3772e8d56ba978d49745e6e9edfbde27.ppt
- Количество слайдов: 34

 Prenatal care Dr. F Mostajeran
Prenatal care Dr. F Mostajeran
 Prenatal care PNC n 1915 10000 consecutive deliveries n 40% of prenatal death prevented by PNC n 1945 organized PNC “more to save mother”
Prenatal care PNC n 1915 10000 consecutive deliveries n 40% of prenatal death prevented by PNC n 1945 organized PNC “more to save mother”
 In adequate PNC Kessner index n Measuring adequacy PNC n Recorded on birth certificate n Length gestation, time first PNC, number of visits n It does not measure quality not consider relative risk of mother 2000 12% American women inadequate PNC n
In adequate PNC Kessner index n Measuring adequacy PNC n Recorded on birth certificate n Length gestation, time first PNC, number of visits n It does not measure quality not consider relative risk of mother 2000 12% American women inadequate PNC n
 n 2000 50% delayed or no PNC n Reason cited (social, ethnic group, age, method of pyment) 1. Women did not know she was pregnant 2. Lack of money or insurance 3. Inability to obtain an appointement
n 2000 50% delayed or no PNC n Reason cited (social, ethnic group, age, method of pyment) 1. Women did not know she was pregnant 2. Lack of money or insurance 3. Inability to obtain an appointement
 Effectiveness of prenatal care past several decades no benefit n ↑ low birth weight n ↑ preterm labor (2 fold) n 1992 compared the cost an benifit PNC n 12000 patient missouri each$ spent PNC n Savings %1. 49 in newborn and postpartum costs
Effectiveness of prenatal care past several decades no benefit n ↑ low birth weight n ↑ preterm labor (2 fold) n 1992 compared the cost an benifit PNC n 12000 patient missouri each$ spent PNC n Savings %1. 49 in newborn and postpartum costs
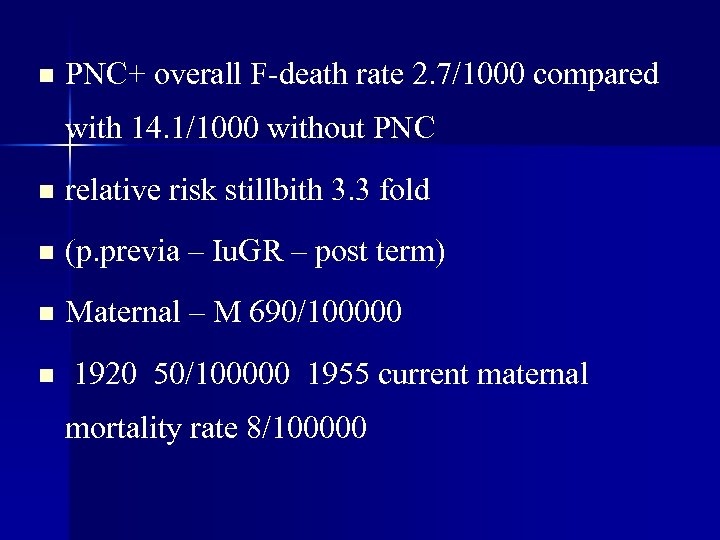 n PNC+ overall F-death rate 2. 7/1000 compared with 14. 1/1000 without PNC n relative risk stillbith 3. 3 fold n (p. previa – Iu. GR – post term) n Maternal – M 690/100000 n 1920 50/100000 1955 current maternal mortality rate 8/100000
n PNC+ overall F-death rate 2. 7/1000 compared with 14. 1/1000 without PNC n relative risk stillbith 3. 3 fold n (p. previa – Iu. GR – post term) n Maternal – M 690/100000 n 1920 50/100000 1955 current maternal mortality rate 8/100000
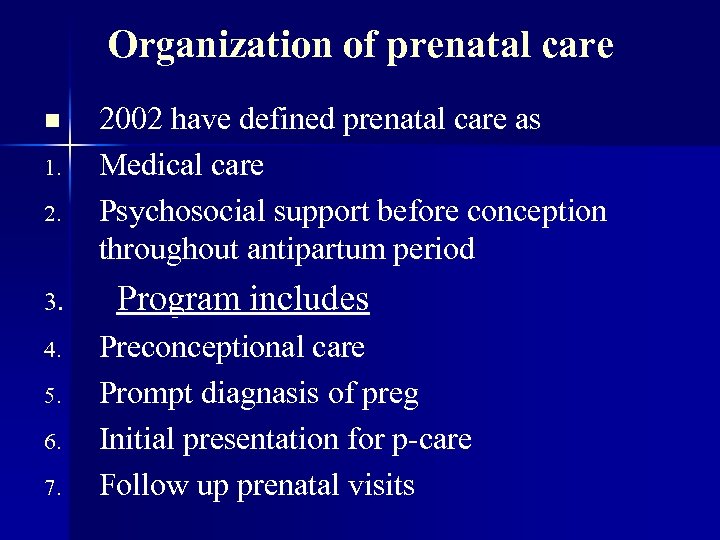 Organization of prenatal care n 1. 2. 3. 4. 5. 6. 7. 2002 have defined prenatal care as Medical care Psychosocial support before conception throughout antipartum period Program includes Preconceptional care Prompt diagnasis of preg Initial presentation for p-care Follow up prenatal visits
