6c1ba927dfc2201ac15cf3cb74767364.ppt
- Количество слайдов: 75
 Presentation to the Portfolio Committee on Health 15 October 2014
Presentation to the Portfolio Committee on Health 15 October 2014
 Structure of the Presentation I. Vision and Mission II. National Development Plan III. National Health Sector Priorities IV. Programme Performance V. Human Resource Management VI. Financial Management VII. Conclusion 2
Structure of the Presentation I. Vision and Mission II. National Development Plan III. National Health Sector Priorities IV. Programme Performance V. Human Resource Management VI. Financial Management VII. Conclusion 2
 Vision and Mission Vision A long and healthy life for all South Africans. Mission To improve the health status through the prevention of illnesses and the promotion of healthy lifestyles and consistently to improve the health care delivery system by focusing on access, equity, efficiency, quality and sustainability. 3 3
Vision and Mission Vision A long and healthy life for all South Africans. Mission To improve the health status through the prevention of illnesses and the promotion of healthy lifestyles and consistently to improve the health care delivery system by focusing on access, equity, efficiency, quality and sustainability. 3 3
 National Development Plan 2030 The Health Sector derives its vision and mandate from NDP 2030. By 2030, South Africa should have: • Raised the life expectancy of South Africans to at least 70 years. • Progressively improve TB prevention and cure. • Reduced maternal, infant and child mortality. • Significantly reduced prevalence of non-communicable diseases. • Reduced injury, accidents and violence by 50 percent from 2010 levels. • Completed health system reforms. • Established primary healthcare teams to provide care to families and communities. • Implement universal health coverage. • Fill posts with skilled, committed and competent individuals.
National Development Plan 2030 The Health Sector derives its vision and mandate from NDP 2030. By 2030, South Africa should have: • Raised the life expectancy of South Africans to at least 70 years. • Progressively improve TB prevention and cure. • Reduced maternal, infant and child mortality. • Significantly reduced prevalence of non-communicable diseases. • Reduced injury, accidents and violence by 50 percent from 2010 levels. • Completed health system reforms. • Established primary healthcare teams to provide care to families and communities. • Implement universal health coverage. • Fill posts with skilled, committed and competent individuals.
 National Development Plan 2030 The NDP also identifies a set of nine (9) priorities that highlight the key interventions required to achieve a more effective health system, which will contribute to the achievement of the desired outcomes. The priorities are as follows: – Address the social determinants that affect health and diseases. – Strengthen the health system. – Improve health information systems. – Prevent and reduce the disease burden and promote health. – Finance universal healthcare coverage. – Improve human resources in the health sector. – Review management positions and appointments and strengthen accountability mechanisms. – Improve quality by using evidence. – Development meaningful public-private partnerships. 5
National Development Plan 2030 The NDP also identifies a set of nine (9) priorities that highlight the key interventions required to achieve a more effective health system, which will contribute to the achievement of the desired outcomes. The priorities are as follows: – Address the social determinants that affect health and diseases. – Strengthen the health system. – Improve health information systems. – Prevent and reduce the disease burden and promote health. – Finance universal healthcare coverage. – Improve human resources in the health sector. – Review management positions and appointments and strengthen accountability mechanisms. – Improve quality by using evidence. – Development meaningful public-private partnerships. 5
 National Health Sector Priorities The major strategic framework for the work of the National Department of Health (NDo. H) during 2013/14 was the Negotiated Service Delivery Agreement (NSDA) 2010 to 2014, which provides key strategies for accelerating progress towards the vision of “A Long and Healthy Life for all South Africans”. The four outputs required from the health sector in terms of the NSDA are: (a) Increased life expectancy; (b) Reduction in maternal and child mortality rates; (c) Tuberculosis; and (d) Strengthening health system effectiveness. These outputs are interlinked. An effective and well-functioning health system is essential for the attainment of the desired improved health outcomes. The NSDA 2010 to 2014 informed the development, implementation and monitoring of the Annual Performance Plan (APP) of the NDo. H for 2013/14. 6 6
National Health Sector Priorities The major strategic framework for the work of the National Department of Health (NDo. H) during 2013/14 was the Negotiated Service Delivery Agreement (NSDA) 2010 to 2014, which provides key strategies for accelerating progress towards the vision of “A Long and Healthy Life for all South Africans”. The four outputs required from the health sector in terms of the NSDA are: (a) Increased life expectancy; (b) Reduction in maternal and child mortality rates; (c) Tuberculosis; and (d) Strengthening health system effectiveness. These outputs are interlinked. An effective and well-functioning health system is essential for the attainment of the desired improved health outcomes. The NSDA 2010 to 2014 informed the development, implementation and monitoring of the Annual Performance Plan (APP) of the NDo. H for 2013/14. 6 6
 Programme Performance q Programme 1: Administration q Programme 2: National Health Insurance, Health Planning and Systems Enablement q Programme 3: HIV and AIDS, TB and Maternal and Child Health q Programme 4: Primary Health Care q Programme 5: Hospital, Tertiary Health Services and Human Resource Development q Programme 6: Health Regulation and Compliance Management 7
Programme Performance q Programme 1: Administration q Programme 2: National Health Insurance, Health Planning and Systems Enablement q Programme 3: HIV and AIDS, TB and Maternal and Child Health q Programme 4: Primary Health Care q Programme 5: Hospital, Tertiary Health Services and Human Resource Development q Programme 6: Health Regulation and Compliance Management 7
 Programme 1 Administration 8
Programme 1 Administration 8
 Programme 1 • Performance management systems have been reviewed and aligned to Department’s strategic direction. • Vacancy rate was reduced to 4. 34% which is below DPSA’s target of 10%. • 103 out of 109 senior managers signed and timeously filed performance agreements with DPSA. • The National Department of Health (NDo. H) has for the last 3 consecutive years obtained an “unqualified audit opinion” on external audit of the financial information by the Auditor-General (SA), including 2013/14 financial year. • 7 out of 9 provinces had qualified audits. All provinces have developed financial improvement plans. 9
Programme 1 • Performance management systems have been reviewed and aligned to Department’s strategic direction. • Vacancy rate was reduced to 4. 34% which is below DPSA’s target of 10%. • 103 out of 109 senior managers signed and timeously filed performance agreements with DPSA. • The National Department of Health (NDo. H) has for the last 3 consecutive years obtained an “unqualified audit opinion” on external audit of the financial information by the Auditor-General (SA), including 2013/14 financial year. • 7 out of 9 provinces had qualified audits. All provinces have developed financial improvement plans. 9
 Programme 2 National Health Insurance, Health Planning and Systems Enablement 10
Programme 2 National Health Insurance, Health Planning and Systems Enablement 10
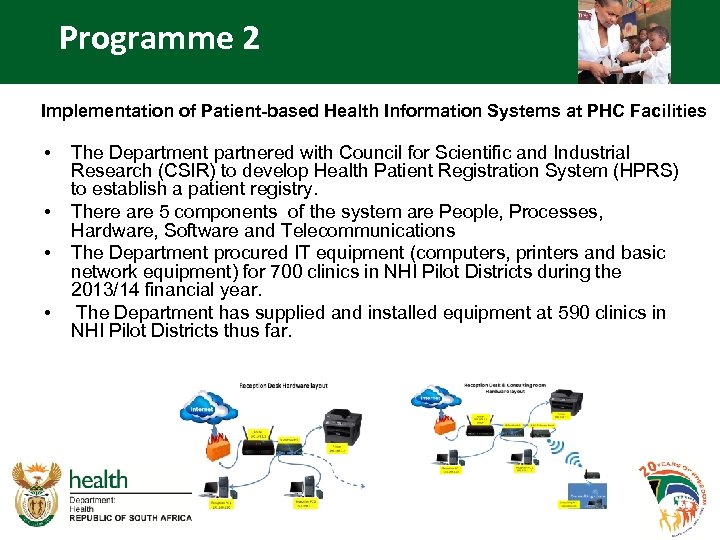 Programme 2 Implementation of Patient-based Health Information Systems at PHC Facilities • • The Department partnered with Council for Scientific and Industrial Research (CSIR) to develop Health Patient Registration System (HPRS) to establish a patient registry. There are 5 components of the system are People, Processes, Hardware, Software and Telecommunications The Department procured IT equipment (computers, printers and basic network equipment) for 700 clinics in NHI Pilot Districts during the 2013/14 financial year. The Department has supplied and installed equipment at 590 clinics in NHI Pilot Districts thus far.
Programme 2 Implementation of Patient-based Health Information Systems at PHC Facilities • • The Department partnered with Council for Scientific and Industrial Research (CSIR) to develop Health Patient Registration System (HPRS) to establish a patient registry. There are 5 components of the system are People, Processes, Hardware, Software and Telecommunications The Department procured IT equipment (computers, printers and basic network equipment) for 700 clinics in NHI Pilot Districts during the 2013/14 financial year. The Department has supplied and installed equipment at 590 clinics in NHI Pilot Districts thus far.
 HARDWARE AND NETWORK INSTALLATION SOFTWARE INSTALLATION AND TRAINING
HARDWARE AND NETWORK INSTALLATION SOFTWARE INSTALLATION AND TRAINING
 Programme 2 Implementation of Patient-based Health Information Systems at PHC Facilities (continue. . . ) Broadband Connectivity is essential to implement the HPRS: • All Clinics in both KZN NHI Pilot Districts were connected during the financial year. • The Department is working with Department of Telecommunications and Postal Services (DTPS) to scale up connectivity to all clinics in NHI Districts through the SA Connect project. The Department is also currently expanding the roll out of web-based District Health Information System (DHIS) daily data capture (DDC) where connectivity exist. Both HPRS and DHIS DDC will be scaled up to 700 clinics in NHI Pilot Districts.
