39c7deb78460ac3ff1115bdc760e4f55.ppt
- Количество слайдов: 87
Power. Point® Lecture Slides prepared by Janice Meeking, Mount Royal College CHAPTER 15 The Special Senses: Part A Copyright © 2010 Pearson Education, Inc.
The Eye and Vision • 70% of all sensory receptors are in the eye • Nearly half of the cerebral cortex is involved in processing visual information! • Most of the eye is protected by a cushion of fat and the bony orbit Copyright © 2010 Pearson Education, Inc.
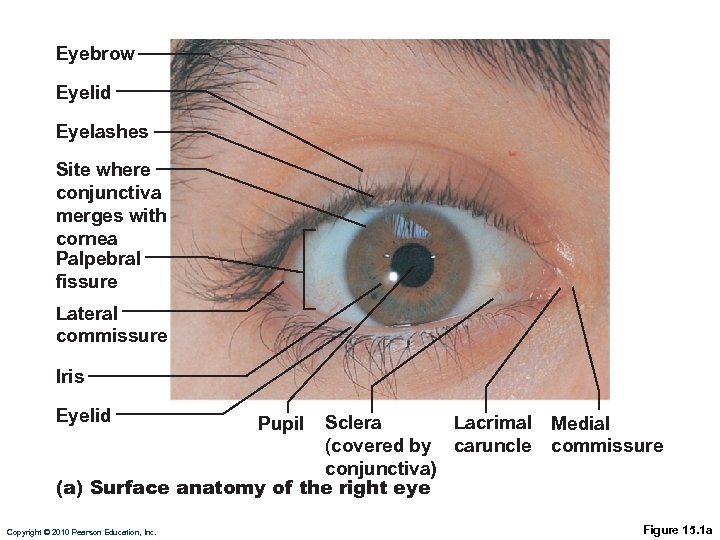
Eyebrow Eyelid Eyelashes Site where conjunctiva merges with cornea Palpebral fissure Lateral commissure Iris Eyelid Sclera Lacrimal (covered by caruncle conjunctiva) (a) Surface anatomy of the right eye Copyright © 2010 Pearson Education, Inc. Pupil Medial commissure Figure 15. 1 a
Eyebrows • Overlie the supraorbital margins • Function in • Shading the eye • Preventing perspiration from reaching the eye Copyright © 2010 Pearson Education, Inc.
Eyelids • Protect the eye anteriorly • Palpebral fissure—slit separating eyelids • Medial & Lateral Canthi – eye angles • Caruncle—fleshy elevation at medial canthus; contains oil and sweat glands • Tarsal plates—internal supporting C. T. sheet • Levator palpebrae superioris—gives the upper eyelid mobility Copyright © 2010 Pearson Education, Inc.
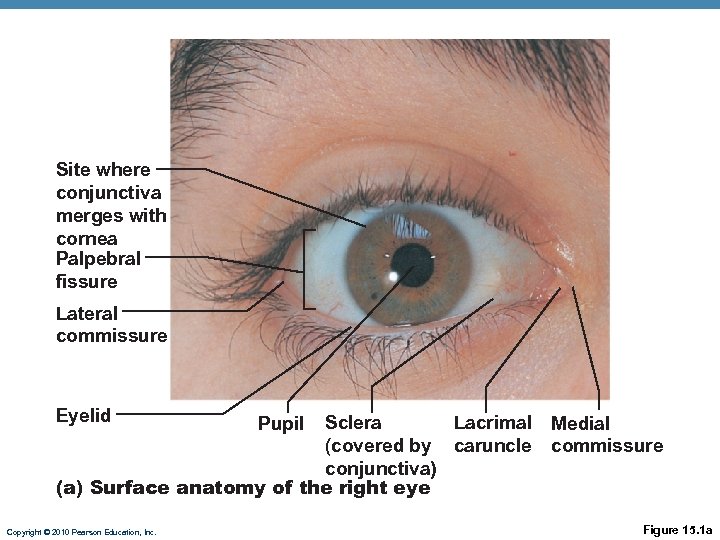
Site where conjunctiva merges with cornea Palpebral fissure Lateral commissure Eyelid Sclera Lacrimal (covered by caruncle conjunctiva) (a) Surface anatomy of the right eye Copyright © 2010 Pearson Education, Inc. Pupil Medial commissure Figure 15. 1 a
Eyelids • Eyelashes • Nerve endings of follicles initiate reflex blinking • Lubricating glands associated with the eyelids • Tarsal glands-sebaceous glands that produce oily secretion to lubricate the eye Copyright © 2010 Pearson Education, Inc.
Conjunctiva • Mucous membranes of the eye • Palpebral conjunctiva: lines the eyelids • Bulbar conjunctiva: covers the white of the eyes (anteriorly) Copyright © 2010 Pearson Education, Inc.
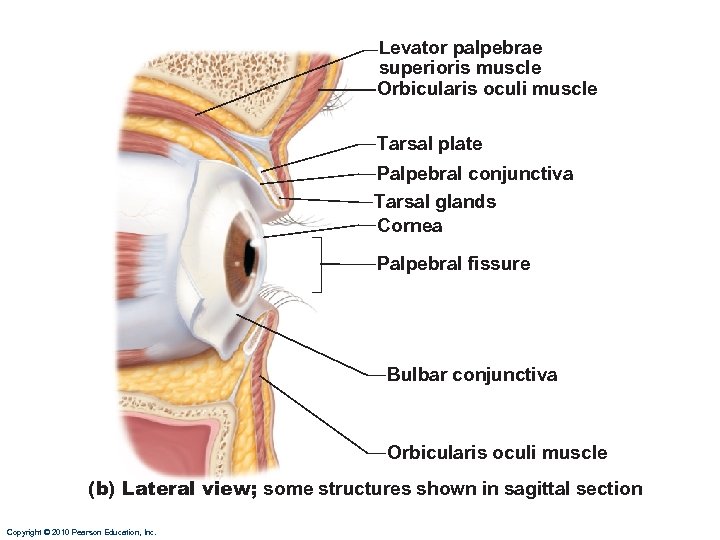
Levator palpebrae superioris muscle Orbicularis oculi muscle Tarsal plate Palpebral conjunctiva Tarsal glands Cornea Palpebral fissure Bulbar conjunctiva Orbicularis oculi muscle (b) Lateral view; some structures shown in sagittal section Copyright © 2010 Pearson Education, Inc.
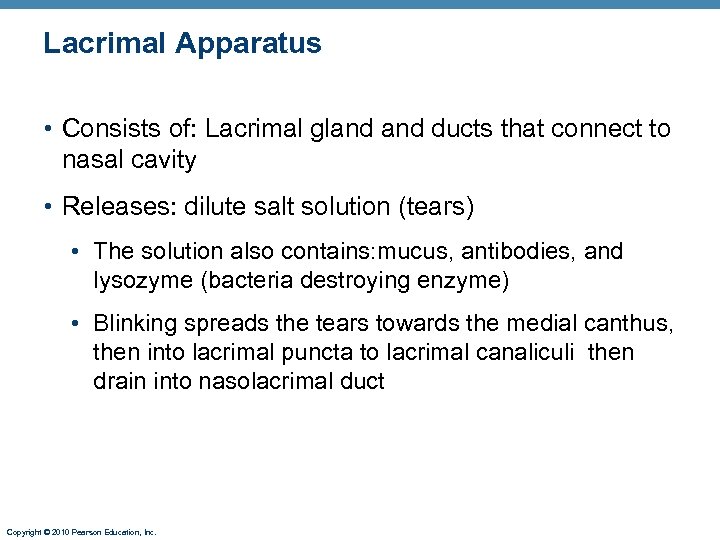
Lacrimal Apparatus • Consists of: Lacrimal gland ducts that connect to nasal cavity • Releases: dilute salt solution (tears) • The solution also contains: mucus, antibodies, and lysozyme (bacteria destroying enzyme) • Blinking spreads the tears towards the medial canthus, then into lacrimal puncta to lacrimal canaliculi then drain into nasolacrimal duct Copyright © 2010 Pearson Education, Inc.
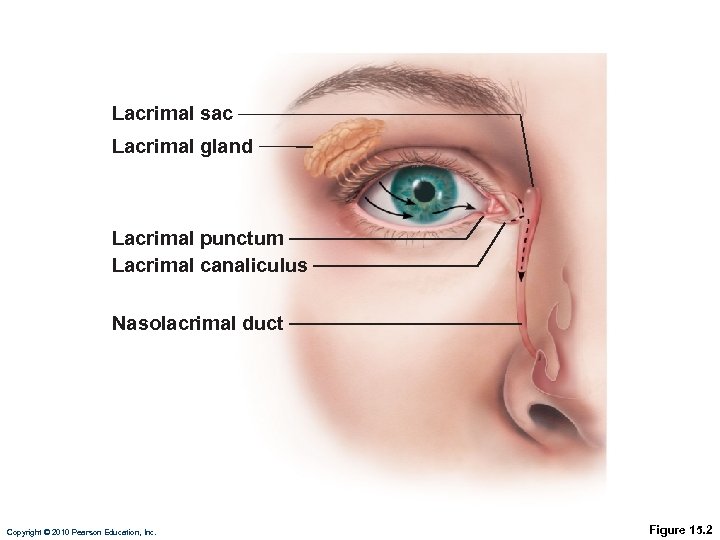
Lacrimal sac Lacrimal gland Lacrimal punctum Lacrimal canaliculus Nasolacrimal duct Copyright © 2010 Pearson Education, Inc. Figure 15. 2
Extrinsic Eye Muscles • The movement of the eye is controlled by six muscles on the external surface of each eye: • Superior rectus: elevates eye • Inferior rectus: depresses eye • Lateral rectus: moves eye laterally • Medial rectus: moves eye medially • Inferior oblique: moves eye up and out • Superior oblique: moves eye down and out Copyright © 2010 Pearson Education, Inc.
