Headache and Pregnancy.ppt
- Количество слайдов: 28
 Pregnancy and Headache Adrian Fawcett MD Ph. D PGY 3 Neurology
Pregnancy and Headache Adrian Fawcett MD Ph. D PGY 3 Neurology
 Outline Case Presentation Multiple Choice Questions Epidemiology of Headache and Pregnancy Evidence Case Epilogue Multiple Choice Answers
Outline Case Presentation Multiple Choice Questions Epidemiology of Headache and Pregnancy Evidence Case Epilogue Multiple Choice Answers
 Multiple Choice Question # 1 What percentage of Pregnancy Patients complain of Headache? A) 10 -30% B) 30 -50% C) 50 -70% D) 70 -90%
Multiple Choice Question # 1 What percentage of Pregnancy Patients complain of Headache? A) 10 -30% B) 30 -50% C) 50 -70% D) 70 -90%
 Multiple Choice Question # 2 What medications for headache are contraindicated in pregnancy? A) NSAIDs B) Corticosteroids C) Triptans D) Topiramate
Multiple Choice Question # 2 What medications for headache are contraindicated in pregnancy? A) NSAIDs B) Corticosteroids C) Triptans D) Topiramate
 Multiple Choice Question # 3 Which imaging modalities are contra-indicated in pregnancy? A) NECT B) CECT C) MRI w/o Gadolinium D) MRI w/ Gadolinium
Multiple Choice Question # 3 Which imaging modalities are contra-indicated in pregnancy? A) NECT B) CECT C) MRI w/o Gadolinium D) MRI w/ Gadolinium
 Case Presentation • Wednesday @ 20: 00 – Called by Ob/Gyn Junior Resident – 23 y. F R-handed married G 1 P 1 (GA 39) post-partum 6 h • Duration of labour approximately 24 h • H/A associated with N/V, fatigue • PMH: – H/A since a teenager, worse w/ this pregnancy – Otherwise Healthy – GCS 14, anisocoria 1 mm, no focal neuro deficits • O/E: Drowsy. No focal deficits. • Q: What is a normal Headache in Pregnancy?
Case Presentation • Wednesday @ 20: 00 – Called by Ob/Gyn Junior Resident – 23 y. F R-handed married G 1 P 1 (GA 39) post-partum 6 h • Duration of labour approximately 24 h • H/A associated with N/V, fatigue • PMH: – H/A since a teenager, worse w/ this pregnancy – Otherwise Healthy – GCS 14, anisocoria 1 mm, no focal neuro deficits • O/E: Drowsy. No focal deficits. • Q: What is a normal Headache in Pregnancy?
 Headache and Pregnancy • 10 -35% of pregnancies are complicated by Headache • Etiologies: – Pre-existing primary headache – New presentation of primary or secondary headache – 1/3 rd Migraine – 1/3 rd H/A secondary to gestational HTN or pre-eclampsia – 1/3 rd other primary or secondary headache
Headache and Pregnancy • 10 -35% of pregnancies are complicated by Headache • Etiologies: – Pre-existing primary headache – New presentation of primary or secondary headache – 1/3 rd Migraine – 1/3 rd H/A secondary to gestational HTN or pre-eclampsia – 1/3 rd other primary or secondary headache
 Etiology of Primary Headache Migraine without Aura 39 -64% Migraine with Aura 10 -13% Tension Headache 15 -26%
