654787ba29e345495943d52ca2331e0f.ppt
- Количество слайдов: 44
 Preschool/School Supportive Health Services Program (SSHSP) Medicaid-in-Education Training on Compliance Agreement, Written Compliance Policies and Program Update 1
Preschool/School Supportive Health Services Program (SSHSP) Medicaid-in-Education Training on Compliance Agreement, Written Compliance Policies and Program Update 1
 NYS Roles in SSHSP State Education Department (SED) n n Implementation Special Education Policy Department of Health/Office of Health Insurance Programs (OHIP) n n Medicaid Policy Payment Methodology Office of Medicaid Inspector General (OMIG) n Audit 2
NYS Roles in SSHSP State Education Department (SED) n n Implementation Special Education Policy Department of Health/Office of Health Insurance Programs (OHIP) n n Medicaid Policy Payment Methodology Office of Medicaid Inspector General (OMIG) n Audit 2
 Agenda n n n How did we get here? NYS Compliance Agreement OMIG Compliance Program Medicaid State Plan Amendment Implementation of New SSHSP Requirements Contact Information 3
Agenda n n n How did we get here? NYS Compliance Agreement OMIG Compliance Program Medicaid State Plan Amendment Implementation of New SSHSP Requirements Contact Information 3
 How Did We Get Here? n Federal Audits n Settlement n Compliance Agreement 4
How Did We Get Here? n Federal Audits n Settlement n Compliance Agreement 4
 Compliance n NYS Compliance Agreement n Implementation Plan n OMIG Compliance Program 5
Compliance n NYS Compliance Agreement n Implementation Plan n OMIG Compliance Program 5
 Compliance Agreement n n n n NYS SSHSP Compliance Policy Confidential Disclosure Policy Compliance Officer/Compliance Committee Audit Requirements Independent Audits Annual Written Reports Training State Plan Amendment 6
Compliance Agreement n n n n NYS SSHSP Compliance Policy Confidential Disclosure Policy Compliance Officer/Compliance Committee Audit Requirements Independent Audits Annual Written Reports Training State Plan Amendment 6
 Compliance Agreement Goals n Remedy the consequences of past practices and policies n Ensure that policies and practices are modified to achieve compliance 7
Compliance Agreement Goals n Remedy the consequences of past practices and policies n Ensure that policies and practices are modified to achieve compliance 7
 Compliance Agreement Adoption of two specific policies: n n NYS Policy Regarding Its Commitment to Ensure Compliance Confidential Disclosure Policy (inappropriate billing) 8
Compliance Agreement Adoption of two specific policies: n n NYS Policy Regarding Its Commitment to Ensure Compliance Confidential Disclosure Policy (inappropriate billing) 8
 Compliance Agreement Confidential Disclosure Policy n The NYS Supportive Health Services Program Compliance Agreement, entered into on July 20, 2009, by the NYS Department of Health (DOH), the NYS Education Department (SED) and the NYS Office of the Medicaid Inspector General (OMIG) requires that the State and local school districts shall establish a confidential disclosure mechanism enabling employees to disclose anonymously any practices or billing procedures, deemed by the employee to be inappropriate, to the State's Compliance Officer. 9
Compliance Agreement Confidential Disclosure Policy n The NYS Supportive Health Services Program Compliance Agreement, entered into on July 20, 2009, by the NYS Department of Health (DOH), the NYS Education Department (SED) and the NYS Office of the Medicaid Inspector General (OMIG) requires that the State and local school districts shall establish a confidential disclosure mechanism enabling employees to disclose anonymously any practices or billing procedures, deemed by the employee to be inappropriate, to the State's Compliance Officer. 9
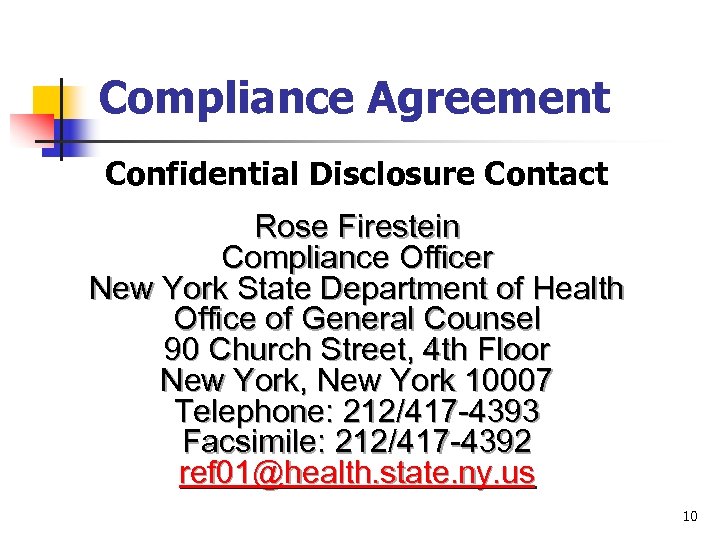 Compliance Agreement Confidential Disclosure Contact Rose Firestein Compliance Officer New York State Department of Health Office of General Counsel 90 Church Street, 4 th Floor New York, New York 10007 Telephone: 212/417 -4393 Facsimile: 212/417 -4392 ref 01@health. state. ny. us 10
