2f7806992590ca8ab449eb7a328168b6.ppt
- Количество слайдов: 28
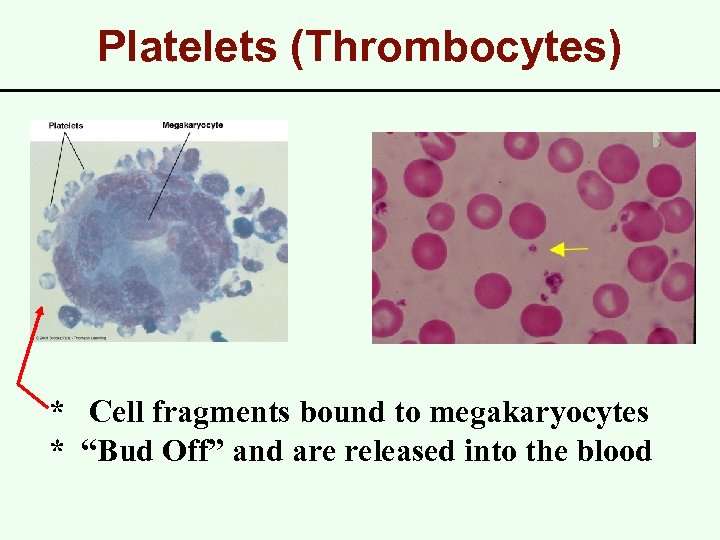
Platelets (Thrombocytes) * Cell fragments bound to megakaryocytes * “Bud Off” and are released into the blood
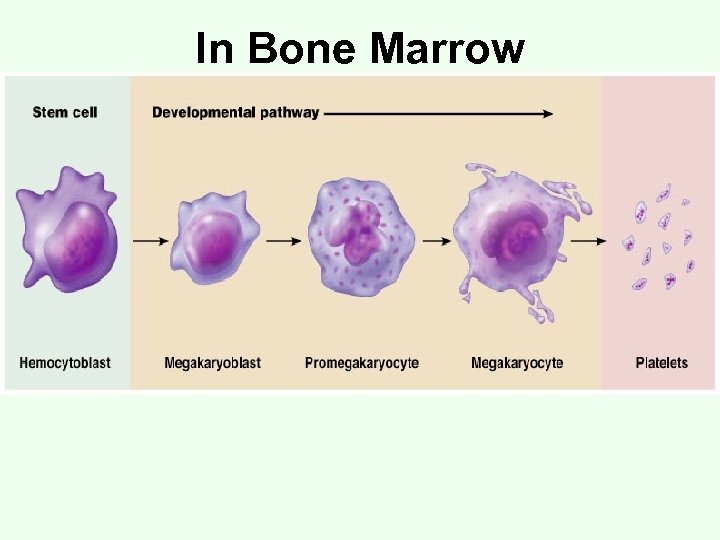
In Bone Marrow
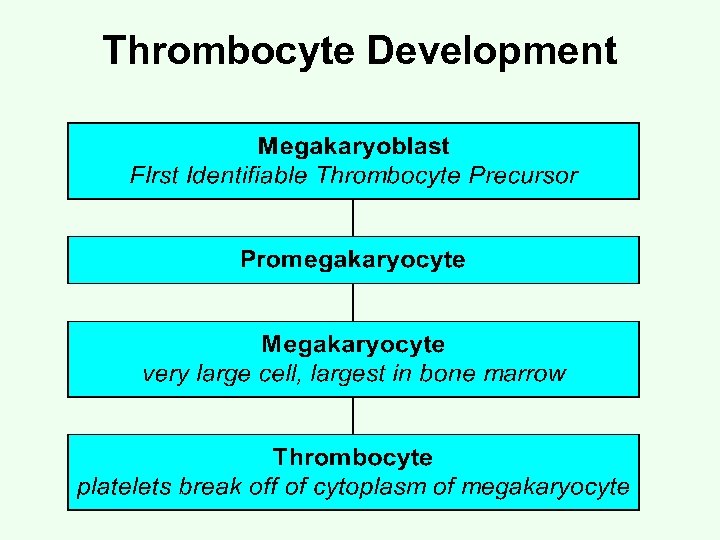
Thrombocyte Development
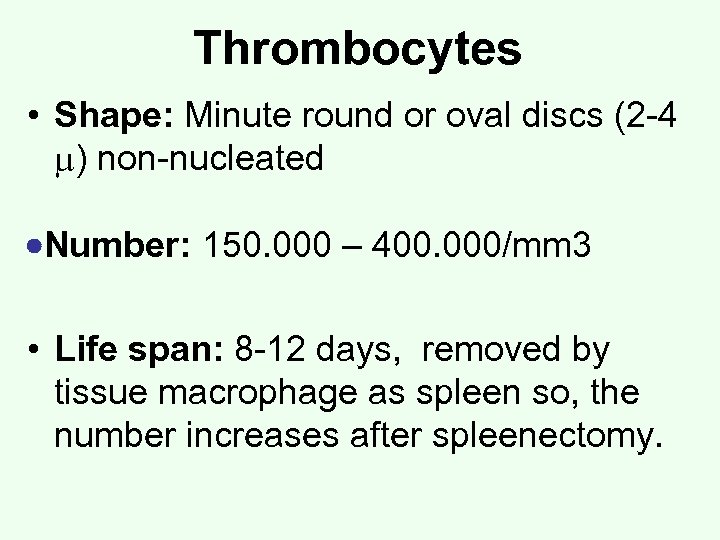
Thrombocytes • Shape: Minute round or oval discs (2 -4 ) non-nucleated Number: 150. 000 – 400. 000/mm 3 • Life span: 8 -12 days, removed by tissue macrophage as spleen so, the number increases after spleenectomy.
