary artery disease Significant CAD on invasive coronary angiography is ≥ 70% diameter stenosis of at least one major epicardial artery segment or ≥ 50% diameter stenosis in the left main coronary artery. Factors intensifying ischaemia • Such factors allow less severe lesions (e. g. ≥ 50%) to produce angina: • reduced oxygen delivery: anaemia, coronary spasm • increased oxygen demand: tachycardia, left ventricular hypertrophy • large mass of ischaemic myocardium: proximally located lesions • longer lesion length. Factors reducing ischaemia Such factors may make severe lesions (≥ 70%) asymptomatic: • well-developed collateral supply • small mass of ischaemic myocardium: distally located lesions, old infarction in the territory of coronary supply. < slide 33 likelihood of CAD 30− 60% Implementing NICE Guidance www. nice. org. uk
Box 9 Coronary artery disease Significant CAD on invasive coronary angiography is ≥ 70% diameter stenosis of at least one major epicardial artery segment or ≥ 50% diameter stenosis in the left main coronary artery. Factors intensifying ischaemia • Such factors allow less severe lesions (e. g. ≥ 50%) to produce angina: • reduced oxygen delivery: anaemia, coronary spasm • increased oxygen demand: tachycardia, left ventricular hypertrophy • large mass of ischaemic myocardium: proximally located lesions • longer lesion length. Factors reducing ischaemia Such factors may make severe lesions (≥ 70%) asymptomatic: • well-developed collateral supply • small mass of ischaemic myocardium: distally located lesions, old infarction in the territory of coronary supply. < slide 33 likelihood of CAD 30− 60% Implementing NICE Guidance www. nice. org. uk
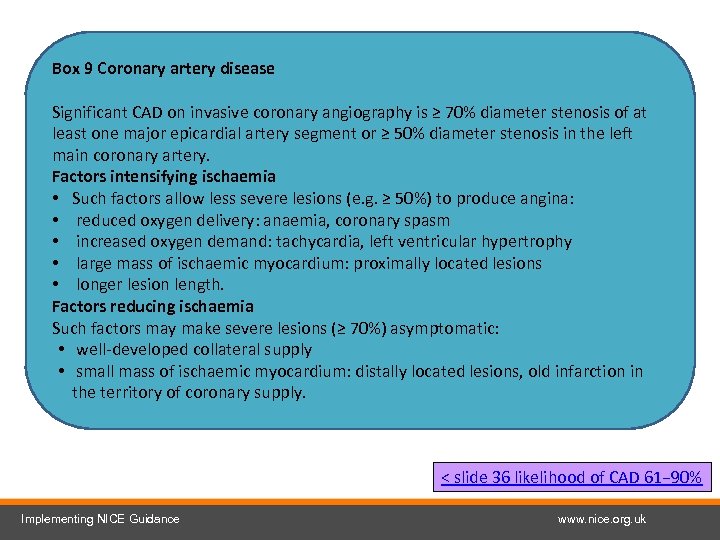 Box 9 Coronary artery disease Significant CAD on invasive coronary angiography is ≥ 70% diameter stenosis of at least one major epicardial artery segment or ≥ 50% diameter stenosis in the left main coronary artery. Factors intensifying ischaemia • Such factors allow less severe lesions (e. g. ≥ 50%) to produce angina: • reduced oxygen delivery: anaemia, coronary spasm • increased oxygen demand: tachycardia, left ventricular hypertrophy • large mass of ischaemic myocardium: proximally located lesions • longer lesion length. Factors reducing ischaemia Such factors may make severe lesions (≥ 70%) asymptomatic: • well-developed collateral supply • small mass of ischaemic myocardium: distally located lesions, old infarction in the territory of coronary supply. < slide 36 likelihood of CAD 61− 90% Implementing NICE Guidance www. nice. org. uk
Box 9 Coronary artery disease Significant CAD on invasive coronary angiography is ≥ 70% diameter stenosis of at least one major epicardial artery segment or ≥ 50% diameter stenosis in the left main coronary artery. Factors intensifying ischaemia • Such factors allow less severe lesions (e. g. ≥ 50%) to produce angina: • reduced oxygen delivery: anaemia, coronary spasm • increased oxygen demand: tachycardia, left ventricular hypertrophy • large mass of ischaemic myocardium: proximally located lesions • longer lesion length. Factors reducing ischaemia Such factors may make severe lesions (≥ 70%) asymptomatic: • well-developed collateral supply • small mass of ischaemic myocardium: distally located lesions, old infarction in the territory of coronary supply. < slide 36 likelihood of CAD 61− 90% Implementing NICE Guidance www. nice. org. uk
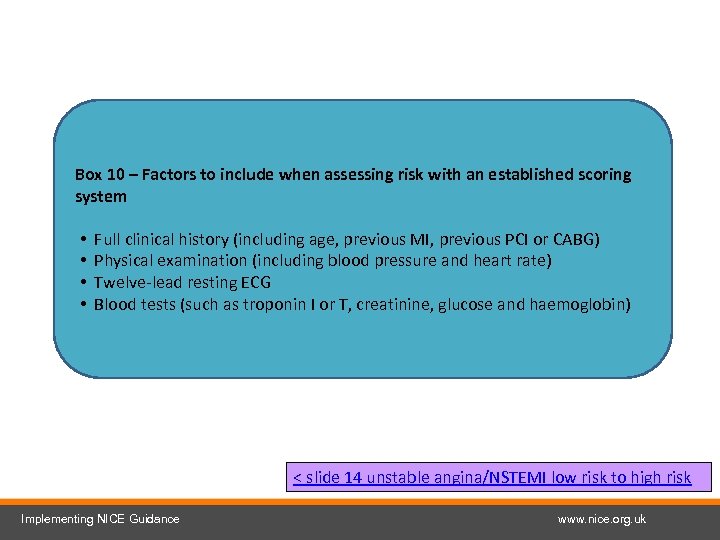 Box 10 – Factors to include when assessing risk with an established scoring system • • Full clinical history (including age, previous MI, previous PCI or CABG) Physical examination (including blood pressure and heart rate) Twelve-lead resting ECG Blood tests (such as troponin I or T, creatinine, glucose and haemoglobin) < slide 14 unstable angina/NSTEMI low risk to high risk Implementing NICE Guidance www. nice. org. uk
Box 10 – Factors to include when assessing risk with an established scoring system • • Full clinical history (including age, previous MI, previous PCI or CABG) Physical examination (including blood pressure and heart rate) Twelve-lead resting ECG Blood tests (such as troponin I or T, creatinine, glucose and haemoglobin) < slide 14 unstable angina/NSTEMI low risk to high risk Implementing NICE Guidance www. nice. org. uk