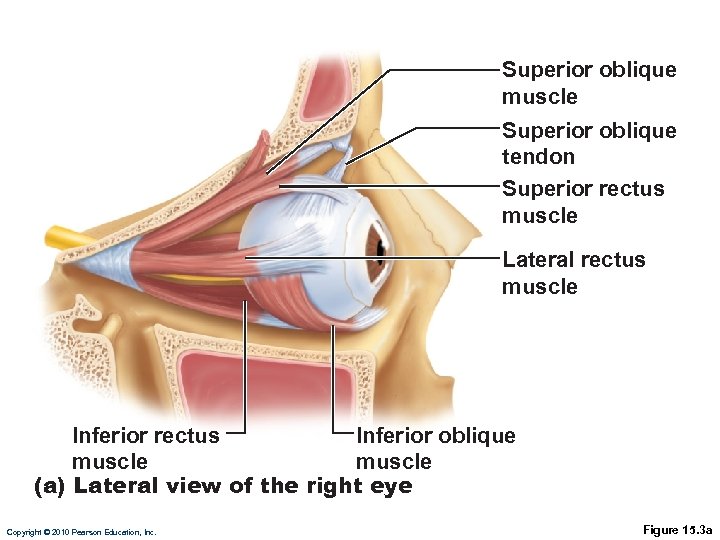
Superior oblique muscle Superior oblique tendon Superior rectus muscle Lateral rectus muscle Inferior rectus Inferior oblique muscle (a) Lateral view of the right eye Copyright © 2010 Pearson Education, Inc. Figure 15. 3 a
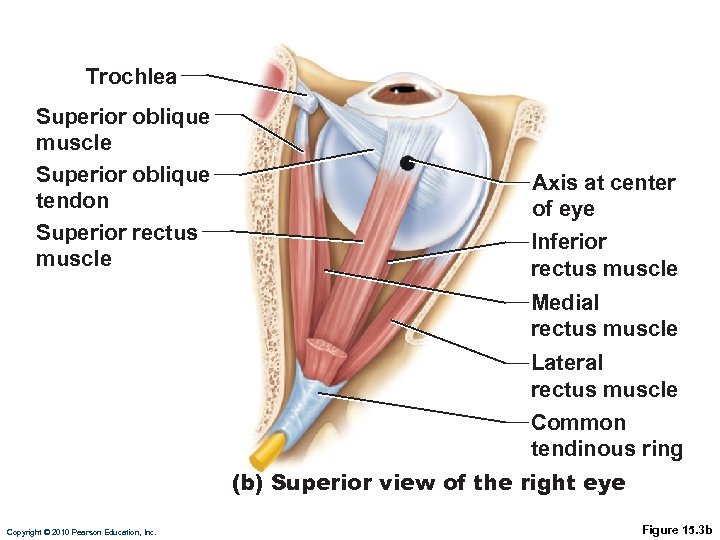
Trochlea Superior oblique muscle Superior oblique tendon Superior rectus muscle Axis at center of eye Inferior rectus muscle Medial rectus muscle Lateral rectus muscle Common tendinous ring (b) Superior view of the right eye Copyright © 2010 Pearson Education, Inc. Figure 15. 3 b
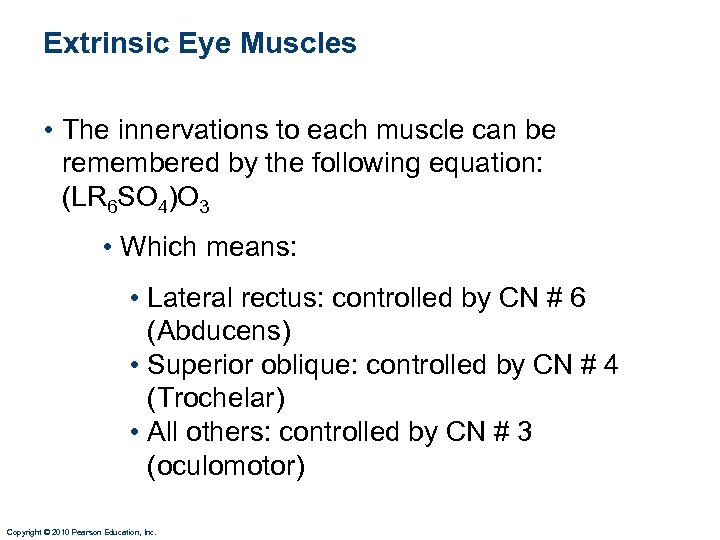
Extrinsic Eye Muscles • The innervations to each muscle can be remembered by the following equation: (LR 6 SO 4)O 3 • Which means: • Lateral rectus: controlled by CN # 6 (Abducens) • Superior oblique: controlled by CN # 4 (Trochelar) • All others: controlled by CN # 3 (oculomotor) Copyright © 2010 Pearson Education, Inc.
Structure of the Eyeball • Wall of eyeball contains three layers • Fibrous • Vascular • Sensory Copyright © 2010 Pearson Education, Inc.
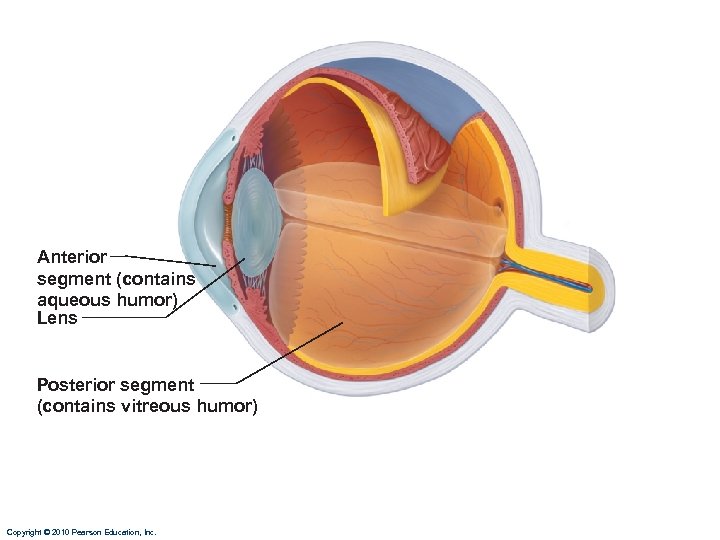
Anterior segment (contains aqueous humor) Lens Posterior segment (contains vitreous humor) Copyright © 2010 Pearson Education, Inc.
Fibrous Layer • Outermost layer of dense avascular CT • Two regions: sclera and cornea 1. Sclera: • Opaque posterior region 2. Cornea: • Transparent anterior part Copyright © 2010 Pearson Education, Inc.
Vascular Layer • Middle layer • Three regions: choroid, ciliary body, and iris 1. Choroid region • Posterior portion • Supplies blood to most of eyeball • Brown pigment absorbs light to prevent its scattering Copyright © 2010 Pearson Education, Inc.
Vascular Layer 2. Ciliary body • Ring of smooth muscle attached to and surrounding the lens • Ciliary zonule (suspensory ligament): holds lens in position Copyright © 2010 Pearson Education, Inc.
Vascular Layer 3. Iris (smooth muscle) • The anterior colored part of the eye • Pupil: central opening of iris; the iris regulates the amount of light entering the eye • Close vision and bright light- pupils constrict • Distant and dim light- pupils dilate Copyright © 2010 Pearson Education, Inc.
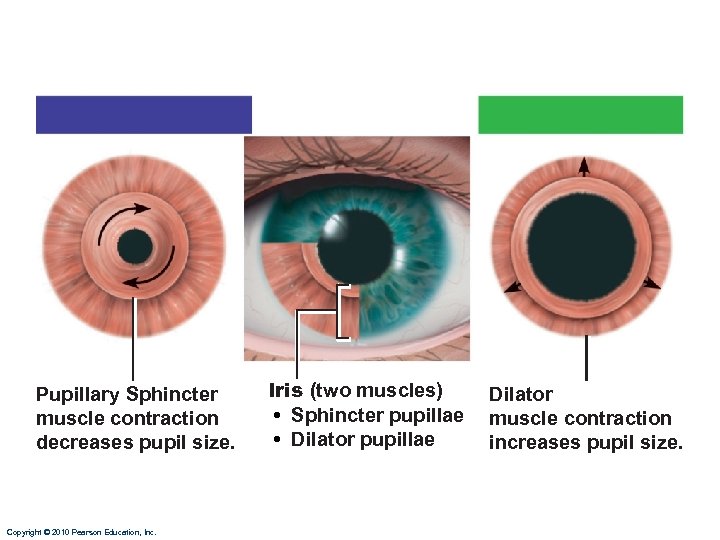
Pupillary Sphincter muscle contraction decreases pupil size. Copyright © 2010 Pearson Education, Inc. Iris (two muscles) • Sphincter pupillae • Dilator pupillae Dilator muscle contraction increases pupil size.
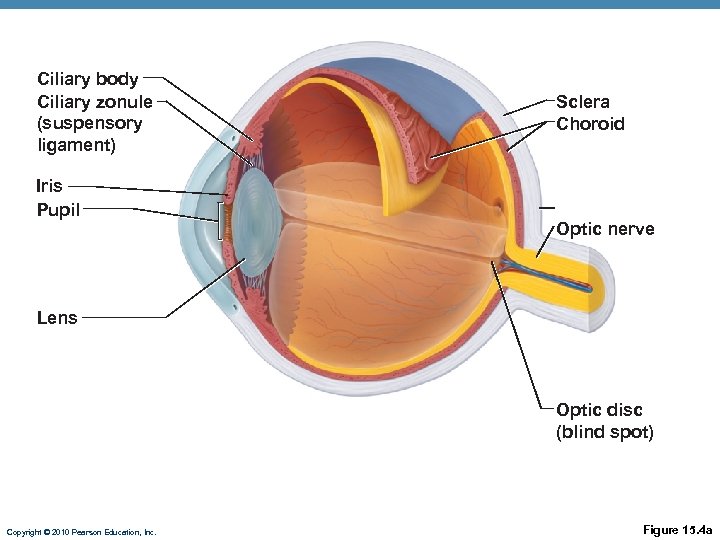
Ciliary body Ciliary zonule (suspensory ligament) Iris Pupil Sclera Choroid Optic nerve Lens Optic disc (blind spot) Copyright © 2010 Pearson Education, Inc. Figure 15. 4 a
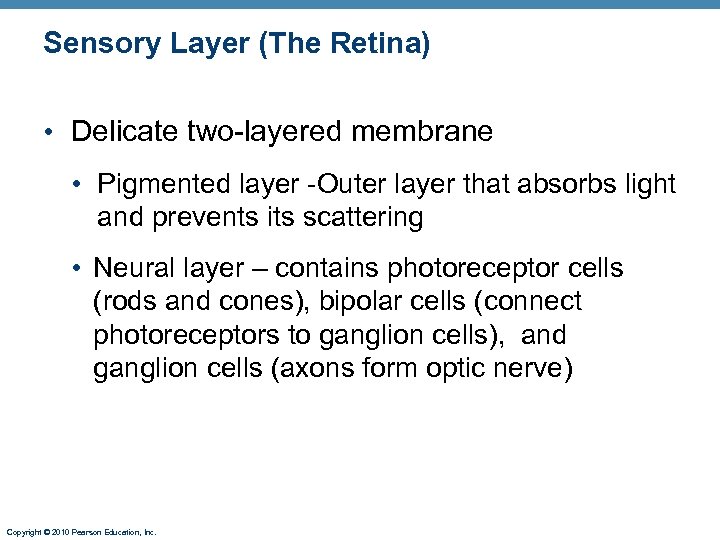
Sensory Layer (The Retina) • Delicate two-layered membrane • Pigmented layer -Outer layer that absorbs light and prevents its scattering • Neural layer – contains photoreceptor cells (rods and cones), bipolar cells (connect photoreceptors to ganglion cells), and ganglion cells (axons form optic nerve) Copyright © 2010 Pearson Education, Inc.