Compliance Agreement Confidential Disclosure Contact Rose Firestein Compliance Officer New York State Department of Health Office of General Counsel 90 Church Street, 4 th Floor New York, New York 10007 Telephone: 212/417 -4393 Facsimile: 212/417 -4392 ref 01@health. state. ny. us 10
 OMIG Compliance Program n n Effective October 1, 2009 all districts and counties billing Medicaid in excess of $500, 000 (gross) require a written Compliance Program Presentation by Robert Hussar, OMIG, is available both as a Power. Point document and in the web cast format on SED’s website OMIG – www. omig. state. ny. us – see Compliance tab 11
OMIG Compliance Program n n Effective October 1, 2009 all districts and counties billing Medicaid in excess of $500, 000 (gross) require a written Compliance Program Presentation by Robert Hussar, OMIG, is available both as a Power. Point document and in the web cast format on SED’s website OMIG – www. omig. state. ny. us – see Compliance tab 11
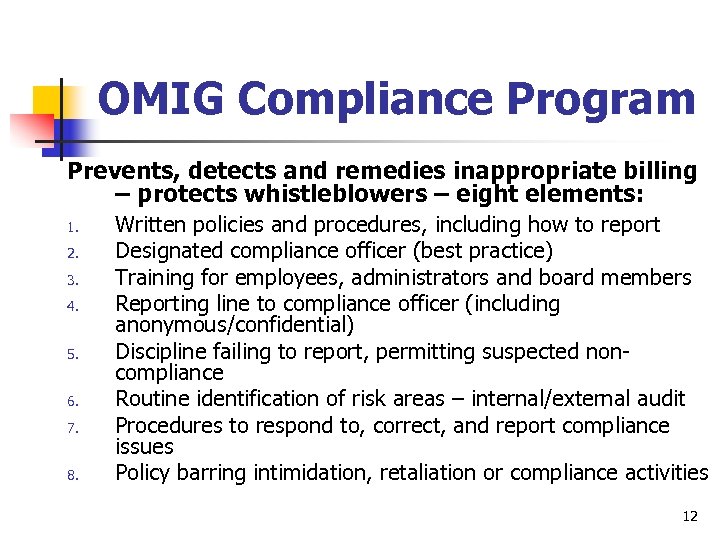 OMIG Compliance Program Prevents, detects and remedies inappropriate billing – protects whistleblowers – eight elements: 1. 2. 3. 4. 5. 6. 7. 8. Written policies and procedures, including how to report Designated compliance officer (best practice) Training for employees, administrators and board members Reporting line to compliance officer (including anonymous/confidential) Discipline failing to report, permitting suspected noncompliance Routine identification of risk areas – internal/external audit Procedures to respond to, correct, and report compliance issues Policy barring intimidation, retaliation or compliance activities 12
OMIG Compliance Program Prevents, detects and remedies inappropriate billing – protects whistleblowers – eight elements: 1. 2. 3. 4. 5. 6. 7. 8. Written policies and procedures, including how to report Designated compliance officer (best practice) Training for employees, administrators and board members Reporting line to compliance officer (including anonymous/confidential) Discipline failing to report, permitting suspected noncompliance Routine identification of risk areas – internal/external audit Procedures to respond to, correct, and report compliance issues Policy barring intimidation, retaliation or compliance activities 12
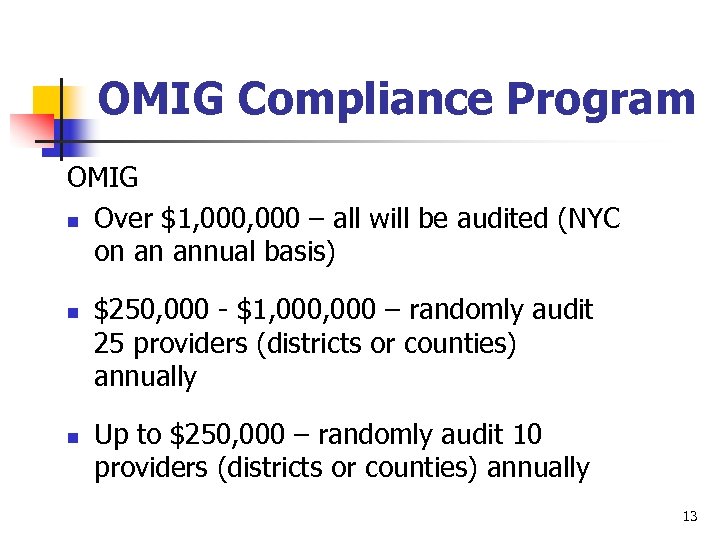 OMIG Compliance Program OMIG n Over $1, 000 – all will be audited (NYC on an annual basis) n n $250, 000 - $1, 000 – randomly audit 25 providers (districts or counties) annually Up to $250, 000 – randomly audit 10 providers (districts or counties) annually 13
OMIG Compliance Program OMIG n Over $1, 000 – all will be audited (NYC on an annual basis) n n $250, 000 - $1, 000 – randomly audit 25 providers (districts or counties) annually Up to $250, 000 – randomly audit 10 providers (districts or counties) annually 13
 Compliance Agreement § OMIG Audits § Independent Audit § Annual Written Reports 14
Compliance Agreement § OMIG Audits § Independent Audit § Annual Written Reports 14
 Compliance Agreement n Training § § § Relevant employee database http: //www. forms 2. nysed. gov/oms/medicaid/shsp. cfm Annual compliance training to relevant employees Training certification for attendees 15
Compliance Agreement n Training § § § Relevant employee database http: //www. forms 2. nysed. gov/oms/medicaid/shsp. cfm Annual compliance training to relevant employees Training certification for attendees 15
 Medicaid State Plan Amendment (09 -61) n n n New York State Plan Amendment (SPA 09 -61) Covered services Documentation requirements Clarify Medicaid billing and program policy Planning ahead 16
Medicaid State Plan Amendment (09 -61) n n n New York State Plan Amendment (SPA 09 -61) Covered services Documentation requirements Clarify Medicaid billing and program policy Planning ahead 16
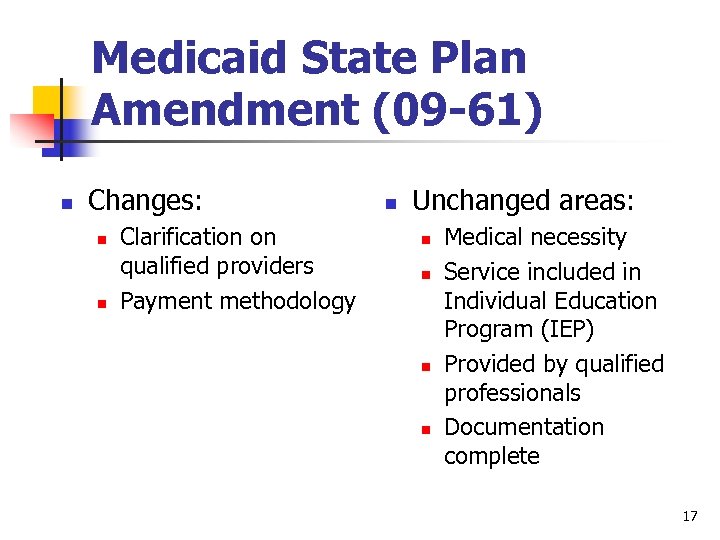 Medicaid State Plan Amendment (09 -61) n Changes: n n Clarification on qualified providers Payment methodology n Unchanged areas: n n Medical necessity Service included in Individual Education Program (IEP) Provided by qualified professionals Documentation complete 17