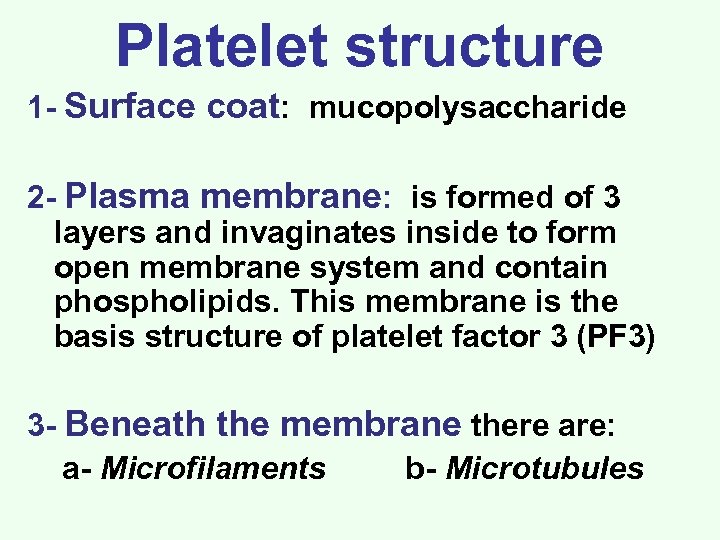
Platelet structure 1 - Surface coat: mucopolysaccharide 2 - Plasma membrane: is formed of 3 layers and invaginates inside to form open membrane system and contain phospholipids. This membrane is the basis structure of platelet factor 3 (PF 3) 3 - Beneath the membrane there are: a- Microfilaments b- Microtubules
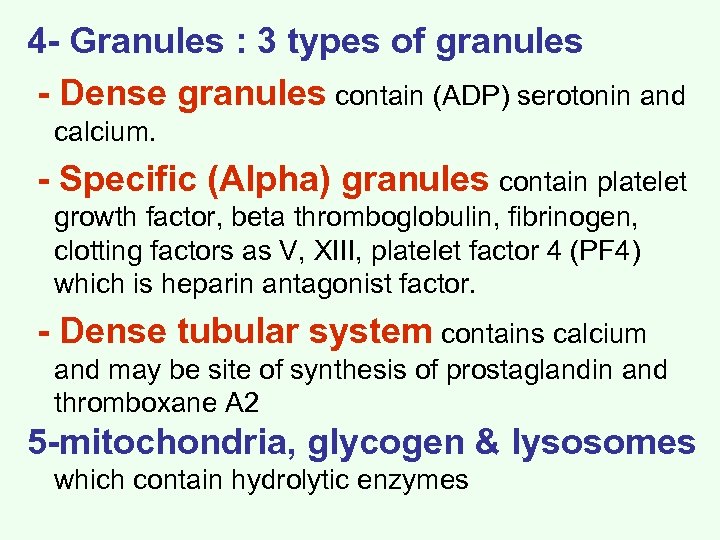
4 - Granules : 3 types of granules - Dense granules contain (ADP) serotonin and calcium. - Specific (Alpha) granules contain platelet growth factor, beta thromboglobulin, fibrinogen, clotting factors as V, XIII, platelet factor 4 (PF 4) which is heparin antagonist factor. - Dense tubular system contains calcium and may be site of synthesis of prostaglandin and thromboxane A 2 5 -mitochondria, glycogen & lysosomes which contain hydrolytic enzymes
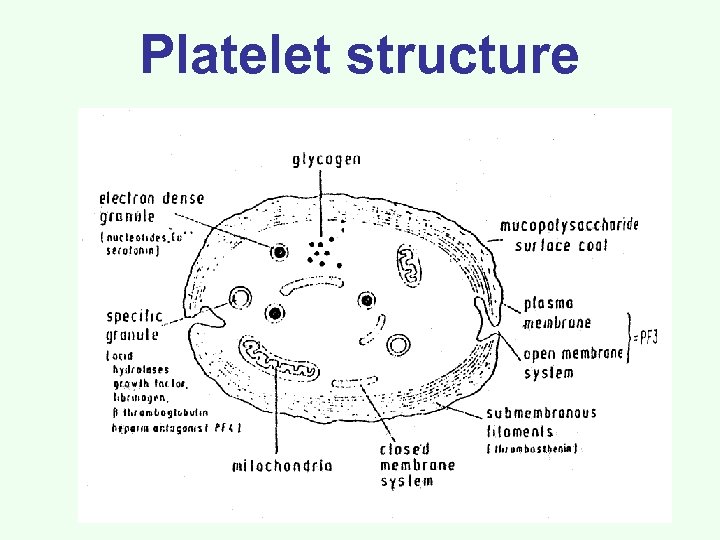
Platelet structure
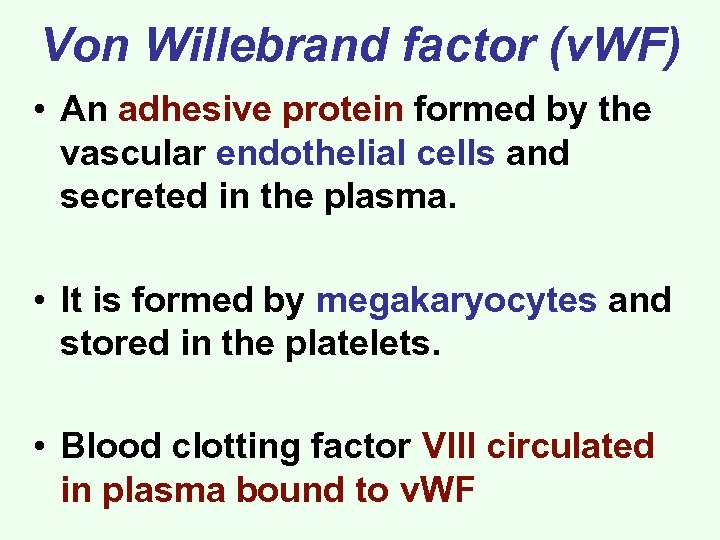
Von Willebrand factor (v. WF) • An adhesive protein formed by the vascular endothelial cells and secreted in the plasma. • It is formed by megakaryocytes and stored in the platelets. • Blood clotting factor VIII circulated in plasma bound to v. WF
