194e34a9f75cc5a145e7564205b108d2.ppt
- Количество слайдов: 39
Planners Forum Melbourne 2011 Nicole Cameron
Current Situation ¡ Department of Health New CE l formation of Department of Families l ¡ Health Reform – opportunity for change Structural changes underway – staged approach l Only at the beginning (11 April 2011) l ¡ Service Planning Historically more of a ‘silo’ approach l Need for integrated planning (continuum/ clinical/ infrastructure) l Likely an official Departmental Planning Unit will be established l Meanwhile work is underway… l 2
Northern Territory – it IS special! ¡ Population Context l l l ¡ Large geographical mass sparsely populated Small resident population with historically younger profile 30% Indigenous people (2. 4% Nationally) 70% Indigenous people live in remote/ very remote areas Greater proportion of Low SEIFA values than any other jurisdiction Population Health (BOD) Lower life expectancy than any other jurisdiction l Highest BOD amongst all jurisdictions l NT indigenous BOD 3. 57 times higher than national average l NT non-indigenous BOD 1. 22 times greater l ¡ Activity Small proportion of population account for high usage of services l ASH - Over 66% inpatient Indigenous & over 80% ED presentations l 3
From today… ¡ Political Context Close political environment l Territory 2030 – strategic direction for major services l Health services will be easier to access for all ¡ Access to services will be at a similar level as other states ¡ New Hospital in Darwin ¡ l Multiple stakeholders (AMSANT/ GPNNT/ Remote) Have commenced integrated planning (noting last point) ¡ Challenge for the NT: ¡ ‘Purist’ influence - service planning technical tools l Pragmatic approach – in the NT context l Creative implementation – multiple challenges (often conflicting) but necessary to think differently and apply national and international learnings to meet these ‘special’ needs l 4