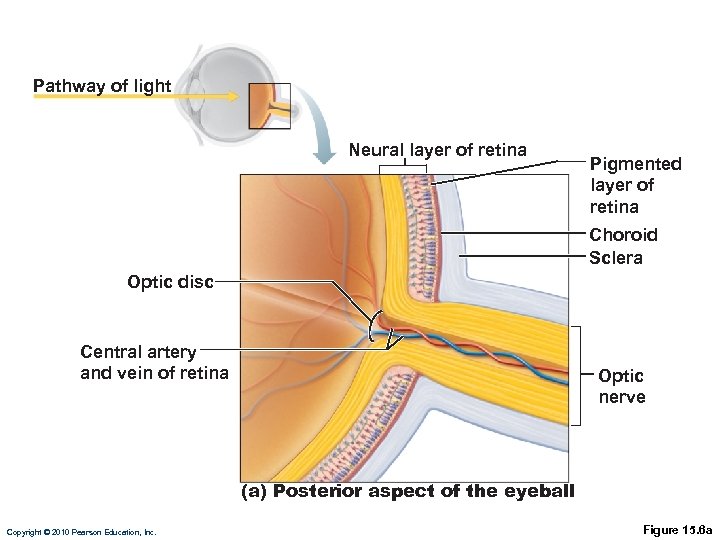
Pathway of light Neural layer of retina Pigmented layer of retina Choroid Sclera Optic disc Central artery and vein of retina Optic nerve (a) Posterior aspect of the eyeball Copyright © 2010 Pearson Education, Inc. Figure 15. 6 a
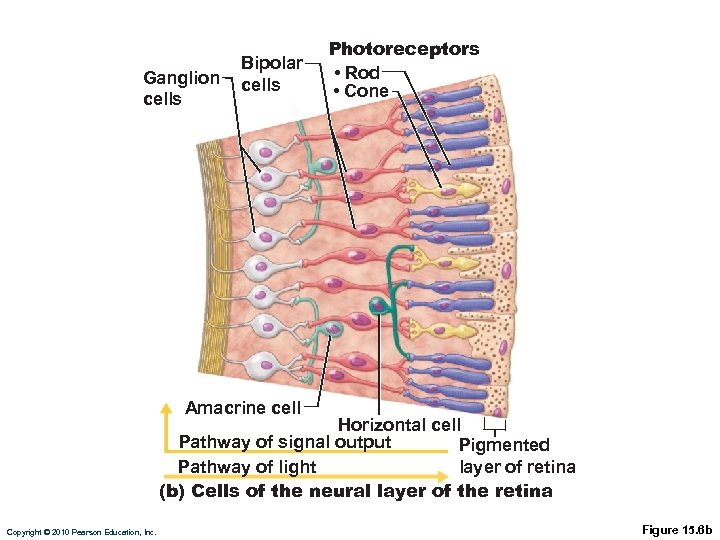
Ganglion cells Bipolar cells Photoreceptors • Rod • Cone Amacrine cell Horizontal cell Pathway of signal output Pigmented layer of retina Pathway of light (b) Cells of the neural layer of the retina Copyright © 2010 Pearson Education, Inc. Figure 15. 6 b
Photoreceptors • Rods • More numerous at peripheral region of retina, away from the fovea centralis (area of retina containing only cones) • Operate in dim light • Provide indistinct, fuzzy, non color peripheral vision Copyright © 2010 Pearson Education, Inc.
Photoreceptors • Cones • Densest in center of retina and concentrated in an area called the fovea centralis (next to blind spot) • Operate in bright light • Provide high-acuity color vision Copyright © 2010 Pearson Education, Inc.
Photoreceptors • Photoreceptor cells are distributed over entire retina except where the optic nerve leaves the eye called the blind spot Copyright © 2010 Pearson Education, Inc.
Cones • There are three types of cones named for the colors of light absorbed: blue, green, and red • Intermediate hues are perceived by activation of more than one type of cone at the same time • Color blindness is due to a congenital lack of one or more of the cone types Copyright © 2010 Pearson Education, Inc.
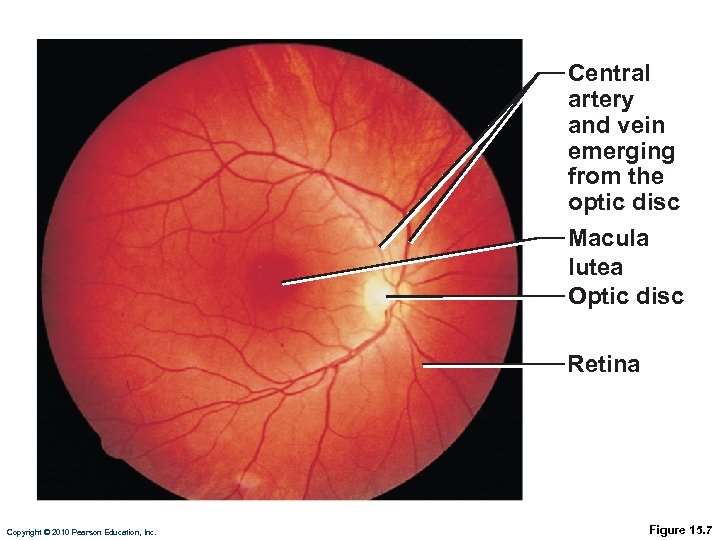
Central artery and vein emerging from the optic disc Macula lutea Optic disc Retina Copyright © 2010 Pearson Education, Inc. Figure 15. 7
Internal Chambers and Fluids • The lens and ciliary zonule separate the anterior and posterior segments • Posterior segment contains vitreous humor that: • A gel like substance which helps reinforce the eye internally Copyright © 2010 Pearson Education, Inc.
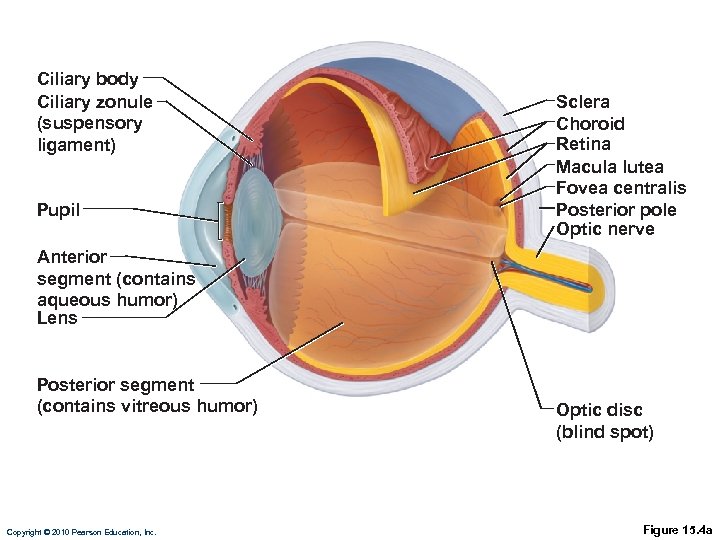
Ciliary body Ciliary zonule (suspensory ligament) Pupil Sclera Choroid Retina Macula lutea Fovea centralis Posterior pole Optic nerve Anterior segment (contains aqueous humor) Lens Posterior segment (contains vitreous humor) Copyright © 2010 Pearson Education, Inc. Optic disc (blind spot) Figure 15. 4 a
Internal Chambers and Fluids • Anterior segment is composed of two chambers • Anterior chamber—between cornea and iris • Posterior chamber—between iris and lens Copyright © 2010 Pearson Education, Inc.
Internal Chambers and Fluids • Anterior segment contains aqueous humor • Watery fluid continuously produced and drained • Glaucoma: compression of the retina and optic nerve if drainage of aqueous humor is blocked Copyright © 2010 Pearson Education, Inc.
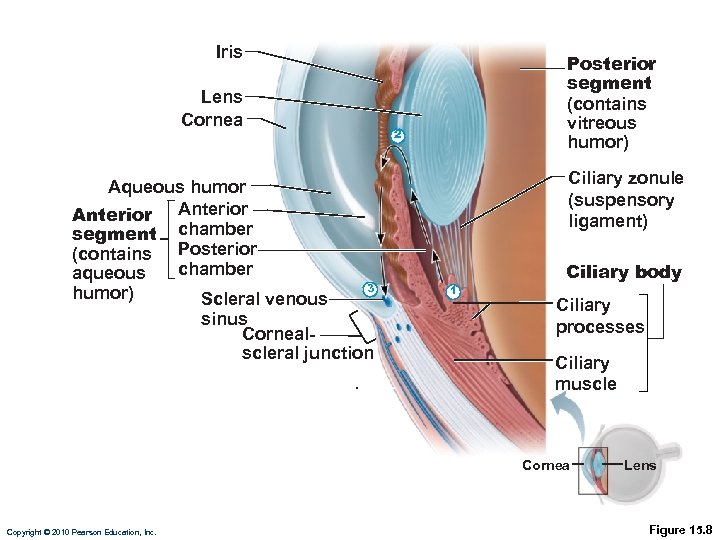
Iris Lens Cornea Aqueous humor Anterior segment chamber (contains Posterior chamber aqueous 3 humor) Scleral venous sinus Cornealscleral junction Posterior segment (contains vitreous humor) 2 Ciliary zonule (suspensory ligament) 1 Ciliary body Ciliary processes Ciliary muscle Cornea Copyright © 2010 Pearson Education, Inc. Lens Figure 15. 8
Lens • Biconvex, transparent, flexible, and avascular • Allows precise focusing of light on the retina • Cataracts (clouding of lens) occur as a consequence of aging, diabetes mellitus, heavy smoking, and frequent exposure to intense sunlight Copyright © 2010 Pearson Education, Inc.
