alia gyne.ppt
- Количество слайдов: 31
Preeclampsia and Eclampsia: Prepared by: Alia Ismail Group no. 552
Plan: z Types of hypertension during pregnancy. z Preeclampsia. z Criteria of preeclampsia. z Causes and pathphysiology. z Prevention and Management z conclusion z reference
Hypertension during Pregnancy: Classification z Pregnancy-induced hypertension y. Hypertension without proteinuria/edema y. Preeclampsia xmild xsevere y. Eclampsia z Coincidental HTN: preexisting or persistent z Pregnancy-aggravated HTN ysuperimposed preeclampsia ysuperimposed eclampsia z Transient HTN: occurs in 3 rd trimester, mild
Preeclampsia: Definition z Hypertension y> 140/90 yrelative no longer considered diagnostic z Proteinuria y> 300 mg/24 hours or 1+ on urine dipstick ynot mandatory for diagnosis; may occur late z Edema (non-dependent) yso common & difficult to quantify it is rarely evoked to make or refute the diagnosis
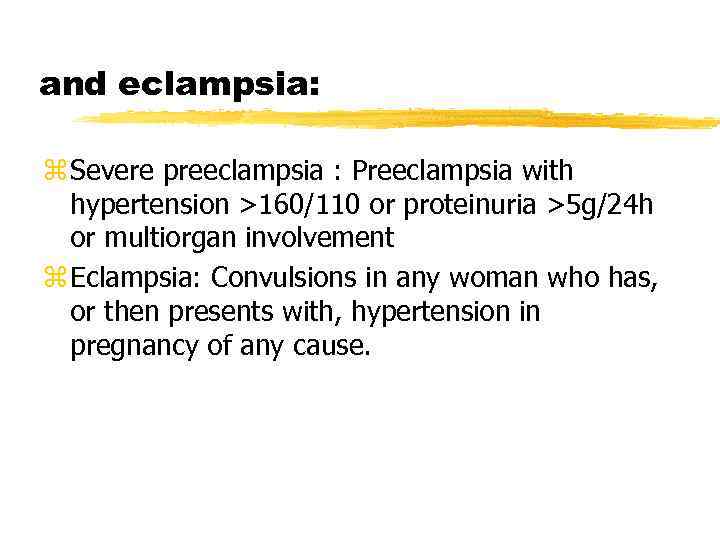
and eclampsia: z Severe preeclampsia : Preeclampsia with hypertension >160/110 or proteinuria >5 g/24 h or multiorgan involvement z Eclampsia: Convulsions in any woman who has, or then presents with, hypertension in pregnancy of any cause.
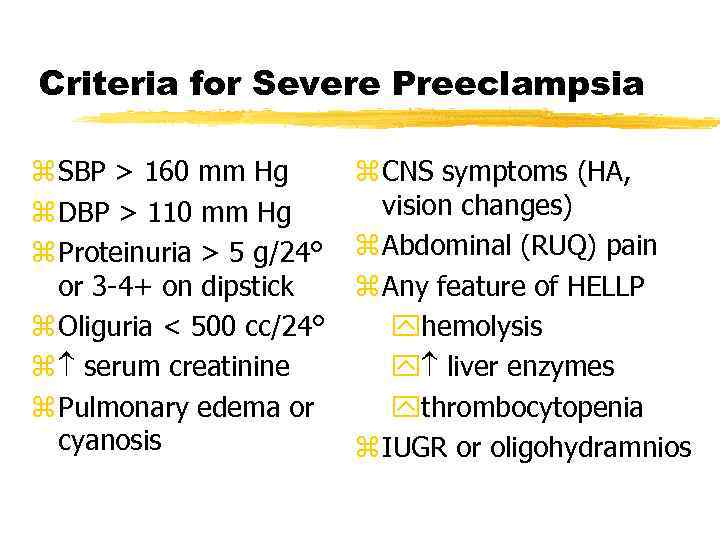
Criteria for Severe Preeclampsia z SBP > 160 mm Hg z DBP > 110 mm Hg z Proteinuria > 5 g/24° or 3 -4+ on dipstick z Oliguria < 500 cc/24° z serum creatinine z Pulmonary edema or cyanosis z CNS symptoms (HA, vision changes) z Abdominal (RUQ) pain z Any feature of HELLP yhemolysis y liver enzymes ythrombocytopenia z IUGR or oligohydramnios
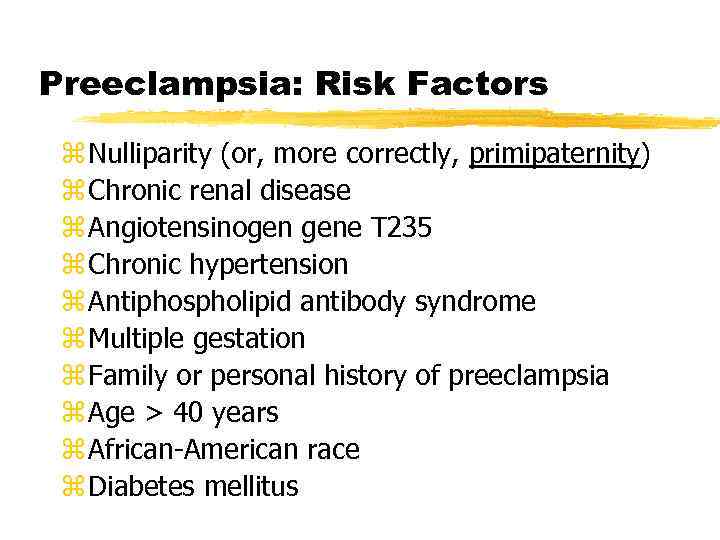
Preeclampsia: Risk Factors z Nulliparity (or, more correctly, primipaternity) z Chronic renal disease z Angiotensinogen gene T 235 z Chronic hypertension z Antiphospholipid antibody syndrome z Multiple gestation z Family or personal history of preeclampsia z Age > 40 years z African-American race z Diabetes mellitus
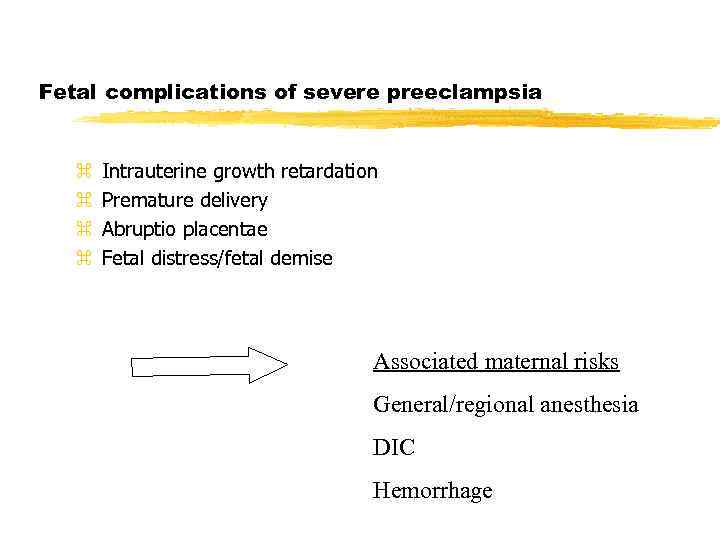
Fetal complications of severe preeclampsia z z Intrauterine growth retardation Premature delivery Abruptio placentae Fetal distress/fetal demise Associated maternal risks General/regional anesthesia DIC Hemorrhage