Creativity in implementation An example for today: RENAL SERVICES IN THE NT 5
The Problem High Chronic Disease and increasing ESKD ¡ Majority from remote community (85% all dialysis patient are Indigenous people) ¡ Centralised service provision ¡ Poor access to health services l Limited access to specialists l ¡ Poor management of CKD l Prior to CTG/ intervention ¡ Poor psychosocial preparation for treatment ¡ We needed to think creatively in the context of the Territory, the patient and also of best practice 6
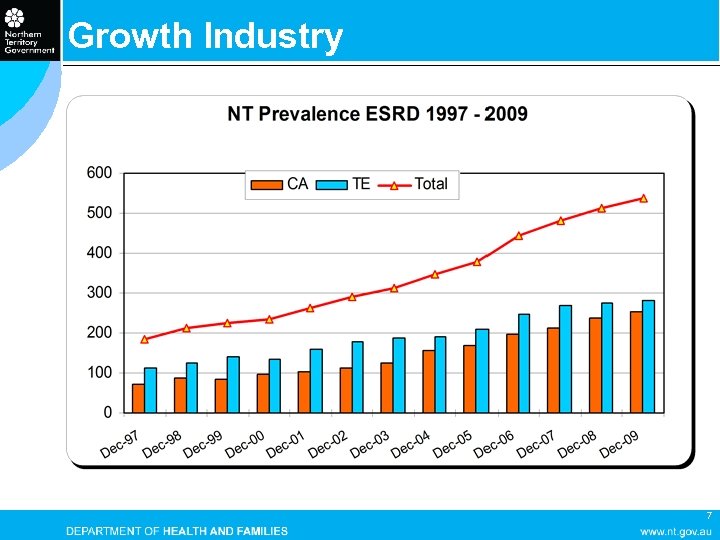
Growth Industry 7
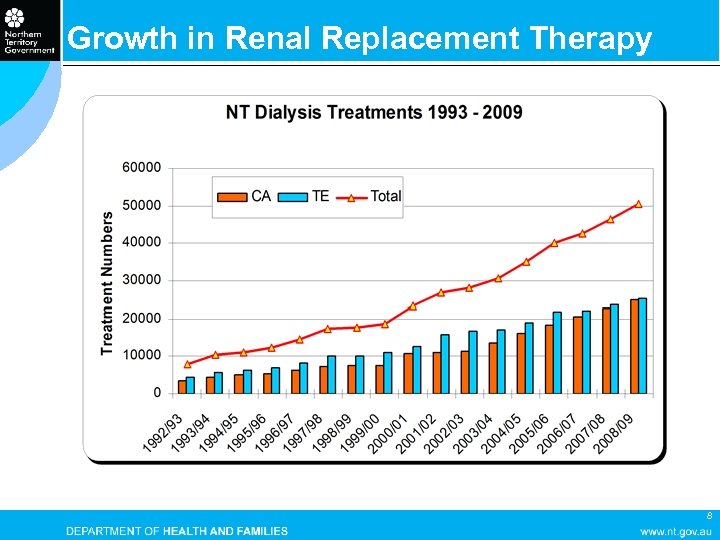
Growth in Renal Replacement Therapy 8
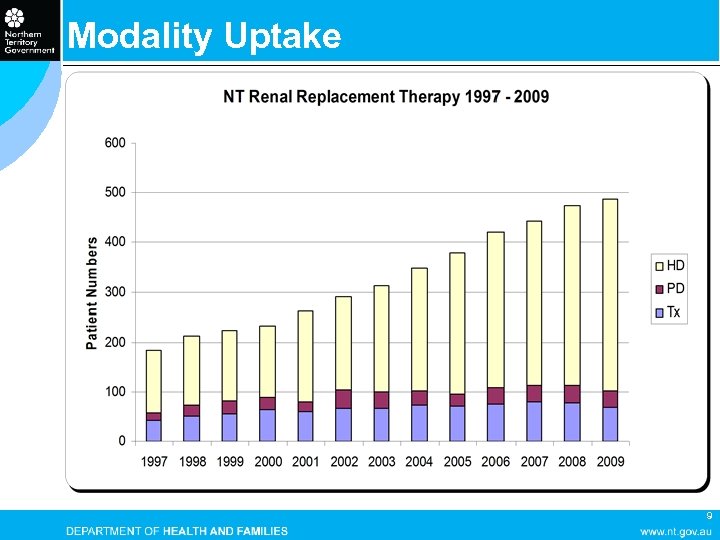
Modality Uptake 9
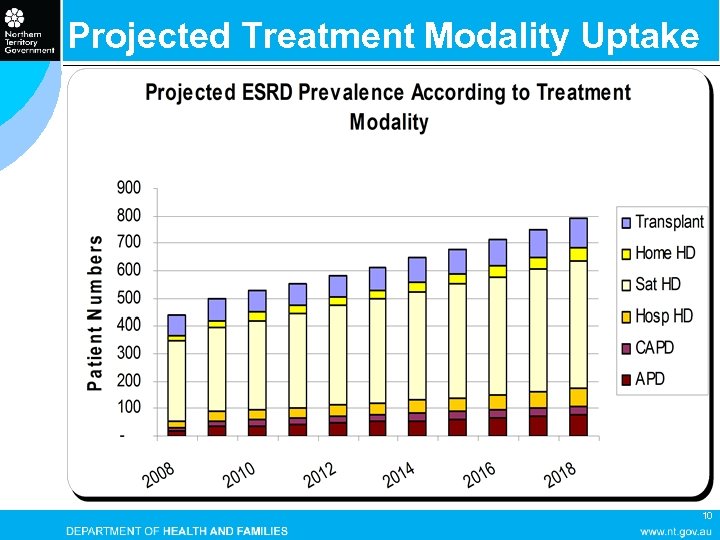
Projected Treatment Modality Uptake 10
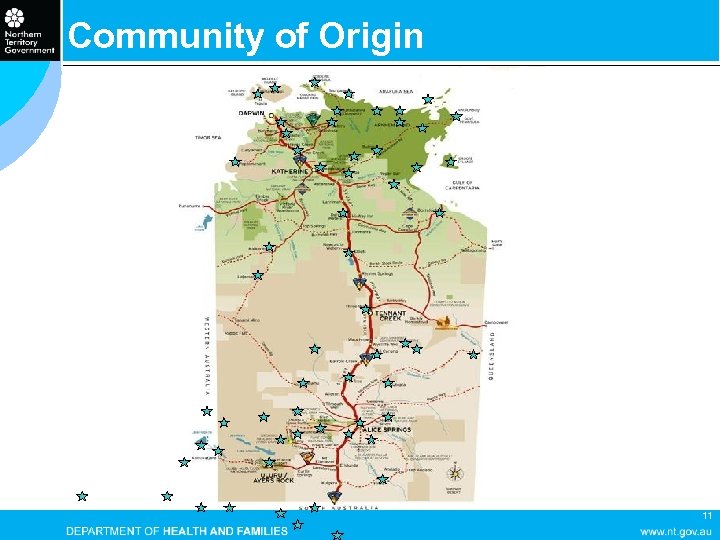
Community of Origin 11
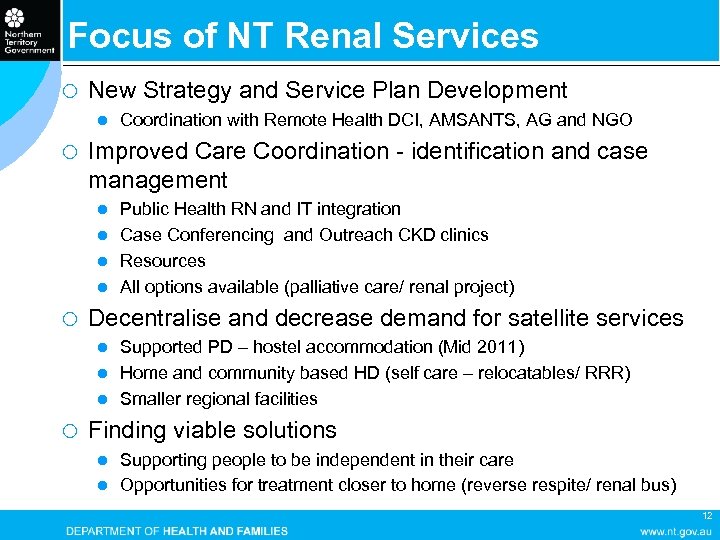
Focus of NT Renal Services ¡ New Strategy and Service Plan Development l ¡ Coordination with Remote Health DCI, AMSANTS, AG and NGO Improved Care Coordination - identification and case management Public Health RN and IT integration l Case Conferencing and Outreach CKD clinics l Resources l All options available (palliative care/ renal project) l ¡ Decentralise and decrease demand for satellite services Supported PD – hostel accommodation (Mid 2011) l Home and community based HD (self care – relocatables/ RRR) l Smaller regional facilities l ¡ Finding viable solutions Supporting people to be independent in their care l Opportunities for treatment closer to home (reverse respite/ renal bus) l 12
