71c214078d38ff5c0316b8ef34f1ab37.ppt
- Количество слайдов: 28
 Physician Wellness: Why We Should Care and What We Can Do About It Mukta Panda MD MACP
Physician Wellness: Why We Should Care and What We Can Do About It Mukta Panda MD MACP
 Background • Physician well-being has come under increased scrutiny in recent years • Common: – Burnout – Low job satisfaction – High stress – Low quality of life • Affects all stages of physician training and practice • Affects all specialties
Background • Physician well-being has come under increased scrutiny in recent years • Common: – Burnout – Low job satisfaction – High stress – Low quality of life • Affects all stages of physician training and practice • Affects all specialties
 Brief Summary of Epidemiology • Medical students matriculate with BETTER wellbeing than their age-group peers • Early in medical school, this reverses • Poor well-being persists through medical school and residency into practice: • National physician burnout rate exceeds 54% • Affects all specialties, perhaps worst in “front line” areas of medicine • >500, 000 physicians burned out at any given time
Brief Summary of Epidemiology • Medical students matriculate with BETTER wellbeing than their age-group peers • Early in medical school, this reverses • Poor well-being persists through medical school and residency into practice: • National physician burnout rate exceeds 54% • Affects all specialties, perhaps worst in “front line” areas of medicine • >500, 000 physicians burned out at any given time
 What is Burnout? Burnout is a syndrome of depersonalization, emotional exhaustion, and low personal accomplishment leading to decreased effectiveness at work.
What is Burnout? Burnout is a syndrome of depersonalization, emotional exhaustion, and low personal accomplishment leading to decreased effectiveness at work.