Organization of prenatal care n 1. 2. 3. 4. 5. 6. 7. 2002 have defined prenatal care as Medical care Psychosocial support before conception throughout antipartum period Program includes Preconceptional care Prompt diagnasis of preg Initial presentation for p-care Follow up prenatal visits
 Initial prenatal evaluation major goals are 1. To define health status mother-fetus 2. Gestational age of the fetus 3. Initiate a plan for continuing obstetrical care
Initial prenatal evaluation major goals are 1. To define health status mother-fetus 2. Gestational age of the fetus 3. Initiate a plan for continuing obstetrical care
 Prenatal record History n Physical Ex n Laboratory tests n Nulligravida: n Not now and never has been pregnant n
Prenatal record History n Physical Ex n Laboratory tests n Nulligravida: n Not now and never has been pregnant n
 n n n n Gravida who is or has been pregnant primigravida – multi Nullipara who has never completed a prey begound 20 wk P± Primipara who has been delivered once fetus or fetvses alive or dead begon 20 wk Multipara two or more pregnancy completed after 20 wk
n n n n Gravida who is or has been pregnant primigravida – multi Nullipara who has never completed a prey begound 20 wk P± Primipara who has been delivered once fetus or fetvses alive or dead begon 20 wk Multipara two or more pregnancy completed after 20 wk
 Normal pregnancy duration n Lmp 280 days 40 wk n Expected date of delivery (Naogele role) n First trimester 14 wk n Second trimester through 28 wk n Third trimester 29 -42
Normal pregnancy duration n Lmp 280 days 40 wk n Expected date of delivery (Naogele role) n First trimester 14 wk n Second trimester through 28 wk n Third trimester 29 -42
 History detailed information past obstetrical history complication tend to recur in subsequent preg n Menstrual history n Regular mens – oligomenorrhea n OCP n
History detailed information past obstetrical history complication tend to recur in subsequent preg n Menstrual history n Regular mens – oligomenorrhea n OCP n
 Psychosocial screening n Cigarette smoking 1. Spontaneous abortion 2. LBW due to PTL or IUGR 3. Infant and fetal death 4. P. abruption
Psychosocial screening n Cigarette smoking 1. Spontaneous abortion 2. LBW due to PTL or IUGR 3. Infant and fetal death 4. P. abruption