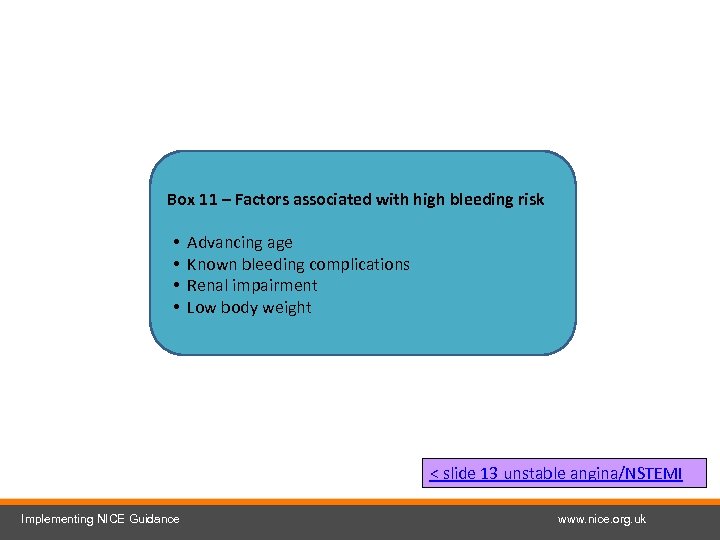 Box 11 – Factors associated with high bleeding risk • • Advancing age Known bleeding complications Renal impairment Low body weight < slide 13 unstable angina/NSTEMI Implementing NICE Guidance www. nice. org. uk
Box 11 – Factors associated with high bleeding risk • • Advancing age Known bleeding complications Renal impairment Low body weight < slide 13 unstable angina/NSTEMI Implementing NICE Guidance www. nice. org. uk
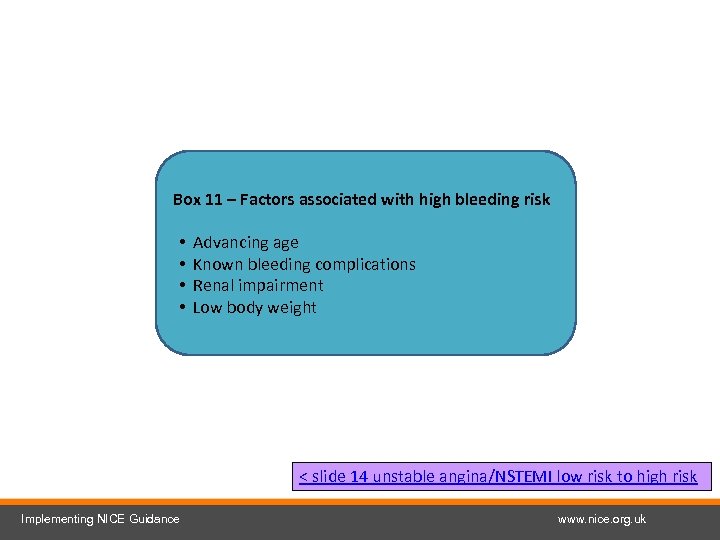 Box 11 – Factors associated with high bleeding risk • • Advancing age Known bleeding complications Renal impairment Low body weight < slide 14 unstable angina/NSTEMI low risk to high risk Implementing NICE Guidance www. nice. org. uk
Box 11 – Factors associated with high bleeding risk • • Advancing age Known bleeding complications Renal impairment Low body weight < slide 14 unstable angina/NSTEMI low risk to high risk Implementing NICE Guidance www. nice. org. uk
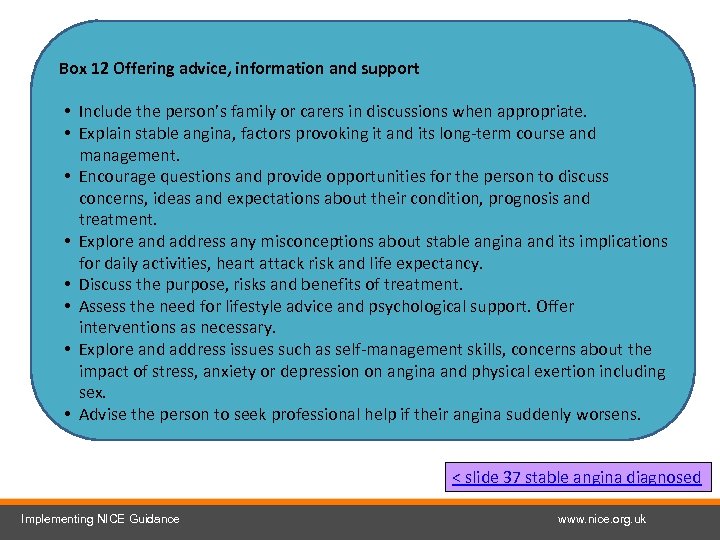 Box 12 Offering advice, information and support • Include the person’s family or carers in discussions when appropriate. • Explain stable angina, factors provoking it and its long-term course and management. • Encourage questions and provide opportunities for the person to discuss concerns, ideas and expectations about their condition, prognosis and treatment. • Explore and address any misconceptions about stable angina and its implications for daily activities, heart attack risk and life expectancy. • Discuss the purpose, risks and benefits of treatment. • Assess the need for lifestyle advice and psychological support. Offer interventions as necessary. • Explore and address issues such as self-management skills, concerns about the impact of stress, anxiety or depression on angina and physical exertion including sex. • Advise the person to seek professional help if their angina suddenly worsens. < slide 37 stable angina diagnosed Implementing NICE Guidance www. nice. org. uk
Box 12 Offering advice, information and support • Include the person’s family or carers in discussions when appropriate. • Explain stable angina, factors provoking it and its long-term course and management. • Encourage questions and provide opportunities for the person to discuss concerns, ideas and expectations about their condition, prognosis and treatment. • Explore and address any misconceptions about stable angina and its implications for daily activities, heart attack risk and life expectancy. • Discuss the purpose, risks and benefits of treatment. • Assess the need for lifestyle advice and psychological support. Offer interventions as necessary. • Explore and address issues such as self-management skills, concerns about the impact of stress, anxiety or depression on angina and physical exertion including sex. • Advise the person to seek professional help if their angina suddenly worsens. < slide 37 stable angina diagnosed Implementing NICE Guidance www. nice. org. uk
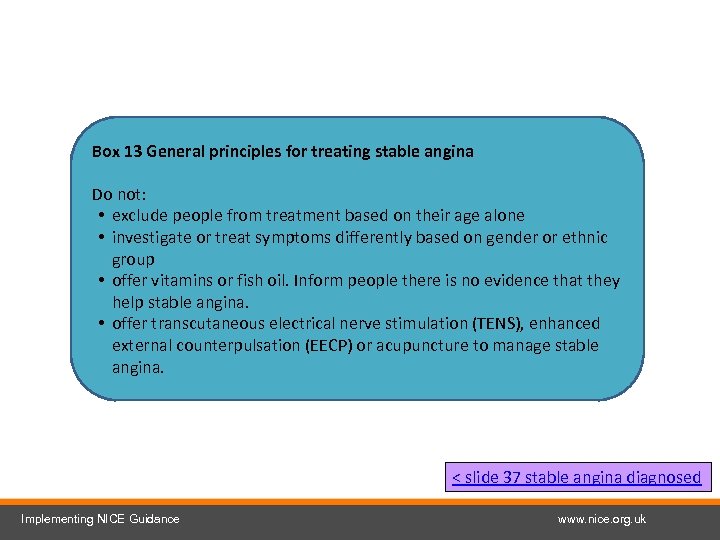 Box 13 General principles for treating stable angina Do not: • exclude people from treatment based on their age alone • investigate or treat symptoms differently based on gender or ethnic group • offer vitamins or fish oil. Inform people there is no evidence that they help stable angina. • offer transcutaneous electrical nerve stimulation (TENS), enhanced external counterpulsation (EECP) or acupuncture to manage stable angina. < slide 37 stable angina diagnosed Implementing NICE Guidance www. nice. org. uk
Box 13 General principles for treating stable angina Do not: • exclude people from treatment based on their age alone • investigate or treat symptoms differently based on gender or ethnic group • offer vitamins or fish oil. Inform people there is no evidence that they help stable angina. • offer transcutaneous electrical nerve stimulation (TENS), enhanced external counterpulsation (EECP) or acupuncture to manage stable angina. < slide 37 stable angina diagnosed Implementing NICE Guidance www. nice. org. uk
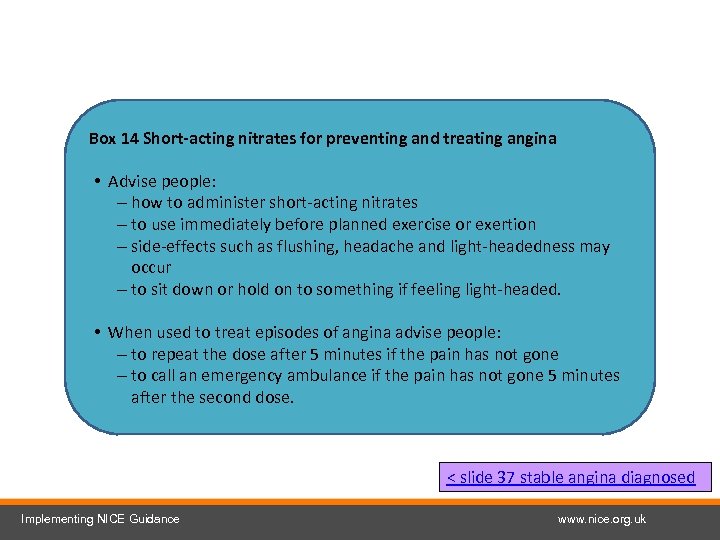 Box 14 Short-acting nitrates for preventing and treating angina • Advise people: – how to administer short-acting nitrates – to use immediately before planned exercise or exertion – side-effects such as flushing, headache and light-headedness may occur – to sit down or hold on to something if feeling light-headed. • When used to treat episodes of angina advise people: – to repeat the dose after 5 minutes if the pain has not gone – to call an emergency ambulance if the pain has not gone 5 minutes after the second dose. < slide 37 stable angina diagnosed Implementing NICE Guidance www. nice. org. uk
