3674601eeefeabfeefd98fc99a8af3d7.ppt
- Количество слайдов: 74
 Post Stroke Pain Syndromes Susan Stickevers, MD Residency Program Director, PM&R SUNY Stony Brook
Post Stroke Pain Syndromes Susan Stickevers, MD Residency Program Director, PM&R SUNY Stony Brook
 Epidemiology • Annually, 500, 000 people in the US have a first stroke • 200, 000 have a recurrent stroke • 80% of strokes are ischemic, either thrombotic or embolic in origin • 5 million people in the US have had a stroke & are living in the community setting • Of these, 1. 1 million have limitations in their daily functioning or ability to perform activities of daily living • 100, 000 people have stroke as their primary diagnosis & are receiving in home health care
Epidemiology • Annually, 500, 000 people in the US have a first stroke • 200, 000 have a recurrent stroke • 80% of strokes are ischemic, either thrombotic or embolic in origin • 5 million people in the US have had a stroke & are living in the community setting • Of these, 1. 1 million have limitations in their daily functioning or ability to perform activities of daily living • 100, 000 people have stroke as their primary diagnosis & are receiving in home health care
 Risk Factors for Stroke • • Increasing age Hypertension Obesity Diabetes Physical Inactivity Heart Disease Tobacco Use
Risk Factors for Stroke • • Increasing age Hypertension Obesity Diabetes Physical Inactivity Heart Disease Tobacco Use
 Epidemiology of Post Stroke Pain • Prevalence of Post Stroke Pain estimated in studies to be as low as 19% of stroke survivors to as high as 70% • Langhorne et al followed more than 300 consecutive patients after stroke • 43% of the stroke patients had pain after their stroke • Increasing levels of dependency correlated with increasing levels of pain
Epidemiology of Post Stroke Pain • Prevalence of Post Stroke Pain estimated in studies to be as low as 19% of stroke survivors to as high as 70% • Langhorne et al followed more than 300 consecutive patients after stroke • 43% of the stroke patients had pain after their stroke • Increasing levels of dependency correlated with increasing levels of pain
 Risk Factors for Post Stroke Pain • Risk factors for the development of post stroke pain have not been fully delineated • Most post stroke pain manifests itself within several weeks to months after the stroke • Pain in the immediate post stroke period is not uncommon
Risk Factors for Post Stroke Pain • Risk factors for the development of post stroke pain have not been fully delineated • Most post stroke pain manifests itself within several weeks to months after the stroke • Pain in the immediate post stroke period is not uncommon
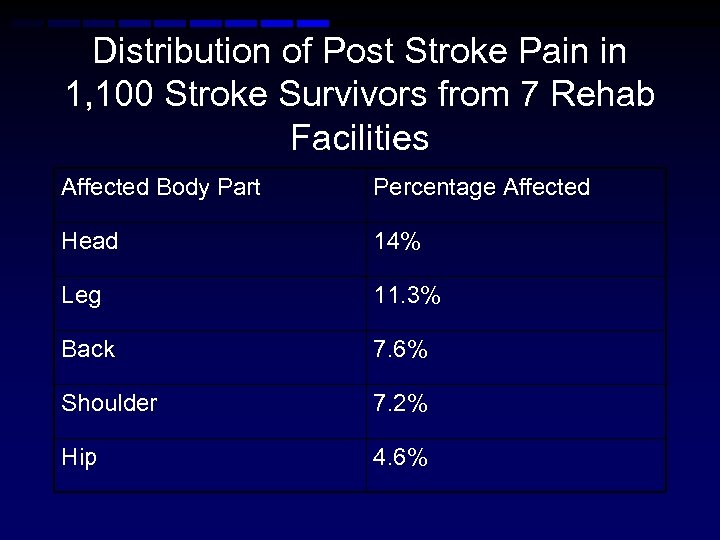 Distribution of Post Stroke Pain in 1, 100 Stroke Survivors from 7 Rehab Facilities Affected Body Part Percentage Affected Head 14% Leg 11. 3% Back 7. 6% Shoulder 7. 2% Hip 4. 6%
Distribution of Post Stroke Pain in 1, 100 Stroke Survivors from 7 Rehab Facilities Affected Body Part Percentage Affected Head 14% Leg 11. 3% Back 7. 6% Shoulder 7. 2% Hip 4. 6%
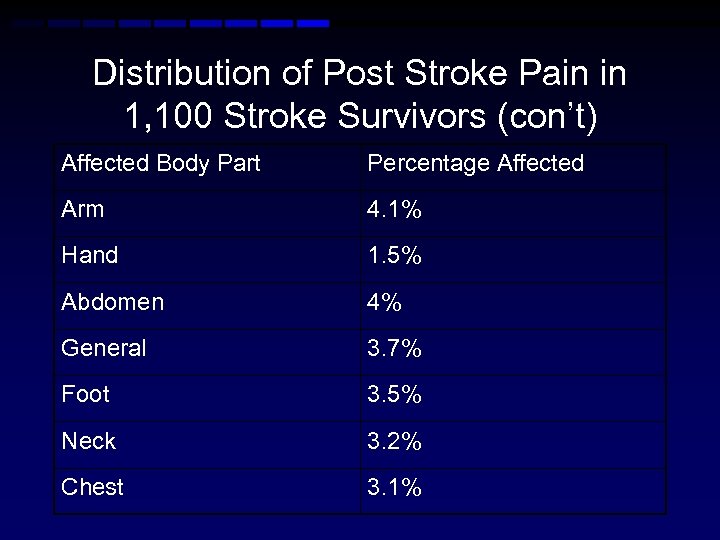 Distribution of Post Stroke Pain in 1, 100 Stroke Survivors (con’t) Affected Body Part Percentage Affected Arm 4. 1% Hand 1. 5% Abdomen 4% General 3. 7% Foot 3. 5% Neck 3. 2% Chest 3. 1%
Distribution of Post Stroke Pain in 1, 100 Stroke Survivors (con’t) Affected Body Part Percentage Affected Arm 4. 1% Hand 1. 5% Abdomen 4% General 3. 7% Foot 3. 5% Neck 3. 2% Chest 3. 1%
 Post Stroke Shoulder Pain • The shoulder may develop pain in the post stroke patient • Pain may be generated by : – – – Adhesive capsulitis / bursitis Traction or compressive neuropathy Soft Tissue Trauma Glenohumeral Subluxation Spasticity Central Post Stroke Pain (CPSP)
Post Stroke Shoulder Pain • The shoulder may develop pain in the post stroke patient • Pain may be generated by : – – – Adhesive capsulitis / bursitis Traction or compressive neuropathy Soft Tissue Trauma Glenohumeral Subluxation Spasticity Central Post Stroke Pain (CPSP)
 Hemiplegic Shoulder Pain • It was formerly believed that upper extremity pain following stroke was due to flaccidity of the upper extremity, and resultant shoulder subluxation • Study : 219 subjects with post stroke shoulder pain – 85% of patients with spasticity had pain – 18% of patients with flaccidity and shoulder subluxation had pain
Hemiplegic Shoulder Pain • It was formerly believed that upper extremity pain following stroke was due to flaccidity of the upper extremity, and resultant shoulder subluxation • Study : 219 subjects with post stroke shoulder pain – 85% of patients with spasticity had pain – 18% of patients with flaccidity and shoulder subluxation had pain
 Pain Related to Spasticity in the Hemiplegic Patient • Post stroke spasticity pain is focal • Most commonly affected sites with post stroke spasticity related pain are : – – – Shoulder Wrist Fingers Legs Feet
Pain Related to Spasticity in the Hemiplegic Patient • Post stroke spasticity pain is focal • Most commonly affected sites with post stroke spasticity related pain are : – – – Shoulder Wrist Fingers Legs Feet
 Treatments – Pain Related to Spasticity • Use of oral anti - spasticity agents • **Dantrolene is preferred due to lack of CNS side effects** • Botulinum Toxin A & chemodenervation with phenol have been demonstrated to be effective in reducing pain in most studies for spasticity related pain in the shoulder, forearm & foot
Treatments – Pain Related to Spasticity • Use of oral anti - spasticity agents • **Dantrolene is preferred due to lack of CNS side effects** • Botulinum Toxin A & chemodenervation with phenol have been demonstrated to be effective in reducing pain in most studies for spasticity related pain in the shoulder, forearm & foot
 Chemodenervation for Muscle Imbalance in Hemiplegic Shoulder • Subscapularis spasticity limits external rotation following stroke, and pectoralis muscle spasticity brings about limitation of shoulder abduction • Chemodenervation offers the ability to alleviate the imbalance & relieve shoulder pain
Chemodenervation for Muscle Imbalance in Hemiplegic Shoulder • Subscapularis spasticity limits external rotation following stroke, and pectoralis muscle spasticity brings about limitation of shoulder abduction • Chemodenervation offers the ability to alleviate the imbalance & relieve shoulder pain
 Chemodenervation for Hemiplegic Shoulder • Hecht, 1992 – Retrospective study of 13 patients with spastic hemiplegia with limited & painful ROM of the shoulder who received phenol nerve blocks to subscapularis muscle innervation – Results : Immediate & significant improvement in ROM observed in abduction, flexion, & external rotation – Relief of pain with previously painful movements noted
Chemodenervation for Hemiplegic Shoulder • Hecht, 1992 – Retrospective study of 13 patients with spastic hemiplegia with limited & painful ROM of the shoulder who received phenol nerve blocks to subscapularis muscle innervation – Results : Immediate & significant improvement in ROM observed in abduction, flexion, & external rotation – Relief of pain with previously painful movements noted
 Botulinum Toxin A for Hemiplegic Shoulder Pain Related to Spasticity • Hecht, 1995 – Prospective study of 20 patients receiving botulinum toxin injections to the subscapularis & pectoralis muscles • Results : – 85% benefited from subscapularis block – 55% benefited from pectoralis major block – 45% exhibited improved AROM
