ea2de7445424f8aa54727546e8212254.ppt
- Количество слайдов: 59
 Preparing for 2011 – Where are we and where are we going Cathie Biga President/CEO Cardiovascular Management of Illinois
Preparing for 2011 – Where are we and where are we going Cathie Biga President/CEO Cardiovascular Management of Illinois
 Agenda • • 2010 in review Technical Correction 2011 Physician Fee Schedule 2011 HOPPS Private Payers in 2011 HCR/ACA – its impact Core 2011 concepts: PQRS/e. Rx….
Agenda • • 2010 in review Technical Correction 2011 Physician Fee Schedule 2011 HOPPS Private Payers in 2011 HCR/ACA – its impact Core 2011 concepts: PQRS/e. Rx….
 Legal Primary Issues • • • HCR/ACA Threats to physician ownership/in-office imaging SGR – will it ever be fixed IPAB CMI Secondary Issues • Key topics – 1) Disclosure requirements for CT, PET, MRI, 2) PECOS, 3) POS/DOS, 4) Timely filing • 2012 Accreditation of labs and 2010 IAC changes • Meaningful use – stretch or a barrier?
Legal Primary Issues • • • HCR/ACA Threats to physician ownership/in-office imaging SGR – will it ever be fixed IPAB CMI Secondary Issues • Key topics – 1) Disclosure requirements for CT, PET, MRI, 2) PECOS, 3) POS/DOS, 4) Timely filing • 2012 Accreditation of labs and 2010 IAC changes • Meaningful use – stretch or a barrier?
 Regulatory • PFS 2011 – – 2 nd year of PPIS implementation Bundling continues Rebase for MEI RUC focus • HOPPS 2011 – Reductions beginning? • Quality focus continues to grow • Ongoing scrutiny of imaging and IOE • EP becomes its own specialty 4/4/11 – ENROLLMENT NEEDED
Regulatory • PFS 2011 – – 2 nd year of PPIS implementation Bundling continues Rebase for MEI RUC focus • HOPPS 2011 – Reductions beginning? • Quality focus continues to grow • Ongoing scrutiny of imaging and IOE • EP becomes its own specialty 4/4/11 – ENROLLMENT NEEDED
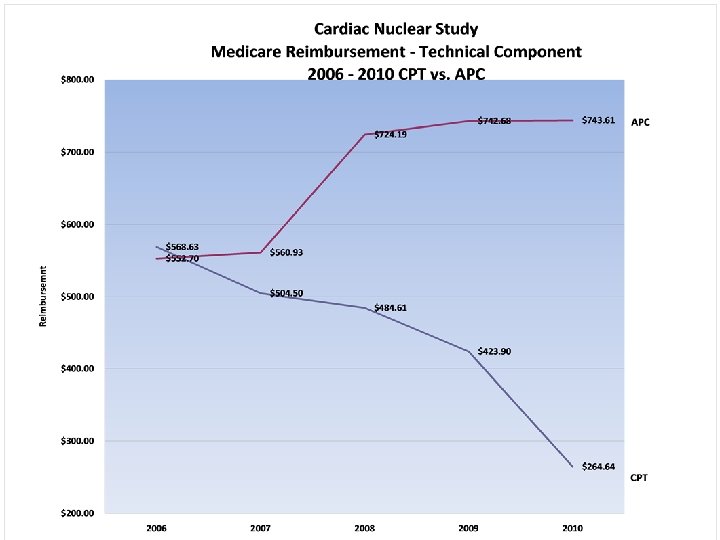
 Economic • Gap in technical – Bundling of nucs ’ 10 – Bundling of caths ’ 11 – Massive PV bundling • RAC’s, MACs, and other attacks • Revenue wherever you can find it – – Clinical integration PQRI e. Rx Meaningful use • Operational efficiencies • New product lines
Economic • Gap in technical – Bundling of nucs ’ 10 – Bundling of caths ’ 11 – Massive PV bundling • RAC’s, MACs, and other attacks • Revenue wherever you can find it – – Clinical integration PQRI e. Rx Meaningful use • Operational efficiencies • New product lines
 Technical Correction • • What is it What do we do What have people done Current status
Technical Correction • • What is it What do we do What have people done Current status
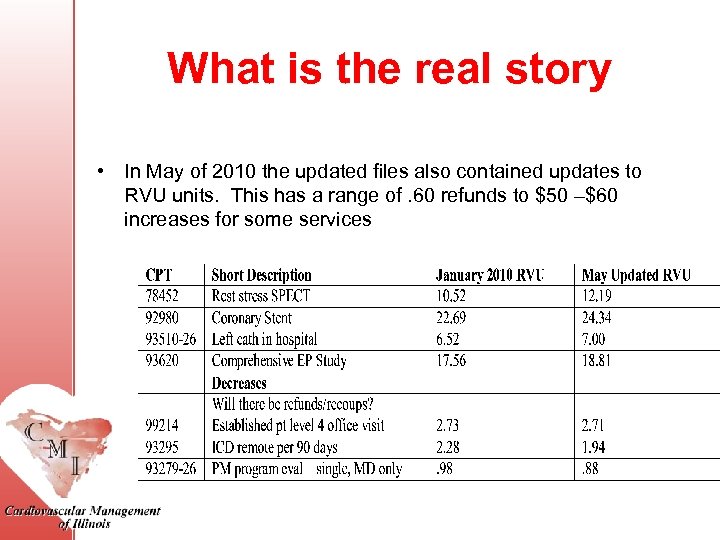 What is the real story • In May of 2010 the updated files also contained updates to RVU units. This has a range of. 60 refunds to $50 –$60 increases for some services
What is the real story • In May of 2010 the updated files also contained updates to RVU units. This has a range of. 60 refunds to $50 –$60 increases for some services
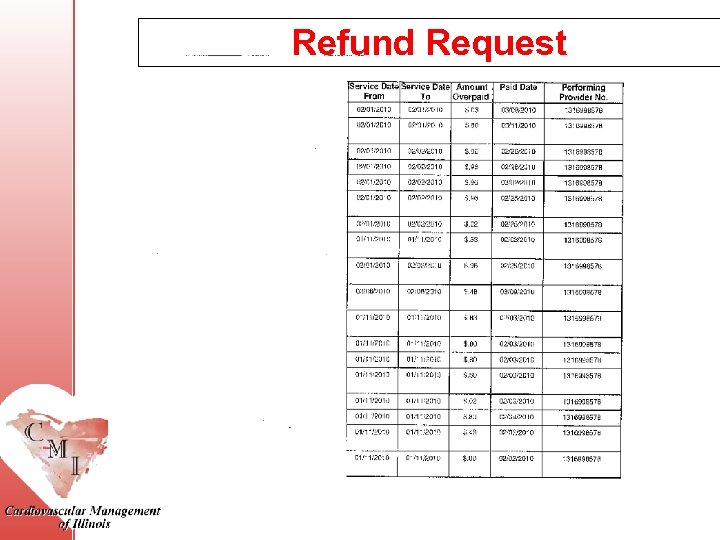 Refund Request
Refund Request
 Technical Correction • $2 M just appropriated for re-filing • How to handle both the upside…. and the downside • Patient responsibility • Secondary's • You have to love it…
Technical Correction • $2 M just appropriated for re-filing • How to handle both the upside…. and the downside • Patient responsibility • Secondary's • You have to love it…
 2011 Fee Schedule • Be sure you have downloaded the one with the $33. 97 CF • Let’s walk through the key elements and lo lights