Box 14 Short-acting nitrates for preventing and treating angina • Advise people: – how to administer short-acting nitrates – to use immediately before planned exercise or exertion – side-effects such as flushing, headache and light-headedness may occur – to sit down or hold on to something if feeling light-headed. • When used to treat episodes of angina advise people: – to repeat the dose after 5 minutes if the pain has not gone – to call an emergency ambulance if the pain has not gone 5 minutes after the second dose. < slide 37 stable angina diagnosed Implementing NICE Guidance www. nice. org. uk
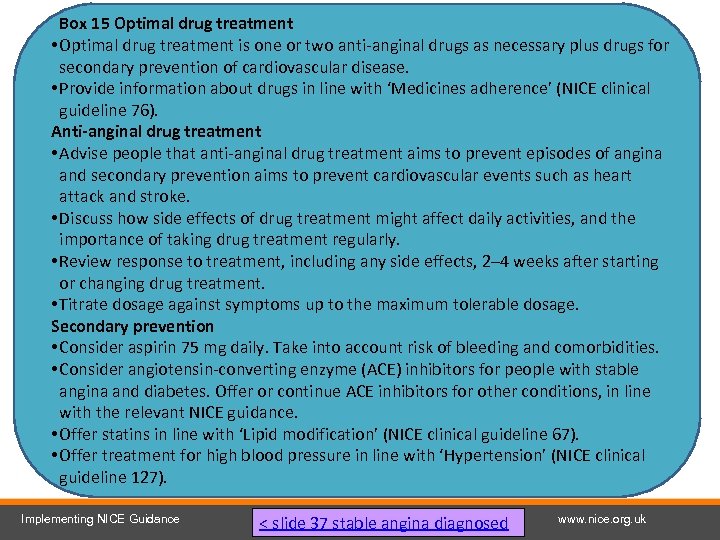 Box 15 Optimal drug treatment • Optimal drug treatment is one or two anti-anginal drugs as necessary plus drugs for secondary prevention of cardiovascular disease. • Provide information about drugs in line with ‘Medicines adherence’ (NICE clinical guideline 76). Anti-anginal drug treatment • Advise people that anti-anginal drug treatment aims to prevent episodes of angina and secondary prevention aims to prevent cardiovascular events such as heart attack and stroke. • Discuss how side effects of drug treatment might affect daily activities, and the importance of taking drug treatment regularly. • Review response to treatment, including any side effects, 2– 4 weeks after starting or changing drug treatment. • Titrate dosage against symptoms up to the maximum tolerable dosage. Secondary prevention • Consider aspirin 75 mg daily. Take into account risk of bleeding and comorbidities. • Consider angiotensin-converting enzyme (ACE) inhibitors for people with stable angina and diabetes. Offer or continue ACE inhibitors for other conditions, in line with the relevant NICE guidance. • Offer statins in line with ‘Lipid modification’ (NICE clinical guideline 67). • Offer treatment for high blood pressure in line with ‘Hypertension’ (NICE clinical guideline 127). Implementing NICE Guidance < slide 37 stable angina diagnosed www. nice. org. uk
Box 15 Optimal drug treatment • Optimal drug treatment is one or two anti-anginal drugs as necessary plus drugs for secondary prevention of cardiovascular disease. • Provide information about drugs in line with ‘Medicines adherence’ (NICE clinical guideline 76). Anti-anginal drug treatment • Advise people that anti-anginal drug treatment aims to prevent episodes of angina and secondary prevention aims to prevent cardiovascular events such as heart attack and stroke. • Discuss how side effects of drug treatment might affect daily activities, and the importance of taking drug treatment regularly. • Review response to treatment, including any side effects, 2– 4 weeks after starting or changing drug treatment. • Titrate dosage against symptoms up to the maximum tolerable dosage. Secondary prevention • Consider aspirin 75 mg daily. Take into account risk of bleeding and comorbidities. • Consider angiotensin-converting enzyme (ACE) inhibitors for people with stable angina and diabetes. Offer or continue ACE inhibitors for other conditions, in line with the relevant NICE guidance. • Offer statins in line with ‘Lipid modification’ (NICE clinical guideline 67). • Offer treatment for high blood pressure in line with ‘Hypertension’ (NICE clinical guideline 127). Implementing NICE Guidance < slide 37 stable angina diagnosed www. nice. org. uk
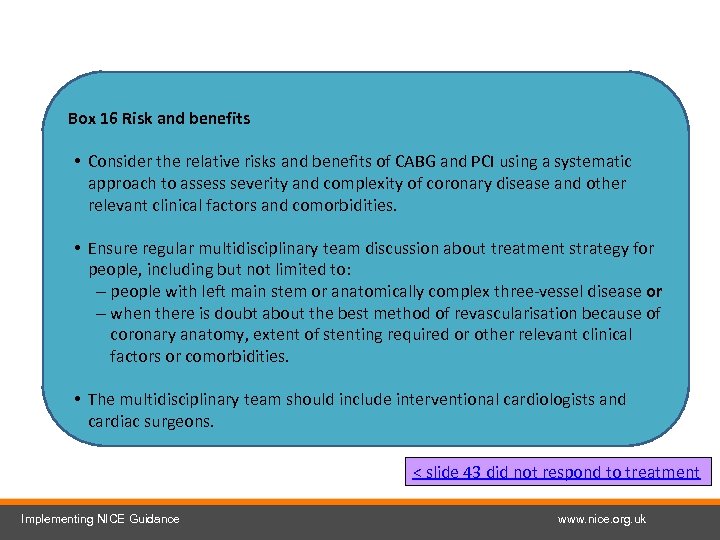 Box 16 Risk and benefits • Consider the relative risks and benefits of CABG and PCI using a systematic approach to assess severity and complexity of coronary disease and other relevant clinical factors and comorbidities. • Ensure regular multidisciplinary team discussion about treatment strategy for people, including but not limited to: – people with left main stem or anatomically complex three-vessel disease or – when there is doubt about the best method of revascularisation because of coronary anatomy, extent of stenting required or other relevant clinical factors or comorbidities. • The multidisciplinary team should include interventional cardiologists and cardiac surgeons. < slide 43 did not respond to treatment Implementing NICE Guidance www. nice. org. uk