Botulinum Toxin A for Hemiplegic Shoulder Pain Related to Spasticity • Hecht, 1995 – Prospective study of 20 patients receiving botulinum toxin injections to the subscapularis & pectoralis muscles • Results : – 85% benefited from subscapularis block – 55% benefited from pectoralis major block – 45% exhibited improved AROM
 Botulinum Toxin Injection for Hemiplegic Shoulder Pain Related to Spasticity • Bhakta et al, 1996 : – 17 patients received a single course of intramuscular botulinum toxin to biceps, FDP, FDS, and FCU – Shoulder pain improved in 6/9 subjects who had shoulder pain prior to injection
Botulinum Toxin Injection for Hemiplegic Shoulder Pain Related to Spasticity • Bhakta et al, 1996 : – 17 patients received a single course of intramuscular botulinum toxin to biceps, FDP, FDS, and FCU – Shoulder pain improved in 6/9 subjects who had shoulder pain prior to injection
 Botulinum Toxin A for Hemiplegic Shoulder Pain – AJPMR Marciniak Study, 2012 • Randomized Double Blind Placebo Controlled trial of botulinum toxin A vs. saline placebo in 37 hemiplegic subjects • Modified Ashworth score of 3 - 4 • 21 patients received the study drug • Patients injected solely in the shoulder adductors and internal rotators, specifically the pectoralis major and some patients were also injected in teres major • Dose administered was limited to 140 -200 units
Botulinum Toxin A for Hemiplegic Shoulder Pain – AJPMR Marciniak Study, 2012 • Randomized Double Blind Placebo Controlled trial of botulinum toxin A vs. saline placebo in 37 hemiplegic subjects • Modified Ashworth score of 3 - 4 • 21 patients received the study drug • Patients injected solely in the shoulder adductors and internal rotators, specifically the pectoralis major and some patients were also injected in teres major • Dose administered was limited to 140 -200 units
 2012 Marciniak Botulinum Toxin A Hemiplegic Shoulder Pain Study • Pain reduction experienced by patients on placebo and treatment group was equivalent – there was no significant reduction in shoulder pain in those receiving botulinum toxin • The patients receiving the botulinum neurotoxins had improved hygiene and disability assessment scores – Marciniak et al, American J. of PM&R December 2012
2012 Marciniak Botulinum Toxin A Hemiplegic Shoulder Pain Study • Pain reduction experienced by patients on placebo and treatment group was equivalent – there was no significant reduction in shoulder pain in those receiving botulinum toxin • The patients receiving the botulinum neurotoxins had improved hygiene and disability assessment scores – Marciniak et al, American J. of PM&R December 2012
 Shoulder Pain Following Stroke • Development of shoulder pain following stroke is associated with loss of external rotation, NOT subluxation – Zorowitz, 1996 • Use of hemisling should be discouraged if at all possible as the sling holds the upper extremity in an adducted & internally rotated position which can lead to a loss of external rotation
Shoulder Pain Following Stroke • Development of shoulder pain following stroke is associated with loss of external rotation, NOT subluxation – Zorowitz, 1996 • Use of hemisling should be discouraged if at all possible as the sling holds the upper extremity in an adducted & internally rotated position which can lead to a loss of external rotation
 Optimal Positioning of the Hemiplegic Shoulder • Randomized Controlled Trial in 36 Australian Hemiplegic Stroke Patients – Positioning of the shoulder in maximal external rotation for two 30 minute treatment sessions per day significantly reduced the development of contractures compared to controls. Ada et al, 2005
Optimal Positioning of the Hemiplegic Shoulder • Randomized Controlled Trial in 36 Australian Hemiplegic Stroke Patients – Positioning of the shoulder in maximal external rotation for two 30 minute treatment sessions per day significantly reduced the development of contractures compared to controls. Ada et al, 2005
 Effect of Slings on the Hemiplegic Shoulder • It is generally believed that hemislings should be used in the initial stages following stroke to support the affected arm. • Their use is controversial because hemislings can encourage flexor synergies, inhibit reciprocal arm swing during ambulation, contribute to flexion contractures of the upper extremity, and discourage use of the affected arm & hand • A hemisling holds the affected shoulder in a position which accentuates adduction & internal rotation, which may lead to shortening of tonically active muscles • A sling is the best method however to support a flaccid arm while a patient is standing or transferring • Lapboards & arm troughs may be used to support the arm while seated • As tone returns to shoulder muscles, the risk of shoulder subluxation decreases, and then sling use may be discontinued
Effect of Slings on the Hemiplegic Shoulder • It is generally believed that hemislings should be used in the initial stages following stroke to support the affected arm. • Their use is controversial because hemislings can encourage flexor synergies, inhibit reciprocal arm swing during ambulation, contribute to flexion contractures of the upper extremity, and discourage use of the affected arm & hand • A hemisling holds the affected shoulder in a position which accentuates adduction & internal rotation, which may lead to shortening of tonically active muscles • A sling is the best method however to support a flaccid arm while a patient is standing or transferring • Lapboards & arm troughs may be used to support the arm while seated • As tone returns to shoulder muscles, the risk of shoulder subluxation decreases, and then sling use may be discontinued
 Evidence Based Medicine : Slings for Hemiplegic Subjects • Cochrane Review, 2005 – The review, conducted by Ada et al, included only 4 randomized controlled trials regarding use of slings & shoulder supports for hemiplegic patients – Conclusion : There was limited evidence that shoulder slings prevented subluxation associated with hemiplegic shoulder pain – There was limited evidence that shoulder slings influence clinical outcomes – The best method to support the hemiplegic shoulder has yet to be determined
Evidence Based Medicine : Slings for Hemiplegic Subjects • Cochrane Review, 2005 – The review, conducted by Ada et al, included only 4 randomized controlled trials regarding use of slings & shoulder supports for hemiplegic patients – Conclusion : There was limited evidence that shoulder slings prevented subluxation associated with hemiplegic shoulder pain – There was limited evidence that shoulder slings influence clinical outcomes – The best method to support the hemiplegic shoulder has yet to be determined
 Strapping the Hemiplegic Shoulder – Common Practice in Australia / New Zealand • Use of adhesive tape, (Fixomull Stretch), or Elastoplast adhesive bandage to prevent or reduce severity of shoulder subluxation – Three studies : Griffin & Bernhardt, Ancliffe et al, Hanger et al. • A review of these three studies in Australia & New Zealand revealed that : – Strapping the hemiplegic shoulder does not improve upper limb function or range of motion – There was conflicting data in the three studies regarding whether or not strapping could reduce shoulder pain.
Strapping the Hemiplegic Shoulder – Common Practice in Australia / New Zealand • Use of adhesive tape, (Fixomull Stretch), or Elastoplast adhesive bandage to prevent or reduce severity of shoulder subluxation – Three studies : Griffin & Bernhardt, Ancliffe et al, Hanger et al. • A review of these three studies in Australia & New Zealand revealed that : – Strapping the hemiplegic shoulder does not improve upper limb function or range of motion – There was conflicting data in the three studies regarding whether or not strapping could reduce shoulder pain.
 Use of Active Therapies to Reduce Pain in the Hemiplegic Shoulder • • • There was evidence that aggressive range of motion of the shoulder with overhead pulleys resulted in increased rates of shoulder pain – Kumar, 1990 There was evidence that Bobath (NDT) for the hemiplegic shoulder was associated with greater pain reduction than cryotherapy – Partridge et al, 1990 There was evidence that gentle range of motion exercises were the preferred method of treatment for the hemiplegic shoulder Addition of ultrasound application to the shoulder to the ROM exercises did not change outcomes – Inaba et al, 1972 There was limited evidence that providing oral NSAIDS to a stroke patient with shoulder pain improved ROM & functional recovery – Poduri et al, 1993 No statistically significant benefit from CPM for the shoulder compared with therapist supervised self ROM – Lynch et al, 2005
Use of Active Therapies to Reduce Pain in the Hemiplegic Shoulder • • • There was evidence that aggressive range of motion of the shoulder with overhead pulleys resulted in increased rates of shoulder pain – Kumar, 1990 There was evidence that Bobath (NDT) for the hemiplegic shoulder was associated with greater pain reduction than cryotherapy – Partridge et al, 1990 There was evidence that gentle range of motion exercises were the preferred method of treatment for the hemiplegic shoulder Addition of ultrasound application to the shoulder to the ROM exercises did not change outcomes – Inaba et al, 1972 There was limited evidence that providing oral NSAIDS to a stroke patient with shoulder pain improved ROM & functional recovery – Poduri et al, 1993 No statistically significant benefit from CPM for the shoulder compared with therapist supervised self ROM – Lynch et al, 2005
 Intraarticular Injections • Subacromial Bursa Injections • Glenohumeral Joint Injections • Often used clinically for adhesive capsulitis or bursitis which develops following CVA • What evidence supports this practice?
Intraarticular Injections • Subacromial Bursa Injections • Glenohumeral Joint Injections • Often used clinically for adhesive capsulitis or bursitis which develops following CVA • What evidence supports this practice?
 Injections for Relief of Hemiplegic Shoulder Pain • There is only one randomized controlled trial in 35 Dutch hemiplegic subjects with shoulder pain injected X 3 with triamcinolone 40 mg vs saline placebo in the affected glenohumeral joint – Snels et al, 2000 • No significant improvement was observed in pain or function of the affected shoulder with triamcinolone injection
Injections for Relief of Hemiplegic Shoulder Pain • There is only one randomized controlled trial in 35 Dutch hemiplegic subjects with shoulder pain injected X 3 with triamcinolone 40 mg vs saline placebo in the affected glenohumeral joint – Snels et al, 2000 • No significant improvement was observed in pain or function of the affected shoulder with triamcinolone injection
 Electrical Stimulation for Preventing & Treating Post Stroke Shoulder Pain • Application of functional electrical stimulation (FES) to the hemiplegic shoulder is believed to improve muscle tone & strength, as well as reduce pain • The **supraspinatus & posterior deltoid** muscles are usually treated as they maintain correct alignment of the glenohumeral joint & reduce shoulder subluxation • Ideal intensity of treatment is 6 hours / day, five days per week, for a total of 6 weeks, at frequencies between 35 – 50 Hz – Paci et al, 2005
Electrical Stimulation for Preventing & Treating Post Stroke Shoulder Pain • Application of functional electrical stimulation (FES) to the hemiplegic shoulder is believed to improve muscle tone & strength, as well as reduce pain • The **supraspinatus & posterior deltoid** muscles are usually treated as they maintain correct alignment of the glenohumeral joint & reduce shoulder subluxation • Ideal intensity of treatment is 6 hours / day, five days per week, for a total of 6 weeks, at frequencies between 35 – 50 Hz – Paci et al, 2005
 Cochrane Review, 2001 – FES for Hemiplegic Shoulder • Price & Pandyan conducted this systematic review of 4 studies on electrical stimulation (both TENS & FES) used for prevention and treatment of post stroke shoulder pain • They concluded that there was insufficient evidence from which to draw conclusions. • There was evidence that FES, in addition to conventional therapy, improved function but was not superior than conventional therapy for preventing shoulder pain • **FES did improve passive external rotation of the shoulder & improved glenohumeral subluxation compared to baseline **
Cochrane Review, 2001 – FES for Hemiplegic Shoulder • Price & Pandyan conducted this systematic review of 4 studies on electrical stimulation (both TENS & FES) used for prevention and treatment of post stroke shoulder pain • They concluded that there was insufficient evidence from which to draw conclusions. • There was evidence that FES, in addition to conventional therapy, improved function but was not superior than conventional therapy for preventing shoulder pain • **FES did improve passive external rotation of the shoulder & improved glenohumeral subluxation compared to baseline **
 Meta – Analysis on Effect of FES on Shoulder Subluxation Following Stroke • Ada & Foongchomcheay (2002) – Review of 6 randomized controlled trials – Results suggested that early treatment with electrical stimulation prevented the development of shoulder subluxation in the hemiplegic subject while later treatment helped to reduce pain when used in conjunction with conventional therapy
Meta – Analysis on Effect of FES on Shoulder Subluxation Following Stroke • Ada & Foongchomcheay (2002) – Review of 6 randomized controlled trials – Results suggested that early treatment with electrical stimulation prevented the development of shoulder subluxation in the hemiplegic subject while later treatment helped to reduce pain when used in conjunction with conventional therapy
 Effect of FES on Hemiplegic Shoulder Pain • 11 studies conducted • All 11 of the studies reported a benefit associated with FES treatment including improved muscle function, tone, EMG activity, pain, subluxation and range of motion • The improvement was maintained for up to 24 months of follow up – Studies : Chae et al, 2005, Yu et al, 2004, Wang et al, 2000, Linn et al, 1999, Renzenbrink & Ijerman, 2004, Baker & Parker, 1986, Faghri et al, 1994, 1997, Chantraine et al, 1999, Kobayshi, 1999.
Effect of FES on Hemiplegic Shoulder Pain • 11 studies conducted • All 11 of the studies reported a benefit associated with FES treatment including improved muscle function, tone, EMG activity, pain, subluxation and range of motion • The improvement was maintained for up to 24 months of follow up – Studies : Chae et al, 2005, Yu et al, 2004, Wang et al, 2000, Linn et al, 1999, Renzenbrink & Ijerman, 2004, Baker & Parker, 1986, Faghri et al, 1994, 1997, Chantraine et al, 1999, Kobayshi, 1999.
 Surgical Treatment for Hemiplegic Shoulder Pain • Involves resection of subscapularis & pectoralis muscle tendons to relieve internal rotation & adduction of shoulder • Surgery was followed up by post op passive range of motion & positioning of the shoulder, as well as pulley exercises • 10/13 patients operated on regained 90 degrees of passive abduction & 20 degrees of external rotation within 2 months of surgery, but six months later, all 13 patients reported pain & discomfort – Braun et al, 1971
Surgical Treatment for Hemiplegic Shoulder Pain • Involves resection of subscapularis & pectoralis muscle tendons to relieve internal rotation & adduction of shoulder • Surgery was followed up by post op passive range of motion & positioning of the shoulder, as well as pulley exercises • 10/13 patients operated on regained 90 degrees of passive abduction & 20 degrees of external rotation within 2 months of surgery, but six months later, all 13 patients reported pain & discomfort – Braun et al, 1971
 Complex Regional Pain Syndrome Type 1 • Typically appears within 9 weeks of following stroke • Studies have shown the incidence of post stroke CRPS to range between 12. 5% - 70% • Symptoms include : – – – Pain Hyperalgesia or allodynia Joint Stiffness Swelling Autonomic Abnormalities
Complex Regional Pain Syndrome Type 1 • Typically appears within 9 weeks of following stroke • Studies have shown the incidence of post stroke CRPS to range between 12. 5% - 70% • Symptoms include : – – – Pain Hyperalgesia or allodynia Joint Stiffness Swelling Autonomic Abnormalities
 Complex Regional Pain Syndrome • The following are predictive of the development & severity of CRPS following stroke : – – Motor deficits Sensory deficits Spasticity Coma following stroke
Complex Regional Pain Syndrome • The following are predictive of the development & severity of CRPS following stroke : – – Motor deficits Sensory deficits Spasticity Coma following stroke
 Keys to Avoiding Development of CRPS • Early rehabilitation interventions! • Avoidance of trauma to the limb
Keys to Avoiding Development of CRPS • Early rehabilitation interventions! • Avoidance of trauma to the limb
 Shoulder Hand Syndrome • Is a type of CRPS that is limited to the upper extremity after stroke • Pathophysiology of this disorder is not known, however, this disorder appears to be related to the severity & the etiology of the stroke, neural reorganization following the stroke, spasticity, motor and sensory deficits following the stroke • Severe motor deficits which are slow to resolve post stroke increase the likelihood of developing shoulder – hand syndrome
Shoulder Hand Syndrome • Is a type of CRPS that is limited to the upper extremity after stroke • Pathophysiology of this disorder is not known, however, this disorder appears to be related to the severity & the etiology of the stroke, neural reorganization following the stroke, spasticity, motor and sensory deficits following the stroke • Severe motor deficits which are slow to resolve post stroke increase the likelihood of developing shoulder – hand syndrome
 Management of Shoulder Hand Syndrome • Early ROM exercises • Avoid shoulder subluxation • Prevention & treatment of upper extremity contractures • Active exercise if possible • Frequent passive range of motion • Heat / Cold Modalities including contrast bathes • Hand desensitization program, including vibration, massage, brushing, stroking • TENS • Analgesics • High Dose Steroids • Stellate Ganglion Block • Guanethidine Bier Block • Sympathectomy
Management of Shoulder Hand Syndrome • Early ROM exercises • Avoid shoulder subluxation • Prevention & treatment of upper extremity contractures • Active exercise if possible • Frequent passive range of motion • Heat / Cold Modalities including contrast bathes • Hand desensitization program, including vibration, massage, brushing, stroking • TENS • Analgesics • High Dose Steroids • Stellate Ganglion Block • Guanethidine Bier Block • Sympathectomy
 Pharmacological Management of Shoulder Hand Syndrome • Braus et al, 1994 : Randomized controlled cross – over trial involving 36 hemiplegic patients with SHS resulting from MCA stroke – Randomized to receive either 8 mg methylprednisolone or placebo over 4 weeks – All patients received daily physical therapy – No significant improvement was noted in SHS in the placebo group after 4 wks. – switched to study drug – Patients on steroid treatment demonstrated significant improvement in shoulder hand syndrome that was maintained at 6 months – 31/36 patients became almost symptom free within 10 days of treatment with low dose corticosteroids
Pharmacological Management of Shoulder Hand Syndrome • Braus et al, 1994 : Randomized controlled cross – over trial involving 36 hemiplegic patients with SHS resulting from MCA stroke – Randomized to receive either 8 mg methylprednisolone or placebo over 4 weeks – All patients received daily physical therapy – No significant improvement was noted in SHS in the placebo group after 4 wks. – switched to study drug – Patients on steroid treatment demonstrated significant improvement in shoulder hand syndrome that was maintained at 6 months – 31/36 patients became almost symptom free within 10 days of treatment with low dose corticosteroids
 Use of Calcitonin for SHS • Hamamci et al, 1996 : – Controlled trial of 41 hemiplegic subjects with SHS – All patients received conventional physical therapy as part of inpatient rehabilitation – 25 patients received 100 IU salmon calcitonin daily for 4 wks – 16 patients received saline placebo injections – Pain was measured on a numerical rating scale – By the end of the 4 th week, patients receiving calcitonin had significantly lower median pain scores compared to controls (Pain Level 1 vs. Level 5) – Patients receiving calcitonin reported less tenderness & improved ROM – No difference in hand edema between groups
Use of Calcitonin for SHS • Hamamci et al, 1996 : – Controlled trial of 41 hemiplegic subjects with SHS – All patients received conventional physical therapy as part of inpatient rehabilitation – 25 patients received 100 IU salmon calcitonin daily for 4 wks – 16 patients received saline placebo injections – Pain was measured on a numerical rating scale – By the end of the 4 th week, patients receiving calcitonin had significantly lower median pain scores compared to controls (Pain Level 1 vs. Level 5) – Patients receiving calcitonin reported less tenderness & improved ROM – No difference in hand edema between groups
 Post Stroke Central Pain Syndrome • Central Pain Syndrome is defined as neuropathic pain that results from damage to or dysfunction of the central nervous system, including the brain, brainstem, and spinal cord • Formerly called the post thalamic syndrome, however, lesions in the brainstem, pons, thalamus, and areas lateral & superior to the thalamus can also cause central post stroke pain – Leijon et al, Pain, 1989 • Estimated as occurring in 8 - 12% of all stroke patients • May occur at any time following a stroke, in the immediate post stroke period, or years later • Develops immediately after the stroke in 20% of patients • Occurs within one month after the stroke in 50% of all patients affected • 30% of patients who develop this syndrome claim onset of pain between one month and three years following the stroke.
Post Stroke Central Pain Syndrome • Central Pain Syndrome is defined as neuropathic pain that results from damage to or dysfunction of the central nervous system, including the brain, brainstem, and spinal cord • Formerly called the post thalamic syndrome, however, lesions in the brainstem, pons, thalamus, and areas lateral & superior to the thalamus can also cause central post stroke pain – Leijon et al, Pain, 1989 • Estimated as occurring in 8 - 12% of all stroke patients • May occur at any time following a stroke, in the immediate post stroke period, or years later • Develops immediately after the stroke in 20% of patients • Occurs within one month after the stroke in 50% of all patients affected • 30% of patients who develop this syndrome claim onset of pain between one month and three years following the stroke.
 Central Post Stroke Pain • Can be caused by both ischemic and hemorrhagic strokes • Pain is mild in 1/3 of affected subjects, and moderate to severe in 2/3 of subjects • CPSP usually results from a lesion of vascular origin, however some cases of CPSP are neoplastic in origin
Central Post Stroke Pain • Can be caused by both ischemic and hemorrhagic strokes • Pain is mild in 1/3 of affected subjects, and moderate to severe in 2/3 of subjects • CPSP usually results from a lesion of vascular origin, however some cases of CPSP are neoplastic in origin
 Post Stroke Central Pain Syndrome • Common Symptoms : – Muscle Pain or Cramping / Squeezing – Dysesthesias – Burning most commonly described (seen in 60% of CPSP pts. ) – Hyperpathia – Allodynia - seen in 50% of CPSP pts. – Intermittent shooting or lancinating pain – Circulatory Pain – Visceral Pain – Pruritis
Post Stroke Central Pain Syndrome • Common Symptoms : – Muscle Pain or Cramping / Squeezing – Dysesthesias – Burning most commonly described (seen in 60% of CPSP pts. ) – Hyperpathia – Allodynia - seen in 50% of CPSP pts. – Intermittent shooting or lancinating pain – Circulatory Pain – Visceral Pain – Pruritis
 Hypoesthesia & Autonomic Instability in CPSP • Hypoesthesia, which is a weaker than normal sensory reaction to stimuli, is common in CPSP • 95% of CPSP pts. have impaired pain & temperature sensation • 50% also have hypoesthesia to touch, vibration, and kinesthesia • Autonomic instability is also seen in these pts, but it is not clear if it is secondary to a superimposed CRPS
Hypoesthesia & Autonomic Instability in CPSP • Hypoesthesia, which is a weaker than normal sensory reaction to stimuli, is common in CPSP • 95% of CPSP pts. have impaired pain & temperature sensation • 50% also have hypoesthesia to touch, vibration, and kinesthesia • Autonomic instability is also seen in these pts, but it is not clear if it is secondary to a superimposed CRPS
 CPSP : The Pain Generators • Large lesions of the ventral posteromedial thalamic nucleus, (VPM), or ventral posterolateral thalamic nucleus, (VPL), or posterior limb of the internal capsule frequently cause hemi – body pain • CPSP may occur following lesions at any level in the spinothalamocortical pathway • Damage to the spinothalamic – cortical sensory pathways (mainly lateral medulla, thalamus, posterior limb of the internal capsule, cortical and subcortical zones of the post central gyrus and insular region) is believed to play a significant role in the pathogenesis of post stroke central pain
CPSP : The Pain Generators • Large lesions of the ventral posteromedial thalamic nucleus, (VPM), or ventral posterolateral thalamic nucleus, (VPL), or posterior limb of the internal capsule frequently cause hemi – body pain • CPSP may occur following lesions at any level in the spinothalamocortical pathway • Damage to the spinothalamic – cortical sensory pathways (mainly lateral medulla, thalamus, posterior limb of the internal capsule, cortical and subcortical zones of the post central gyrus and insular region) is believed to play a significant role in the pathogenesis of post stroke central pain
 Theories on the Pathogenesis of CPSP • Dejerine & Roussy : – an irritable focus in the lesioned tracts produces this pain syndrome • Boivie : – CPSP originates from hyperirritability in surviving cells in a lesion along the pain pathway (spinothalamic or thalamocortical pathway)
Theories on the Pathogenesis of CPSP • Dejerine & Roussy : – an irritable focus in the lesioned tracts produces this pain syndrome • Boivie : – CPSP originates from hyperirritability in surviving cells in a lesion along the pain pathway (spinothalamic or thalamocortical pathway)
 CSPS Secondary to Brainstem Involvement • In CSPS secondary to brainstem involvement, impairments in facial sensation are generally ipsilateral to the lesion, whereas extremity involvement is contralateral, and the distribution of pain may follow the same pattern
CSPS Secondary to Brainstem Involvement • In CSPS secondary to brainstem involvement, impairments in facial sensation are generally ipsilateral to the lesion, whereas extremity involvement is contralateral, and the distribution of pain may follow the same pattern
 Treatments for Central Post Stroke Pain • • Antidepressants Anticonvulsants Antiarrhythmics Opioids Steroids Intrathecal Baclofen Rehab Techniques • • Regional Anesthesia Electrical Stimulation Deep Brain Stimulation Neuroablative Procedures • Transcranial Magnetic Stimulation
Treatments for Central Post Stroke Pain • • Antidepressants Anticonvulsants Antiarrhythmics Opioids Steroids Intrathecal Baclofen Rehab Techniques • • Regional Anesthesia Electrical Stimulation Deep Brain Stimulation Neuroablative Procedures • Transcranial Magnetic Stimulation
 Amitriptyline for Central Post Stroke Pain • Double blind, three phase, crossover placebo controlled trial in 15 patients, mean age 66, started with 25 mg elavil titrating up to 75 mg • Treatment given in randomized order for 4 weeks, separated by 1 week washout period in which patients were administered amitriptyline, carbamazepine, or placebo • Amitriptyline produced a significantly greater reduction of pain when compared to placebo at week 4 • Pain reduction was positively correlated with plasma concentration of Elavil > 300 nmol/l • Carbamazepine did not produce a statistically significant reduction in pain at doses up to 800 mg / day – Leijon & Boivie, Central Post Stroke Pain, A Controlled Trial of Amitriptyline & Carbamazepine. Pain, 1989, 36: 27 - 36
Amitriptyline for Central Post Stroke Pain • Double blind, three phase, crossover placebo controlled trial in 15 patients, mean age 66, started with 25 mg elavil titrating up to 75 mg • Treatment given in randomized order for 4 weeks, separated by 1 week washout period in which patients were administered amitriptyline, carbamazepine, or placebo • Amitriptyline produced a significantly greater reduction of pain when compared to placebo at week 4 • Pain reduction was positively correlated with plasma concentration of Elavil > 300 nmol/l • Carbamazepine did not produce a statistically significant reduction in pain at doses up to 800 mg / day – Leijon & Boivie, Central Post Stroke Pain, A Controlled Trial of Amitriptyline & Carbamazepine. Pain, 1989, 36: 27 - 36
 Mexilitene for Central Post Stroke Pain • Awerbuch, 1990 : – 9 patients with central pain following stroke were administered 150 mg / day of mexilitene for 3 days followed by 300 mg / day for 3 days, followed by 10 mg / kg / day for one month – Mexilitene produced a significant improvement in pain in 8/9 patients – Need to monitor for QT interval prolongation while on mexilitene • Follow Up Study : up to 800 mg oral mexilitene / day for up to 12 weeks in 12 subjects : No effect Nicholson, Neurology, 2004
Mexilitene for Central Post Stroke Pain • Awerbuch, 1990 : – 9 patients with central pain following stroke were administered 150 mg / day of mexilitene for 3 days followed by 300 mg / day for 3 days, followed by 10 mg / kg / day for one month – Mexilitene produced a significant improvement in pain in 8/9 patients – Need to monitor for QT interval prolongation while on mexilitene • Follow Up Study : up to 800 mg oral mexilitene / day for up to 12 weeks in 12 subjects : No effect Nicholson, Neurology, 2004
 Morphine • Generally ineffective for CPSP • Attal, Neurology, 2002 : Double blind placebo controlled study in 15 subjects with central pain, only 5/15 had CPSP : – IV morphine (average dose 16 mg) decreased pain for up to 120 minutes, but did not decrease evoked pain to stimulus. – In a subsequent follow up year long study with oral morphine 60 – 140 mg / day, only 3/15 patients remained on the oral morphine after one year due to side effects or limited efficacy of the drug • Arner & Meyerson, Pain, 1991 : Minimal clinical response to opiates prescribed for central post stroke pain
Morphine • Generally ineffective for CPSP • Attal, Neurology, 2002 : Double blind placebo controlled study in 15 subjects with central pain, only 5/15 had CPSP : – IV morphine (average dose 16 mg) decreased pain for up to 120 minutes, but did not decrease evoked pain to stimulus. – In a subsequent follow up year long study with oral morphine 60 – 140 mg / day, only 3/15 patients remained on the oral morphine after one year due to side effects or limited efficacy of the drug • Arner & Meyerson, Pain, 1991 : Minimal clinical response to opiates prescribed for central post stroke pain