Medicaid State Plan Amendment (09 -61) n Changes: n n Clarification on qualified providers Payment methodology n Unchanged areas: n n Medical necessity Service included in Individual Education Program (IEP) Provided by qualified professionals Documentation complete 17
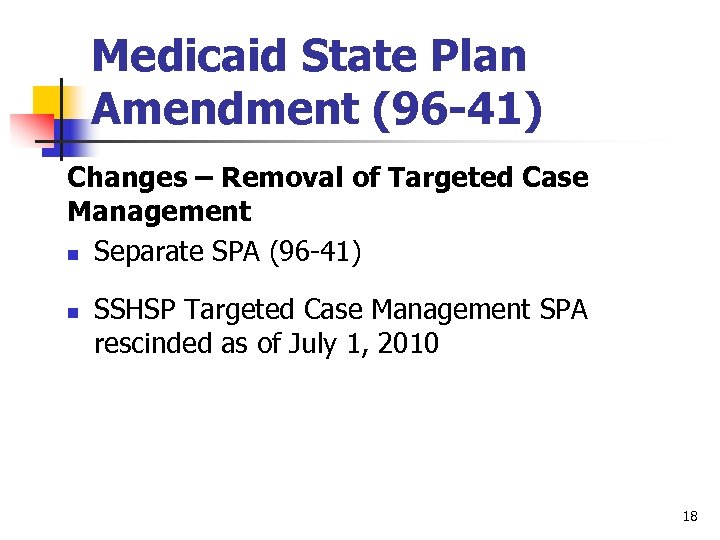 Medicaid State Plan Amendment (96 -41) Changes – Removal of Targeted Case Management n Separate SPA (96 -41) n SSHSP Targeted Case Management SPA rescinded as of July 1, 2010 18
Medicaid State Plan Amendment (96 -41) Changes – Removal of Targeted Case Management n Separate SPA (96 -41) n SSHSP Targeted Case Management SPA rescinded as of July 1, 2010 18
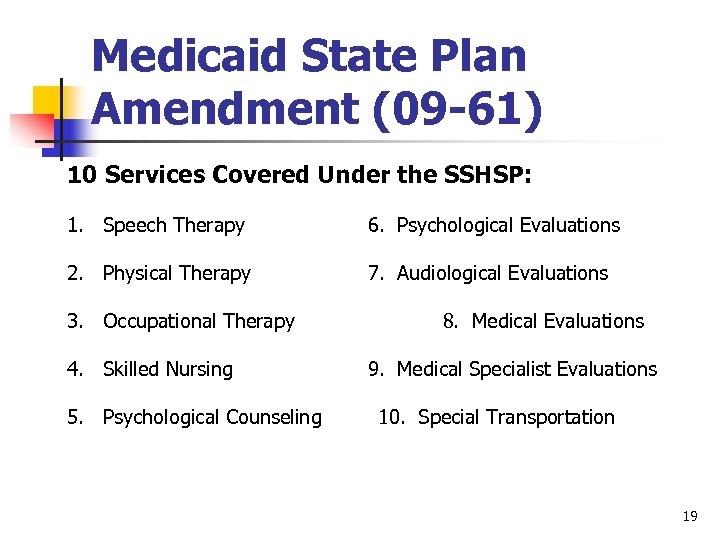 Medicaid State Plan Amendment (09 -61) 10 Services Covered Under the SSHSP: 1. Speech Therapy 6. Psychological Evaluations 2. Physical Therapy 7. Audiological Evaluations 3. Occupational Therapy 4. Skilled Nursing 5. Psychological Counseling 8. Medical Evaluations 9. Medical Specialist Evaluations 10. Special Transportation 19
Medicaid State Plan Amendment (09 -61) 10 Services Covered Under the SSHSP: 1. Speech Therapy 6. Psychological Evaluations 2. Physical Therapy 7. Audiological Evaluations 3. Occupational Therapy 4. Skilled Nursing 5. Psychological Counseling 8. Medical Evaluations 9. Medical Specialist Evaluations 10. Special Transportation 19
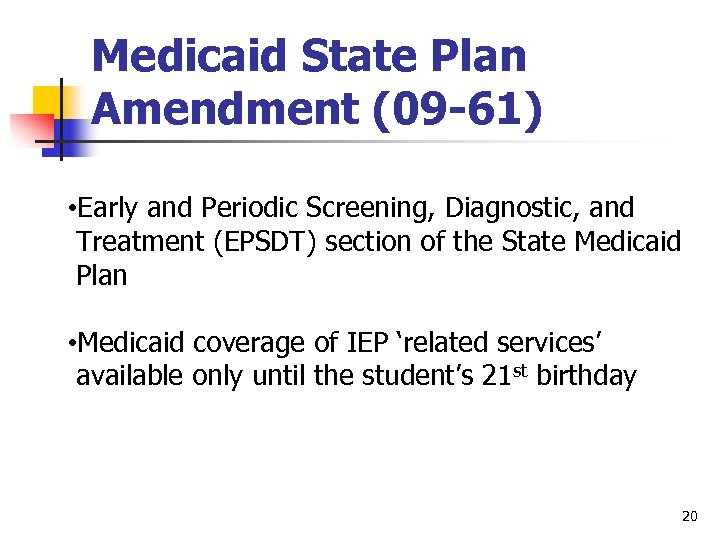 Medicaid State Plan Amendment (09 -61) • Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) section of the State Medicaid Plan • Medicaid coverage of IEP ‘related services’ available only until the student’s 21 st birthday 20
Medicaid State Plan Amendment (09 -61) • Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) section of the State Medicaid Plan • Medicaid coverage of IEP ‘related services’ available only until the student’s 21 st birthday 20
 Medicaid State Plan Amendment (09 -61) Clarifications Related to Service Provision n See handout #1 for specific provider qualifications n Documentation of qualification kept on file (license, certification, or registration) n NYS licensed/registered provider, acting within his/her scope of practice under NYS Law 21
Medicaid State Plan Amendment (09 -61) Clarifications Related to Service Provision n See handout #1 for specific provider qualifications n Documentation of qualification kept on file (license, certification, or registration) n NYS licensed/registered provider, acting within his/her scope of practice under NYS Law 21
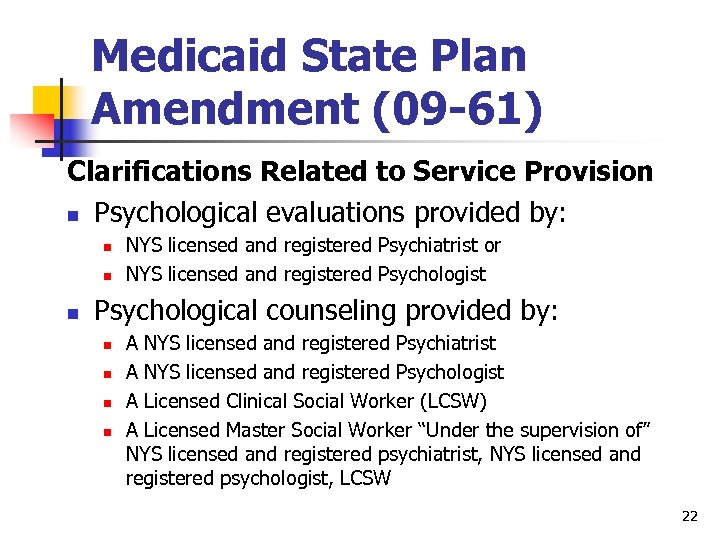 Medicaid State Plan Amendment (09 -61) Clarifications Related to Service Provision n Psychological evaluations provided by: n n n NYS licensed and registered Psychiatrist or NYS licensed and registered Psychologist Psychological counseling provided by: n n A NYS licensed and registered Psychiatrist A NYS licensed and registered Psychologist A Licensed Clinical Social Worker (LCSW) A Licensed Master Social Worker “Under the supervision of” NYS licensed and registered psychiatrist, NYS licensed and registered psychologist, LCSW 22
Medicaid State Plan Amendment (09 -61) Clarifications Related to Service Provision n Psychological evaluations provided by: n n n NYS licensed and registered Psychiatrist or NYS licensed and registered Psychologist Psychological counseling provided by: n n A NYS licensed and registered Psychiatrist A NYS licensed and registered Psychologist A Licensed Clinical Social Worker (LCSW) A Licensed Master Social Worker “Under the supervision of” NYS licensed and registered psychiatrist, NYS licensed and registered psychologist, LCSW 22
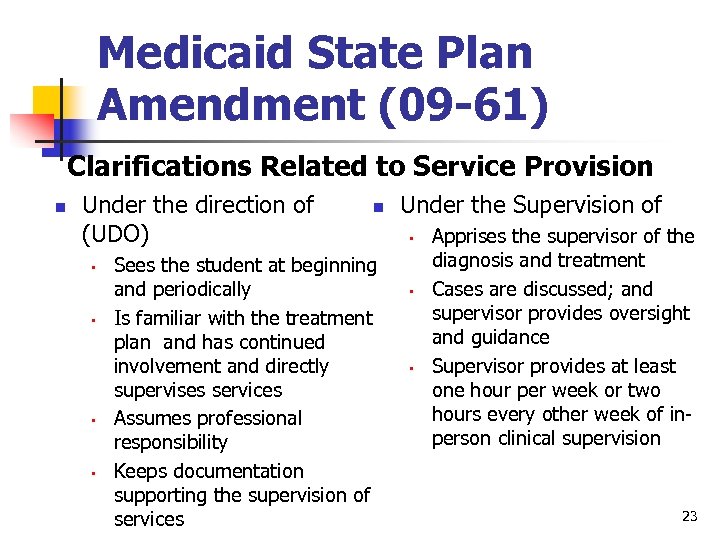 Medicaid State Plan Amendment (09 -61) Clarifications Related to Service Provision n Under the direction of (UDO) • • n Sees the student at beginning and periodically Is familiar with the treatment plan and has continued involvement and directly supervises services Assumes professional responsibility Keeps documentation supporting the supervision of services Under the Supervision of • • • Apprises the supervisor of the diagnosis and treatment Cases are discussed; and supervisor provides oversight and guidance Supervisor provides at least one hour per week or two hours every other week of inperson clinical supervision 23