Box 16 Risk and benefits • Consider the relative risks and benefits of CABG and PCI using a systematic approach to assess severity and complexity of coronary disease and other relevant clinical factors and comorbidities. • Ensure regular multidisciplinary team discussion about treatment strategy for people, including but not limited to: – people with left main stem or anatomically complex three-vessel disease or – when there is doubt about the best method of revascularisation because of coronary anatomy, extent of stenting required or other relevant clinical factors or comorbidities. • The multidisciplinary team should include interventional cardiologists and cardiac surgeons. < slide 43 did not respond to treatment Implementing NICE Guidance www. nice. org. uk
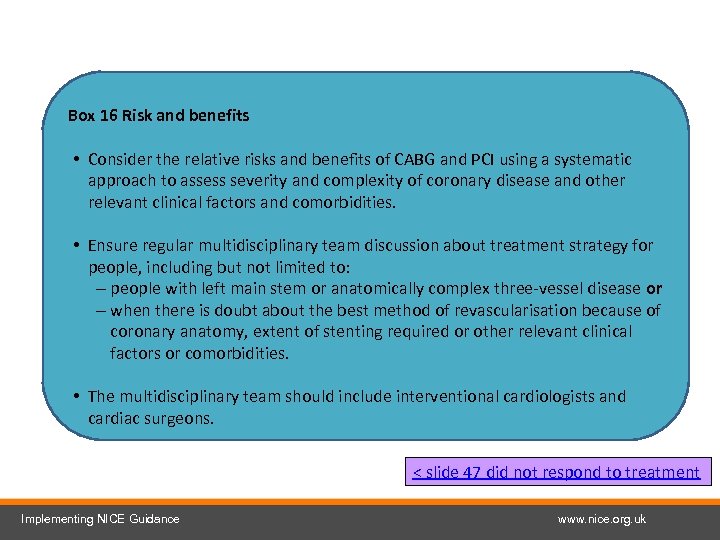 Box 16 Risk and benefits • Consider the relative risks and benefits of CABG and PCI using a systematic approach to assess severity and complexity of coronary disease and other relevant clinical factors and comorbidities. • Ensure regular multidisciplinary team discussion about treatment strategy for people, including but not limited to: – people with left main stem or anatomically complex three-vessel disease or – when there is doubt about the best method of revascularisation because of coronary anatomy, extent of stenting required or other relevant clinical factors or comorbidities. • The multidisciplinary team should include interventional cardiologists and cardiac surgeons. < slide 47 did not respond to treatment Implementing NICE Guidance www. nice. org. uk
Box 16 Risk and benefits • Consider the relative risks and benefits of CABG and PCI using a systematic approach to assess severity and complexity of coronary disease and other relevant clinical factors and comorbidities. • Ensure regular multidisciplinary team discussion about treatment strategy for people, including but not limited to: – people with left main stem or anatomically complex three-vessel disease or – when there is doubt about the best method of revascularisation because of coronary anatomy, extent of stenting required or other relevant clinical factors or comorbidities. • The multidisciplinary team should include interventional cardiologists and cardiac surgeons. < slide 47 did not respond to treatment Implementing NICE Guidance www. nice. org. uk
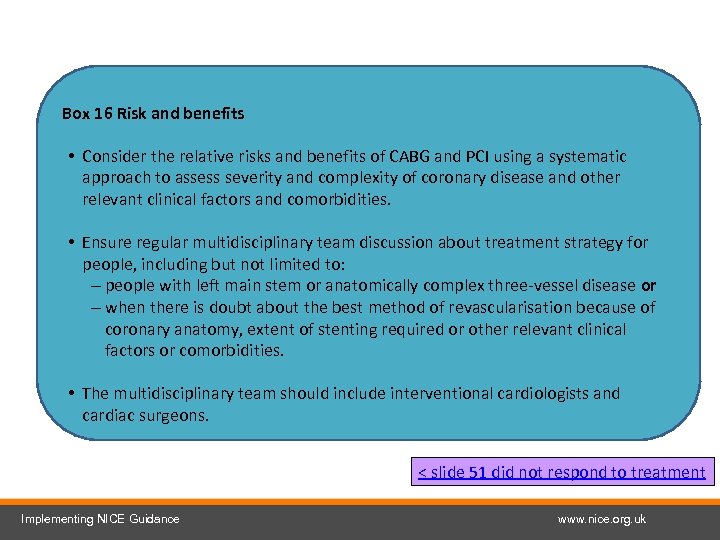 Box 16 Risk and benefits • Consider the relative risks and benefits of CABG and PCI using a systematic approach to assess severity and complexity of coronary disease and other relevant clinical factors and comorbidities. • Ensure regular multidisciplinary team discussion about treatment strategy for people, including but not limited to: – people with left main stem or anatomically complex three-vessel disease or – when there is doubt about the best method of revascularisation because of coronary anatomy, extent of stenting required or other relevant clinical factors or comorbidities. • The multidisciplinary team should include interventional cardiologists and cardiac surgeons. < slide 51 did not respond to treatment Implementing NICE Guidance www. nice. org. uk
Box 16 Risk and benefits • Consider the relative risks and benefits of CABG and PCI using a systematic approach to assess severity and complexity of coronary disease and other relevant clinical factors and comorbidities. • Ensure regular multidisciplinary team discussion about treatment strategy for people, including but not limited to: – people with left main stem or anatomically complex three-vessel disease or – when there is doubt about the best method of revascularisation because of coronary anatomy, extent of stenting required or other relevant clinical factors or comorbidities. • The multidisciplinary team should include interventional cardiologists and cardiac surgeons. < slide 51 did not respond to treatment Implementing NICE Guidance www. nice. org. uk
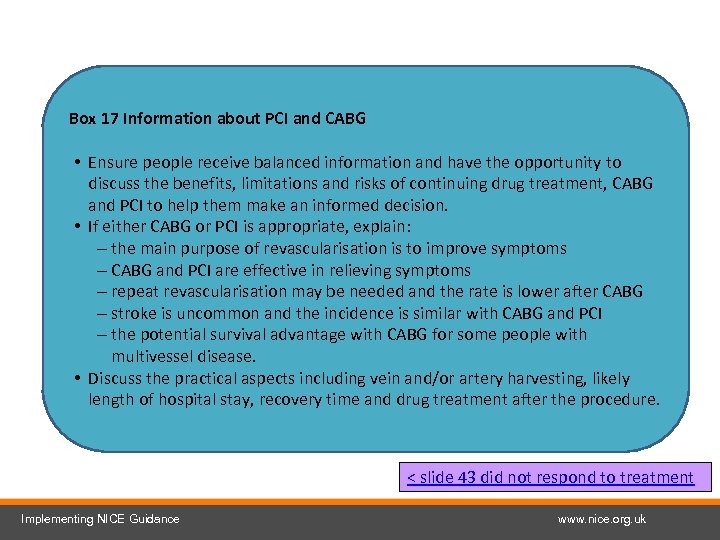 Box 17 Information about PCI and CABG • Ensure people receive balanced information and have the opportunity to discuss the benefits, limitations and risks of continuing drug treatment, CABG and PCI to help them make an informed decision. • If either CABG or PCI is appropriate, explain: – the main purpose of revascularisation is to improve symptoms – CABG and PCI are effective in relieving symptoms – repeat revascularisation may be needed and the rate is lower after CABG – stroke is uncommon and the incidence is similar with CABG and PCI – the potential survival advantage with CABG for some people with multivessel disease. • Discuss the practical aspects including vein and/or artery harvesting, likely length of hospital stay, recovery time and drug treatment after the procedure. < slide 43 did not respond to treatment Implementing NICE Guidance www. nice. org. uk