Hemostasis It is the stoppage of bleeding in case of small vascular injury. It depends on: the vascular wall, platelets and the clotting factors
![[I] Vascular factor (local vascular spasm) • Causes a- Direct effect of serotonin and [I] Vascular factor (local vascular spasm) • Causes a- Direct effect of serotonin and](https://present5.com/presentation/2f7806992590ca8ab449eb7a328168b6/image-10.jpg)
[I] Vascular factor (local vascular spasm) • Causes a- Direct effect of serotonin and thromboxane A 2 released from platelets V. C. b- Injury of endothelium endothelial derived relaxing substance V. C. c- Pain nervous V. C. reflex
![[II] Formation of platelet plug 1) Platelet adhesion: Following blood vessel injury, platelets adhere [II] Formation of platelet plug 1) Platelet adhesion: Following blood vessel injury, platelets adhere](https://present5.com/presentation/2f7806992590ca8ab449eb7a328168b6/image-11.jpg)
[II] Formation of platelet plug 1) Platelet adhesion: Following blood vessel injury, platelets adhere to the exposed subendothelial collagen. Adhesion depends on a. A surface membrane glycoportein b. Von-Willebrand factor
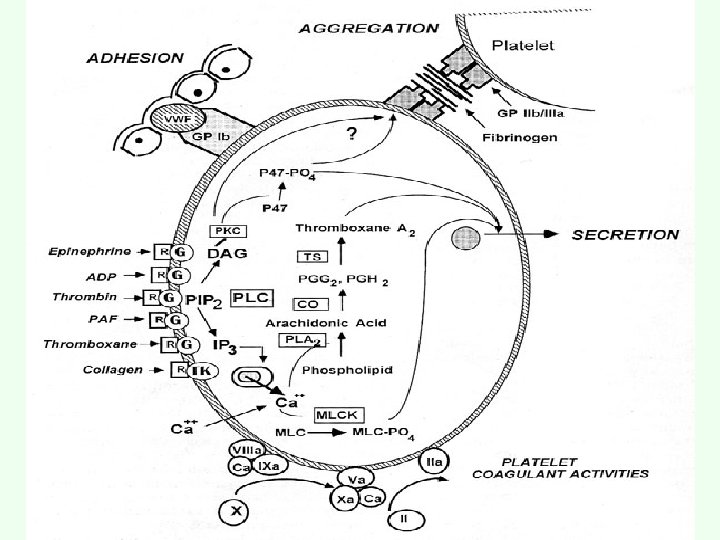
