9816c0fcc707030f2ffe68d96536e0df.ppt
- Количество слайдов: 33
 Preparing for an Audit: DMHRSi Time vs. Workload Reporting Navy Resources Symposium 4 June 2012 Herb Escobar Analytics and Services, Inc. hescobar@easincorporated. com
Preparing for an Audit: DMHRSi Time vs. Workload Reporting Navy Resources Symposium 4 June 2012 Herb Escobar Analytics and Services, Inc. hescobar@easincorporated. com
 Objectives After completing this session the attendee can: • • Describe the Defense Medical Human Resources Reporting System internet (DMHRSi). Characterize data that can be analyzed with DMHRSi not available in MEPRS. Characterize the extent to which workload and timesheet reporting differs at MTF and MEPRS Code level in Navy Medicine. Describe methods that can be used to test the extent to which timesheet and workload reporting differ. 2
Objectives After completing this session the attendee can: • • Describe the Defense Medical Human Resources Reporting System internet (DMHRSi). Characterize data that can be analyzed with DMHRSi not available in MEPRS. Characterize the extent to which workload and timesheet reporting differs at MTF and MEPRS Code level in Navy Medicine. Describe methods that can be used to test the extent to which timesheet and workload reporting differ. 2
 Outline • DMHRSi Data and Application • DMHRSi Data Quality Challenges • Tri-Service Labor Reporting vs. Workload Study • Questions 3
Outline • DMHRSi Data and Application • DMHRSi Data Quality Challenges • Tri-Service Labor Reporting vs. Workload Study • Questions 3
 DMHRSi Data and Application 4
DMHRSi Data and Application 4
 DMHRSi Overview • Defense Medical Human Resources System - internet (DMHRSi) • • • Repository for MHS human capital and labor cost assignment data Source for tri-Service medical human capital information Source of FTE data and personnel expenses in MEPRS and M 2 Self-reported labor hours across Functional Cost Codes (4 th-level MEPRS Codes) Labor hours across MEPRS Codes lead to personnel costs • • • Actual salary for Civilians Uniform composite pay tables for Military No personnel costs for Contractors 5