 Depersonalization “I’ve become more callous toward people since I took this job. ”
Depersonalization “I’ve become more callous toward people since I took this job. ”
 Emotional Exhaustion “I feel like I’m at the end of my rope. ”
Emotional Exhaustion “I feel like I’m at the end of my rope. ”
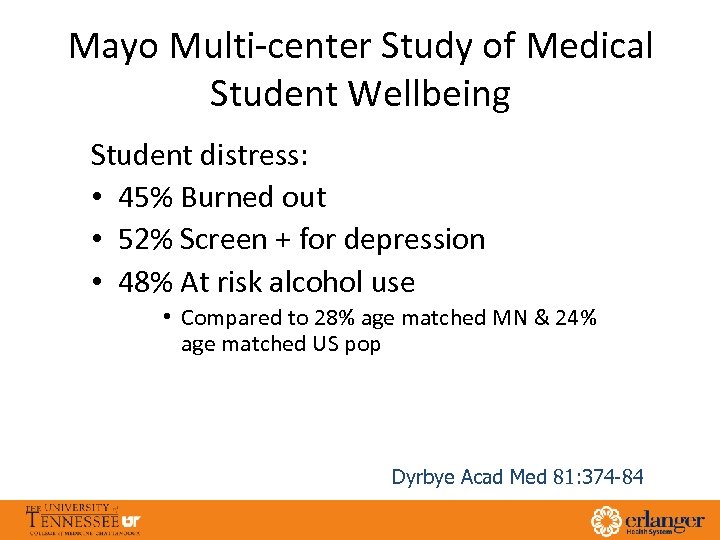 Mayo Multi-center Study of Medical Student Wellbeing Student distress: • 45% Burned out • 52% Screen + for depression • 48% At risk alcohol use • Compared to 28% age matched MN & 24% age matched US pop Dyrbye Acad Med 81: 374 -84
Mayo Multi-center Study of Medical Student Wellbeing Student distress: • 45% Burned out • 52% Screen + for depression • 48% At risk alcohol use • Compared to 28% age matched MN & 24% age matched US pop Dyrbye Acad Med 81: 374 -84
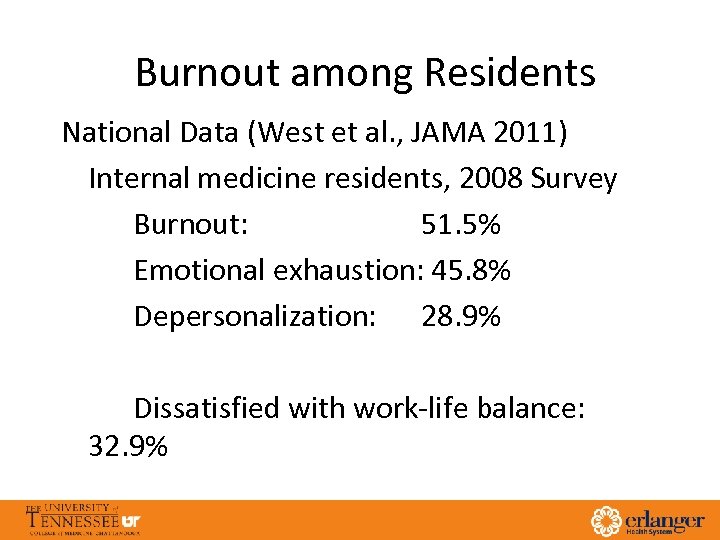 Burnout among Residents National Data (West et al. , JAMA 2011) Internal medicine residents, 2008 Survey Burnout: 51. 5% Emotional exhaustion: 45. 8% Depersonalization: 28. 9% Dissatisfied with work-life balance: 32. 9%
Burnout among Residents National Data (West et al. , JAMA 2011) Internal medicine residents, 2008 Survey Burnout: 51. 5% Emotional exhaustion: 45. 8% Depersonalization: 28. 9% Dissatisfied with work-life balance: 32. 9%
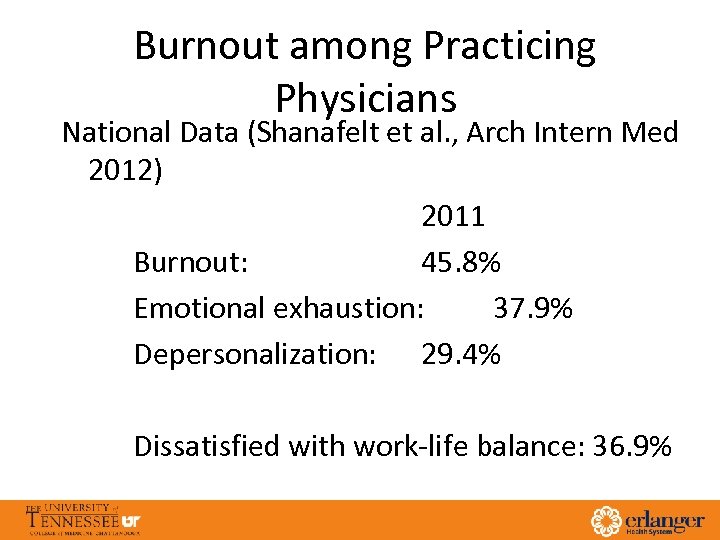 Burnout among Practicing Physicians National Data (Shanafelt et al. , Arch Intern Med 2012) 2011 Burnout: 45. 8% Emotional exhaustion: 37. 9% Depersonalization: 29. 4% Dissatisfied with work-life balance: 36. 9%
Burnout among Practicing Physicians National Data (Shanafelt et al. , Arch Intern Med 2012) 2011 Burnout: 45. 8% Emotional exhaustion: 37. 9% Depersonalization: 29. 4% Dissatisfied with work-life balance: 36. 9%