2) Platelets release: a- Release of platelets contents such as ADP, serotonin, VWF, fibrinogen and platelet factor b- Platelets enzymes form thromboxane A 2 release of platelets contents. 3) Platelet aggregation Released ADP and thromboxane. A 2 platelet aggregation further release more aggregation and so on.
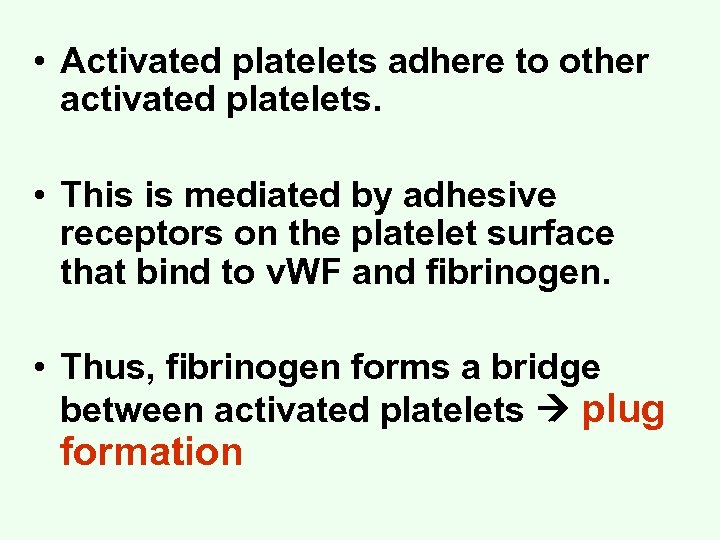
• Activated platelets adhere to other activated platelets. • This is mediated by adhesive receptors on the platelet surface that bind to v. WF and fibrinogen. • Thus, fibrinogen forms a bridge between activated platelets plug formation
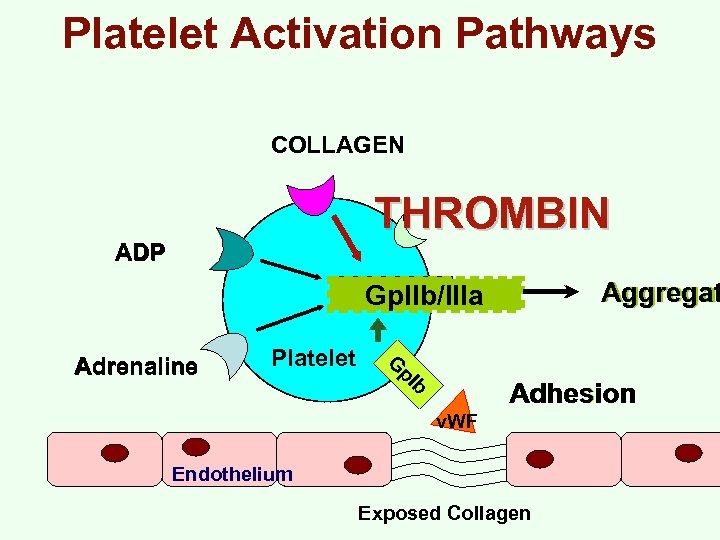
Platelet Activation Pathways COLLAGEN THROMBIN ADP Aggregat Gp. IIb/IIIa Platelet G p. I Adrenaline b Adhesion v. WF Endothelium Exposed Collagen
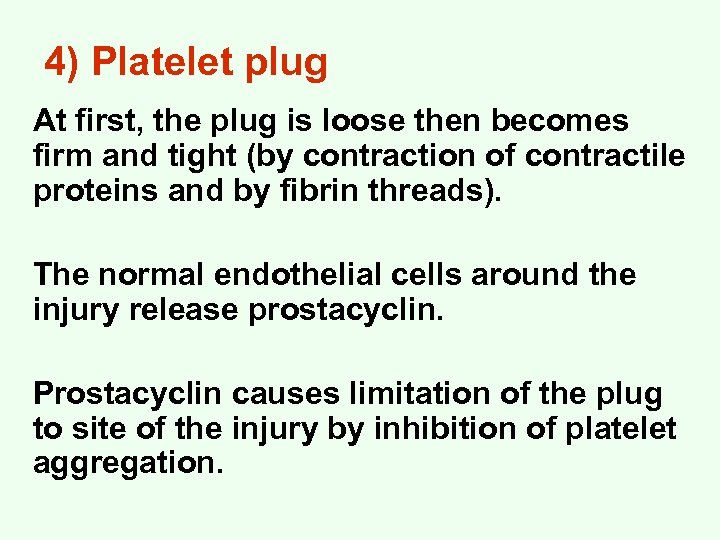
4) Platelet plug At first, the plug is loose then becomes firm and tight (by contraction of contractile proteins and by fibrin threads). The normal endothelial cells around the injury release prostacyclin. Prostacyclin causes limitation of the plug to site of the injury by inhibition of platelet aggregation.
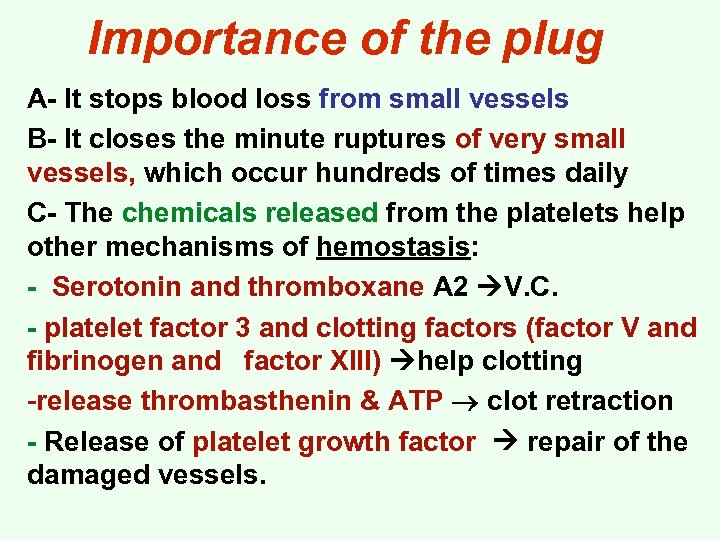