Programme 2 Implementation of Patient-based Health Information Systems at PHC Facilities (continue. . . ) Broadband Connectivity is essential to implement the HPRS: • All Clinics in both KZN NHI Pilot Districts were connected during the financial year. • The Department is working with Department of Telecommunications and Postal Services (DTPS) to scale up connectivity to all clinics in NHI Districts through the SA Connect project. The Department is also currently expanding the roll out of web-based District Health Information System (DHIS) daily data capture (DDC) where connectivity exist. Both HPRS and DHIS DDC will be scaled up to 700 clinics in NHI Pilot Districts.
 Programme 2 Information Systems, Monitoring & Evaluation • The Normative Standards Framework for e. Health for the public health sector was developed and approved. The e. Health Strategy seeks to ensure an Integrated National Patient-Based Information System. • Electronic Register (TIER. Net) was implemented in 2754 health facilities. • Rapid Mortality Surveillance was conducted by MRC and UCT School of Actuary Sciences to provide estimates for life expectancy, maternal and child mortality rates. 14
Programme 2 Information Systems, Monitoring & Evaluation • The Normative Standards Framework for e. Health for the public health sector was developed and approved. The e. Health Strategy seeks to ensure an Integrated National Patient-Based Information System. • Electronic Register (TIER. Net) was implemented in 2754 health facilities. • Rapid Mortality Surveillance was conducted by MRC and UCT School of Actuary Sciences to provide estimates for life expectancy, maternal and child mortality rates. 14
 Programme 2 Research • The Council for Scientific and Industrial Research (CSIR) undertook an assessment of Patient Information Systems used in Primary Health Care settings to make recommendations for effective patient information system. • Under the auspices of the National Health Research Council a National Health Research Database is being established. • The National Health Research Scholars Programme which seeks to produce 1 000 Ph. D graduates in all fields of Health Sciences over the next 10 years, was expanded in 2013/14. 13 Ph. D candidates were enrolled in 2012/13; and 26 candidates enrolled in 2013/14. 15
Programme 2 Research • The Council for Scientific and Industrial Research (CSIR) undertook an assessment of Patient Information Systems used in Primary Health Care settings to make recommendations for effective patient information system. • Under the auspices of the National Health Research Council a National Health Research Database is being established. • The National Health Research Scholars Programme which seeks to produce 1 000 Ph. D graduates in all fields of Health Sciences over the next 10 years, was expanded in 2013/14. 13 Ph. D candidates were enrolled in 2012/13; and 26 candidates enrolled in 2013/14. 15
 Programme 2 Sector-wide Procurement • An early warning system has been implemented to prevent stock-outs at facility level. • A toll free line is also available to report low stock levels. • In an effort to improve access and to decongest public facilities, work has started in NHI pilot districts whereby stable patients on chronic medicines are offered the opportunity to collect their chronic medicines at a point close to their homes or workplaces. • To monitor the overall performance of the Provincial Pharmaceutical Services, a dashboard of key pharmaceutical indicators has been developed. 16
Programme 2 Sector-wide Procurement • An early warning system has been implemented to prevent stock-outs at facility level. • A toll free line is also available to report low stock levels. • In an effort to improve access and to decongest public facilities, work has started in NHI pilot districts whereby stable patients on chronic medicines are offered the opportunity to collect their chronic medicines at a point close to their homes or workplaces. • To monitor the overall performance of the Provincial Pharmaceutical Services, a dashboard of key pharmaceutical indicators has been developed. 16
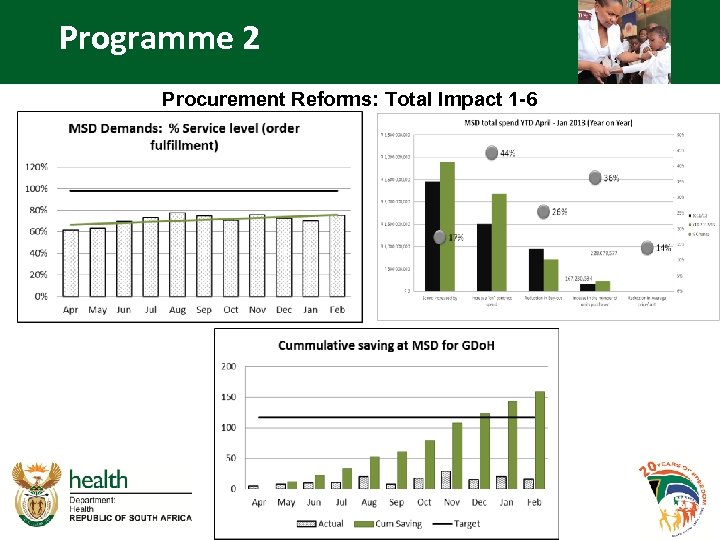 Programme 2 Procurement Reforms: Total Impact 1 -6
Programme 2 Procurement Reforms: Total Impact 1 -6
 Programme 2 Procurement Reforms Impact • • Availability of drugs has improved from 58% to 73% Out of contract procurement decreased from 36% to 12% Buy-outs decreased by 26% Warehouse productivity has improved by 26% reducing the requirement for overtime as well additional hiring of staff Order processing time has been improved from pre project levels of 32 days on average to current levels of 11 days Cost of distribution has decreased by 27% Non Essential Medicine List orders reduced from 50% to 40% Backorders have reduced by 30% Financial savings of over R 150, 000 have been achieved through the improved governance around procurement and contract management.
Programme 2 Procurement Reforms Impact • • Availability of drugs has improved from 58% to 73% Out of contract procurement decreased from 36% to 12% Buy-outs decreased by 26% Warehouse productivity has improved by 26% reducing the requirement for overtime as well additional hiring of staff Order processing time has been improved from pre project levels of 32 days on average to current levels of 11 days Cost of distribution has decreased by 27% Non Essential Medicine List orders reduced from 50% to 40% Backorders have reduced by 30% Financial savings of over R 150, 000 have been achieved through the improved governance around procurement and contract management.
 Programme 2 National Health Insurance (NHI) • • • The Department continued to implement the new re-engineered Primary Health Care (PHC) model for South Africa which consist of District Clinical Specialist Teams; Ward Based Primary Health Care Outreach Teams, the Integrated School Health Programme and the Contracting of General Practitioners to work in Primary Health Care Facilities. District Clinical Specialist Teams with at least three specialists were established in 46 of the 52 health districts. A total of 1 063 Municipal Ward Based Primary Health Care Outreach Teams (WBPHCOT) were established. 119 GPs were contracted for NHI. The various interventions implemented in the pilot districts focused on developing capacity in the area of monitoring and evaluation, supply chain management, and planning and strengthening the referral system. 19
