3f6525a0b165f4aa17561b030bc90a75.ppt
- Количество слайдов: 48
Phenomics By: Larry Burd, Ph. D. Director, North Dakota Fetal Alcohol Syndrome Center University of North Dakota, School of Medicine and Health Sciences Grand Forks, ND
Study of Outcomes
Detection n Classification n
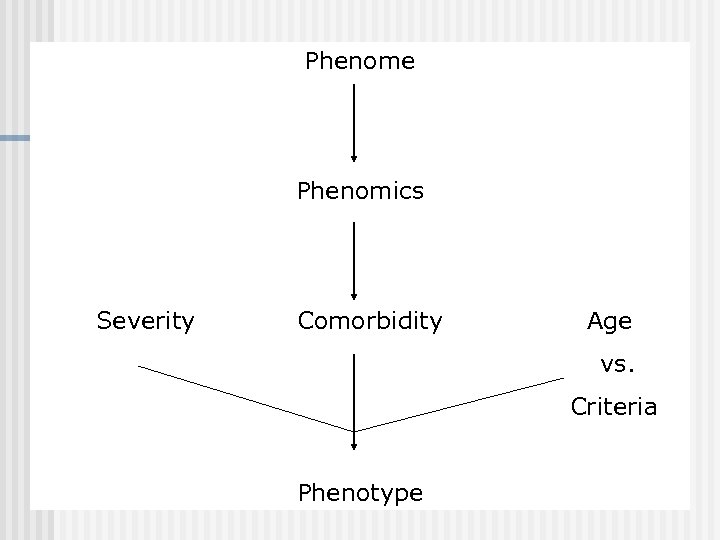
Phenome Phenomics Severity Comorbidity Age vs. Criteria Phenotype
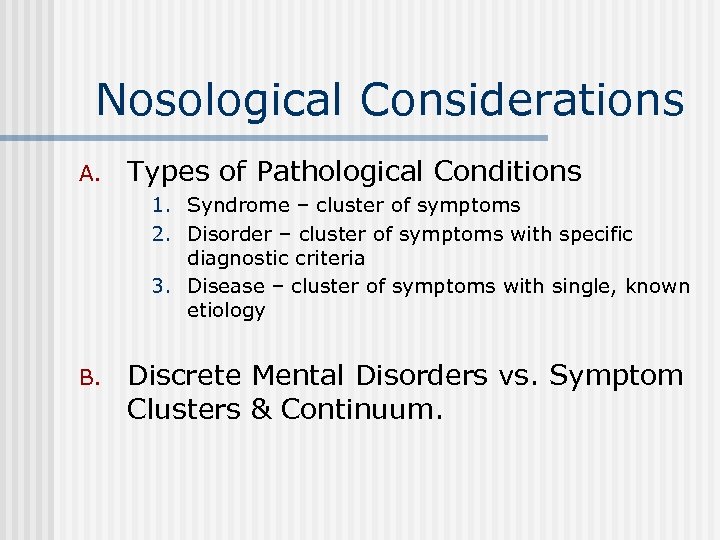
Nosological Considerations A. Types of Pathological Conditions 1. Syndrome – cluster of symptoms 2. Disorder – cluster of symptoms with specific diagnostic criteria 3. Disease – cluster of symptoms with single, known etiology B. Discrete Mental Disorders vs. Symptom Clusters & Continuum.