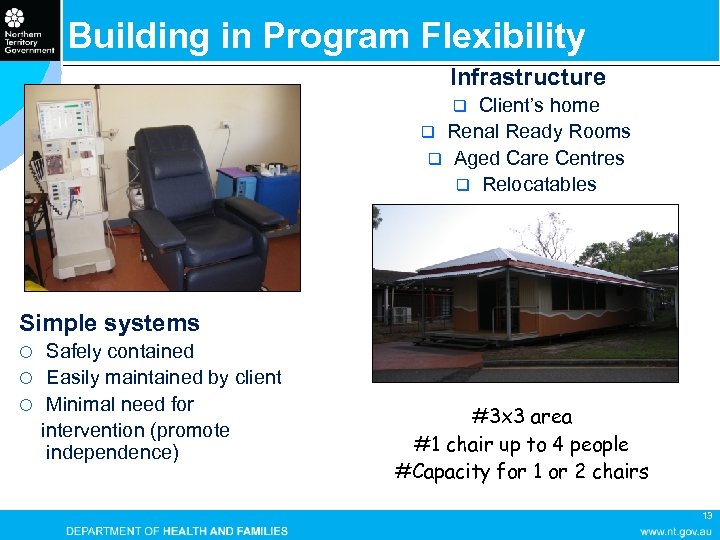
Building in Program Flexibility Infrastructure Client’s home q Renal Ready Rooms q Aged Care Centres q Relocatables q Simple systems Safely contained ¡ Easily maintained by client ¡ Minimal need for intervention (promote independence) ¡ #3 x 3 area #1 chair up to 4 people #Capacity for 1 or 2 chairs 13
Training Program Training Agreement l Client responsible for treatment l Client agrees to attend all training sessions l Client trains partner l Competency Checklists Interpreters Community Consultation (up to 3 visits) l Community Health Centre Staff l Local Shire Staff and store managers if required Community Partnership Agreements Client and Staff Support l Hot Line l Regular site visits 14
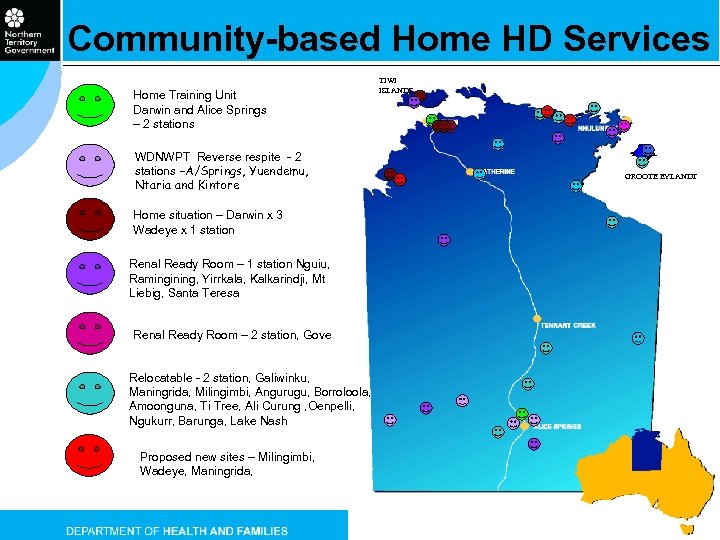
Community-based Home HD Services Home Training Unit Darwin and Alice Springs – 2 stations WDNWPT Reverse respite - 2 stations –A/Springs, Yuendemu, Ntaria and Kintore TIWI ISLANDS GROOTE EYLANDT Home situation – Darwin x 3 Wadeye x 1 station Renal Ready Room – 1 station Nguiu, Ramingining, Yirrkala, Kalkarindji, Mt Liebig, Santa Teresa Renal Ready Room – 2 station, Gove Relocatable - 2 station, Galiwinku, Maningrida, Milingimbi, Angurugu, Borroloola, Amoonguna, Ti Tree, Ali Curung , Oenpelli, Ngukurr, Barunga, Lake Nash Proposed new sites – Milingimbi, Wadeye, Maningrida, 15
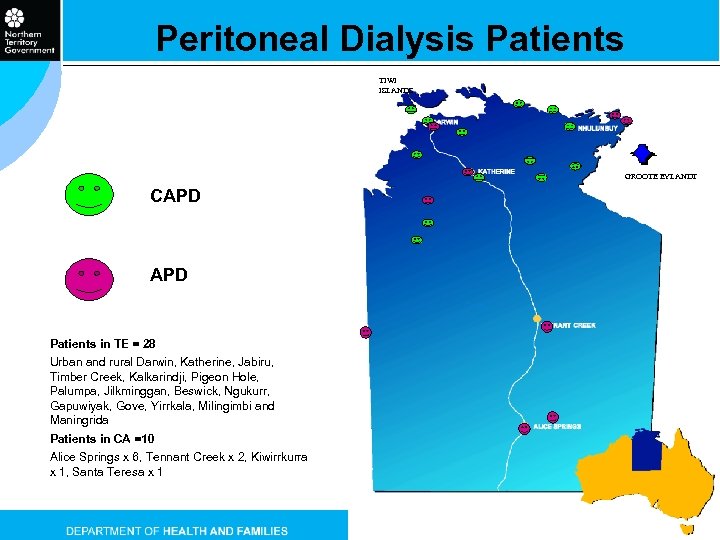