 Levorphanol for CPSP • Rowbotham et al, 2003 : – 5 CPSP patients placed on 0. 75 mg Levorphanol – 5 CPSP patients placed on 0. 15 mg Levorphanol for 8 weeks – 0. 75 mg dose of levorphanol reduced pain by 36 % as compared with a 21% pain reduction in the low strength group – Only 3/10 patients with CPSP remained in the study due to side effects or limited efficacy of the study drug
Levorphanol for CPSP • Rowbotham et al, 2003 : – 5 CPSP patients placed on 0. 75 mg Levorphanol – 5 CPSP patients placed on 0. 15 mg Levorphanol for 8 weeks – 0. 75 mg dose of levorphanol reduced pain by 36 % as compared with a 21% pain reduction in the low strength group – Only 3/10 patients with CPSP remained in the study due to side effects or limited efficacy of the study drug
 Tramadol • One case report describes a treatment resistant case of CPSP which responded to one infusion of IV tramadol 50 mg followed by daily oral administration of codeine 20 mg and milnacipran 25 mg • The patient had complete relief for 6 days • Symptom recurrence developed after cessation of the codeine and milnacipran • Further research is needed
Tramadol • One case report describes a treatment resistant case of CPSP which responded to one infusion of IV tramadol 50 mg followed by daily oral administration of codeine 20 mg and milnacipran 25 mg • The patient had complete relief for 6 days • Symptom recurrence developed after cessation of the codeine and milnacipran • Further research is needed
 IV Ketamine for CPSP • Vick & Lamer, 2001 : – Case Report of a 68 year old female with refractory CPSP formerly treated with opioids, lidocaine, NSAIDS, mexilitene, & antidepressants – Patient received Ketamine 14 mg IV – Reported marked pain relief & reduced allodynia & hyperalgesia – Oral doses of 50 mg TID were continued – Need to monitor for QT interval prolongation – Long term effects of ketamine are significant
IV Ketamine for CPSP • Vick & Lamer, 2001 : – Case Report of a 68 year old female with refractory CPSP formerly treated with opioids, lidocaine, NSAIDS, mexilitene, & antidepressants – Patient received Ketamine 14 mg IV – Reported marked pain relief & reduced allodynia & hyperalgesia – Oral doses of 50 mg TID were continued – Need to monitor for QT interval prolongation – Long term effects of ketamine are significant
 Opioids in CPSP • Opioid analgesics should only be considered when otherapeutic options fail in CPSP • It has been suggested that the following opioids be considered for use in CPSP if otherapeutic options fail : oxycodone, methadone, buprenorphine, tramadol, and tapentadol
Opioids in CPSP • Opioid analgesics should only be considered when otherapeutic options fail in CPSP • It has been suggested that the following opioids be considered for use in CPSP if otherapeutic options fail : oxycodone, methadone, buprenorphine, tramadol, and tapentadol
 Naloxone for Central Post Stroke Pain • Bainton et al, Pain, 1992 : – Double blind randomized placebo controlled crossover trial in 20 patients of intravenous naloxone 8 mg vs. saline placebo – After a 2 – 3 week washout period, patients switched treatments – 3/20 patients obtained transient relief with naloxone, 4/20 obtained relief from placebo, and 4/20 obtained relief from both – In all cases but one, pain relief disappeared within 24 hours of administration of either naloxone or placebo
Naloxone for Central Post Stroke Pain • Bainton et al, Pain, 1992 : – Double blind randomized placebo controlled crossover trial in 20 patients of intravenous naloxone 8 mg vs. saline placebo – After a 2 – 3 week washout period, patients switched treatments – 3/20 patients obtained transient relief with naloxone, 4/20 obtained relief from placebo, and 4/20 obtained relief from both – In all cases but one, pain relief disappeared within 24 hours of administration of either naloxone or placebo
 Anti Hypertensive Agents in CPSP • Calcium Channel Blockers : No effect on CPSP, but may decrease the sensation of coldness that patients experience • Clonidine : no studies to date in CPSP • Propranolol : potentiates the effect of doxepin in an open label trial in CPSP – Tourian, Pain, 1987
Anti Hypertensive Agents in CPSP • Calcium Channel Blockers : No effect on CPSP, but may decrease the sensation of coldness that patients experience • Clonidine : no studies to date in CPSP • Propranolol : potentiates the effect of doxepin in an open label trial in CPSP – Tourian, Pain, 1987
 Gabapentin For Central Post Stroke Pain • No placebo controlled trial of this drug specifically for CPSP to date • 18 patients with peripheral nerve injuries or CPSP (2 patients) received gabapentin in gradually increasing doses up to 2400 mg/day for a period of 6 weeks • All patients with peripheral nerve injuries and the two patients with CSPS experienced significant relief of ongoing spontaneous pain & reduced paroxysmal pain – Attal et al, 1998
Gabapentin For Central Post Stroke Pain • No placebo controlled trial of this drug specifically for CPSP to date • 18 patients with peripheral nerve injuries or CPSP (2 patients) received gabapentin in gradually increasing doses up to 2400 mg/day for a period of 6 weeks • All patients with peripheral nerve injuries and the two patients with CSPS experienced significant relief of ongoing spontaneous pain & reduced paroxysmal pain – Attal et al, 1998
 Gabapentin For CPSP • Chen et al, AJPMR 2002 : – Case Report of 45 year old male with CPSP on Gabapentin 300 mg po TID whose pain reduced from level 10 to level 4 • Randomized, blinded placebo controlled trial of gabapentin 2400 mg / day for patients with various neuropathic pain conditions, only 2. 9% of the study population had CPSP • Study concluded that patients with all neuropathic pain conditions improved slightly when compared to the placebo group, but the study failed to provide separate data for CPSP – Serpell , Pain, 2002
Gabapentin For CPSP • Chen et al, AJPMR 2002 : – Case Report of 45 year old male with CPSP on Gabapentin 300 mg po TID whose pain reduced from level 10 to level 4 • Randomized, blinded placebo controlled trial of gabapentin 2400 mg / day for patients with various neuropathic pain conditions, only 2. 9% of the study population had CPSP • Study concluded that patients with all neuropathic pain conditions improved slightly when compared to the placebo group, but the study failed to provide separate data for CPSP – Serpell , Pain, 2002
 Lamotrigine for Central Stroke Pain Syndromes • Lamotrigine is an AED which suppresses the release of glutamate and blocks sodium channels • 30 patients with central post stroke pain were treated with lamotrigine in a randomized crossover double blind study • Participants took lamotrigine 200 mg / day or placebo for 8 weeks • Washout period of 2 weeks • Lamotrigine or placebo for 8 weeks • Lamotrigine reduced the pain patients experienced by an average of 30% • 12 patients reported reductions of pain of 2 or more points on the numerical rating scale • Adverse Events : Headache, mild rash, dose escalations are only advised every two weeks as per package insert – Vestergaard et al, Neurology, 2001; 56 (2)
Lamotrigine for Central Stroke Pain Syndromes • Lamotrigine is an AED which suppresses the release of glutamate and blocks sodium channels • 30 patients with central post stroke pain were treated with lamotrigine in a randomized crossover double blind study • Participants took lamotrigine 200 mg / day or placebo for 8 weeks • Washout period of 2 weeks • Lamotrigine or placebo for 8 weeks • Lamotrigine reduced the pain patients experienced by an average of 30% • 12 patients reported reductions of pain of 2 or more points on the numerical rating scale • Adverse Events : Headache, mild rash, dose escalations are only advised every two weeks as per package insert – Vestergaard et al, Neurology, 2001; 56 (2)
 Topiramate & Levetiracetam in CPSP • Topiramate : Second generation AED • Studied in seven patients with central post stroke pain refractory to other agents, including elavil, lamictal, mexilitene, neurontin) • Not found to be effective – Canavero et al, Lack of Effect of Topiramate for Central Pain, Neurology, 2002 • Levetiracetam found ineffective for CPSP in 42 patients receiving a maximum dose of 3000 mg / day
Topiramate & Levetiracetam in CPSP • Topiramate : Second generation AED • Studied in seven patients with central post stroke pain refractory to other agents, including elavil, lamictal, mexilitene, neurontin) • Not found to be effective – Canavero et al, Lack of Effect of Topiramate for Central Pain, Neurology, 2002 • Levetiracetam found ineffective for CPSP in 42 patients receiving a maximum dose of 3000 mg / day
 Pregabalin for Central Post Stroke Pain • Vranken et al. Pregabalin in Patients with Central Neuropathic Pain: A Randomized Double Blind Placebo Controlled Trial of a Flexible Dose Regimen Pain, 2008 – Oral Pregabalin 300 -600 mg po QD was effective in relieving pain in 19 patients with central post stroke pain and 21 SCI patients with central pain syndrome
Pregabalin for Central Post Stroke Pain • Vranken et al. Pregabalin in Patients with Central Neuropathic Pain: A Randomized Double Blind Placebo Controlled Trial of a Flexible Dose Regimen Pain, 2008 – Oral Pregabalin 300 -600 mg po QD was effective in relieving pain in 19 patients with central post stroke pain and 21 SCI patients with central pain syndrome
 Pregabalin for CPSP in 219 Patients • Randomized double blind, parallel group, placebo controlled trial of pregabalin 150 – 600 mg / day in 219 CPSP patients. • The Mean Pain Score on the Daily Pain Rating Scale was not statistically significant between the placebo and treatment groups • The majority of patients on pregabalin did not achieve a 30% or greater reduction in mean pain score compared to baseline. • Patients receiving pregabalin did however have improved sleep and lower anxiety levels than those patients receiving placebo •
Pregabalin for CPSP in 219 Patients • Randomized double blind, parallel group, placebo controlled trial of pregabalin 150 – 600 mg / day in 219 CPSP patients. • The Mean Pain Score on the Daily Pain Rating Scale was not statistically significant between the placebo and treatment groups • The majority of patients on pregabalin did not achieve a 30% or greater reduction in mean pain score compared to baseline. • Patients receiving pregabalin did however have improved sleep and lower anxiety levels than those patients receiving placebo •
 Fluvoxamine for Central Post Stroke Pain • Shimodozono et al, 2002 : – 28 patients with CPSP – Started on Fluvoxamine 25 mg po BID – Doses increased to a maximum of 125 mg per day based on patient symptoms – Treatment period 2 – 4 weeks – Patients with stroke less than one year ago had significant relief of pain – Patients with stroke > 1 yr. ago did not have relief – Celexa and reboxetine (SSRIs) have not been shown to be effective in CPSP
Fluvoxamine for Central Post Stroke Pain • Shimodozono et al, 2002 : – 28 patients with CPSP – Started on Fluvoxamine 25 mg po BID – Doses increased to a maximum of 125 mg per day based on patient symptoms – Treatment period 2 – 4 weeks – Patients with stroke less than one year ago had significant relief of pain – Patients with stroke > 1 yr. ago did not have relief – Celexa and reboxetine (SSRIs) have not been shown to be effective in CPSP
 Intrathecal Baclofen • Several boluses of intrathecal baclofen 50 – 150 mcg was administered to 5 patients with CPSP over the course of one week • 4/5 patients reported relief that lasted 12 – 24 hours post procedure • No response was noted to an intrathecal saline bolus in the subjects • All patients received oral baclofen following intrathecal administration and none of the subjects reported relief
Intrathecal Baclofen • Several boluses of intrathecal baclofen 50 – 150 mcg was administered to 5 patients with CPSP over the course of one week • 4/5 patients reported relief that lasted 12 – 24 hours post procedure • No response was noted to an intrathecal saline bolus in the subjects • All patients received oral baclofen following intrathecal administration and none of the subjects reported relief
 Steroids for CPSP • Retrospective study of 12 patients with CPSP • 7 patients treated with an oral methylprednisolone taper • 5 patients treated with various combinations of more typical drugs • Compared the numerical rating scales for pain in both groups • Methylprednisolone group numerical pain ratings of 1. 7 +/- 2. 1 • Patients receiving typical medications in the control group had numerical pain ratings of 5. 0 +/- 1. 9 – Pellicane et al, J Pain Research, 2013
Steroids for CPSP • Retrospective study of 12 patients with CPSP • 7 patients treated with an oral methylprednisolone taper • 5 patients treated with various combinations of more typical drugs • Compared the numerical rating scales for pain in both groups • Methylprednisolone group numerical pain ratings of 1. 7 +/- 2. 1 • Patients receiving typical medications in the control group had numerical pain ratings of 5. 0 +/- 1. 9 – Pellicane et al, J Pain Research, 2013
 IV Lidocaine Infusion for CPSP • Attal et al, Neurology, 2000 : – 6 patients with CPSP and 10 patients with SCI related central pain syndromes received both lidocaine and saline IV injections 3 weeks apart in a randomized crossover trial – Dose of lidocaine administered : 5 mg / kg – Pain measured on VAS every 15 minutes for 6 hours – Lidocaine treatment group was significantly better than saline tx group for 45 minutes following injection – By 6 hrs post injection, only 1 patient in the lidocaine group and no patients in the saline group reported significant pain relief – This treatment is contraindicated in patients with second or third degree heart block
IV Lidocaine Infusion for CPSP • Attal et al, Neurology, 2000 : – 6 patients with CPSP and 10 patients with SCI related central pain syndromes received both lidocaine and saline IV injections 3 weeks apart in a randomized crossover trial – Dose of lidocaine administered : 5 mg / kg – Pain measured on VAS every 15 minutes for 6 hours – Lidocaine treatment group was significantly better than saline tx group for 45 minutes following injection – By 6 hrs post injection, only 1 patient in the lidocaine group and no patients in the saline group reported significant pain relief – This treatment is contraindicated in patients with second or third degree heart block
 IV Propofol for Post Stroke Pain • 0. 2 mg/kg Propofol bolus was used to treat CPSP in 8 subjects in a double blind placebo controlled study with EKG and BP monitoring. • Patients enrolled in the study had failed previous trials of oral anticonvulsants and antidepressants. • Following administration of the Propofol bolus (or Intralipid placebo) , VAS was measured at 5 minute intervals for 30 minutes • Pain was reduced by 3 – 4 points on the VAS on average with administration of Propofol but not the placebo • Allodynia was abolished in all subjects who received Propofol
IV Propofol for Post Stroke Pain • 0. 2 mg/kg Propofol bolus was used to treat CPSP in 8 subjects in a double blind placebo controlled study with EKG and BP monitoring. • Patients enrolled in the study had failed previous trials of oral anticonvulsants and antidepressants. • Following administration of the Propofol bolus (or Intralipid placebo) , VAS was measured at 5 minute intervals for 30 minutes • Pain was reduced by 3 – 4 points on the VAS on average with administration of Propofol but not the placebo • Allodynia was abolished in all subjects who received Propofol
 Regional Sympathetic Blockade • Has not demonstrated any long term benefit in central post stroke pain – Boivie, “Central Pain” in Melzack & Wall’s Textbook of Pain, 1994 – Bowsher, The Management of Central Post Stroke Pain, Post Grad Med Journal, 1995 – Loh et al, Pain due to Lesion of the Central Nervous System Removed by Sympathetic Block, British Medical Journal, 1981
Regional Sympathetic Blockade • Has not demonstrated any long term benefit in central post stroke pain – Boivie, “Central Pain” in Melzack & Wall’s Textbook of Pain, 1994 – Bowsher, The Management of Central Post Stroke Pain, Post Grad Med Journal, 1995 – Loh et al, Pain due to Lesion of the Central Nervous System Removed by Sympathetic Block, British Medical Journal, 1981