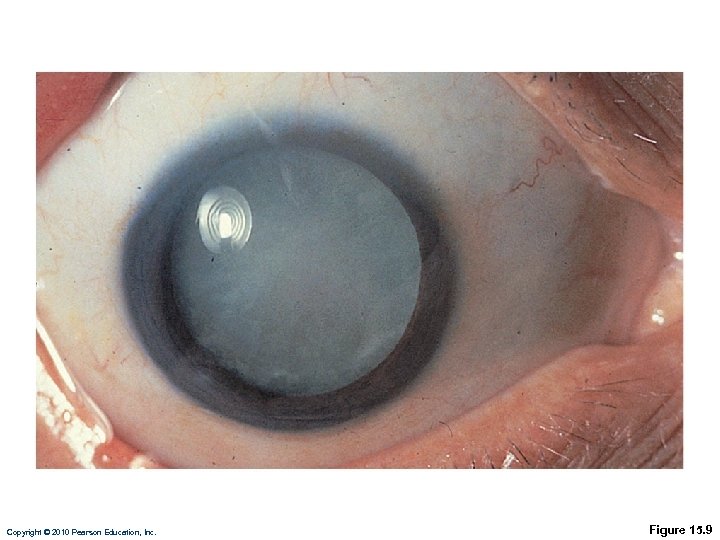
Copyright © 2010 Pearson Education, Inc. Figure 15. 9
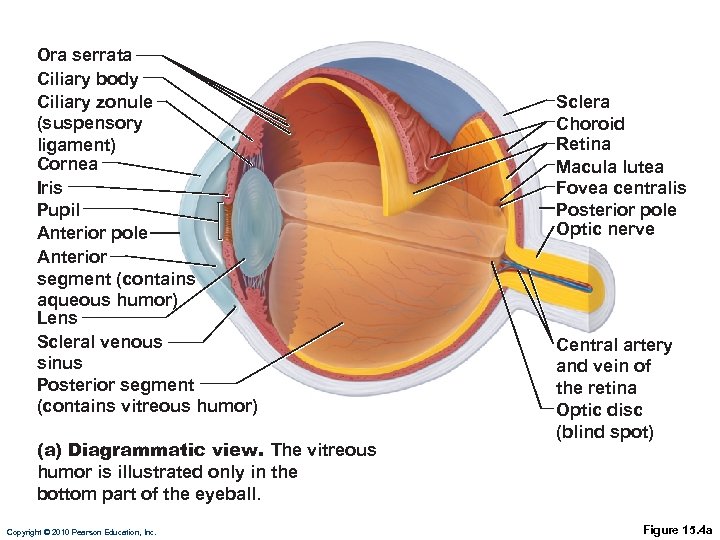
Ora serrata Ciliary body Ciliary zonule (suspensory ligament) Cornea Iris Pupil Anterior pole Anterior segment (contains aqueous humor) Lens Scleral venous sinus Posterior segment (contains vitreous humor) (a) Diagrammatic view. The vitreous humor is illustrated only in the bottom part of the eyeball. Copyright © 2010 Pearson Education, Inc. Sclera Choroid Retina Macula lutea Fovea centralis Posterior pole Optic nerve Central artery and vein of the retina Optic disc (blind spot) Figure 15. 4 a
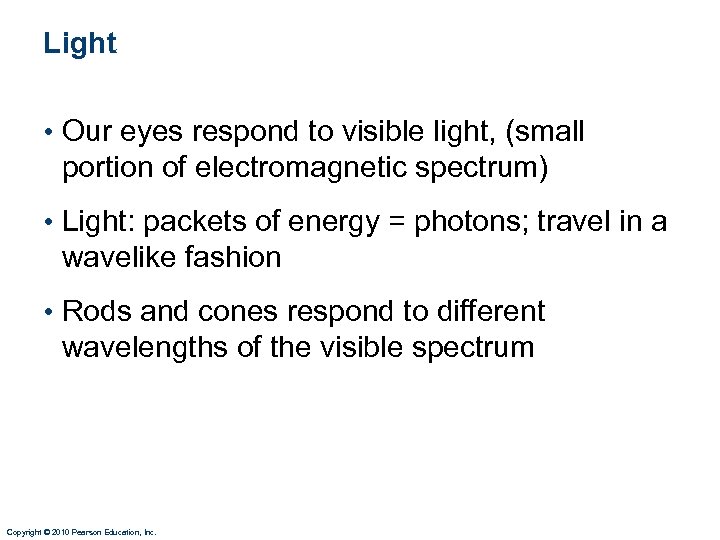
Light • Our eyes respond to visible light, (small portion of electromagnetic spectrum) • Light: packets of energy = photons; travel in a wavelike fashion • Rods and cones respond to different wavelengths of the visible spectrum Copyright © 2010 Pearson Education, Inc.
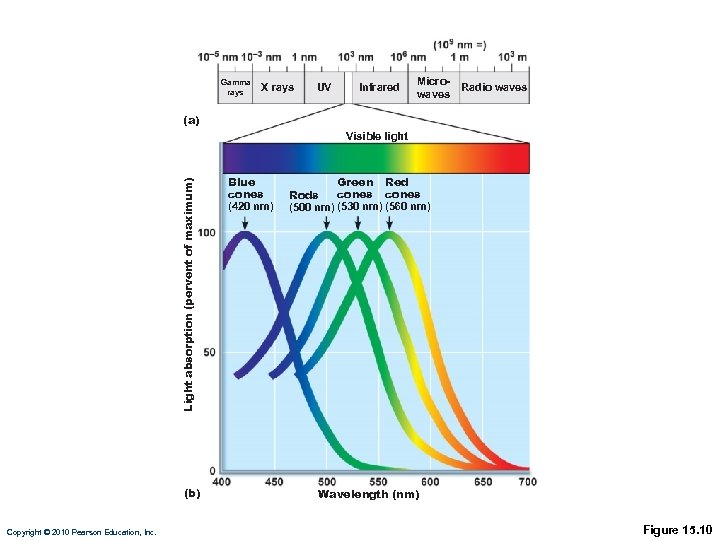
Gamma rays X rays UV Infrared Microwaves Radio waves (a) Light absorption (pervent of maximum) Visible light (b) Copyright © 2010 Pearson Education, Inc. Blue cones (420 nm) Green Red cones Rods (500 nm) (530 nm) (560 nm) Wavelength (nm) Figure 15. 10
Refraction and Lenses • Refraction • Bending of a light ray when light passes from one transparent medium to another Copyright © 2010 Pearson Education, Inc.
Refraction and Lenses • Light passing through a convex lens is: bent so that the rays converge at a focal point • The image formed at the focal point is: upsidedown and reversed right to left Copyright © 2010 Pearson Education, Inc.
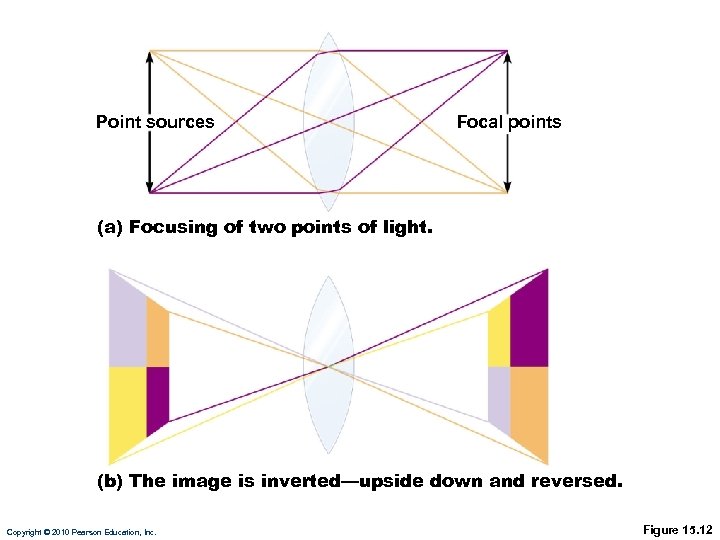
Point sources Focal points (a) Focusing of two points of light. (b) The image is inverted—upside down and reversed. Copyright © 2010 Pearson Education, Inc. Figure 15. 12
Focusing Light on the Retina • Pathway of light entering the eye: cornea, aqueous humor, lens, vitreous humor, neural layer of retina, photoreceptors • Light is refracted • At the cornea • Entering the lens • Leaving the lens • Change in lens curvature allows for fine focusing of an image Copyright © 2010 Pearson Education, Inc.
Focusing for Distant Vision • Light rays from distant objects are parallel and need little refraction • Ciliary muscles are relaxed • Lens is stretched flat by tension in the ciliary zonule Copyright © 2010 Pearson Education, Inc.
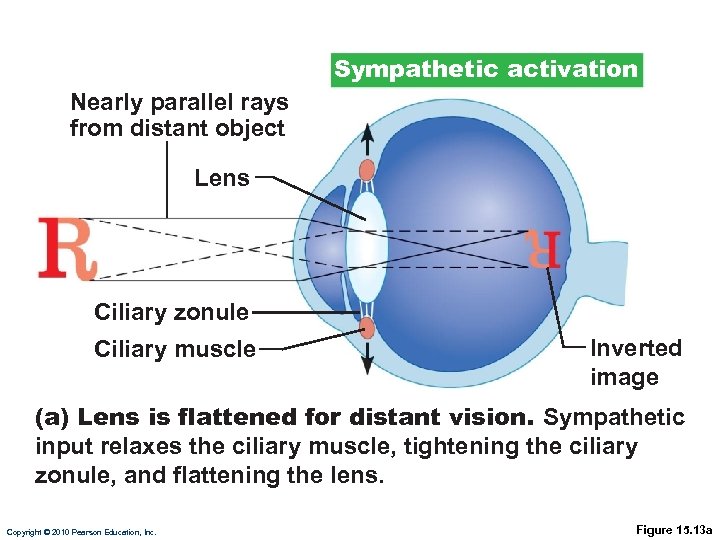
Sympathetic activation Nearly parallel rays from distant object Lens Ciliary zonule Ciliary muscle Inverted image (a) Lens is flattened for distant vision. Sympathetic input relaxes the ciliary muscle, tightening the ciliary zonule, and flattening the lens. Copyright © 2010 Pearson Education, Inc. Figure 15. 13 a
Focusing for Close Vision • Light from a close object diverges as it approaches the eye; requires that the eye make three active adjustments Copyright © 2010 Pearson Education, Inc.