Box 17 Information about PCI and CABG • Ensure people receive balanced information and have the opportunity to discuss the benefits, limitations and risks of continuing drug treatment, CABG and PCI to help them make an informed decision. • If either CABG or PCI is appropriate, explain: – the main purpose of revascularisation is to improve symptoms – CABG and PCI are effective in relieving symptoms – repeat revascularisation may be needed and the rate is lower after CABG – stroke is uncommon and the incidence is similar with CABG and PCI – the potential survival advantage with CABG for some people with multivessel disease. • Discuss the practical aspects including vein and/or artery harvesting, likely length of hospital stay, recovery time and drug treatment after the procedure. < slide 43 did not respond to treatment Implementing NICE Guidance www. nice. org. uk
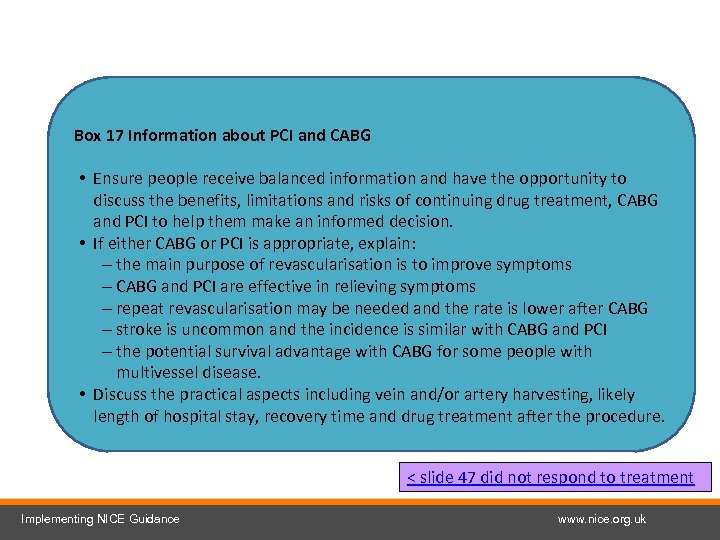 Box 17 Information about PCI and CABG • Ensure people receive balanced information and have the opportunity to discuss the benefits, limitations and risks of continuing drug treatment, CABG and PCI to help them make an informed decision. • If either CABG or PCI is appropriate, explain: – the main purpose of revascularisation is to improve symptoms – CABG and PCI are effective in relieving symptoms – repeat revascularisation may be needed and the rate is lower after CABG – stroke is uncommon and the incidence is similar with CABG and PCI – the potential survival advantage with CABG for some people with multivessel disease. • Discuss the practical aspects including vein and/or artery harvesting, likely length of hospital stay, recovery time and drug treatment after the procedure. < slide 47 did not respond to treatment Implementing NICE Guidance www. nice. org. uk
Box 17 Information about PCI and CABG • Ensure people receive balanced information and have the opportunity to discuss the benefits, limitations and risks of continuing drug treatment, CABG and PCI to help them make an informed decision. • If either CABG or PCI is appropriate, explain: – the main purpose of revascularisation is to improve symptoms – CABG and PCI are effective in relieving symptoms – repeat revascularisation may be needed and the rate is lower after CABG – stroke is uncommon and the incidence is similar with CABG and PCI – the potential survival advantage with CABG for some people with multivessel disease. • Discuss the practical aspects including vein and/or artery harvesting, likely length of hospital stay, recovery time and drug treatment after the procedure. < slide 47 did not respond to treatment Implementing NICE Guidance www. nice. org. uk
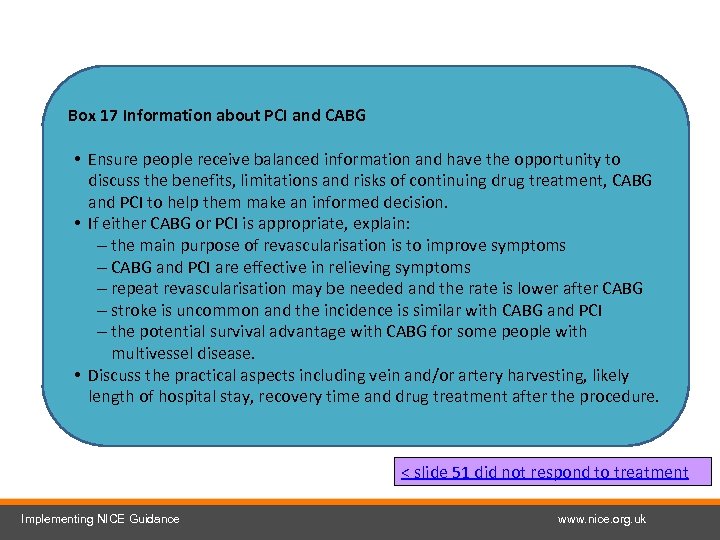 Box 17 Information about PCI and CABG • Ensure people receive balanced information and have the opportunity to discuss the benefits, limitations and risks of continuing drug treatment, CABG and PCI to help them make an informed decision. • If either CABG or PCI is appropriate, explain: – the main purpose of revascularisation is to improve symptoms – CABG and PCI are effective in relieving symptoms – repeat revascularisation may be needed and the rate is lower after CABG – stroke is uncommon and the incidence is similar with CABG and PCI – the potential survival advantage with CABG for some people with multivessel disease. • Discuss the practical aspects including vein and/or artery harvesting, likely length of hospital stay, recovery time and drug treatment after the procedure. < slide 51 did not respond to treatment Implementing NICE Guidance www. nice. org. uk
Box 17 Information about PCI and CABG • Ensure people receive balanced information and have the opportunity to discuss the benefits, limitations and risks of continuing drug treatment, CABG and PCI to help them make an informed decision. • If either CABG or PCI is appropriate, explain: – the main purpose of revascularisation is to improve symptoms – CABG and PCI are effective in relieving symptoms – repeat revascularisation may be needed and the rate is lower after CABG – stroke is uncommon and the incidence is similar with CABG and PCI – the potential survival advantage with CABG for some people with multivessel disease. • Discuss the practical aspects including vein and/or artery harvesting, likely length of hospital stay, recovery time and drug treatment after the procedure. < slide 51 did not respond to treatment Implementing NICE Guidance www. nice. org. uk