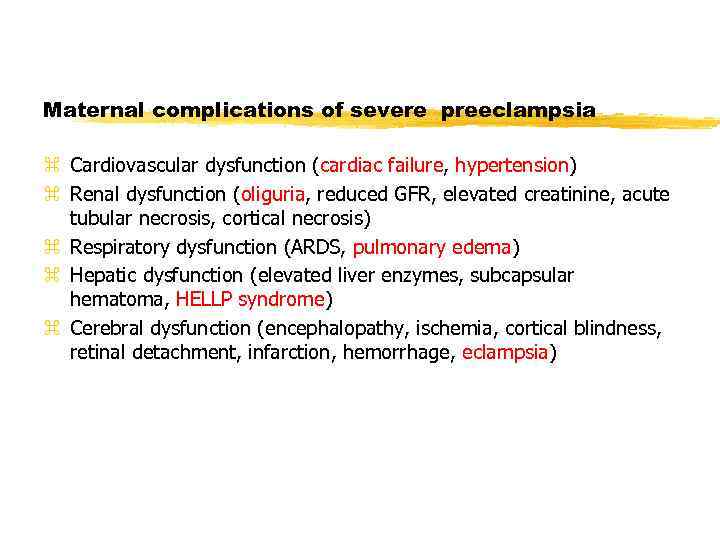
Maternal complications of severe preeclampsia z Cardiovascular dysfunction (cardiac failure, hypertension) z Renal dysfunction (oliguria, reduced GFR, elevated creatinine, acute tubular necrosis, cortical necrosis) z Respiratory dysfunction (ARDS, pulmonary edema) z Hepatic dysfunction (elevated liver enzymes, subcapsular hematoma, HELLP syndrome) z Cerebral dysfunction (encephalopathy, ischemia, cortical blindness, retinal detachment, infarction, hemorrhage, eclampsia)
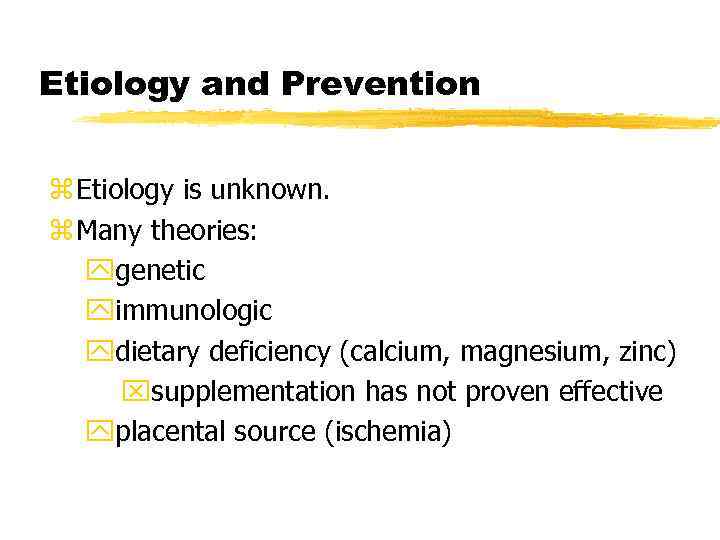
Etiology and Prevention z Etiology is unknown. z Many theories: ygenetic yimmunologic ydietary deficiency (calcium, magnesium, zinc) xsupplementation has not proven effective yplacental source (ischemia)
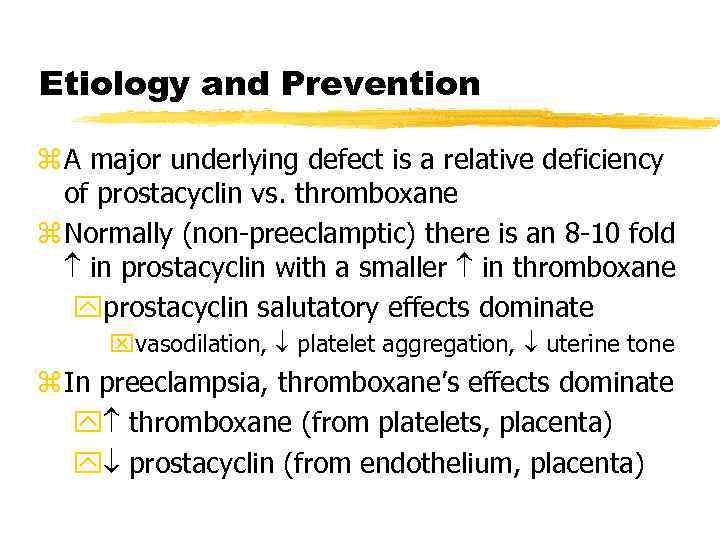
Etiology and Prevention z A major underlying defect is a relative deficiency of prostacyclin vs. thromboxane z Normally (non-preeclamptic) there is an 8 -10 fold in prostacyclin with a smaller in thromboxane yprostacyclin salutatory effects dominate xvasodilation, platelet aggregation, uterine tone z In preeclampsia, thromboxane’s effects dominate y thromboxane (from platelets, placenta) y prostacyclin (from endothelium, placenta)
Preeclampsia Prophylaxis: Aspirin z Aspirin has been extensively studied as a targeted therapy to thromboxane production
Preeclampsia: Mechanism z At this time the most widely accepted proposed mechanism for preeclampsia is: xglobal endothelial cell dysfunction z Redman: endothelial cell dysfunction is just one manifestation of a broader intravascular inflammatory response ypresent in normal pregnancy yexcessive in preeclampsia y. Proposed source of inflammatory stimulus: placenta
Pathophysiology: Cardiovascular z In severe preeclampsia, typically hyperdynamic with normal-high CO, normal-mod. high SVR, and normal PCWP and CVP. z Despite normal filling pressures, intravascular fluid volume is reduced (30 -40% in severe PIH) z Variations in presentation depending on prior treatment and severity and duration of disease z Total body water is increased (generalized edema)