2011 Fee Schedule • Be sure you have downloaded the one with the $33. 97 CF • Let’s walk through the key elements and lo lights
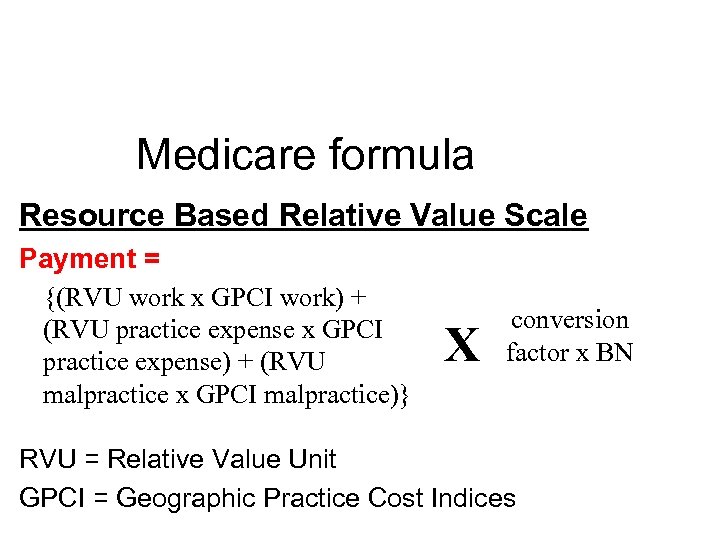 Medicare formula Resource Based Relative Value Scale Payment = {(RVU work x GPCI work) + (RVU practice expense x GPCI practice expense) + (RVU malpractice x GPCI malpractice)} X conversion factor x BN RVU = Relative Value Unit GPCI = Geographic Practice Cost Indices
Medicare formula Resource Based Relative Value Scale Payment = {(RVU work x GPCI work) + (RVU practice expense x GPCI practice expense) + (RVU malpractice x GPCI malpractice)} X conversion factor x BN RVU = Relative Value Unit GPCI = Geographic Practice Cost Indices
 SGR…. . • SGR …. • Rollercoaster throughout 2011 • 13 month “fix” – That only cost $19 BILLION – No increase for physicians • After the May technical correction the CF was $36. 8729 • Sunset – Dec 1, 2010 (was to be a 23. 6% hit) • Sunset – Jan. 1, 2011 – 12 month extension • 2011: Conversion Factor = $33. 9764
SGR…. . • SGR …. • Rollercoaster throughout 2011 • 13 month “fix” – That only cost $19 BILLION – No increase for physicians • After the May technical correction the CF was $36. 8729 • Sunset – Dec 1, 2010 (was to be a 23. 6% hit) • Sunset – Jan. 1, 2011 – 12 month extension • 2011: Conversion Factor = $33. 9764
 MEI …impact • CMS is rebasing and revising the MEI to use a 2006 base year in place of a 2000 base year. – This update to the MEI is the first time it has been rebased and revised since 2004. • For practices with high technical this will result in an increase • Total RVU’s attributed to work will see a decrease • Bottom line – mitigated a bit of the PPIS hit – Resulted in a major CF change
MEI …impact • CMS is rebasing and revising the MEI to use a 2006 base year in place of a 2000 base year. – This update to the MEI is the first time it has been rebased and revised since 2004. • For practices with high technical this will result in an increase • Total RVU’s attributed to work will see a decrease • Bottom line – mitigated a bit of the PPIS hit – Resulted in a major CF change
 Why do my fees keep changing RVU changes • This is the last year of a 4 yr phase in on how PE are determined – we are DONE with this • This is the 2 nd yr (of a 4 yr plan) due to the PPIS • This is the 1 st time MEI has been re-based • The RUC keeps messing with us – Bundling – Revaluing
Why do my fees keep changing RVU changes • This is the last year of a 4 yr phase in on how PE are determined – we are DONE with this • This is the 2 nd yr (of a 4 yr plan) due to the PPIS • This is the 1 st time MEI has been re-based • The RUC keeps messing with us – Bundling – Revaluing
 Other key factors of 2011 Fee schedule • Financial Disclosure letter and sites – MRI, CT, PET – Time of referral – 5 suppliers within 25 miles – Document compliance • EU rate – 75% • Multiple procedure reduction – Affects technical component – 25% increases to 50%
Other key factors of 2011 Fee schedule • Financial Disclosure letter and sites – MRI, CT, PET – Time of referral – 5 suppliers within 25 miles – Document compliance • EU rate – 75% • Multiple procedure reduction – Affects technical component – 25% increases to 50%
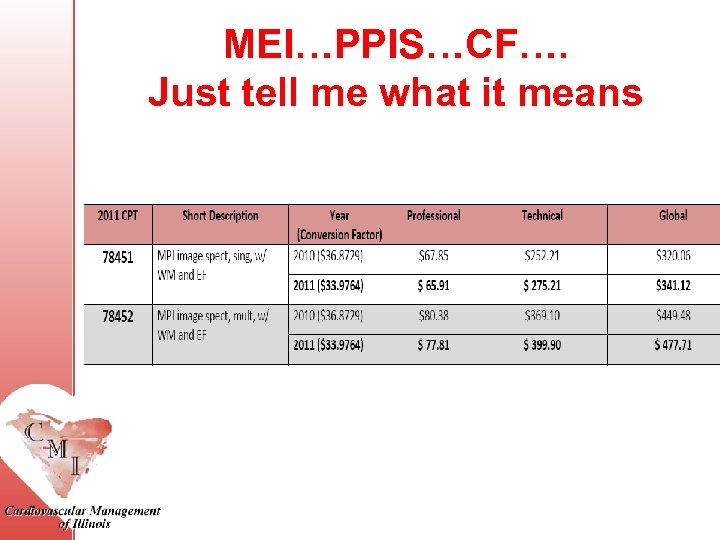 MEI…PPIS…CF…. Just tell me what it means
MEI…PPIS…CF…. Just tell me what it means
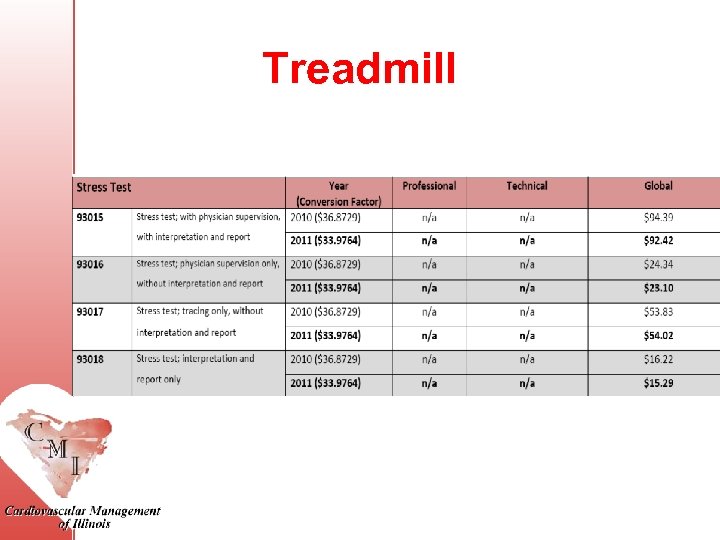 Treadmill
Treadmill
 Hopps • Echo payment reduced – 13. 5% • PET reduced • Supervision re-defined – Hospital outpt on campus – Hospital outpt off campus
Hopps • Echo payment reduced – 13. 5% • PET reduced • Supervision re-defined – Hospital outpt on campus – Hospital outpt off campus