Importance of the plug A- It stops blood loss from small vessels B- It closes the minute ruptures of very small vessels, which occur hundreds of times daily C- The chemicals released from the platelets help other mechanisms of hemostasis: - Serotonin and thromboxane A 2 V. C. - platelet factor 3 and clotting factors (factor V and fibrinogen and factor XIII) help clotting -release thrombasthenin & ATP clot retraction - Release of platelet growth factor repair of the damaged vessels.
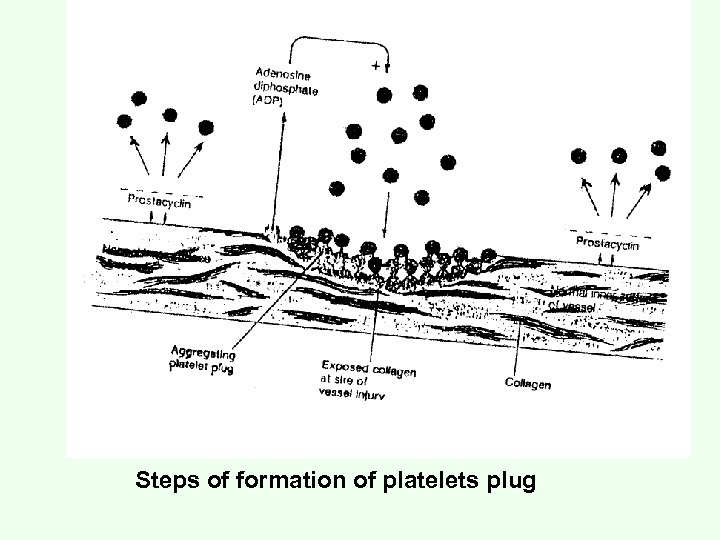
Steps of formation of platelets plug
![[III] Blood coagulation It needs the following clotting factors I (Fibrinogen) III (thromboplastin) tissue [III] Blood coagulation It needs the following clotting factors I (Fibrinogen) III (thromboplastin) tissue](https://present5.com/presentation/2f7806992590ca8ab449eb7a328168b6/image-19.jpg)
[III] Blood coagulation It needs the following clotting factors I (Fibrinogen) III (thromboplastin) tissue factor V (Labile factor) VIII (anti-haemophilia globulin) X (Stuart prower factor) XII (Hageman factor) Platelet factor-3 (phospholipid) II (prothrombin) IV (Calcium) VII (stable factor) IX (christmas factor) XI (plasma thromboplastin antecadent) XIII (fibrin stabilizing factor) v. WF High molecular weight kininogen and prekallikrein.