Peritoneal Dialysis Patients TIWI ISLANDS GROOTE EYLANDT CAPD Patients in TE = 28 Urban and rural Darwin, Katherine, Jabiru, Timber Creek, Kalkarindji, Pigeon Hole, Palumpa, Jilkminggan, Beswick, Ngukurr, Gapuwiyak, Gove, Yirrkala, Milingimbi and Maningrida Patients in CA =10 Alice Springs x 6, Tennant Creek x 2, Kiwirrkurra x 1, Santa Teresa x 1 16
Waste Management in Remote Areas ¡ Remote community waste directed to land fill ¡ Each HHD patient generates 1 bin every 4 -6 weeks. ¡ Removal of biohazard waste ¡ Tracking and management resource intense ¡ Biohazard waste management legislation ¡ Need a new management strategy 17
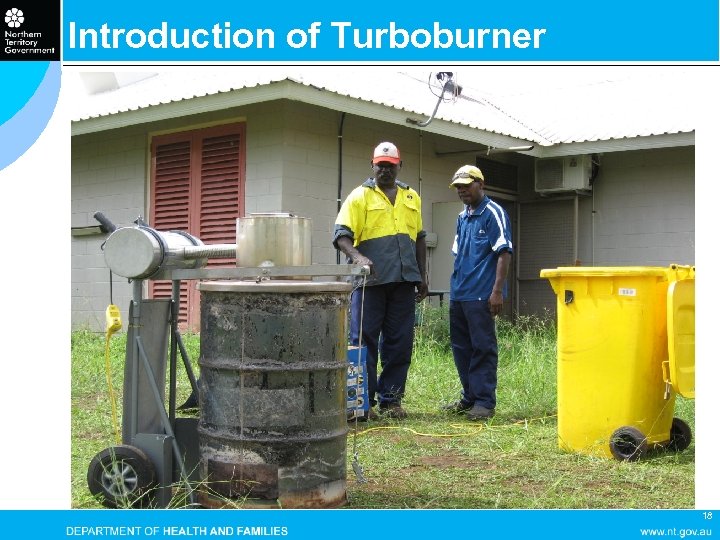
Introduction of Turboburner 18
Turbo Burner Requirements ¡ 200 L drum in reasonable condition to ensure a snug fit of the turbo burner lid. ¡ Weatherproof storage facility due to electrical components ¡ Wood/cardboard/old oil or substitute combustible to achieve the best burn ¡ Requires the management (loading, lighting, storing) to be allocated 19
After burn 20
Outcomes ¡ Complete burn of medical waste with minimal accelerants (waste oil or diesel) ¡ Produced a smoke free and odourless burn ¡ No hazardous gas emissions ¡ A preferable option of disposing of dialysate waste to landfill ¡ A more cost effective option than removing waste from communities 21
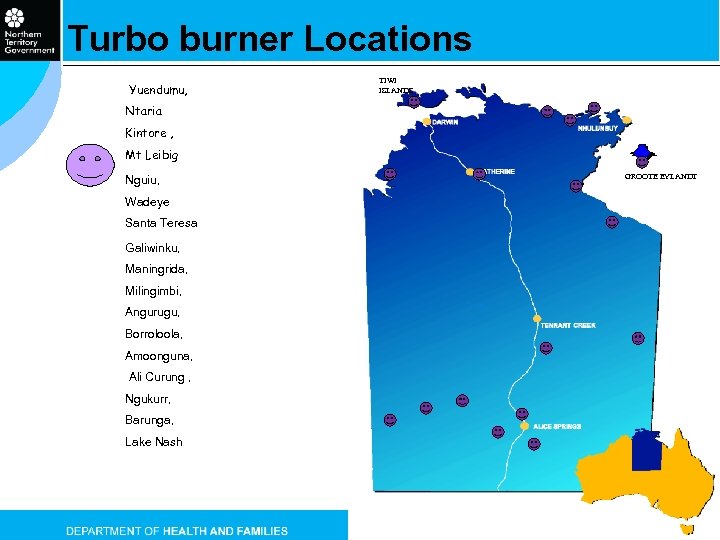
Turbo burner Locations Yuendumu, TIWI ISLANDS Ntaria Kintore , Mt Leibig Nguiu, GROOTE EYLANDT Wadeye Santa Teresa Galiwinku, Maningrida, Milingimbi, Angurugu, Borroloola, Amoonguna, Ali Curung , Ngukurr, Barunga, Lake Nash 22