DMHRSi Overview • Defense Medical Human Resources System - internet (DMHRSi) • • • Repository for MHS human capital and labor cost assignment data Source for tri-Service medical human capital information Source of FTE data and personnel expenses in MEPRS and M 2 Self-reported labor hours across Functional Cost Codes (4 th-level MEPRS Codes) Labor hours across MEPRS Codes lead to personnel costs • • • Actual salary for Civilians Uniform composite pay tables for Military No personnel costs for Contractors 5
 DMHRSi Data Sources • “DMHRSi Discoverer. Plus” is the integrated reporting tool • • Interactive Corporate Reports Ad-hoc queries Performance and documentation challenges SMART receives regular DMHRSi extracts 6
DMHRSi Data Sources • “DMHRSi Discoverer. Plus” is the integrated reporting tool • • Interactive Corporate Reports Ad-hoc queries Performance and documentation challenges SMART receives regular DMHRSi extracts 6
 DMHRSi Data Sources (Cont. ) • Monthly DMHRSi HR extract available in MDR • Person-level assignment data from 1 Oct 2008 – Present • /mdr/pub/dmhrsi/hr/dmhrsi. sas 7 bdat • • EDIPN/NPI/SSN Name/Rank/Grade Person Category/Skill Type/Suffix Occupation Code/Taxonomy/Job/Position Assignment MTF/Organization/People Group Labor Reporting MTF/Organization/People Group Assignment Start/End Dates 7
DMHRSi Data Sources (Cont. ) • Monthly DMHRSi HR extract available in MDR • Person-level assignment data from 1 Oct 2008 – Present • /mdr/pub/dmhrsi/hr/dmhrsi. sas 7 bdat • • EDIPN/NPI/SSN Name/Rank/Grade Person Category/Skill Type/Suffix Occupation Code/Taxonomy/Job/Position Assignment MTF/Organization/People Group Labor Reporting MTF/Organization/People Group Assignment Start/End Dates 7
 Analytic Applications of DMHRSi data • Richness of DMHRSi data facilitates analyses not possible with MEPRS or M 2 personnel data alone • Workload and cost metrics by Facility/Service of assignment – Army or Air Force providers in Navy facilities • Assigned/Available MEPRS codes by person – where are people actually working • National Practitioner Identifier (NPI) and Electronic Data Interchange Person Number (EDIPN) facilitates linking workload from CAPER/SIDR to specific provider characteristics • Labor reporting vs. workload across Functional Cost Codes 8
