5534ddc352eef75eca61e5ae04949127.ppt
- Количество слайдов: 37
Preparing for the Predictable Planning for common threats to comfort in the final days. Tamara Wells RN MN CNS Dr. M. Harlos Medical Director WRHA Palliative Care Program
Disclosures • No conflicts of interest • Many thanks to all the members of my team and others for their insights and help with this presentation.
Objectives • To review some of the common predictable symptom scenarios at end of life • To review both pharmacologic and nonpharmacologic symptom management strategies • To discuss how end of life care is a team effort
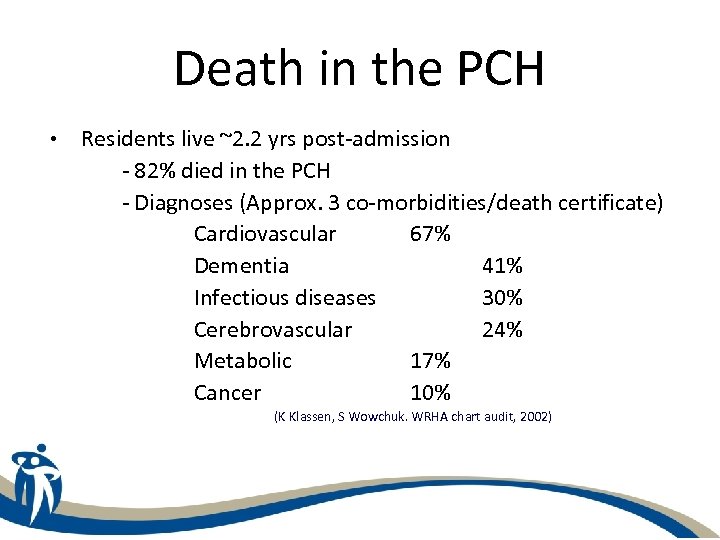
Death in the PCH • Residents live ~2. 2 yrs post-admission - 82% died in the PCH - Diagnoses (Approx. 3 co-morbidities/death certificate) Cardiovascular 67% Dementia 41% Infectious diseases 30% Cerebrovascular 24% Metabolic 17% Cancer 10% (K Klassen, S Wowchuk. WRHA chart audit, 2002)
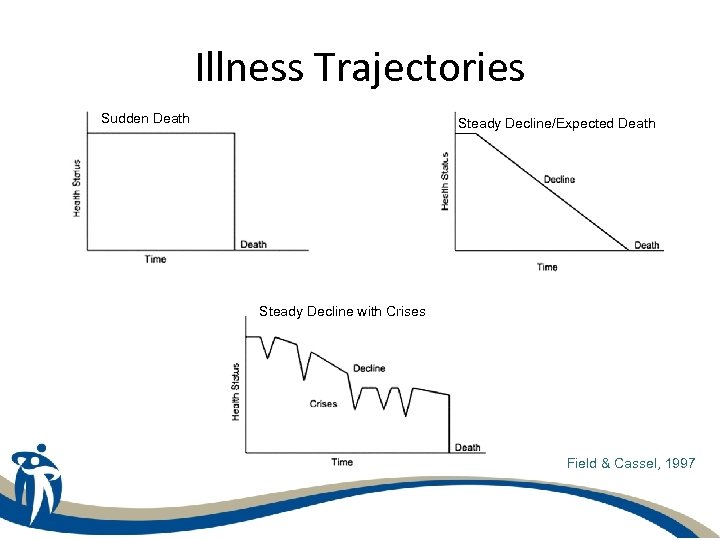
Illness Trajectories Sudden Death Steady Decline/Expected Death Steady Decline with Crises Field & Cassel, 1997
Common Signs • Functional decline • transfers, toileting, eating • • Difficulty swallowing medications Fatigue and decreased activity tolerance Increased presentation of symptoms Concerns of family and friends