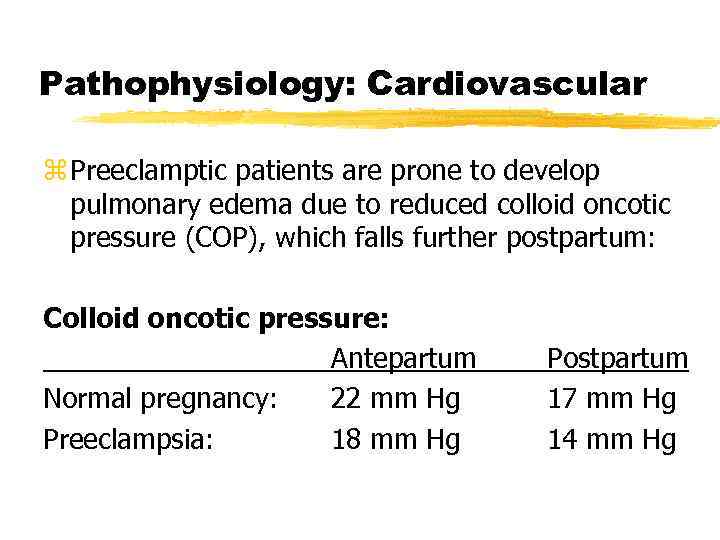
Pathophysiology: Cardiovascular z Preeclamptic patients are prone to develop pulmonary edema due to reduced colloid oncotic pressure (COP), which falls further postpartum: Colloid oncotic pressure: Antepartum Normal pregnancy: 22 mm Hg Preeclampsia: 18 mm Hg Postpartum 17 mm Hg 14 mm Hg
Pathophysiology z Respiratory: y. Airway is edematous; use smaller ET tube (6. 5) y risk of pulmonary edema; 70% postpartum z Renal: y. Renal blood flow & GFR are decreased y. Renal failure due to plasma volume or renal artery vasospasm y. Proteinuria due to glomerulopathy xglomerular capillary endothelial swelling w/subendothelial protein deposits y. Renal function recovers quickly postpartum
Pathophysiology: Hepatic z RUQ pain is a serious complaint ywarrants imaging, especially when accompanied by liver enzymes ycaused by liver swelling, periportal hemorrhage, subcapsular hematoma, hepatic rupture (30% mortality) z HELLP syndrome occurs in ~ 20% of severe preeclamptics.
Pathophysiology z Coagulation: y. Generally hypercoagulable with evidence of platelet activation and increased fibrinolysis y. Thrombocytopenia is common, but fewer than 10% have platelet count < 100, 000 y. DIC may occur, esp. with placental abruption z Neurologic: y. Symptoms: headache, visual changes, seizures y. Hyperreflexia is usually present y. Eclamptic seizures may occur even w/out BP x. Possible causes: hypertensive encephalopathy, cerebral edema, thrombosis, hemorrhage, vasospasm
Obstetric Management z Classically “stabilize and deliver” z Medical management while awaiting delivery: yuse of steroids X 48 hours if fetus < 34 wks yantihypertensives to maintain DBP < 105 -110 ymagnesium sulfate for seizure prophylaxis ymonitor fluid balance, I/O, daily weights, symptoms, reflexes, HCT, plts, LFT’s, proteinuria z Indications for expedited delivery: yfetal distress y BP despite aggressive Rx yworsening end-organ function ydevelopment or worsening of HELLP syndrome ydevelopment of eclampsia
Antihypertensive Therapy z Most commonly, for acute control: hydralazine, labetolol z Nifedipine may be used, but unexpected hypotension may occur when given with Mg. SO 4 z For refractory hypertension: nitroglycerin or nitroprusside may be used y. Nitroprusside dose and duration should be limited to avoid fetal cyanide toxicity y. Usually require invasive arterial pressure mon z Angiotensin-converting enzyme (ACE) inhibitors contraindicated due to severe adverse fetal effects
Seizure Prophylaxis z Evidence is strong that magnesium sulfate is indicated for yseizure treatment in eclamptics yseizure prophylaxis in severe preeclamptics z Role of magnesium prophylaxis in mild preeclamptics is less clear yawaits large, prospective, randomized, placebo-controlled trial
Magnesium Sulfate z Magnesium sulfate has many effects; its mechanism in seizure control is not clear. y. NMDA (N-methyl-D-aspartate) antagonist yvasodilator x. Brain parenchymal vasodilation demonstrated in preeclamptics by Doppler ultrasonography yincreases release of prostacyclin z Potential adverse effects: ytoxicity from overdose (respiratory, cardiac) y bleeding y hypotension with hemorrhage y uterine contractility
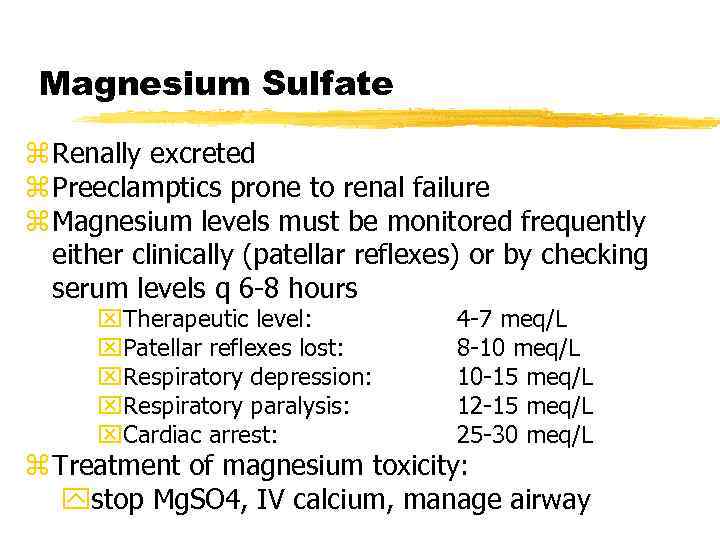
Magnesium Sulfate z Renally excreted z Preeclamptics prone to renal failure z Magnesium levels must be monitored frequently either clinically (patellar reflexes) or by checking serum levels q 6 -8 hours x. Therapeutic level: x. Patellar reflexes lost: x. Respiratory depression: x. Respiratory paralysis: x. Cardiac arrest: 4 -7 meq/L 8 -10 meq/L 10 -15 meq/L 12 -15 meq/L 25 -30 meq/L z Treatment of magnesium toxicity: ystop Mg. SO 4, IV calcium, manage airway
Treatment of Eclampsia z Seizures are usually short-lived. z If necessary, small doses of barbiturate or benzodiazepine (STP, 50 mg, or midazolam, 1 -2 mg) and supplemental oxygen by mask. z If seizure persists or patient is not breathing, rapid sequence induction with cricoid pressure and intubation should be performed. z Patient may be extubated once she is completely awake, recovered from neuromuscular blockade, and magnesium sulfate has been administered.