Analytic Applications of DMHRSi data • Richness of DMHRSi data facilitates analyses not possible with MEPRS or M 2 personnel data alone • Workload and cost metrics by Facility/Service of assignment – Army or Air Force providers in Navy facilities • Assigned/Available MEPRS codes by person – where are people actually working • National Practitioner Identifier (NPI) and Electronic Data Interchange Person Number (EDIPN) facilitates linking workload from CAPER/SIDR to specific provider characteristics • Labor reporting vs. workload across Functional Cost Codes 8
 DMHRSi Data Quality Challenges 9
DMHRSi Data Quality Challenges 9
 DMHRSi Data Quality • Common of DQ issues observed – some easy to spot • • Manual data entry errors: UIC “KV!MFV 9 P" vs. "KV 1 MFV 9 P” Inconsistent data entry: “TMA” vs. “TRICARE MGT”, “PHS” vs. “Public Health” Caps vs. Lower Case: “Navy” vs. “NAVY” More serious DQ issues affect reconciliation of data transmitted to downstream systems 10
DMHRSi Data Quality • Common of DQ issues observed – some easy to spot • • Manual data entry errors: UIC “KV!MFV 9 P" vs. "KV 1 MFV 9 P” Inconsistent data entry: “TMA” vs. “TRICARE MGT”, “PHS” vs. “Public Health” Caps vs. Lower Case: “Navy” vs. “NAVY” More serious DQ issues affect reconciliation of data transmitted to downstream systems 10
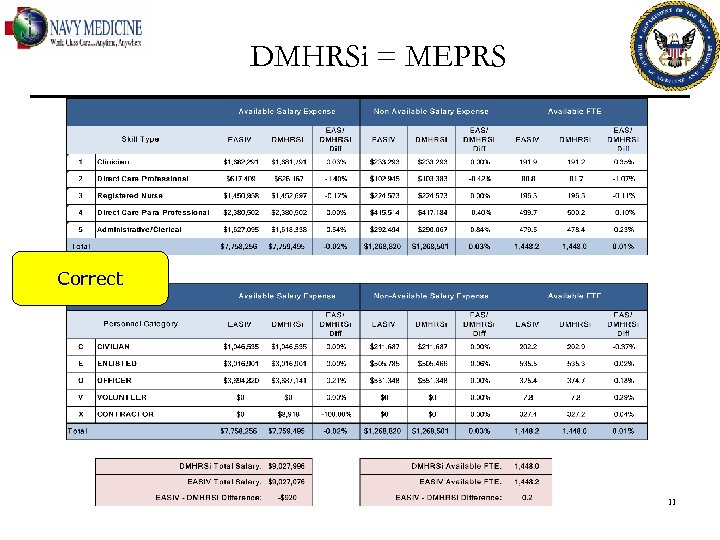 DMHRSi = MEPRS Correct 11
DMHRSi = MEPRS Correct 11
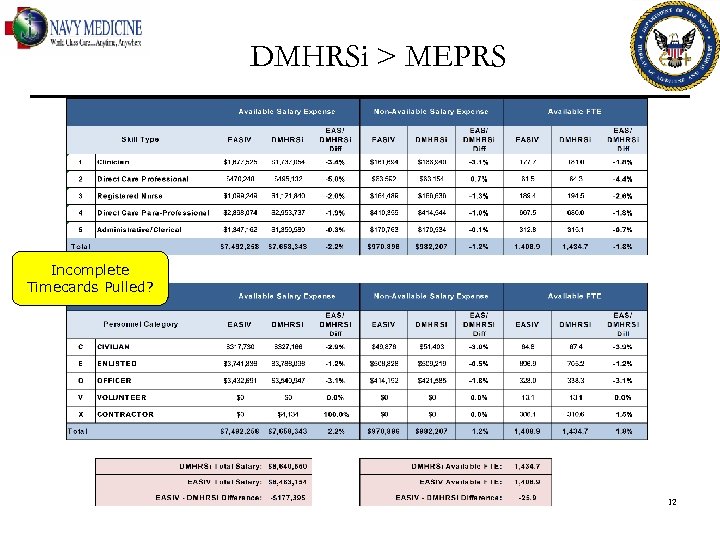 DMHRSi > MEPRS Incomplete Timecards Pulled? 12
DMHRSi > MEPRS Incomplete Timecards Pulled? 12
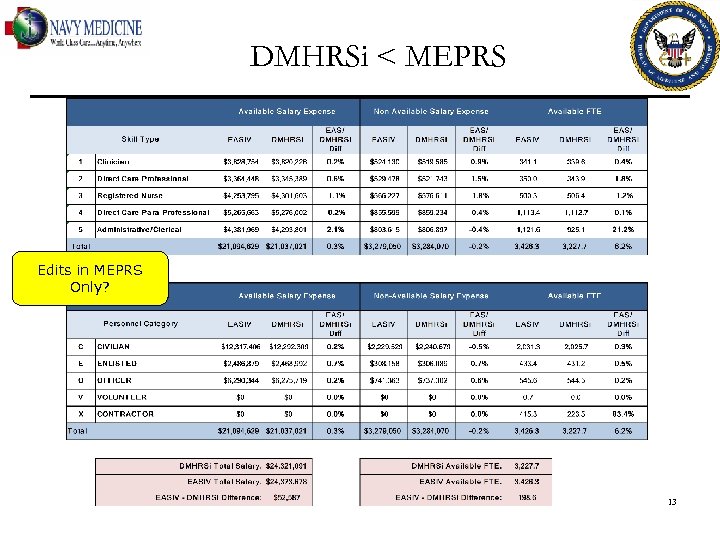 DMHRSi < MEPRS Edits in MEPRS Only? 13
DMHRSi < MEPRS Edits in MEPRS Only? 13
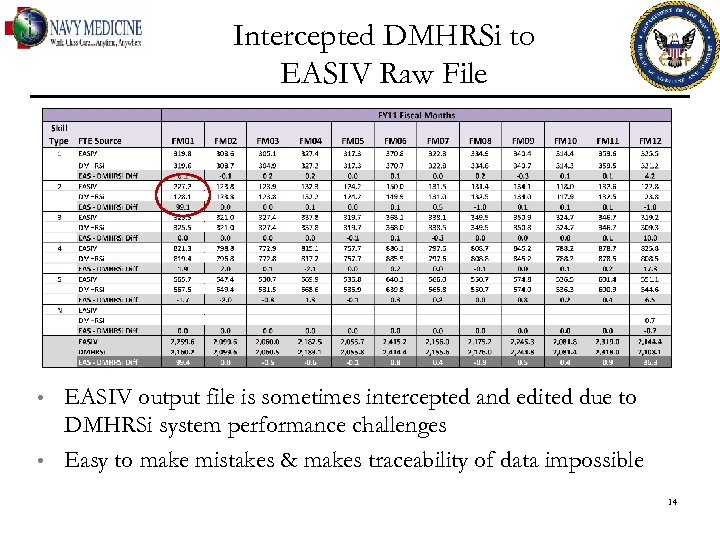 Intercepted DMHRSi to EASIV Raw File • • EASIV output file is sometimes intercepted and edited due to DMHRSi system performance challenges Easy to make mistakes & makes traceability of data impossible 14
Intercepted DMHRSi to EASIV Raw File • • EASIV output file is sometimes intercepted and edited due to DMHRSi system performance challenges Easy to make mistakes & makes traceability of data impossible 14
 Tri-Service Labor Reporting vs. Workload Study 15
Tri-Service Labor Reporting vs. Workload Study 15