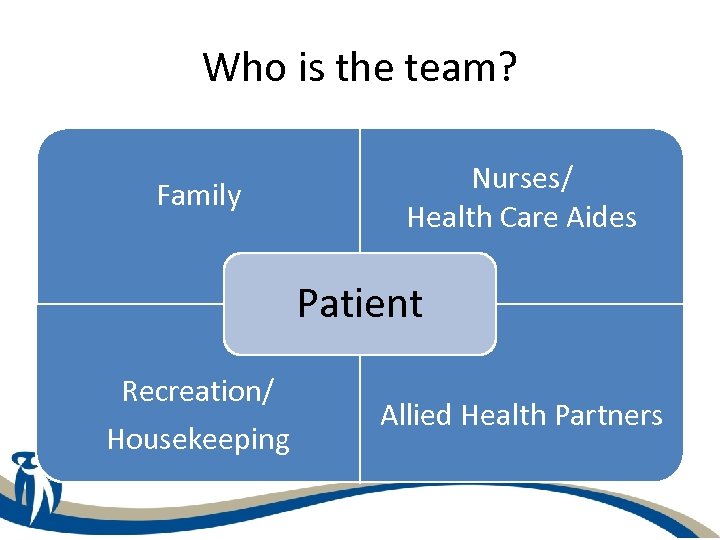
Who is the team? Family Nurses/ Health Care Aides Patient Recreation/ Housekeeping Allied Health Partners
Common Symptoms 1. 2. 3. 4. 5. 6. 7. Shortness of Breath Confusion/Delirium Pain Loss of Appetite & Dehydration Constipation Nausea & Vomiting Secretions
LTC End of Life Pathways
Dyspnea - Assessment Resident describes air hunger/breathlessness Or Resident unable to describe dyspnea but exhibits evidence of respiratory distress: • Increased work of breathing • Increased respiratory rate • Using accessory muscles • Agitated, restless, fearfulness
Non-Pharmacological Management • • Position sitting upright Cool air (fan or open window) Oxygen for alert resident (& hypoxic) Pace or minimize activity Light bed covers, loose clothing Good mouth care Quiet music, calm presence, distraction
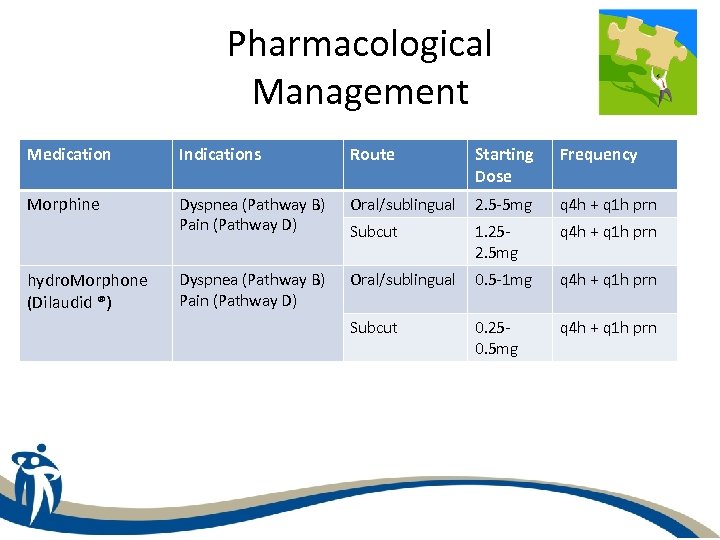
Pharmacological Management Medication Indications Route Starting Dose Frequency Morphine Dyspnea (Pathway B) Pain (Pathway D) Oral/sublingual 2. 5 -5 mg q 4 h + q 1 h prn Subcut 1. 252. 5 mg q 4 h + q 1 h prn Dyspnea (Pathway B) Pain (Pathway D) Oral/sublingual 0. 5 -1 mg q 4 h + q 1 h prn Subcut 0. 250. 5 mg q 4 h + q 1 h prn hydro. Morphone (Dilaudid ®)