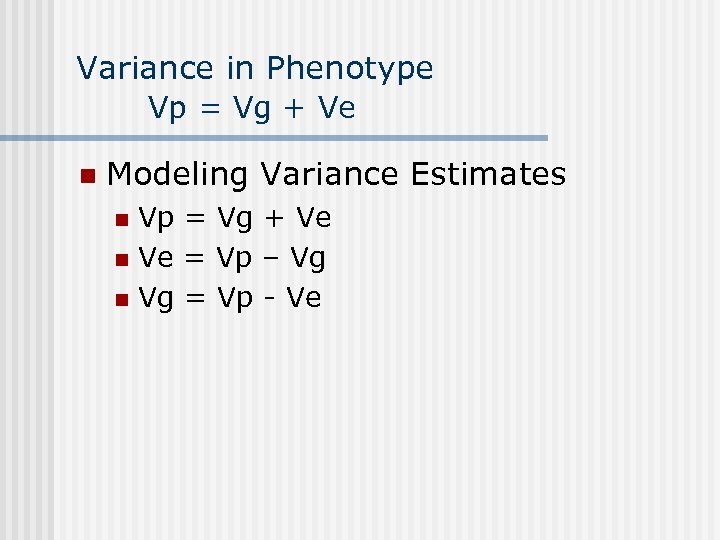
Variance in Phenotype Vp = Vg + Ve n Modeling Variance Estimates Vp = Vg + Ve n Ve = Vp – Vg n Vg = Vp - Ve n
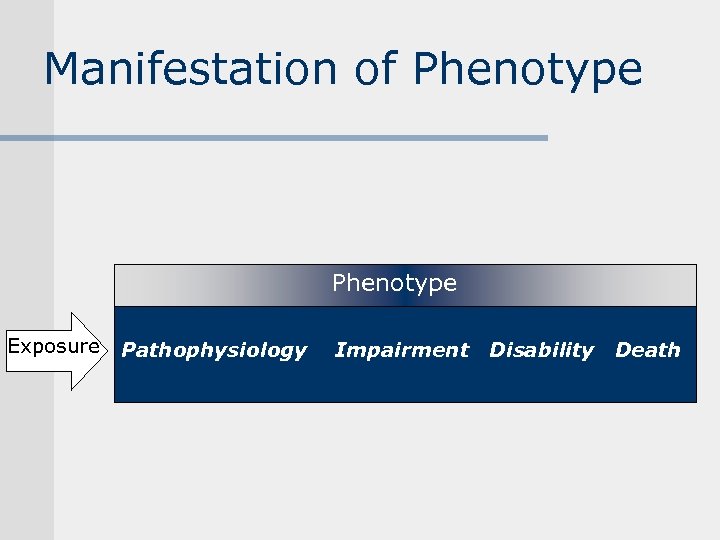
Manifestation of Phenotype Exposure Pathophysiology Impairment Disability Death
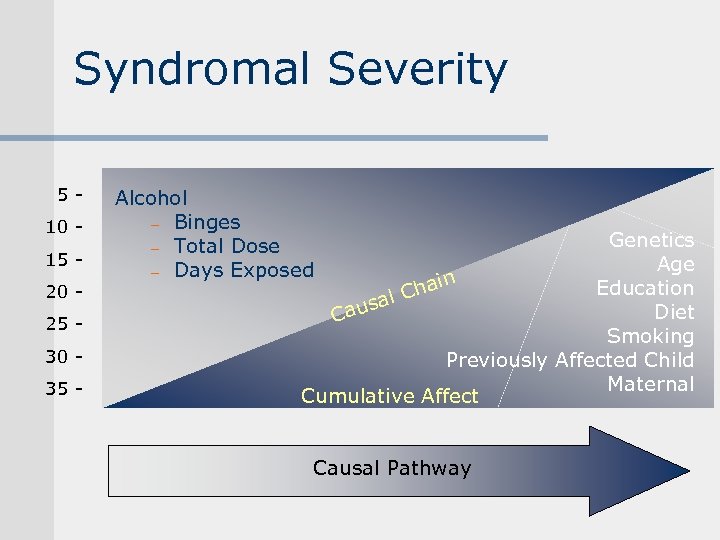
Syndromal Severity 510 15 20 25 30 35 - Alcohol - Binges - Total Dose - Days Exposed Genetics Age Education hain al C s Diet Cau Smoking Previously Affected Child Maternal Cumulative Affect Causal Pathway