Medicaid State Plan Amendment (09 -61) Clarifications Related to Service Provision n Under the direction of (UDO) • • n Sees the student at beginning and periodically Is familiar with the treatment plan and has continued involvement and directly supervises services Assumes professional responsibility Keeps documentation supporting the supervision of services Under the Supervision of • • • Apprises the supervisor of the diagnosis and treatment Cases are discussed; and supervisor provides oversight and guidance Supervisor provides at least one hour per week or two hours every other week of inperson clinical supervision 23
 “Under the Direction of” (UDO) & “Under the Supervision of” n n See handout #2 UDO Applies to: n n Teacher of the Speech and Hearing Handicapped (TSHH) Physical Therapy Assistant (PTA) Occupational Therapy Assistant (OTA) Under the Supervision of applies only to Licensed Master Social Worker 24
“Under the Direction of” (UDO) & “Under the Supervision of” n n See handout #2 UDO Applies to: n n Teacher of the Speech and Hearing Handicapped (TSHH) Physical Therapy Assistant (PTA) Occupational Therapy Assistant (OTA) Under the Supervision of applies only to Licensed Master Social Worker 24
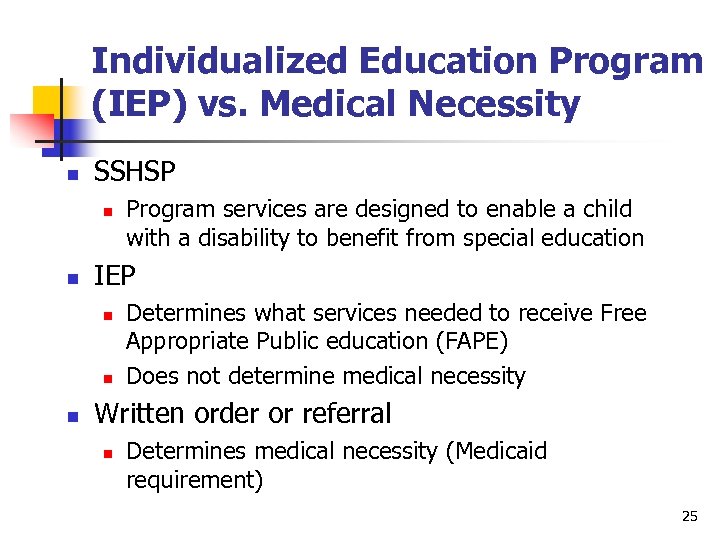 Individualized Education Program (IEP) vs. Medical Necessity n SSHSP n n IEP n n n Program services are designed to enable a child with a disability to benefit from special education Determines what services needed to receive Free Appropriate Public education (FAPE) Does not determine medical necessity Written order or referral n Determines medical necessity (Medicaid requirement) 25
Individualized Education Program (IEP) vs. Medical Necessity n SSHSP n n IEP n n n Program services are designed to enable a child with a disability to benefit from special education Determines what services needed to receive Free Appropriate Public education (FAPE) Does not determine medical necessity Written order or referral n Determines medical necessity (Medicaid requirement) 25
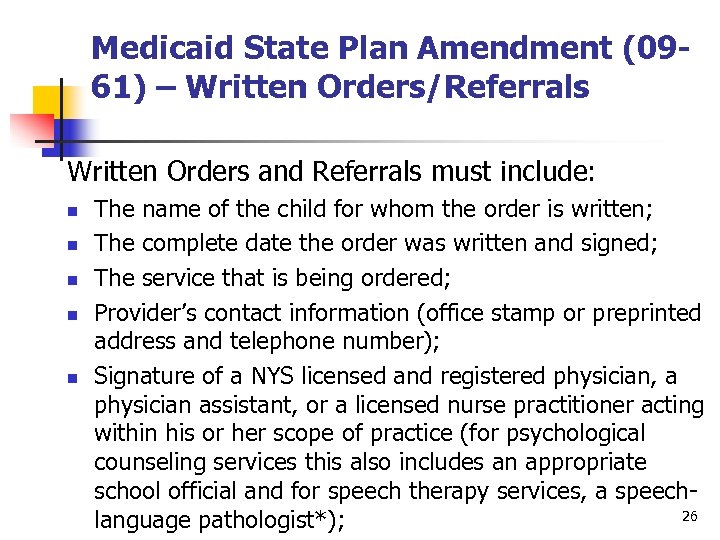 Medicaid State Plan Amendment (0961) – Written Orders/Referrals Written Orders and Referrals must include: n n n The name of the child for whom the order is written; The complete date the order was written and signed; The service that is being ordered; Provider’s contact information (office stamp or preprinted address and telephone number); Signature of a NYS licensed and registered physician, a physician assistant, or a licensed nurse practitioner acting within his or her scope of practice (for psychological counseling services this also includes an appropriate school official and for speech therapy services, a speech 26 language pathologist*);
Medicaid State Plan Amendment (0961) – Written Orders/Referrals Written Orders and Referrals must include: n n n The name of the child for whom the order is written; The complete date the order was written and signed; The service that is being ordered; Provider’s contact information (office stamp or preprinted address and telephone number); Signature of a NYS licensed and registered physician, a physician assistant, or a licensed nurse practitioner acting within his or her scope of practice (for psychological counseling services this also includes an appropriate school official and for speech therapy services, a speech 26 language pathologist*);
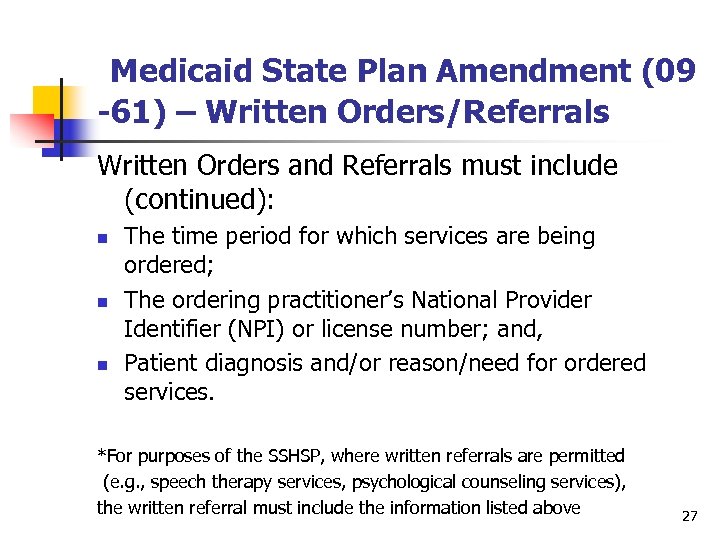 Medicaid State Plan Amendment (09 -61) – Written Orders/Referrals Written Orders and Referrals must include (continued): n n n The time period for which services are being ordered; The ordering practitioner’s National Provider Identifier (NPI) or license number; and, Patient diagnosis and/or reason/need for ordered services. *For purposes of the SSHSP, where written referrals are permitted (e. g. , speech therapy services, psychological counseling services), the written referral must include the information listed above 27