 Background • • Labor costs account for about 70% of MHS facility expenses. Accurate reporting of labor hours across facility work centers is critical for valid healthcare cost and productivity analysis. Do. D 6010. 13 M provides detailed labor reporting policy and instructions. First-of-its-kind study sponsored by the Methods, Measures and Analyses Directorate at TMA/DHCAPE through Axiom – Resource Management examined reported labor and associated workload across clinics. 16
Background • • Labor costs account for about 70% of MHS facility expenses. Accurate reporting of labor hours across facility work centers is critical for valid healthcare cost and productivity analysis. Do. D 6010. 13 M provides detailed labor reporting policy and instructions. First-of-its-kind study sponsored by the Methods, Measures and Analyses Directorate at TMA/DHCAPE through Axiom – Resource Management examined reported labor and associated workload across clinics. 16
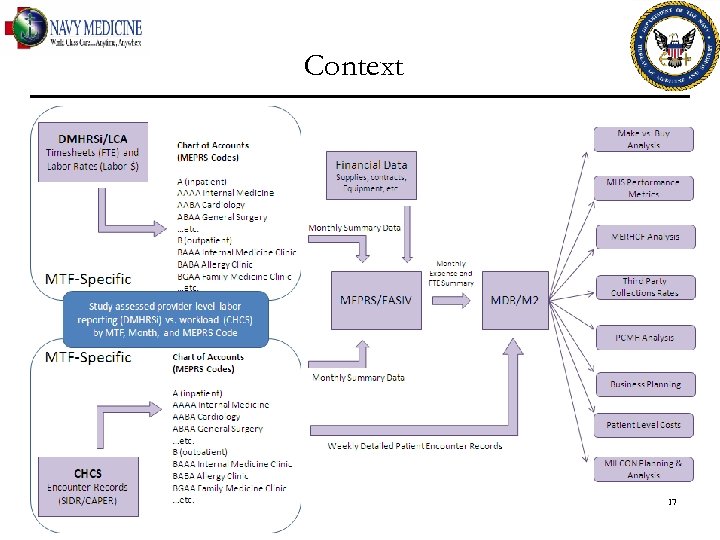 Context 17
Context 17
 Method • • • Darnall AMC - Ft. Hood, NH Pensacola, and the 60 th Medical Group –Travis AFB Fiscal Year 2011 data were analyzed Person-specific Available hours by facility, fiscal month, and cost center were obtained from DMHRSi Labor Cost Assignment (LCA) module via Discoverer CAPER and SIDR workload records by facility, fiscal month, and cost center were extracted from the MHS Data Repository (MDR) EDIPN and NPI data were added to the LCA extract to facilitate provider-level matching to CAPER/SIDR workload datasets LCA data matched to CAPER/SIDR by facility, fiscal month, and 4 th-level Functional Cost Code 18
Method • • • Darnall AMC - Ft. Hood, NH Pensacola, and the 60 th Medical Group –Travis AFB Fiscal Year 2011 data were analyzed Person-specific Available hours by facility, fiscal month, and cost center were obtained from DMHRSi Labor Cost Assignment (LCA) module via Discoverer CAPER and SIDR workload records by facility, fiscal month, and cost center were extracted from the MHS Data Repository (MDR) EDIPN and NPI data were added to the LCA extract to facilitate provider-level matching to CAPER/SIDR workload datasets LCA data matched to CAPER/SIDR by facility, fiscal month, and 4 th-level Functional Cost Code 18