Programme 2 National Health Insurance (NHI) • • • The Department continued to implement the new re-engineered Primary Health Care (PHC) model for South Africa which consist of District Clinical Specialist Teams; Ward Based Primary Health Care Outreach Teams, the Integrated School Health Programme and the Contracting of General Practitioners to work in Primary Health Care Facilities. District Clinical Specialist Teams with at least three specialists were established in 46 of the 52 health districts. A total of 1 063 Municipal Ward Based Primary Health Care Outreach Teams (WBPHCOT) were established. 119 GPs were contracted for NHI. The various interventions implemented in the pilot districts focused on developing capacity in the area of monitoring and evaluation, supply chain management, and planning and strengthening the referral system. 19
 Programme 2 Integrated School Health Programme • In order to strengthen the school health programme launched in October 2012, the National Department of Health has purchased 60 mobiles which have been deployed and are being used in the NHI pilot districts • A further 28 mobiles are currently on order for delivering in this financial year
Programme 2 Integrated School Health Programme • In order to strengthen the school health programme launched in October 2012, the National Department of Health has purchased 60 mobiles which have been deployed and are being used in the NHI pilot districts • A further 28 mobiles are currently on order for delivering in this financial year
 • • 33 1668 medical male circumcision were performed 6 688950 people aged 15 -49 were tested for HIV 662312 new clients were put on ARVs Immunization coverage under 1 year reached 91. 8% 77. 5% of Antenatal clients initiated on ART 89% of pregnant women delivered at facilities TB cure rate at 75. 9% 88. 7% of TB clients were tested for HIV 21
• • 33 1668 medical male circumcision were performed 6 688950 people aged 15 -49 were tested for HIV 662312 new clients were put on ARVs Immunization coverage under 1 year reached 91. 8% 77. 5% of Antenatal clients initiated on ART 89% of pregnant women delivered at facilities TB cure rate at 75. 9% 88. 7% of TB clients were tested for HIV 21
 Programme 2 1 st AU International Maternal, Newborn & Child Health Conference • Co-hosted with the AU and held in August 2013 • Attended by Ministers and deputy Ministers from as well as officials from more than 30 countries • The objective was to review progress in the implementation of the Campaign on the accelerated reduction of maternal and child mortality (CARMMA) • Recommendations from the conference were adopted by the joint AU/AFRO Health Ministers meeting held on 16 -17 April 2014 22
Programme 2 1 st AU International Maternal, Newborn & Child Health Conference • Co-hosted with the AU and held in August 2013 • Attended by Ministers and deputy Ministers from as well as officials from more than 30 countries • The objective was to review progress in the implementation of the Campaign on the accelerated reduction of maternal and child mortality (CARMMA) • Recommendations from the conference were adopted by the joint AU/AFRO Health Ministers meeting held on 16 -17 April 2014 22
 Programme 2 Strategies to Improve: National Health Insurance (APP 2014/15) • Installation of consulting rooms • GPs programme for NHI – Contracting – Accurate documentation – GP induction programme • Expand from GP contracting to other health professionals 23
Programme 2 Strategies to Improve: National Health Insurance (APP 2014/15) • Installation of consulting rooms • GPs programme for NHI – Contracting – Accurate documentation – GP induction programme • Expand from GP contracting to other health professionals 23
 24
24
 Programme 2 Strategies to Improve: Performance Data Quality • Implement web based District Health Information System to improve data quality and timeliness of routine health information. • Strengthen the implementation of the District Health Management Information System (DHMIS) Policy • Improve the quality of data collection tools at PHC Facilities – Conclude the review of the National Indicator Data Set (NIDS) 2015 -2017 – Develop and implement standardised guidelines for review of Provincial Indicator Data Set 2015 -2017 – Rationalisation of PHC Registers Project • Integrate TB (ETR. net) and HIV (Tier. net) Health Information Systems • Accelerate the implementation of the e. Health strategy
Programme 2 Strategies to Improve: Performance Data Quality • Implement web based District Health Information System to improve data quality and timeliness of routine health information. • Strengthen the implementation of the District Health Management Information System (DHMIS) Policy • Improve the quality of data collection tools at PHC Facilities – Conclude the review of the National Indicator Data Set (NIDS) 2015 -2017 – Develop and implement standardised guidelines for review of Provincial Indicator Data Set 2015 -2017 – Rationalisation of PHC Registers Project • Integrate TB (ETR. net) and HIV (Tier. net) Health Information Systems • Accelerate the implementation of the e. Health strategy
 Programme 3 HIV and AIDS, TB and Maternal and Child Health 26
Programme 3 HIV and AIDS, TB and Maternal and Child Health 26
 27
27
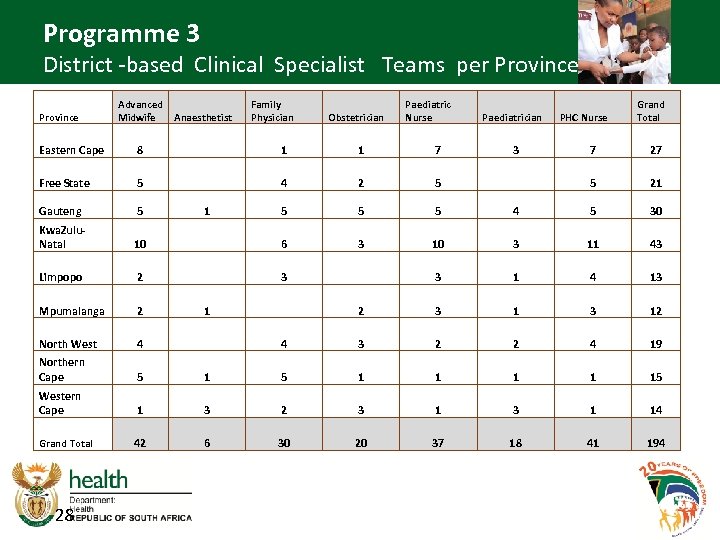 Programme 3 District -based Clinical Specialist Teams per Province Advanced Anaesthetist Midwife Family Physician Obstetrician Paediatric Nurse Paediatrician PHC Nurse Grand Total Eastern Cape 8 1 1 7 3 7 27 Free State 5 4 2 5 5 21 Gauteng 5 1 5 5 5 4 5 30 Kwa. Zulu. Natal 10 6 3 10 3 11 43 Limpopo 2 3 3 1 4 13 Mpumalanga 2 1 2 3 12 North West 4 4 3 2 2 4 19 Northern Cape 5 1 1 15 Western Cape 1 3 2 3 1 14 Grand Total 42 6 30 20 37 18 41 194 28
Programme 3 District -based Clinical Specialist Teams per Province Advanced Anaesthetist Midwife Family Physician Obstetrician Paediatric Nurse Paediatrician PHC Nurse Grand Total Eastern Cape 8 1 1 7 3 7 27 Free State 5 4 2 5 5 21 Gauteng 5 1 5 5 5 4 5 30 Kwa. Zulu. Natal 10 6 3 10 3 11 43 Limpopo 2 3 3 1 4 13 Mpumalanga 2 1 2 3 12 North West 4 4 3 2 2 4 19 Northern Cape 5 1 1 15 Western Cape 1 3 2 3 1 14 Grand Total 42 6 30 20 37 18 41 194 28
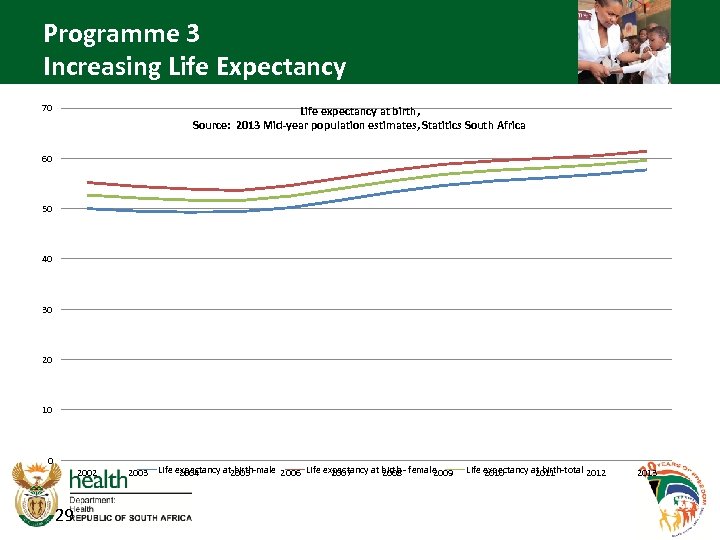 Programme 3 Increasing Life Expectancy 70 Life expectancy at birth, Source: 2013 Mid-year population estimates, Statitics South Africa 60 50 40 30 20 10 0 2002 29 2003 Life expectancy at 2005 birth-male 2006 Life expectancy at birth - female 2004 2007 2008 2009 Life expectancy at birth-total 2012 2010 2011 2013
Programme 3 Increasing Life Expectancy 70 Life expectancy at birth, Source: 2013 Mid-year population estimates, Statitics South Africa 60 50 40 30 20 10 0 2002 29 2003 Life expectancy at 2005 birth-male 2006 Life expectancy at birth - female 2004 2007 2008 2009 Life expectancy at birth-total 2012 2010 2011 2013