Western Desert Nganampa Walytja Palyantjaku Tjutaku (WNDWPT) ¡ ¡ ¡ Reverse Respite Program – non-gov service delivery model Supported through funding from sales of art and mining royalties Supported by a board of elders from the Kintore region and a separate board from Yuendumu (providing own funds, under the guidance of WDNWPT) Alice Springs location at the Purple house providing Social support, advocacy, PHC services, self care training and respite dialysis Nurse assisted dialysis and Return to Country trips provided: ¡ Kintore ¡ Yuendumu ¡ Hermannsburg Nurses employed under a private contract arrangement 23
Requirements for Community Dialysis NT Renal Services has a SLA with WDNWPT to support with machines and chairs to provide reverse respite. WDNWPT ensure clients: ¡ have clearance from the Nephrologist to be dialysed away from the Renal unit ¡ trip is planned (ie you can’t turn up at your community dialysis facility and expect to be dialysed) ¡ have family support for your visit ¡ have been going regularly to dialysis, taking meds to be considered for a trip home ¡ Who miss scheduled dialysis out bush are returned to town ¡ WDNWPT is responsible for the dialysis care of the patient. 24
Renal Indigenous Resources 25
Renal Indigenous Resources 26
Mobile Bus Feasibility - Service Gap ¡ Limited rural satellite units and limited placements Tiwi Dialysis Centre – fly in fly out basis, difficult to expand l Katherine Dialysis Unit – most from surrounding regions, issues of relocation l Tennant Creek Dialysis Unit – at capacity l ¡ Self-care Therapies Home HD - growing but long training periods, self-reliance important, infrastructure rollout slow and costly l Peritoneal Dialysis – uptake improving but ‘churn’ high l Resistance from community relating to poor perceptions of RRT l Disincentive of staffed facilities l ¡ Patient Personal Capacity Many patients will never attain self-care status l Reliance on ‘partners’ – spectacularly unsuccessful l 27