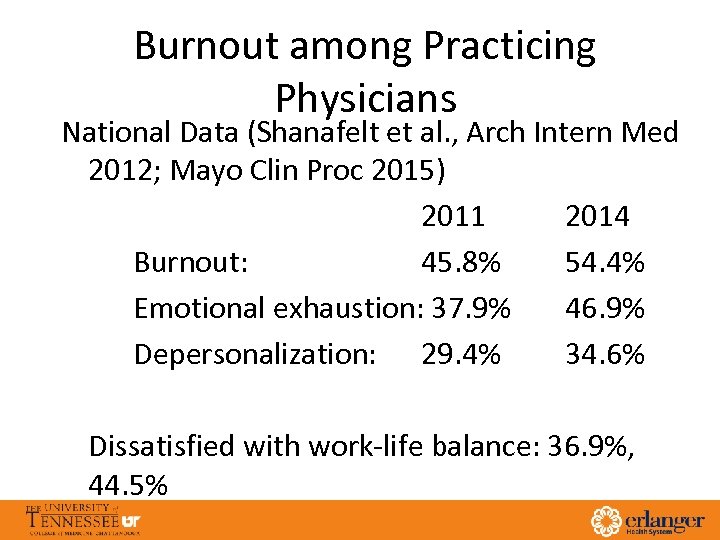 Burnout among Practicing Physicians National Data (Shanafelt et al. , Arch Intern Med 2012; Mayo Clin Proc 2015) 2011 2014 Burnout: 45. 8% 54. 4% Emotional exhaustion: 37. 9% 46. 9% Depersonalization: 29. 4% 34. 6% Dissatisfied with work-life balance: 36. 9%, 44. 5%
Burnout among Practicing Physicians National Data (Shanafelt et al. , Arch Intern Med 2012; Mayo Clin Proc 2015) 2011 2014 Burnout: 45. 8% 54. 4% Emotional exhaustion: 37. 9% 46. 9% Depersonalization: 29. 4% 34. 6% Dissatisfied with work-life balance: 36. 9%, 44. 5%
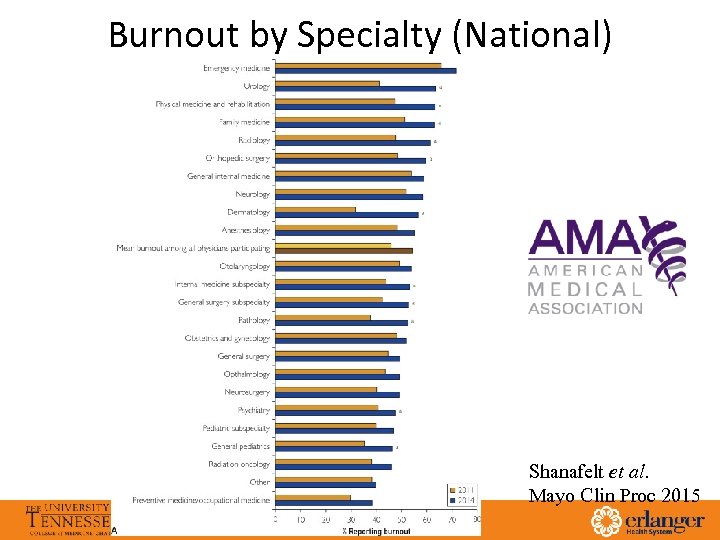 Burnout by Specialty (National) Emergency Medicine General Internal Medicine Neurology Family Medicine Otolaryngology Orthopedic Surgery Anesthesiology OB/GYN Radiology Physical medicine/Rehab Average all physicians General Surgery Internal Medicine Subspecialty Ophthalmology General Surgery Sub-specialty Urology Psychiatry Neurosurgery Pediatric Subspecialty Other Radiation Oncology Pathology General Pediatrics Dermatology Shanafelt et al. Mayo Clin Proc 2015
Burnout by Specialty (National) Emergency Medicine General Internal Medicine Neurology Family Medicine Otolaryngology Orthopedic Surgery Anesthesiology OB/GYN Radiology Physical medicine/Rehab Average all physicians General Surgery Internal Medicine Subspecialty Ophthalmology General Surgery Sub-specialty Urology Psychiatry Neurosurgery Pediatric Subspecialty Other Radiation Oncology Pathology General Pediatrics Dermatology Shanafelt et al. Mayo Clin Proc 2015
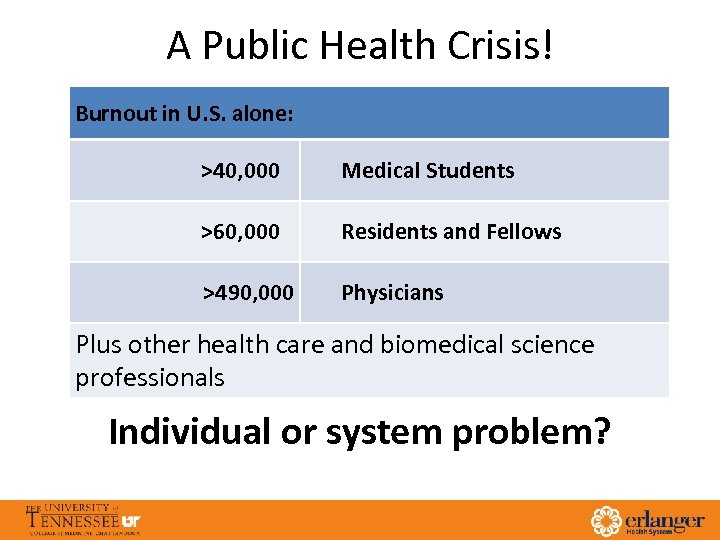 A Public Health Crisis! Burnout in U. S. alone: >40, 000 Medical Students >60, 000 Residents and Fellows >490, 000 Physicians Plus other health care and biomedical science professionals Individual or system problem?