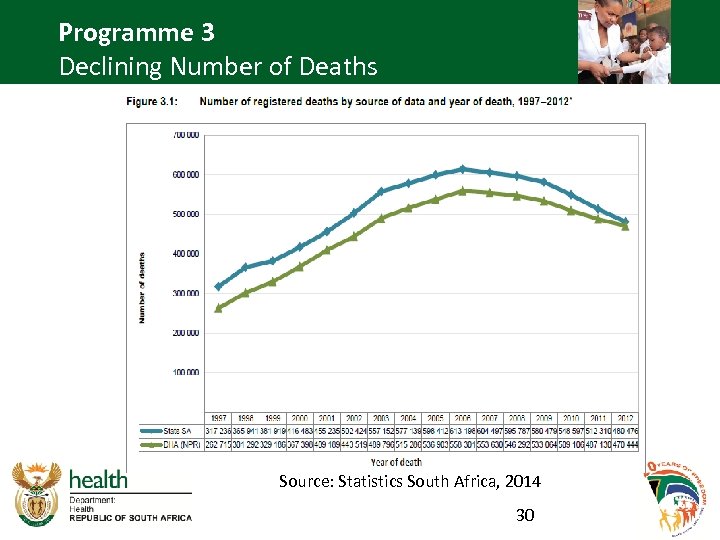 Programme 3 Declining Number of Deaths Source: Statistics South Africa, 2014 30
Programme 3 Declining Number of Deaths Source: Statistics South Africa, 2014 30
 Programme 3 Death Trends • The total number of deaths registered by Home Affairs was 480 476, which was a decline of 6, 2% from the 512 310 deaths that occurred in 2011. • The median age at death (age at which deaths occurred, indicating early or late mortality in the population) is increasing. • From 2008 – 2011, the highest proportion of deaths occurred amongst young adults. However, the 2012 data show that the age profile of deaths in South Africa is starting to normalise, with the older age groups having a higher proportion of deaths than young adults. 31
Programme 3 Death Trends • The total number of deaths registered by Home Affairs was 480 476, which was a decline of 6, 2% from the 512 310 deaths that occurred in 2011. • The median age at death (age at which deaths occurred, indicating early or late mortality in the population) is increasing. • From 2008 – 2011, the highest proportion of deaths occurred amongst young adults. However, the 2012 data show that the age profile of deaths in South Africa is starting to normalise, with the older age groups having a higher proportion of deaths than young adults. 31
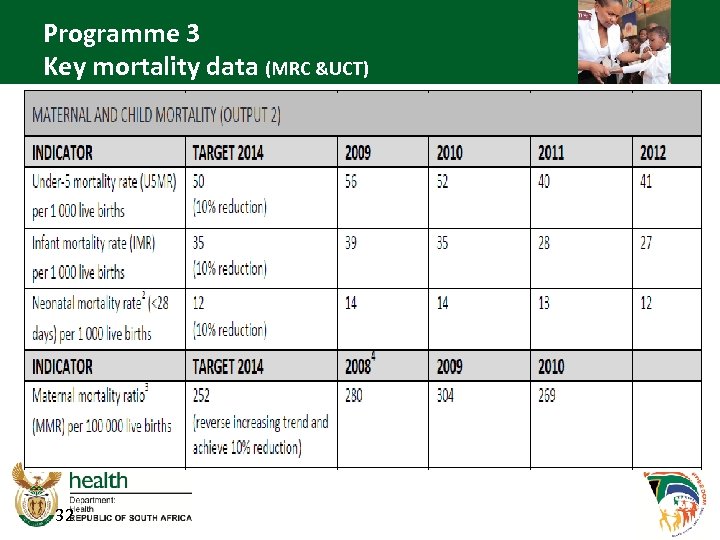 Programme 3 Key mortality data (MRC &UCT) 32
Programme 3 Key mortality data (MRC &UCT) 32
 Programme 4 Primary Health Care 33
Programme 4 Primary Health Care 33
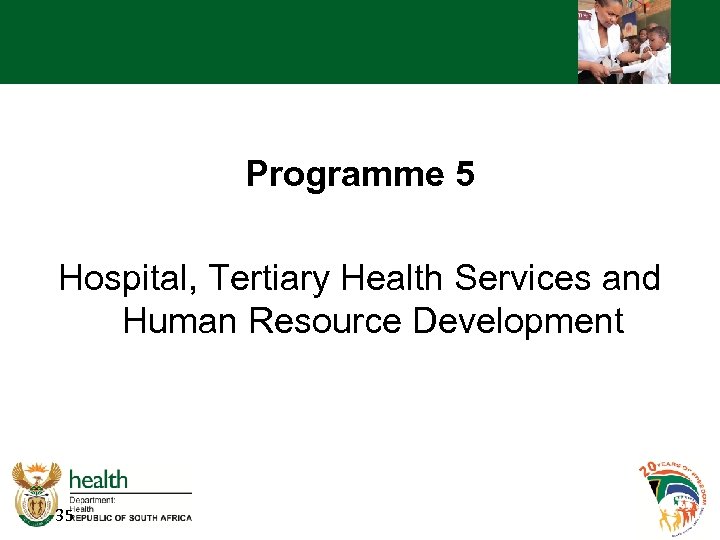
 Programme 4 • PHC utilization rate is of 2. 4 visits person per annum was achieved • A total of 1063 Municipal Ward Based Primary Health Care Outreach teams established. • “Ideal Clinic” initiative is being implemented in primary health care facility to improve quality. • National Environmental Health Policy was approved and published in the Government Gazette for implementation. • Malaria incidence reduced from 0. 60 to 0. 17 per 1000. • Infant & Young Child Feeding Policy was approved and published. • A diagnostic & implementation of evaluation of Government Nutrition Programme for under five years of age was undertaken. 34
Programme 4 • PHC utilization rate is of 2. 4 visits person per annum was achieved • A total of 1063 Municipal Ward Based Primary Health Care Outreach teams established. • “Ideal Clinic” initiative is being implemented in primary health care facility to improve quality. • National Environmental Health Policy was approved and published in the Government Gazette for implementation. • Malaria incidence reduced from 0. 60 to 0. 17 per 1000. • Infant & Young Child Feeding Policy was approved and published. • A diagnostic & implementation of evaluation of Government Nutrition Programme for under five years of age was undertaken. 34
 Programme 5 Hospital, Tertiary Health Services and Human Resource Development 35
Programme 5 Hospital, Tertiary Health Services and Human Resource Development 35
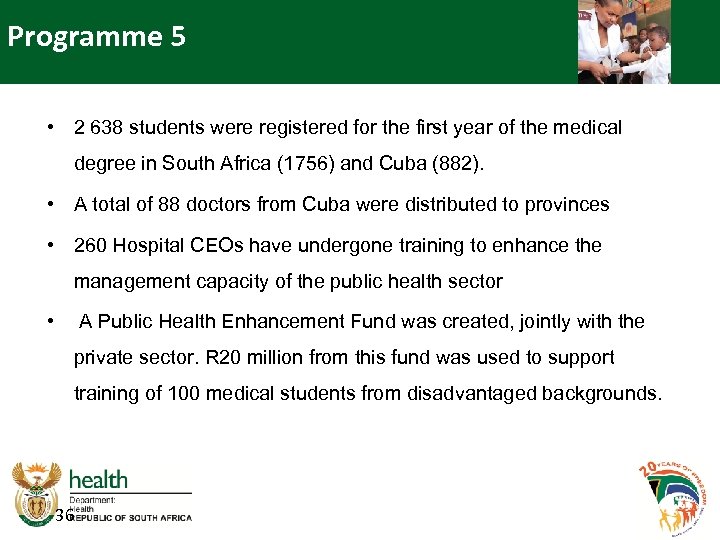 Programme 5 • 2 638 students were registered for the first year of the medical degree in South Africa (1756) and Cuba (882). • A total of 88 doctors from Cuba were distributed to provinces • 260 Hospital CEOs have undergone training to enhance the management capacity of the public health sector • A Public Health Enhancement Fund was created, jointly with the private sector. R 20 million from this fund was used to support training of 100 medical students from disadvantaged backgrounds. 36
Programme 5 • 2 638 students were registered for the first year of the medical degree in South Africa (1756) and Cuba (882). • A total of 88 doctors from Cuba were distributed to provinces • 260 Hospital CEOs have undergone training to enhance the management capacity of the public health sector • A Public Health Enhancement Fund was created, jointly with the private sector. R 20 million from this fund was used to support training of 100 medical students from disadvantaged backgrounds. 36
 Programme 5 9 898 Community Health Workers (CHWs) were trained on Phase One Foundation Training. They have been placed in the Municipal Ward Based Outreach Teams to support the PHC re-engineering process. 37
Programme 5 9 898 Community Health Workers (CHWs) were trained on Phase One Foundation Training. They have been placed in the Municipal Ward Based Outreach Teams to support the PHC re-engineering process. 37
 Programme 5 Human Resources for Health • During 2013/14, the Workload Indicators for Staffing Need (WISN) model from WHO was used to determine health workforce staffing requirements. Staffing norms for clinics and community health centres were developed and adopted as guidelines for implementation by National Health Council. • A total of 75 521 health professionals and non-professional were trained in programmes dealing with HIV and AIDS, STIs, TB and chronic disease management. • The National Department of Health enrolled 70 Forensic Interns out of a pool of qualified but unemployed applicants. 38
Programme 5 Human Resources for Health • During 2013/14, the Workload Indicators for Staffing Need (WISN) model from WHO was used to determine health workforce staffing requirements. Staffing norms for clinics and community health centres were developed and adopted as guidelines for implementation by National Health Council. • A total of 75 521 health professionals and non-professional were trained in programmes dealing with HIV and AIDS, STIs, TB and chronic disease management. • The National Department of Health enrolled 70 Forensic Interns out of a pool of qualified but unemployed applicants. 38
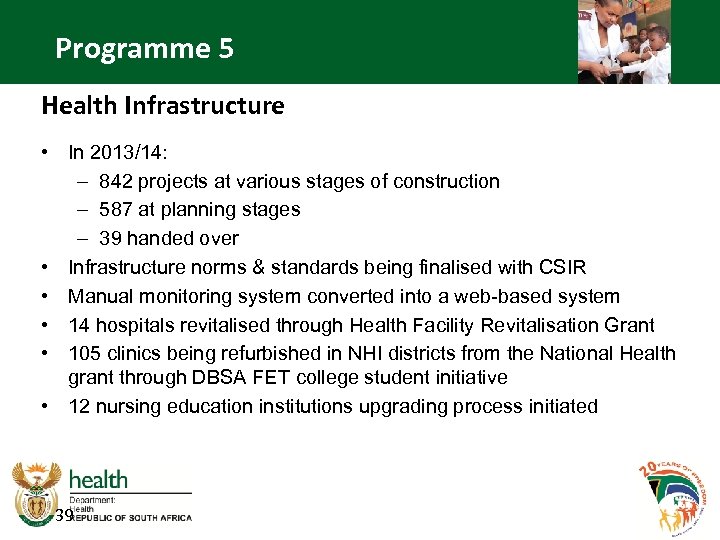 Programme 5 Health Infrastructure • In 2013/14: – 842 projects at various stages of construction – 587 at planning stages – 39 handed over • Infrastructure norms & standards being finalised with CSIR • Manual monitoring system converted into a web-based system • 14 hospitals revitalised through Health Facility Revitalisation Grant • 105 clinics being refurbished in NHI districts from the National Health grant through DBSA FET college student initiative • 12 nursing education institutions upgrading process initiated 39