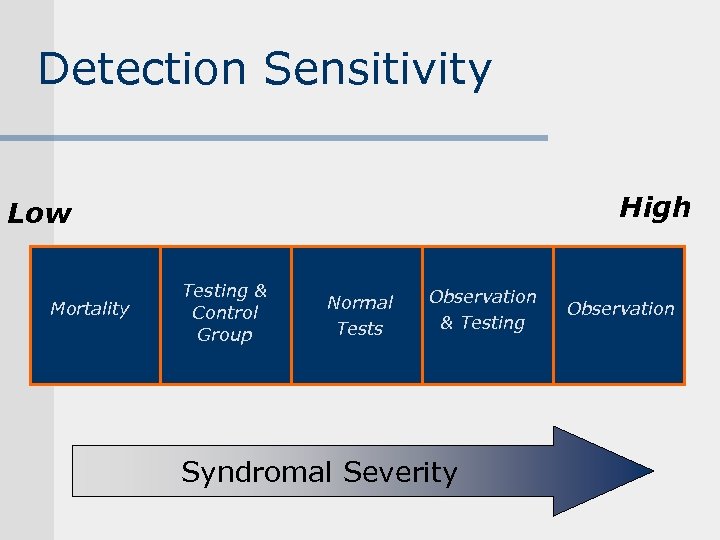
Detection Sensitivity High Low Mortality Testing & Control Group Normal Tests Observation & Testing Syndromal Severity Observation
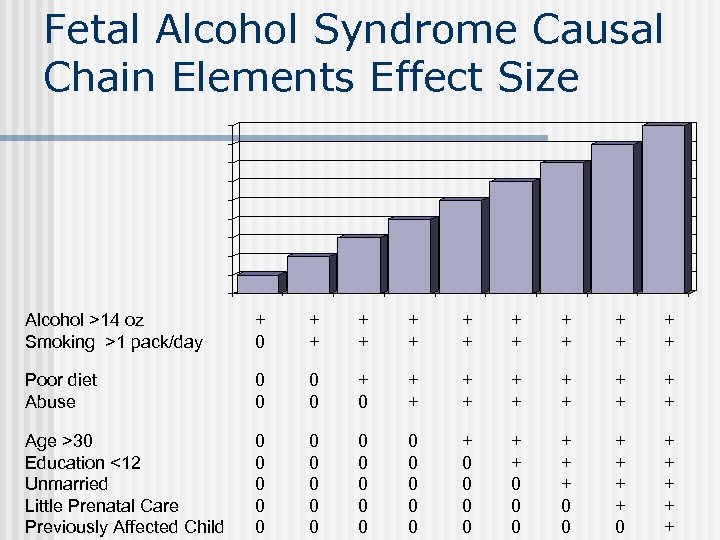
Fetal Alcohol Syndrome Causal Chain Elements Effect Size Alcohol >14 oz Smoking >1 pack/day + 0 + + + + Poor diet Abuse 0 0 + 0 + + + Age >30 Education <12 Unmarried Little Prenatal Care Previously Affected Child 0 0 0 0 0 + 0 0 + + 0 0 0 + + + + 0 + + +