A Public Health Crisis! Burnout in U. S. alone: >40, 000 Medical Students >60, 000 Residents and Fellows >490, 000 Physicians Plus other health care and biomedical science professionals Individual or system problem?
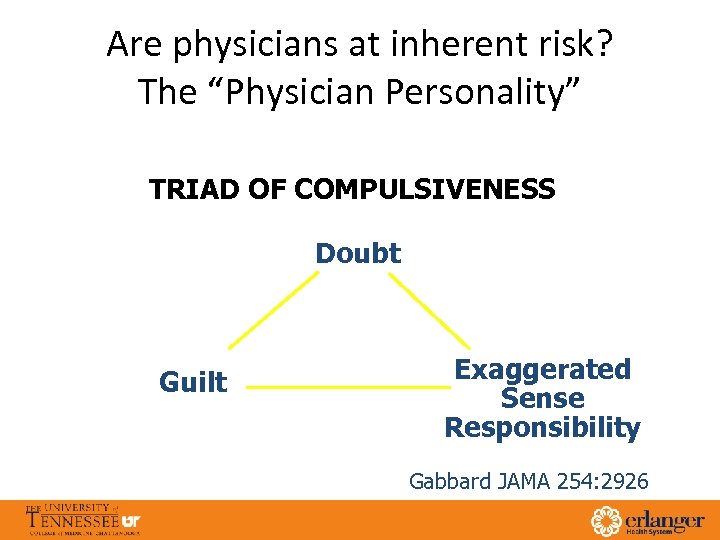 Are physicians at inherent risk? The “Physician Personality” TRIAD OF COMPULSIVENESS Doubt Guilt Exaggerated Sense Responsibility Gabbard JAMA 254: 2926
Are physicians at inherent risk? The “Physician Personality” TRIAD OF COMPULSIVENESS Doubt Guilt Exaggerated Sense Responsibility Gabbard JAMA 254: 2926
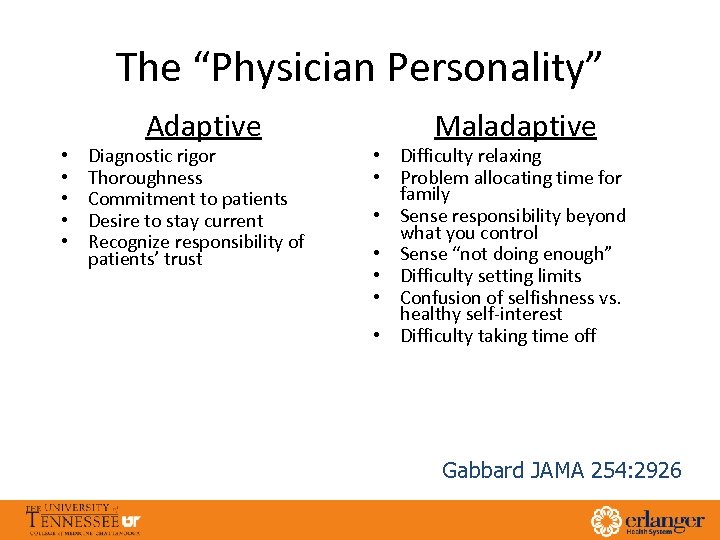 The “Physician Personality” • • • Adaptive Diagnostic rigor Thoroughness Commitment to patients Desire to stay current Recognize responsibility of patients’ trust Maladaptive • Difficulty relaxing • Problem allocating time for family • Sense responsibility beyond what you control • Sense “not doing enough” • Difficulty setting limits • Confusion of selfishness vs. healthy self-interest • Difficulty taking time off Gabbard JAMA 254: 2926
The “Physician Personality” • • • Adaptive Diagnostic rigor Thoroughness Commitment to patients Desire to stay current Recognize responsibility of patients’ trust Maladaptive • Difficulty relaxing • Problem allocating time for family • Sense responsibility beyond what you control • Sense “not doing enough” • Difficulty setting limits • Confusion of selfishness vs. healthy self-interest • Difficulty taking time off Gabbard JAMA 254: 2926
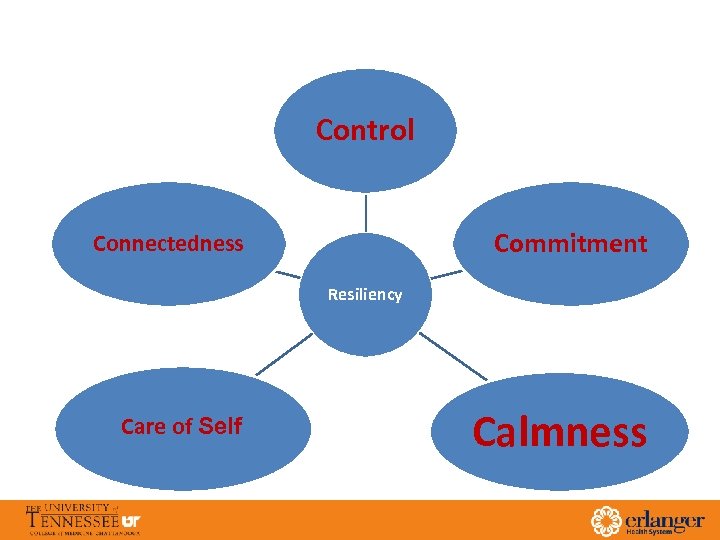 Control Commitment Connectedness Resiliency Care of Self Calmness
Control Commitment Connectedness Resiliency Care of Self Calmness
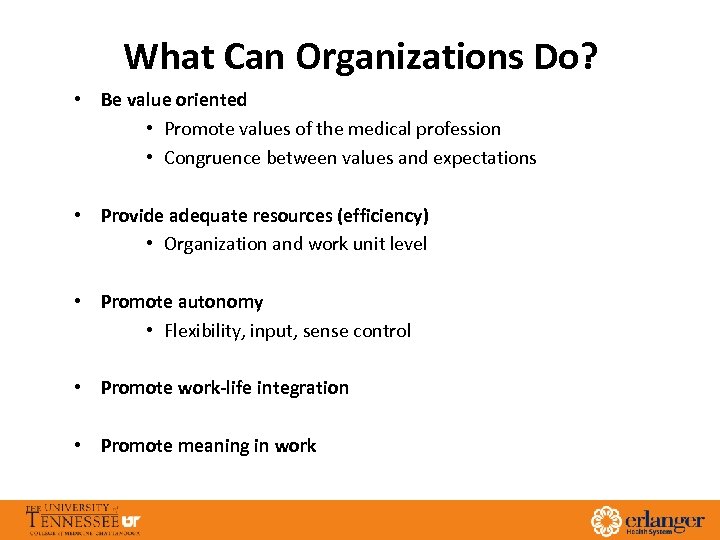 What Can Organizations Do? • Be value oriented • Promote values of the medical profession • Congruence between values and expectations • Provide adequate resources (efficiency) • Organization and work unit level • Promote autonomy • Flexibility, input, sense control • Promote work-life integration • Promote meaning in work
What Can Organizations Do? • Be value oriented • Promote values of the medical profession • Congruence between values and expectations • Provide adequate resources (efficiency) • Organization and work unit level • Promote autonomy • Flexibility, input, sense control • Promote work-life integration • Promote meaning in work
 Physician Well-Being: Expanding the Triple Aim Colin P. West, MD, Ph. D J Gen Intern Med Feb 2016 17
Physician Well-Being: Expanding the Triple Aim Colin P. West, MD, Ph. D J Gen Intern Med Feb 2016 17