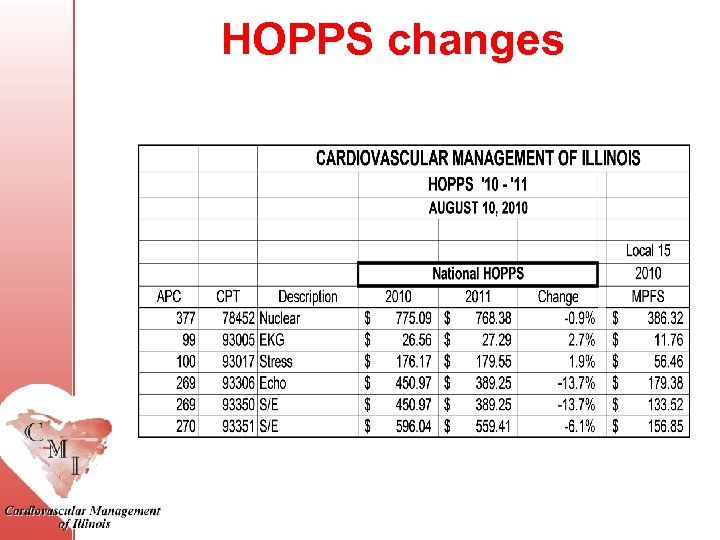 HOPPS changes
HOPPS changes
 Private payor shenanigans • Highmark…. . – Substitute echo for nuc • United pre-notification • Humana pre-notification • Report cards
Private payor shenanigans • Highmark…. . – Substitute echo for nuc • United pre-notification • Humana pre-notification • Report cards
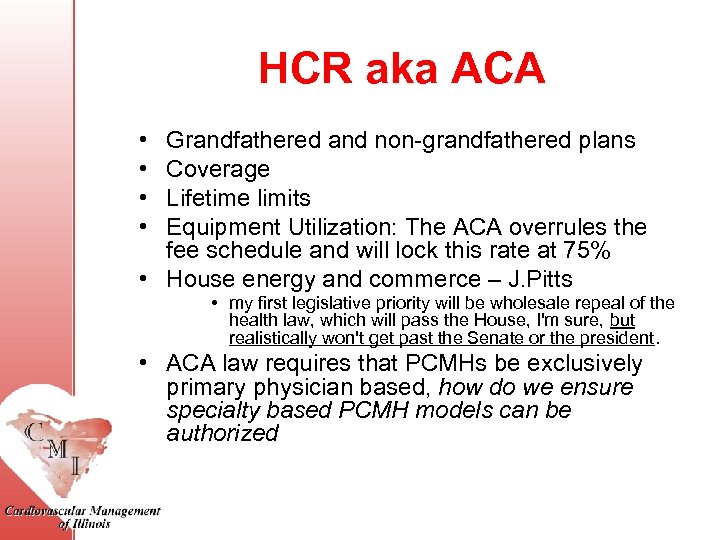 HCR aka ACA • • Grandfathered and non-grandfathered plans Coverage Lifetime limits Equipment Utilization: The ACA overrules the fee schedule and will lock this rate at 75% • House energy and commerce – J. Pitts • my first legislative priority will be wholesale repeal of the health law, which will pass the House, I'm sure, but realistically won't get past the Senate or the president. • ACA law requires that PCMHs be exclusively primary physician based, how do we ensure specialty based PCMH models can be authorized
HCR aka ACA • • Grandfathered and non-grandfathered plans Coverage Lifetime limits Equipment Utilization: The ACA overrules the fee schedule and will lock this rate at 75% • House energy and commerce – J. Pitts • my first legislative priority will be wholesale repeal of the health law, which will pass the House, I'm sure, but realistically won't get past the Senate or the president. • ACA law requires that PCMHs be exclusively primary physician based, how do we ensure specialty based PCMH models can be authorized
 Integration • Drivers – HCR – Med. Pac and imaging scrutiny – Payment reform mandates – HOPPS vs PFS • Is it here to stay? ? ?
Integration • Drivers – HCR – Med. Pac and imaging scrutiny – Payment reform mandates – HOPPS vs PFS • Is it here to stay? ? ?
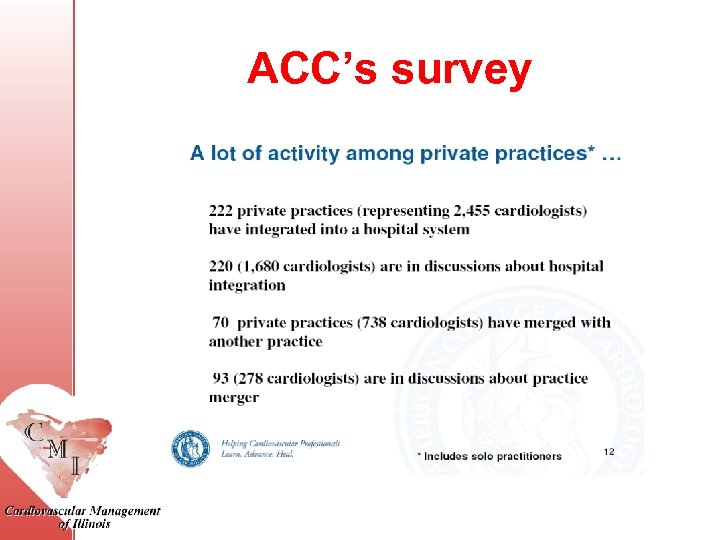 ACC’s survey
ACC’s survey
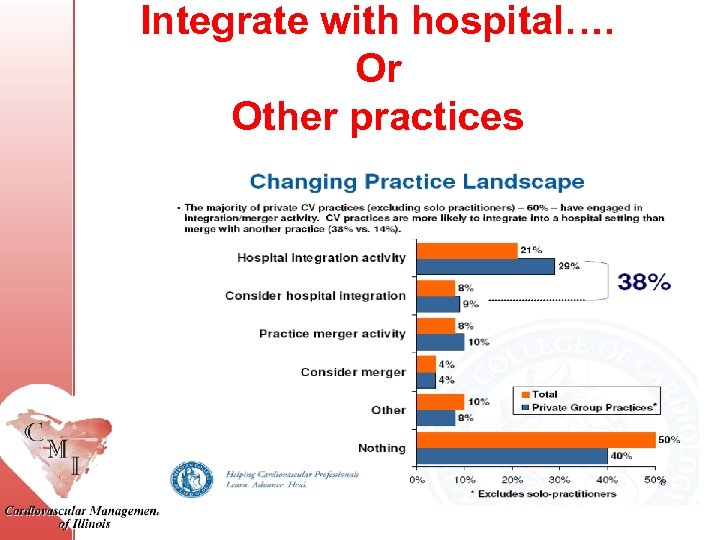 Integrate with hospital…. Or Other practices
Integrate with hospital…. Or Other practices
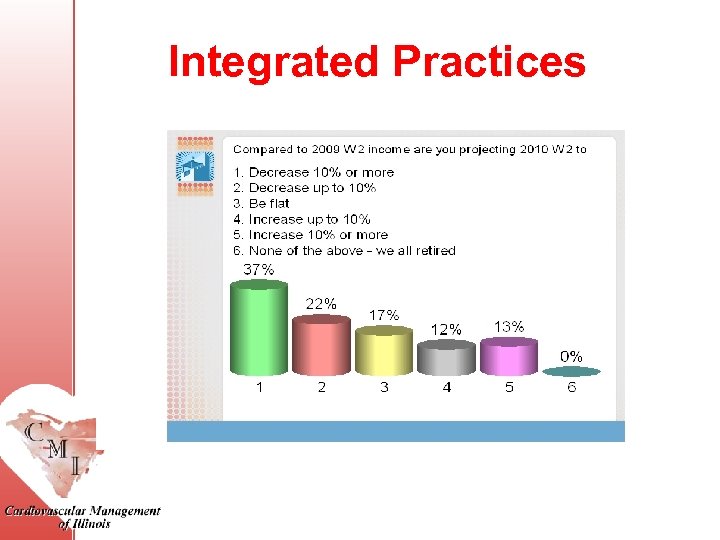 Integrated Practices
Integrated Practices
 ACO’s…. . • Rules due out in Jan • ACA attributes patients to ACOs (by virtue of the doctors and hospitals they currently use) --patients do not enroll in them. – This is confusing, because if patients do not want to be in an ACO and instead stay with their doctor who chooses not to participate, they may. But if their doctor is in, so is the patient. This issue may need to be amended somehow
ACO’s…. . • Rules due out in Jan • ACA attributes patients to ACOs (by virtue of the doctors and hospitals they currently use) --patients do not enroll in them. – This is confusing, because if patients do not want to be in an ACO and instead stay with their doctor who chooses not to participate, they may. But if their doctor is in, so is the patient. This issue may need to be amended somehow
 AUC…. . where is it going • Midei case in Baltimore – ACE from SCAI (accreditation for cardiovascular excellence) • JAMA article on ICD • FOCUS – nuclear • Lab accreditation – MIPPA – IAC – focus on use of AUC
AUC…. . where is it going • Midei case in Baltimore – ACE from SCAI (accreditation for cardiovascular excellence) • JAMA article on ICD • FOCUS – nuclear • Lab accreditation – MIPPA – IAC – focus on use of AUC
 Quality …where is it going? • Recent CMS report – 3 demo projects • Hospital Quality Incentive Demonstration (HQID) • the Physician Group Practice (PGP) • 500 small and solo physician practices participating in the Medicare Care Management Performance (MCMP – http: //www. cms. hhs. gov/Demo. Projects. Ev al. Rpts/MD/list. asp.