 Method (Cont. ) • • • All skill types were included in the LCA analysis dataset (i. e. , providers, nurses, techs, etc. ) Only MEPRS-B CAPERs were included Provider 1 – 5 Work RVUs and individual providers in CAPERs were included (only 1 – 3 were populated) CAPER/LCA match on EDIPN then NPI SIDR analyses included Attending, Admitting, and procedure-specific providers; Total RWPs retained SIDR/LCA match on NPI 19
Method (Cont. ) • • • All skill types were included in the LCA analysis dataset (i. e. , providers, nurses, techs, etc. ) Only MEPRS-B CAPERs were included Provider 1 – 5 Work RVUs and individual providers in CAPERs were included (only 1 – 3 were populated) CAPER/LCA match on EDIPN then NPI SIDR analyses included Attending, Admitting, and procedure-specific providers; Total RWPs retained SIDR/LCA match on NPI 19
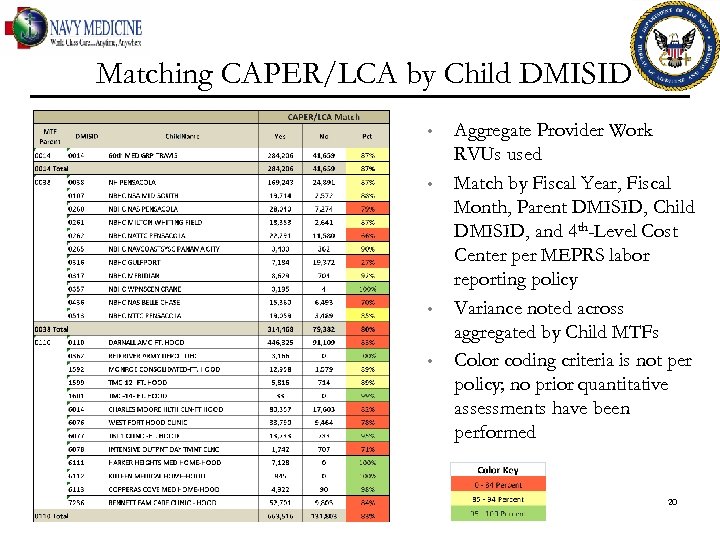 Matching CAPER/LCA by Child DMISID • • Aggregate Provider Work RVUs used Match by Fiscal Year, Fiscal Month, Parent DMISID, Child DMISID, and 4 th-Level Cost Center per MEPRS labor reporting policy Variance noted across aggregated by Child MTFs Color coding criteria is not per policy; no prior quantitative assessments have been performed 20
Matching CAPER/LCA by Child DMISID • • Aggregate Provider Work RVUs used Match by Fiscal Year, Fiscal Month, Parent DMISID, Child DMISID, and 4 th-Level Cost Center per MEPRS labor reporting policy Variance noted across aggregated by Child MTFs Color coding criteria is not per policy; no prior quantitative assessments have been performed 20
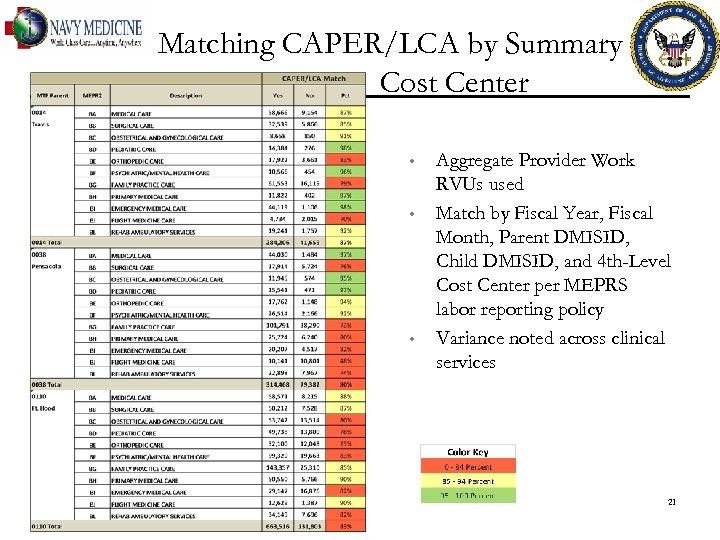 Matching CAPER/LCA by Summary Cost Center • • • Aggregate Provider Work RVUs used Match by Fiscal Year, Fiscal Month, Parent DMISID, Child DMISID, and 4 th-Level Cost Center per MEPRS labor reporting policy Variance noted across clinical services 21
Matching CAPER/LCA by Summary Cost Center • • • Aggregate Provider Work RVUs used Match by Fiscal Year, Fiscal Month, Parent DMISID, Child DMISID, and 4 th-Level Cost Center per MEPRS labor reporting policy Variance noted across clinical services 21
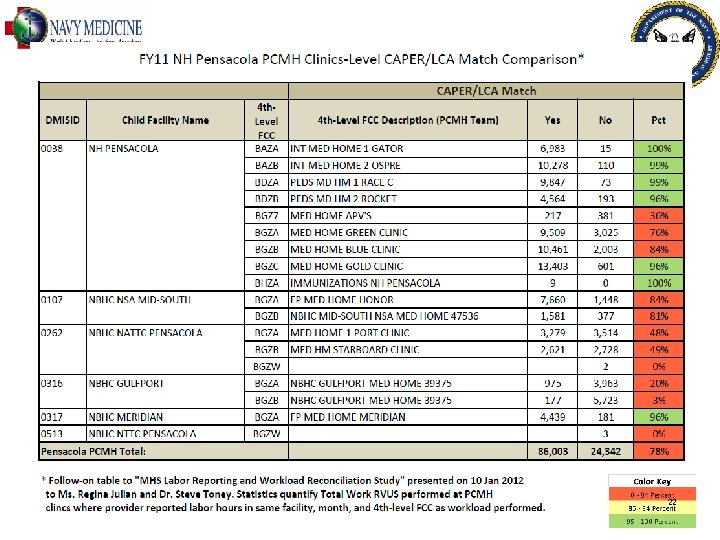 22
22
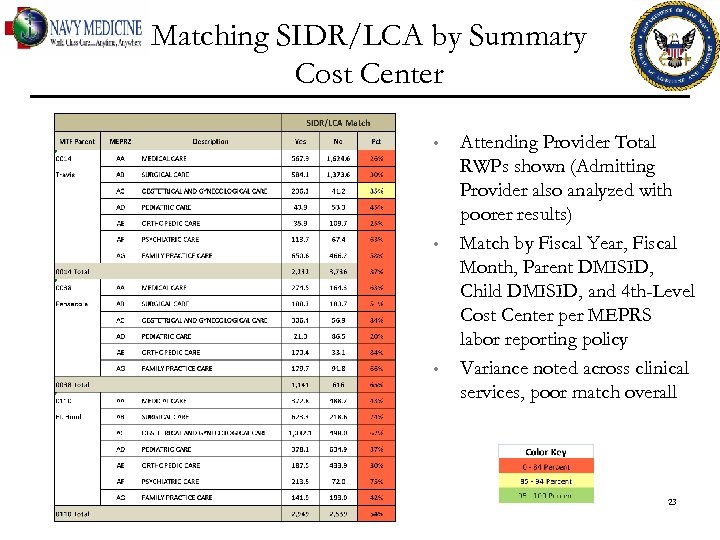 Matching SIDR/LCA by Summary Cost Center • • • Attending Provider Total RWPs shown (Admitting Provider also analyzed with poorer results) Match by Fiscal Year, Fiscal Month, Parent DMISID, Child DMISID, and 4 th-Level Cost Center per MEPRS labor reporting policy Variance noted across clinical services, poor match overall 23