Etiology of Primary Headache Migraine without Aura 39 -64% Migraine with Aura 10 -13% Tension Headache 15 -26%
 Etiology of Secondary Headache • Most common: – Fasting > Nasal/Sinus > Trauma • Miscellaneous: – HTN, Pre-eclampsia, OSA, post LP, Medication overuse/withdrawal – ICH, Mass lesion, AVM, Infection, Vasculitides, CVST, Pituitary Apoplexy, RCVS, Spontaneous Intracranial Hypotension, IIH – Cancer: Metastatic disease – Immunocompromised: Opportunistic infections
Etiology of Secondary Headache • Most common: – Fasting > Nasal/Sinus > Trauma • Miscellaneous: – HTN, Pre-eclampsia, OSA, post LP, Medication overuse/withdrawal – ICH, Mass lesion, AVM, Infection, Vasculitides, CVST, Pituitary Apoplexy, RCVS, Spontaneous Intracranial Hypotension, IIH – Cancer: Metastatic disease – Immunocompromised: Opportunistic infections
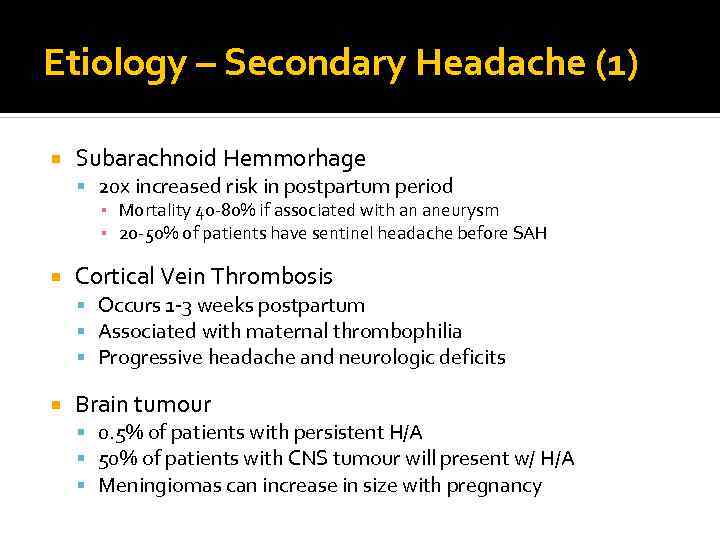 Etiology – Secondary Headache (1) Subarachnoid Hemmorhage 20 x increased risk in postpartum period ▪ Mortality 40 -80% if associated with an aneurysm ▪ 20 -50% of patients have sentinel headache before SAH Cortical Vein Thrombosis Occurs 1 -3 weeks postpartum Associated with maternal thrombophilia Progressive headache and neurologic deficits Brain tumour 0. 5% of patients with persistent H/A 50% of patients with CNS tumour will present w/ H/A Meningiomas can increase in size with pregnancy
Etiology – Secondary Headache (1) Subarachnoid Hemmorhage 20 x increased risk in postpartum period ▪ Mortality 40 -80% if associated with an aneurysm ▪ 20 -50% of patients have sentinel headache before SAH Cortical Vein Thrombosis Occurs 1 -3 weeks postpartum Associated with maternal thrombophilia Progressive headache and neurologic deficits Brain tumour 0. 5% of patients with persistent H/A 50% of patients with CNS tumour will present w/ H/A Meningiomas can increase in size with pregnancy
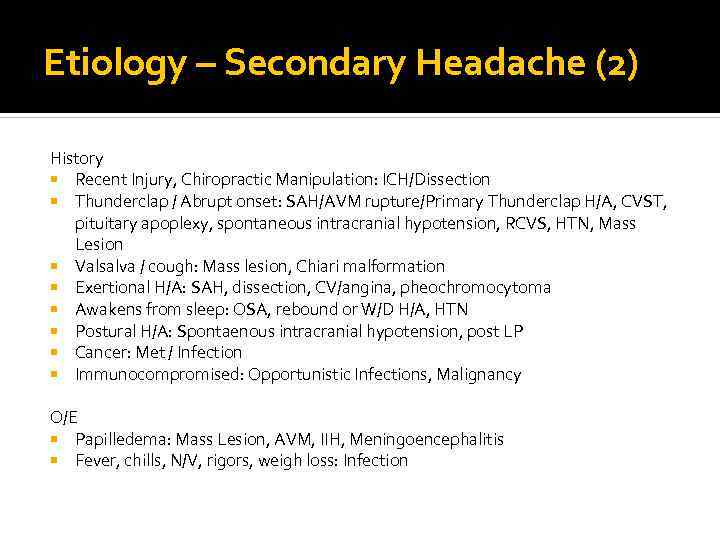 Etiology – Secondary Headache (2) History Recent Injury, Chiropractic Manipulation: ICH/Dissection Thunderclap / Abrupt onset: SAH/AVM rupture/Primary Thunderclap H/A, CVST, pituitary apoplexy, spontaneous intracranial hypotension, RCVS, HTN, Mass Lesion Valsalva / cough: Mass lesion, Chiari malformation Exertional H/A: SAH, dissection, CV/angina, pheochromocytoma Awakens from sleep: OSA, rebound or W/D H/A, HTN Postural H/A: Spontaenous intracranial hypotension, post LP Cancer: Met / Infection Immunocompromised: Opportunistic Infections, Malignancy O/E Papilledema: Mass Lesion, AVM, IIH, Meningoencephalitis Fever, chills, N/V, rigors, weigh loss: Infection
Etiology – Secondary Headache (2) History Recent Injury, Chiropractic Manipulation: ICH/Dissection Thunderclap / Abrupt onset: SAH/AVM rupture/Primary Thunderclap H/A, CVST, pituitary apoplexy, spontaneous intracranial hypotension, RCVS, HTN, Mass Lesion Valsalva / cough: Mass lesion, Chiari malformation Exertional H/A: SAH, dissection, CV/angina, pheochromocytoma Awakens from sleep: OSA, rebound or W/D H/A, HTN Postural H/A: Spontaenous intracranial hypotension, post LP Cancer: Met / Infection Immunocompromised: Opportunistic Infections, Malignancy O/E Papilledema: Mass Lesion, AVM, IIH, Meningoencephalitis Fever, chills, N/V, rigors, weigh loss: Infection