Quality …where is it going? • Recent CMS report – 3 demo projects • Hospital Quality Incentive Demonstration (HQID) • the Physician Group Practice (PGP) • 500 small and solo physician practices participating in the Medicare Care Management Performance (MCMP – http: //www. cms. hhs. gov/Demo. Projects. Ev al. Rpts/MD/list. asp.
 Physician Compare • • Public reporting of data Starts 1/1/13 Mandated by ACA Physicians need to be able to update their contact info • Comment period is now
Physician Compare • • Public reporting of data Starts 1/1/13 Mandated by ACA Physicians need to be able to update their contact info • Comment period is now
 Few more…. • Sunshine Act – 2012 – Anything over $10 will be reported • PECOS – CMS is working “diligently” – Edit not turned on for referring MD – NO DATE has been announced • Red Flag – finally gone
Few more…. • Sunshine Act – 2012 – Anything over $10 will be reported • PECOS – CMS is working “diligently” – Edit not turned on for referring MD – NO DATE has been announced • Red Flag – finally gone
 What is this “new” MOC • MOC = Maintenance of certification • Additional. 5% in PQRS payments if enrolled in MOC • Must submit PQRS data for 12 months, participate in MOC, and complete MOC practice assessment – FOCUS and CPIP
What is this “new” MOC • MOC = Maintenance of certification • Additional. 5% in PQRS payments if enrolled in MOC • Must submit PQRS data for 12 months, participate in MOC, and complete MOC practice assessment – FOCUS and CPIP
 PQRS aka PQRI • • • PVRP was initial program in 2006 PQRI - 7/1/07 – 1. 5% incentive payment 2008 – Few structural changes 2009 and 2010 - 2% incentive payment Yes you can do this + Meaningful use 2011 – Physician Quality Reporting System • 194 measures
PQRS aka PQRI • • • PVRP was initial program in 2006 PQRI - 7/1/07 – 1. 5% incentive payment 2008 – Few structural changes 2009 and 2010 - 2% incentive payment Yes you can do this + Meaningful use 2011 – Physician Quality Reporting System • 194 measures
 PQRS Resources A Guide for Understanding the 2011 Physician Quality Reporting System (PQRS) Incentive Payment • www. cms. gov/pqrs • https: //www. cms. gov/PQRI/15_Measures. Codes. a sp#Top. Of. Page • http: //www. cms. hhs. gov/Medicare. Provider. Sup. En roll • http: //www. cms. hhs. gov/IACS • https: //www. cms. gov/PQRI/30_Educational. Resou rces. asp#Top. Of. Page
PQRS Resources A Guide for Understanding the 2011 Physician Quality Reporting System (PQRS) Incentive Payment • www. cms. gov/pqrs • https: //www. cms. gov/PQRI/15_Measures. Codes. a sp#Top. Of. Page • http: //www. cms. hhs. gov/Medicare. Provider. Sup. En roll • http: //www. cms. hhs. gov/IACS • https: //www. cms. gov/PQRI/30_Educational. Resou rces. asp#Top. Of. Page
 Key Changes • • Penalties start in 2015 2011 – 1% payment 2012 – 2014 - 0. 5% payment Reporting sample reduced from 80% to 50% for claims ONLY – Registry still must meet 80% on 3 measures • Registries no longer can report on non. Medicare FFS • Measures with 0% will not be counted • New group reporting option <200 – 26 measures
Key Changes • • Penalties start in 2015 2011 – 1% payment 2012 – 2014 - 0. 5% payment Reporting sample reduced from 80% to 50% for claims ONLY – Registry still must meet 80% on 3 measures • Registries no longer can report on non. Medicare FFS • Measures with 0% will not be counted • New group reporting option <200 – 26 measures
 Changes to Structure and Function • • • In response to ACA Penalty: 1. 5% in 2015 & 2. 0% after Timely feedback Interim reports Informal appeal process Physician Compare Website – Reports 2012 PQRS • Integration with MU