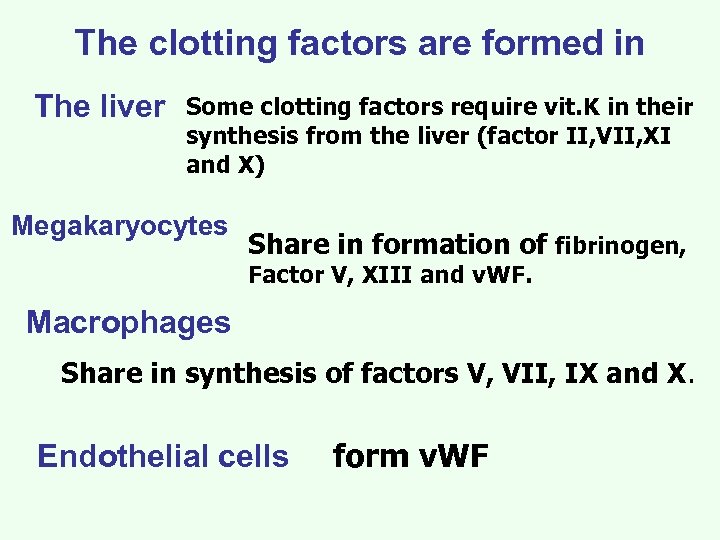
The clotting factors are formed in The liver Some clotting factors require vit. K in their synthesis from the liver (factor II, VII, XI and X) Megakaryocytes Share in formation of fibrinogen, Factor V, XIII and v. WF. Macrophages Share in synthesis of factors V, VII, IX and X. Endothelial cells form v. WF
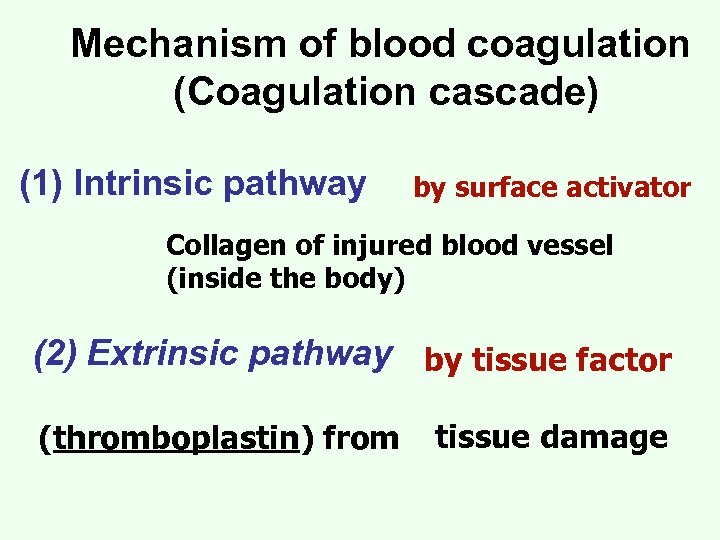
Mechanism of blood coagulation (Coagulation cascade) (1) Intrinsic pathway by surface activator Collagen of injured blood vessel (inside the body) (2) Extrinsic pathway by tissue factor (thromboplastin) from tissue damage
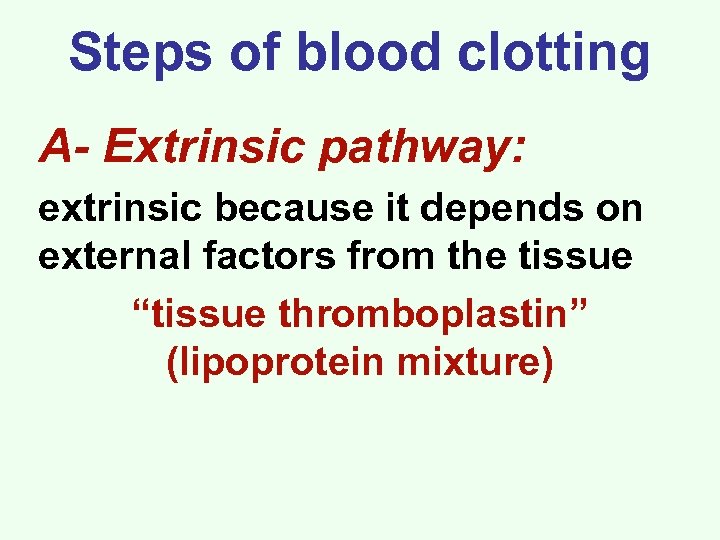