Delirium - Assessment • Acute onset of global cognitive impairment related to general medical condition with: • • Fluctuating consciousness Disorientation Disrupted sleep-wake cycle Reduced attention Perceptual disturbances Disorganized thinking Paranoid ideation
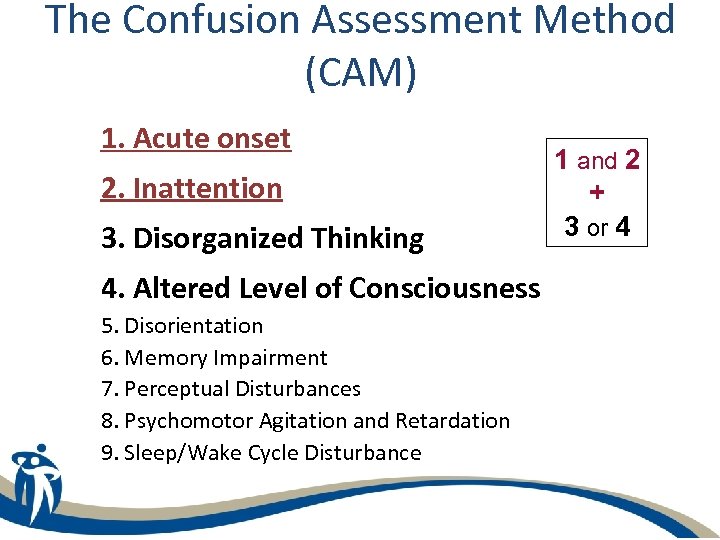
The Confusion Assessment Method (CAM) 1. Acute onset 2. Inattention 3. Disorganized Thinking 4. Altered Level of Consciousness 5. Disorientation 6. Memory Impairment 7. Perceptual Disturbances 8. Psychomotor Agitation and Retardation 9. Sleep/Wake Cycle Disturbance 1 and 2 + 3 or 4
Delirium - Assessment • If clinically appropriate & consistent with goals of care- assess & treat potentially reversible causes of delirium such as: • • • Infections Adverse medication effects Metabolic abnormalities Pain Urinary retention Hypoxia
Management Is the resident agitated, restless or demonstrating responsive behaviours? NO Hypoactive Delirium • Sedation not indicated • Provide general comfort measures • Support family
Management Is the resident agitated, restless or demonstrating responsive behaviours? YES=Hyperactive Delirium • • • Non-pharmacological Keep a calm and reassuring presence Decrease environmental stimuli Pace or modify activity Monitor other factors that can impact comfort (constipation, urinary retention) Communicate with the team and family Encourage sips of fluid