Matching SIDR/LCA by Summary Cost Center • • • Attending Provider Total RWPs shown (Admitting Provider also analyzed with poorer results) Match by Fiscal Year, Fiscal Month, Parent DMISID, Child DMISID, and 4 th-Level Cost Center per MEPRS labor reporting policy Variance noted across clinical services, poor match overall 23
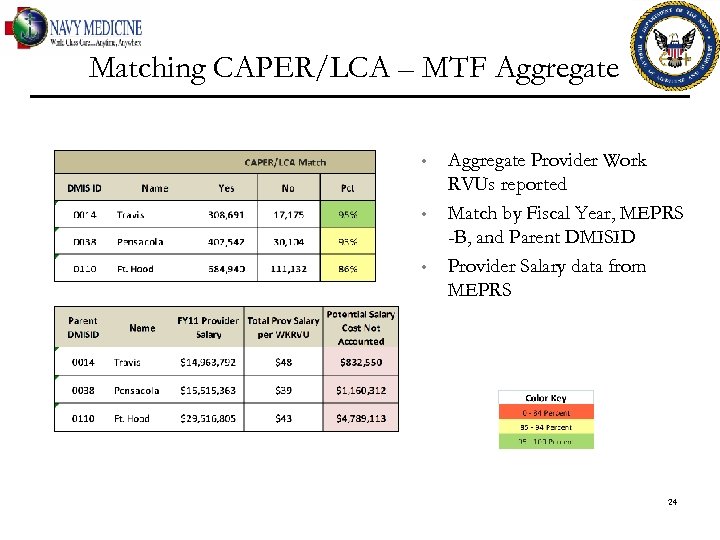 Matching CAPER/LCA – MTF Aggregate • • • Aggregate Provider Work RVUs reported Match by Fiscal Year, MEPRS -B, and Parent DMISID Provider Salary data from MEPRS 24
Matching CAPER/LCA – MTF Aggregate • • • Aggregate Provider Work RVUs reported Match by Fiscal Year, MEPRS -B, and Parent DMISID Provider Salary data from MEPRS 24
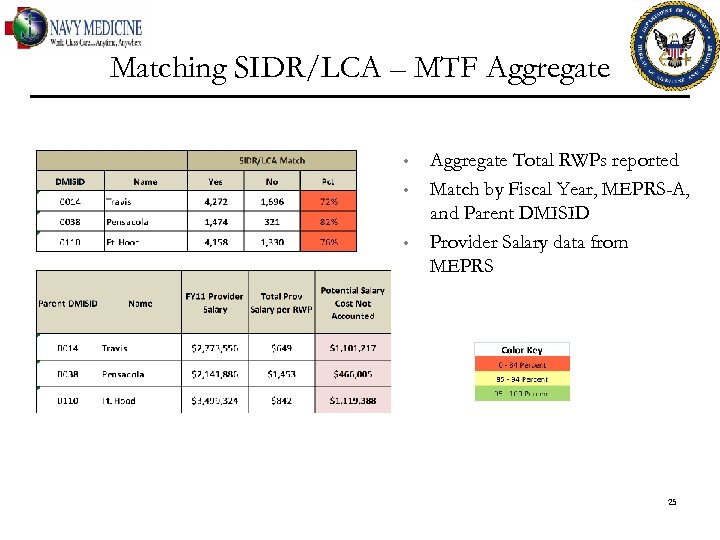 Matching SIDR/LCA – MTF Aggregate • • • Aggregate Total RWPs reported Match by Fiscal Year, MEPRS-A, and Parent DMISID Provider Salary data from MEPRS 25
Matching SIDR/LCA – MTF Aggregate • • • Aggregate Total RWPs reported Match by Fiscal Year, MEPRS-A, and Parent DMISID Provider Salary data from MEPRS 25
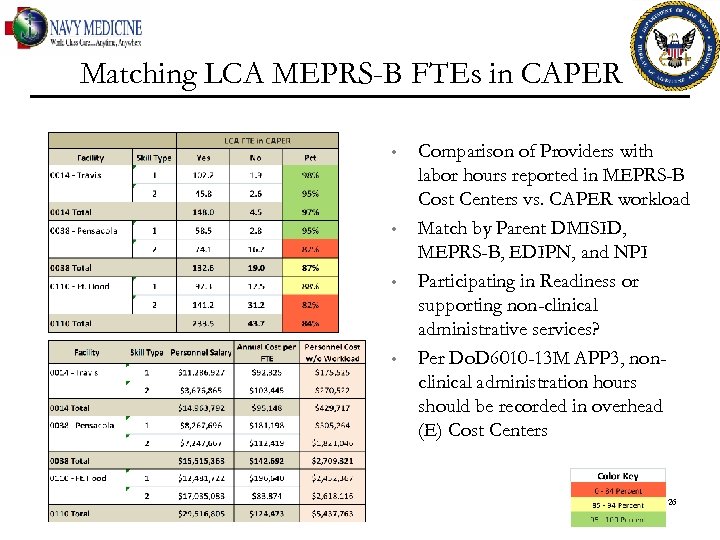 Matching LCA MEPRS-B FTEs in CAPER • • Comparison of Providers with labor hours reported in MEPRS-B Cost Centers vs. CAPER workload Match by Parent DMISID, MEPRS-B, EDIPN, and NPI Participating in Readiness or supporting non-clinical administrative services? Per Do. D 6010 -13 M APP 3, nonclinical administration hours should be recorded in overhead (E) Cost Centers 26
Matching LCA MEPRS-B FTEs in CAPER • • Comparison of Providers with labor hours reported in MEPRS-B Cost Centers vs. CAPER workload Match by Parent DMISID, MEPRS-B, EDIPN, and NPI Participating in Readiness or supporting non-clinical administrative services? Per Do. D 6010 -13 M APP 3, nonclinical administration hours should be recorded in overhead (E) Cost Centers 26
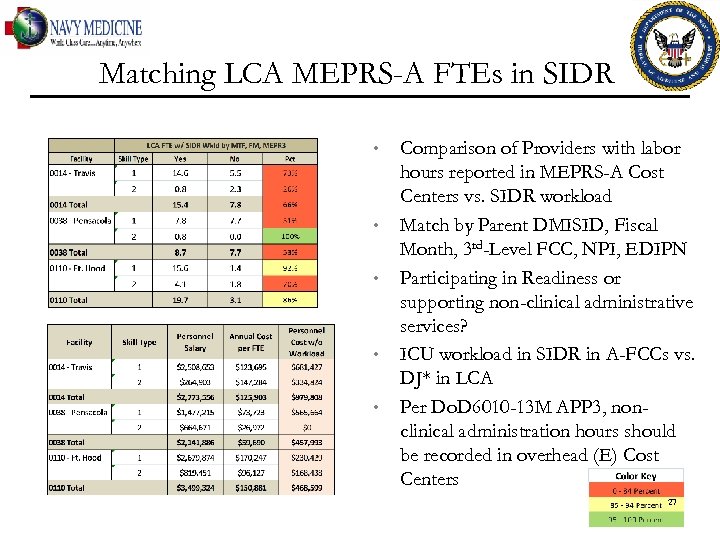 Matching LCA MEPRS-A FTEs in SIDR • • • Comparison of Providers with labor hours reported in MEPRS-A Cost Centers vs. SIDR workload Match by Parent DMISID, Fiscal Month, 3 rd-Level FCC, NPI, EDIPN Participating in Readiness or supporting non-clinical administrative services? ICU workload in SIDR in A-FCCs vs. DJ* in LCA Per Do. D 6010 -13 M APP 3, nonclinical administration hours should be recorded in overhead (E) Cost Centers 27