Focusing for Close Vision • Close vision requires • Accommodation—changing the lens shape by ciliary muscles to increase refractory power • Presbyopia—loss of accommodation over age 50 • Constriction—constriction of pupils to prevent the most divergent rays from entering eye • Convergence—medial rotation of the eyeballs toward the object being viewed Copyright © 2010 Pearson Education, Inc.
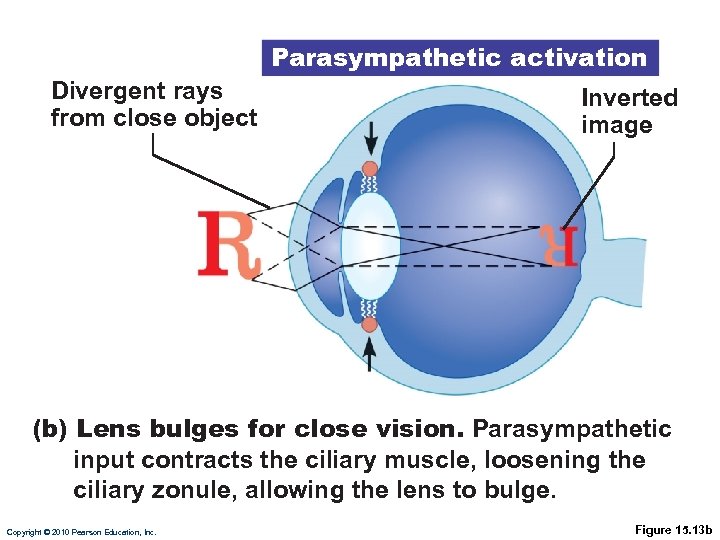
Parasympathetic activation Divergent rays from close object Inverted image (b) Lens bulges for close vision. Parasympathetic input contracts the ciliary muscle, loosening the ciliary zonule, allowing the lens to bulge. Copyright © 2010 Pearson Education, Inc. Figure 15. 13 b
Problems of Refraction • Myopia (nearsightedness)—focal point in front of retina • Hyperopia (farsightedness)—focal point behind retina • Astigmatism—caused by unequal curvatures in different parts of the cornea or lens Copyright © 2010 Pearson Education, Inc.
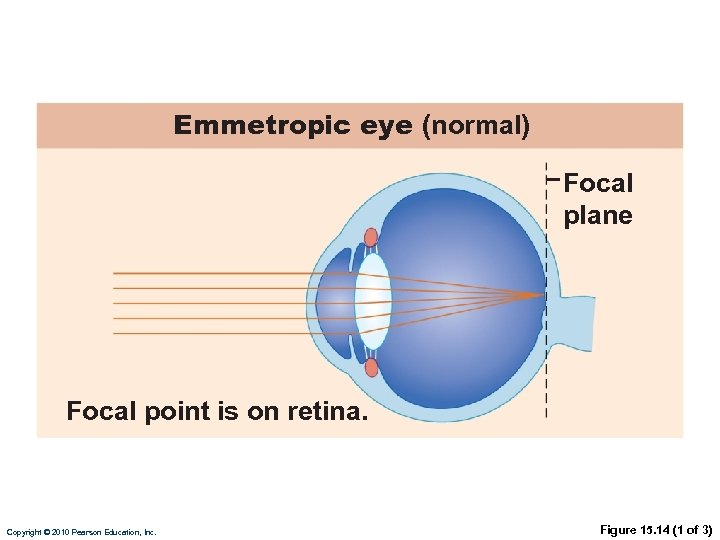
Emmetropic eye (normal) Focal plane Focal point is on retina. Copyright © 2010 Pearson Education, Inc. Figure 15. 14 (1 of 3)
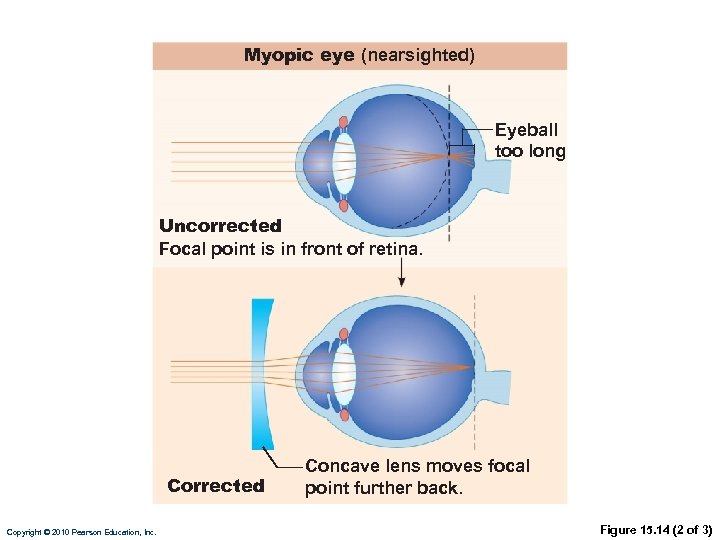
Myopic eye (nearsighted) Eyeball too long Uncorrected Focal point is in front of retina. Corrected Copyright © 2010 Pearson Education, Inc. Concave lens moves focal point further back. Figure 15. 14 (2 of 3)
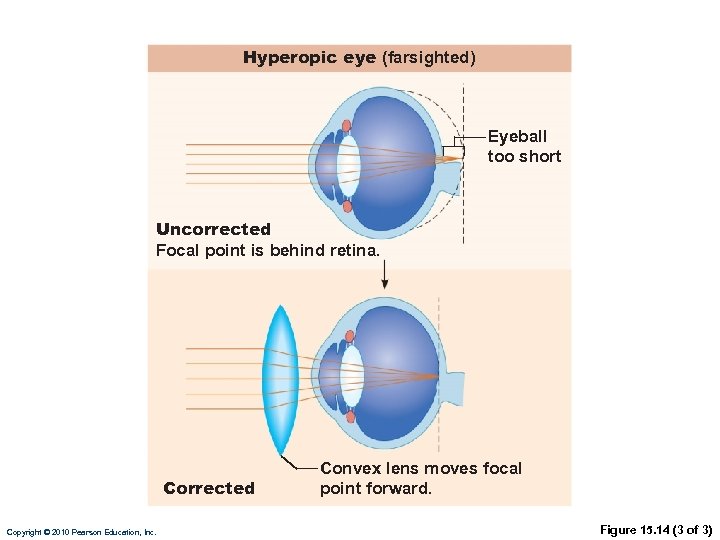
Hyperopic eye (farsighted) Eyeball too short Uncorrected Focal point is behind retina. Corrected Copyright © 2010 Pearson Education, Inc. Convex lens moves focal point forward. Figure 15. 14 (3 of 3)
Functional Anatomy of Photoreceptors • Rods and cones • Outer segment of each contains visual pigments -molecules that change shape as they absorb light • Inner segment of each joins the cell body Copyright © 2010 Pearson Education, Inc.