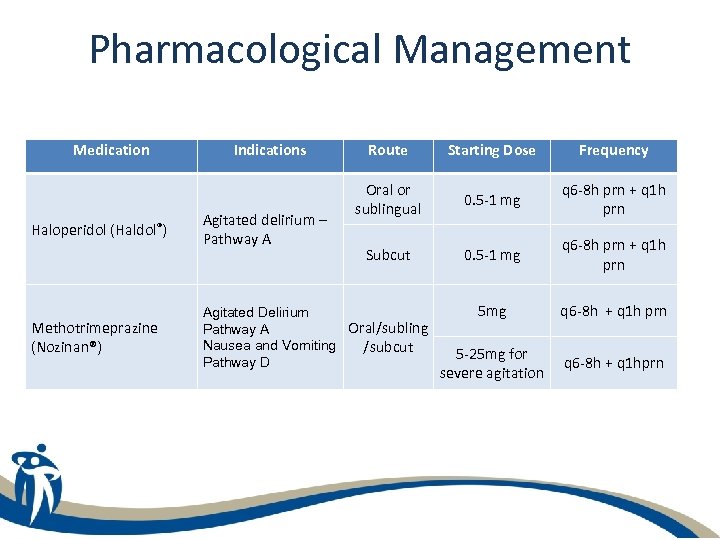
Pharmacological Management Medication Haloperidol (Haldol®) Methotrimeprazine (Nozinan®) Indications Agitated delirium – Pathway A Route Starting Dose Frequency Oral or sublingual 0. 5 -1 mg q 6 -8 h prn + q 1 h prn Subcut 0. 5 -1 mg q 6 -8 h prn + q 1 h prn 5 mg q 6 -8 h + q 1 h prn 5 -25 mg for severe agitation q 6 -8 h + q 1 hprn Agitated Delirium Oral/subling Pathway A Nausea and Vomiting /subcut Pathway D
Delirium Monitoring • Reassess every 24 hours or sooner depending upon response • Consider increasing dosages dependent upon starting dose • Consider stopping Haldol and moving to methotrimeprazine if delirium non-responsive to initial therapies
Noisy Secretions Non-pharmacologic treatment • Noisy secretions present AND distressing to resident and/or family • 1 st: Try repositioning. “Best side” • Oral suction? Only if visible oral or posterior pharyngeal secretions • No deep suctioning
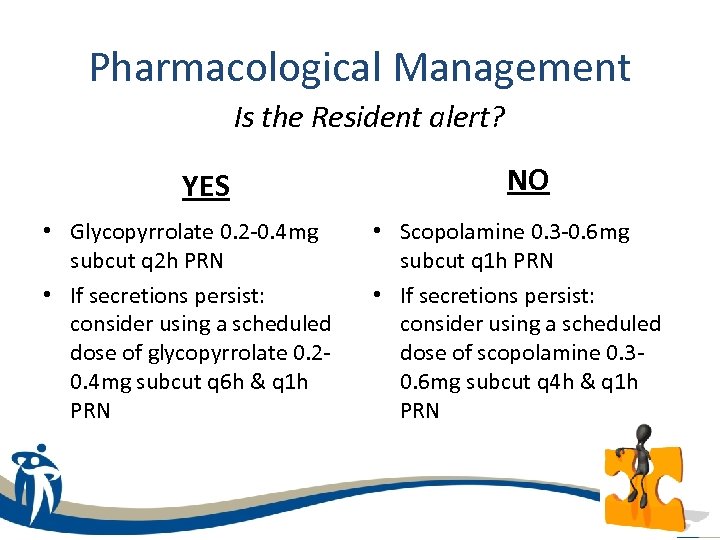
Pharmacological Management Is the Resident alert? YES • Glycopyrrolate 0. 2 -0. 4 mg subcut q 2 h PRN • If secretions persist: consider using a scheduled dose of glycopyrrolate 0. 20. 4 mg subcut q 6 h & q 1 h PRN NO • Scopolamine 0. 3 -0. 6 mg subcut q 1 h PRN • If secretions persist: consider using a scheduled dose of scopolamine 0. 30. 6 mg subcut q 4 h & q 1 h PRN