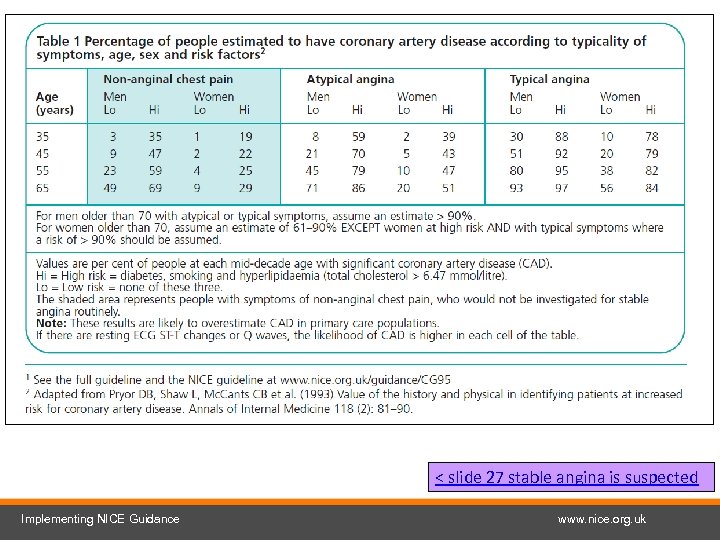 < slide 27 stable angina is suspected Implementing NICE Guidance www. nice. org. uk
< slide 27 stable angina is suspected Implementing NICE Guidance www. nice. org. uk
 Find out more and tell us what you think Next slide Implementing NICE Guidance www. nice. org. uk
Find out more and tell us what you think Next slide Implementing NICE Guidance www. nice. org. uk
 Find out more – Unstable angina and NSTEMI guideline Visit www. nice. org. uk/guidance/CG 94 for: • • the guideline the quick reference guide ‘Understanding NICE guidance’ slide set costing statement audit support, including patient questionnaire online educational tool Next slide Implementing NICE Guidance www. nice. org. uk
Find out more – Unstable angina and NSTEMI guideline Visit www. nice. org. uk/guidance/CG 94 for: • • the guideline the quick reference guide ‘Understanding NICE guidance’ slide set costing statement audit support, including patient questionnaire online educational tool Next slide Implementing NICE Guidance www. nice. org. uk
 Find out more – Chest pain of recent onset guideline Visit www. nice. org. uk/CG 0 XX for: • the guideline • the quick reference guide • ‘Understanding NICE guidance’ • slide set • costing report and template • audit support • implementation advice • online educational tool • referral checklist • calcium scoring factsheet Implementing NICE Guidance Next slide www. nice. org. uk
Find out more – Chest pain of recent onset guideline Visit www. nice. org. uk/CG 0 XX for: • the guideline • the quick reference guide • ‘Understanding NICE guidance’ • slide set • costing report and template • audit support • implementation advice • online educational tool • referral checklist • calcium scoring factsheet Implementing NICE Guidance Next slide www. nice. org. uk
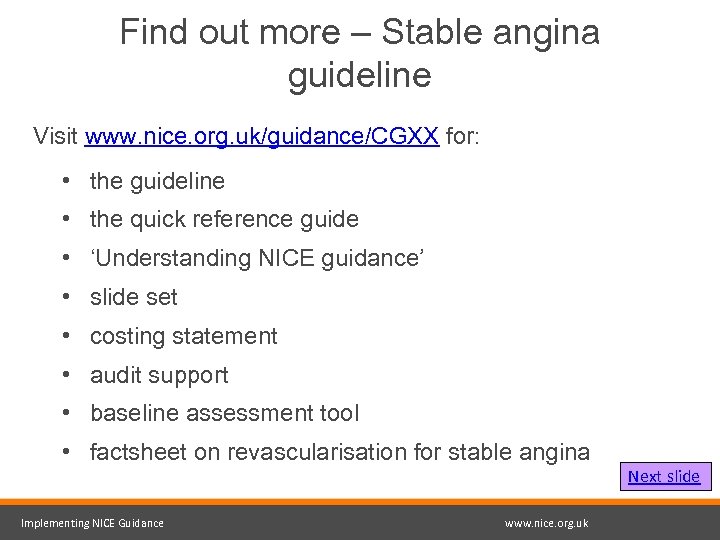 Find out more – Stable angina guideline Visit www. nice. org. uk/guidance/CGXX for: • the guideline • the quick reference guide • ‘Understanding NICE guidance’ • slide set • costing statement • audit support • baseline assessment tool • factsheet on revascularisation for stable angina Implementing NICE Guidance www. nice. org. uk Next slide
Find out more – Stable angina guideline Visit www. nice. org. uk/guidance/CGXX for: • the guideline • the quick reference guide • ‘Understanding NICE guidance’ • slide set • costing statement • audit support • baseline assessment tool • factsheet on revascularisation for stable angina Implementing NICE Guidance www. nice. org. uk Next slide
 Find out more – related guidance Visit www. nice. org. uk for guidance on: • • • Stable angina quality standard New generation cardiac CT scanners Hypertension Management of hyperglycaemia in patients with ACS Chronic heart failure Ticagrelor Prasugrel Lipid modification MI: secondary prevention Implementing NICE Guidance Next slide www. nice. org. uk
Find out more – related guidance Visit www. nice. org. uk for guidance on: • • • Stable angina quality standard New generation cardiac CT scanners Hypertension Management of hyperglycaemia in patients with ACS Chronic heart failure Ticagrelor Prasugrel Lipid modification MI: secondary prevention Implementing NICE Guidance Next slide www. nice. org. uk
 What do you think? Did the implementation tool you accessed today meet your requirements, and will it help you to put the NICE guidance into practice? We value your opinion and are looking for ways to improve our tools. Please complete this short evaluation form. If you are experiencing problems accessing or using this tool, please email implementation@nice. org. uk To open the links in this slide set right click over the link and choose ‘open link’ Shortcut to contents page Implementing NICE Guidance www. nice. org. uk
What do you think? Did the implementation tool you accessed today meet your requirements, and will it help you to put the NICE guidance into practice? We value your opinion and are looking for ways to improve our tools. Please complete this short evaluation form. If you are experiencing problems accessing or using this tool, please email implementation@nice. org. uk To open the links in this slide set right click over the link and choose ‘open link’ Shortcut to contents page Implementing NICE Guidance www. nice. org. uk