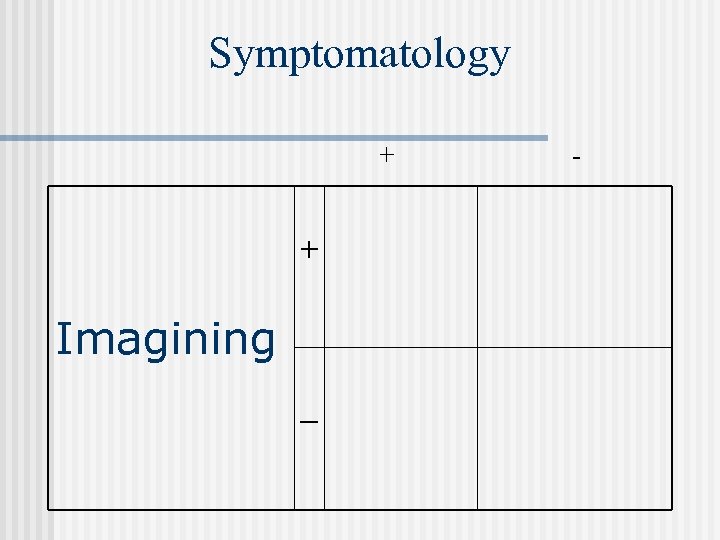
Symptomatology + + Imagining _ -
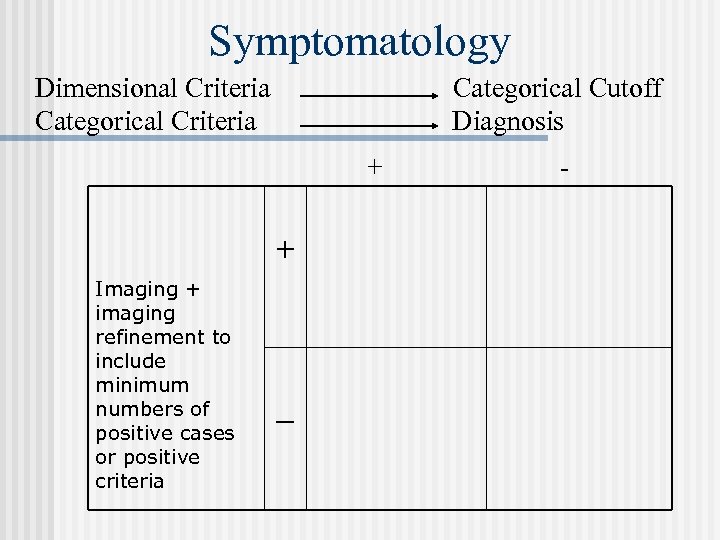
Symptomatology Dimensional Criteria. Categorical Criteria Categorical Cutoff Diagnosis + + Imaging + imaging refinement to include minimum numbers of positive cases or positive criteria _ -
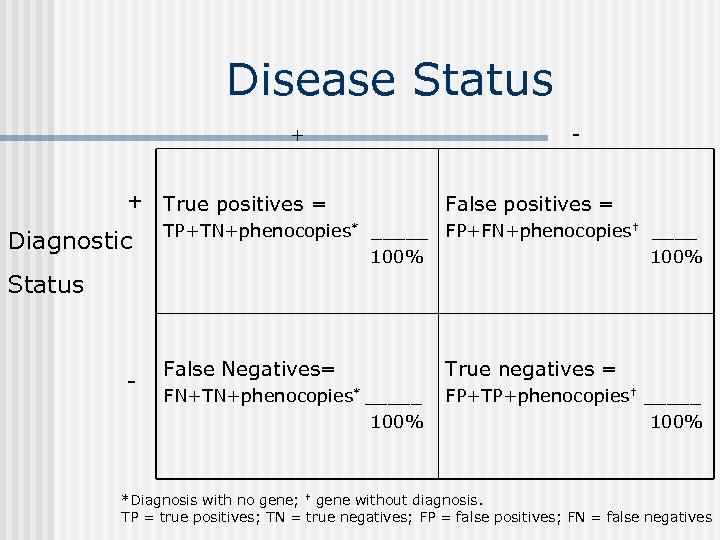
Disease Status + + True positives = Diagnostic - False positives = TP+TN+phenocopies* _____ FP+FN+phenocopies† ____ 100% Status - False Negatives= True negatives = FN+TN+phenocopies* _____ 100% FP+TP+phenocopies† _____ 100% *Diagnosis with no gene; † gene without diagnosis. TP = true positives; TN = true negatives; FP = false positives; FN = false negatives
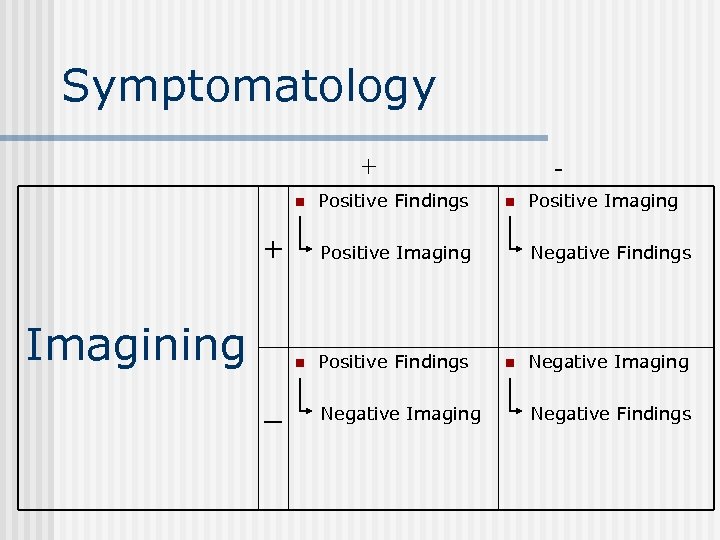
Symptomatology + n + Imagining n Positive Imaging n _ Positive Findings - Positive Findings Negative Imaging Positive Imaging Negative Findings n Negative Imaging Negative Findings