Changes to Structure and Function • • • In response to ACA Penalty: 1. 5% in 2015 & 2. 0% after Timely feedback Interim reports Informal appeal process Physician Compare Website – Reports 2012 PQRS • Integration with MU
 Measures • 170 measures continue (24 new) • 45 registry measures continue – 11 new registry only • 14 Measure Groups • EHR current 10 + 10 new
Measures • 170 measures continue (24 new) • 45 registry measures continue – 11 new registry only • 14 Measure Groups • EHR current 10 + 10 new
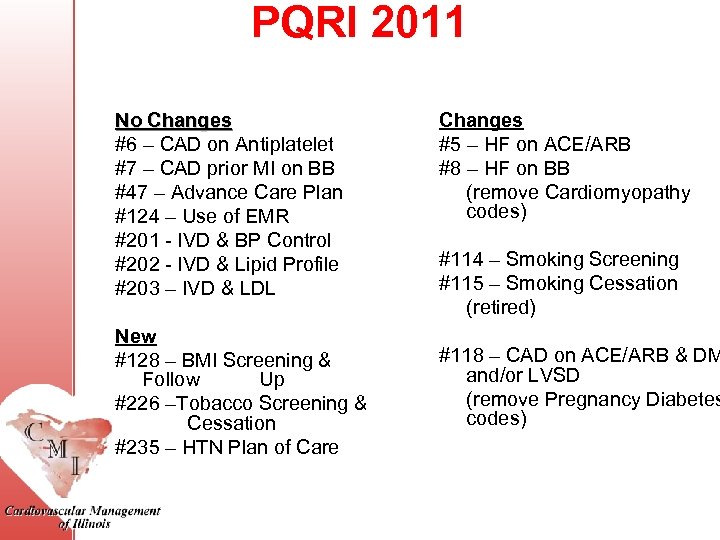 PQRI 2011 No Changes #6 – CAD on Antiplatelet #7 – CAD prior MI on BB #47 – Advance Care Plan #124 – Use of EMR #201 - IVD & BP Control #202 - IVD & Lipid Profile #203 – IVD & LDL New #128 – BMI Screening & Follow Up #226 –Tobacco Screening & Cessation #235 – HTN Plan of Care Changes #5 – HF on ACE/ARB #8 – HF on BB (remove Cardiomyopathy codes) #114 – Smoking Screening #115 – Smoking Cessation (retired) #118 – CAD on ACE/ARB & DM and/or LVSD (remove Pregnancy Diabetes codes)
PQRI 2011 No Changes #6 – CAD on Antiplatelet #7 – CAD prior MI on BB #47 – Advance Care Plan #124 – Use of EMR #201 - IVD & BP Control #202 - IVD & Lipid Profile #203 – IVD & LDL New #128 – BMI Screening & Follow Up #226 –Tobacco Screening & Cessation #235 – HTN Plan of Care Changes #5 – HF on ACE/ARB #8 – HF on BB (remove Cardiomyopathy codes) #114 – Smoking Screening #115 – Smoking Cessation (retired) #118 – CAD on ACE/ARB & DM and/or LVSD (remove Pregnancy Diabetes codes)
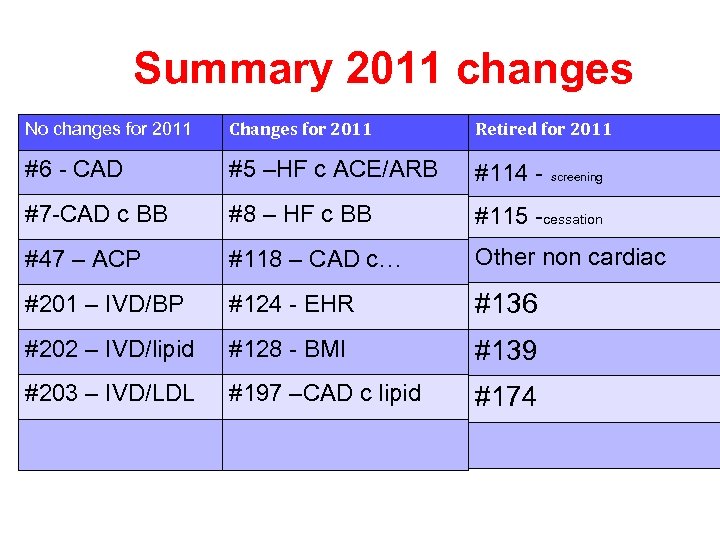 Summary 2011 changes No changes for 2011 Changes for 2011 Retired for 2011 #6 - CAD #5 –HF c ACE/ARB #114 - screening #7 -CAD c BB #8 – HF c BB #115 -cessation #47 – ACP #118 – CAD c… Other non cardiac #201 – IVD/BP #124 - EHR #136 #202 – IVD/lipid #128 - BMI #139 #203 – IVD/LDL #197 –CAD c lipid #174
Summary 2011 changes No changes for 2011 Changes for 2011 Retired for 2011 #6 - CAD #5 –HF c ACE/ARB #114 - screening #7 -CAD c BB #8 – HF c BB #115 -cessation #47 – ACP #118 – CAD c… Other non cardiac #201 – IVD/BP #124 - EHR #136 #202 – IVD/lipid #128 - BMI #139 #203 – IVD/LDL #197 –CAD c lipid #174
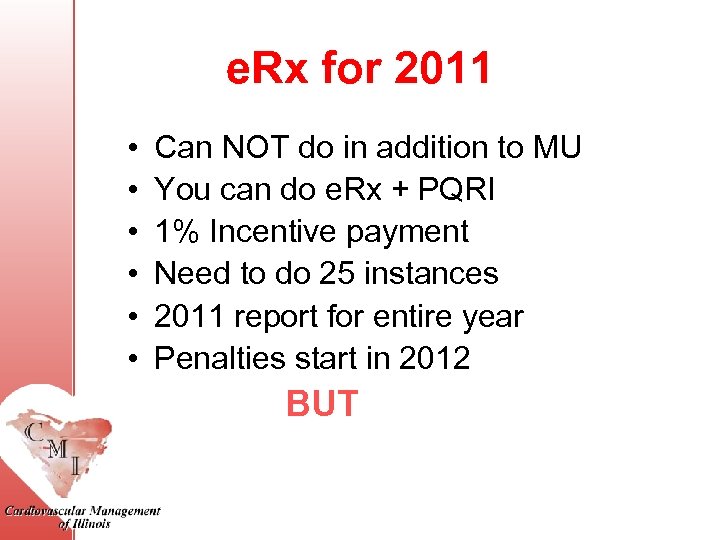 e. Rx for 2011 • • • Can NOT do in addition to MU You can do e. Rx + PQRI 1% Incentive payment Need to do 25 instances 2011 report for entire year Penalties start in 2012 BUT
e. Rx for 2011 • • • Can NOT do in addition to MU You can do e. Rx + PQRI 1% Incentive payment Need to do 25 instances 2011 report for entire year Penalties start in 2012 BUT
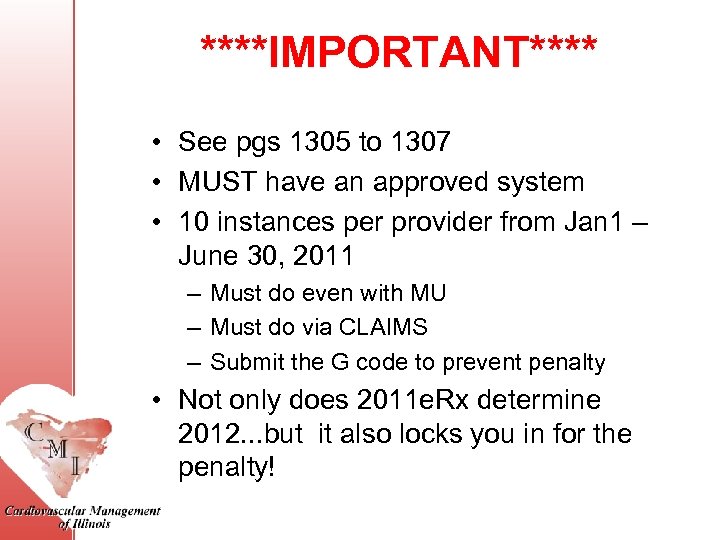 ****IMPORTANT**** • See pgs 1305 to 1307 • MUST have an approved system • 10 instances per provider from Jan 1 – June 30, 2011 – Must do even with MU – Must do via CLAIMS – Submit the G code to prevent penalty • Not only does 2011 e. Rx determine 2012. . . but it also locks you in for the penalty!
****IMPORTANT**** • See pgs 1305 to 1307 • MUST have an approved system • 10 instances per provider from Jan 1 – June 30, 2011 – Must do even with MU – Must do via CLAIMS – Submit the G code to prevent penalty • Not only does 2011 e. Rx determine 2012. . . but it also locks you in for the penalty!
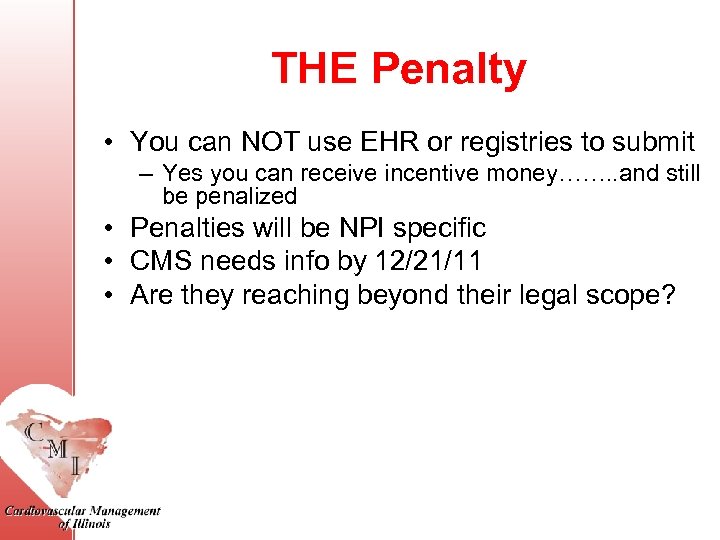 THE Penalty • You can NOT use EHR or registries to submit – Yes you can receive incentive money……. . and still be penalized • Penalties will be NPI specific • CMS needs info by 12/21/11 • Are they reaching beyond their legal scope?
THE Penalty • You can NOT use EHR or registries to submit – Yes you can receive incentive money……. . and still be penalized • Penalties will be NPI specific • CMS needs info by 12/21/11 • Are they reaching beyond their legal scope?