 Pathophysiologycal mechanism n Increased fetal carbonxhemoglobin n ↓ utero placental blood flow n Fetal hyponxia
Pathophysiologycal mechanism n Increased fetal carbonxhemoglobin n ↓ utero placental blood flow n Fetal hyponxia
 Alcohol Potent teratogen F-alcohol syn n Growth restriction n Facial abnormalities n CNS disfunction n
Alcohol Potent teratogen F-alcohol syn n Growth restriction n Facial abnormalities n CNS disfunction n
 n Chronic VSC or lange quantities illicit drugs including opium barbiturates amphetamines n F- distress, LBW drug withdrawal
n Chronic VSC or lange quantities illicit drugs including opium barbiturates amphetamines n F- distress, LBW drug withdrawal
 Physical Examination n General physical Exam at initial PNC n Pelvic exam n Lubricated speculum warm water n Bluish-red passive hyperemia n Nabathian cysts n Identify cytological abnor pap smear n Specimens Identification neisseria gonorrhea n Chlamydia trachomatis
Physical Examination n General physical Exam at initial PNC n Pelvic exam n Lubricated speculum warm water n Bluish-red passive hyperemia n Nabathian cysts n Identify cytological abnor pap smear n Specimens Identification neisseria gonorrhea n Chlamydia trachomatis
 Digital P. EX n Consistency length dilatation cervix n Presentation fetus n Bony architecture pelvis n Anomaly vagina perineum cystocle rectocele
Digital P. EX n Consistency length dilatation cervix n Presentation fetus n Bony architecture pelvis n Anomaly vagina perineum cystocle rectocele
 Subsequent prenatal visits n Traditionally timing subsequent PN visits n Interval 4 wk until 28 wk n Then every 2 wk until 36 wk thereafter weekly n Complicated pregnancy 1 to 2 wk intervals
Subsequent prenatal visits n Traditionally timing subsequent PN visits n Interval 4 wk until 28 wk n Then every 2 wk until 36 wk thereafter weekly n Complicated pregnancy 1 to 2 wk intervals
 Prenatal surveillance n To determine well-being mother and fetus n Fetal n Heart rate n Size current – rate of change n AF n n Presentation Activity
Prenatal surveillance n To determine well-being mother and fetus n Fetal n Heart rate n Size current – rate of change n AF n n Presentation Activity
 Maternal n BP change n Weight change n n n symptoms headache, altered vision, ab-pain vomiting, bleeding, vaginal fluid leakage dysuria Height uterine fondues V. E lat in prey (present, station, dilatation, effacement p-capacity)