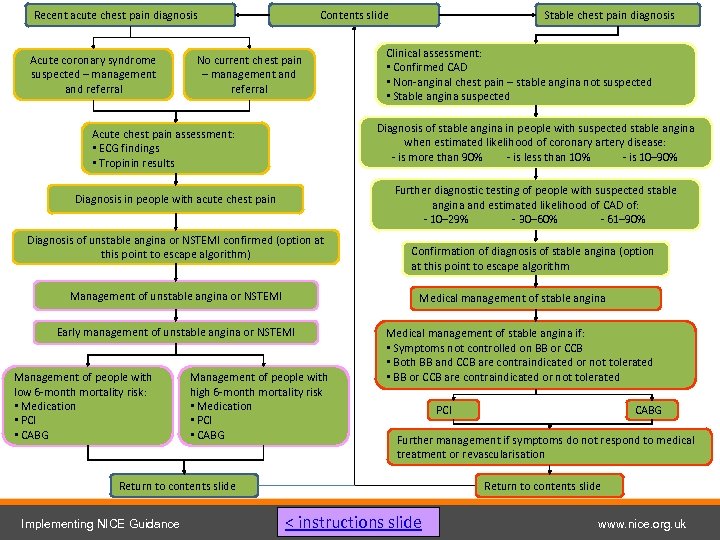 Recent acute chest pain diagnosis Acute coronary syndrome suspected – management and referral Contents slide No current chest pain – management and referral Clinical assessment: • Confirmed CAD • Non-anginal chest pain – stable angina not suspected • Stable angina suspected Diagnosis of stable angina in people with suspected stable angina when estimated likelihood of coronary artery disease: - is more than 90% - is less than 10% - is 10− 90% Acute chest pain assessment: • ECG findings • Tropinin results Further diagnostic testing of people with suspected stable angina and estimated likelihood of CAD of: - 10– 29% - 30– 60% - 61– 90% Diagnosis in people with acute chest pain Diagnosis of unstable angina or NSTEMI confirmed (option at this point to escape algorithm) Management of unstable angina or NSTEMI Confirmation of diagnosis of stable angina (option at this point to escape algorithm Medical management of stable angina Early management of unstable angina or NSTEMI Management of people with low 6 -month mortality risk: • Medication • PCI • CABG Stable chest pain diagnosis Management of people with high 6 -month mortality risk • Medication • PCI • CABG Medical management of stable angina if: • Symptoms not controlled on BB or CCB • Both BB and CCB are contraindicated or not tolerated • BB or CCB are contraindicated or not tolerated PCI Further management if symptoms do not respond to medical treatment or revascularisation Return to contents slide Implementing NICE Guidance CABG Return to contents slide < instructions slide www. nice. org. uk
Recent acute chest pain diagnosis Acute coronary syndrome suspected – management and referral Contents slide No current chest pain – management and referral Clinical assessment: • Confirmed CAD • Non-anginal chest pain – stable angina not suspected • Stable angina suspected Diagnosis of stable angina in people with suspected stable angina when estimated likelihood of coronary artery disease: - is more than 90% - is less than 10% - is 10− 90% Acute chest pain assessment: • ECG findings • Tropinin results Further diagnostic testing of people with suspected stable angina and estimated likelihood of CAD of: - 10– 29% - 30– 60% - 61– 90% Diagnosis in people with acute chest pain Diagnosis of unstable angina or NSTEMI confirmed (option at this point to escape algorithm) Management of unstable angina or NSTEMI Confirmation of diagnosis of stable angina (option at this point to escape algorithm Medical management of stable angina Early management of unstable angina or NSTEMI Management of people with low 6 -month mortality risk: • Medication • PCI • CABG Stable chest pain diagnosis Management of people with high 6 -month mortality risk • Medication • PCI • CABG Medical management of stable angina if: • Symptoms not controlled on BB or CCB • Both BB and CCB are contraindicated or not tolerated • BB or CCB are contraindicated or not tolerated PCI Further management if symptoms do not respond to medical treatment or revascularisation Return to contents slide Implementing NICE Guidance CABG Return to contents slide < instructions slide www. nice. org. uk
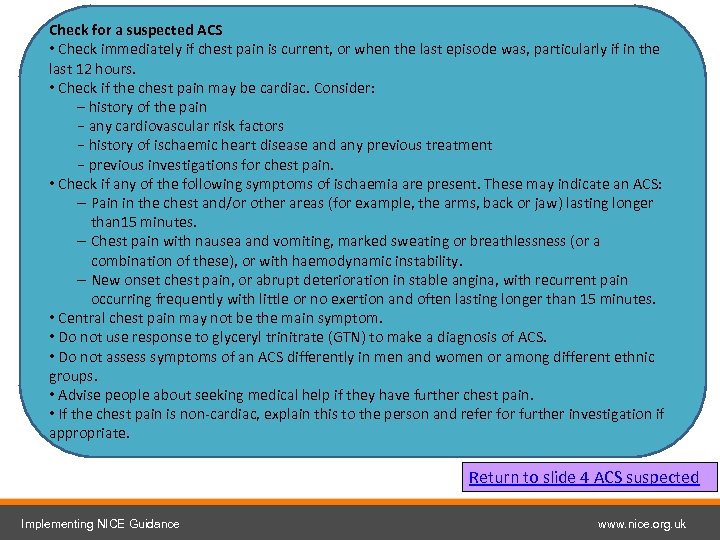 Check for a suspected ACS • Check immediately if chest pain is current, or when the last episode was, particularly if in the last 12 hours. • Check if the chest pain may be cardiac. Consider: – history of the pain − any cardiovascular risk factors − history of ischaemic heart disease and any previous treatment − previous investigations for chest pain. • Check if any of the following symptoms of ischaemia are present. These may indicate an ACS: – Pain in the chest and/or other areas (for example, the arms, back or jaw) lasting longer than 15 minutes. – Chest pain with nausea and vomiting, marked sweating or breathlessness (or a combination of these), or with haemodynamic instability. – New onset chest pain, or abrupt deterioration in stable angina, with recurrent pain occurring frequently with little or no exertion and often lasting longer than 15 minutes. • Central chest pain may not be the main symptom. • Do not use response to glyceryl trinitrate (GTN) to make a diagnosis of ACS. • Do not assess symptoms of an ACS differently in men and women or among different ethnic groups. • Advise people about seeking medical help if they have further chest pain. • If the chest pain is non-cardiac, explain this to the person and refer for further investigation if appropriate. Return to slide 4 ACS suspected Implementing NICE Guidance www. nice. org. uk