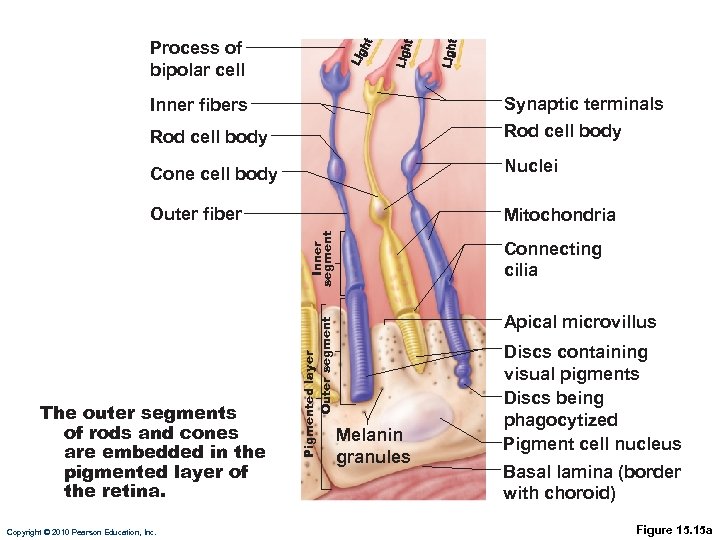
Process of bipolar cell Synaptic terminals Rod cell body Cone cell body Nuclei Outer fiber Mitochondria The outer segments of rods and cones are embedded in the pigmented layer of the retina. Copyright © 2010 Pearson Education, Inc. Pigmented layer Outer segment Inner fibers Connecting cilia Apical microvillus Melanin granules Discs containing visual pigments Discs being phagocytized Pigment cell nucleus Basal lamina (border with choroid) Figure 15. 15 a
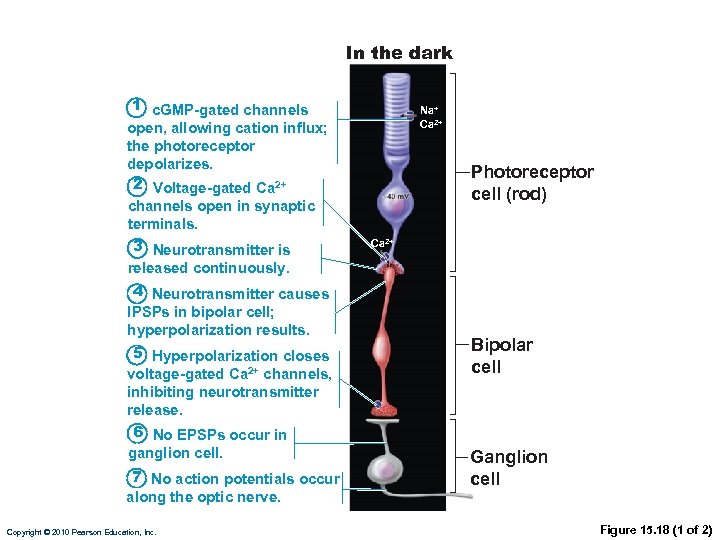
In the dark 1 c. GMP-gated channels open, allowing cation influx; the photoreceptor depolarizes. 2 Voltage-gated Ca 2+ channels open in synaptic terminals. 3 Neurotransmitter is released continuously. 4 Neurotransmitter causes IPSPs in bipolar cell; hyperpolarization results. 5 Hyperpolarization closes voltage-gated Ca 2+ channels, inhibiting neurotransmitter release. 6 No EPSPs occur in ganglion cell. 7 No action potentials occur along the optic nerve. Copyright © 2010 Pearson Education, Inc. Na+ Ca 2+ Photoreceptor cell (rod) Ca 2+ Bipolar cell Ganglion cell Figure 15. 18 (1 of 2)
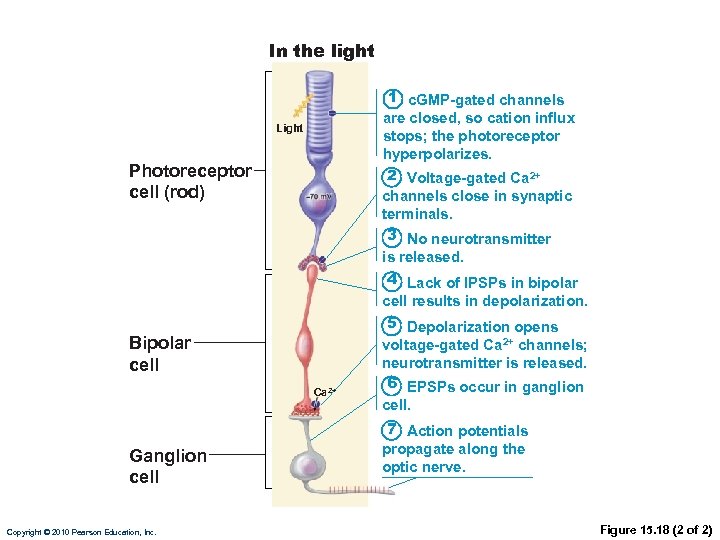
In the light 1 c. GMP-gated channels are closed, so cation influx stops; the photoreceptor hyperpolarizes. Light Photoreceptor cell (rod) 2 Voltage-gated Ca 2+ channels close in synaptic terminals. 3 No neurotransmitter is released. 4 Lack of IPSPs in bipolar cell results in depolarization. Bipolar cell Ca 2+ Ganglion cell Copyright © 2010 Pearson Education, Inc. 5 Depolarization opens voltage-gated Ca 2+ channels; neurotransmitter is released. 6 EPSPs occur in ganglion cell. 7 Action potentials propagate along the optic nerve. Figure 15. 18 (2 of 2)
Visual Pathway • Medial fibers of the optic nerve cross at the optic chiasma then to optic tract • Most fibers of the optic tracts continue to the thalamus • From the thalamus to the primary visual cortex in the occipital lobe Copyright © 2010 Pearson Education, Inc.
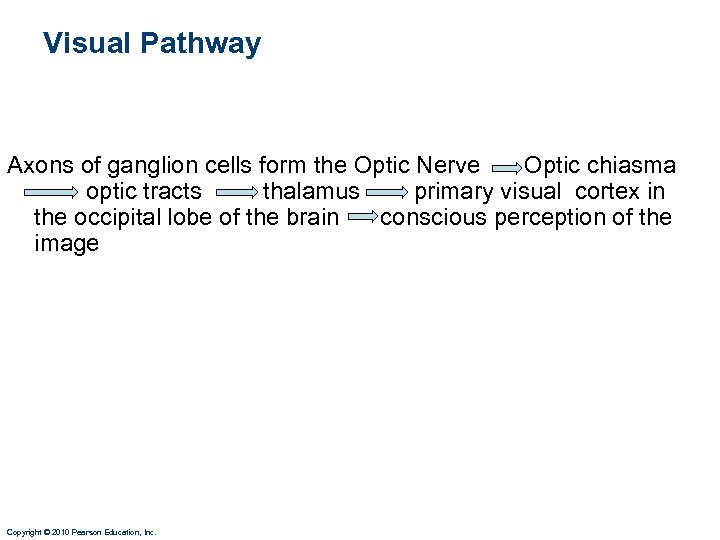
Visual Pathway Axons of ganglion cells form the Optic Nerve Optic chiasma optic tracts thalamus primary visual cortex in the occipital lobe of the brain conscious perception of the image Copyright © 2010 Pearson Education, Inc.
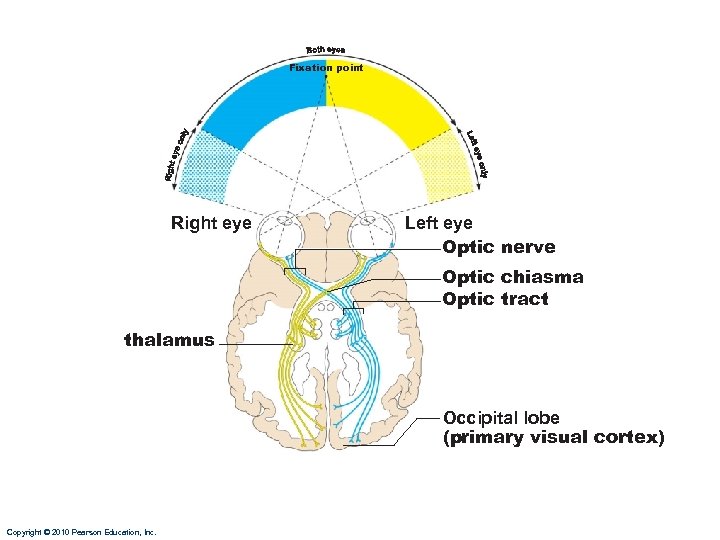
Fixation point Right eye Left eye Optic nerve Optic chiasma Optic tract thalamus Occipital lobe (primary visual cortex) Copyright © 2010 Pearson Education, Inc.
HEARING AND BALANCE Copyright © 2010 Pearson Education, Inc.
The Ear: Hearing and Balance • Three parts of the ear 1. External ear 2. Middle ear 3. Internal ear Copyright © 2010 Pearson Education, Inc.
The Ear: Hearing and Balance • External ear and middle ear are involved with: hearing • Internal ear (labyrinth) functions in both: hearing and equilibrium Copyright © 2010 Pearson Education, Inc.
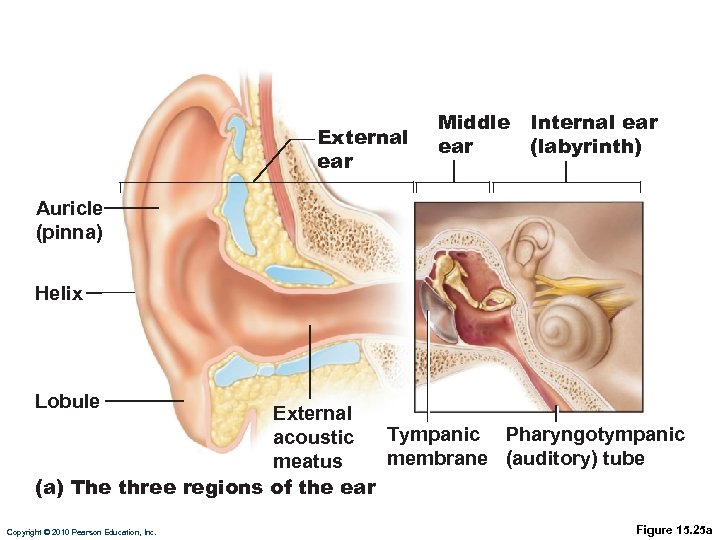
External ear Middle ear Internal ear (labyrinth) Auricle (pinna) Helix Lobule External Tympanic Pharyngotympanic acoustic membrane (auditory) tube meatus (a) The three regions of the ear Copyright © 2010 Pearson Education, Inc. Figure 15. 25 a
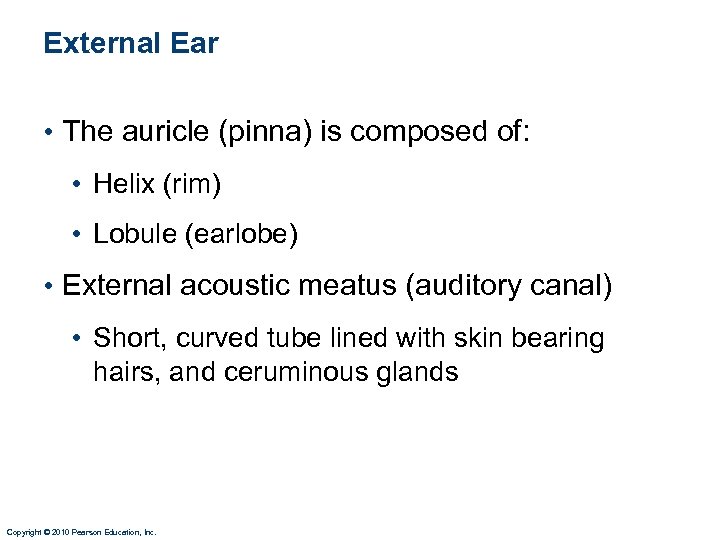
External Ear • The auricle (pinna) is composed of: • Helix (rim) • Lobule (earlobe) • External acoustic meatus (auditory canal) • Short, curved tube lined with skin bearing hairs, and ceruminous glands Copyright © 2010 Pearson Education, Inc.