Maternal n BP change n Weight change n n n symptoms headache, altered vision, ab-pain vomiting, bleeding, vaginal fluid leakage dysuria Height uterine fondues V. E lat in prey (present, station, dilatation, effacement p-capacity)
 Assessment gestational age n LMP F. height (20 -31) 34 wk n Fetal Heart sounds 16 -19 wk Delee fetal stethoscope n n ultra sound Between 8 and 16 wk slightly more accurate
Assessment gestational age n LMP F. height (20 -31) 34 wk n Fetal Heart sounds 16 -19 wk Delee fetal stethoscope n n ultra sound Between 8 and 16 wk slightly more accurate
 n Lab test n Hct hb blood type AR factor n Antibody screen n u/c u/a FBS n Pap smear
n Lab test n Hct hb blood type AR factor n Antibody screen n u/c u/a FBS n Pap smear
 Subsequent lab tests n Maternal serum 15 -20 NTD and chramosomal anomalies n MSAF free B HCG E 2 inhebin A n Syphilis serology n Cystic fibrosis
Subsequent lab tests n Maternal serum 15 -20 NTD and chramosomal anomalies n MSAF free B HCG E 2 inhebin A n Syphilis serology n Cystic fibrosis
 Ancillary prenatal tests n n n Gestational diabetes 24 -28 wk Ghlamydial infection n Group BS infection n Gonococcal infection n Ac OG 2002 centers for disease contral recommend vaginal and rectal GBS cultures in all women 35 to 37 wk if + intrapartum antimicrobial praphylanis n GBS bacteriuria n Previous infant with invasive disease
Ancillary prenatal tests n n n Gestational diabetes 24 -28 wk Ghlamydial infection n Group BS infection n Gonococcal infection n Ac OG 2002 centers for disease contral recommend vaginal and rectal GBS cultures in all women 35 to 37 wk if + intrapartum antimicrobial praphylanis n GBS bacteriuria n Previous infant with invasive disease
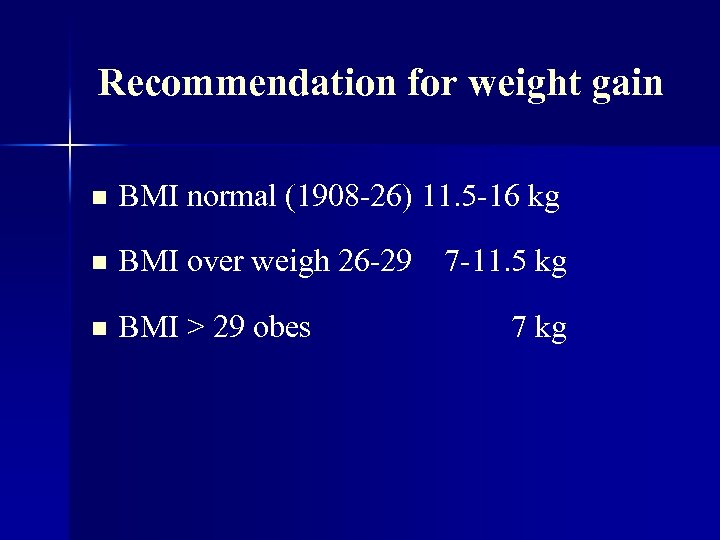 Recommendation for weight gain n BMI normal (1908 -26) 11. 5 -16 kg n BMI over weigh 26 -29 7 -11. 5 kg n BMI > 29 obes 7 kg
Recommendation for weight gain n BMI normal (1908 -26) 11. 5 -16 kg n BMI over weigh 26 -29 7 -11. 5 kg n BMI > 29 obes 7 kg
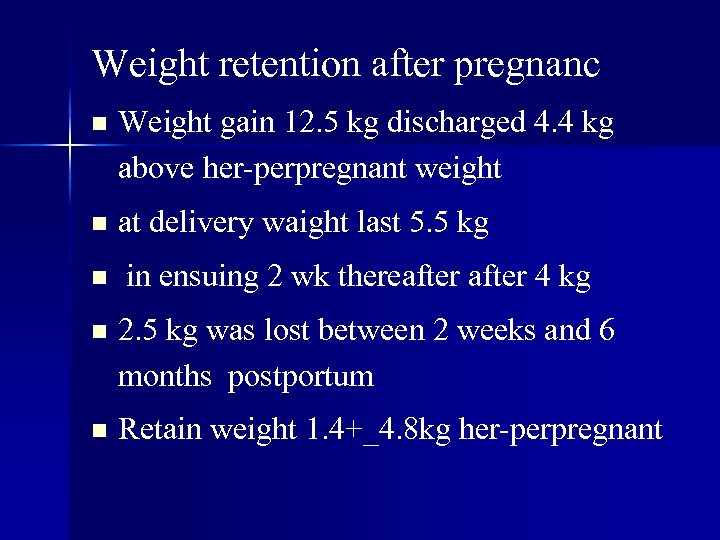 Weight retention after pregnanc n Weight gain 12. 5 kg discharged 4. 4 kg above her-perpregnant weight n at delivery waight last 5. 5 kg n in ensuing 2 wk thereafter 4 kg n 2. 5 kg was lost between 2 weeks and 6 months postportum n Retain weight 1. 4+_4. 8 kg her-perpregnant
Weight retention after pregnanc n Weight gain 12. 5 kg discharged 4. 4 kg above her-perpregnant weight n at delivery waight last 5. 5 kg n in ensuing 2 wk thereafter 4 kg n 2. 5 kg was lost between 2 weeks and 6 months postportum n Retain weight 1. 4+_4. 8 kg her-perpregnant