 From The Triple Aim TO The Quadruple Aim: care, health, cost and meaning in work • The classic ‘Triple Aim’ for healthcare is a framework developed by the IHI in 2008 by Donald Berwick and colleagues • Describes an approach to optimizing health system performance 1. Improving the patient experience of care (including quality and satisfaction) 2. Improving the health of populations 3. Reducing the per capita cost of health care • Winning healthcare delivery organizations recognize that the Quadruple Aim will deliver sustainable success. • The “forgotten aim” is a better experience for the health professional. Sikka R, Morath JM, Leape L BMJ Qual Saf doi: 10. 1136/bmjqs-2015 -004160 18
From The Triple Aim TO The Quadruple Aim: care, health, cost and meaning in work • The classic ‘Triple Aim’ for healthcare is a framework developed by the IHI in 2008 by Donald Berwick and colleagues • Describes an approach to optimizing health system performance 1. Improving the patient experience of care (including quality and satisfaction) 2. Improving the health of populations 3. Reducing the per capita cost of health care • Winning healthcare delivery organizations recognize that the Quadruple Aim will deliver sustainable success. • The “forgotten aim” is a better experience for the health professional. Sikka R, Morath JM, Leape L BMJ Qual Saf doi: 10. 1136/bmjqs-2015 -004160 18
 Physician Wellness: A Missing Quality Indicator Jean E Wallace, Jane B Lemaire, William A Ghali Lancet 2009; 374: 1714– 21 • When physicians are unwell, the performance of health-care systems can be suboptimum • Physician wellness might not only benefit the individual physician, it could also be vital to the delivery of high-quality health care 19
Physician Wellness: A Missing Quality Indicator Jean E Wallace, Jane B Lemaire, William A Ghali Lancet 2009; 374: 1714– 21 • When physicians are unwell, the performance of health-care systems can be suboptimum • Physician wellness might not only benefit the individual physician, it could also be vital to the delivery of high-quality health care 19
 “Healthy citizens are the greatest asset any country can have. ” Sir Winston Churchill 20
“Healthy citizens are the greatest asset any country can have. ” Sir Winston Churchill 20
 How might the Quadruple Aim be implemented? 1. Physician well-being should be recognized as a central element of professionalism in medicine, and therefore as a professional responsibility shared by both individual physicians and the healthcare systems in which they impact patients. 2. A focus on physician well-being should not be viewed as selfish or self-serving professional 3. Integration of clinician well-being into the professional fabric of medicine 21
