09b4eb3391d6f18ff4b62dcc4d2eba77.ppt
- Количество слайдов: 40
POWERPOINT® LECTURE SLIDE PRESENTATION by LYNN CIALDELLA, MBA, The University of Texas at Austin Additional Text by J Padilla exclusively for physiology at ECC UNIT 3 17 & 18 Mechanics of Breathing HUMAN PHYSIOLOGY AN INTEGRATED APPROACH DEE UNGLAUB SILVERTHORN Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings FOURTH EDITION
Respiratory System Functions & Structures § Fuctions: § Exchange of gases between the atmosphere and the blood- inhale O 2 and exhale CO 2 § Homeostatic regulation of body p. H- the amounts of CO 2 in the blood affect the p. H § Protection from inhaled pathogens and irritating substancespreventive mechanisms against pathogens that could cause harm § Vocalization- voice production is possible when one exhales § Structures or zones § Conducting system (zone)- components of the respiratory tract that are involved with the flow of air and not the exchange § Respiratory zones- site where gas exchange occurs § Alveoli- site for quick two-way transfer of substances between the blood and the lung tissue § Bones and muscle of thorax- (muscular pump) use to increase or decrease pressure. Includes the diaphram, internal/external intercostal, abdominals, ect. Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings
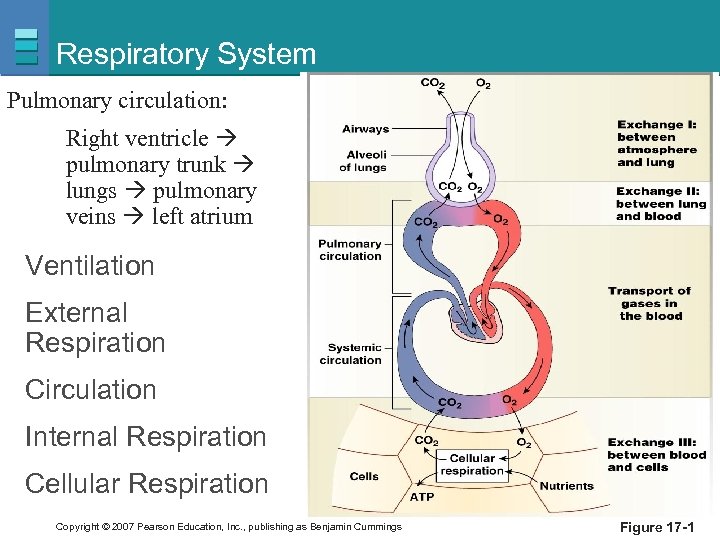
Respiratory System Pulmonary circulation: Right ventricle pulmonary trunk lungs pulmonary veins left atrium Ventilation External Respiration Circulation Internal Respiration Cellular Respiration Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings Figure 17 -1
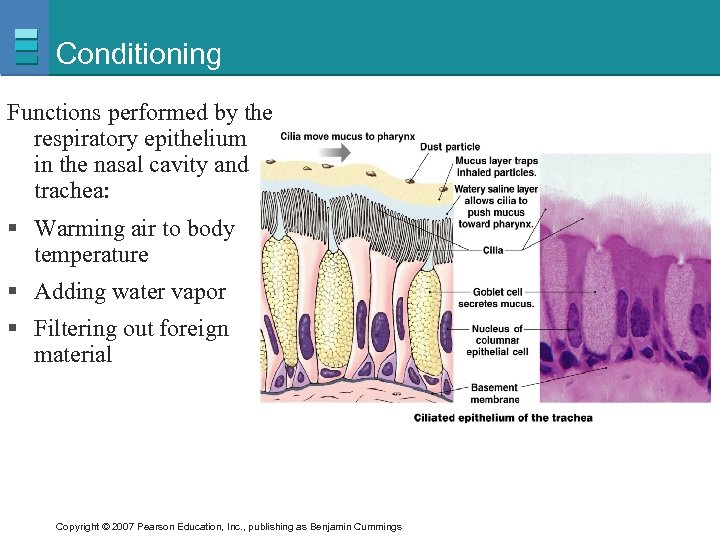
Conditioning Functions performed by the respiratory epithelium found in the nasal cavity and trachea: § Warming air to body temperature § Adding water vapor § Filtering out foreign material Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings
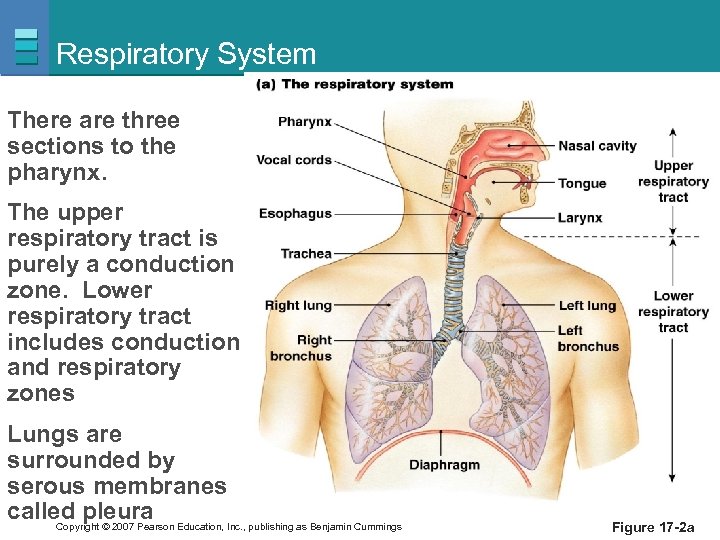
Respiratory System There are three sections to the pharynx. The upper respiratory tract is purely a conduction zone. Lower respiratory tract includes conduction and respiratory zones Lungs are surrounded by serous membranes called pleura Education, Inc. , publishing as Benjamin Cummings Copyright © 2007 Pearson Figure 17 -2 a
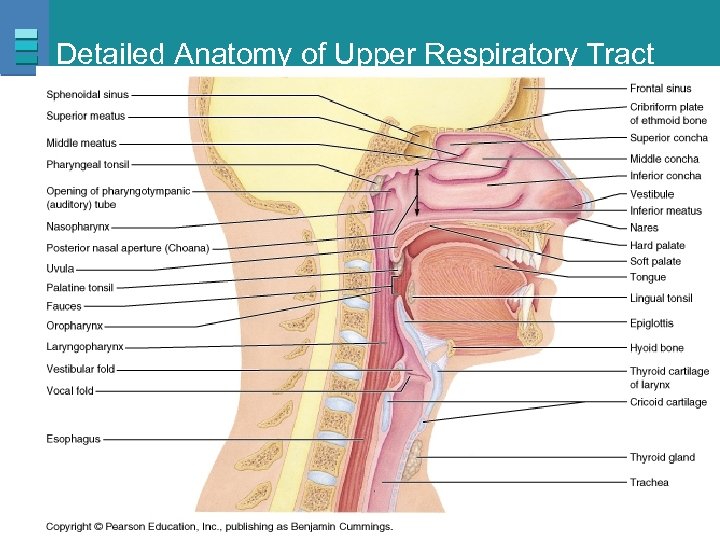
Detailed Anatomy of Upper Respiratory Tract Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings
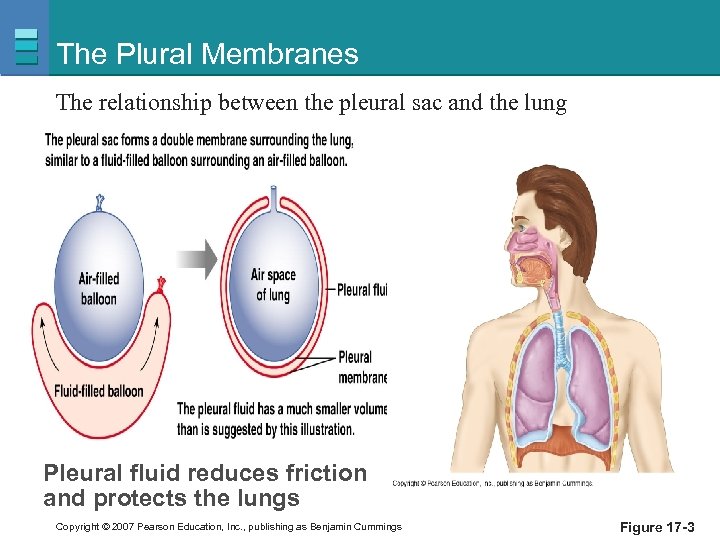
The Plural Membranes The relationship between the pleural sac and the lung Pleural fluid reduces friction and protects the lungs Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings Figure 17 -3
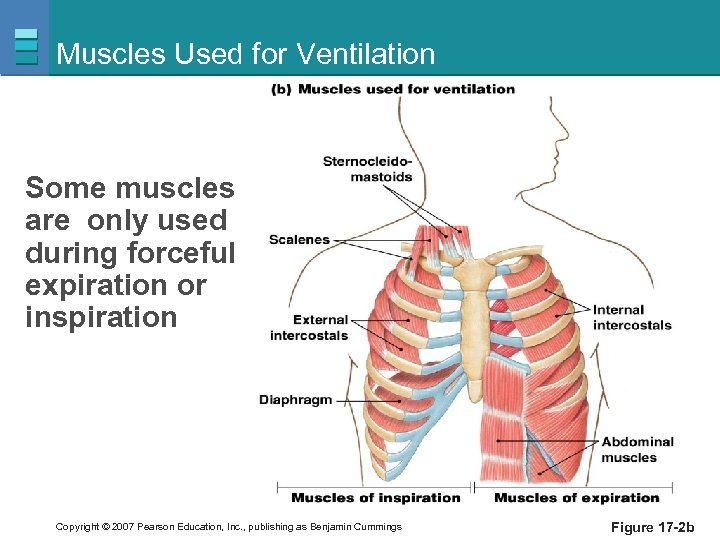
Muscles Used for Ventilation Some muscles are only used during forceful expiration or inspiration Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings Figure 17 -2 b
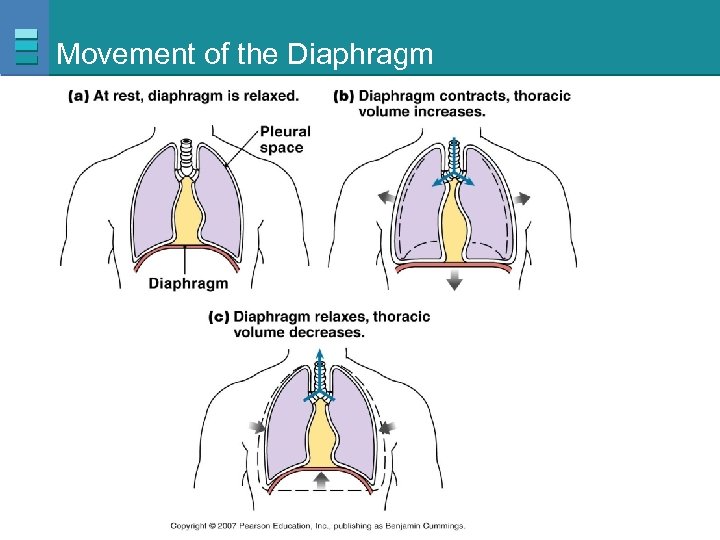
Movement of the Diaphragm Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings
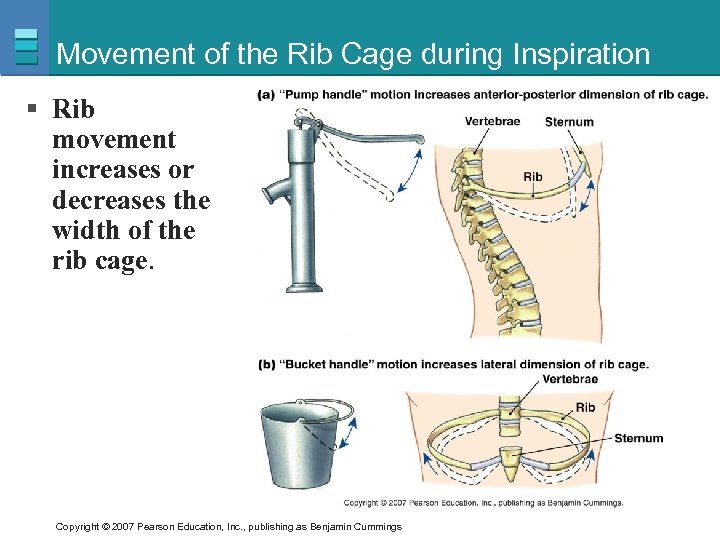
Movement of the Rib Cage during Inspiration § Rib movement increases or decreases the width of the rib cage. Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings
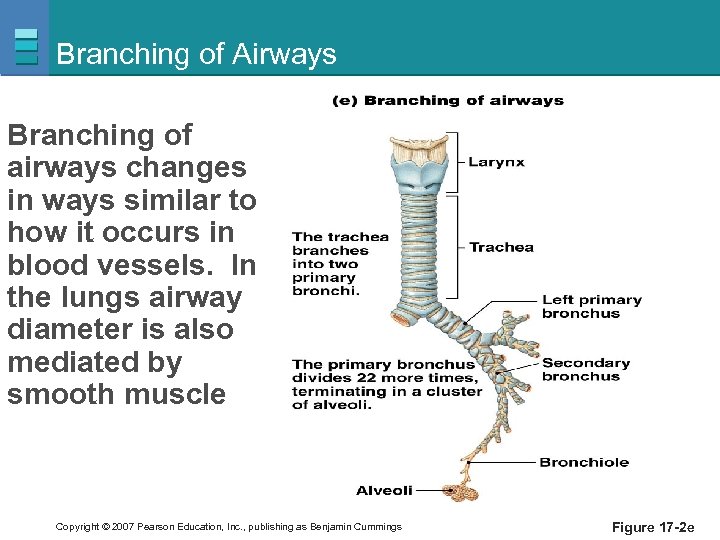
Branching of Airways Branching of airways changes in ways similar to how it occurs in blood vessels. In the lungs airway diameter is also mediated by smooth muscle Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings Figure 17 -2 e
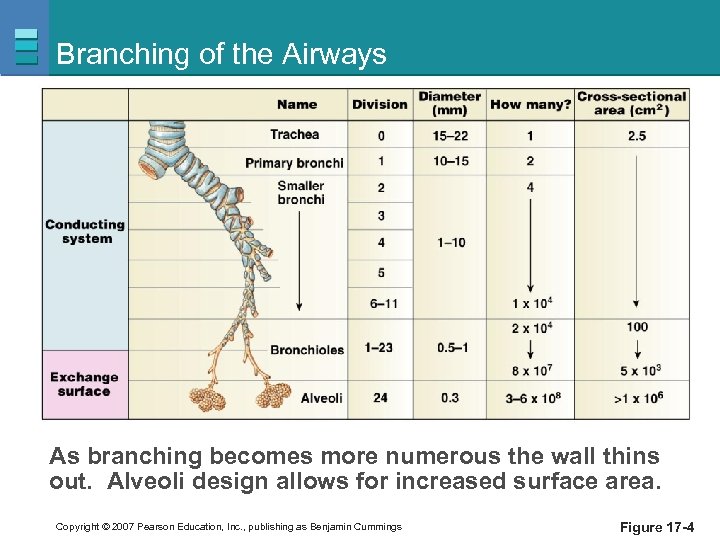