Programme 5 Health Infrastructure • In 2013/14: – 842 projects at various stages of construction – 587 at planning stages – 39 handed over • Infrastructure norms & standards being finalised with CSIR • Manual monitoring system converted into a web-based system • 14 hospitals revitalised through Health Facility Revitalisation Grant • 105 clinics being refurbished in NHI districts from the National Health grant through DBSA FET college student initiative • 12 nursing education institutions upgrading process initiated 39


 Physical Progress in the MP Province Ermelo Clinic (Gert Sibande) Lebohang Clinic (Gert Sibande) 42
Physical Progress in the MP Province Ermelo Clinic (Gert Sibande) Lebohang Clinic (Gert Sibande) 42
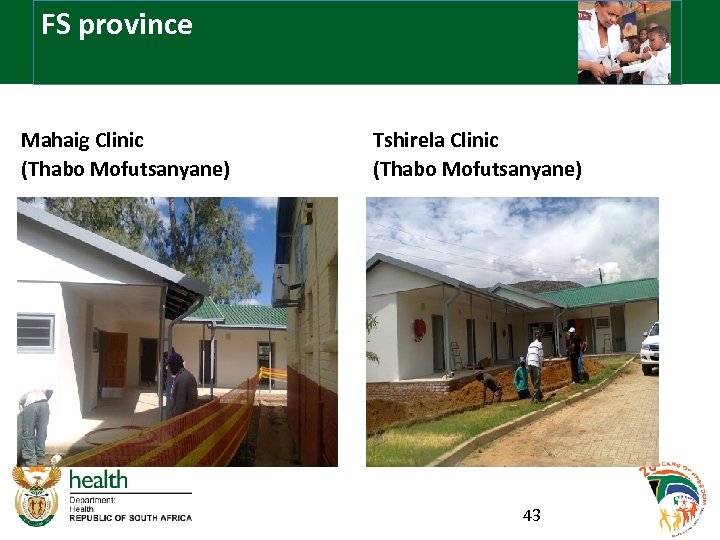 FS province Mahaig Clinic (Thabo Mofutsanyane) Tshirela Clinic (Thabo Mofutsanyane) 43
FS province Mahaig Clinic (Thabo Mofutsanyane) Tshirela Clinic (Thabo Mofutsanyane) 43
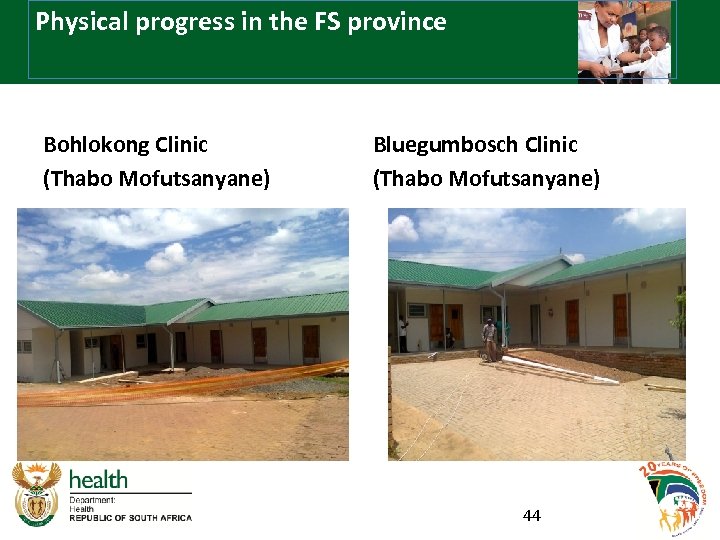 Physical progress in the FS province Bohlokong Clinic (Thabo Mofutsanyane) Bluegumbosch Clinic (Thabo Mofutsanyane) 44
Physical progress in the FS province Bohlokong Clinic (Thabo Mofutsanyane) Bluegumbosch Clinic (Thabo Mofutsanyane) 44
 Portchefstroom clinic close to completion 45
Portchefstroom clinic close to completion 45
 Portchefstroom clinic furniture and medical equipment 46
Portchefstroom clinic furniture and medical equipment 46
 Human Resource Management 47
Human Resource Management 47
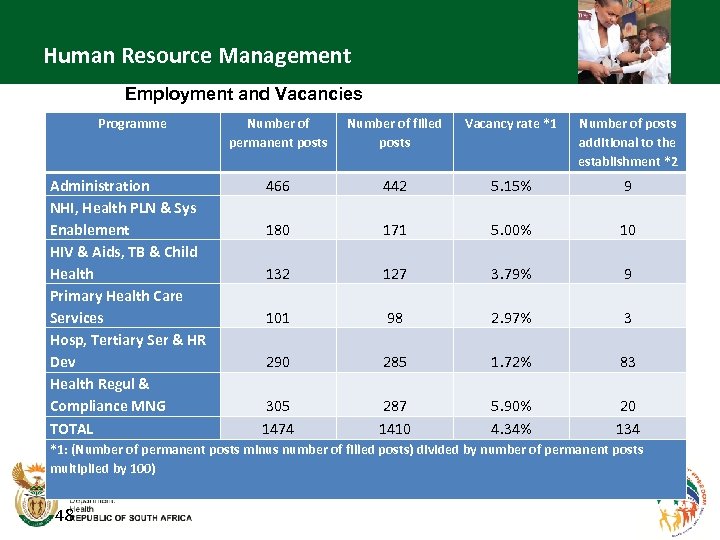 Human Resource Management Employment and Vacancies Programme Number of permanent posts Number of filled posts Vacancy rate *1 Number of posts additional to the establishment *2 Administration NHI, Health PLN & Sys Enablement HIV & Aids, TB & Child Health Primary Health Care Services Hosp, Tertiary Ser & HR Dev Health Regul & Compliance MNG TOTAL 466 442 5. 15% 9 180 171 5. 00% 10 132 127 3. 79% 9 101 98 2. 97% 3 290 285 1. 72% 83 305 1474 287 1410 5. 90% 4. 34% 20 134 *1: (Number of permanent posts minus number of filled posts) divided by number of permanent posts multiplied by 100) 48
Human Resource Management Employment and Vacancies Programme Number of permanent posts Number of filled posts Vacancy rate *1 Number of posts additional to the establishment *2 Administration NHI, Health PLN & Sys Enablement HIV & Aids, TB & Child Health Primary Health Care Services Hosp, Tertiary Ser & HR Dev Health Regul & Compliance MNG TOTAL 466 442 5. 15% 9 180 171 5. 00% 10 132 127 3. 79% 9 101 98 2. 97% 3 290 285 1. 72% 83 305 1474 287 1410 5. 90% 4. 34% 20 134 *1: (Number of permanent posts minus number of filled posts) divided by number of permanent posts multiplied by 100) 48
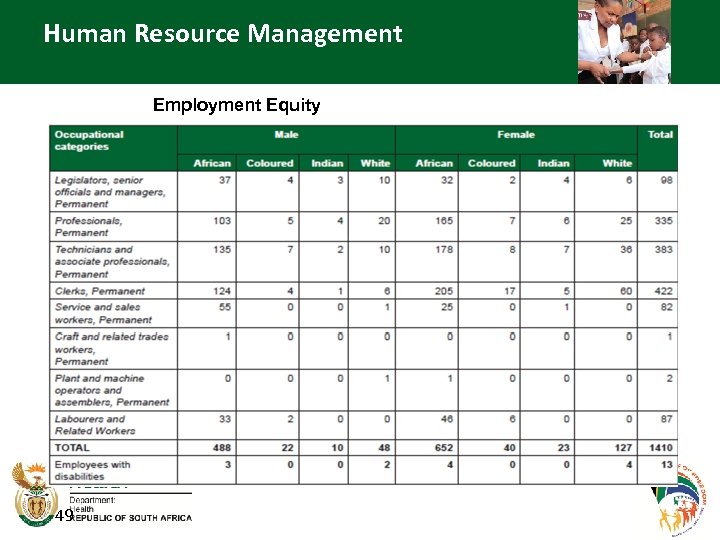 Human Resource Management Employment Equity 49
Human Resource Management Employment Equity 49
 Programme 6 Health Regulation and Compliance Management 50
Programme 6 Health Regulation and Compliance Management 50
 Programme 6 • Formalised the establishment of the Office of Health Standards Compliance (OHSC) as an independent public entity. Approval of the National Health Amendment Act by Parliament and its signing into law by the President, in July 2013. The proclamation of the National Health Amendment Health Act (Act 12 of 2013) by the President of the Republic of South Africa on 2 nd September 2013 and inauguration of the Board in January 2014. • “Mock” inspections in 582 facilities, thus exceeding the target of 567 and more than doubling the number conducted in the previous year. • A total of 1 928 health facilities conducted self-assessments and 868 facilities developed annual Quality Improvement Plans. • Improved management of patient complaints in preparation for the establishment of the Health Standards Ombudsman, was supported through training in five provinces (reaching 1 221 officials) on a new in-house complaints management database and the revision of the national complaints protocol. 51
Programme 6 • Formalised the establishment of the Office of Health Standards Compliance (OHSC) as an independent public entity. Approval of the National Health Amendment Act by Parliament and its signing into law by the President, in July 2013. The proclamation of the National Health Amendment Health Act (Act 12 of 2013) by the President of the Republic of South Africa on 2 nd September 2013 and inauguration of the Board in January 2014. • “Mock” inspections in 582 facilities, thus exceeding the target of 567 and more than doubling the number conducted in the previous year. • A total of 1 928 health facilities conducted self-assessments and 868 facilities developed annual Quality Improvement Plans. • Improved management of patient complaints in preparation for the establishment of the Health Standards Ombudsman, was supported through training in five provinces (reaching 1 221 officials) on a new in-house complaints management database and the revision of the national complaints protocol. 51
 Financial Management 52
Financial Management 52
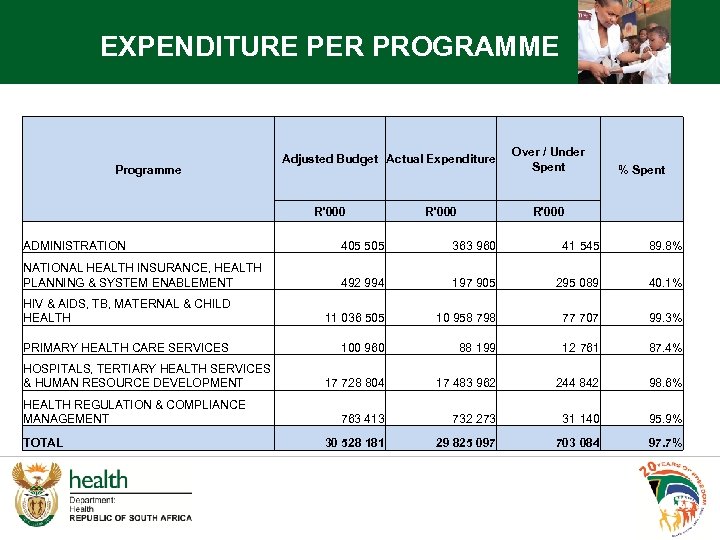 EXPENDITURE PER PROGRAMME Programme Adjusted Budget Actual Expenditure R'000 Over / Under Spent % Spent R'000 ADMINISTRATION 405 505 363 960 41 545 89. 8% NATIONAL HEALTH INSURANCE, HEALTH PLANNING & SYSTEM ENABLEMENT 492 994 197 905 295 089 40. 1% HIV & AIDS, TB, MATERNAL & CHILD HEALTH 11 036 505 10 958 798 77 707 99. 3% PRIMARY HEALTH CARE SERVICES 100 960 88 199 12 761 87. 4% 17 728 804 17 483 962 244 842 98. 6% 763 413 732 273 31 140 95. 9% 30 528 181 29 825 097 703 084 97. 7% HOSPITALS, TERTIARY HEALTH SERVICES & HUMAN RESOURCE DEVELOPMENT HEALTH REGULATION & COMPLIANCE MANAGEMENT TOTAL
EXPENDITURE PER PROGRAMME Programme Adjusted Budget Actual Expenditure R'000 Over / Under Spent % Spent R'000 ADMINISTRATION 405 505 363 960 41 545 89. 8% NATIONAL HEALTH INSURANCE, HEALTH PLANNING & SYSTEM ENABLEMENT 492 994 197 905 295 089 40. 1% HIV & AIDS, TB, MATERNAL & CHILD HEALTH 11 036 505 10 958 798 77 707 99. 3% PRIMARY HEALTH CARE SERVICES 100 960 88 199 12 761 87. 4% 17 728 804 17 483 962 244 842 98. 6% 763 413 732 273 31 140 95. 9% 30 528 181 29 825 097 703 084 97. 7% HOSPITALS, TERTIARY HEALTH SERVICES & HUMAN RESOURCE DEVELOPMENT HEALTH REGULATION & COMPLIANCE MANAGEMENT TOTAL
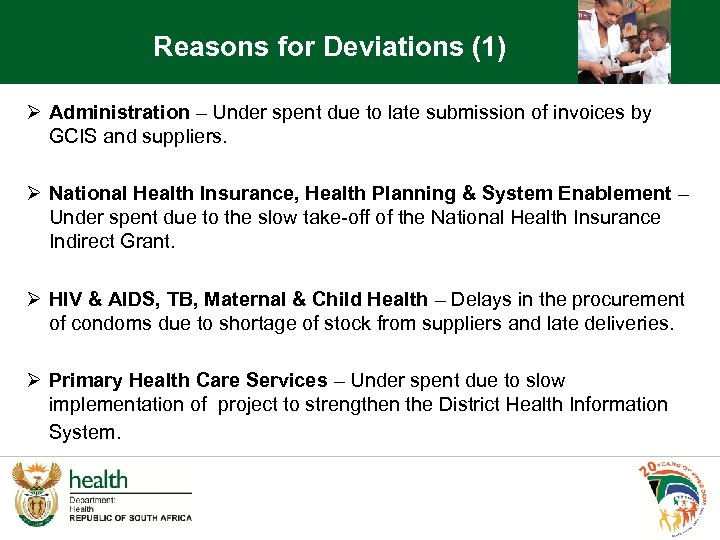 Reasons for Deviations (1) Ø Administration – Under spent due to late submission of invoices by GCIS and suppliers. Ø National Health Insurance, Health Planning & System Enablement – Under spent due to the slow take-off of the National Health Insurance Indirect Grant. Ø HIV & AIDS, TB, Maternal & Child Health – Delays in the procurement of condoms due to shortage of stock from suppliers and late deliveries. Ø Primary Health Care Services – Under spent due to slow implementation of project to strengthen the District Health Information System.