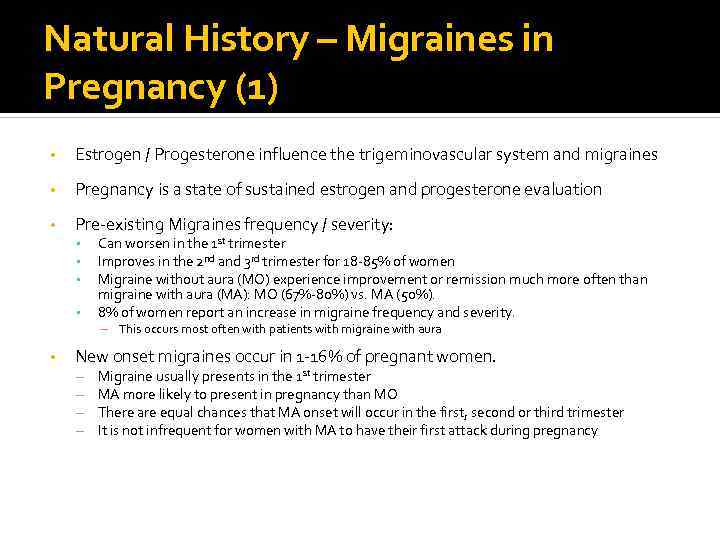 Natural History – Migraines in Pregnancy (1) • Estrogen / Progesterone influence the trigeminovascular system and migraines • Pregnancy is a state of sustained estrogen and progesterone evaluation • Pre-existing Migraines frequency / severity: • • Can worsen in the 1 st trimester Improves in the 2 nd and 3 rd trimester for 18 -85% of women Migraine without aura (MO) experience improvement or remission much more often than migraine with aura (MA): MO (67%-80%) vs. MA (50%). 8% of women report an increase in migraine frequency and severity. – This occurs most often with patients with migraine with aura • New onset migraines occur in 1 -16% of pregnant women. – – Migraine usually presents in the 1 st trimester MA more likely to present in pregnancy than MO There are equal chances that MA onset will occur in the first, second or third trimester It is not infrequent for women with MA to have their first attack during pregnancy
Natural History – Migraines in Pregnancy (1) • Estrogen / Progesterone influence the trigeminovascular system and migraines • Pregnancy is a state of sustained estrogen and progesterone evaluation • Pre-existing Migraines frequency / severity: • • Can worsen in the 1 st trimester Improves in the 2 nd and 3 rd trimester for 18 -85% of women Migraine without aura (MO) experience improvement or remission much more often than migraine with aura (MA): MO (67%-80%) vs. MA (50%). 8% of women report an increase in migraine frequency and severity. – This occurs most often with patients with migraine with aura • New onset migraines occur in 1 -16% of pregnant women. – – Migraine usually presents in the 1 st trimester MA more likely to present in pregnancy than MO There are equal chances that MA onset will occur in the first, second or third trimester It is not infrequent for women with MA to have their first attack during pregnancy
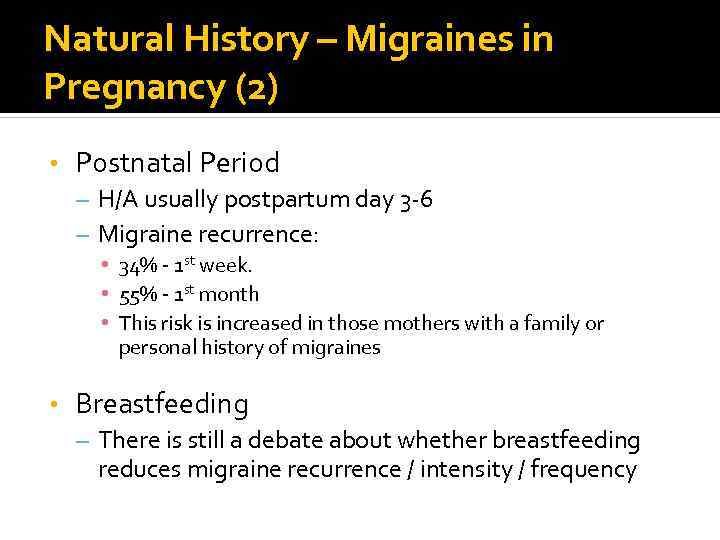 Natural History – Migraines in Pregnancy (2) • Postnatal Period – H/A usually postpartum day 3 -6 – Migraine recurrence: • 34% - 1 st week. • 55% - 1 st month • This risk is increased in those mothers with a family or personal history of migraines • Breastfeeding – There is still a debate about whether breastfeeding reduces migraine recurrence / intensity / frequency
Natural History – Migraines in Pregnancy (2) • Postnatal Period – H/A usually postpartum day 3 -6 – Migraine recurrence: • 34% - 1 st week. • 55% - 1 st month • This risk is increased in those mothers with a family or personal history of migraines • Breastfeeding – There is still a debate about whether breastfeeding reduces migraine recurrence / intensity / frequency