Branching of the Airways As branching becomes more numerous the wall thins out. Alveoli design allows for increased surface area. Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings Figure 17 -4
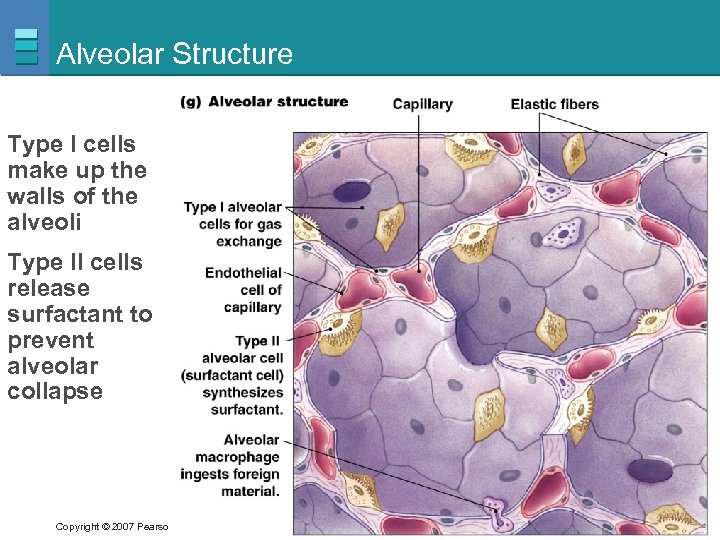
Alveolar Structure Type I cells make up the walls of the alveoli Type II cells release surfactant to prevent alveolar collapse Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings Figure 17 -2 g
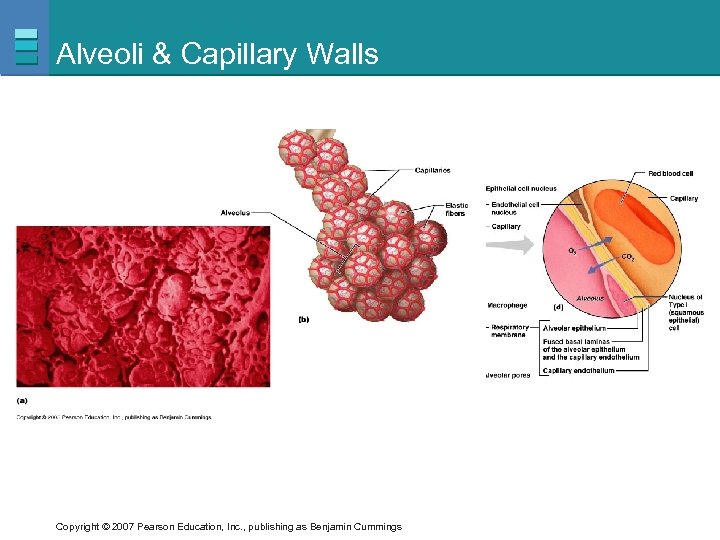
Alveoli & Capillary Walls Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings
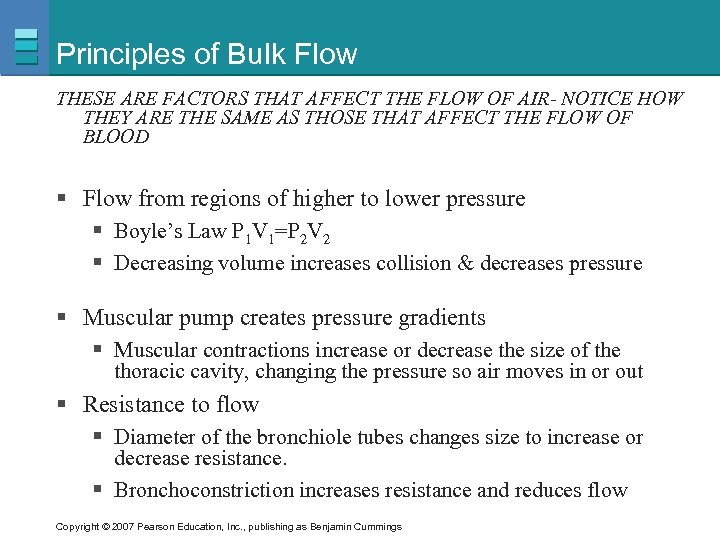
Principles of Bulk Flow THESE ARE FACTORS THAT AFFECT THE FLOW OF AIR- NOTICE HOW THEY ARE THE SAME AS THOSE THAT AFFECT THE FLOW OF BLOOD § Flow from regions of higher to lower pressure § Boyle’s Law P 1 V 1=P 2 V 2 § Decreasing volume increases collision & decreases pressure § Muscular pump creates pressure gradients § Muscular contractions increase or decrease the size of the thoracic cavity, changing the pressure so air moves in or out § Resistance to flow § Diameter of the bronchiole tubes changes size to increase or decrease resistance. § Bronchoconstriction increases resistance and reduces flow Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings
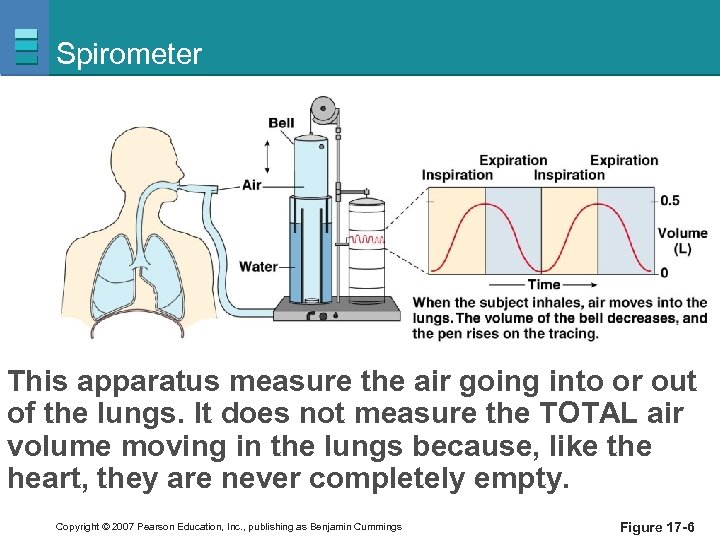
Spirometer This apparatus measure the air going into or out of the lungs. It does not measure the TOTAL air volume moving in the lungs because, like the heart, they are never completely empty. Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings Figure 17 -6
Air Flow § Flow P/R = air flows due to pressure gradient and decreased with increased resistance § Alveolar pressure or intrapleural pressure can be measured = the amount of air that moves in/out can be used to infer pressure § Single respiratory cycle consists of inspiration followed by expiration= remember- there is quiet and forced breathing Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings
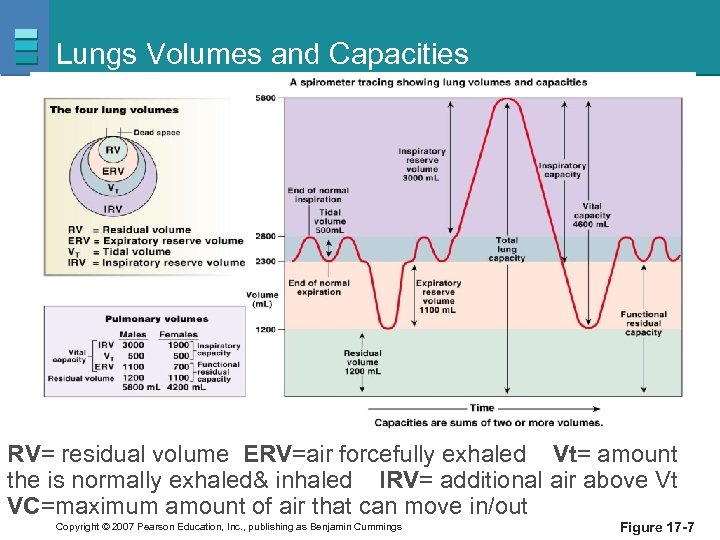
Lungs Volumes and Capacities RV= residual volume ERV=air forcefully exhaled Vt= amount the is normally exhaled& inhaled IRV= additional air above Vt VC=maximum amount of air that can move in/out Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings Figure 17 -7
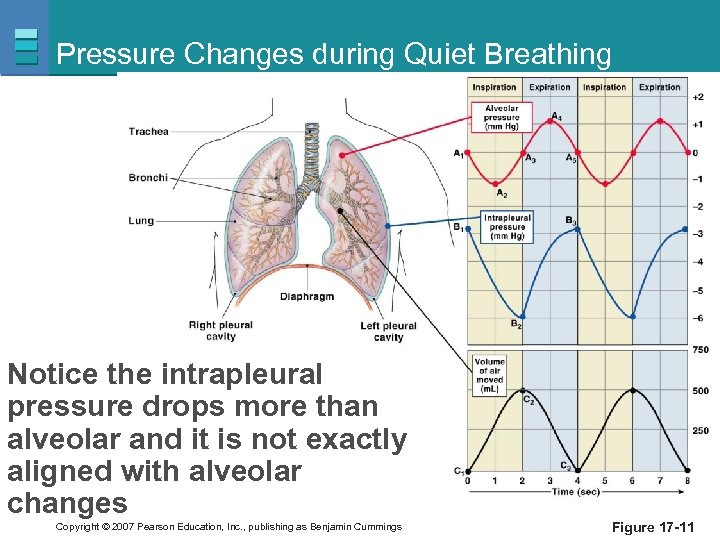
Pressure Changes during Quiet Breathing Notice the intrapleural pressure drops more than alveolar and it is not exactly aligned with alveolar changes Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings Figure 17 -11
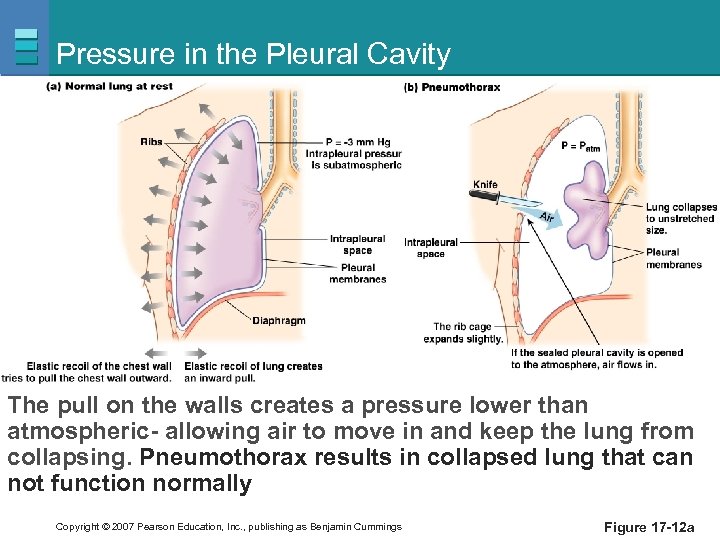
Pressure in the Pleural Cavity The pull on the walls creates a pressure lower than atmospheric- allowing air to move in and keep the lung from collapsing. Pneumothorax results in collapsed lung that can not function normally Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings Figure 17 -12 a
Compliance and Elastance § Compliance: ability to stretch § High compliance- not a helpful condition in lungs § Stretches easily- but has low recoil thus its hard to exhale § Low compliance § Requires more force- more work is needed to stretch a stiff lung § Restrictive lung diseases- pathology decreasing compliance § Fibrotic lung diseases and inadequate surfactant production- inelastic scar tissue and alveolar walls that stick together § Elastance: returning to its resting volume when stretching force is released Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings
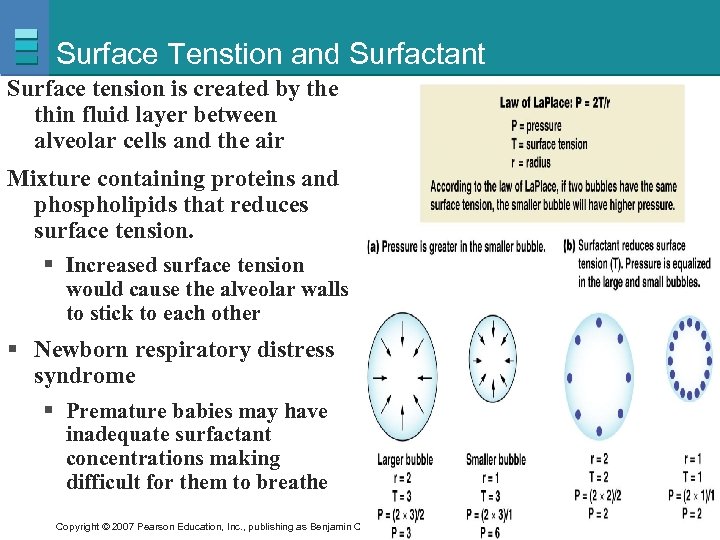