Matching LCA MEPRS-A FTEs in SIDR • • • Comparison of Providers with labor hours reported in MEPRS-A Cost Centers vs. SIDR workload Match by Parent DMISID, Fiscal Month, 3 rd-Level FCC, NPI, EDIPN Participating in Readiness or supporting non-clinical administrative services? ICU workload in SIDR in A-FCCs vs. DJ* in LCA Per Do. D 6010 -13 M APP 3, nonclinical administration hours should be recorded in overhead (E) Cost Centers 27
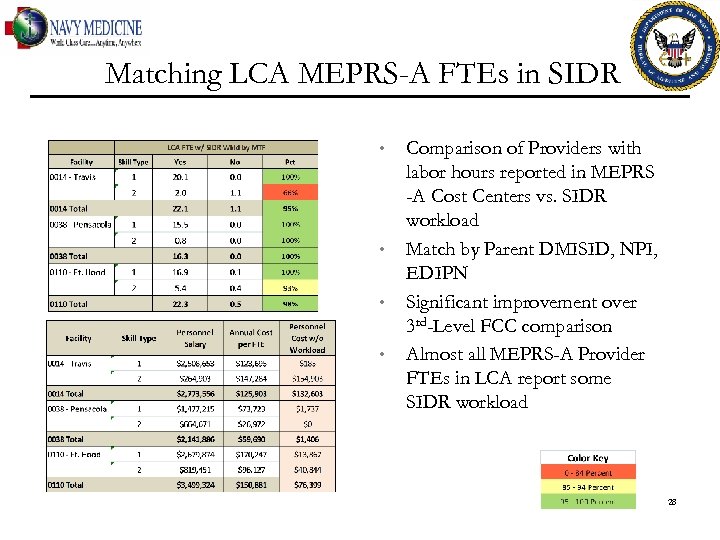 Matching LCA MEPRS-A FTEs in SIDR • • Comparison of Providers with labor hours reported in MEPRS -A Cost Centers vs. SIDR workload Match by Parent DMISID, NPI, EDIPN Significant improvement over 3 rd-Level FCC comparison Almost all MEPRS-A Provider FTEs in LCA report some SIDR workload 28
Matching LCA MEPRS-A FTEs in SIDR • • Comparison of Providers with labor hours reported in MEPRS -A Cost Centers vs. SIDR workload Match by Parent DMISID, NPI, EDIPN Significant improvement over 3 rd-Level FCC comparison Almost all MEPRS-A Provider FTEs in LCA report some SIDR workload 28
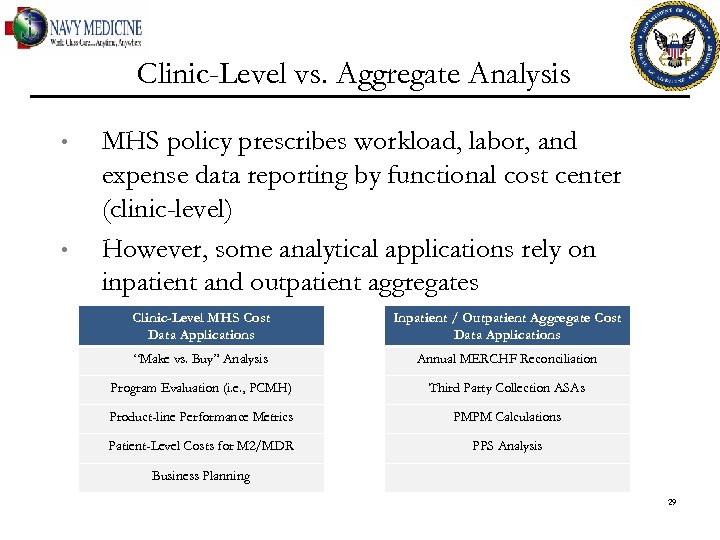 Clinic-Level vs. Aggregate Analysis • • MHS policy prescribes workload, labor, and expense data reporting by functional cost center (clinic-level) However, some analytical applications rely on inpatient and outpatient aggregates Clinic-Level MHS Cost Data Applications Inpatient / Outpatient Aggregate Cost Data Applications “Make vs. Buy” Analysis Annual MERCHF Reconciliation Program Evaluation (i. e. , PCMH) Third Party Collection ASAs Product-line Performance Metrics PMPM Calculations Patient-Level Costs for M 2/MDR PPS Analysis Business Planning 29
Clinic-Level vs. Aggregate Analysis • • MHS policy prescribes workload, labor, and expense data reporting by functional cost center (clinic-level) However, some analytical applications rely on inpatient and outpatient aggregates Clinic-Level MHS Cost Data Applications Inpatient / Outpatient Aggregate Cost Data Applications “Make vs. Buy” Analysis Annual MERCHF Reconciliation Program Evaluation (i. e. , PCMH) Third Party Collection ASAs Product-line Performance Metrics PMPM Calculations Patient-Level Costs for M 2/MDR PPS Analysis Business Planning 29