How might the Quadruple Aim be implemented? 1. Physician well-being should be recognized as a central element of professionalism in medicine, and therefore as a professional responsibility shared by both individual physicians and the healthcare systems in which they impact patients. 2. A focus on physician well-being should not be viewed as selfish or self-serving professional 3. Integration of clinician well-being into the professional fabric of medicine 21
 What If Joy in Practice Were a Metric? Christine A. Sinsky, MD
What If Joy in Practice Were a Metric? Christine A. Sinsky, MD
 Sinsky shares some action steps to bring back joy in practice: • For institutions: “Be bold. ” Recognize the importance of higher staffing rations for optimal patient and provider care, and reengineer workflows to increase physician time spent with patients and with family at home. • For measure developers: “Keep it simple and add it up. ” Add the total time for compliance with all regulations and measures. “Less is more here, ” • For regulators and technology vendors: “Support advanced models of team-based care. ” Physicians often spend more time documenting care than delivering it. Health care regulations and electronic health records designed to support team-based care will help reverse that problem. • http: //catalyst. nejm. org/videos/joy-practice-core-metric/
Sinsky shares some action steps to bring back joy in practice: • For institutions: “Be bold. ” Recognize the importance of higher staffing rations for optimal patient and provider care, and reengineer workflows to increase physician time spent with patients and with family at home. • For measure developers: “Keep it simple and add it up. ” Add the total time for compliance with all regulations and measures. “Less is more here, ” • For regulators and technology vendors: “Support advanced models of team-based care. ” Physicians often spend more time documenting care than delivering it. Health care regulations and electronic health records designed to support team-based care will help reverse that problem. • http: //catalyst. nejm. org/videos/joy-practice-core-metric/
 Enhancing Health Care Provider Engagement And Promoting A Healthy And Well Organization, a Erlanger health System and University of Tennessee Partnership
Enhancing Health Care Provider Engagement And Promoting A Healthy And Well Organization, a Erlanger health System and University of Tennessee Partnership
 Data
Data
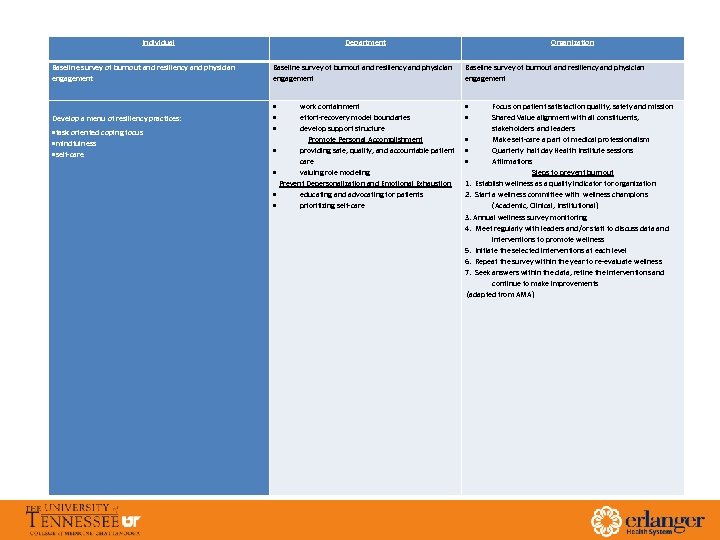 Individual Department Baseline survey of burnout and resiliency and physician engagement Develop a menu of resiliency practices: task oriented coping focus mindfulness self-care Organization Baseline survey of burnout and resiliency and physician engagement work containment effort-recovery model boundaries develop support structure Promote Personal Accomplishment providing