Medicaid State Plan Amendment (09 -61) – Written Orders/Referrals Written Orders and Referrals must include (continued): n n n The time period for which services are being ordered; The ordering practitioner’s National Provider Identifier (NPI) or license number; and, Patient diagnosis and/or reason/need for ordered services. *For purposes of the SSHSP, where written referrals are permitted (e. g. , speech therapy services, psychological counseling services), the written referral must include the information listed above 27
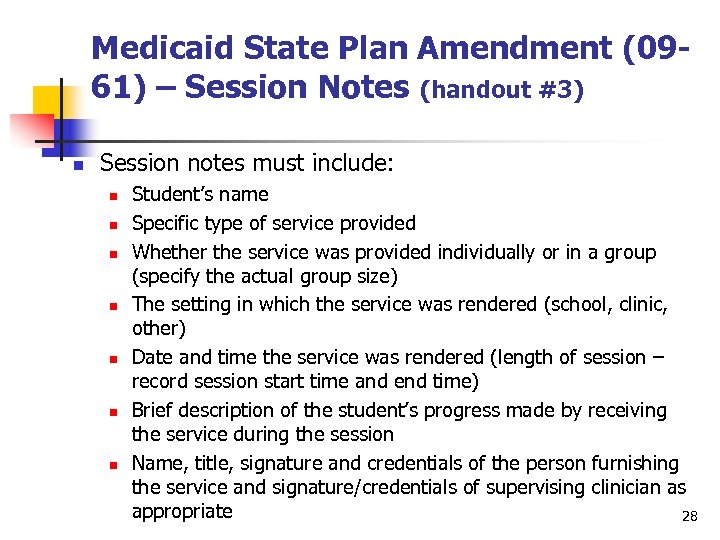 Medicaid State Plan Amendment (0961) – Session Notes (handout #3) n Session notes must include: n n n n Student’s name Specific type of service provided Whether the service was provided individually or in a group (specify the actual group size) The setting in which the service was rendered (school, clinic, other) Date and time the service was rendered (length of session – record session start time and end time) Brief description of the student’s progress made by receiving the service during the session Name, title, signature and credentials of the person furnishing the service and signature/credentials of supervising clinician as appropriate 28
Medicaid State Plan Amendment (0961) – Session Notes (handout #3) n Session notes must include: n n n n Student’s name Specific type of service provided Whether the service was provided individually or in a group (specify the actual group size) The setting in which the service was rendered (school, clinic, other) Date and time the service was rendered (length of session – record session start time and end time) Brief description of the student’s progress made by receiving the service during the session Name, title, signature and credentials of the person furnishing the service and signature/credentials of supervising clinician as appropriate 28
 Medicaid State Plan Amendment (0961) – Session Notes n Other Documentation Requirements may exist under other programs – for example: n IDEA-required quarterly progress notes n IDEA-required parental consent 29
Medicaid State Plan Amendment (0961) – Session Notes n Other Documentation Requirements may exist under other programs – for example: n IDEA-required quarterly progress notes n IDEA-required parental consent 29
 Medicaid State Plan Amendment (09 -61) Evaluations n See flow chart handout #4 n Student suspected of having a disability n Referred to CSE/CPSE n Evaluation process initiated (written order/referral on file) n Student not found to have a disability n n No IEP is developed and evaluation can not be reimbursed by Medicaid Student found to have a disability n Evaluation must be listed on IEP in order to be reimbursed by Medicaid 30
Medicaid State Plan Amendment (09 -61) Evaluations n See flow chart handout #4 n Student suspected of having a disability n Referred to CSE/CPSE n Evaluation process initiated (written order/referral on file) n Student not found to have a disability n n No IEP is developed and evaluation can not be reimbursed by Medicaid Student found to have a disability n Evaluation must be listed on IEP in order to be reimbursed by Medicaid 30
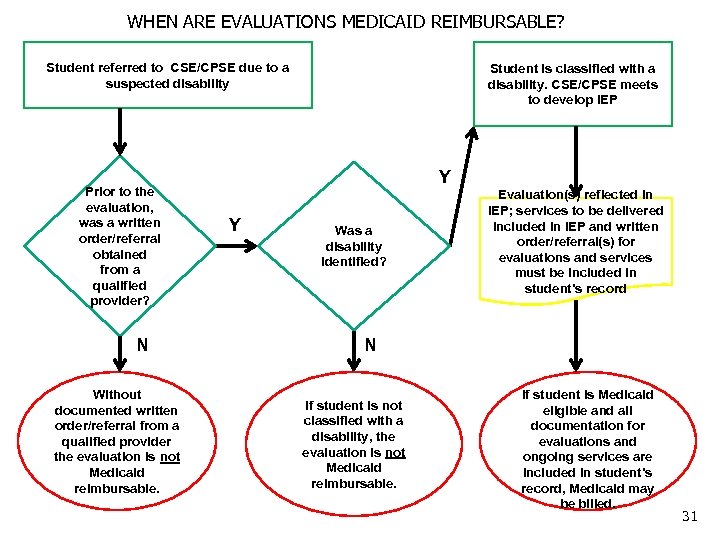 WHEN ARE EVALUATIONS MEDICAID REIMBURSABLE? Student referred to CSE/CPSE due to a suspected disability N Without documented written order/referral from a qualified provider the evaluation is not Medicaid reimbursable. Y Y Was a disability identified? Evaluation(s) reflected in IEP; services to be delivered included in IEP and written order/referral(s) for evaluations and services must be included in student’s record N Prior to the evaluation, was a written order/referral obtained from a qualified provider? Student is classified with a disability. CSE/CPSE meets to develop IEP If student is not classified with a disability, the evaluation is not Medicaid reimbursable. If student is Medicaid eligible and all documentation for evaluations and ongoing services are included in student’s record, Medicaid may be billed. 31