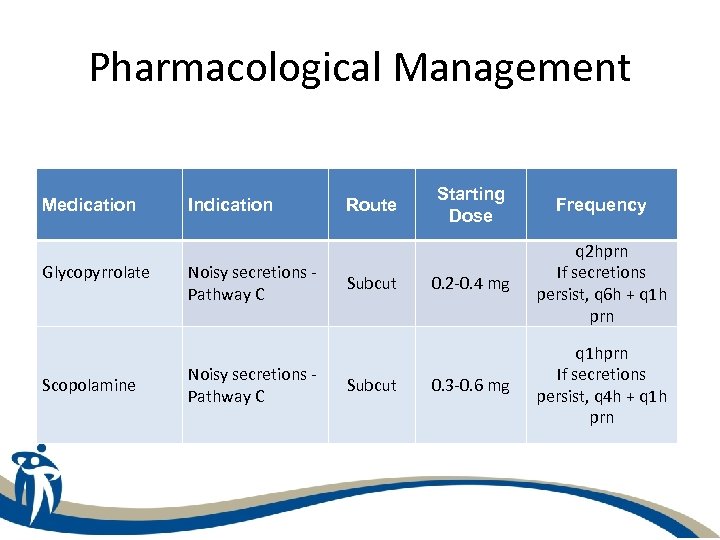
Pharmacological Management Medication Glycopyrrolate Scopolamine Indication Noisy secretions Pathway C Route Subcut Starting Dose Frequency 0. 2 -0. 4 mg q 2 hprn If secretions persist, q 6 h + q 1 h prn 0. 3 -0. 6 mg q 1 hprn If secretions persist, q 4 h + q 1 h prn
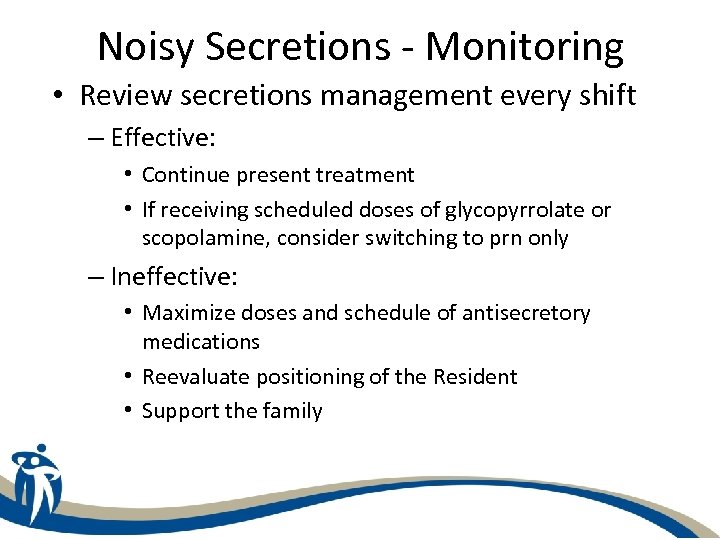
Noisy Secretions - Monitoring • Review secretions management every shift – Effective: • Continue present treatment • If receiving scheduled doses of glycopyrrolate or scopolamine, consider switching to prn only – Ineffective: • Maximize doses and schedule of antisecretory medications • Reevaluate positioning of the Resident • Support the family
Pain • Pain may be related to medical complications • Pain may be related to chronic conditions • If pain exists it should be treated until end of life • Dying of itself is not painful
Pain Assessment • • Ask the patient (verbal indicators) Observe the patient (non-verbal indicators) Talk to family Investigate the medical history Present pain medications Standardized reporting PQRST – Provoking factors, Quality of pain, Relieving factors, Severity and Timing