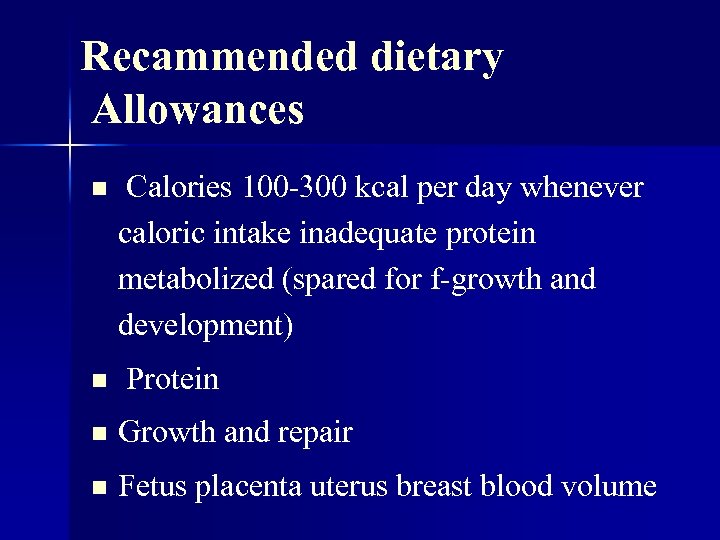 Recammended dietary Allowances n n Calories 100 -300 kcal per day whenever caloric intake inadequate protein metabolized (spared for f-growth and development) Protein n Growth and repair n Fetus placenta uterus breast blood volume
Recammended dietary Allowances n n Calories 100 -300 kcal per day whenever caloric intake inadequate protein metabolized (spared for f-growth and development) Protein n Growth and repair n Fetus placenta uterus breast blood volume
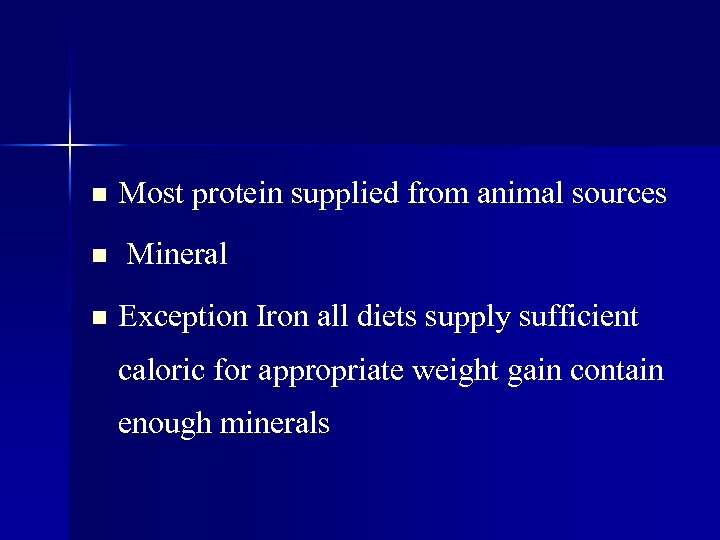 n n n Most protein supplied from animal sources Mineral Exception Iron all diets supply sufficient caloric for appropriate weight gain contain enough minerals
n n n Most protein supplied from animal sources Mineral Exception Iron all diets supply sufficient caloric for appropriate weight gain contain enough minerals
 Iron n 300 mg Iron trans ferred tofetus placenta 500 mg expanding M Hb mass nearly all is used after mid pregnancy n diet seldom contains enough iron to meet this demand recommended at least 27 mg ferrous iron supplement daily n This amount is contained in most prenatal vitamins n If she is large , twin fetuses, begin late in pregnancy or has depressed Hb level benefit from 60 -100 mg first for months of pregnancy not necessary
Iron n 300 mg Iron trans ferred tofetus placenta 500 mg expanding M Hb mass nearly all is used after mid pregnancy n diet seldom contains enough iron to meet this demand recommended at least 27 mg ferrous iron supplement daily n This amount is contained in most prenatal vitamins n If she is large , twin fetuses, begin late in pregnancy or has depressed Hb level benefit from 60 -100 mg first for months of pregnancy not necessary
 vitamins n Usually supplied by general diet provides adequate calories protein n Exception folic and during times of un usual requirements vomiting, hemolytic anemia or multiple fetuses
vitamins n Usually supplied by general diet provides adequate calories protein n Exception folic and during times of un usual requirements vomiting, hemolytic anemia or multiple fetuses
 Folic acid n 4000 pregnancy affected by NTD each year > 50 y prevented daily 400 Ng preconception recurrent NTD 3100 n 4 mg daily folic acid for the month before and 3 month after preg.
Folic acid n 4000 pregnancy affected by NTD each year > 50 y prevented daily 400 Ng preconception recurrent NTD 3100 n 4 mg daily folic acid for the month before and 3 month after preg.