WHEN ARE EVALUATIONS MEDICAID REIMBURSABLE? Student referred to CSE/CPSE due to a suspected disability N Without documented written order/referral from a qualified provider the evaluation is not Medicaid reimbursable. Y Y Was a disability identified? Evaluation(s) reflected in IEP; services to be delivered included in IEP and written order/referral(s) for evaluations and services must be included in student’s record N Prior to the evaluation, was a written order/referral obtained from a qualified provider? Student is classified with a disability. CSE/CPSE meets to develop IEP If student is not classified with a disability, the evaluation is not Medicaid reimbursable. If student is Medicaid eligible and all documentation for evaluations and ongoing services are included in student’s record, Medicaid may be billed. 31
 Medicaid State Plan Amendment (09 -61) Evaluations n Must be reflected in the IEP n n Assist with determination of medical necessity (critical for billing Medicaid) Service provided by appropriate qualified provider 32
Medicaid State Plan Amendment (09 -61) Evaluations n Must be reflected in the IEP n n Assist with determination of medical necessity (critical for billing Medicaid) Service provided by appropriate qualified provider 32
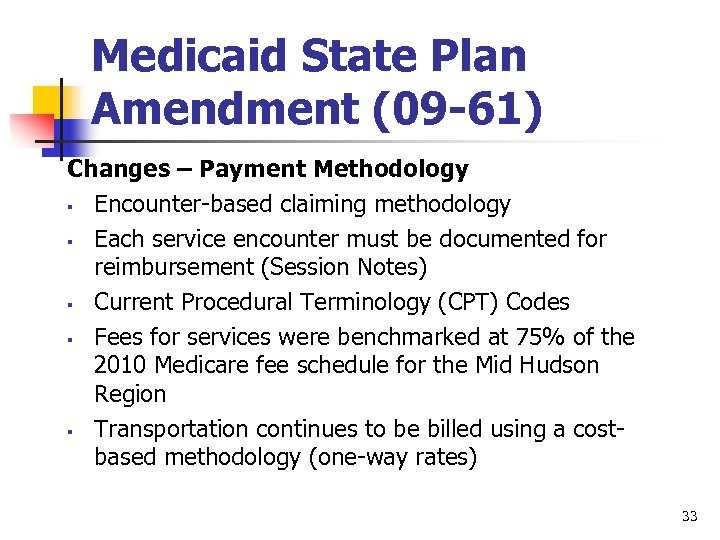 Medicaid State Plan Amendment (09 -61) Changes – Payment Methodology § Encounter-based claiming methodology § Each service encounter must be documented for reimbursement (Session Notes) § Current Procedural Terminology (CPT) Codes § Fees for services were benchmarked at 75% of the 2010 Medicare fee schedule for the Mid Hudson Region § Transportation continues to be billed using a costbased methodology (one-way rates) 33
Medicaid State Plan Amendment (09 -61) Changes – Payment Methodology § Encounter-based claiming methodology § Each service encounter must be documented for reimbursement (Session Notes) § Current Procedural Terminology (CPT) Codes § Fees for services were benchmarked at 75% of the 2010 Medicare fee schedule for the Mid Hudson Region § Transportation continues to be billed using a costbased methodology (one-way rates) 33
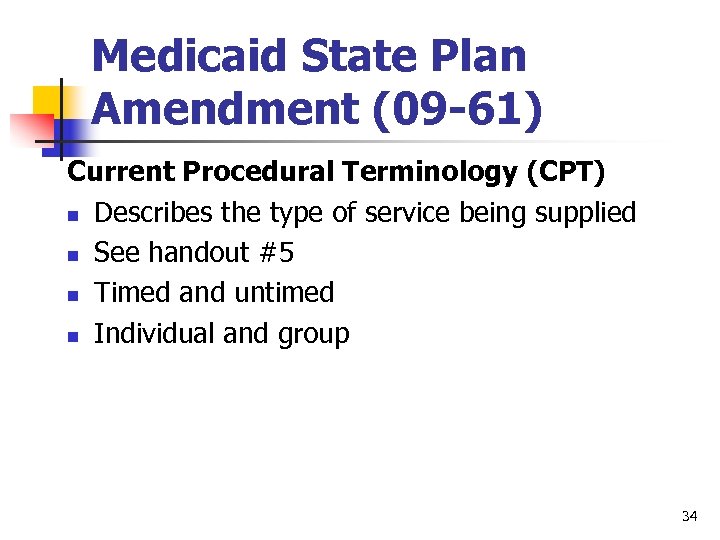 Medicaid State Plan Amendment (09 -61) Current Procedural Terminology (CPT) n Describes the type of service being supplied n See handout #5 n Timed and untimed n Individual and group 34
Medicaid State Plan Amendment (09 -61) Current Procedural Terminology (CPT) n Describes the type of service being supplied n See handout #5 n Timed and untimed n Individual and group 34
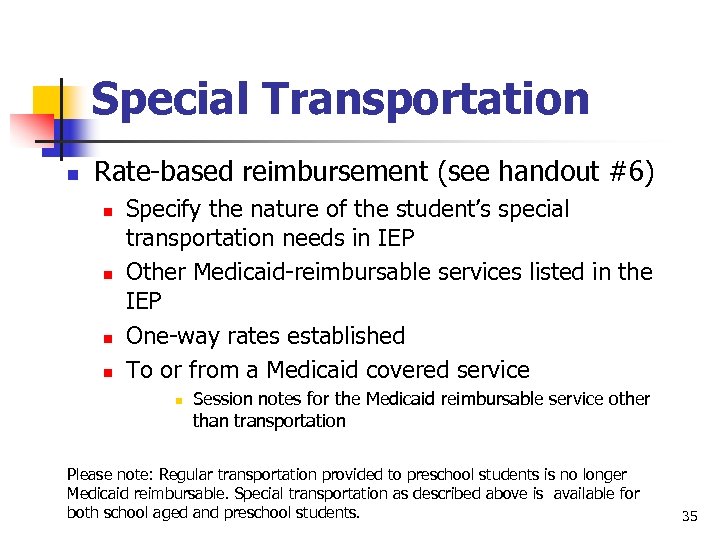 Special Transportation n Rate-based reimbursement (see handout #6) n n Specify the nature of the student’s special transportation needs in IEP Other Medicaid-reimbursable services listed in the IEP One-way rates established To or from a Medicaid covered service n Session notes for the Medicaid reimbursable service other than transportation Please note: Regular transportation provided to preschool students is no longer Medicaid reimbursable. Special transportation as described above is available for both school aged and preschool students. 35
Special Transportation n Rate-based reimbursement (see handout #6) n n Specify the nature of the student’s special transportation needs in IEP Other Medicaid-reimbursable services listed in the IEP One-way rates established To or from a Medicaid covered service n Session notes for the Medicaid reimbursable service other than transportation Please note: Regular transportation provided to preschool students is no longer Medicaid reimbursable. Special transportation as described above is available for both school aged and preschool students. 35
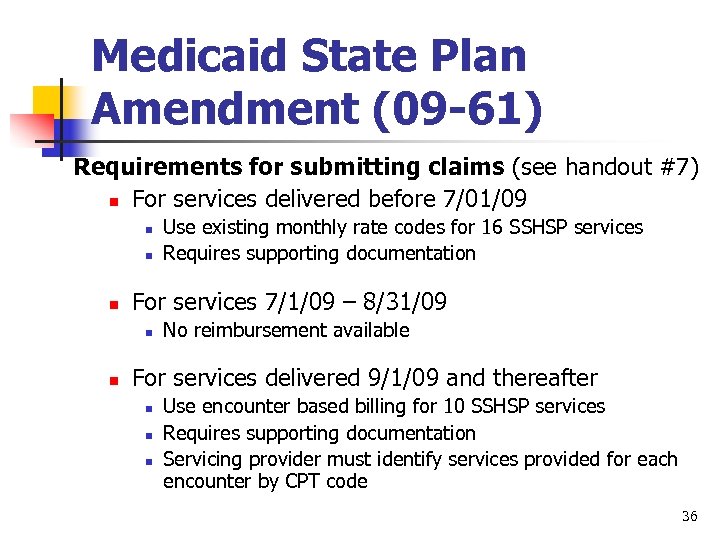 Medicaid State Plan Amendment (09 -61) Requirements for submitting claims (see handout #7) n For services delivered before 7/01/09 n n n For services 7/1/09 – 8/31/09 n n Use existing monthly rate codes for 16 SSHSP services Requires supporting documentation No reimbursement available For services delivered 9/1/09 and thereafter n n n Use encounter based billing for 10 SSHSP services Requires supporting documentation Servicing provider must identify services provided for each encounter by CPT code 36