 Study Conclusions • • Study demonstrates ability to link reported labor hours by provider to specific workload production Unquestionable problem dictating further attention and examination Next Steps • • Follow-on study will seek to validate initial results and expand analyses Explore centrally developed metrics to monitor: • • DMHRSi Labor vs. workload match DMHRSi Available FTE vs. EASIV Available FTE 30
Study Conclusions • • Study demonstrates ability to link reported labor hours by provider to specific workload production Unquestionable problem dictating further attention and examination Next Steps • • Follow-on study will seek to validate initial results and expand analyses Explore centrally developed metrics to monitor: • • DMHRSi Labor vs. workload match DMHRSi Available FTE vs. EASIV Available FTE 30
 Review of Objectives 31
Review of Objectives 31
 Objectives Review After completing this session the attendee can: • • Describe the Defense Medical Human Resources Reporting System internet (DMHRSi). Characterize data that can be analyzed with DMHRSi not available in MEPRS. Characterize the extent to which workload and timesheet reporting differs at MTF and MEPRS Code level in Navy Medicine. Describe methods that can be used to test the extent to which timesheet and workload reporting differ. 32
Objectives Review After completing this session the attendee can: • • Describe the Defense Medical Human Resources Reporting System internet (DMHRSi). Characterize data that can be analyzed with DMHRSi not available in MEPRS. Characterize the extent to which workload and timesheet reporting differs at MTF and MEPRS Code level in Navy Medicine. Describe methods that can be used to test the extent to which timesheet and workload reporting differ. 32
 Preparing for an Audit: DMHRSi Time vs. Workload Reporting Navy Resources Symposium 4 June 2012 Herb Escobar Analytics and Services, Inc. hescobar@easincorporated. com
Preparing for an Audit: DMHRSi Time vs. Workload Reporting Navy Resources Symposium 4 June 2012 Herb Escobar Analytics and Services, Inc. hescobar@easincorporated. com