 Natural History – Tension and Cluster Headache in Pregancy ▪ Tension Headache: ▪ TTH has not been shown to change in character due to pregnancy. ▪ Overall 28% to 50% of TTH sufferers experience remission or improvement in pregnancy, and 5% worsen. ▪ Cluster Headache ▪ No change in the frequency or intensity with pregnancy
Natural History – Tension and Cluster Headache in Pregancy ▪ Tension Headache: ▪ TTH has not been shown to change in character due to pregnancy. ▪ Overall 28% to 50% of TTH sufferers experience remission or improvement in pregnancy, and 5% worsen. ▪ Cluster Headache ▪ No change in the frequency or intensity with pregnancy
 Complications Associated with Headache Patients with Migraine have an increased risk of HTN and 3 x risk of pre-eclapsia vs. non-migraneurs (9. 1% vs. 3. 1%) Pre-eclampsia occurs in 5% of pregnancies. If patients is GA > 20 w/ H/A not relieved by OTC pain medication - need to r/o pre-eclampsia • Women with migraine also showed a tendency to increased risk of low birth weight infants • The incidence of preterm delivery (<37 weeks’ gestation) was significantly higher in patients suffering from headache than in controls
Complications Associated with Headache Patients with Migraine have an increased risk of HTN and 3 x risk of pre-eclapsia vs. non-migraneurs (9. 1% vs. 3. 1%) Pre-eclampsia occurs in 5% of pregnancies. If patients is GA > 20 w/ H/A not relieved by OTC pain medication - need to r/o pre-eclampsia • Women with migraine also showed a tendency to increased risk of low birth weight infants • The incidence of preterm delivery (<37 weeks’ gestation) was significantly higher in patients suffering from headache than in controls
 Investigations Blood Pressure CBC, lytes, Liver enzymes, Cr, Urine protein C&S Blood, Urine, Sputum
Investigations Blood Pressure CBC, lytes, Liver enzymes, Cr, Urine protein C&S Blood, Urine, Sputum
 Investigations – Imaging (1) Non-emergent: MRI Brain ▪ No problems reported with 1. 5 T ▪ No evidence with ≥ 2. 5 T ▪ Gadolinium crosses placenta and remains in amniotic fluid ▪ Safe with breastfeeding Lumbar puncture is safe in pregnancy
Investigations – Imaging (1) Non-emergent: MRI Brain ▪ No problems reported with 1. 5 T ▪ No evidence with ≥ 2. 5 T ▪ Gadolinium crosses placenta and remains in amniotic fluid ▪ Safe with breastfeeding Lumbar puncture is safe in pregnancy
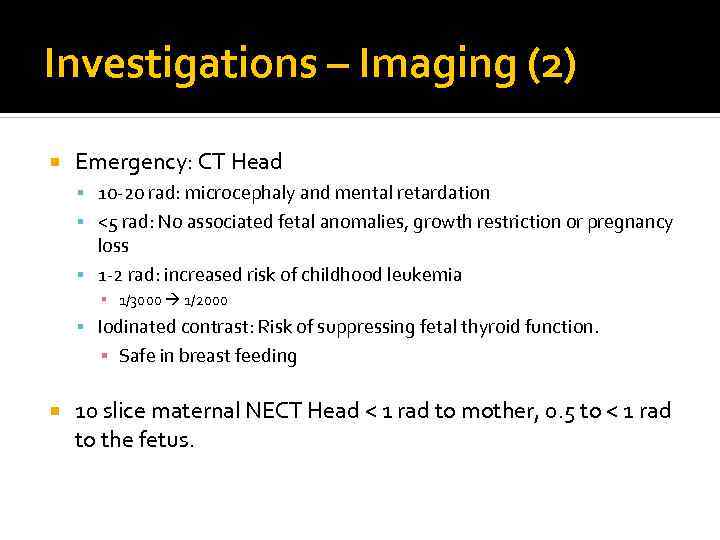 Investigations – Imaging (2) Emergency: CT Head 10 -20 rad: microcephaly and mental retardation <5 rad: No associated fetal anomalies, growth restriction or pregnancy loss 1 -2 rad: increased risk of childhood leukemia ▪ 1/3000 1/2000 Iodinated contrast: Risk of suppressing fetal thyroid function. ▪ Safe in breast feeding 10 slice maternal NECT Head < 1 rad to mother, 0. 5 to < 1 rad to the fetus.