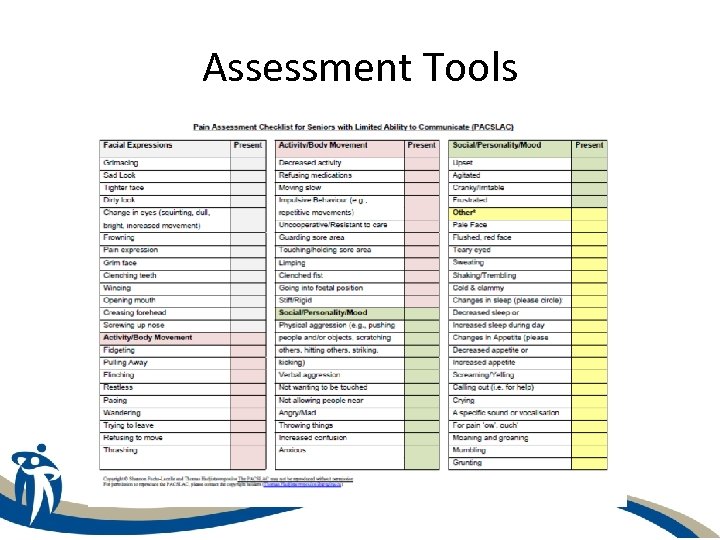
Assessment Tools
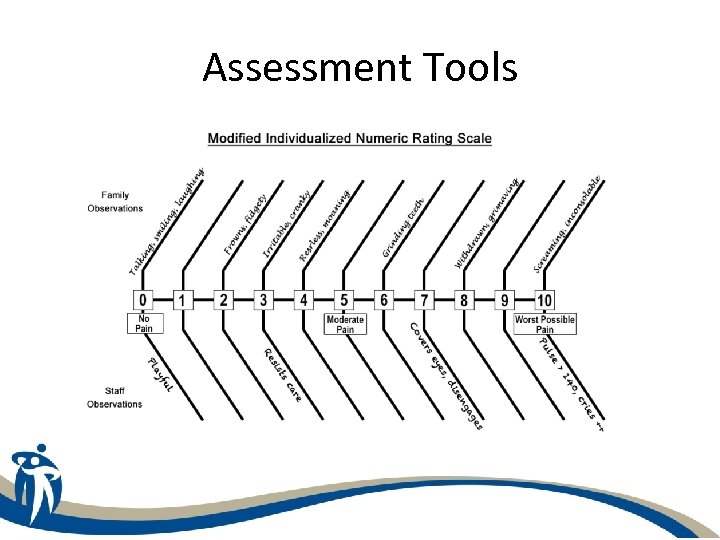
Assessment Tools
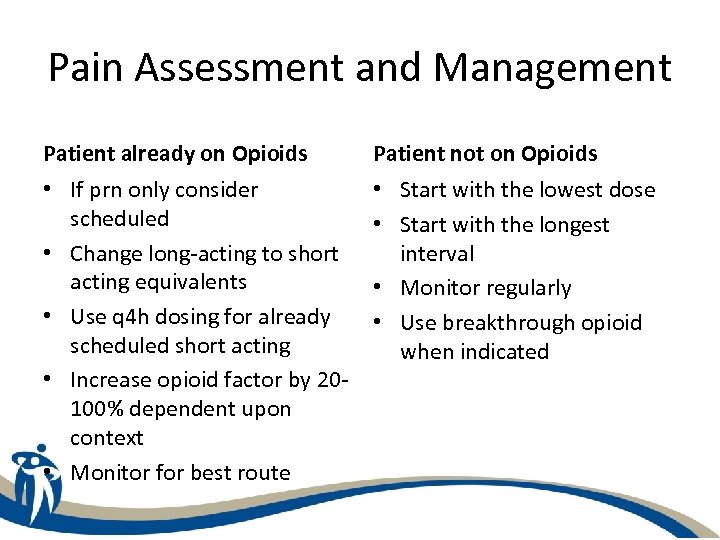
Pain Assessment and Management Patient already on Opioids Patient not on Opioids • If prn only consider scheduled • Change long-acting to short acting equivalents • Use q 4 h dosing for already scheduled short acting • Increase opioid factor by 20100% dependent upon context • Monitor for best route • Start with the lowest dose • Start with the longest interval • Monitor regularly • Use breakthrough opioid when indicated
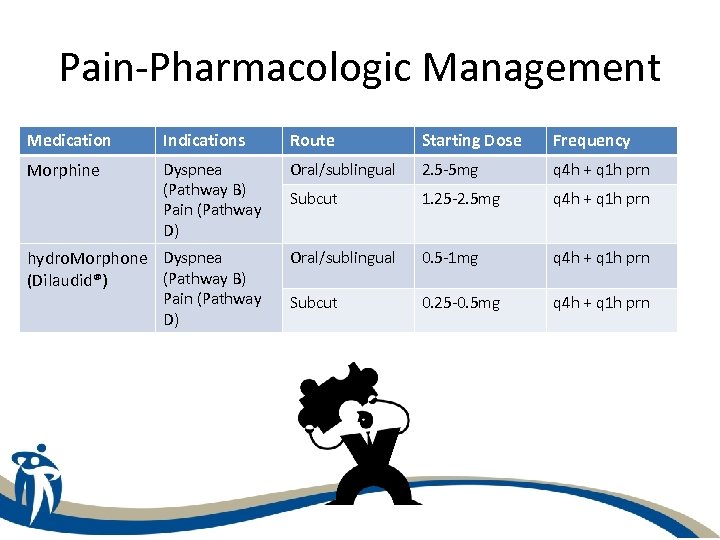
Pain-Pharmacologic Management Medication Indications Route Starting Dose Frequency Morphine Dyspnea (Pathway B) Pain (Pathway D) Oral/sublingual 2. 5 -5 mg q 4 h + q 1 h prn Subcut 1. 25 -2. 5 mg q 4 h + q 1 h prn Oral/sublingual 0. 5 -1 mg q 4 h + q 1 h prn Subcut 0. 25 -0. 5 mg q 4 h + q 1 h prn hydro. Morphone Dyspnea (Pathway B) (Dilaudid®) Pain (Pathway D)
Pain-Nonpharmacologic Management • • Pace and prepare for activity Use distraction and diversion Communicate between team members Decrease environmental stimuli Provide for spiritual/psychosocial support Reassure the patient/family Manage hydration when able
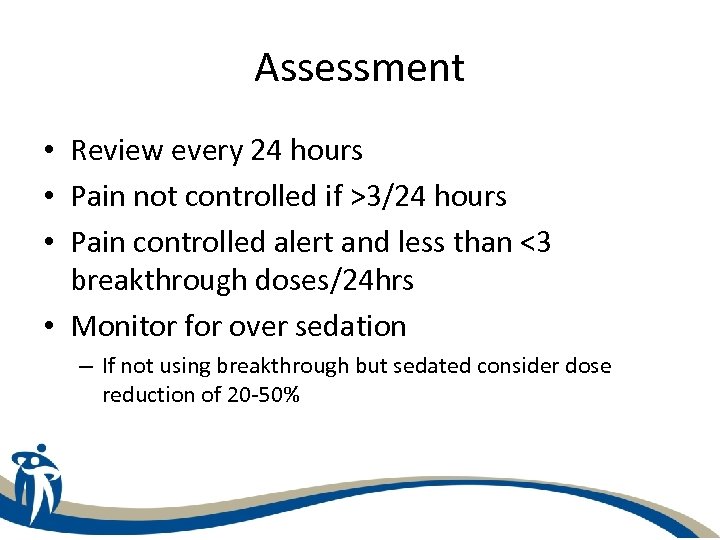
