c07b735c9dbf608d849b81b29c4e7cb2.ppt
- Количество слайдов: 80
Positional Plagiocephaly The Shape of Affairs November 21, 2009 Patricia Mortenson Dr. P. Steinbok Alan Keith

Agenda (Approximate) 1: 00 - 1: 15 Definition, incidence, risk factors l 1: 15 - 1: 45 Synostosis differential (Dr. Steinbok) l 1: 45 - 2: 30 Assessment, treatment, outcomes, sequelae l 15 minute stretch break l 2: 45 - 3: 15 Head banding (Alan Keith) l 3: 15 - 3: 30 Clinical pathways, future, resources l 3: 30 - 4: 00 Questions & problem solving l
OBJECTIVES 1. 2. 3. 4. 5. 6. Define positional plagiocephaly & risk factors Be aware of differential diagnoses Learn assessment techniques Understand treatment guidelines Describe outcomes & sequelae Know how and when to make appropriate referrals in BC
PLAGIOCEPHALY? l l “oblique head” Causes – – – Deformational forces on moldable skull Nature of the infant skull Uterine & post-natal positioning Gravitational forces Correlation with torticollis
INCIDENCE l More cases with Back to Sleep (Persing et al. , 2003) l At birth – – – 13% in singletons Flat spots in 56% of twins (Peitsch et al. , 2002) 61% asymmetry of the head; 16% torticollis (Stelleagen et al. , 2008)
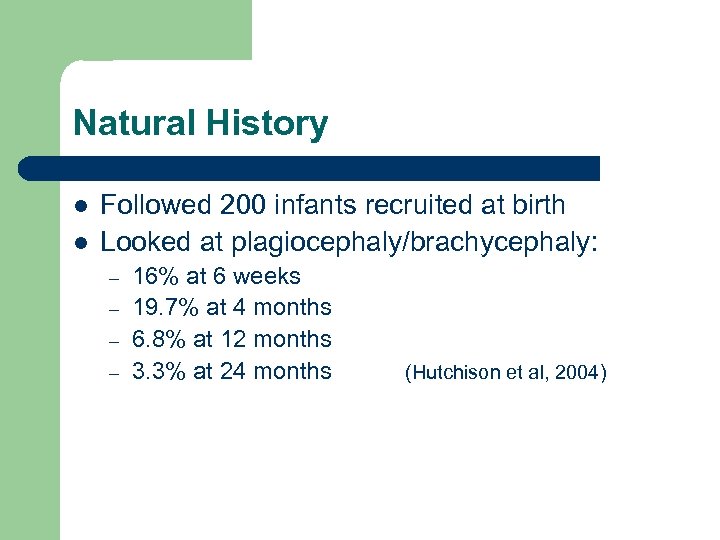
Natural History l l Followed 200 infants recruited at birth Looked at plagiocephaly/brachycephaly: – – 16% at 6 weeks 19. 7% at 4 months 6. 8% at 12 months 3. 3% at 24 months (Hutchison et al, 2004)
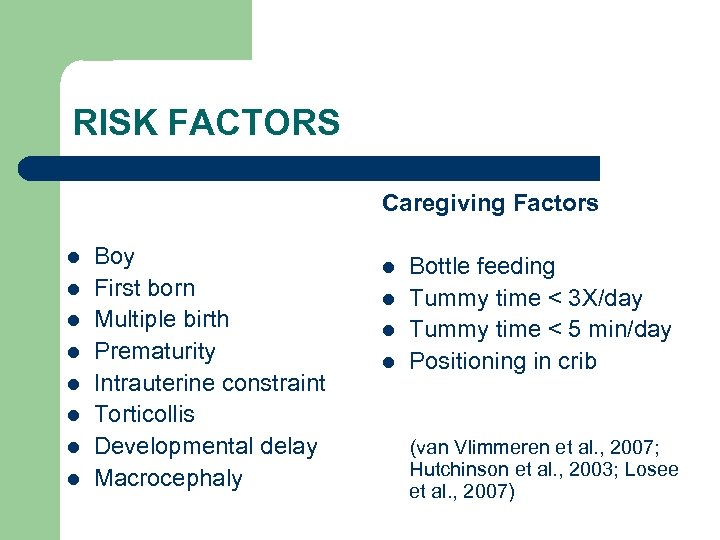
RISK FACTORS Caregiving Factors l l l l Boy First born Multiple birth Prematurity Intrauterine constraint Torticollis Developmental delay Macrocephaly l l Bottle feeding Tummy time < 3 X/day Tummy time < 5 min/day Positioning in crib (van Vlimmeren et al. , 2007; Hutchinson et al. , 2003; Losee et al. , 2007)
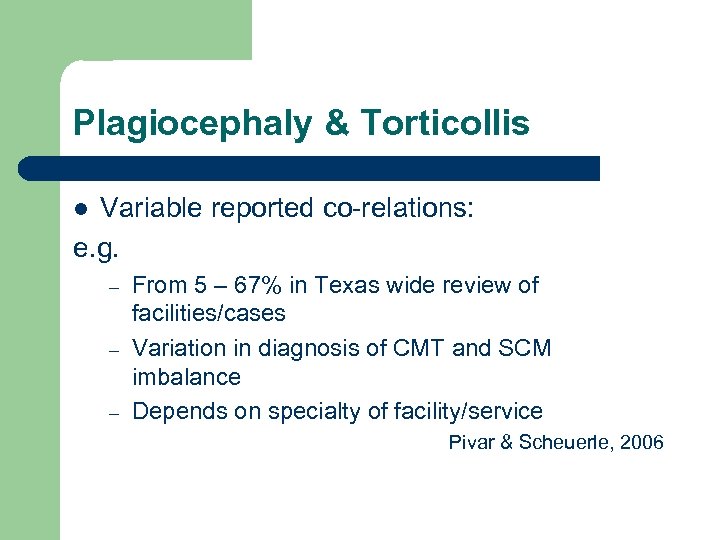
Plagiocephaly & Torticollis Variable reported co-relations: e. g. l – – – From 5 – 67% in Texas wide review of facilities/cases Variation in diagnosis of CMT and SCM imbalance Depends on specialty of facility/service Pivar & Scheuerle, 2006
TYPES
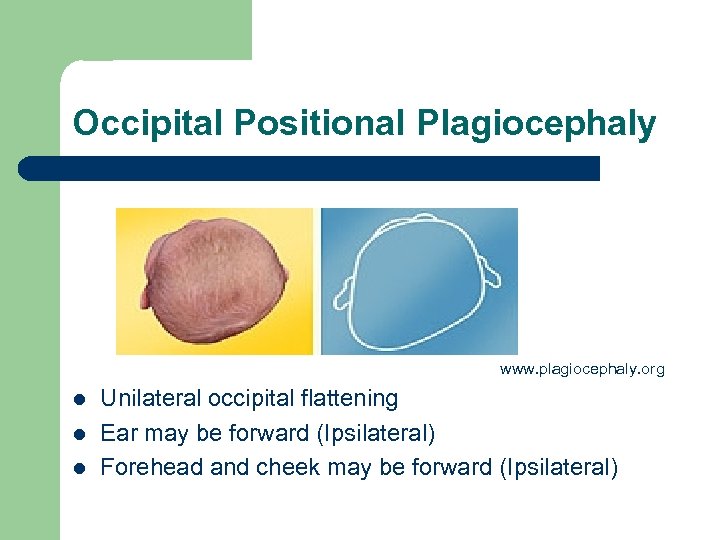
Occipital Positional Plagiocephaly www. plagiocephaly. org l l l Unilateral occipital flattening Ear may be forward (Ipsilateral) Forehead and cheek may be forward (Ipsilateral)
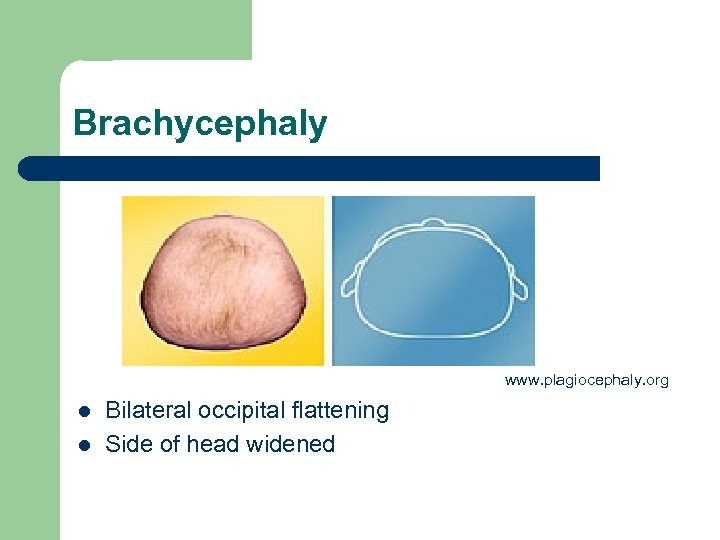
Brachycephaly www. plagiocephaly. org l l Bilateral occipital flattening Side of head widened
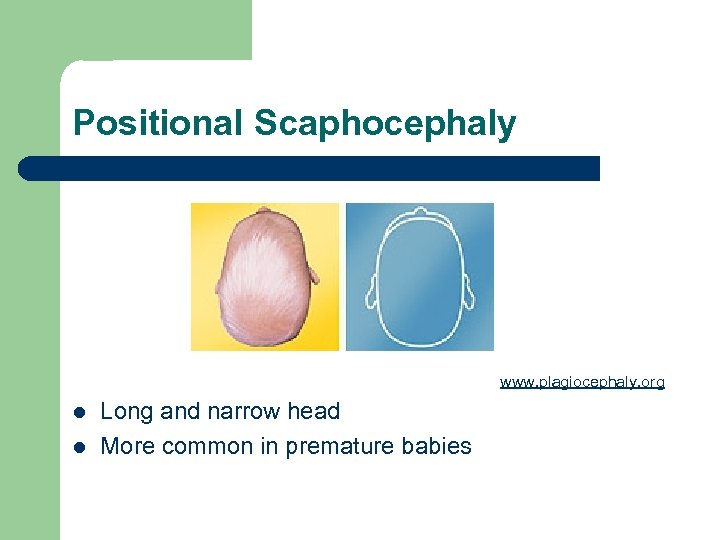
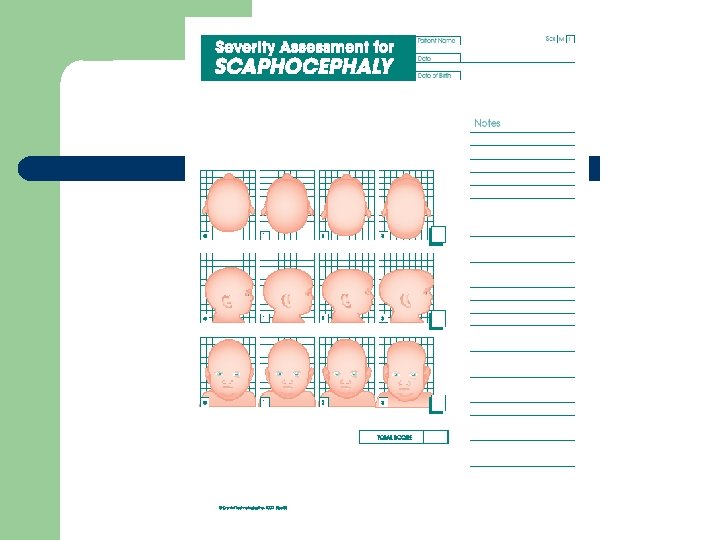
Positional Scaphocephaly www. plagiocephaly. org l l Long and narrow head More common in premature babies

ASSESSMENT & TREATMENT
HISTORY l l l Pregnancy, Birth & Neonatal history When did parents first notice Stayed same, gotten better/worse? Torticollis? What strategies have they already tried
HISTORY l l Positioning for sleep, feeding, play ? Tummy Time spent in car seats, swings etc. Development
CLINICAL ASSESSMENT l View from top, back, sides, front
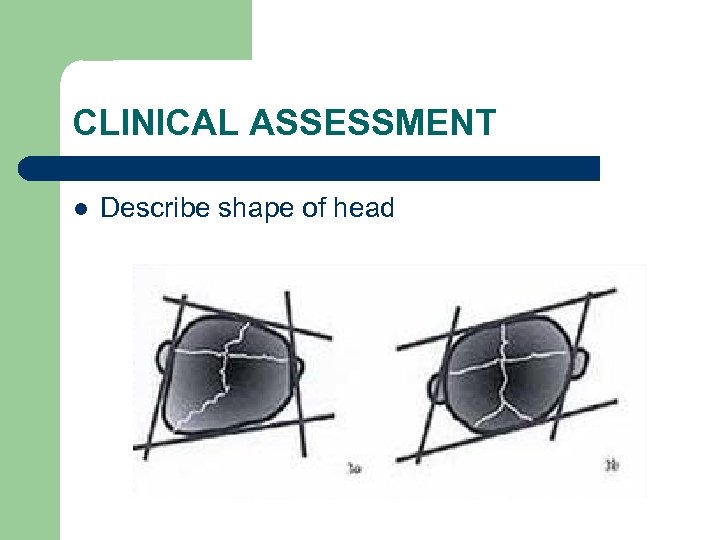
CLINICAL ASSESSMENT l Describe shape of head
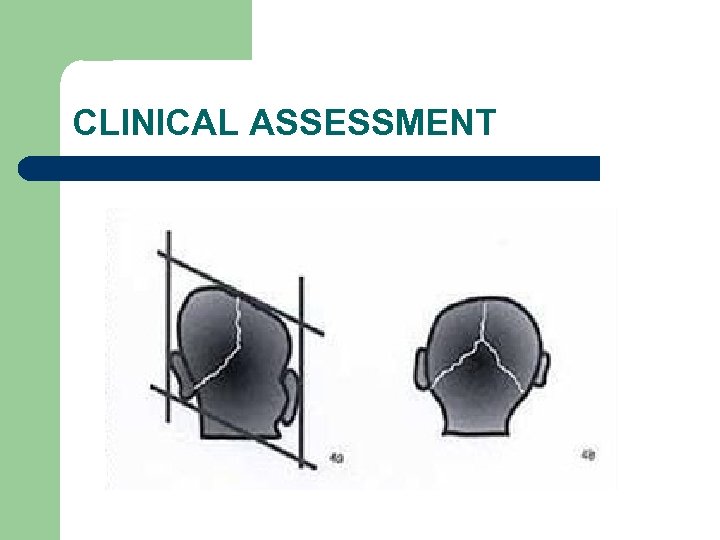
CLINICAL ASSESSMENT
CLINICAL ASSESSMENT l l Eye symmetry & shape When in doubt refer to neurosurgery
Clinical Assessment l Check head turning and tilt l If possible, assess in sitting, supine & prone
? HOW TO QUANTIFY
Measurement l Challenges: – – 2 D measures on 3 D object Squirmy subjects l Variety of methods: – – – Visual ratings Anthropometric (caliper measures) Digital photos CT scan Laser scanner
Measurement Issues l Issues with – – Classification Reliability Cost Radiation & Sedation (Mortenson & Steinbok, 2006) l Need standardized classification system (Mc. Garry et al. , 2008)

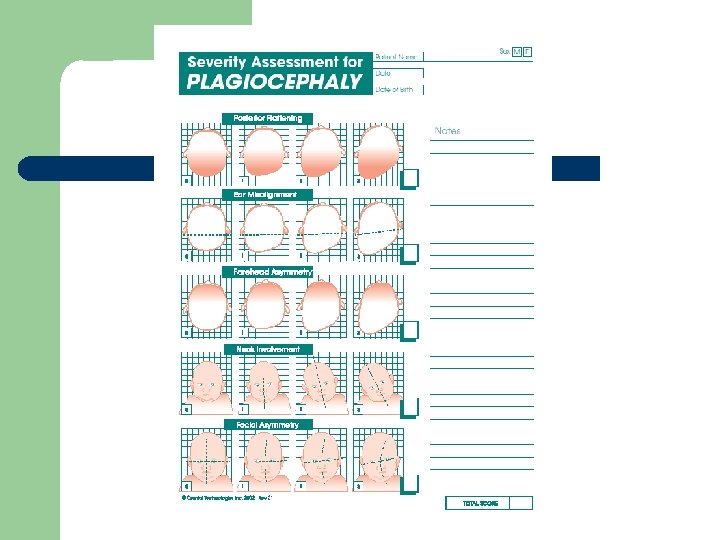
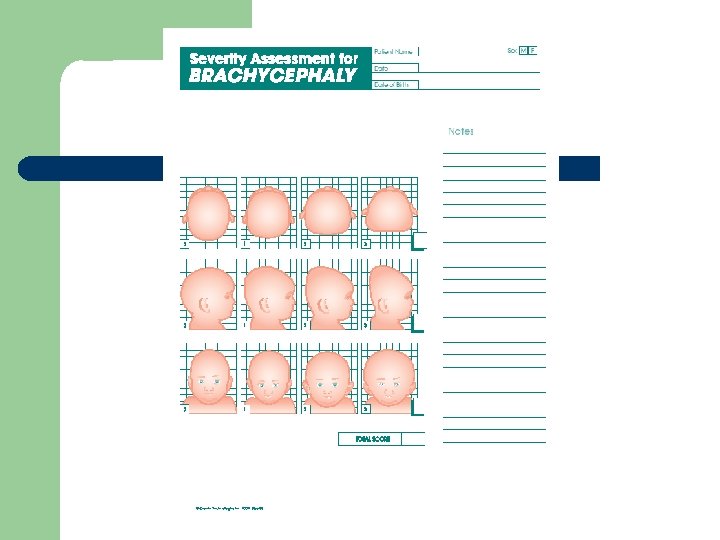
For now…. l Argenta’s clinical classification l Severity assessment sheets available at: www. cranialtech. com – ? Reliability / validity
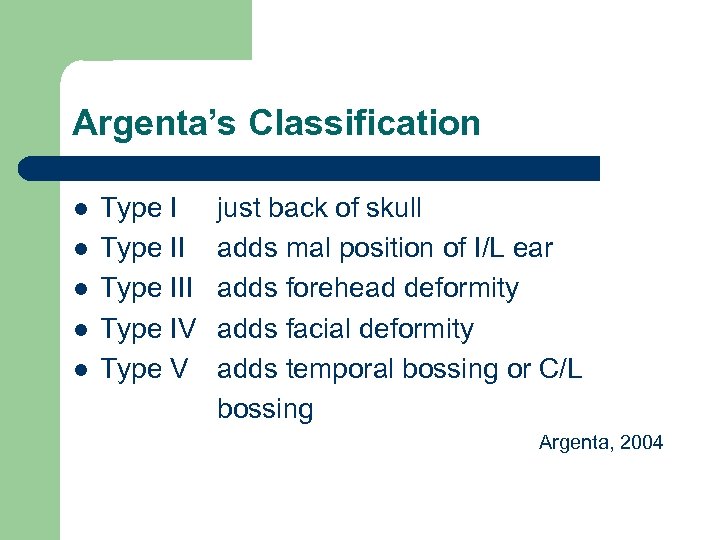
Argenta’s Classification l l l Type III Type IV Type V just back of skull adds mal position of I/L ear adds forehead deformity adds facial deformity adds temporal bossing or C/L bossing Argenta, 2004
Argenta’s Classification l Moderately reliable for Types I – IV (flatenning, ear malposition, frontal bossing, facial asymmetry) l but NOT for vertical skull height (Spermon et al, 2008) l ? Degree & responsiveness, ? Validity
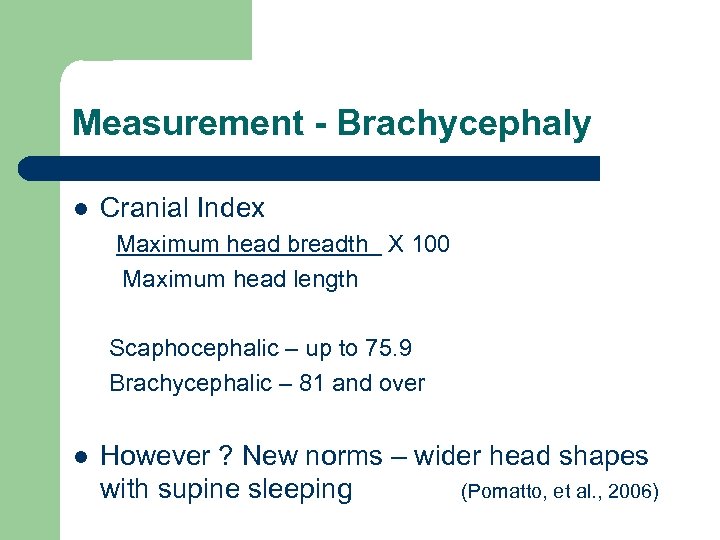
Measurement - Brachycephaly l Cranial Index Maximum head breadth X 100 Maximum head length Scaphocephalic – up to 75. 9 Brachycephalic – 81 and over l However ? New norms – wider head shapes with supine sleeping (Pomatto, et al. , 2006)
Argenta’s Classification l l l Type I central posterior skull Type II widening of the skull Type III Temporal or vertical skull growth Argenta, 2004 l ? Reliability/validity

TREATMENT
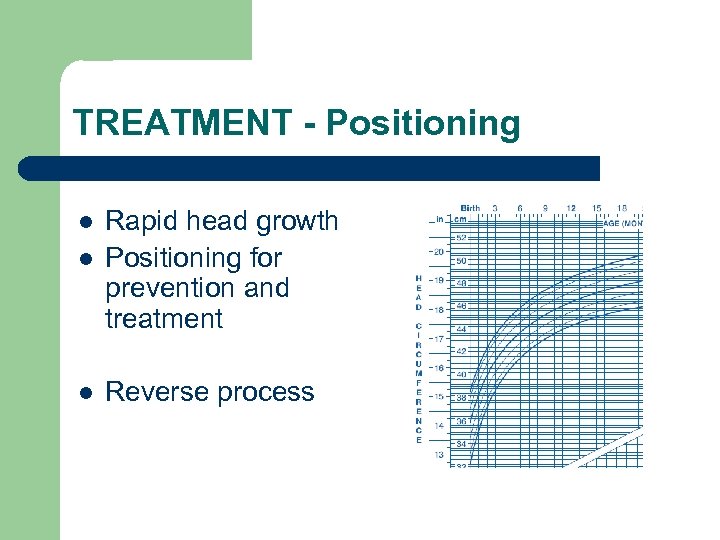
TREATMENT - Positioning l Rapid head growth Positioning for prevention and treatment l Reverse process l
SLEEP POSITION l l l Place in crib so baby looks into room on the “round” side Place mobile/crib mirror on “round” side Turn head when asleep
SLEEP PRODUCTS l American Academy Position Statement “We recommend that firm flat bedding be used for normal healthy infants, with sheets and light blankets as needed, but without products to maintain the sleeping position. ” www. cps. ca/english/statements/IP/cps 98 -01. htm#sleep

POTENTIAL PRODUCTS Safe T Sleep l www. safetsleep. com l l Not approved by CPA Cautious use, Hutchison et al. , 2007
POTENTIAL PRODUCTS l Cranial cup l Custom molded “dish” for head to rest in during sleep Weak evidence that effective in correcting early plagio l (Rogers et al. , 2008) l ? Safety and approval for use
UPRIGHT l l Use of carriers Hip belts & wide straps Ergo carrier Baby Trecker
PLAY POSITION Awake & up l Tummy time l Supported sitting l Side lying for play l
TUMMY TIME l Start with short but FREQUENT times l Options include: – On chest – Over legs – Supported on Floor
TUMMY TIME TEACHING BE: l Encouraging l Realistic l Demonstrate on baby OR doll
BUMBO • Not all babies tolerate • never use on an elevated surface • supervise • www. bumbosafety. com
SIDE LYING l l On Round side Best for pre-rollers Rolled blankets “Sleep” positioning devices
FEEDING POSITION Bottle feed from “round” side l Feed from “round” side in highchair l
BABY EQUIPMENT l l Car seat stays in car Stroller 101 Limit Swing Use Good equipment
IMPORTANT FACTORS l Multiple options for caregivers Realistic Demonstration as needed l Address any developmental factors l l
TREATMENT - Orthotic Headband l Indications – – – l l How it works Wear – l Moderate/severe Face involved Positioning not working 23 hours/day for months Limitations – – – Cost Commitment Hot weather
TREATMENT – Other issues l Torticollis – need to treat – Positioning not as effective (Losee et al. , 2007) l l Motor & Developmental delays Parental guilt
OUTCOMES & SEQUELAE
OUTCOMES l Natural improvement (Hutchison et al. , 2004) l Conflicting evidence – 3 systematic reviews – – – Positioning OR headband > than leaving be Positioning = headband but takes longer Helmet > positioning (most studies) (Bialocerkowski et al. , 2005; Mc. Garry, 2008; Xia et al. , 2008)
Controversies l 1. 2. 3. Limitations in studies: No standard measures, poor reliability & validity No Randomization Observer and intervention biases – – Observers not blinded More severe cases selected to head band groups
Intensive Intervention RCT van Vlimmeren, et al. , 2008 l 380 neonates at 7 wks → 68 had positional preference l 65 Randomized to 2 groups: – – Control → pamphlet only Intervention → 8 PT sessions for positioning & development l Intervention group → severe plagio reduced by 46% (6 mos) & 57% (12 mos) l At 12 months: No differences in motor development No positional preferences either group
Head banding – long term f/u l Changes post head band are stable at 5 years post treatment (Lee et al. , 2008)
What to do in cases of poor evidence? l What is the goal? Ø l Potential benefits Potential harm Uncertainty about estimates of these Regret with a wrong decision Ø l l Ø Ø Ø Improved quality of life Improved cosmetics Cost and time High degree of uncertainty ? Likely low Phelps, 2008
OUTCOMES l Age of identification & treatment is important l Early identification & treatment = better results (Losee et al. , 2007; Persing et al. , 2003; Mc. Garry et al. , 2008)) l > 12 months – little improvement
EMERGING CONSENSUS? l Infants < 5 -6 months → positioning l Infants > 6 months → headband (if no improvement and facial involvement) l Infants > 12 months →limited efficacy (Losee & Mason, 2005; Graham et al. , 2005; Mc. Garry et al. , 2008; Xia et al. , 2008)
SEQUELAE l Not well studied Weak evidence l Many claims unsubstantiated: l – – Migraines Vision problems
Sequelae l Bonding – l Hearing & Vision – – l Infants with molding less cute (Budrea, 1989) No strabismus (Gupta et al. , 2003) ↓Auditory responses (Balan et al. , 2002) Dental – At 5 yrs, ? Occlusal deformities that may impact orthodontic planning – not formally studied (Lee et al. , 2008)
SEQUELAE - Development l Different distribution of Bayley II scores than norms (Kordestani et al. , 2006; Panchal et al. , 2001) Mental → 90% normal; 0 accelerated; 7% mild delay; 3% severe delay – Motor → 74% normal; 0 accelerated; 19% mild delay; 7% severe delay – Other confounding variables – Overstate delay - ? Significant mental delay (yet % delays within standardized norms) –
SEQUELAE - Development l ↑Special needs at school (39. 7%) (Habal et al. , 2003) l More likely to have altered tone compared to control group – No sig. difference in development (Ages & Stages) (Fowler et al. , 2008) l Anthropological evidence - head deformation does not lead to cognitive impairment (Lekovic et al. , 2007)
Development Factors l l l Delay is a risk factor for PP Children sleeping supine have slower motor development Most children with PP have Normal develop. ? PP a risk factor for delay VS children with delays at ↑ risk of PP Co relation NOT Cause/effect
PRONE DEVELOPMENT Systematic review by Pin et al. , 2007: Time in prone correlated to earlier motor milestones - BUT effect was transitory - Similar for pre-term infants, but only 2 studies l Baby equipment use does not seem to impact motor l ? Movement quality differences l ? Impact of lower SES & infant position on development l
LONG TERM SEQUELAE l l Not well studied At 5+ years: – – – Questionnaires completed by 65 families (278 eligible) Residual asymmetry noted by parents in 58%; 21% concerned 2 felt to be “very abnormal”; 25 “mildly abnormal” (Steinbok et al. , 2007)
LONG TERM SEQUELAE l 18 had used headbands – 14 felt had helped “quite a bit” – l l Little difference in outcome, but initial bias for who had been referred for bands 7. 7% of children had commented about their head shape 4. 6% teased occasionally
LONG TERM SEQUELAE l 14% received special assistance in school (BC average is 10. 2%) At initial diagnosis 8% had comorbid diagnoses consistent with delay; 5% had risk factors l Overall reassurance for parents l
LONG TERM Govaert et al. , 2008 l l QOL in post helmet group at preschool age by questionnaire (47% response rate) No differences in QOL compared to normal group 44/46 parents reported would do helmetting again Weak study
PARENTAL CONCERN l l l Awareness vs. Information overload fueling consumer drive TV, newspaper and magazine stories Parent support networks, chat groups – l www. cappskids. org Commercial products
WHAT WE ARE DOING IN BC
BCCH PROGRAM l l l 4 years ago reaching “critical level” of referrals to neurosurgery Impact on wait times for critical neurosurgical consults & infants with PP Limited resources
BCCH PROGRAM OT Plagiocephaly Clinic l l Parent education group with individual assessment Concurrent with Torticollis & Neurosurgery clinics 4 new patients/wk, 2 follow-ups
BCCH PROGRAM l Parent Satisfaction & waitlists tracked over first year of program: l Parents reported: – – l feeling comfortable in the group setting meeting other families was helpful having all of their questions answered positive experience Wait times for infants with PP decreased from 4 to <1 months.
BCCH PROGRAM l l Small program (0. 1 FTE) Impact of over referrals – No need to refer mild cases
Other Health Regions l l l Families outside lower mainland not well served Often sent down inappropriately or too late Opportunities for collaboration & regional clinics
WITHIN BC - Headbands l Valley Orthocare Scanner? l No MSP coverage for headbands l – – – Pharmacare Ministry Extended Health Plans
WHAT TO DO - Prevention l l Back to sleep, tummy for play Early parental awareness l Evaluation of head shape & care giving routines at well baby visits l Early identification and treatment = better results … but don’t stress parents
WHAT TO DO - Plagiocephaly l < 5 months – reposition and monitor l 5 + months If positioning not working – Facial / ear involvement – Moderate to severe → consider headband → can refer to BCCH OT dept (need physician referral) –
WHAT TO DO - Brachycephaly l More difficult to treat – l l Can try if severe, treat early Look at family pattern Flatter & wider may be the new norm (Pomatto et al. , 2006)
TAKE HOME MESSAGES l l PREVENTION Reassurance for mild cases – Monitor, but usually no need for further referral l Early Identification & treatment for moderate to severe cases l Opportunity for collaboration for “Closer to home” services
RESOURCES l Clinician’s Guide available Coming - Caregivers’ Guide l Reference list l Websites with caution l www. cheo. on. ca www. sickkids. ca – search plagiocephaly www. plagiocephaly. org www. cranialtech. com www. cappskids. org
Comments? Questions?
c07b735c9dbf608d849b81b29c4e7cb2.ppt