Investigations – Imaging (2) Emergency: CT Head 10 -20 rad: microcephaly and mental retardation <5 rad: No associated fetal anomalies, growth restriction or pregnancy loss 1 -2 rad: increased risk of childhood leukemia ▪ 1/3000 1/2000 Iodinated contrast: Risk of suppressing fetal thyroid function. ▪ Safe in breast feeding 10 slice maternal NECT Head < 1 rad to mother, 0. 5 to < 1 rad to the fetus.
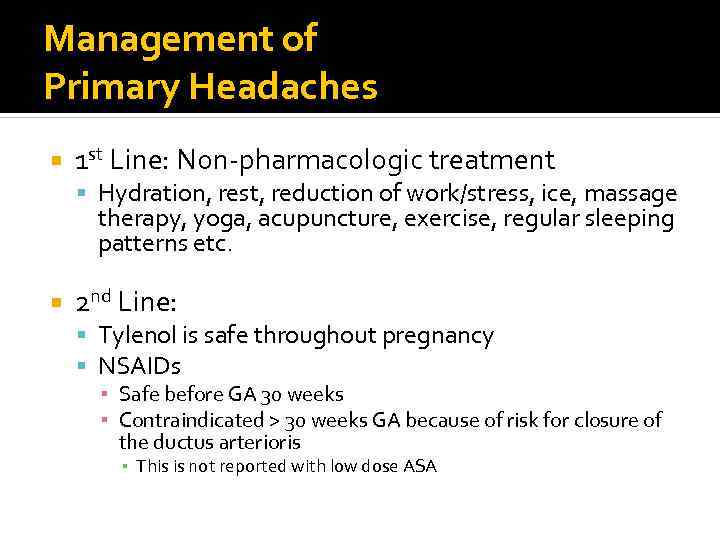 Management of Primary Headaches 1 st Line: Non-pharmacologic treatment Hydration, rest, reduction of work/stress, ice, massage therapy, yoga, acupuncture, exercise, regular sleeping patterns etc. 2 nd Line: Tylenol is safe throughout pregnancy NSAIDs ▪ Safe before GA 30 weeks ▪ Contraindicated > 30 weeks GA because of risk for closure of the ductus arterioris ▪ This is not reported with low dose ASA
Management of Primary Headaches 1 st Line: Non-pharmacologic treatment Hydration, rest, reduction of work/stress, ice, massage therapy, yoga, acupuncture, exercise, regular sleeping patterns etc. 2 nd Line: Tylenol is safe throughout pregnancy NSAIDs ▪ Safe before GA 30 weeks ▪ Contraindicated > 30 weeks GA because of risk for closure of the ductus arterioris ▪ This is not reported with low dose ASA
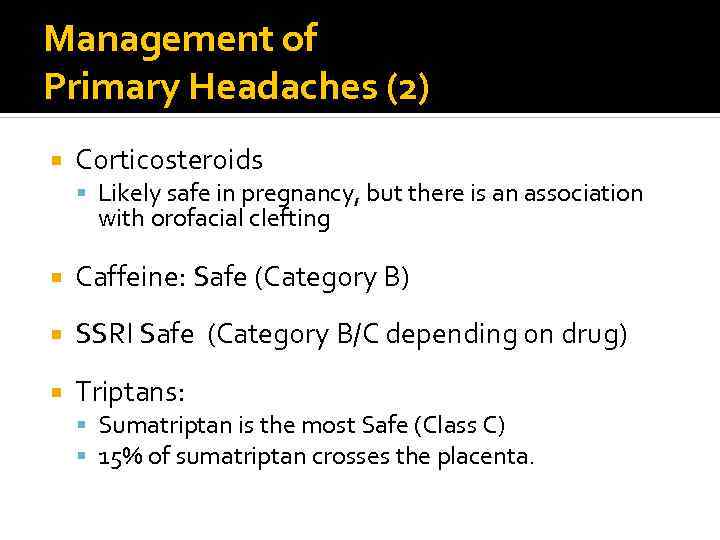 Management of Primary Headaches (2) Corticosteroids Likely safe in pregnancy, but there is an association with orofacial clefting Caffeine: Safe (Category B) SSRI Safe (Category B/C depending on drug) Triptans: Sumatriptan is the most Safe (Class C) 15% of sumatriptan crosses the placenta.