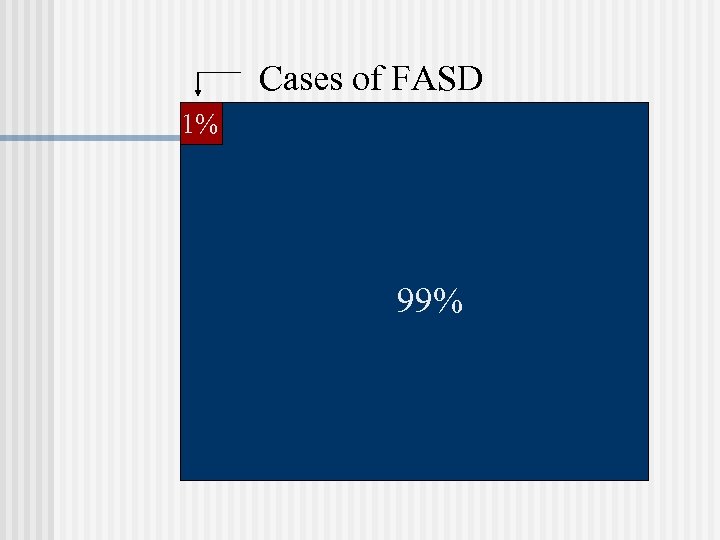
Cases of FASD 1% 99%
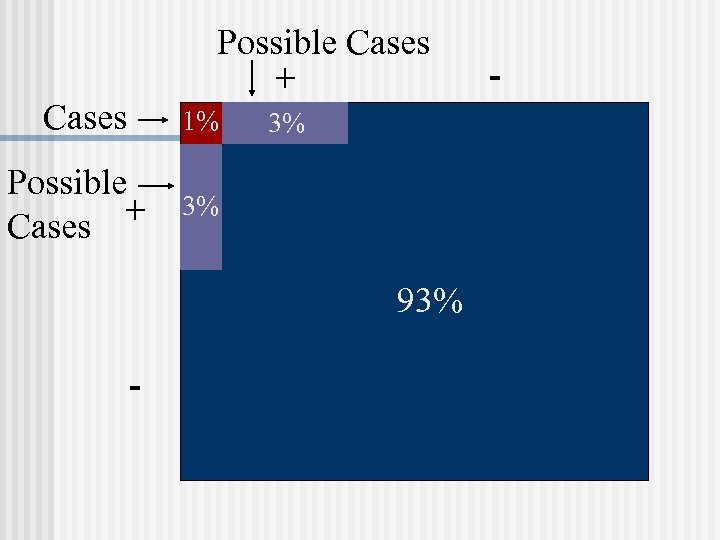
Possible Cases + Cases 1% Possible + Cases 3% 3% 93% - -
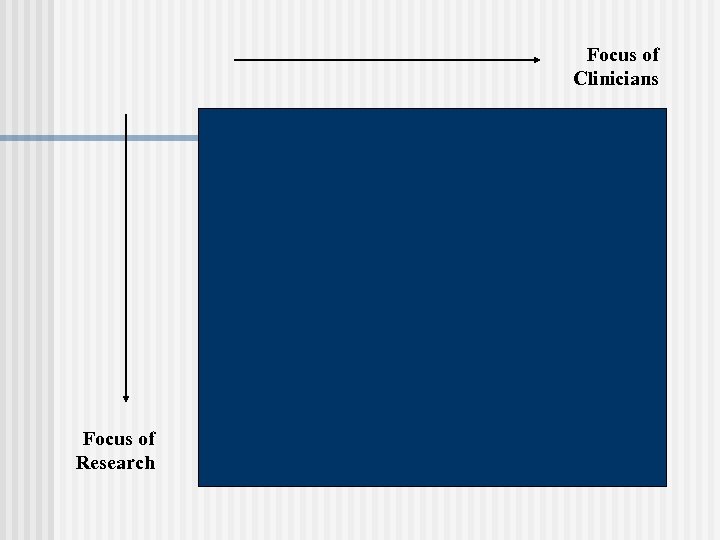
Focus of Clinicians Focus of Research
Transmission of Effects Familial n Generational n Genetic n
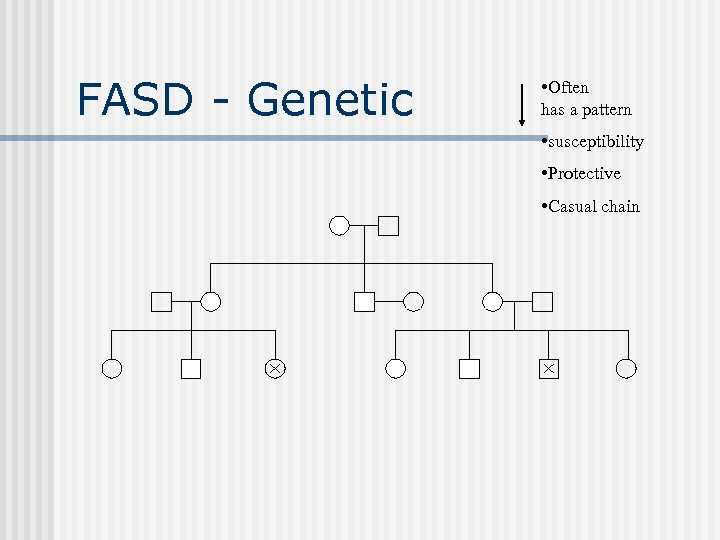
FASD - Genetic • Often has a pattern • susceptibility • Protective • Casual chain
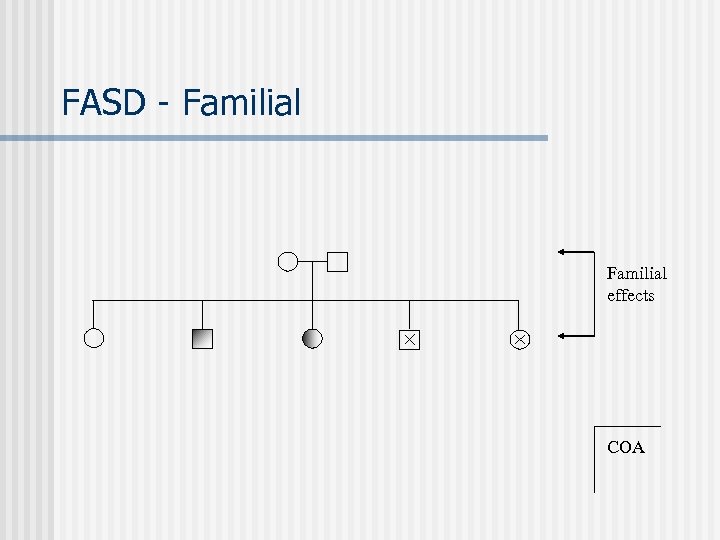
FASD - