abdb4d57762184495ba3528ec9243497.ppt
- Количество слайдов: 72
 Play file: 0 - Tequila 1
Play file: 0 - Tequila 1
 The Medical Management of ALCOHOL WITHDRAWAL John J. Stasinos, M. D. LTC(P), MC, USA Chief, Chemical Addictions Treatment Services Department of Psychiatry Tripler Army Medical Center 2
The Medical Management of ALCOHOL WITHDRAWAL John J. Stasinos, M. D. LTC(P), MC, USA Chief, Chemical Addictions Treatment Services Department of Psychiatry Tripler Army Medical Center 2
 Disclosures I have no affiliation or financial relationship with any pharmaceutical companies n The opinions stated herein are my own n Off-label use of medications will be discussed n I am not on any medications or moodaltering substances. . . n 3
Disclosures I have no affiliation or financial relationship with any pharmaceutical companies n The opinions stated herein are my own n Off-label use of medications will be discussed n I am not on any medications or moodaltering substances. . . n 3
 Outline n n n Epidemiology Definitions Pathophysiology n n n Diagnosis Manifestations Management 4
Outline n n n Epidemiology Definitions Pathophysiology n n n Diagnosis Manifestations Management 4
 Objectives n By the end of this briefing, you will be able to… n n Identify, assess, & diagnose patients in acute Et. OH withdrawal Determine the best setting for conducting management of withdrawal symptoms Manage patients with medically complicated Et. OH withdrawal Grasp systemic & administrative issues that complicate care & put patients at unnecessary risk 5
Objectives n By the end of this briefing, you will be able to… n n Identify, assess, & diagnose patients in acute Et. OH withdrawal Determine the best setting for conducting management of withdrawal symptoms Manage patients with medically complicated Et. OH withdrawal Grasp systemic & administrative issues that complicate care & put patients at unnecessary risk 5
 Why Are We Even Talking About This? . . . Joint Commission standards & policies have impacted our perceptions & decisions regarding medical management of Et. OH withdrawal n Disagreement persists among health care providers regarding how & where these patients are best cared for n 6
Why Are We Even Talking About This? . . . Joint Commission standards & policies have impacted our perceptions & decisions regarding medical management of Et. OH withdrawal n Disagreement persists among health care providers regarding how & where these patients are best cared for n 6
 What Standards? . . . n n n Joint Commission recently published new standards that specifically apply to procedure of “detoxification” Standards require personnel, training, & equipment that represent considerable $ Some institutions sidestep the issue by declaring: “WE DON’T DO DETOX” 7
What Standards? . . . n n n Joint Commission recently published new standards that specifically apply to procedure of “detoxification” Standards require personnel, training, & equipment that represent considerable $ Some institutions sidestep the issue by declaring: “WE DON’T DO DETOX” 7
 What Disagreement? . . . 8
What Disagreement? . . . 8
 The Good Patient n n n n Acknowledges illness & need for treatment Seeks out medical care appropriately Communicates clearly & transparently with health care provider Complies with treatment Responds to treatment Thanks the M. D. (& pays their medical bills) Goes away 9
The Good Patient n n n n Acknowledges illness & need for treatment Seeks out medical care appropriately Communicates clearly & transparently with health care provider Complies with treatment Responds to treatment Thanks the M. D. (& pays their medical bills) Goes away 9
 But these patients… n n n n Deny their illness Use up precious medical resources Can’t be reasoned with Do not comply with treatment Are unruly, agitated, uncooperative, & ungrateful Refuse potentially lifesaving care And they keep coming back ! 10
But these patients… n n n n Deny their illness Use up precious medical resources Can’t be reasoned with Do not comply with treatment Are unruly, agitated, uncooperative, & ungrateful Refuse potentially lifesaving care And they keep coming back ! 10
 HOT POTATO! = 11
HOT POTATO! = 11
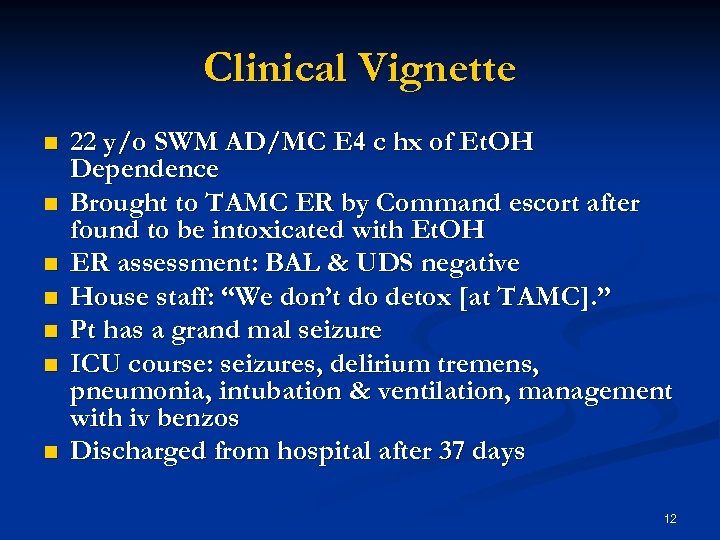 Clinical Vignette n n n n 22 y/o SWM AD/MC E 4 c hx of Et. OH Dependence Brought to TAMC ER by Command escort after found to be intoxicated with Et. OH ER assessment: BAL & UDS negative House staff: “We don’t do detox [at TAMC]. ” Pt has a grand mal seizure ICU course: seizures, delirium tremens, pneumonia, intubation & ventilation, management with iv benzos Discharged from hospital after 37 days 12
Clinical Vignette n n n n 22 y/o SWM AD/MC E 4 c hx of Et. OH Dependence Brought to TAMC ER by Command escort after found to be intoxicated with Et. OH ER assessment: BAL & UDS negative House staff: “We don’t do detox [at TAMC]. ” Pt has a grand mal seizure ICU course: seizures, delirium tremens, pneumonia, intubation & ventilation, management with iv benzos Discharged from hospital after 37 days 12
 13
13
 Terminology n Withdrawal n Characteristic group of signs & symptoms that typically develop after rapid, marked decrease or discontinuation of a substance of dependence, which may or may not be clinically significantly or life threatening. 14
Terminology n Withdrawal n Characteristic group of signs & symptoms that typically develop after rapid, marked decrease or discontinuation of a substance of dependence, which may or may not be clinically significantly or life threatening. 14
 Terminology n Detoxification: n Interventions aimed at managing acute intoxication & withdrawal in order to clear toxins from body & minimize physical harm from substance use. n Generic Marine (has he been drinking? . . . ) 15
Terminology n Detoxification: n Interventions aimed at managing acute intoxication & withdrawal in order to clear toxins from body & minimize physical harm from substance use. n Generic Marine (has he been drinking? . . . ) 15
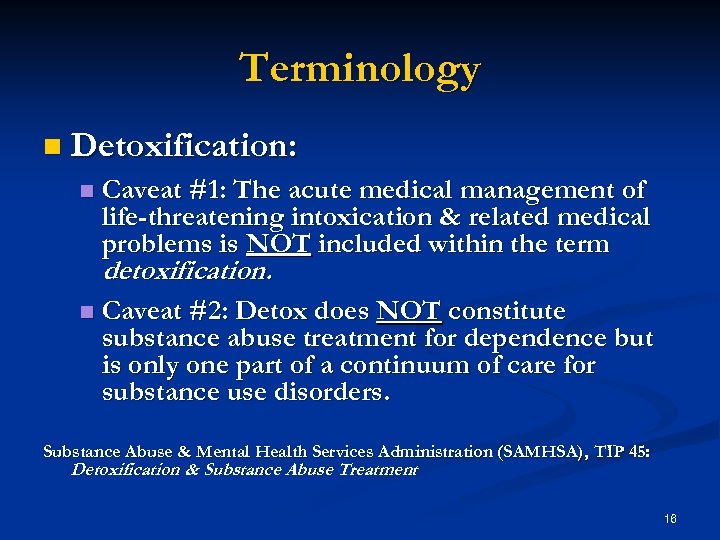 Terminology n Detoxification: n Caveat #1: The acute medical management of life-threatening intoxication & related medical problems is NOT included within the term detoxification. n Caveat #2: Detox does NOT constitute substance abuse treatment for dependence but is only one part of a continuum of care for substance use disorders. Substance Abuse & Mental Health Services Administration (SAMHSA), TIP 45: Detoxification & Substance Abuse Treatment 16
Terminology n Detoxification: n Caveat #1: The acute medical management of life-threatening intoxication & related medical problems is NOT included within the term detoxification. n Caveat #2: Detox does NOT constitute substance abuse treatment for dependence but is only one part of a continuum of care for substance use disorders. Substance Abuse & Mental Health Services Administration (SAMHSA), TIP 45: Detoxification & Substance Abuse Treatment 16
 Do we do inpatient detox? . . . n Patients ARE NOT hospitalized on an elective basis for detox purposes if… n n patient’s withdrawal symptoms can be managed in a less restrictive setting; patient has access to outpatient resources; patient has the benefit of family or other supports to monitor & provide support during detox process. We DO hospitalize patients for the clinical management of Medically Complicated Withdrawal. 17
Do we do inpatient detox? . . . n Patients ARE NOT hospitalized on an elective basis for detox purposes if… n n patient’s withdrawal symptoms can be managed in a less restrictive setting; patient has access to outpatient resources; patient has the benefit of family or other supports to monitor & provide support during detox process. We DO hospitalize patients for the clinical management of Medically Complicated Withdrawal. 17
 Do we do inpatient detox? . . . n Medical complications of substance withdrawal may be benign or life-threatening, depending on… n n n Substance used: e. g. , Et. OH, Benzodiazepines, etc. Patient’s hx of prior withdrawals Patient’s age: older more severe Number & severity of medical problems Severe or high risk withdrawal requires inpatient medical treatment 18
Do we do inpatient detox? . . . n Medical complications of substance withdrawal may be benign or life-threatening, depending on… n n n Substance used: e. g. , Et. OH, Benzodiazepines, etc. Patient’s hx of prior withdrawals Patient’s age: older more severe Number & severity of medical problems Severe or high risk withdrawal requires inpatient medical treatment 18
 Management of Et. OH Withdrawal n Consists of 3 essential components: Clinical assessment n Management of medical complications of withdrawal n Transition of patient into substance abuse treatment (REHAB) n n Intervention that does not incorporate all 3 components is incomplete & inadequate 19
Management of Et. OH Withdrawal n Consists of 3 essential components: Clinical assessment n Management of medical complications of withdrawal n Transition of patient into substance abuse treatment (REHAB) n n Intervention that does not incorporate all 3 components is incomplete & inadequate 19
 Et. OH Intoxication Diagnostic Criteria n n n Recent Ingestion of Et. OH Clinically significant maladaptive behavioral or psychological changes One or more of the following signs, following Et. OH use: n n n n Slurred speech Incoordination Unsteady gait Nystagmus Impairment in attention or memory Stupor or coma Symptoms are not due to a general medical condition or another mental disorder 20
Et. OH Intoxication Diagnostic Criteria n n n Recent Ingestion of Et. OH Clinically significant maladaptive behavioral or psychological changes One or more of the following signs, following Et. OH use: n n n n Slurred speech Incoordination Unsteady gait Nystagmus Impairment in attention or memory Stupor or coma Symptoms are not due to a general medical condition or another mental disorder 20
 21
21
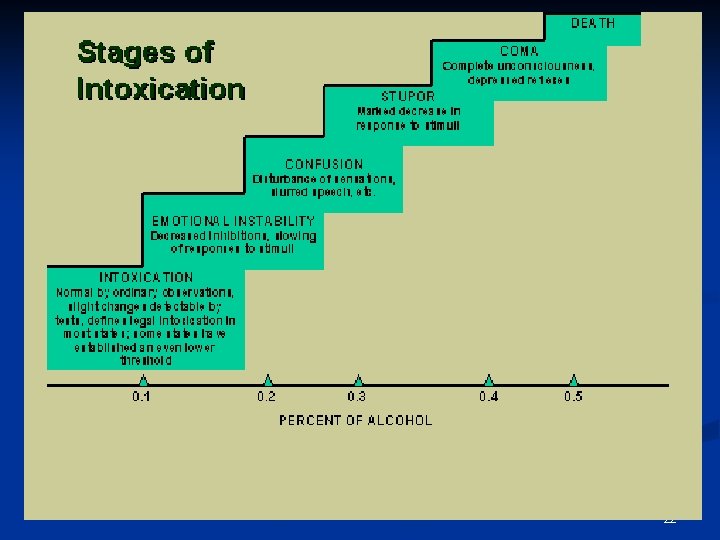 22
22
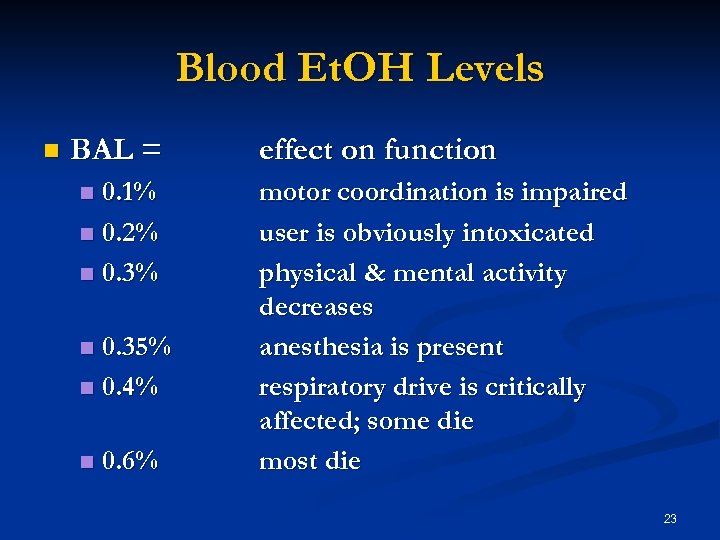 Blood Et. OH Levels n BAL = 0. 1% n 0. 2% n 0. 35% n 0. 4% n n 0. 6% effect on function motor coordination is impaired user is obviously intoxicated physical & mental activity decreases anesthesia is present respiratory drive is critically affected; some die most die 23
Blood Et. OH Levels n BAL = 0. 1% n 0. 2% n 0. 35% n 0. 4% n n 0. 6% effect on function motor coordination is impaired user is obviously intoxicated physical & mental activity decreases anesthesia is present respiratory drive is critically affected; some die most die 23
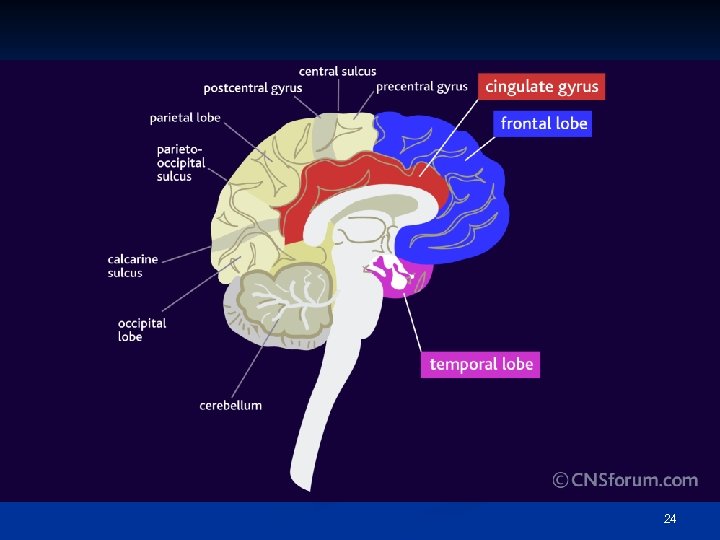 24
24
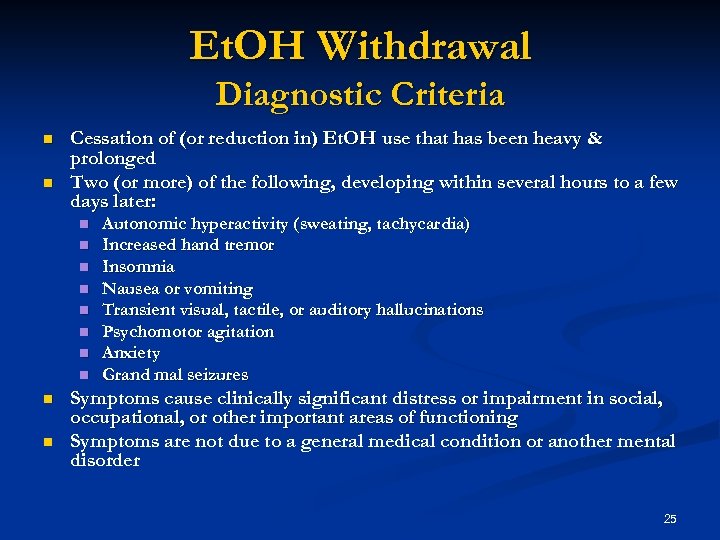 Et. OH Withdrawal Diagnostic Criteria n n Cessation of (or reduction in) Et. OH use that has been heavy & prolonged Two (or more) of the following, developing within several hours to a few days later: n n n n n Autonomic hyperactivity (sweating, tachycardia) Increased hand tremor Insomnia Nausea or vomiting Transient visual, tactile, or auditory hallucinations Psychomotor agitation Anxiety Grand mal seizures Symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning Symptoms are not due to a general medical condition or another mental disorder 25
Et. OH Withdrawal Diagnostic Criteria n n Cessation of (or reduction in) Et. OH use that has been heavy & prolonged Two (or more) of the following, developing within several hours to a few days later: n n n n n Autonomic hyperactivity (sweating, tachycardia) Increased hand tremor Insomnia Nausea or vomiting Transient visual, tactile, or auditory hallucinations Psychomotor agitation Anxiety Grand mal seizures Symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning Symptoms are not due to a general medical condition or another mental disorder 25
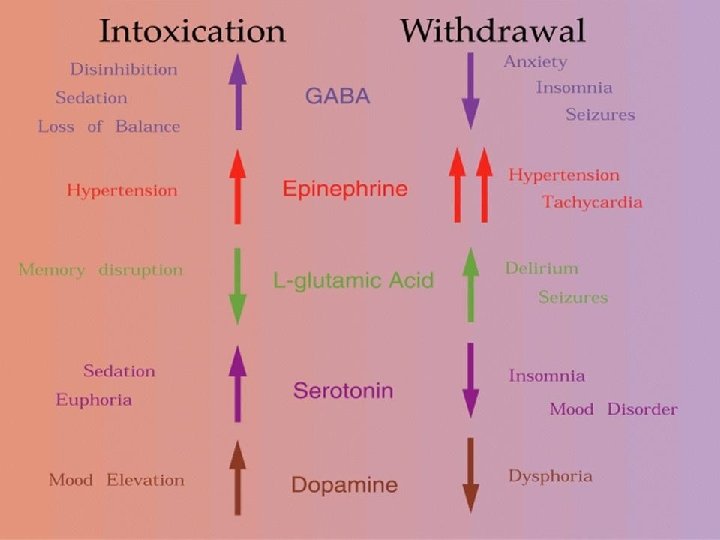
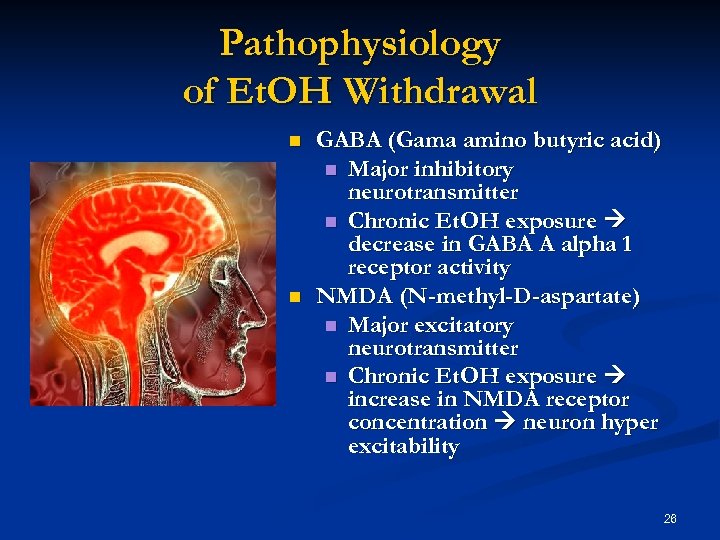 Pathophysiology of Et. OH Withdrawal n n GABA (Gama amino butyric acid) n Major inhibitory neurotransmitter n Chronic Et. OH exposure decrease in GABA A alpha 1 receptor activity NMDA (N-methyl-D-aspartate) n Major excitatory neurotransmitter n Chronic Et. OH exposure increase in NMDA receptor concentration neuron hyper excitability 26
Pathophysiology of Et. OH Withdrawal n n GABA (Gama amino butyric acid) n Major inhibitory neurotransmitter n Chronic Et. OH exposure decrease in GABA A alpha 1 receptor activity NMDA (N-methyl-D-aspartate) n Major excitatory neurotransmitter n Chronic Et. OH exposure increase in NMDA receptor concentration neuron hyper excitability 26
 27
27
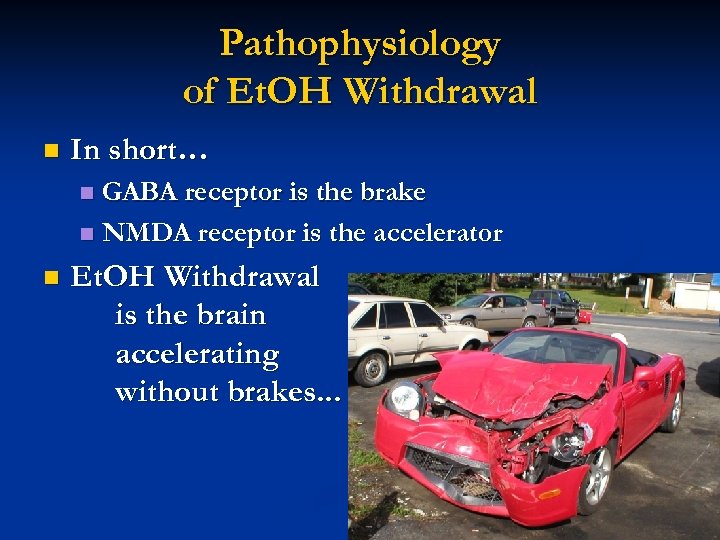 Pathophysiology of Et. OH Withdrawal n In short… GABA receptor is the brake n NMDA receptor is the accelerator n n Et. OH Withdrawal is the brain accelerating without brakes. . . 28
Pathophysiology of Et. OH Withdrawal n In short… GABA receptor is the brake n NMDA receptor is the accelerator n n Et. OH Withdrawal is the brain accelerating without brakes. . . 28
 Factors affecting Course of Withdrawal Severity & duration of withdrawal depend on: 1. 2. 3. 4. 5. 6. 7. Nature of substance Half-life & duration of action Length of time substance used Amount used Use of other substances Presence of other medical & psychiatric conditions Individual biopsychosocial variables 29
Factors affecting Course of Withdrawal Severity & duration of withdrawal depend on: 1. 2. 3. 4. 5. 6. 7. Nature of substance Half-life & duration of action Length of time substance used Amount used Use of other substances Presence of other medical & psychiatric conditions Individual biopsychosocial variables 29
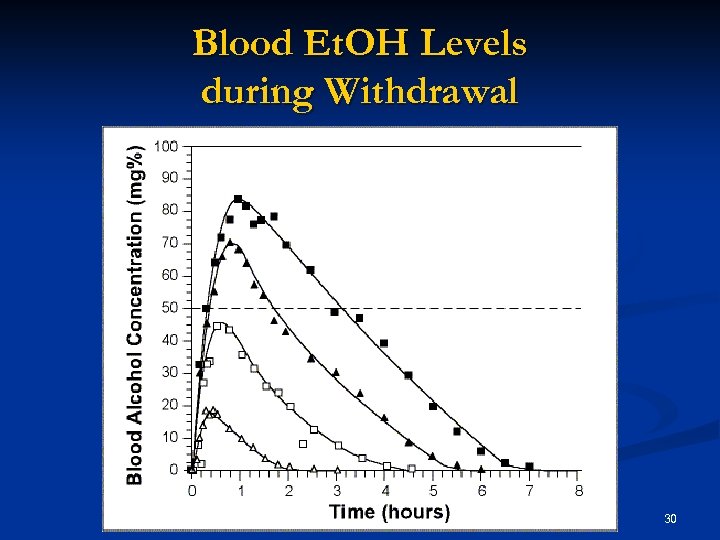 Blood Et. OH Levels during Withdrawal 30
Blood Et. OH Levels during Withdrawal 30
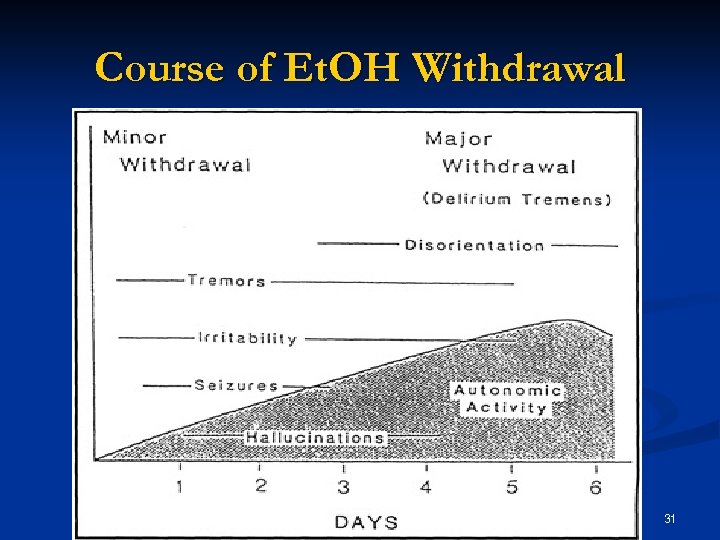 Course of Et. OH Withdrawal 31
Course of Et. OH Withdrawal 31
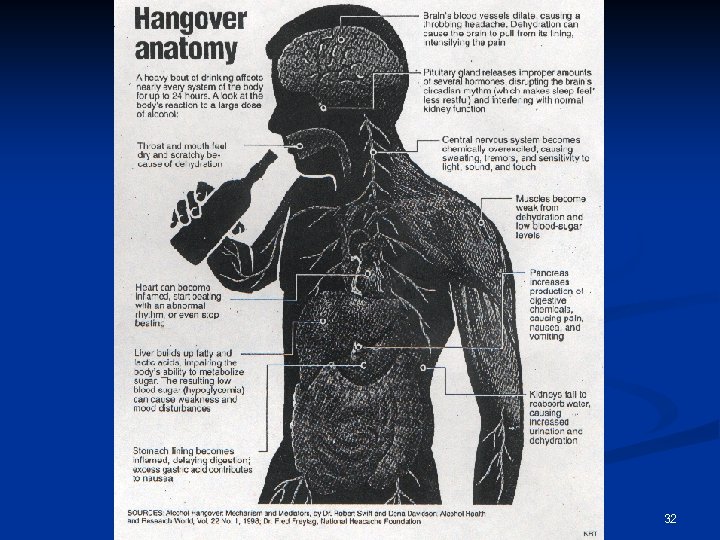 32
32
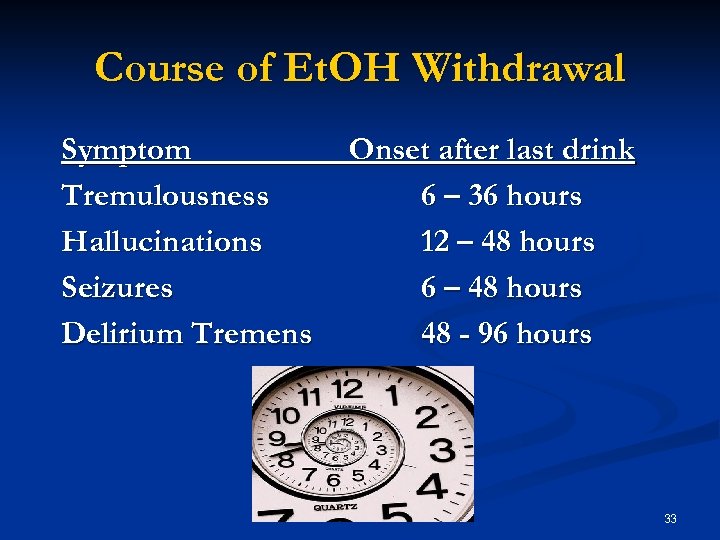 Course of Et. OH Withdrawal Symptom Tremulousness Hallucinations Seizures Delirium Tremens Onset after last drink 6 – 36 hours 12 – 48 hours 6 – 48 hours 48 - 96 hours 33
Course of Et. OH Withdrawal Symptom Tremulousness Hallucinations Seizures Delirium Tremens Onset after last drink 6 – 36 hours 12 – 48 hours 6 – 48 hours 48 - 96 hours 33
 Tremulousness occurs within 6 – 36 hours 2 ndary to autonomic hyperactivity n Symptoms n n n n Tremor Anxiety Agitation Insomnia Anorexia Nausea Palpitations n Signs n n n Tachycardia Hypertension Hyper-reflexia Hyperthermia Diaphoresis 34
Tremulousness occurs within 6 – 36 hours 2 ndary to autonomic hyperactivity n Symptoms n n n n Tremor Anxiety Agitation Insomnia Anorexia Nausea Palpitations n Signs n n n Tachycardia Hypertension Hyper-reflexia Hyperthermia Diaphoresis 34
 Hallucinations n n n Occurs within 12 – 48 hours of last drink 3 – 10% of cases develop hallucinations Duration is variable Usually visual (e. g. , pink elephants) Occasionally auditory, tactile, or olfactory Et. OH Hallucinosis: reality testing is intact 35
Hallucinations n n n Occurs within 12 – 48 hours of last drink 3 – 10% of cases develop hallucinations Duration is variable Usually visual (e. g. , pink elephants) Occasionally auditory, tactile, or olfactory Et. OH Hallucinosis: reality testing is intact 35
 Seizures n n n n Occur within 6 – 48 hours of last drink 11 -35% of patients develop seizures in hospital setting Risk correlates with duration Et. OH use Manifests as grand mal tonic-clonic activity Always rule out other causes 40% are single episodes 30% of untreated patients go on to develop delirium tremens 36
Seizures n n n n Occur within 6 – 48 hours of last drink 11 -35% of patients develop seizures in hospital setting Risk correlates with duration Et. OH use Manifests as grand mal tonic-clonic activity Always rule out other causes 40% are single episodes 30% of untreated patients go on to develop delirium tremens 36
 Seizures n n Et. OH is an independent risk factor for seizures Retrospective study of 308 patients in a city hospital with new onset of seizures during Et. OH withdrawal n Et. OH (gm/day) 51 – 100 101 – 200 201 – 300 n 10 gm = 1 beer n n n Risk 3 x 8 x 20 x Stephen KC. “Alcohol Consumption & Withdrawal in New-Onset Seizures. ” NEJM, 1988 37
Seizures n n Et. OH is an independent risk factor for seizures Retrospective study of 308 patients in a city hospital with new onset of seizures during Et. OH withdrawal n Et. OH (gm/day) 51 – 100 101 – 200 201 – 300 n 10 gm = 1 beer n n n Risk 3 x 8 x 20 x Stephen KC. “Alcohol Consumption & Withdrawal in New-Onset Seizures. ” NEJM, 1988 37
 Delirium Tremens n n n Begins 3 to 5 days after last drink Occurs in less than 5% of withdrawal patients Not always predictable or preventable Usually lasts 2 -3 days, but can last up to 30 days Delirium can occur with/without “tremens” Risk factors n n n Acute concurrent medical illness History of seizures or delirium tremens Heavier & longer Et. OH history Age > 60 Elevated BAL on admission (greater than 300 mg/dl) 38
Delirium Tremens n n n Begins 3 to 5 days after last drink Occurs in less than 5% of withdrawal patients Not always predictable or preventable Usually lasts 2 -3 days, but can last up to 30 days Delirium can occur with/without “tremens” Risk factors n n n Acute concurrent medical illness History of seizures or delirium tremens Heavier & longer Et. OH history Age > 60 Elevated BAL on admission (greater than 300 mg/dl) 38
 Delirium Tremens n Symptoms n n n Confusion & disorientation Hallucinations Hyper-responsiveness n Signs n n n Hypertension Tachycardia Fever 39
Delirium Tremens n Symptoms n n n Confusion & disorientation Hallucinations Hyper-responsiveness n Signs n n n Hypertension Tachycardia Fever 39
 Delirium Tremens Mortality n Mortality: n n n without treatment = 20% with treatment = 2 – 10% Temperature > 104 45% mortality Seizures & DTs 24% mortality Cause of death n n Pneumonia Liver disease Hypotension Trauma 40
Delirium Tremens Mortality n Mortality: n n n without treatment = 20% with treatment = 2 – 10% Temperature > 104 45% mortality Seizures & DTs 24% mortality Cause of death n n Pneumonia Liver disease Hypotension Trauma 40
 Clinical Assessment n History n n n Presentation Intake: amount, type, time of last drink, etc. ? Hx of complicated withdrawal? Use of other substances? Medical & psychiatric history Mental Status Examination n n Cognitive impairment? Hallucinations? Impulsivity? Suicide/homicide risk? 41
Clinical Assessment n History n n n Presentation Intake: amount, type, time of last drink, etc. ? Hx of complicated withdrawal? Use of other substances? Medical & psychiatric history Mental Status Examination n n Cognitive impairment? Hallucinations? Impulsivity? Suicide/homicide risk? 41
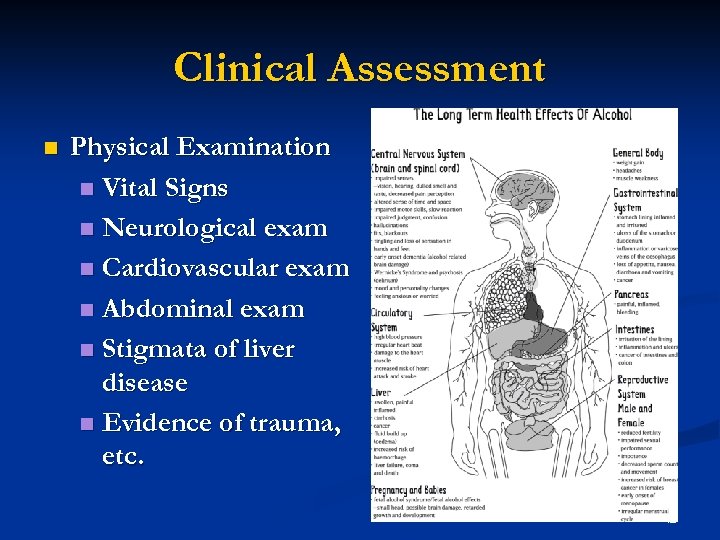 Clinical Assessment n Physical Examination n Vital Signs n Neurological exam n Cardiovascular exam n Abdominal exam n Stigmata of liver disease n Evidence of trauma, etc. 42
Clinical Assessment n Physical Examination n Vital Signs n Neurological exam n Cardiovascular exam n Abdominal exam n Stigmata of liver disease n Evidence of trauma, etc. 42
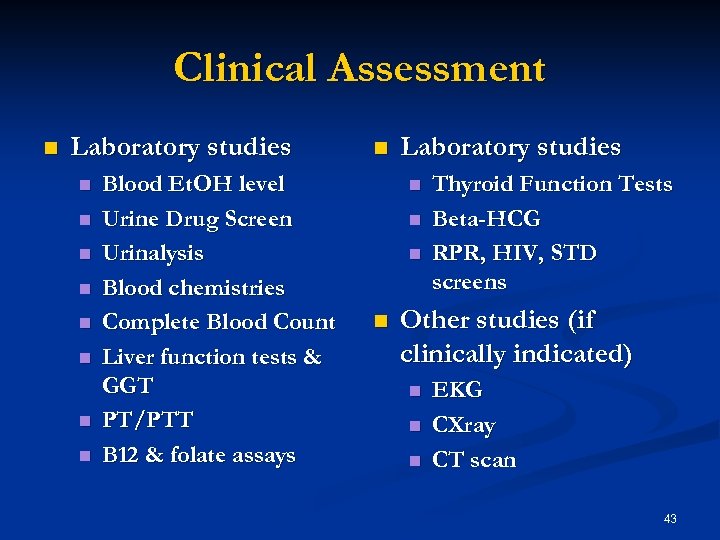 Clinical Assessment n Laboratory studies n n n n Blood Et. OH level Urine Drug Screen Urinalysis Blood chemistries Complete Blood Count Liver function tests & GGT PT/PTT B 12 & folate assays n Laboratory studies n n Thyroid Function Tests Beta-HCG RPR, HIV, STD screens Other studies (if clinically indicated) n n n EKG CXray CT scan 43
Clinical Assessment n Laboratory studies n n n n Blood Et. OH level Urine Drug Screen Urinalysis Blood chemistries Complete Blood Count Liver function tests & GGT PT/PTT B 12 & folate assays n Laboratory studies n n Thyroid Function Tests Beta-HCG RPR, HIV, STD screens Other studies (if clinically indicated) n n n EKG CXray CT scan 43
 Et. OH Withdrawal Differential Diagnosis n Acute stimulant intoxication n cocaine, methamphetamine, caffeine Sepsis n Thyrotoxicosis n Heat stroke n Hypoglycemia n Intracranial processes (e. g. , trauma, CVA) n Encephalitis/encephalopathy n 44
Et. OH Withdrawal Differential Diagnosis n Acute stimulant intoxication n cocaine, methamphetamine, caffeine Sepsis n Thyrotoxicosis n Heat stroke n Hypoglycemia n Intracranial processes (e. g. , trauma, CVA) n Encephalitis/encephalopathy n 44
 Et. OH Withdrawal Treatment Setting Severity of withdrawal dictates level of care: Social Detoxification: 24 hour care, nonhospital/residential setting without professional medical staff n Medically Supported Detoxification: 24 hour care, non-hospital/residential setting with profession medical staff n n Medical Detoxification: 24 -hour care, hospital setting 45
Et. OH Withdrawal Treatment Setting Severity of withdrawal dictates level of care: Social Detoxification: 24 hour care, nonhospital/residential setting without professional medical staff n Medically Supported Detoxification: 24 hour care, non-hospital/residential setting with profession medical staff n n Medical Detoxification: 24 -hour care, hospital setting 45
 Treatment Setting ASAM Criteria n n n Level I-D: Ambulatory Detoxification Without Extended Onsite Monitoring Level II-D: Ambulatory Detoxification With Extended Onsite Monitoring Level II. 2 -D: Clinically Managed Residential Detoxification Level III. 7 -D: Medically Monitored Inpatient Detoxification (hospital ward) Level IV-D: Medically Managed Intensive Inpatient Detoxification (ICU) 46
Treatment Setting ASAM Criteria n n n Level I-D: Ambulatory Detoxification Without Extended Onsite Monitoring Level II-D: Ambulatory Detoxification With Extended Onsite Monitoring Level II. 2 -D: Clinically Managed Residential Detoxification Level III. 7 -D: Medically Monitored Inpatient Detoxification (hospital ward) Level IV-D: Medically Managed Intensive Inpatient Detoxification (ICU) 46
 Indications for Admission (Level III) n n n n Hx of severe withdrawal symptoms Hx of withdrawal seizures or delirium tremens Hx of heavy prolonged Et. OH use with a high degree of tolerance Abuse of multiple substances Concomitant psychiatric or medical illness Pregnancy Lack of reliable support network 47
Indications for Admission (Level III) n n n n Hx of severe withdrawal symptoms Hx of withdrawal seizures or delirium tremens Hx of heavy prolonged Et. OH use with a high degree of tolerance Abuse of multiple substances Concomitant psychiatric or medical illness Pregnancy Lack of reliable support network 47
 Who goes to the ICU? . . . (Level IV) Age > 65 n Significant cardiac disease n Hemodynamic instability n Marked acid-base disturbances n Severe respiratory disease n Serious infection n Active delirium tremens n 48
Who goes to the ICU? . . . (Level IV) Age > 65 n Significant cardiac disease n Hemodynamic instability n Marked acid-base disturbances n Severe respiratory disease n Serious infection n Active delirium tremens n 48
 Who goes to the ICU? . . . (Level IV) Serious GI pathology n Temp > 103 F n Rhabdomyolysis n Acute renal failure n Hx of recurrent withdrawal seizures n Hx of delirium tremens n IV benzodiazepine drip n (Ativan 12+ mg/day) 49
Who goes to the ICU? . . . (Level IV) Serious GI pathology n Temp > 103 F n Rhabdomyolysis n Acute renal failure n Hx of recurrent withdrawal seizures n Hx of delirium tremens n IV benzodiazepine drip n (Ativan 12+ mg/day) 49
 Treatment Strategy Reduce symptoms n Prevent seizures n Prevent delirium tremens n Prevent &/or manage medical complications & comorbidities n 50
Treatment Strategy Reduce symptoms n Prevent seizures n Prevent delirium tremens n Prevent &/or manage medical complications & comorbidities n 50
 Supportive Care Ensure ABCs!. . . n Secure patient in safe environment n Provide IV hydration n Correct electrolyte imbalances n Provide nutritional support n 51
Supportive Care Ensure ABCs!. . . n Secure patient in safe environment n Provide IV hydration n Correct electrolyte imbalances n Provide nutritional support n 51
 Supportive Care Nursing care: reassurance, orientation n Monitor for signs & symptoms of withdrawal n Involve Psychiatrist on Duty (Pso. D) if patient c/o suicidal/ homicidal ideation &/or psychotic symptoms n 52