Surface Tenstion and Surfactant Surface tension is created by the thin fluid layer between alveolar cells and the air Mixture containing proteins and phospholipids that reduces surface tension. § Increased surface tension would cause the alveolar walls to stick to each other § Newborn respiratory distress syndrome § Premature babies may have inadequate surfactant concentrations making difficult for them to breathe Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings
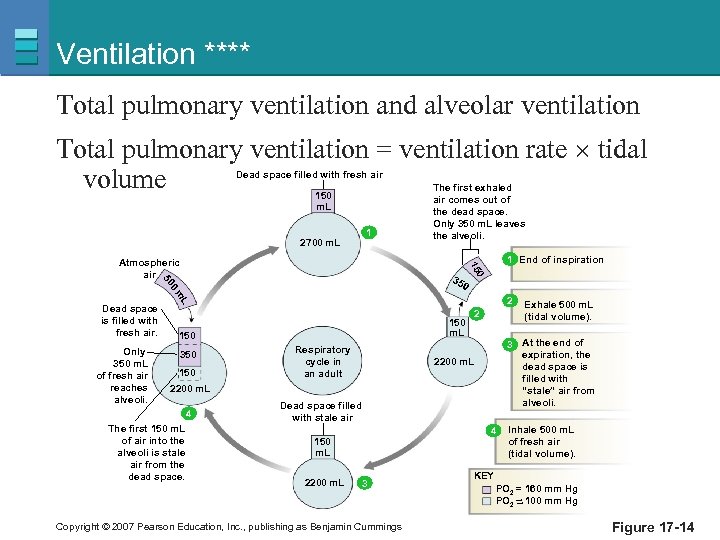
Ventilation **** Total pulmonary ventilation and alveolar ventilation Total pulmonary ventilation = ventilation rate tidal volume Dead space filled with fresh air 150 m. L 2700 m. L 1 0 0 m 2 L Only 350 m. L of fresh air reaches alveoli. 0 35 50 Dead space is filled with fresh air. 1 End of inspiration 15 Atmospheric air The first exhaled air comes out of the dead space. Only 350 m. L leaves the alveoli. 150 m. L 150 350 150 Respiratory cycle in an adult 2 3 At the end of expiration, the dead space is filled with “stale” air from alveoli. 2200 m. L 4 The first 150 m. L of air into the alveoli is stale air from the dead space. Dead space filled with stale air 4 150 m. L 2200 m. L 3 Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings Exhale 500 m. L (tidal volume). Inhale 500 m. L of fresh air (tidal volume). KEY PO 2 = 160 mm Hg PO 2 ~ 100 mm Hg ~ Figure 17 -14
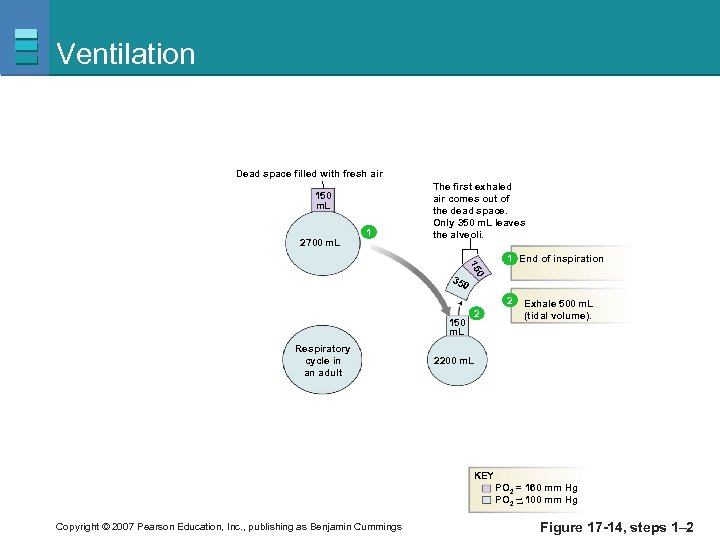
Ventilation Dead space filled with fresh air 150 m. L 2700 m. L 1 The first exhaled air comes out of the dead space. Only 350 m. L leaves the alveoli. 0 15 1 End of inspiration 35 0 2 150 m. L Respiratory cycle in an adult 2 Exhale 500 m. L (tidal volume). 2200 m. L KEY PO 2 = 160 mm Hg PO 2 ~ 100 mm Hg ~ Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings Figure 17 -14, steps 1– 2
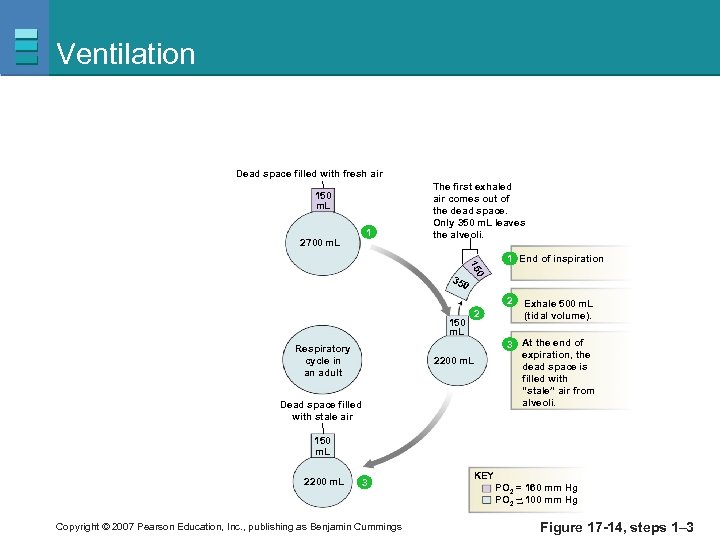