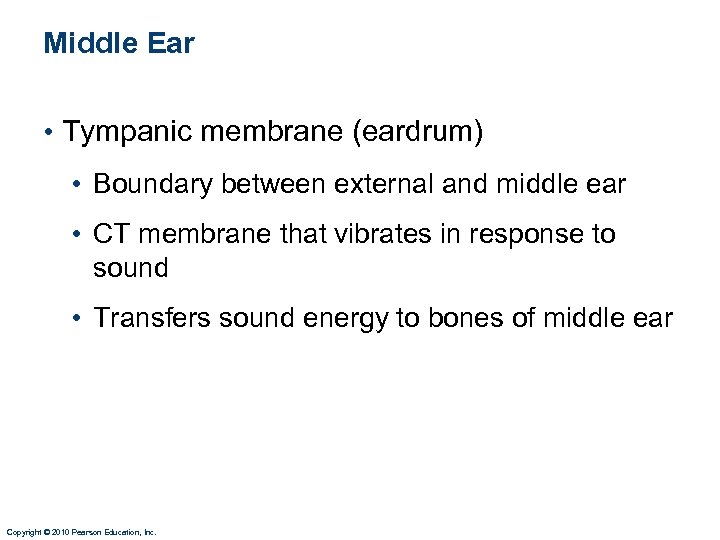
Middle Ear • Tympanic membrane (eardrum) • Boundary between external and middle ear • CT membrane that vibrates in response to sound • Transfers sound energy to bones of middle ear Copyright © 2010 Pearson Education, Inc.
Middle Ear • Pharyngotympanic tube—connects the middle ear to the nasopharynx • Equalizes pressure in the middle ear cavity with the external air pressure Copyright © 2010 Pearson Education, Inc.
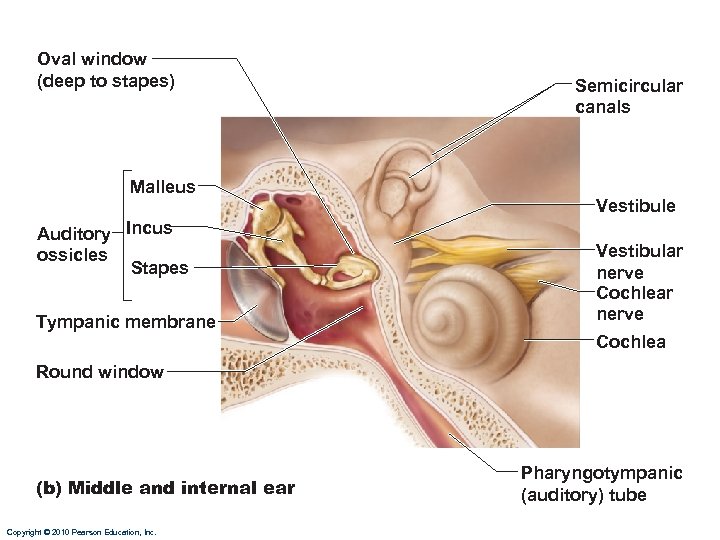
Oval window (deep to stapes) Malleus Auditory Incus ossicles Stapes Tympanic membrane Semicircular canals Vestibule Vestibular nerve Cochlea Round window (b) Middle and internal ear Copyright © 2010 Pearson Education, Inc. Pharyngotympanic (auditory) tube
Ear Ossicles • Three small bones in middle ear cavity: the malleus, incus, and stapes • Transmit vibratory motion of the eardrum to the oval window • Tensor tympani and stapedius muscles contract reflexively in response to loud sounds to prevent damage to the hearing receptors Copyright © 2010 Pearson Education, Inc.
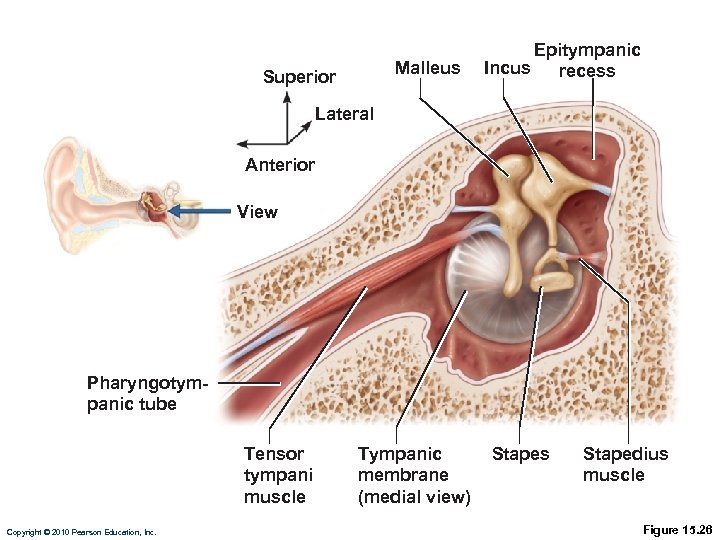
Malleus Superior Epitympanic Incus recess Lateral Anterior View Pharyngotympanic tube Tensor tympani muscle Copyright © 2010 Pearson Education, Inc. Tympanic membrane (medial view) Stapes Stapedius muscle Figure 15. 26
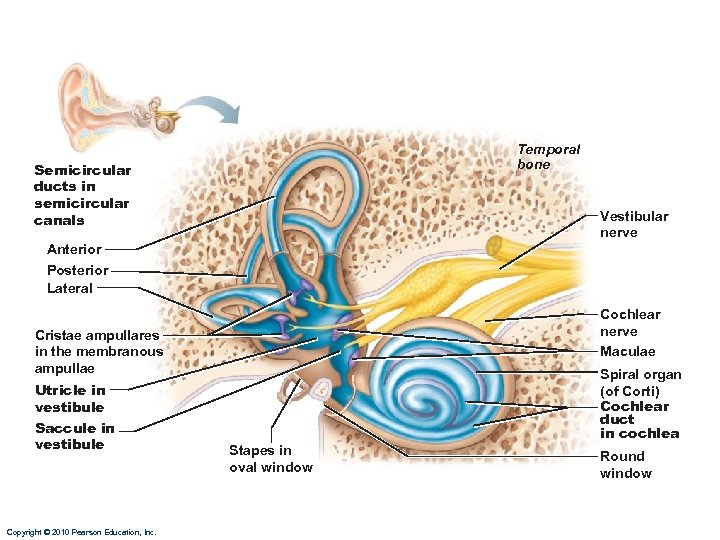
Internal Ear • Bony labyrinth • Winding channels in the temporal bone • Three parts: vestibule, semicircular canals, and cochlea • Filled with perilymph • Series of membranous sacs within the bony labyrinth • Filled with endolymph Copyright © 2010 Pearson Education, Inc.
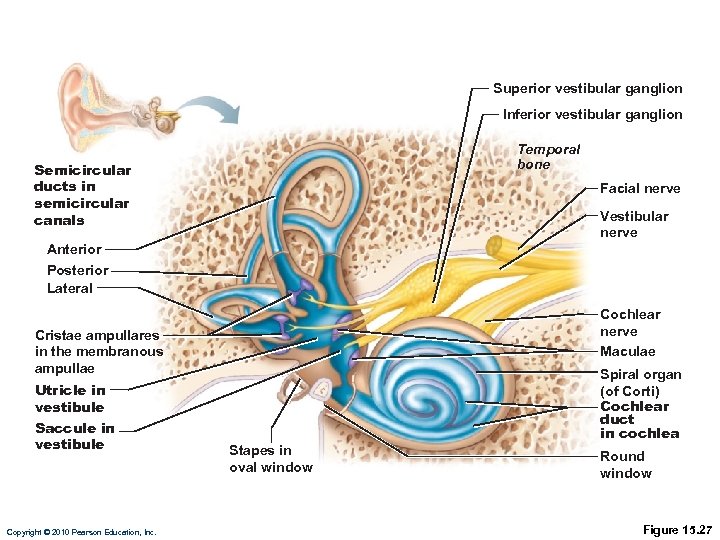
Superior vestibular ganglion Inferior vestibular ganglion Temporal bone Semicircular ducts in semicircular canals Facial nerve Vestibular nerve Anterior Posterior Lateral Cochlear nerve Maculae Cristae ampullares in the membranous ampullae Spiral organ (of Corti) Cochlear duct in cochlea Utricle in vestibule Saccule in vestibule Copyright © 2010 Pearson Education, Inc. Stapes in oval window Round window Figure 15. 27
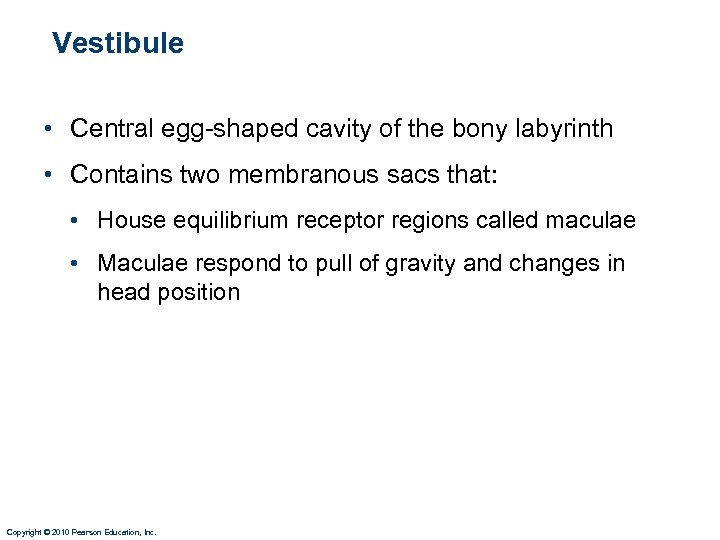
Vestibule • Central egg-shaped cavity of the bony labyrinth • Contains two membranous sacs that: • House equilibrium receptor regions called maculae • Maculae respond to pull of gravity and changes in head position Copyright © 2010 Pearson Education, Inc.