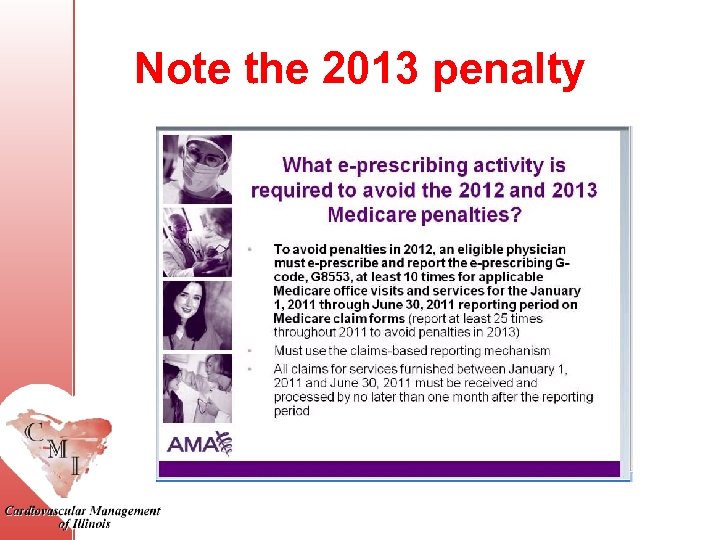 Note the 2013 penalty
Note the 2013 penalty
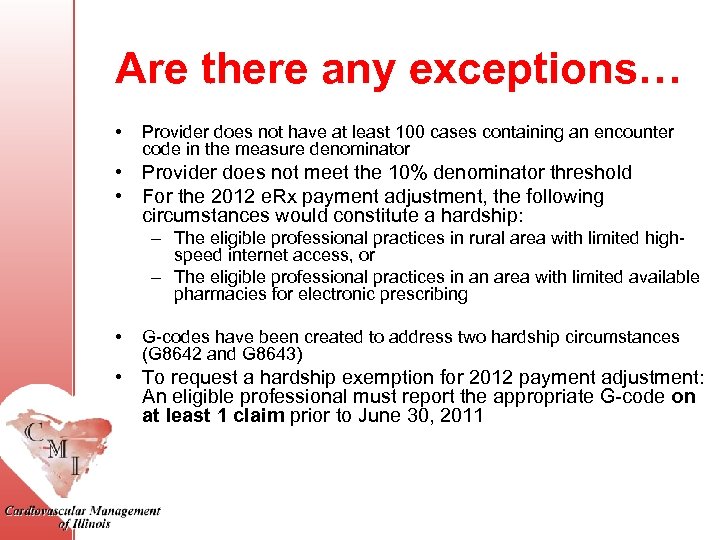 Are there any exceptions… • Provider does not have at least 100 cases containing an encounter code in the measure denominator • Provider does not meet the 10% denominator threshold • For the 2012 e. Rx payment adjustment, the following circumstances would constitute a hardship: – The eligible professional practices in rural area with limited highspeed internet access, or – The eligible professional practices in an area with limited available pharmacies for electronic prescribing • G-codes have been created to address two hardship circumstances (G 8642 and G 8643) • To request a hardship exemption for 2012 payment adjustment: An eligible professional must report the appropriate G-code on at least 1 claim prior to June 30, 2011
Are there any exceptions… • Provider does not have at least 100 cases containing an encounter code in the measure denominator • Provider does not meet the 10% denominator threshold • For the 2012 e. Rx payment adjustment, the following circumstances would constitute a hardship: – The eligible professional practices in rural area with limited highspeed internet access, or – The eligible professional practices in an area with limited available pharmacies for electronic prescribing • G-codes have been created to address two hardship circumstances (G 8642 and G 8643) • To request a hardship exemption for 2012 payment adjustment: An eligible professional must report the appropriate G-code on at least 1 claim prior to June 30, 2011
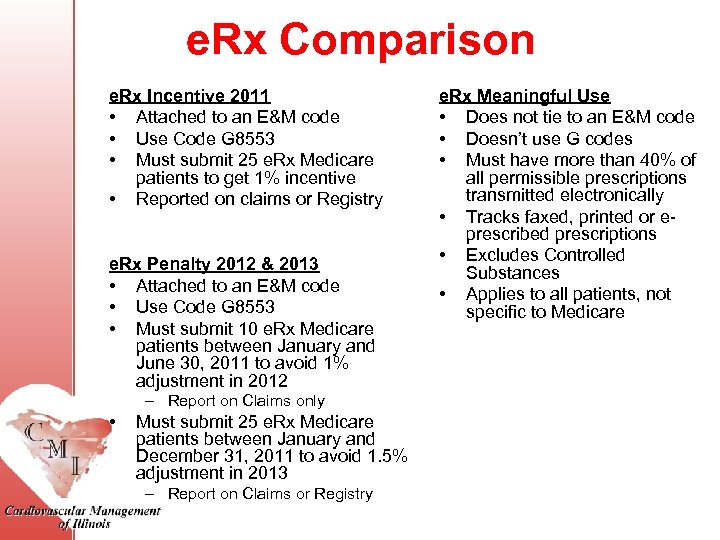 e. Rx Comparison e. Rx Incentive 2011 • Attached to an E&M code • Use Code G 8553 • Must submit 25 e. Rx Medicare patients to get 1% incentive • Reported on claims or Registry e. Rx Penalty 2012 & 2013 • Attached to an E&M code • Use Code G 8553 • Must submit 10 e. Rx Medicare patients between January and June 30, 2011 to avoid 1% adjustment in 2012 – Report on Claims only • Must submit 25 e. Rx Medicare patients between January and December 31, 2011 to avoid 1. 5% adjustment in 2013 – Report on Claims or Registry e. Rx Meaningful Use • Does not tie to an E&M code • Doesn’t use G codes • Must have more than 40% of all permissible prescriptions transmitted electronically • Tracks faxed, printed or eprescribed prescriptions • Excludes Controlled Substances • Applies to all patients, not specific to Medicare
e. Rx Comparison e. Rx Incentive 2011 • Attached to an E&M code • Use Code G 8553 • Must submit 25 e. Rx Medicare patients to get 1% incentive • Reported on claims or Registry e. Rx Penalty 2012 & 2013 • Attached to an E&M code • Use Code G 8553 • Must submit 10 e. Rx Medicare patients between January and June 30, 2011 to avoid 1% adjustment in 2012 – Report on Claims only • Must submit 25 e. Rx Medicare patients between January and December 31, 2011 to avoid 1. 5% adjustment in 2013 – Report on Claims or Registry e. Rx Meaningful Use • Does not tie to an E&M code • Doesn’t use G codes • Must have more than 40% of all permissible prescriptions transmitted electronically • Tracks faxed, printed or eprescribed prescriptions • Excludes Controlled Substances • Applies to all patients, not specific to Medicare