Ventilation Dead space filled with fresh air 150 m. L 2700 m. L 1 The first exhaled air comes out of the dead space. Only 350 m. L leaves the alveoli. 0 15 1 End of inspiration 35 0 2 150 m. L Respiratory cycle in an adult 2 2200 m. L Dead space filled with stale air Exhale 500 m. L (tidal volume). 3 At the end of expiration, the dead space is filled with “stale” air from alveoli. 150 m. L 2200 m. L 3 Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings KEY PO 2 = 160 mm Hg PO 2 ~ 100 mm Hg ~ Figure 17 -14, steps 1– 3
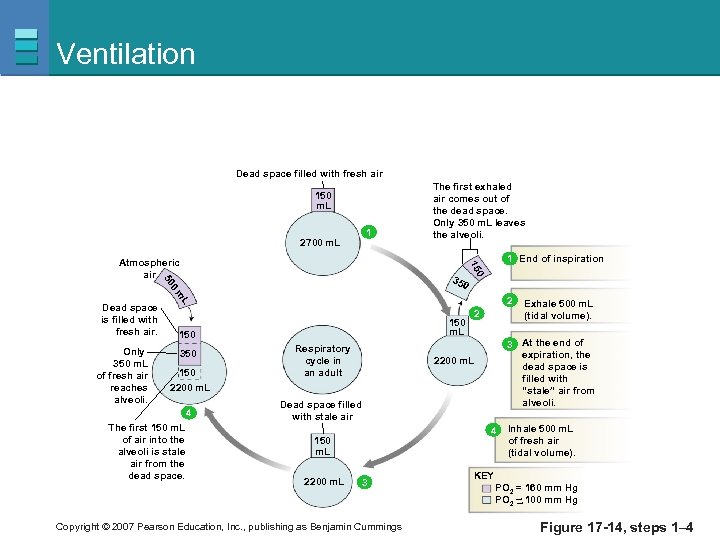
Ventilation Dead space filled with fresh air 150 m. L 2700 m. L 1 0 0 m 2 L Only 350 m. L of fresh air reaches alveoli. 0 35 50 Dead space is filled with fresh air. 1 End of inspiration 15 Atmospheric air The first exhaled air comes out of the dead space. Only 350 m. L leaves the alveoli. 150 m. L 150 350 150 2 Respiratory cycle in an adult 3 At the end of expiration, the dead space is filled with “stale” air from alveoli. 2200 m. L 4 The first 150 m. L of air into the alveoli is stale air from the dead space. Dead space filled with stale air 4 150 m. L 2200 m. L 3 Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings Exhale 500 m. L (tidal volume). Inhale 500 m. L of fresh air (tidal volume). KEY PO 2 = 160 mm Hg PO 2 ~ 100 mm Hg ~ Figure 17 -14, steps 1– 4
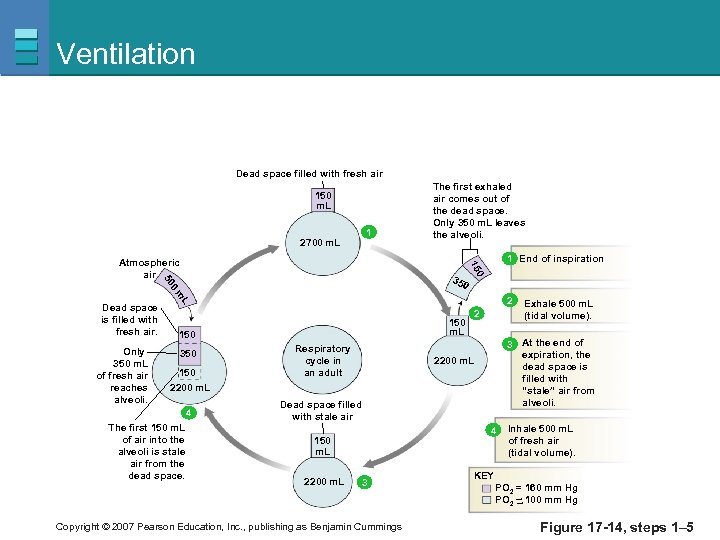
Ventilation Dead space filled with fresh air 150 m. L 2700 m. L 1 0 0 m 2 L Only 350 m. L of fresh air reaches alveoli. 0 35 50 Dead space is filled with fresh air. 1 End of inspiration 15 Atmospheric air The first exhaled air comes out of the dead space. Only 350 m. L leaves the alveoli. 150 m. L 150 350 150 2 Respiratory cycle in an adult 3 At the end of expiration, the dead space is filled with “stale” air from alveoli. 2200 m. L 4 The first 150 m. L of air into the alveoli is stale air from the dead space. Dead space filled with stale air 4 150 m. L 2200 m. L 3 Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings Exhale 500 m. L (tidal volume). Inhale 500 m. L of fresh air (tidal volume). KEY PO 2 = 160 mm Hg PO 2 ~ 100 mm Hg ~ Figure 17 -14, steps 1– 5