Check for a suspected ACS • Check immediately if chest pain is current, or when the last episode was, particularly if in the last 12 hours. • Check if the chest pain may be cardiac. Consider: – history of the pain − any cardiovascular risk factors − history of ischaemic heart disease and any previous treatment − previous investigations for chest pain. • Check if any of the following symptoms of ischaemia are present. These may indicate an ACS: – Pain in the chest and/or other areas (for example, the arms, back or jaw) lasting longer than 15 minutes. – Chest pain with nausea and vomiting, marked sweating or breathlessness (or a combination of these), or with haemodynamic instability. – New onset chest pain, or abrupt deterioration in stable angina, with recurrent pain occurring frequently with little or no exertion and often lasting longer than 15 minutes. • Central chest pain may not be the main symptom. • Do not use response to glyceryl trinitrate (GTN) to make a diagnosis of ACS. • Do not assess symptoms of an ACS differently in men and women or among different ethnic groups. • Advise people about seeking medical help if they have further chest pain. • If the chest pain is non-cardiac, explain this to the person and refer for further investigation if appropriate. Return to slide 4 ACS suspected Implementing NICE Guidance www. nice. org. uk
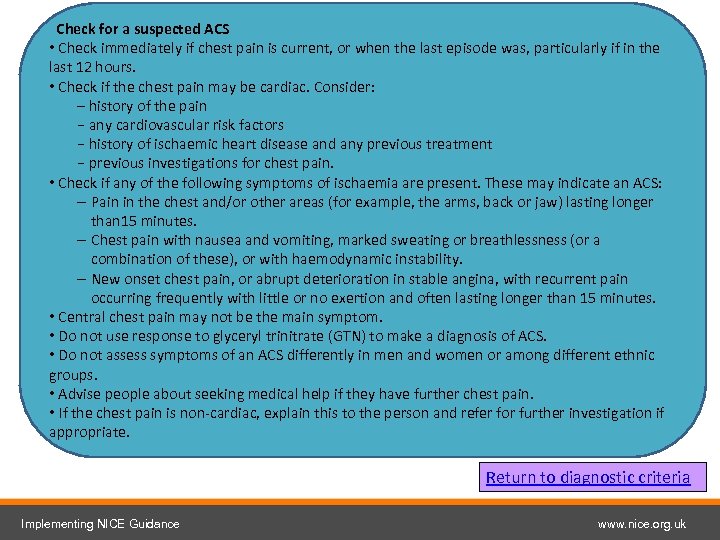 Check for a suspected ACS • Check immediately if chest pain is current, or when the last episode was, particularly if in the last 12 hours. • Check if the chest pain may be cardiac. Consider: – history of the pain − any cardiovascular risk factors − history of ischaemic heart disease and any previous treatment − previous investigations for chest pain. • Check if any of the following symptoms of ischaemia are present. These may indicate an ACS: – Pain in the chest and/or other areas (for example, the arms, back or jaw) lasting longer than 15 minutes. – Chest pain with nausea and vomiting, marked sweating or breathlessness (or a combination of these), or with haemodynamic instability. – New onset chest pain, or abrupt deterioration in stable angina, with recurrent pain occurring frequently with little or no exertion and often lasting longer than 15 minutes. • Central chest pain may not be the main symptom. • Do not use response to glyceryl trinitrate (GTN) to make a diagnosis of ACS. • Do not assess symptoms of an ACS differently in men and women or among different ethnic groups. • Advise people about seeking medical help if they have further chest pain. • If the chest pain is non-cardiac, explain this to the person and refer for further investigation if appropriate. Return to diagnostic criteria Implementing NICE Guidance www. nice. org. uk
Check for a suspected ACS • Check immediately if chest pain is current, or when the last episode was, particularly if in the last 12 hours. • Check if the chest pain may be cardiac. Consider: – history of the pain − any cardiovascular risk factors − history of ischaemic heart disease and any previous treatment − previous investigations for chest pain. • Check if any of the following symptoms of ischaemia are present. These may indicate an ACS: – Pain in the chest and/or other areas (for example, the arms, back or jaw) lasting longer than 15 minutes. – Chest pain with nausea and vomiting, marked sweating or breathlessness (or a combination of these), or with haemodynamic instability. – New onset chest pain, or abrupt deterioration in stable angina, with recurrent pain occurring frequently with little or no exertion and often lasting longer than 15 minutes. • Central chest pain may not be the main symptom. • Do not use response to glyceryl trinitrate (GTN) to make a diagnosis of ACS. • Do not assess symptoms of an ACS differently in men and women or among different ethnic groups. • Advise people about seeking medical help if they have further chest pain. • If the chest pain is non-cardiac, explain this to the person and refer for further investigation if appropriate. Return to diagnostic criteria Implementing NICE Guidance www. nice. org. uk