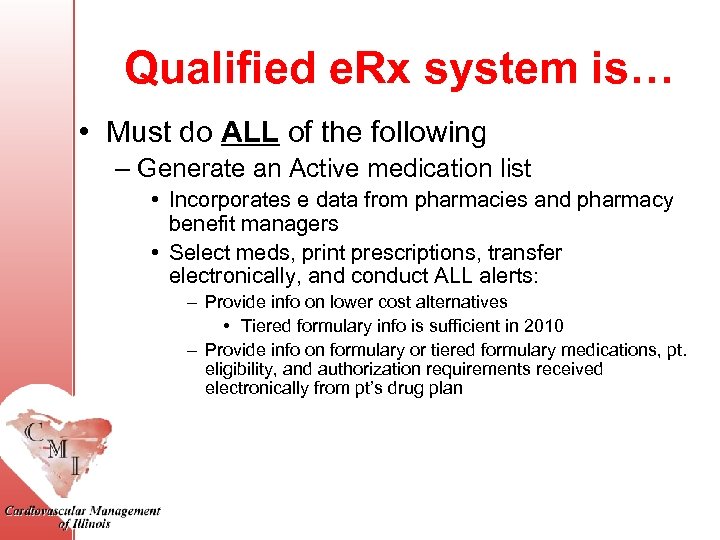 Qualified e. Rx system is… • Must do ALL of the following – Generate an Active medication list • Incorporates e data from pharmacies and pharmacy benefit managers • Select meds, print prescriptions, transfer electronically, and conduct ALL alerts: – Provide info on lower cost alternatives • Tiered formulary info is sufficient in 2010 – Provide info on formulary or tiered formulary medications, pt. eligibility, and authorization requirements received electronically from pt’s drug plan
Qualified e. Rx system is… • Must do ALL of the following – Generate an Active medication list • Incorporates e data from pharmacies and pharmacy benefit managers • Select meds, print prescriptions, transfer electronically, and conduct ALL alerts: – Provide info on lower cost alternatives • Tiered formulary info is sufficient in 2010 – Provide info on formulary or tiered formulary medications, pt. eligibility, and authorization requirements received electronically from pt’s drug plan
 Lessons learned • Remember the 10% rule • Don’t forget mid levels • How penalty will be applied… www. cms. gov/erxincentive
Lessons learned • Remember the 10% rule • Don’t forget mid levels • How penalty will be applied… www. cms. gov/erxincentive
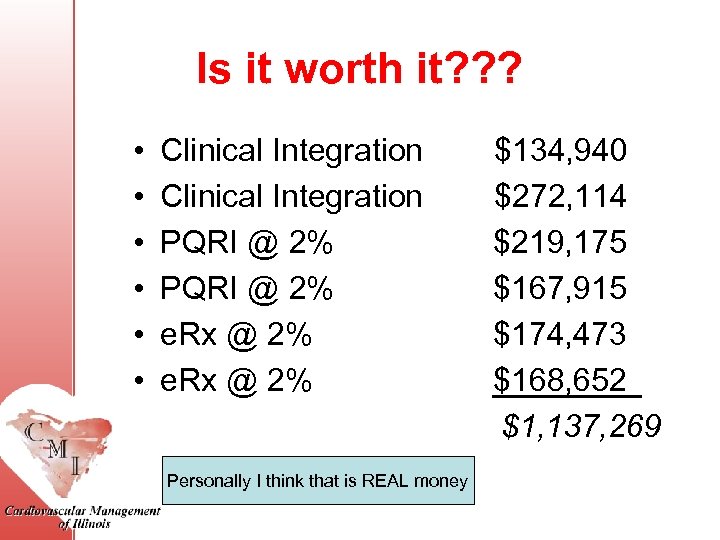 Is it worth it? ? ? • • • Clinical Integration $134, 940 Clinical Integration $272, 114 PQRI @ 2% $219, 175 PQRI @ 2% $167, 915 e. Rx @ 2% $174, 473 e. Rx @ 2% $168, 652 $1, 137, 269 Personally I think that is REAL money
Is it worth it? ? ? • • • Clinical Integration $134, 940 Clinical Integration $272, 114 PQRI @ 2% $219, 175 PQRI @ 2% $167, 915 e. Rx @ 2% $174, 473 e. Rx @ 2% $168, 652 $1, 137, 269 Personally I think that is REAL money
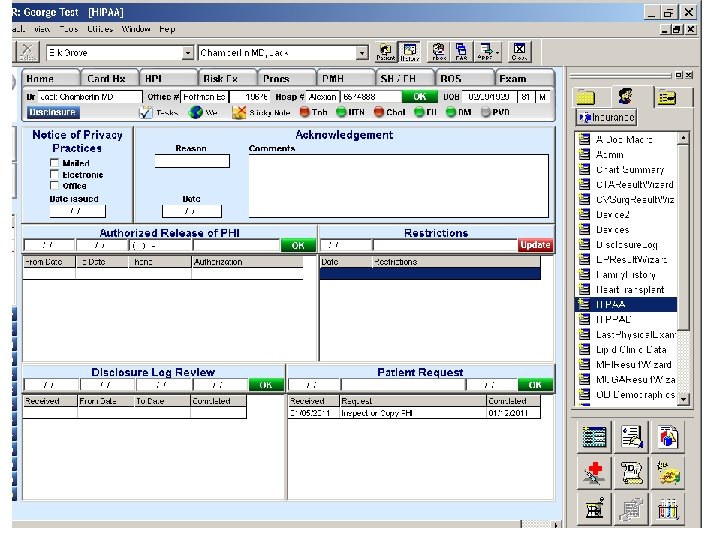
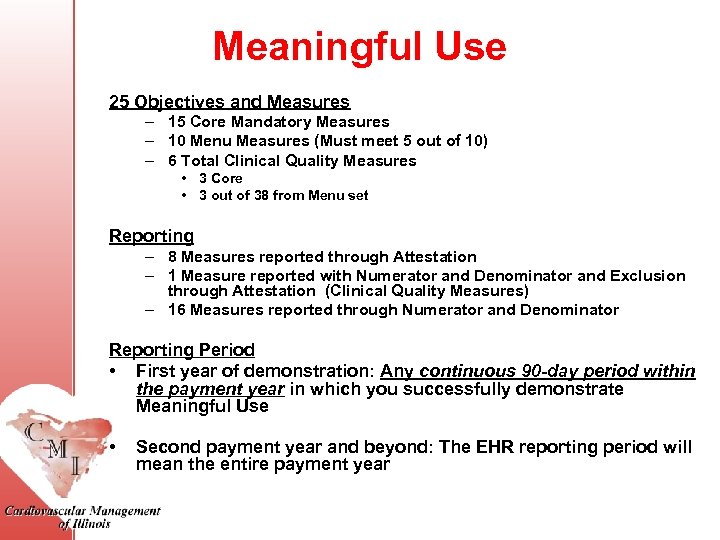 Meaningful Use 25 Objectives and Measures – 15 Core Mandatory Measures – 10 Menu Measures (Must meet 5 out of 10) – 6 Total Clinical Quality Measures • 3 Core • 3 out of 38 from Menu set Reporting – 8 Measures reported through Attestation – 1 Measure reported with Numerator and Denominator and Exclusion through Attestation (Clinical Quality Measures) – 16 Measures reported through Numerator and Denominator Reporting Period • First year of demonstration: Any continuous 90 -day period within the payment year in which you successfully demonstrate Meaningful Use • Second payment year and beyond: The EHR reporting period will mean the entire payment year
Meaningful Use 25 Objectives and Measures – 15 Core Mandatory Measures – 10 Menu Measures (Must meet 5 out of 10) – 6 Total Clinical Quality Measures • 3 Core • 3 out of 38 from Menu set Reporting – 8 Measures reported through Attestation – 1 Measure reported with Numerator and Denominator and Exclusion through Attestation (Clinical Quality Measures) – 16 Measures reported through Numerator and Denominator Reporting Period • First year of demonstration: Any continuous 90 -day period within the payment year in which you successfully demonstrate Meaningful Use • Second payment year and beyond: The EHR reporting period will mean the entire payment year