Medicaid State Plan Amendment (09 -61) Requirements for submitting claims (see handout #7) n For services delivered before 7/01/09 n n n For services 7/1/09 – 8/31/09 n n Use existing monthly rate codes for 16 SSHSP services Requires supporting documentation No reimbursement available For services delivered 9/1/09 and thereafter n n n Use encounter based billing for 10 SSHSP services Requires supporting documentation Servicing provider must identify services provided for each encounter by CPT code 36
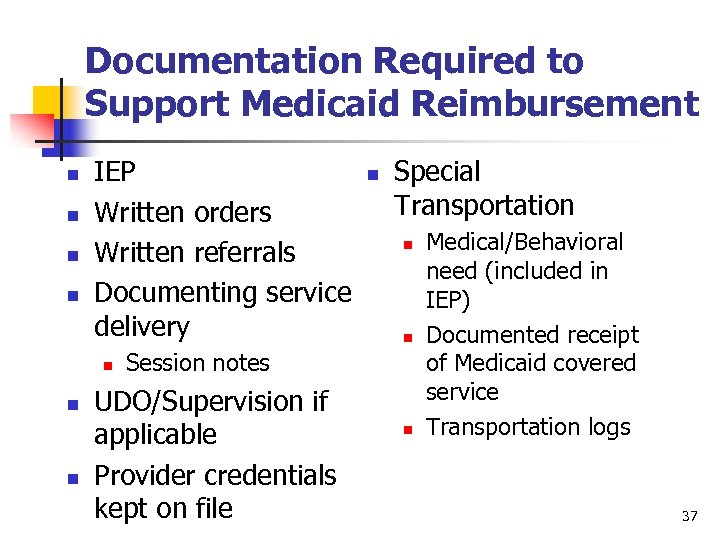 Documentation Required to Support Medicaid Reimbursement n n IEP Written orders Written referrals Documenting service delivery n n Special Transportation n n Session notes UDO/Supervision if applicable Provider credentials kept on file n Medical/Behavioral need (included in IEP) Documented receipt of Medicaid covered service Transportation logs 37
Documentation Required to Support Medicaid Reimbursement n n IEP Written orders Written referrals Documenting service delivery n n Special Transportation n n Session notes UDO/Supervision if applicable Provider credentials kept on file n Medical/Behavioral need (included in IEP) Documented receipt of Medicaid covered service Transportation logs 37
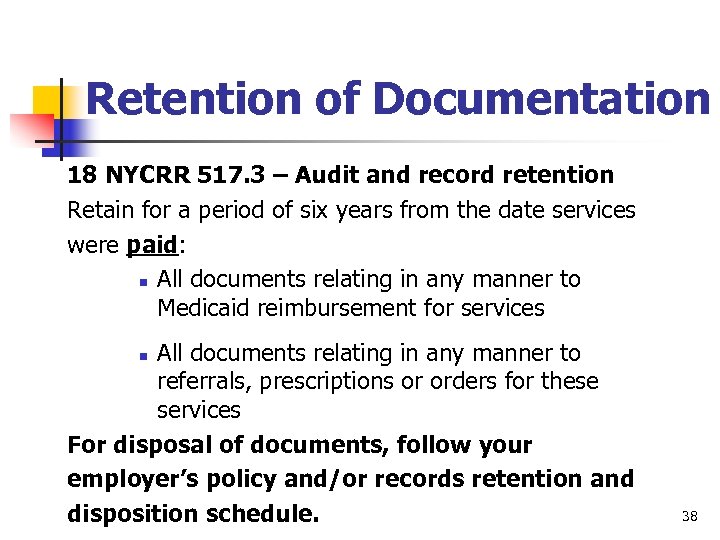 Retention of Documentation 18 NYCRR 517. 3 – Audit and record retention Retain for a period of six years from the date services were paid: n All documents relating in any manner to Medicaid reimbursement for services All documents relating in any manner to referrals, prescriptions or orders for these services For disposal of documents, follow your employer’s policy and/or records retention and disposition schedule. n 38
Retention of Documentation 18 NYCRR 517. 3 – Audit and record retention Retain for a period of six years from the date services were paid: n All documents relating in any manner to Medicaid reimbursement for services All documents relating in any manner to referrals, prescriptions or orders for these services For disposal of documents, follow your employer’s policy and/or records retention and disposition schedule. n 38
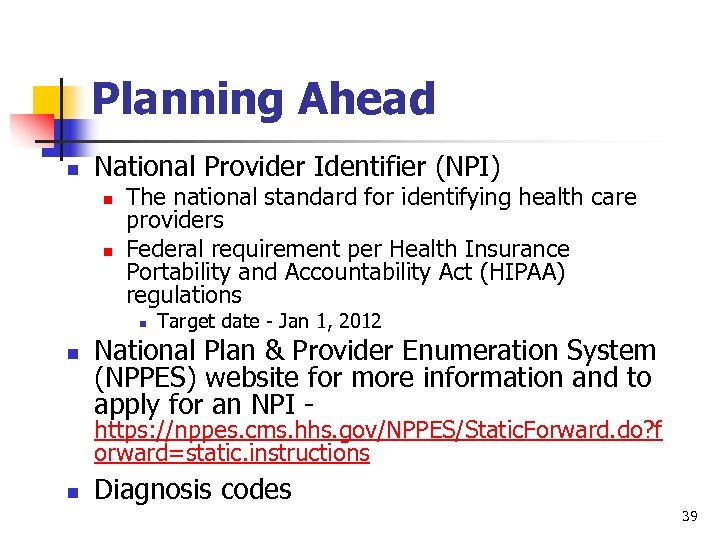 Planning Ahead n National Provider Identifier (NPI) n n The national standard for identifying health care providers Federal requirement per Health Insurance Portability and Accountability Act (HIPAA) regulations n n Target date - Jan 1, 2012 National Plan & Provider Enumeration System (NPPES) website for more information and to apply for an NPI - https: //nppes. cms. hhs. gov/NPPES/Static. Forward. do? f orward=static. instructions n Diagnosis codes 39
Planning Ahead n National Provider Identifier (NPI) n n The national standard for identifying health care providers Federal requirement per Health Insurance Portability and Accountability Act (HIPAA) regulations n n Target date - Jan 1, 2012 National Plan & Provider Enumeration System (NPPES) website for more information and to apply for an NPI - https: //nppes. cms. hhs. gov/NPPES/Static. Forward. do? f orward=static. instructions n Diagnosis codes 39
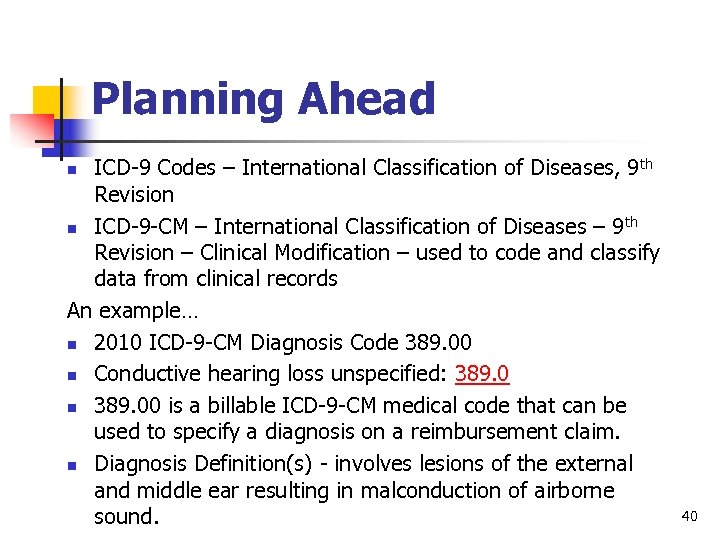 Planning Ahead ICD-9 Codes – International Classification of Diseases, 9 th Revision n ICD-9 -CM – International Classification of Diseases – 9 th Revision – Clinical Modification – used to code and classify data from clinical records An example… n 2010 ICD-9 -CM Diagnosis Code 389. 00 n Conductive hearing loss unspecified: 389. 0 n 389. 00 is a billable ICD-9 -CM medical code that can be used to specify a diagnosis on a reimbursement claim. n Diagnosis Definition(s) - involves lesions of the external and middle ear resulting in malconduction of airborne sound. n 40
Planning Ahead ICD-9 Codes – International Classification of Diseases, 9 th Revision n ICD-9 -CM – International Classification of Diseases – 9 th Revision – Clinical Modification – used to code and classify data from clinical records An example… n 2010 ICD-9 -CM Diagnosis Code 389. 00 n Conductive hearing loss unspecified: 389. 0 n 389. 00 is a billable ICD-9 -CM medical code that can be used to specify a diagnosis on a reimbursement claim. n Diagnosis Definition(s) - involves lesions of the external and middle ear resulting in malconduction of airborne sound. n 40