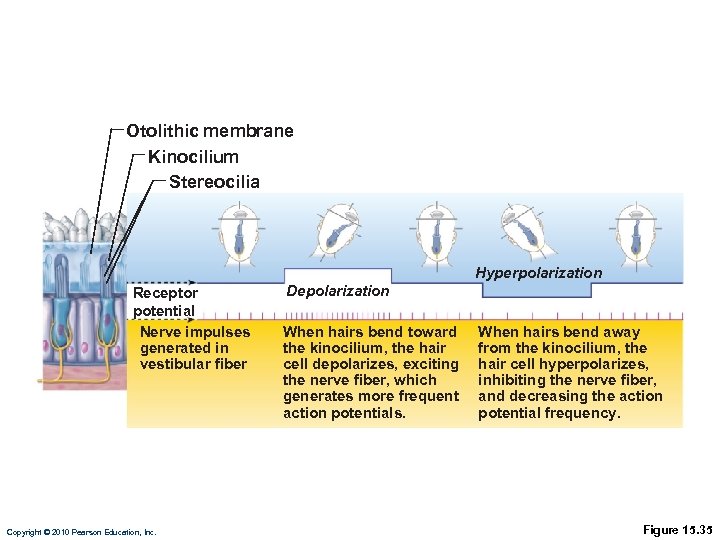
Otolithic membrane Kinocilium Stereocilia Hyperpolarization Receptor potential Nerve impulses generated in vestibular fiber Copyright © 2010 Pearson Education, Inc. Depolarization When hairs bend toward the kinocilium, the hair cell depolarizes, exciting the nerve fiber, which generates more frequent action potentials. When hairs bend away from the kinocilium, the hair cell hyperpolarizes, inhibiting the nerve fiber, and decreasing the action potential frequency. Figure 15. 35
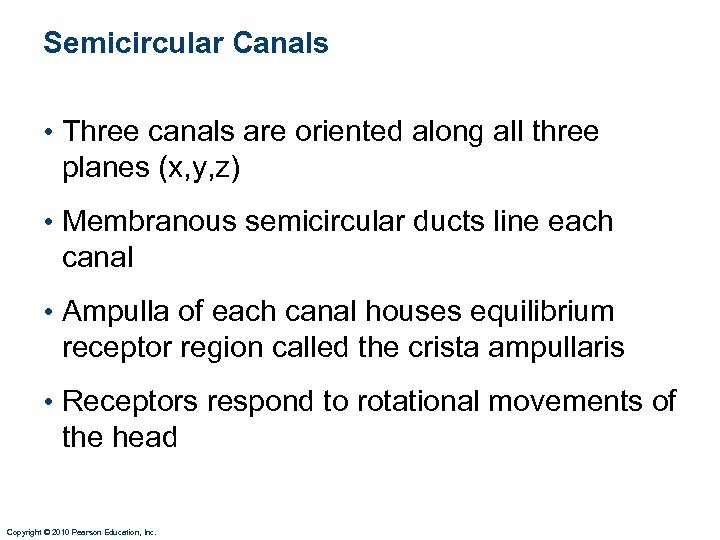
Semicircular Canals • Three canals are oriented along all three planes (x, y, z) • Membranous semicircular ducts line each canal • Ampulla of each canal houses equilibrium receptor region called the crista ampullaris • Receptors respond to rotational movements of the head Copyright © 2010 Pearson Education, Inc.
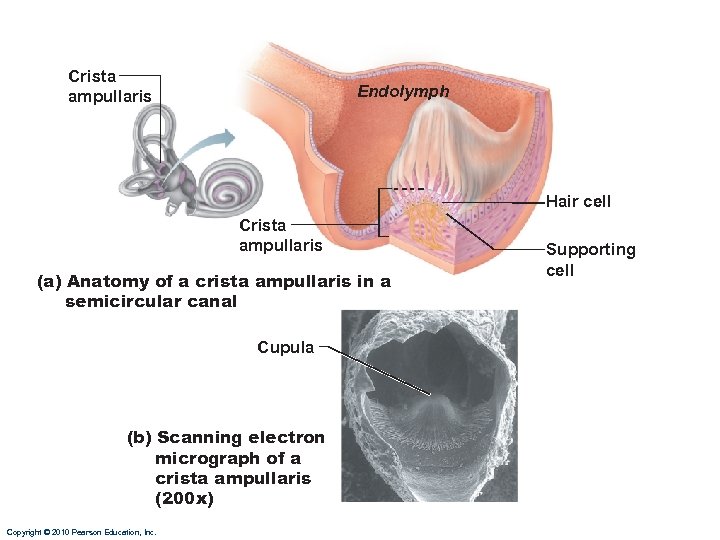
Crista ampullaris Endolymph Hair cell Crista ampullaris (a) Anatomy of a crista ampullaris in a semicircular canal Cupula (b) Scanning electron micrograph of a crista ampullaris (200 x) Copyright © 2010 Pearson Education, Inc. Supporting cell
Equilibrium • Impulses sent from the vestibule (maculae) or from ampulla (crista ampullaris) travel along the vestibular nerve which quickly merges with the cochlear nerve to form the vestibulocochlear nerve (CN #8) Copyright © 2010 Pearson Education, Inc.
Temporal bone Semicircular ducts in semicircular canals Vestibular nerve Anterior Posterior Lateral Cochlear nerve Maculae Cristae ampullares in the membranous ampullae Spiral organ (of Corti) Cochlear duct in cochlea Utricle in vestibule Saccule in vestibule Copyright © 2010 Pearson Education, Inc. Stapes in oval window Round window
The Cochlea • A spiral, conical, bony chamber • Extends from the vestibule • Contains the cochlear duct, which houses the spiral organ (of Corti) Copyright © 2010 Pearson Education, Inc.
Sound and the Cochlea • Organ of Corti • Runs through center of cochlea • Has hair cells(nerve cells) and supporting cells • Tectorial membrane- gel-like mass that cilia of hair cells are embedded in • Basilar membrane-fibrous “floor” of organ of corti • Bending of the cilia: excites hair cells Copyright © 2010 Pearson Education, Inc.
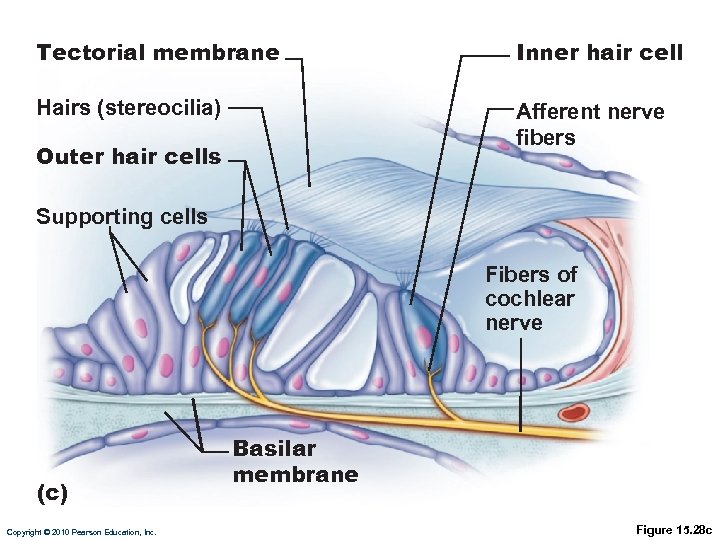
Tectorial membrane Inner hair cell Hairs (stereocilia) Afferent nerve fibers Outer hair cells Supporting cells Fibers of cochlear nerve (c) Copyright © 2010 Pearson Education, Inc. Basilar membrane Figure 15. 28 c
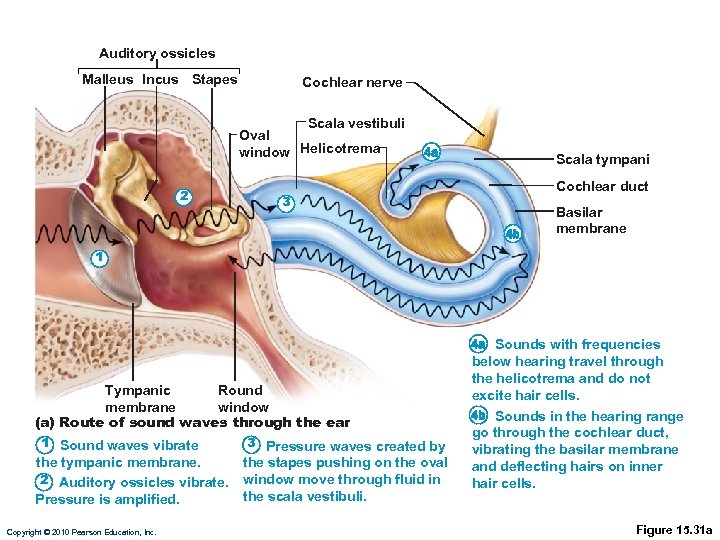
Auditory ossicles Malleus Incus Stapes Cochlear nerve Scala vestibuli Oval window Helicotrema 2 3 Scala tympani Cochlear duct Basilar membrane 1 Tympanic Round membrane window (a) Route of sound waves through the ear 1 Sound waves vibrate the tympanic membrane. 2 Auditory ossicles vibrate. Pressure is amplified. Copyright © 2010 Pearson Education, Inc. 3 Pressure waves created by the stapes pushing on the oval window move through fluid in the scala vestibuli. Sounds with frequencies below hearing travel through the helicotrema and do not excite hair cells. Sounds in the hearing range go through the cochlear duct, vibrating the basilar membrane and deflecting hairs on inner hair cells. Figure 15. 31 a
Transmission of Sound to the Internal Ear • Transmission of Sound to the Inner Ear • Sound waves enter the external acoustic canal and cause tympanic membrane to vibrate • Ossicles vibrate and amplify the pressure at the oval window • Pressure waves move through perilymph • Sounds in the hearing range go through the cochlear duct, ultimately causing bending of hair cells • Impulses from the cochlea pass: along the cochlear nerve, which then merges with the vestibular nerve (forming vestibulocochlear N. ) that travels to the primary auditory cortex in temporal lobe of brain Copyright © 2010 Pearson Education, Inc.
Deafness • Hearing loss can be temporary or permanent • Common causes: • Middle ear infections • Conduction deafness • Can be caused by: • Impacted earwax • Ruptured eardrum • Middle ear inflammations • Otosclerosis Copyright © 2010 Pearson Education, Inc.
Deafness • Nerve Deafness • Can be caused by: • Gradual loss of hair cells throughout life • Single explosive loud noise • Prolonged exposure to loud noise • Degeneration of cochlear nerve, tumors in auditory cortex, etc. Copyright © 2010 Pearson Education, Inc.
Tinnitus • Ringing or clicking sound in ears in the absence of auditory stimuli • One of the first symptoms of cochlear degeneration • Can be caused by middle ear inflammation Copyright © 2010 Pearson Education, Inc.
39c7deb78460ac3ff1115bdc760e4f55.ppt