Supportive Care Nursing care: reassurance, orientation n Monitor for signs & symptoms of withdrawal n Involve Psychiatrist on Duty (Pso. D) if patient c/o suicidal/ homicidal ideation &/or psychotic symptoms n 52
 Role of Pharmacotherapy Stabilize psychological or physiological withdrawal symptoms n Manage medical emergencies n Remediate non-life threatening, relapsetriggering symptoms n Stabilize co-morbid conditions n 53
Role of Pharmacotherapy Stabilize psychological or physiological withdrawal symptoms n Manage medical emergencies n Remediate non-life threatening, relapsetriggering symptoms n Stabilize co-morbid conditions n 53
 Thiamine & Multivitamins n n n 30 -80% of patients are deficient Thiamine does not reduce risk of seizures or delirium tremens Thiamine does reduce risk of Wernicke’s encephalopathy Give thiamine 50 – 100 mg IV or IM x 1, then po qd Administer thiamine before glucose Add MV 1 tab po qd 54
Thiamine & Multivitamins n n n 30 -80% of patients are deficient Thiamine does not reduce risk of seizures or delirium tremens Thiamine does reduce risk of Wernicke’s encephalopathy Give thiamine 50 – 100 mg IV or IM x 1, then po qd Administer thiamine before glucose Add MV 1 tab po qd 54
 Benzodiazepines n Ideal for management of Et. OH withdrawal symptoms Cross-tolerance with Et. OH n Fairly wide therapeutic window (compared to barbiturates) n Short- vs. long-acting n Liver disease limits use to short acting benzos n 55
Benzodiazepines n Ideal for management of Et. OH withdrawal symptoms Cross-tolerance with Et. OH n Fairly wide therapeutic window (compared to barbiturates) n Short- vs. long-acting n Liver disease limits use to short acting benzos n 55
 Benzodiazepines Short-acting n n Oxazepam & Lorazepam Advantages n n They can be administered IM or IV (in monitored settings) They have no significant active metabolites They are metabolized & excreted principally through kidneys (& do not jeopardize already-damaged liver) Disadvantages n They need to be administered more frequently. 56
Benzodiazepines Short-acting n n Oxazepam & Lorazepam Advantages n n They can be administered IM or IV (in monitored settings) They have no significant active metabolites They are metabolized & excreted principally through kidneys (& do not jeopardize already-damaged liver) Disadvantages n They need to be administered more frequently. 56
 Other Medications n Beta-blockers & Clonidine Reduce autonomic hyperarousal (tachycardia, hypertension) n May reduce total dosage of benzos & result in less sedation n Do not reduce risk of seizures or delirium tremens n 57
Other Medications n Beta-blockers & Clonidine Reduce autonomic hyperarousal (tachycardia, hypertension) n May reduce total dosage of benzos & result in less sedation n Do not reduce risk of seizures or delirium tremens n 57
 Other Medications n Carbamazepine Reduces risk of seizure activity n Does little for autonomic hyper-arousal n Requires monitoring of CBC, LFTs, & serum levels n Risks include liver & bone marrow toxicity n 58
Other Medications n Carbamazepine Reduces risk of seizure activity n Does little for autonomic hyper-arousal n Requires monitoring of CBC, LFTs, & serum levels n Risks include liver & bone marrow toxicity n 58
 Other Medications n Antipsychotic agents Can be used for management of agitation, aggression, & psychotic symptoms n CAUTION: Can also lower seizure threshold n n Bottom line: other medications are best used as adjuncts instead of substitutes for benzos 59
Other Medications n Antipsychotic agents Can be used for management of agitation, aggression, & psychotic symptoms n CAUTION: Can also lower seizure threshold n n Bottom line: other medications are best used as adjuncts instead of substitutes for benzos 59
 Play file: Roughmorning 2 60
Play file: Roughmorning 2 60