Steps of blood clotting A- Extrinsic pathway: extrinsic because it depends on external factors from the tissue “tissue thromboplastin” (lipoprotein mixture)
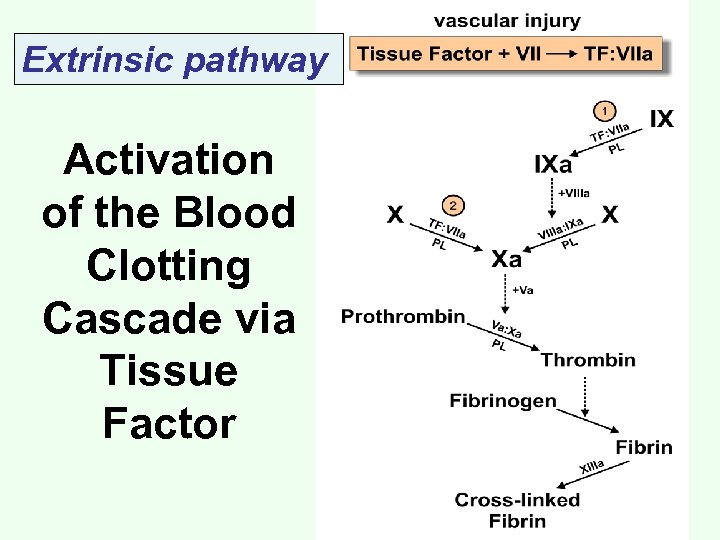
Extrinsic pathway Activation of the Blood Clotting Cascade via Tissue Factor
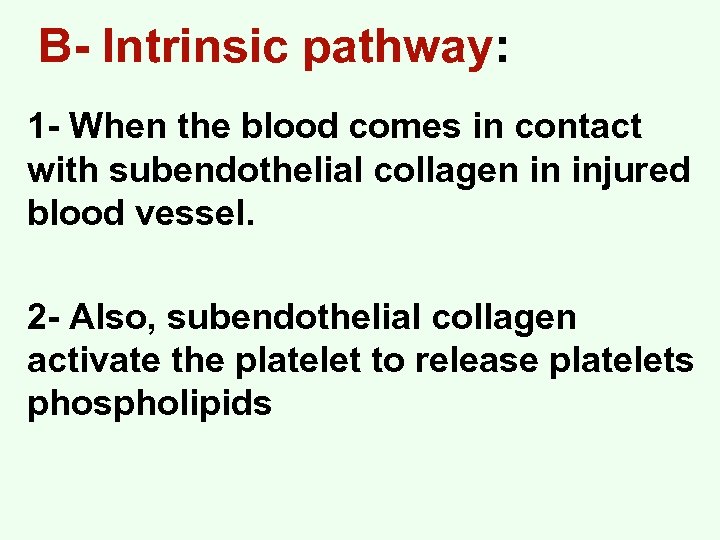
B- Intrinsic pathway: 1 - When the blood comes in contact with subendothelial collagen in injured blood vessel. 2 - Also, subendothelial collagen activate the platelet to release platelets phospholipids
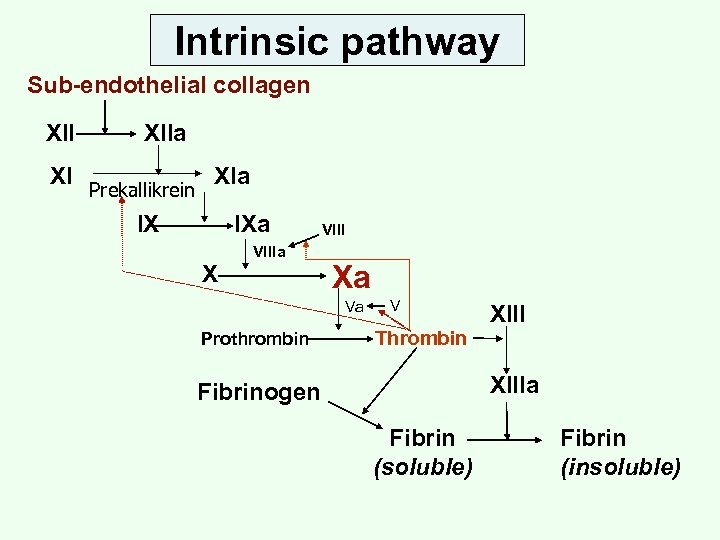
Intrinsic pathway Sub-endothelial collagen XII XI XIIa Prekallikrein XIa IX IXa VIIIa X VIII Xa Va Prothrombin V Thrombin XIIIa Fibrinogen Fibrin (soluble) Fibrin (insoluble)
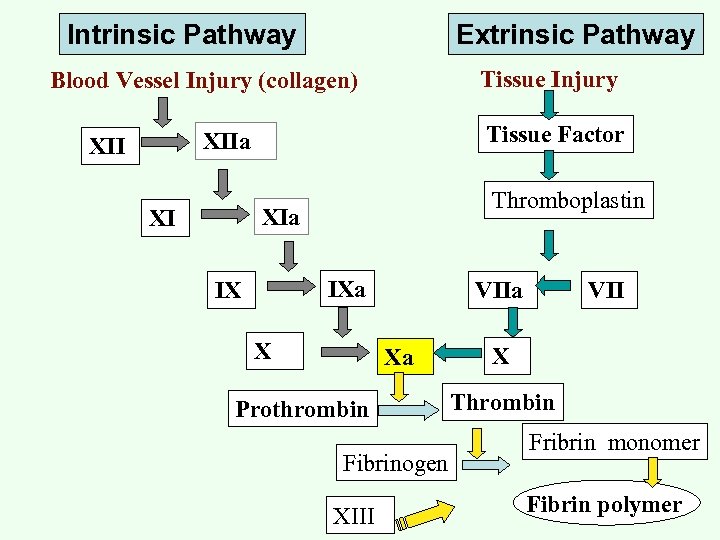