Management of Primary Headaches (2) Corticosteroids Likely safe in pregnancy, but there is an association with orofacial clefting Caffeine: Safe (Category B) SSRI Safe (Category B/C depending on drug) Triptans: Sumatriptan is the most Safe (Class C) 15% of sumatriptan crosses the placenta.
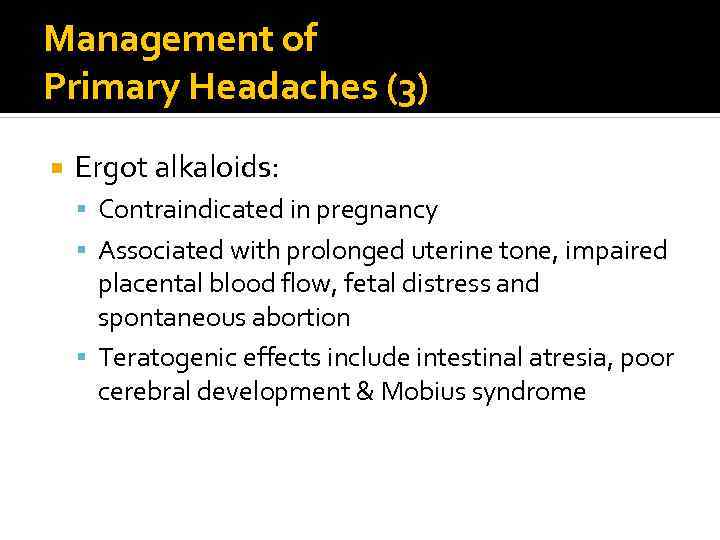 Management of Primary Headaches (3) Ergot alkaloids: Contraindicated in pregnancy Associated with prolonged uterine tone, impaired placental blood flow, fetal distress and spontaneous abortion Teratogenic effects include intestinal atresia, poor cerebral development & Mobius syndrome
Management of Primary Headaches (3) Ergot alkaloids: Contraindicated in pregnancy Associated with prolonged uterine tone, impaired placental blood flow, fetal distress and spontaneous abortion Teratogenic effects include intestinal atresia, poor cerebral development & Mobius syndrome
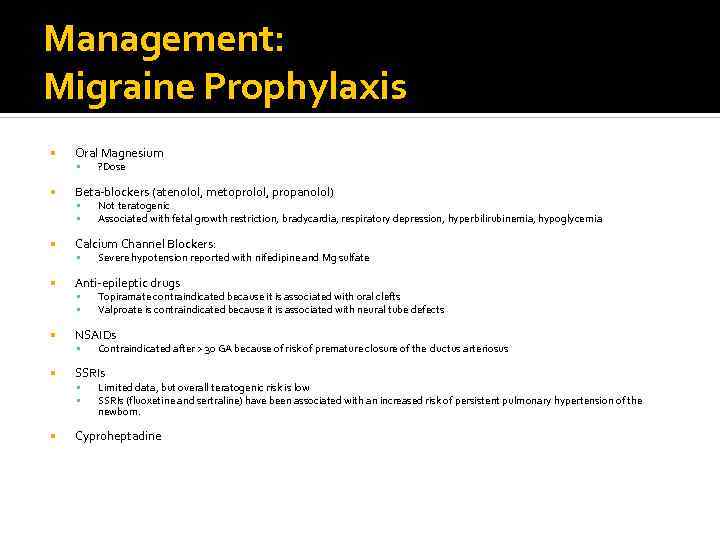 Management: Migraine Prophylaxis Oral Magnesium Beta-blockers (atenolol, metoprolol, propanolol) Contraindicated after > 30 GA because of risk of premature closure of the ductus arteriosus SSRIs Topiramate contraindicated because it is associated with oral clefts Valproate is contraindicated because it is associated with neural tube defects NSAIDs Severe hypotension reported with nifedipine and Mg sulfate Anti-epileptic drugs Not teratogenic Associated with fetal growth restriction, bradycardia, respiratory depression, hyperbilirubinemia, hypoglycemia Calcium Channel Blockers: ? Dose Limited data, but overall teratogenic risk is low SSRIs (fluoxetine and sertraline) have been associated with an increased risk of persistent pulmonary hypertension of the newborn. Cyproheptadine
Management: Migraine Prophylaxis Oral Magnesium Beta-blockers (atenolol, metoprolol, propanolol) Contraindicated after > 30 GA because of risk of premature closure of the ductus arteriosus SSRIs Topiramate contraindicated because it is associated with oral clefts Valproate is contraindicated because it is associated with neural tube defects NSAIDs Severe hypotension reported with