 Routine vs. Symptom-driven Protocols n n Study: 100 VA patients in Et. OH withdrawal Outcomes n n n Treatment time = 68 hrs vs. 9 hrs. Total dose Librium = 425 mg vs. 100 mg Advantages n n Reduced hospital length of stay Reduced total dosage of medication Reduced cost of care Less sedation 61
Routine vs. Symptom-driven Protocols n n Study: 100 VA patients in Et. OH withdrawal Outcomes n n n Treatment time = 68 hrs vs. 9 hrs. Total dose Librium = 425 mg vs. 100 mg Advantages n n Reduced hospital length of stay Reduced total dosage of medication Reduced cost of care Less sedation 61
 Symptom-driven Protocols n Clinical Institute Withdrawal Assessment for Alcohol Scale (CIWA) 10 -item clinical rating system for Et. OH withdrawal assessment n Patient is assessed q 4 hours (while awake) n CIWA can be administered in under 2 minutes n Each item (but one) is scored on a scale of 0 – 7 n Maximum score of 67 points n Medicate for scores > 8 -10 n Sullivan, JT. British Journal of Addiction, 1989; 84: 1353 -7 62
Symptom-driven Protocols n Clinical Institute Withdrawal Assessment for Alcohol Scale (CIWA) 10 -item clinical rating system for Et. OH withdrawal assessment n Patient is assessed q 4 hours (while awake) n CIWA can be administered in under 2 minutes n Each item (but one) is scored on a scale of 0 – 7 n Maximum score of 67 points n Medicate for scores > 8 -10 n Sullivan, JT. British Journal of Addiction, 1989; 84: 1353 -7 62
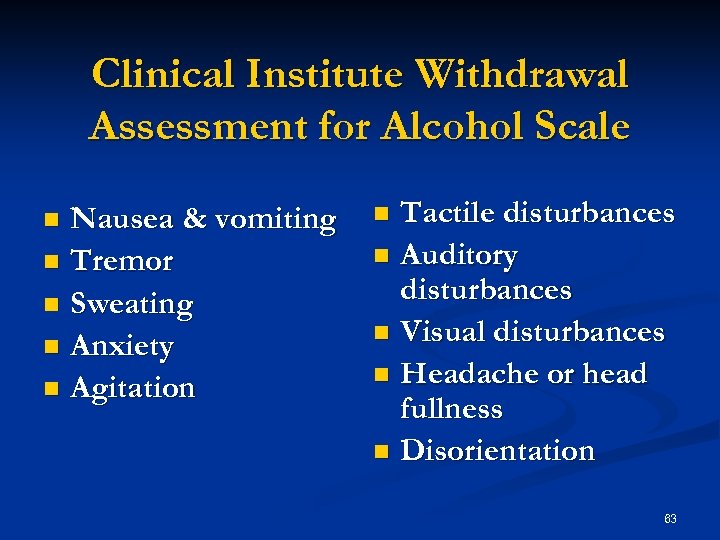 Clinical Institute Withdrawal Assessment for Alcohol Scale Nausea & vomiting n Tremor n Sweating n Anxiety n Agitation n Tactile disturbances n Auditory disturbances n Visual disturbances n Headache or head fullness n Disorientation n 63
Clinical Institute Withdrawal Assessment for Alcohol Scale Nausea & vomiting n Tremor n Sweating n Anxiety n Agitation n Tactile disturbances n Auditory disturbances n Visual disturbances n Headache or head fullness n Disorientation n 63
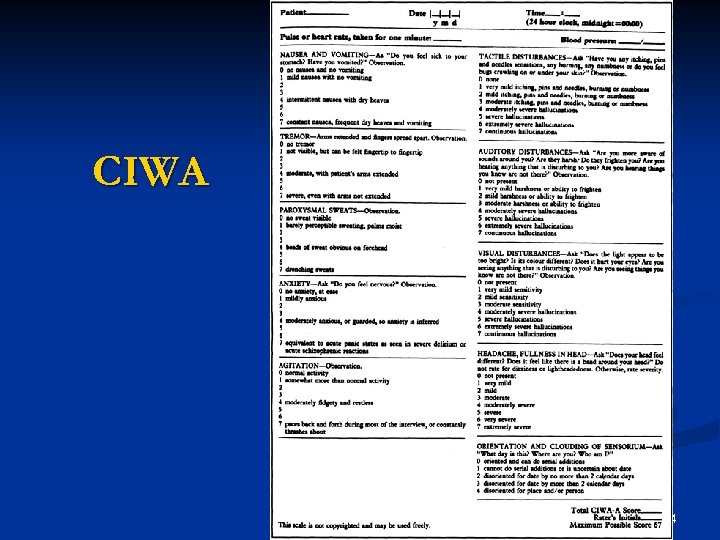 CIWA 64
CIWA 64
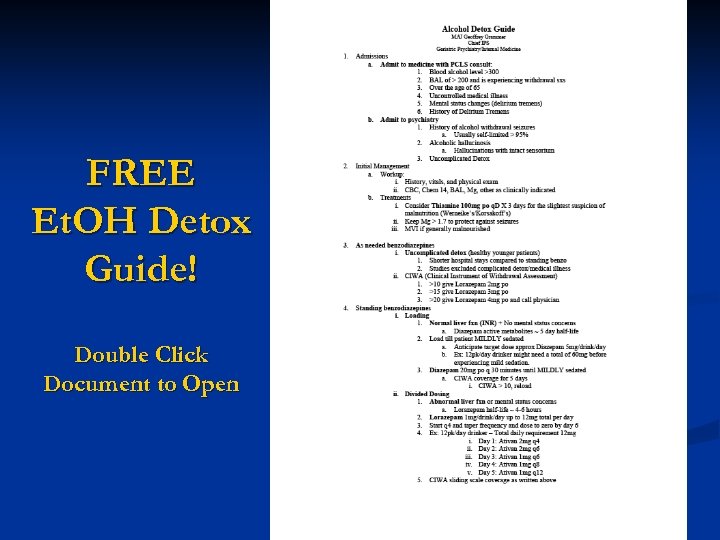 FREE Et. OH Detox Guide! Double Click Document to Open 65
FREE Et. OH Detox Guide! Double Click Document to Open 65
 Discharge Criteria n n n Neurologically stable for last 24 hrs No withdrawal symptoms; CIWA scores < 10 for last 24 hrs Vital signs are stable & within normal limits No c/o of suicidal/homicidal thoughts or behavior Detox protocol/taper must be completed; seizures are controlled Enrollment in rehab program, ideally within 24 hrs of discharge 66
Discharge Criteria n n n Neurologically stable for last 24 hrs No withdrawal symptoms; CIWA scores < 10 for last 24 hrs Vital signs are stable & within normal limits No c/o of suicidal/homicidal thoughts or behavior Detox protocol/taper must be completed; seizures are controlled Enrollment in rehab program, ideally within 24 hrs of discharge 66
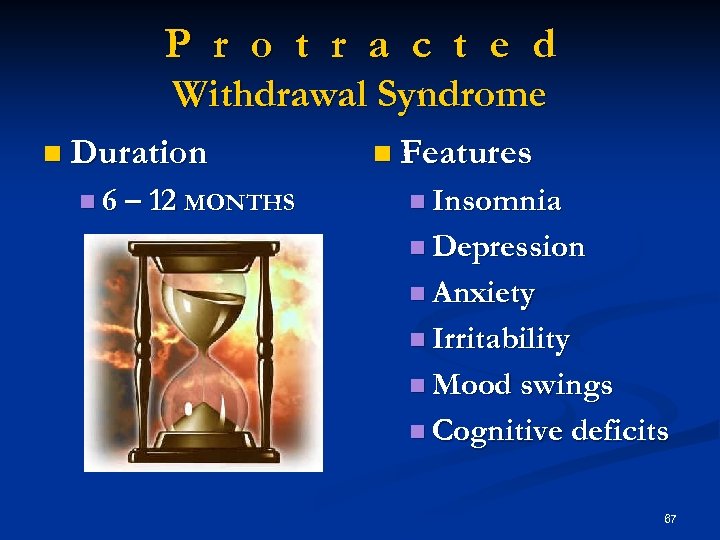 P r o t r a c t e d Withdrawal Syndrome n Duration n 6 – 12 MONTHS n Features n Insomnia n Depression n Anxiety n Irritability n Mood swings n Cognitive deficits 67
P r o t r a c t e d Withdrawal Syndrome n Duration n 6 – 12 MONTHS n Features n Insomnia n Depression n Anxiety n Irritability n Mood swings n Cognitive deficits 67
 TAMC Process Action Team Et. OH Withdrawal Protocols n Membership Psychiatry n Internal Medicine n Family Medicine n Emergency Medicine n n Process Literature review n Discussion & collaboration n 68
TAMC Process Action Team Et. OH Withdrawal Protocols n Membership Psychiatry n Internal Medicine n Family Medicine n Emergency Medicine n n Process Literature review n Discussion & collaboration n 68
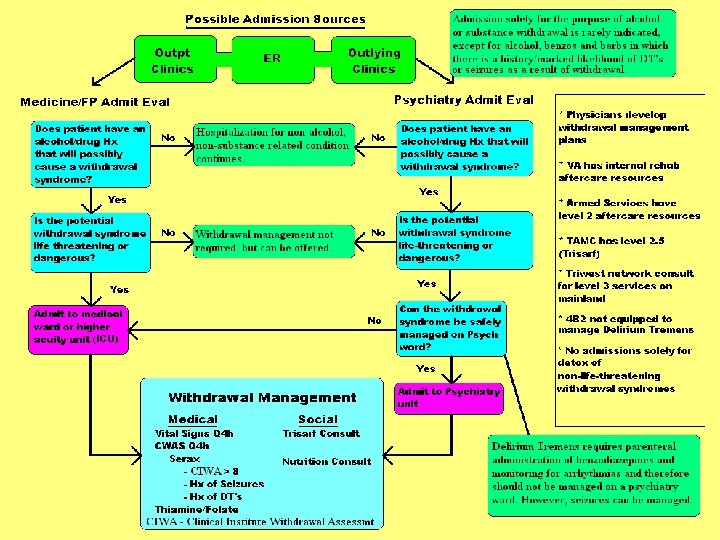 69
69
 ? 70
? 70
 71
71
 Contact Information John J. Stasinos, M. D. LTC(P), MC, USA Chief, Chemical Addictions Treatment Services, TAMC Director, Addiction Psychiatry Fellowship Program (808) 433 -6566 john. j. stasinos@us. army. mil 72
Contact Information John J. Stasinos, M. D. LTC(P), MC, USA Chief, Chemical Addictions Treatment Services, TAMC Director, Addiction Psychiatry Fellowship Program (808) 433 -6566 john. j. stasinos@us. army. mil 72