Reasons for Deviations (1) Ø Administration – Under spent due to late submission of invoices by GCIS and suppliers. Ø National Health Insurance, Health Planning & System Enablement – Under spent due to the slow take-off of the National Health Insurance Indirect Grant. Ø HIV & AIDS, TB, Maternal & Child Health – Delays in the procurement of condoms due to shortage of stock from suppliers and late deliveries. Ø Primary Health Care Services – Under spent due to slow implementation of project to strengthen the District Health Information System.
 Reasons for Deviation (2) Ø Hospitals, Tertiary Health Services & Human Resource Development – Under spent due to late submission of invoices by Forensic Chemistry Laboratories and incomplete infrastructure projects funded through Health Facility Infrastructure Indirect Grant. Ø Health Regulation & Compliance Management – Under spent on Goods and Services under Pharmaceutical Trade & Product Regulation, Office of Health Standards Compliance and the Commissioner for Occupational Diseases.
Reasons for Deviation (2) Ø Hospitals, Tertiary Health Services & Human Resource Development – Under spent due to late submission of invoices by Forensic Chemistry Laboratories and incomplete infrastructure projects funded through Health Facility Infrastructure Indirect Grant. Ø Health Regulation & Compliance Management – Under spent on Goods and Services under Pharmaceutical Trade & Product Regulation, Office of Health Standards Compliance and the Commissioner for Occupational Diseases.
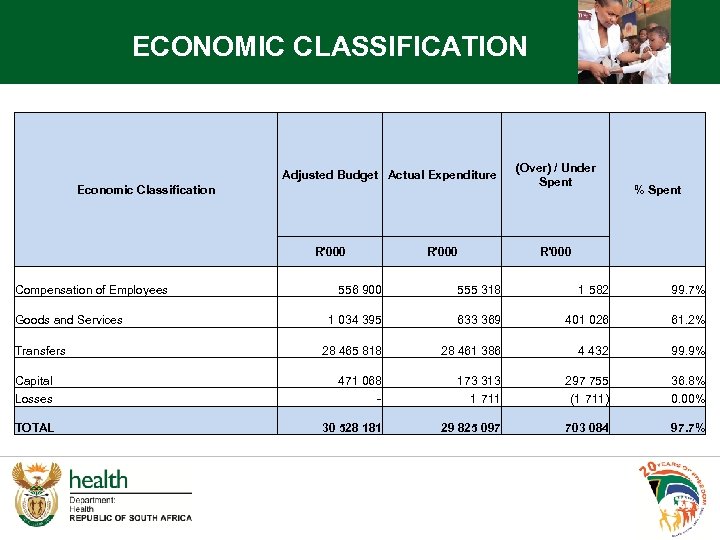 ECONOMIC CLASSIFICATION Adjusted Budget Actual Expenditure Economic Classification R'000 (Over) / Under Spent % Spent R'000 Compensation of Employees 556 900 555 318 1 582 99. 7% Goods and Services 1 034 395 633 369 401 026 61. 2% Transfers 28 465 818 28 461 386 4 432 99. 9% Capital 471 068 173 313 297 755 36. 8% Losses - 1 711 (1 711) 0. 00% 29 825 097 703 084 97. 7% TOTAL 30 528 181
ECONOMIC CLASSIFICATION Adjusted Budget Actual Expenditure Economic Classification R'000 (Over) / Under Spent % Spent R'000 Compensation of Employees 556 900 555 318 1 582 99. 7% Goods and Services 1 034 395 633 369 401 026 61. 2% Transfers 28 465 818 28 461 386 4 432 99. 9% Capital 471 068 173 313 297 755 36. 8% Losses - 1 711 (1 711) 0. 00% 29 825 097 703 084 97. 7% TOTAL 30 528 181
 Reasons for Deviation Ø Compensation of Employees and Transfers spent within the target norm. Contributors to under spending Ø Goods and Services – Slow take-off of the National Health Insurance Indirect Grant and delays in delivery of condoms. Ø Capital – Incomplete infrastructure projects funded through Health Facility Infrastructure Indirect Grant.
Reasons for Deviation Ø Compensation of Employees and Transfers spent within the target norm. Contributors to under spending Ø Goods and Services – Slow take-off of the National Health Insurance Indirect Grant and delays in delivery of condoms. Ø Capital – Incomplete infrastructure projects funded through Health Facility Infrastructure Indirect Grant.
 Conditional Grants
Conditional Grants
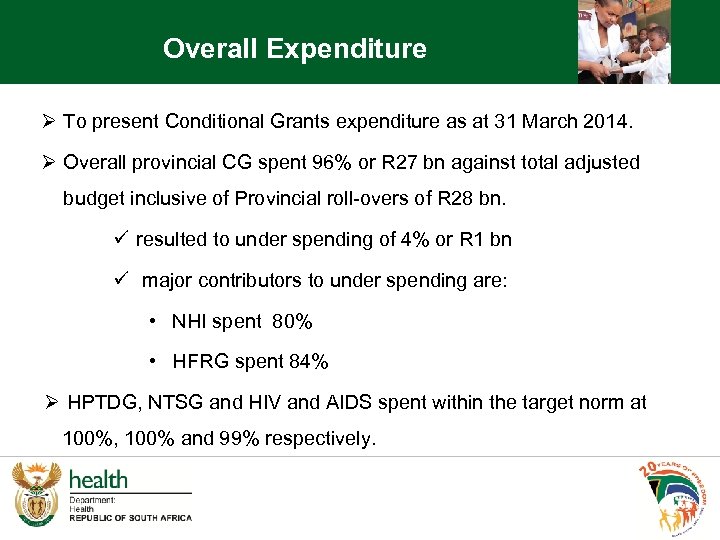 Overall Expenditure Ø To present Conditional Grants expenditure as at 31 March 2014. Ø Overall provincial CG spent 96% or R 27 bn against total adjusted budget inclusive of Provincial roll-overs of R 28 bn. ü resulted to under spending of 4% or R 1 bn ü major contributors to under spending are: • NHI spent 80% • HFRG spent 84% Ø HPTDG, NTSG and HIV and AIDS spent within the target norm at 100%, 100% and 99% respectively.
Overall Expenditure Ø To present Conditional Grants expenditure as at 31 March 2014. Ø Overall provincial CG spent 96% or R 27 bn against total adjusted budget inclusive of Provincial roll-overs of R 28 bn. ü resulted to under spending of 4% or R 1 bn ü major contributors to under spending are: • NHI spent 80% • HFRG spent 84% Ø HPTDG, NTSG and HIV and AIDS spent within the target norm at 100%, 100% and 99% respectively.