safe, quality, and accountable patient care valuing role modeling Prevent Depersonalization and Emotional Exhaustion educating and advocating for patients prioritizing self-care Focus on patient satisfaction quality, safety and mission Shared Value alignment with all constituents, stakeholders and leaders Make self-care a part of medical professionalism Quarterly half day Health Institute sessions Affirmations Steps to prevent burnout 1. Establish wellness as a quality indicator for organization 2. Start a wellness committee with wellness champions (Academic, Clinical, Institutional) 3. Annual wellness survey monitoring 4. Meet regularly with leaders and/or staff to discuss data and interventions to promote wellness 5. Initiate the selected interventions at each level 6. Repeat the survey within the year to re-evaluate wellness 7. Seek answers within the data, refine the interventions and continue to make improvements (adapted from AMA)
Individual Department Baseline survey of burnout and resiliency and physician engagement Develop a menu of resiliency practices: task oriented coping focus mindfulness self-care Organization Baseline survey of burnout and resiliency and physician engagement work containment effort-recovery model boundaries develop support structure Promote Personal Accomplishment providing safe, quality, and accountable patient care valuing role modeling Prevent Depersonalization and Emotional Exhaustion educating and advocating for patients prioritizing self-care Focus on patient satisfaction quality, safety and mission Shared Value alignment with all constituents, stakeholders and leaders Make self-care a part of medical professionalism Quarterly half day Health Institute sessions Affirmations Steps to prevent burnout 1. Establish wellness as a quality indicator for organization 2. Start a wellness committee with wellness champions (Academic, Clinical, Institutional) 3. Annual wellness survey monitoring 4. Meet regularly with leaders and/or staff to discuss data and interventions to promote wellness 5. Initiate the selected interventions at each level 6. Repeat the survey within the year to re-evaluate wellness 7. Seek answers within the data, refine the interventions and continue to make improvements (adapted from AMA)
 Physician Distress: Key Drivers • Excessive workload • Inefficient work environment, inadequate support • Problems with work-life integration • Loss autonomy/flexibility/control • Loss of values and meaning in work
Physician Distress: Key Drivers • Excessive workload • Inefficient work environment, inadequate support • Problems with work-life integration • Loss autonomy/flexibility/control • Loss of values and meaning in work
 Worksheets
Worksheets