nifedipine and Mg sulfate Anti-epileptic drugs Not teratogenic Associated with fetal growth restriction, bradycardia, respiratory depression, hyperbilirubinemia, hypoglycemia Calcium Channel Blockers: ? Dose Limited data, but overall teratogenic risk is low SSRIs (fluoxetine and sertraline) have been associated with an increased risk of persistent pulmonary hypertension of the newborn. Cyproheptadine
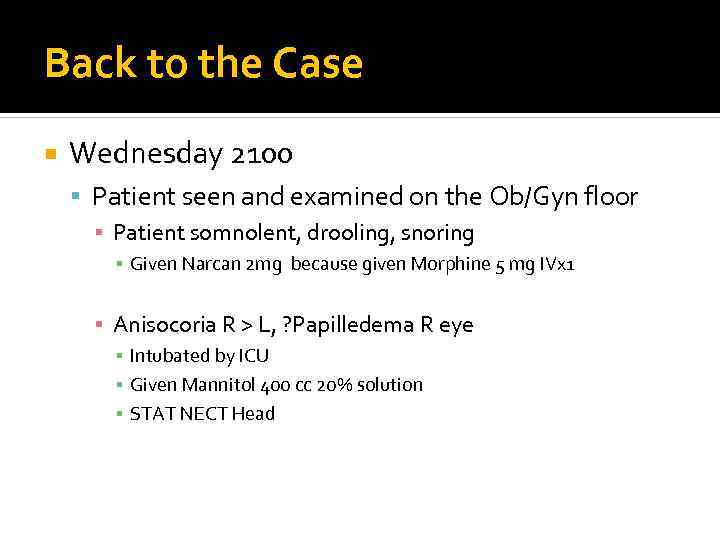 Back to the Case Wednesday 2100 Patient seen and examined on the Ob/Gyn floor ▪ Patient somnolent, drooling, snoring ▪ Given Narcan 2 mg because given Morphine 5 mg IVx 1 ▪ Anisocoria R > L, ? Papilledema R eye ▪ Intubated by ICU ▪ Given Mannitol 400 cc 20% solution ▪ STAT NECT Head
Back to the Case Wednesday 2100 Patient seen and examined on the Ob/Gyn floor ▪ Patient somnolent, drooling, snoring ▪ Given Narcan 2 mg because given Morphine 5 mg IVx 1 ▪ Anisocoria R > L, ? Papilledema R eye ▪ Intubated by ICU ▪ Given Mannitol 400 cc 20% solution ▪ STAT NECT Head
 Case Imaging
Case Imaging
 Case Epilogue Patient transferred to ICU under NSx Improved neurologically w/ Mannitol Taken to OR later that day No post-operative neurologic deficits immediately after OR or on follow-up a few weeks later
Case Epilogue Patient transferred to ICU under NSx Improved neurologically w/ Mannitol Taken to OR later that day No post-operative neurologic deficits immediately after OR or on follow-up a few weeks later
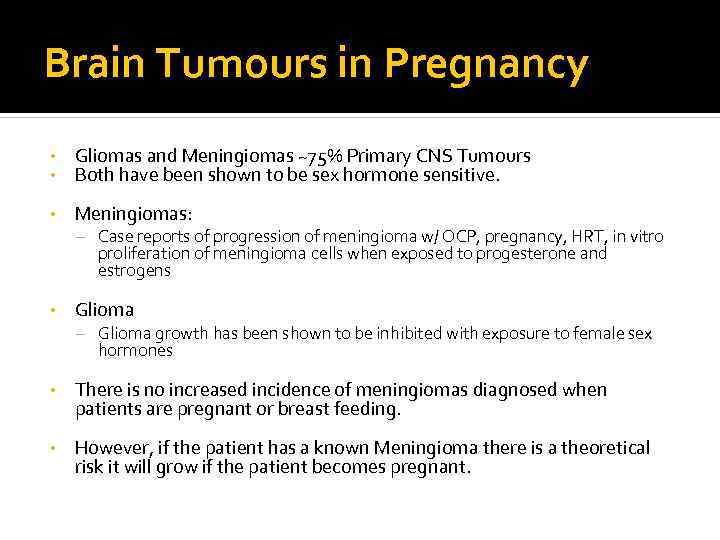 Brain Tumours in Pregnancy • • Gliomas and Meningiomas ~75% Primary CNS Tumours Both have been shown to be sex hormone sensitive. • Meningiomas: – Case reports of progression of meningioma w/ OCP, pregnancy, HRT, in vitro proliferation of meningioma cells when exposed to progesterone and estrogens • Glioma – Glioma growth has been shown to be inhibited with exposure to female sex hormones • There is no increased incidence of meningiomas diagnosed when patients are pregnant or breast feeding. • However, if the patient has a known Meningioma there is a theoretical risk it will grow if the patient becomes pregnant.