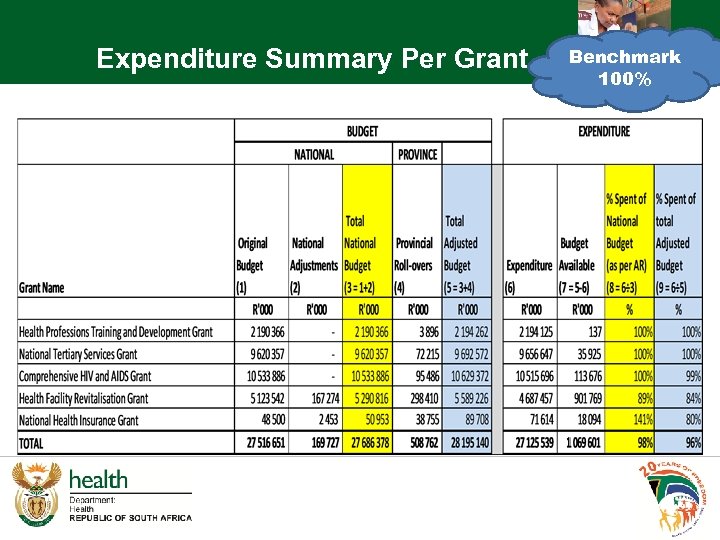 Expenditure Summary Per Grant Benchmark 100%
Expenditure Summary Per Grant Benchmark 100%
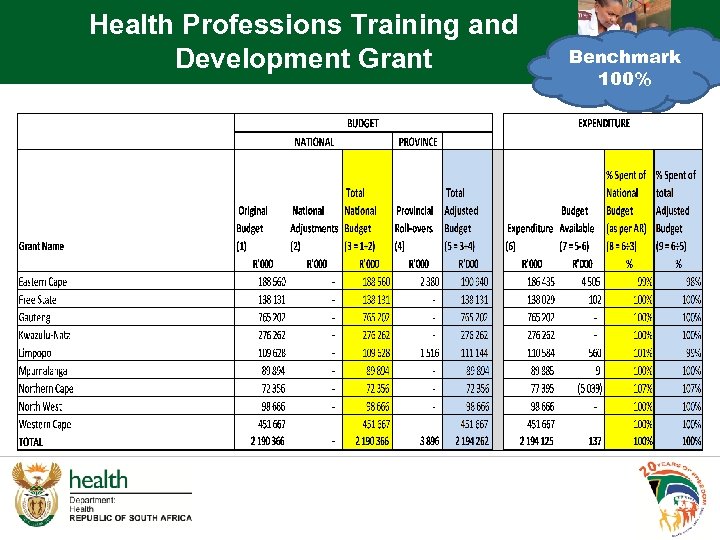 Health Professions Training and Development Grant Benchmark 33, 3% 100%
Health Professions Training and Development Grant Benchmark 33, 3% 100%
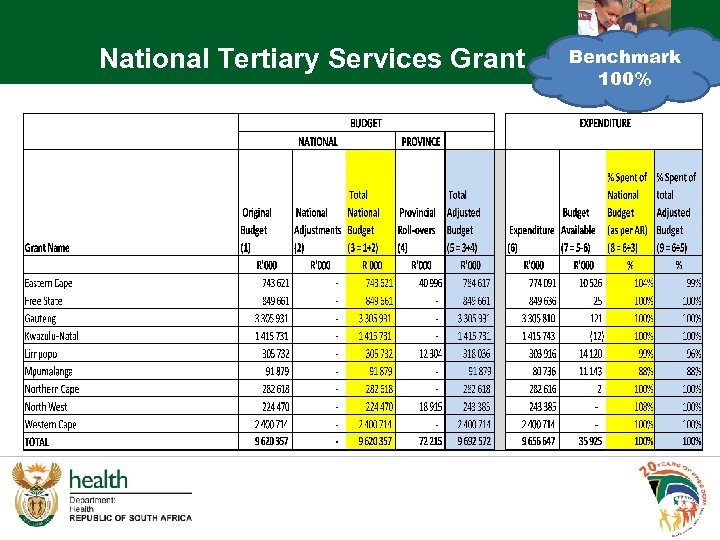 National Tertiary Services Grant Benchmark 100%
National Tertiary Services Grant Benchmark 100%
 Reasons for Deviations National Tertiary Services Grant: • With exception of Limpopo and Mpumalanga all other provinces spent within the target norm. Limpopo • Delay in the completion of installation of Cathlab resulted in under spending on CAPEX. Mpumalanga • Delays in the delivery of medical equipment.
Reasons for Deviations National Tertiary Services Grant: • With exception of Limpopo and Mpumalanga all other provinces spent within the target norm. Limpopo • Delay in the completion of installation of Cathlab resulted in under spending on CAPEX. Mpumalanga • Delays in the delivery of medical equipment.
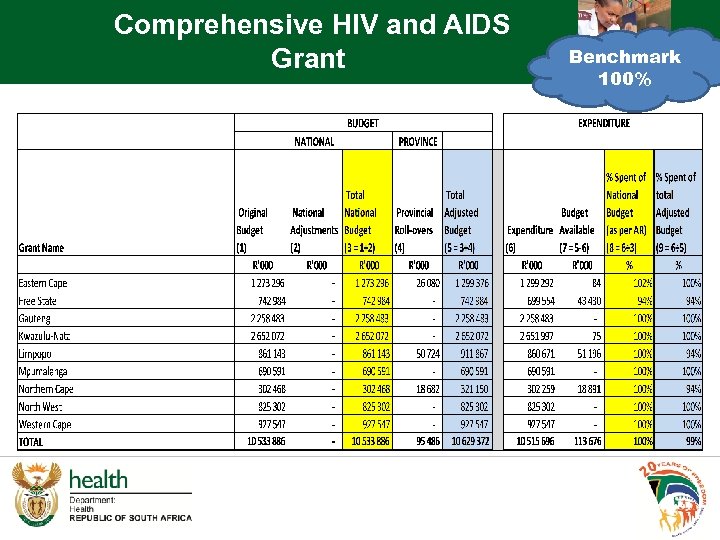 Comprehensive HIV and AIDS Grant Benchmark 100%
Comprehensive HIV and AIDS Grant Benchmark 100%
 Reasons for Deviations Comprehensive HIV/AIDS Grant: Free State • Under spent due Provincial cash flow challenges experienced. Limpopo • Delays in delivery of condoms by suppliers. Northern Cape • Delays in the procurement of condoms due shortage of stock from suppliers.
Reasons for Deviations Comprehensive HIV/AIDS Grant: Free State • Under spent due Provincial cash flow challenges experienced. Limpopo • Delays in delivery of condoms by suppliers. Northern Cape • Delays in the procurement of condoms due shortage of stock from suppliers.
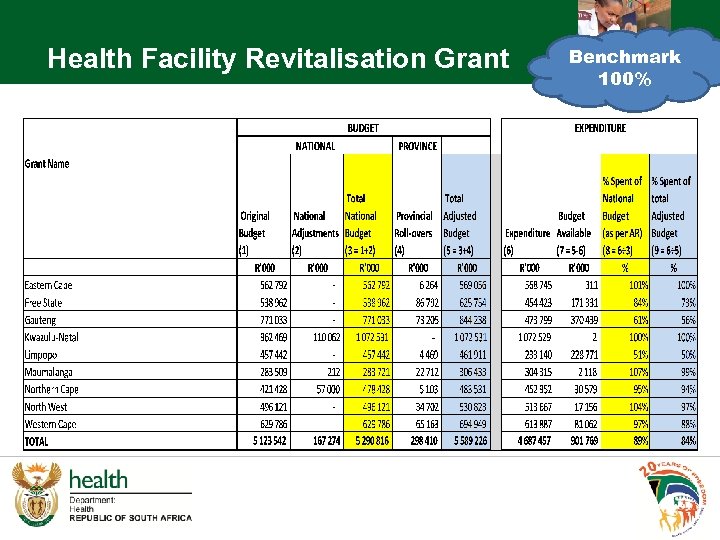 Health Facility Revitalisation Grant Benchmark 100%
Health Facility Revitalisation Grant Benchmark 100%
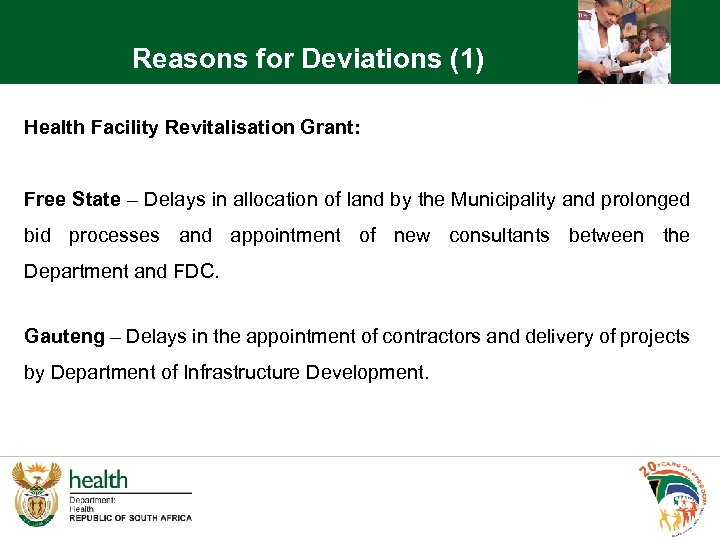 Reasons for Deviations (1) Health Facility Revitalisation Grant: Free State – Delays in allocation of land by the Municipality and prolonged bid processes and appointment of new consultants between the Department and FDC. Gauteng – Delays in the appointment of contractors and delivery of projects by Department of Infrastructure Development.
Reasons for Deviations (1) Health Facility Revitalisation Grant: Free State – Delays in allocation of land by the Municipality and prolonged bid processes and appointment of new consultants between the Department and FDC. Gauteng – Delays in the appointment of contractors and delivery of projects by Department of Infrastructure Development.