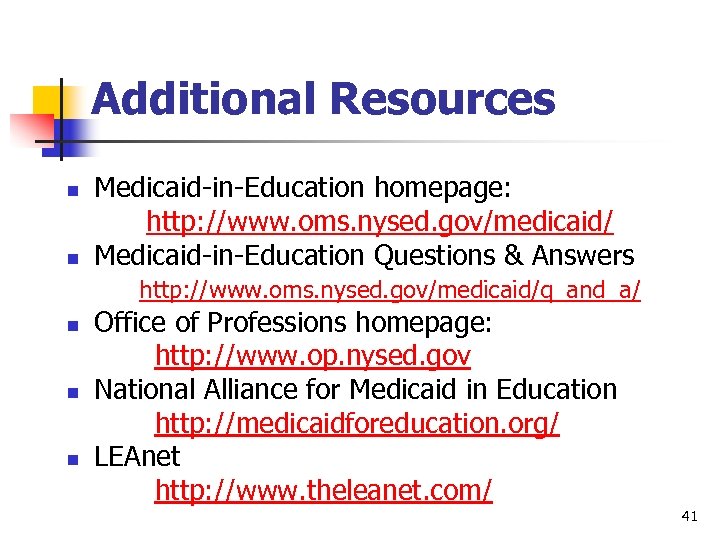 Additional Resources n n Medicaid-in-Education homepage: http: //www. oms. nysed. gov/medicaid/ Medicaid-in-Education Questions & Answers http: //www. oms. nysed. gov/medicaid/q_and_a/ n n n Office of Professions homepage: http: //www. op. nysed. gov National Alliance for Medicaid in Education http: //medicaidforeducation. org/ LEAnet http: //www. theleanet. com/ 41
Additional Resources n n Medicaid-in-Education homepage: http: //www. oms. nysed. gov/medicaid/ Medicaid-in-Education Questions & Answers http: //www. oms. nysed. gov/medicaid/q_and_a/ n n n Office of Professions homepage: http: //www. op. nysed. gov National Alliance for Medicaid in Education http: //medicaidforeducation. org/ LEAnet http: //www. theleanet. com/ 41
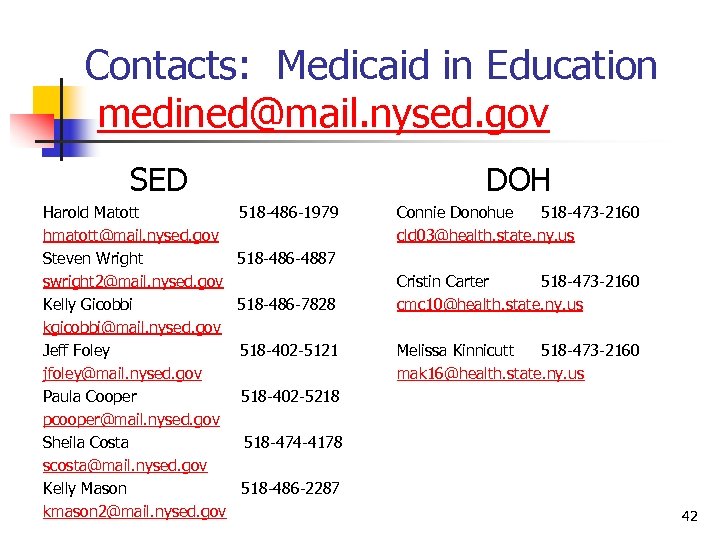 Contacts: Medicaid in Education medined@mail. nysed. gov SED Harold Matott hmatott@mail. nysed. gov Steven Wright swright 2@mail. nysed. gov Kelly Gicobbi kgicobbi@mail. nysed. gov Jeff Foley jfoley@mail. nysed. gov Paula Cooper pcooper@mail. nysed. gov Sheila Costa scosta@mail. nysed. gov Kelly Mason kmason 2@mail. nysed. gov DOH 518 -486 -1979 Connie Donohue 518 -473 -2160 cld 03@health. state. ny. us 518 -486 -4887 518 -486 -7828 518 -402 -5121 Cristin Carter 518 -473 -2160 cmc 10@health. state. ny. us Melissa Kinnicutt 518 -473 -2160 mak 16@health. state. ny. us 518 -402 -5218 518 -474 -4178 518 -486 -2287 42
Contacts: Medicaid in Education medined@mail. nysed. gov SED Harold Matott hmatott@mail. nysed. gov Steven Wright swright 2@mail. nysed. gov Kelly Gicobbi kgicobbi@mail. nysed. gov Jeff Foley jfoley@mail. nysed. gov Paula Cooper pcooper@mail. nysed. gov Sheila Costa scosta@mail. nysed. gov Kelly Mason kmason 2@mail. nysed. gov DOH 518 -486 -1979 Connie Donohue 518 -473 -2160 cld 03@health. state. ny. us 518 -486 -4887 518 -486 -7828 518 -402 -5121 Cristin Carter 518 -473 -2160 cmc 10@health. state. ny. us Melissa Kinnicutt 518 -473 -2160 mak 16@health. state. ny. us 518 -402 -5218 518 -474 -4178 518 -486 -2287 42
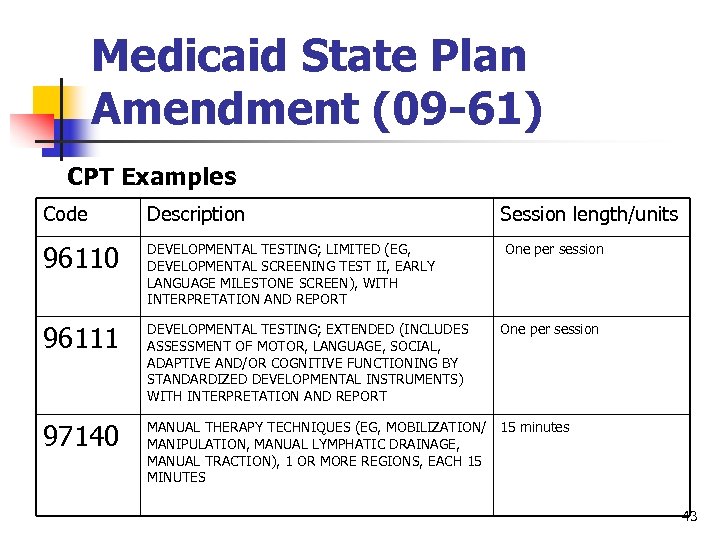 Medicaid State Plan Amendment (09 -61) CPT Examples Code Description Session length/units 96110 DEVELOPMENTAL TESTING; LIMITED (EG, DEVELOPMENTAL SCREENING TEST II, EARLY LANGUAGE MILESTONE SCREEN), WITH INTERPRETATION AND REPORT 96111 DEVELOPMENTAL TESTING; EXTENDED (INCLUDES ASSESSMENT OF MOTOR, LANGUAGE, SOCIAL, ADAPTIVE AND/OR COGNITIVE FUNCTIONING BY STANDARDIZED DEVELOPMENTAL INSTRUMENTS) WITH INTERPRETATION AND REPORT 97140 MANUAL THERAPY TECHNIQUES (EG, MOBILIZATION/ 15 minutes MANIPULATION, MANUAL LYMPHATIC DRAINAGE, MANUAL TRACTION), 1 OR MORE REGIONS, EACH 15 MINUTES One per session 43
Medicaid State Plan Amendment (09 -61) CPT Examples Code Description Session length/units 96110 DEVELOPMENTAL TESTING; LIMITED (EG, DEVELOPMENTAL SCREENING TEST II, EARLY LANGUAGE MILESTONE SCREEN), WITH INTERPRETATION AND REPORT 96111 DEVELOPMENTAL TESTING; EXTENDED (INCLUDES ASSESSMENT OF MOTOR, LANGUAGE, SOCIAL, ADAPTIVE AND/OR COGNITIVE FUNCTIONING BY STANDARDIZED DEVELOPMENTAL INSTRUMENTS) WITH INTERPRETATION AND REPORT 97140 MANUAL THERAPY TECHNIQUES (EG, MOBILIZATION/ 15 minutes MANIPULATION, MANUAL LYMPHATIC DRAINAGE, MANUAL TRACTION), 1 OR MORE REGIONS, EACH 15 MINUTES One per session 43
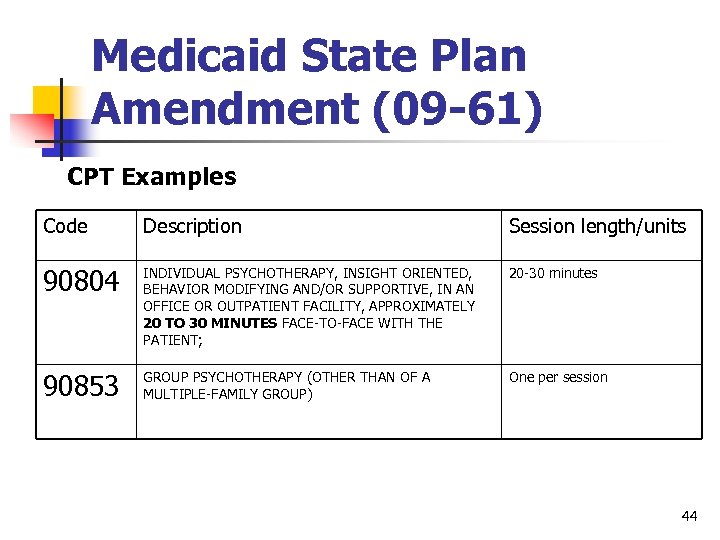 Medicaid State Plan Amendment (09 -61) CPT Examples Code Description Session length/units 90804 INDIVIDUAL PSYCHOTHERAPY, INSIGHT ORIENTED, BEHAVIOR MODIFYING AND/OR SUPPORTIVE, IN AN OFFICE OR OUTPATIENT FACILITY, APPROXIMATELY 20 TO 30 MINUTES FACE-TO-FACE WITH THE PATIENT; 20 -30 minutes 90853 GROUP PSYCHOTHERAPY (OTHER THAN OF A MULTIPLE-FAMILY GROUP) One per session 44
Medicaid State Plan Amendment (09 -61) CPT Examples Code Description Session length/units 90804 INDIVIDUAL PSYCHOTHERAPY, INSIGHT ORIENTED, BEHAVIOR MODIFYING AND/OR SUPPORTIVE, IN AN OFFICE OR OUTPATIENT FACILITY, APPROXIMATELY 20 TO 30 MINUTES FACE-TO-FACE WITH THE PATIENT; 20 -30 minutes 90853 GROUP PSYCHOTHERAPY (OTHER THAN OF A MULTIPLE-FAMILY GROUP) One per session 44