Assessment • Review every 24 hours • Pain not controlled if >3/24 hours • Pain controlled alert and less than <3 breakthrough doses/24 hrs • Monitor for over sedation – If not using breakthrough but sedated consider dose reduction of 20 -50%
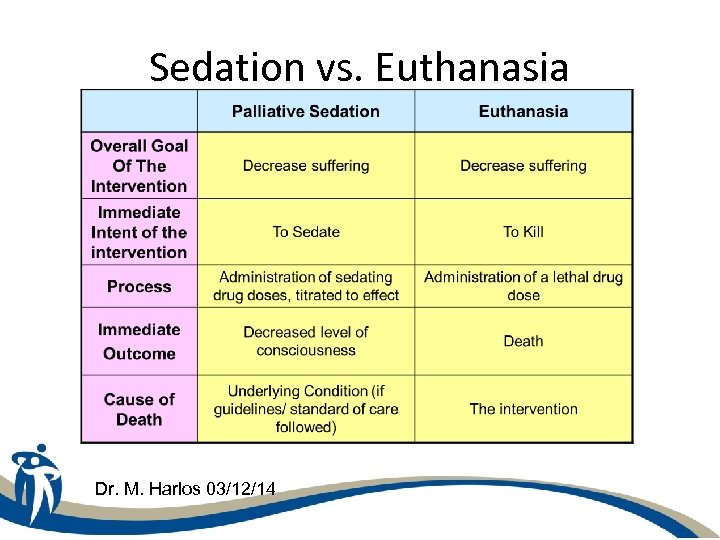
Sedation vs. Euthanasia Dr. M. Harlos 03/12/14
When Death is Near Declining energy and alertness Decreasing intake of food and fluids Difficulty swallowing Mottling of the extremities Changes in breathing pattern Decreased urine output Return to basic reflexes
When should you ask for help? • Symptom control not being achieved • Disagreement between team members • Feeling uncertain about the steps you are taking • Goals of care have been unclear • Help with conversion of medication • other
Who can you call? • WRHA Palliative Care Program – 204 -237 -2400 – A Clinical Nurse Specialist or Physician will be able to assist
Questions/Comments
Resources 1. Long Term Care Website: http: //home. wrha. mb. ca/prog/pch/Endof. Life. Care. Education. Handouts. php 2. Canadian Virtual Hospice: http: //www. virtualhospice. ca 3. WRHA Palliative Program: 204 -237 -2400 4. Hospice and Palliative Care Manitoba for volunteer visiting and grief support Phone: 204 -889 -5825
5534ddc352eef75eca61e5ae04949127.ppt