Opportunity for Improvement ¡ Psychosocial l maintenance of relationships with kin and country, l Enable important events to be attended safely – community business, funerals, festivals ¡ Improved morbidity and mortality ¡ Reduce acute care costs l medical evacuation events, decrease hospitalisations ¡ Increase opportunities for education around renal disease ¡ Opportunity to change community perceptions ¡ Increase opportunities to attract and retain staff 28
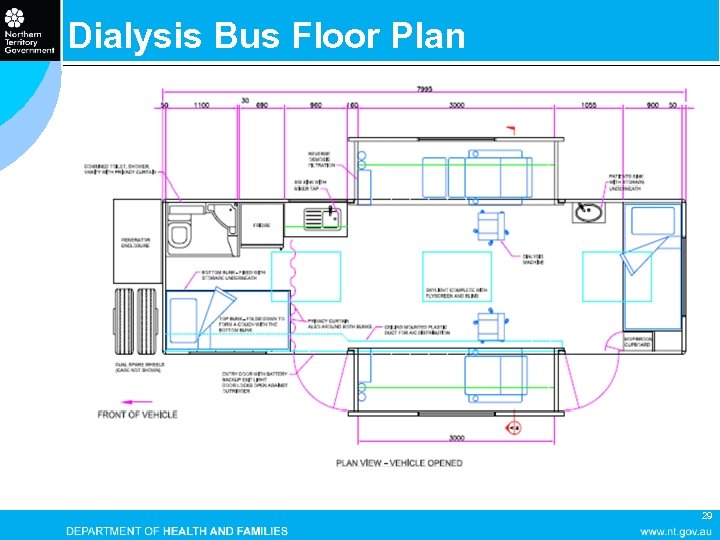
Dialysis Bus Floor Plan 29
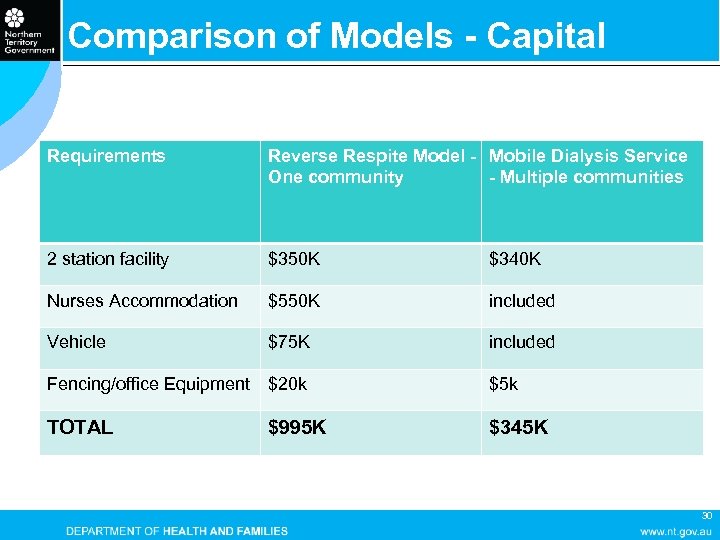
Comparison of Models - Capital Requirements Reverse Respite Model - Mobile Dialysis Service One community - Multiple communities 2 station facility $350 K $340 K Nurses Accommodation $550 K included Vehicle $75 K included Fencing/office Equipment $20 k $5 k TOTAL $995 K $345 K 30
Pros and Cons of Mobile Service ¡ Benefits l l l ¡ Can provide respite dialysis to a broad range of communities Infrastructure and recurrent costs are lower Can be utilised to provide education and undertake clinics Is self-contained with minimal impact on community Only requires access to water High interest in service implementation (recruitment) Risks Robustness of dialysis machinery over un-graded roads untested l Continuous access to water maybe an issue l Will need time to work out teething problems l Space configuration for dialysis, sleeping and living yet to be tested l 31

32

33

34

35

Ali Curung Visit 36

37

38
THANK YOU 39
194e34a9f75cc5a145e7564205b108d2.ppt