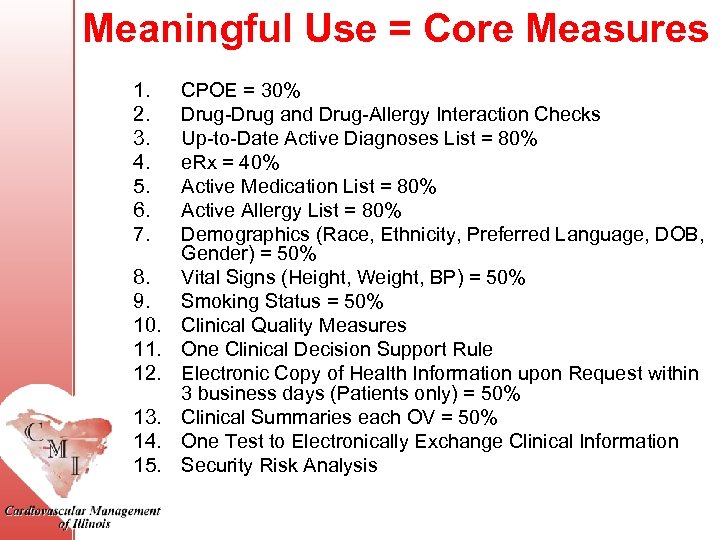 Meaningful Use = Core Measures 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. CPOE = 30% Drug-Drug and Drug-Allergy Interaction Checks Up-to-Date Active Diagnoses List = 80% e. Rx = 40% Active Medication List = 80% Active Allergy List = 80% Demographics (Race, Ethnicity, Preferred Language, DOB, Gender) = 50% Vital Signs (Height, Weight, BP) = 50% Smoking Status = 50% Clinical Quality Measures One Clinical Decision Support Rule Electronic Copy of Health Information upon Request within 3 business days (Patients only) = 50% Clinical Summaries each OV = 50% One Test to Electronically Exchange Clinical Information Security Risk Analysis
Meaningful Use = Core Measures 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. CPOE = 30% Drug-Drug and Drug-Allergy Interaction Checks Up-to-Date Active Diagnoses List = 80% e. Rx = 40% Active Medication List = 80% Active Allergy List = 80% Demographics (Race, Ethnicity, Preferred Language, DOB, Gender) = 50% Vital Signs (Height, Weight, BP) = 50% Smoking Status = 50% Clinical Quality Measures One Clinical Decision Support Rule Electronic Copy of Health Information upon Request within 3 business days (Patients only) = 50% Clinical Summaries each OV = 50% One Test to Electronically Exchange Clinical Information Security Risk Analysis
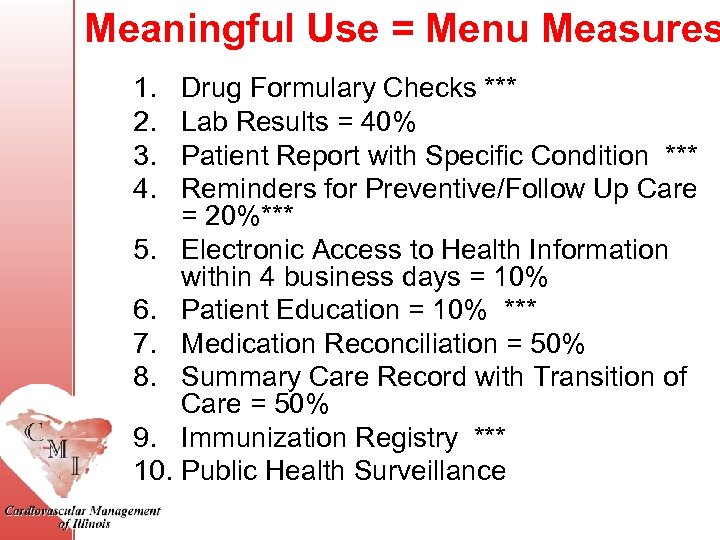 Meaningful Use = Menu Measures 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Drug Formulary Checks *** Lab Results = 40% Patient Report with Specific Condition *** Reminders for Preventive/Follow Up Care = 20%*** Electronic Access to Health Information within 4 business days = 10% Patient Education = 10% *** Medication Reconciliation = 50% Summary Care Record with Transition of Care = 50% Immunization Registry *** Public Health Surveillance
Meaningful Use = Menu Measures 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Drug Formulary Checks *** Lab Results = 40% Patient Report with Specific Condition *** Reminders for Preventive/Follow Up Care = 20%*** Electronic Access to Health Information within 4 business days = 10% Patient Education = 10% *** Medication Reconciliation = 50% Summary Care Record with Transition of Care = 50% Immunization Registry *** Public Health Surveillance
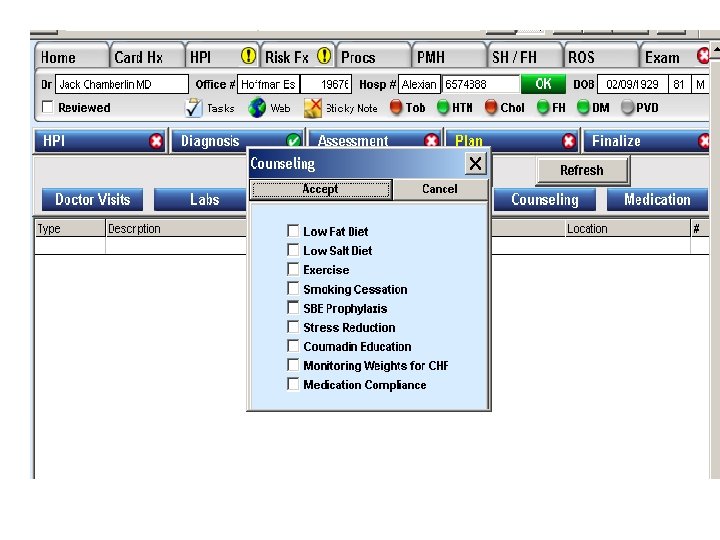
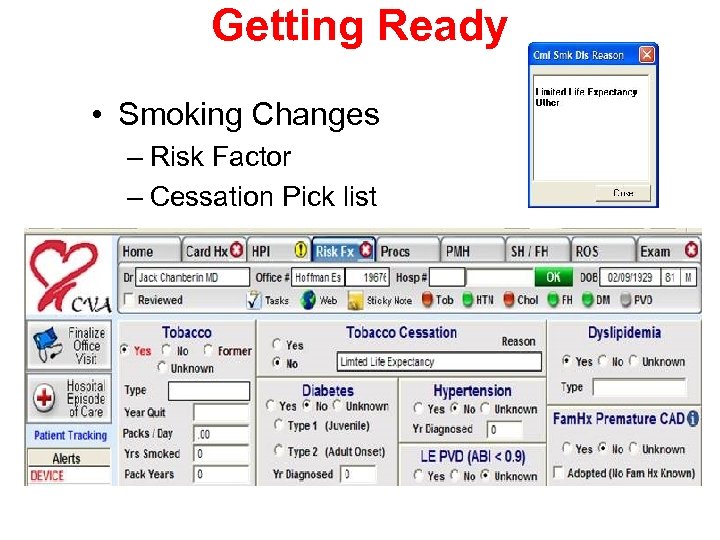 Getting Ready • Smoking Changes – Risk Factor – Cessation Pick list
Getting Ready • Smoking Changes – Risk Factor – Cessation Pick list
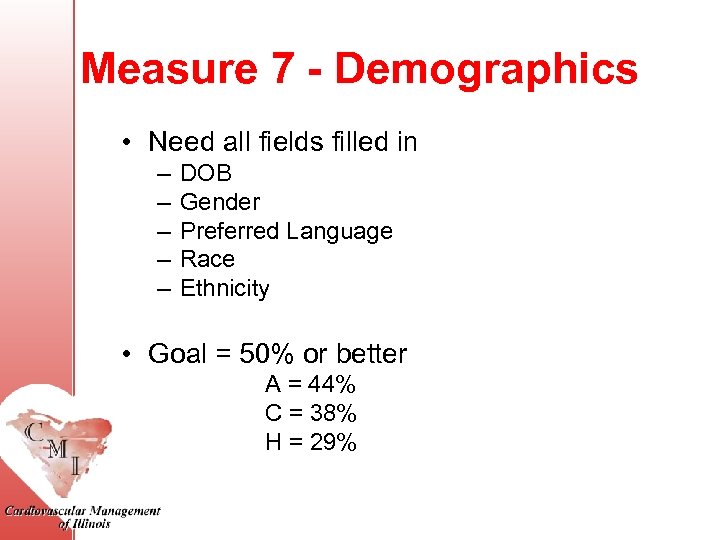 Measure 7 - Demographics • Need all fields filled in – – – DOB Gender Preferred Language Race Ethnicity • Goal = 50% or better A = 44% C = 38% H = 29%
Measure 7 - Demographics • Need all fields filled in – – – DOB Gender Preferred Language Race Ethnicity • Goal = 50% or better A = 44% C = 38% H = 29%
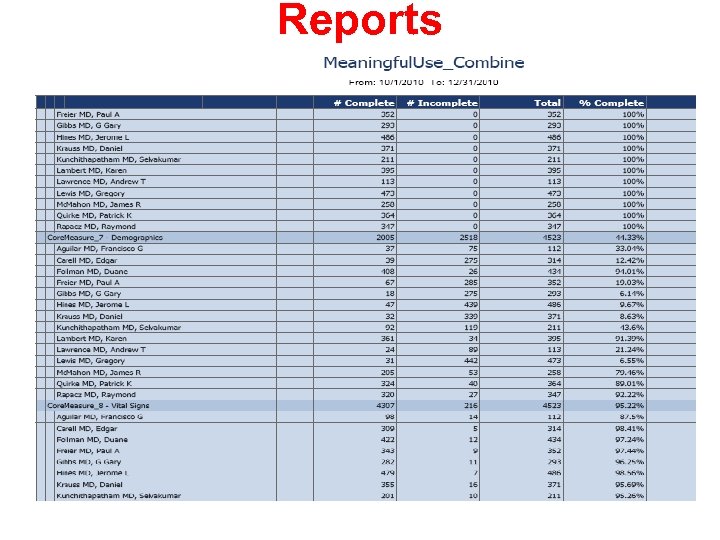 Reports
Reports
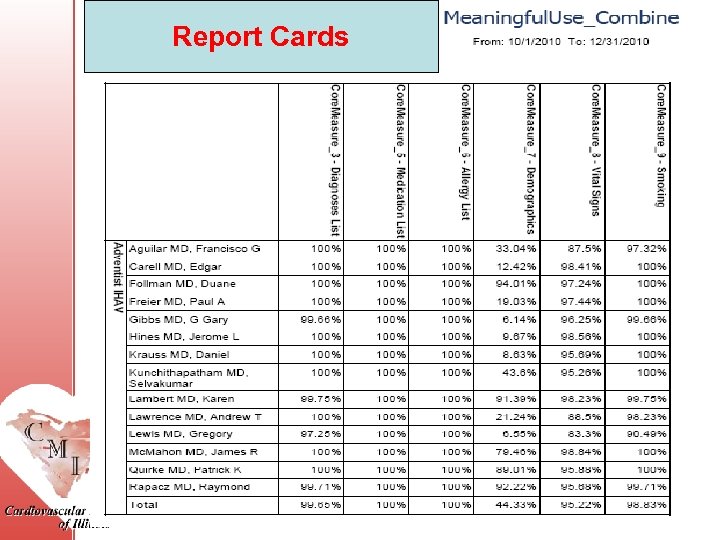 Report Cards
Report Cards
 THANK YOU QUESTIONS? ? ?
THANK YOU QUESTIONS? ? ?