Intrinsic Pathway Extrinsic Pathway Tissue Injury Blood Vessel Injury (collagen) Tissue Factor XIIa XII Thromboplastin XIa XI IXa IX X VIIa Xa Prothrombin Fibrinogen XIII VII X Thrombin Fribrin monomer Fibrin polymer
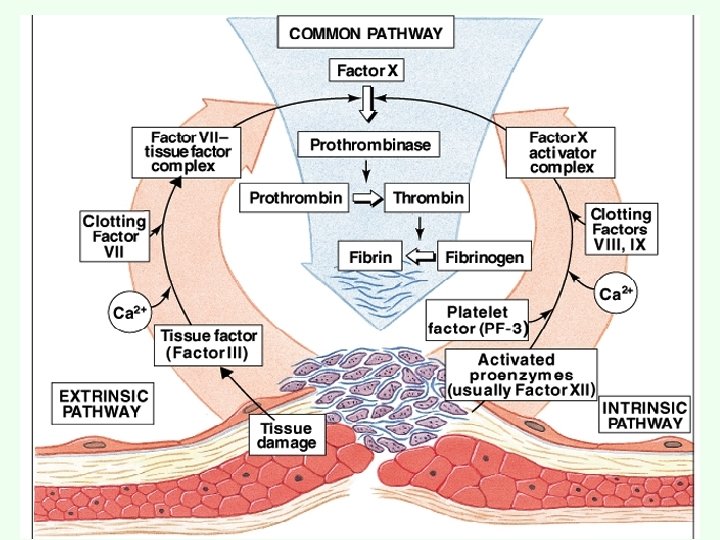
Interaction between the extrinsic and intrinsic mechanisms 1 - Both pathways begins at the same time but the extrinsic mechanism takes 15 -20 seconds whereas the extrinsic mechanism takes 2 -10 minutes. 2 - The intrinsic mechanism clots the blood in the injured vessel, whereas the extrinsic mechanism clots the blood that escapes into the tissue 3 - Both pathways are complementary as factor VIIa activate IX also XIIa, X 1, Xa and thrombin activate VII
2f7806992590ca8ab449eb7a328168b6.ppt