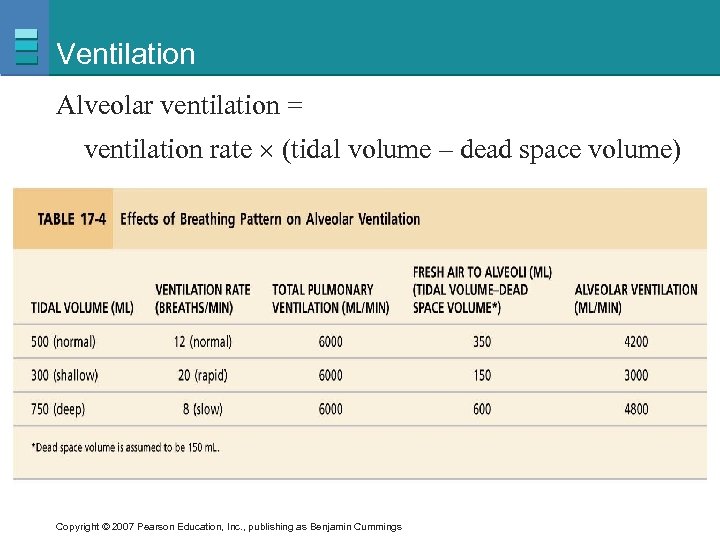
Ventilation Alveolar ventilation = ventilation rate (tidal volume – dead space volume) Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings
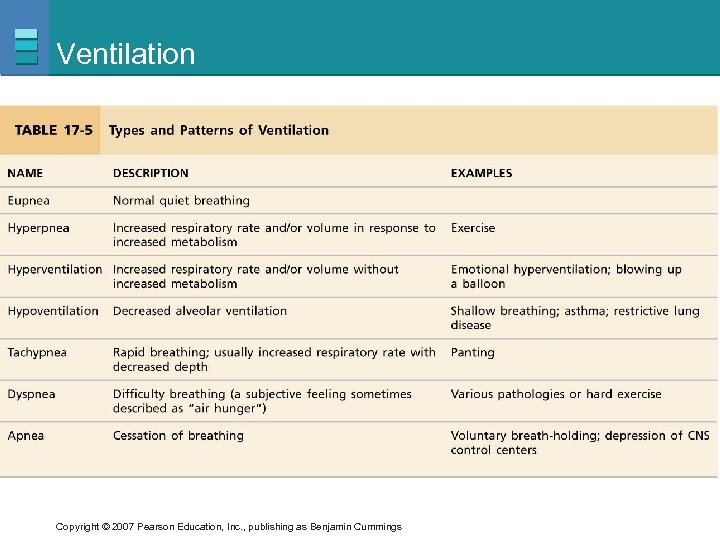
Ventilation Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings
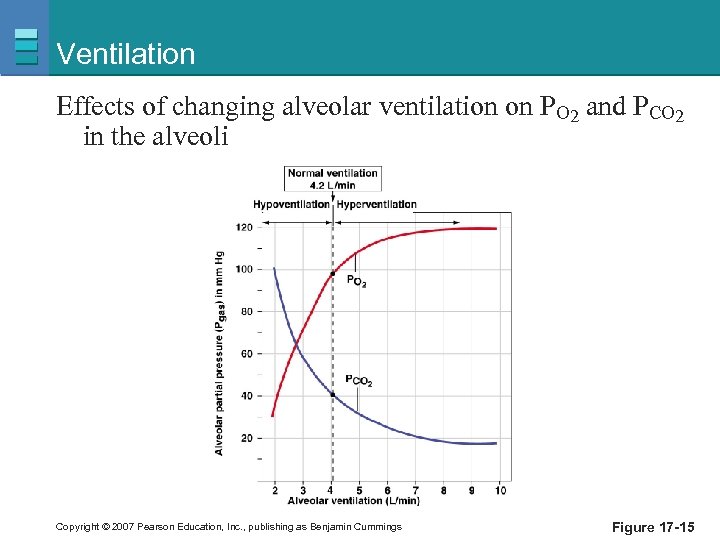
Ventilation Effects of changing alveolar ventilation on PO 2 and PCO 2 in the alveoli Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings Figure 17 -15
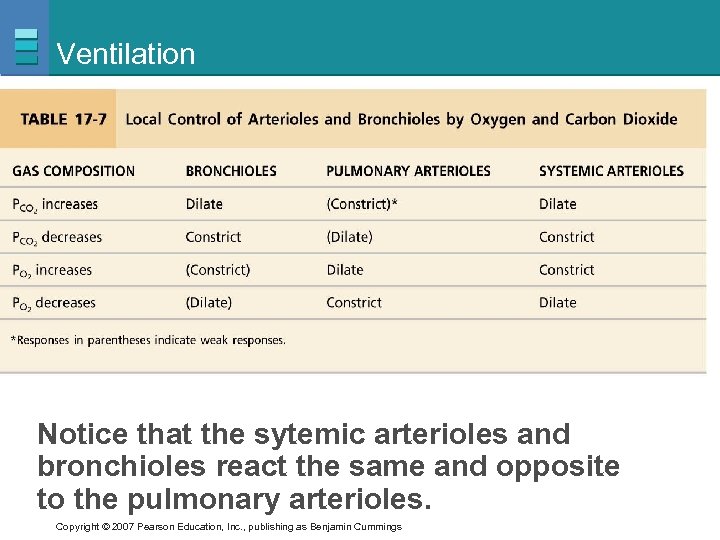
Ventilation Notice that the sytemic arterioles and bronchioles react the same and opposite to the pulmonary arterioles. Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings
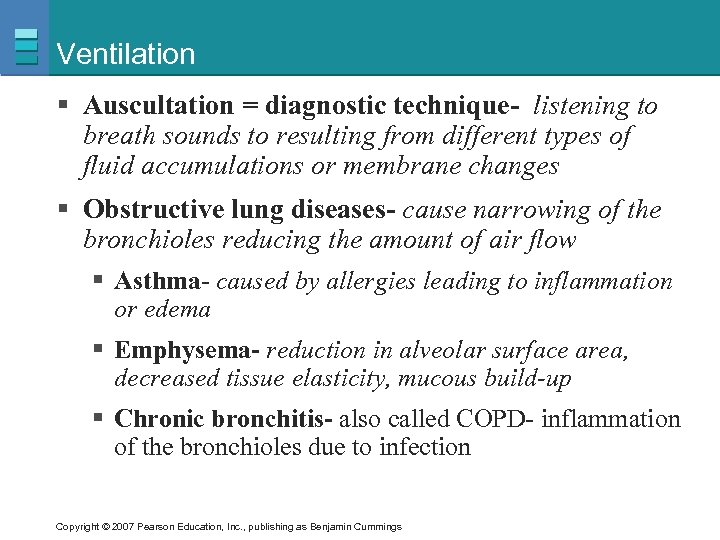
Ventilation § Auscultation = diagnostic technique- listening to breath sounds to resulting from different types of fluid accumulations or membrane changes § Obstructive lung diseases- cause narrowing of the bronchioles reducing the amount of air flow § Asthma- caused by allergies leading to inflammation or edema § Emphysema- reduction in alveolar surface area, decreased tissue elasticity, mucous build-up § Chronic bronchitis- also called COPD- inflammation of the bronchioles due to infection Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings
Causes of Low Alveolar PO 2 (Chapter 18) § Inspired air has abnormally low oxygen content § Altitude § Alveolar ventilation is inadequate § Decreased lung compliance § Increased airway resistance § Overdose of drugs § Pathological changes § Decrease in amount of alveolar surface area § Increase in thickness of alveolar membrane § Increase in diffusion distance between alveoli and blood Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings
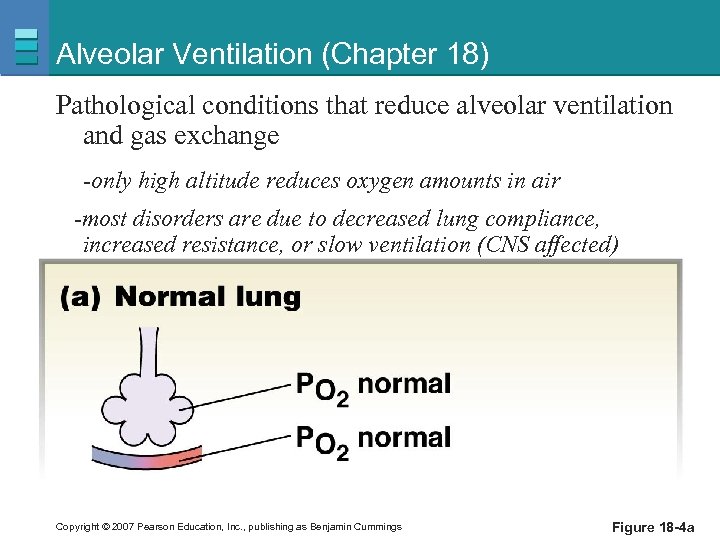
Alveolar Ventilation (Chapter 18) Pathological conditions that reduce alveolar ventilation and gas exchange -only high altitude reduces oxygen amounts in air -most disorders are due to decreased lung compliance, increased resistance, or slow ventilation (CNS affected) Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings Figure 18 -4 a
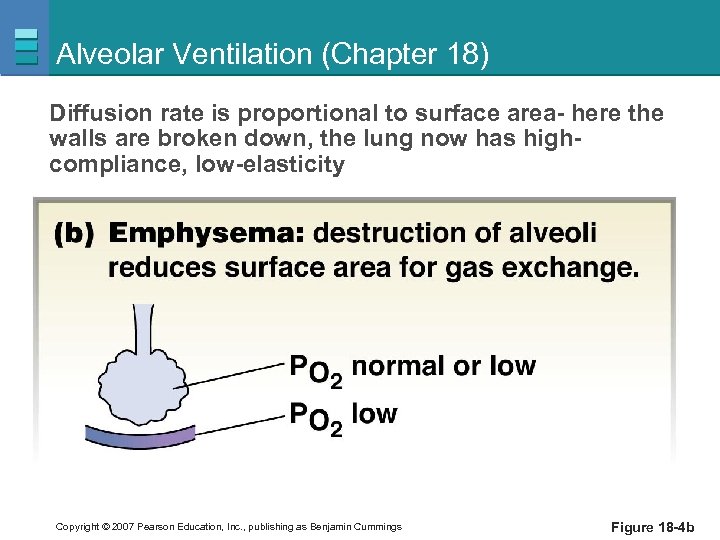
Alveolar Ventilation (Chapter 18) Diffusion rate is proportional to surface area- here the walls are broken down, the lung now has highcompliance, low-elasticity Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings Figure 18 -4 b
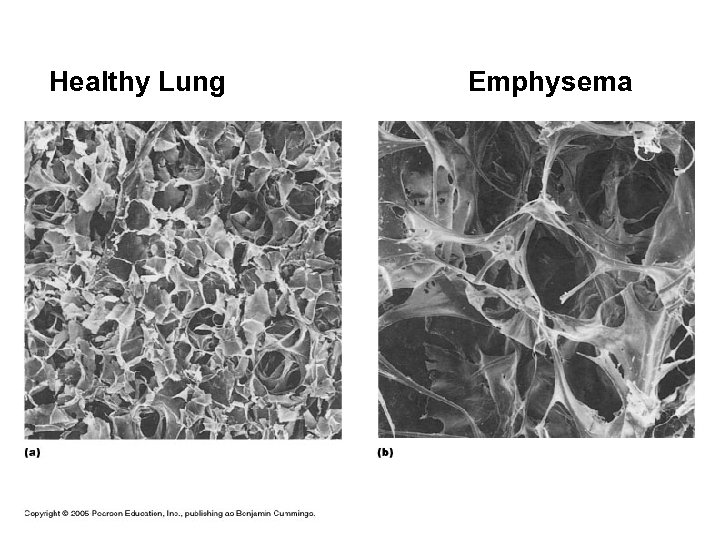
Healthy Lung Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings Emphysema
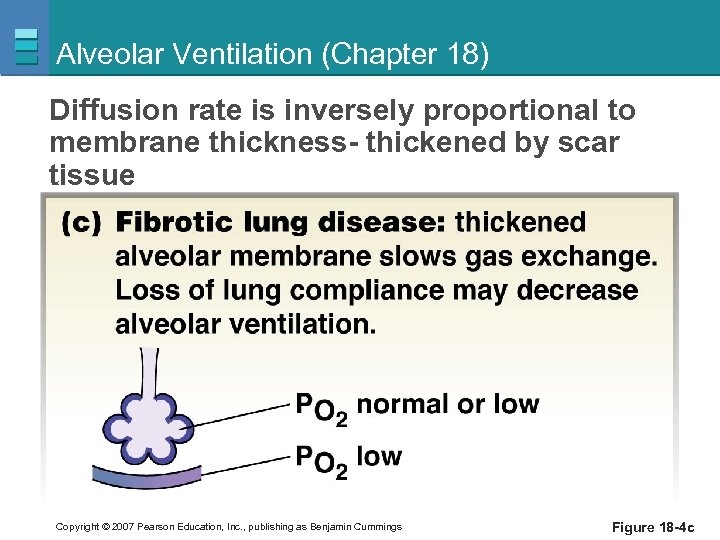
Alveolar Ventilation (Chapter 18) Diffusion rate is inversely proportional to membrane thickness- thickened by scar tissue Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings Figure 18 -4 c
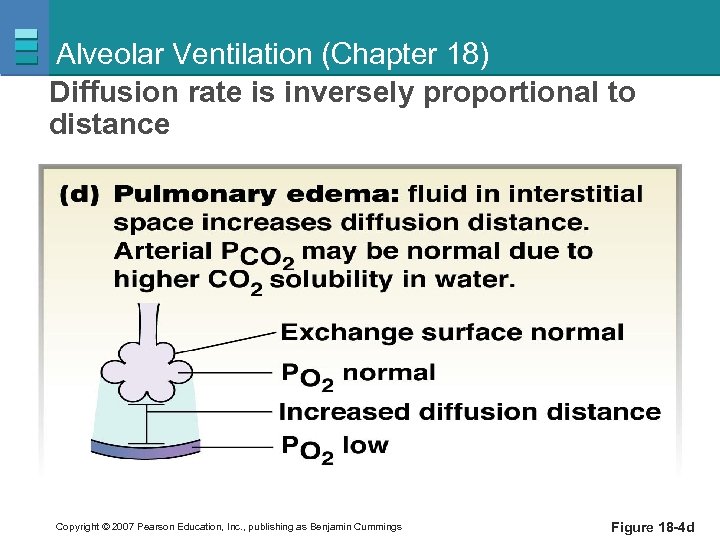
Alveolar Ventilation (Chapter 18) Diffusion rate is inversely proportional to distance Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings Figure 18 -4 d
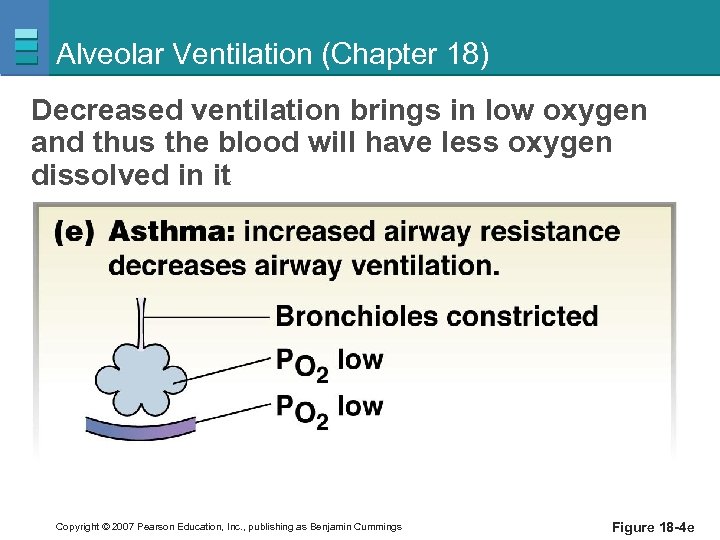
Alveolar Ventilation (Chapter 18) Decreased ventilation brings in low oxygen and thus the blood will have less oxygen dissolved in it Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings Figure 18 -4 e
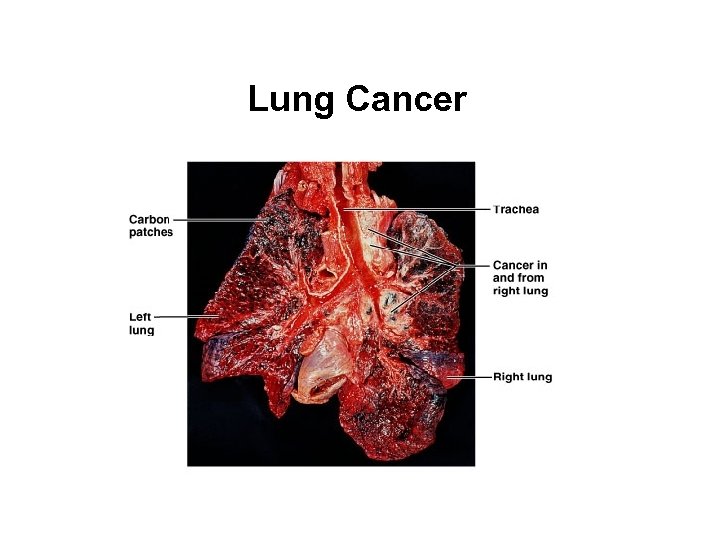
Lung Cancer Copyright © 2007 Pearson Education, Inc. , publishing as Benjamin Cummings
09b4eb3391d6f18ff4b62dcc4d2eba77.ppt