 Use of Implantable Stimulators for Refractory Post Stroke Pain • Katayama & his associates investigated the effect of implantable stimulators on 45 patients with central post stroke pain syndrome • Spinal Cord Stimulation for Post Stroke Pain – effective in only 7% of patients • Deep Brain Stimulation of the thalamic nucleus ventralis caudalis – effective in 25% of patients • Motor Cortex Stimulation – effective in 45% of patients with post stroke pain – Katayama et al, Stereotactic & Functional Neurosurgery, 2001
Use of Implantable Stimulators for Refractory Post Stroke Pain • Katayama & his associates investigated the effect of implantable stimulators on 45 patients with central post stroke pain syndrome • Spinal Cord Stimulation for Post Stroke Pain – effective in only 7% of patients • Deep Brain Stimulation of the thalamic nucleus ventralis caudalis – effective in 25% of patients • Motor Cortex Stimulation – effective in 45% of patients with post stroke pain – Katayama et al, Stereotactic & Functional Neurosurgery, 2001
 Neuro - Ablative Procedures • Thalamotomy of the ventrobasal cortex, post central gyrus cortectomy, and cingulotomy are irrevocable procedures with low probabilities of long term success • These procedures are frequently complicated by unacceptable morbidity, such as new dysesthesias, hemiparesis, cognitive deficits, and even death
Neuro - Ablative Procedures • Thalamotomy of the ventrobasal cortex, post central gyrus cortectomy, and cingulotomy are irrevocable procedures with low probabilities of long term success • These procedures are frequently complicated by unacceptable morbidity, such as new dysesthesias, hemiparesis, cognitive deficits, and even death
 Rehabilitation Techniques for CPSP • Desensitization Protocols – rubbing affected areas with materials of different textures, starting with soft and advancing to rough has been described as helpful – but there are no controlled trials published on efficacy • Contrast Bathes for Hands • Relaxation Techniques • Self Hypnosis • Contracture Prevention thru ROM, splinting • Biofeedback – may reduce muscle tension and increase limb temperature improving patient comfort – Bowsher, Post Grad Med Journal, 1995 – Mohr, Textbook of Stroke, 2004
Rehabilitation Techniques for CPSP • Desensitization Protocols – rubbing affected areas with materials of different textures, starting with soft and advancing to rough has been described as helpful – but there are no controlled trials published on efficacy • Contrast Bathes for Hands • Relaxation Techniques • Self Hypnosis • Contracture Prevention thru ROM, splinting • Biofeedback – may reduce muscle tension and increase limb temperature improving patient comfort – Bowsher, Post Grad Med Journal, 1995 – Mohr, Textbook of Stroke, 2004
 Electroconvulsive Therapy for Treatment of Post Stroke Pain • Fukui et al, The Pain Clinic Journal, 14 (2) August, 2002 – Case Report From Japan regarding a patient with history of thalamic infarction who failed to respond to oral medications, who responded to unilateral ECT applied over the affected hemisphere – Proton magnetic resonance spectroscopy of the affected thalamus was compared pre and post ECT – Post ECT, there was a 32% increase in neural function in the affected portion of thalamus, as measured by n acetylaspartate / creatine ratio measured by proton MR spectroscopy
Electroconvulsive Therapy for Treatment of Post Stroke Pain • Fukui et al, The Pain Clinic Journal, 14 (2) August, 2002 – Case Report From Japan regarding a patient with history of thalamic infarction who failed to respond to oral medications, who responded to unilateral ECT applied over the affected hemisphere – Proton magnetic resonance spectroscopy of the affected thalamus was compared pre and post ECT – Post ECT, there was a 32% increase in neural function in the affected portion of thalamus, as measured by n acetylaspartate / creatine ratio measured by proton MR spectroscopy
 Repetitive Transcranial Magnetic Stimulation for CPSP • In a study of 24 patients with unilateral CPSP, transcranial magnetic stimulation applied over the hand area of the motor cortex for 5 consecutive days at 20 Hz, 10 X 10 stimulation trains, at 80% of motor threshold produced improvements in pain levels for two weeks after stimulation ceased when compared to sham stimulation • Hypothesized to act by increasing cerebral blood flow in thalamus, orbitofrontal area, upper brain stem and cingulate gyrus – Khedr et al, Journal of Neurology, Neurosurgery, and Psychiatry, 2005
Repetitive Transcranial Magnetic Stimulation for CPSP • In a study of 24 patients with unilateral CPSP, transcranial magnetic stimulation applied over the hand area of the motor cortex for 5 consecutive days at 20 Hz, 10 X 10 stimulation trains, at 80% of motor threshold produced improvements in pain levels for two weeks after stimulation ceased when compared to sham stimulation • Hypothesized to act by increasing cerebral blood flow in thalamus, orbitofrontal area, upper brain stem and cingulate gyrus – Khedr et al, Journal of Neurology, Neurosurgery, and Psychiatry, 2005
 Acupuncture for Post Stroke Central Pain Syndrome • Habot et al, Treatments for the Relief of Central Post Stroke Pain in Elderly Patients : A Comparative Study – 40 patients with central post stroke pain at a geriatric center in Israel – Randomly assigned to one of four groups • Group A : Acupuncture • Group B : Carbamazepine • Group C : Maprotiline • Group D : Placebo • Improvement occurred in all treatment groups, however, Improvement was only statistically significant in the acupuncture treatment group • Acupuncture was free of side effects, more efficient in relieving pain, and well tolerated by patients
Acupuncture for Post Stroke Central Pain Syndrome • Habot et al, Treatments for the Relief of Central Post Stroke Pain in Elderly Patients : A Comparative Study – 40 patients with central post stroke pain at a geriatric center in Israel – Randomly assigned to one of four groups • Group A : Acupuncture • Group B : Carbamazepine • Group C : Maprotiline • Group D : Placebo • Improvement occurred in all treatment groups, however, Improvement was only statistically significant in the acupuncture treatment group • Acupuncture was free of side effects, more efficient in relieving pain, and well tolerated by patients
 TENS for Central Post Stroke Pain • • Leijon & Boivie, Central Post Stroke Pain : Effects of High & Low Frequency TENS, Pain, 1989 : – 15 stroke patients received both high (70 – 100 Hz) & low frequency (1 - 4 Hz) TENS 3 times per day for 16 days – VAS assessed at baseline, 60, and 120 minutes following stimulation – Final follow up at 23 – 30 months – 4 patients reported at least a 20% reduction in their pain with ipsilateral stimulation , mean pain reduction was reported at 43% – Significant and long lasting pain relief was obtained in 20% of subjects – 3 patients had relief with high & low frequency stimulation applied ipsilaterally, and 2 patients also had relief with contralateral stimulation – 3 patients continued to use TENS & reported an improvement in their pain symptoms for up to 30 months. Contraindications to the use of TENS : pacemaker or defibrillator
TENS for Central Post Stroke Pain • • Leijon & Boivie, Central Post Stroke Pain : Effects of High & Low Frequency TENS, Pain, 1989 : – 15 stroke patients received both high (70 – 100 Hz) & low frequency (1 - 4 Hz) TENS 3 times per day for 16 days – VAS assessed at baseline, 60, and 120 minutes following stimulation – Final follow up at 23 – 30 months – 4 patients reported at least a 20% reduction in their pain with ipsilateral stimulation , mean pain reduction was reported at 43% – Significant and long lasting pain relief was obtained in 20% of subjects – 3 patients had relief with high & low frequency stimulation applied ipsilaterally, and 2 patients also had relief with contralateral stimulation – 3 patients continued to use TENS & reported an improvement in their pain symptoms for up to 30 months. Contraindications to the use of TENS : pacemaker or defibrillator
 Thanks for Your Attention! • Questions ?
Thanks for Your Attention! • Questions ?