Brain Tumours in Pregnancy • • Gliomas and Meningiomas ~75% Primary CNS Tumours Both have been shown to be sex hormone sensitive. • Meningiomas: – Case reports of progression of meningioma w/ OCP, pregnancy, HRT, in vitro proliferation of meningioma cells when exposed to progesterone and estrogens • Glioma – Glioma growth has been shown to be inhibited with exposure to female sex hormones • There is no increased incidence of meningiomas diagnosed when patients are pregnant or breast feeding. • However, if the patient has a known Meningioma there is a theoretical risk it will grow if the patient becomes pregnant.
 Summary Go see the patient Headache is a common complication of pregnancy Headache in pregnancy is usually benign, but can be a manifestation of a serious etiology A good history and a high index of suspicion are important in making the diagnosis Management of primary headache in pregnancy is complicated by a reduced choice of pharmacotherapies
Summary Go see the patient Headache is a common complication of pregnancy Headache in pregnancy is usually benign, but can be a manifestation of a serious etiology A good history and a high index of suspicion are important in making the diagnosis Management of primary headache in pregnancy is complicated by a reduced choice of pharmacotherapies
 References Pearce CF, Hansen WF. “Headache and neurological disease in pregnancy. ” Clin Obstet Gynecol. 2012 Sep; 55(3): 810 -28. Marozio L, Facchinetti F et al. “Headache and adverse pregnancy outcomes: a prospective study. ” Eur J Obstet Gynecol Reprod Biol. 2012 Apr; 161(2): 140 -3. Epub 2012 Jan 27. Kvisvik EV, Stovner LJ et al. “Headache and migraine during pregnancy and puerperium: the MIGRAstudy. ” J Headache Pain. 2011 Aug; 12(4): 443 -51. Epub 2011 Mar 26. Torelli P, Allais G, Manzoni GC. “Clinical review of headache in pregnancy. ” Neurol Sci. 2010 Jun; 31 Suppl 1: S 55 -8. Menon R, Bushnell CD. “Headache and pregnancy. ” Neurologist. 2008 Mar; 14(2): 108 -19. Melhado EM, Maciel JA Jr, Guerreiro CA. “Headache during gestation: evaluation of 1101 women. ” Can J Neurol Sci. 2007 May; 34(2): 187 -92. Rizzoli, PB. “Acute and Preventive Treatment of Migraine” CONTINUUM: Lifelong Learning in Neurology August 2012; Volume 18(4) Headache; p 764– 782 Lee, MJ, Guinn D, Hickenbottom S. “Headache in pregnancy” Up. To. Date Jan 2012.
References Pearce CF, Hansen WF. “Headache and neurological disease in pregnancy. ” Clin Obstet Gynecol. 2012 Sep; 55(3): 810 -28. Marozio L, Facchinetti F et al. “Headache and adverse pregnancy outcomes: a prospective study. ” Eur J Obstet Gynecol Reprod Biol. 2012 Apr; 161(2): 140 -3. Epub 2012 Jan 27. Kvisvik EV, Stovner LJ et al. “Headache and migraine during pregnancy and puerperium: the MIGRAstudy. ” J Headache Pain. 2011 Aug; 12(4): 443 -51. Epub 2011 Mar 26. Torelli P, Allais G, Manzoni GC. “Clinical review of headache in pregnancy. ” Neurol Sci. 2010 Jun; 31 Suppl 1: S 55 -8. Menon R, Bushnell CD. “Headache and pregnancy. ” Neurologist. 2008 Mar; 14(2): 108 -19. Melhado EM, Maciel JA Jr, Guerreiro CA. “Headache during gestation: evaluation of 1101 women. ” Can J Neurol Sci. 2007 May; 34(2): 187 -92. Rizzoli, PB. “Acute and Preventive Treatment of Migraine” CONTINUUM: Lifelong Learning in Neurology August 2012; Volume 18(4) Headache; p 764– 782 Lee, MJ, Guinn D, Hickenbottom S. “Headache in pregnancy” Up. To. Date Jan 2012.