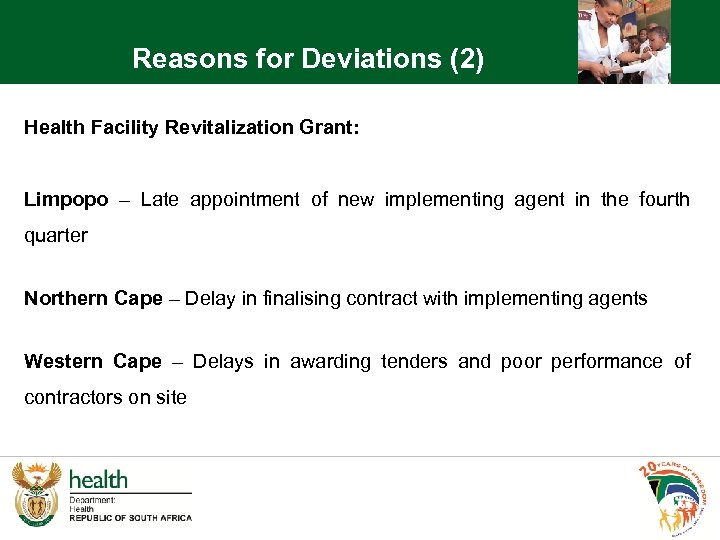 Reasons for Deviations (2) Health Facility Revitalization Grant: Limpopo – Late appointment of new implementing agent in the fourth quarter Northern Cape – Delay in finalising contract with implementing agents Western Cape – Delays in awarding tenders and poor performance of contractors on site
Reasons for Deviations (2) Health Facility Revitalization Grant: Limpopo – Late appointment of new implementing agent in the fourth quarter Northern Cape – Delay in finalising contract with implementing agents Western Cape – Delays in awarding tenders and poor performance of contractors on site
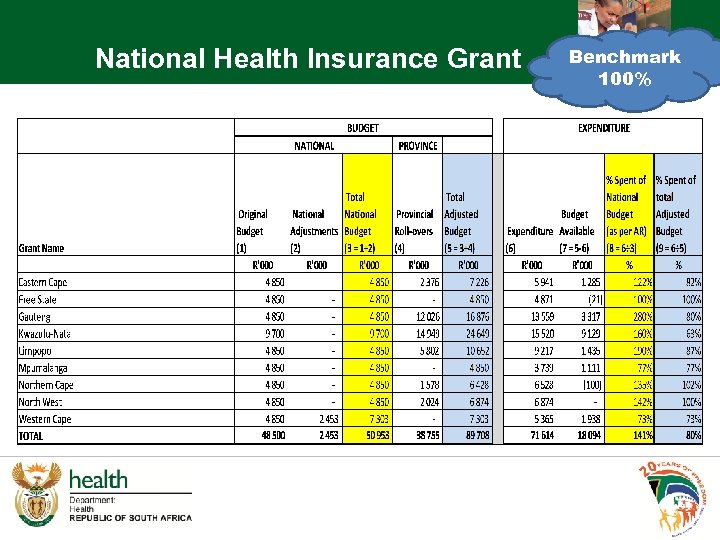 National Health Insurance Grant Benchmark 100%
National Health Insurance Grant Benchmark 100%
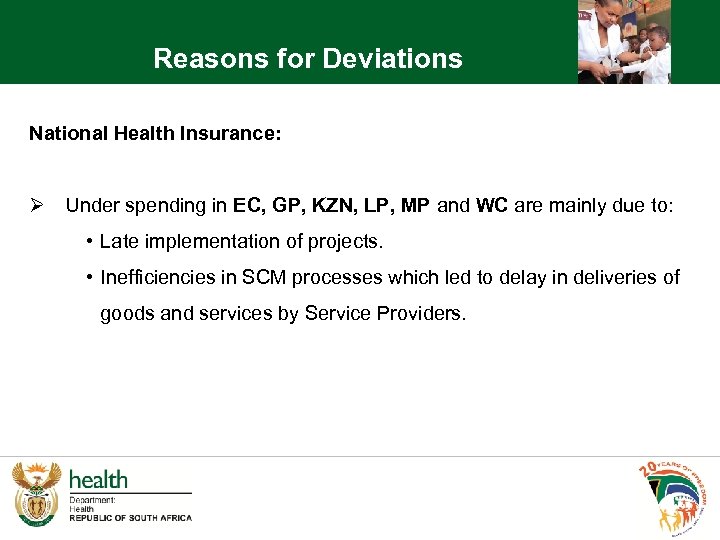 Reasons for Deviations National Health Insurance: Ø Under spending in EC, GP, KZN, LP, MP and WC are mainly due to: • Late implementation of projects. • Inefficiencies in SCM processes which led to delay in deliveries of goods and services by Service Providers.
Reasons for Deviations National Health Insurance: Ø Under spending in EC, GP, KZN, LP, MP and WC are mainly due to: • Late implementation of projects. • Inefficiencies in SCM processes which led to delay in deliveries of goods and services by Service Providers.
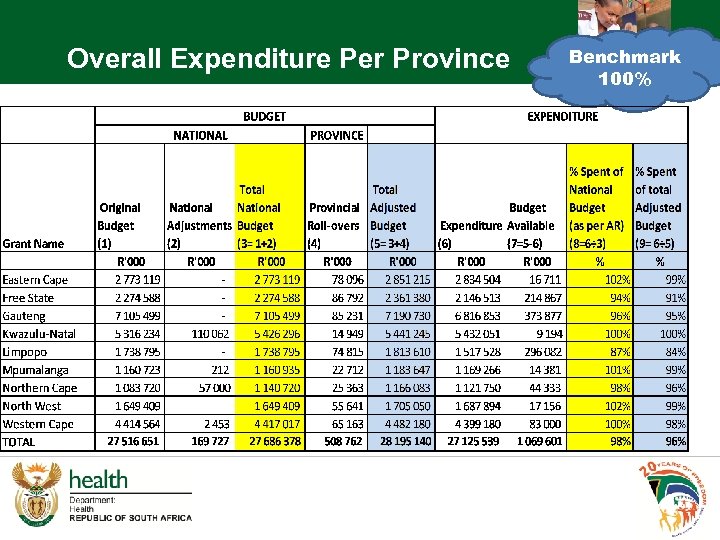 Overall Expenditure Per Province Benchmark 100%
Overall Expenditure Per Province Benchmark 100%
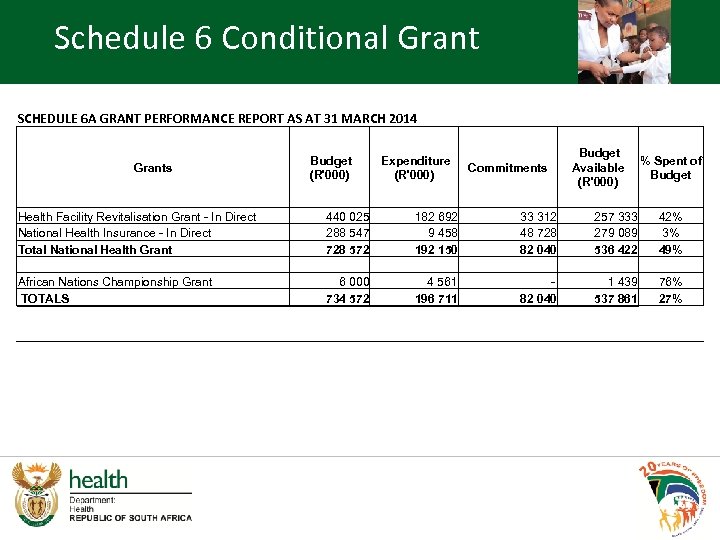 Schedule 6 Conditional Grant SCHEDULE 6 A GRANT PERFORMANCE REPORT AS AT 31 MARCH 2014 Grants Health Facility Revitalisation Grant - In Direct National Health Insurance - In Direct Total National Health Grant African Nations Championship Grant TOTALS Budget (R'000) 440 025 288 547 728 572 6 000 734 572 Expenditure (R'000) 182 692 9 458 192 150 4 561 196 711 Commitments 33 312 48 728 82 040 - 82 040 Budget Available (R'000) 257 333 279 089 536 422 1 439 537 861 % Spent of Budget 42% 3% 49% 76% 27%
Schedule 6 Conditional Grant SCHEDULE 6 A GRANT PERFORMANCE REPORT AS AT 31 MARCH 2014 Grants Health Facility Revitalisation Grant - In Direct National Health Insurance - In Direct Total National Health Grant African Nations Championship Grant TOTALS Budget (R'000) 440 025 288 547 728 572 6 000 734 572 Expenditure (R'000) 182 692 9 458 192 150 4 561 196 711 Commitments 33 312 48 728 82 040 - 82 040 Budget Available (R'000) 257 333 279 089 536 422 1 439 537 861 % Spent of Budget 42% 3% 49% 76% 27%
 Reasons for Deviations (Schedule 6) Health Facility Revitalisation Grant - Indirect • Poor management of projects by implementing agents • Delays in awarding of tenders and appointment of contractors. National Health Insurance • Under spending caused by challenges in attracting GPs across the country. • Submission of inaccurate and incomplete timesheets by GPs leading to delay in process of payments – service provider sourced to administer payroll system for GPs. African Nations Championship (CHAN) • Failure to procure capital items by Western Cape province.
Reasons for Deviations (Schedule 6) Health Facility Revitalisation Grant - Indirect • Poor management of projects by implementing agents • Delays in awarding of tenders and appointment of contractors. National Health Insurance • Under spending caused by challenges in attracting GPs across the country. • Submission of inaccurate and incomplete timesheets by GPs leading to delay in process of payments – service provider sourced to administer payroll system for GPs. African Nations Championship (CHAN) • Failure to procure capital items by Western Cape province.
 Conclusions § Key milestones were achieved during the financial year 2013/14, in relation to the objectives and targets set in the National Do. H Annual Performance Plan for this period § Challenges were also experienced, which affected some areas of service delivery. § These challenges are addressed in the National Do. H Annual Performance Plan for 2014/15. 74
Conclusions § Key milestones were achieved during the financial year 2013/14, in relation to the objectives and targets set in the National Do. H Annual Performance Plan for this period § Challenges were also experienced, which affected some areas of service delivery. § These challenges are addressed in the National Do. H Annual Performance Plan for 2014/15. 74
 Thank You 75
Thank You 75