Anesthetic Goals of Labor Analgesia in Preeclampsia z To establish & maintain hemodynamic stability (control hypertension & avoid hypotension) z To provide excellent labor analgesia z To prevent complications of preeclampsia yintracerebral hemorrhage yrenal failure ypulmonary edema yeclampsia z To be able to rapidly provide anesthesia for C/S
Benefits of Regional Analgesia for Labor in Preeclampsia z Superior pain relief over parenteral narcotics z Beneficial hemodynamic effects: 20% reduction in blood pressure with a small reduction in SVR & maintenance of CI z Doppler velocimetry shows epidural analgesia reduces the S-D flow ratio in the uterine artery by 25% to levels seen in non-preeclamptics y vascular resistance & relief of vasospasm
Hazards of General Anesthesia in Preeclampsia z Airway edema is common y. Mandatory to reexamine the airway soon before induction y. Edema may appear or worsen at any time during the course of disease xtongue & facial, as well as laryngeal z Laryngoscopy and intubation may severe BP y. Labetolol & NTG are commonly used acutely y. Fentanyl (2. 5 mcg/kg), alfentanil (10 mcg/kg), lidocaine may be given to blunt response
Hazards of General Anesthesia in Preeclampsia z Magnesium sulfate potentiates depolarizing & non-depolarizing muscle relaxants y. Pre-curarization is not indicated. y. Initial dose of succinylcholine is not reduced. y. Neuromuscular blockade should be monitored & reversal confirmed.
Conclusions z Preeclampsia is a serious multi-organ system disorder of pregnancy that continues to defy our complete understanding. z It is characterized by global endothelial cell dysfunction. z The cause remains unknown. z There is no effective prophylaxis.
Conclusions z Delivery is the only effective cure. z Magnesium sulfate is now proven as the best medication to prevent and treat eclampsia. z Epidural analgesia for labor pain management & regional anesthesia for C/S have many beneficial effects & are preferred.
References: z www. google. com z www. wikipedia. com z dutta book of gynecolgy
alia gyne.ppt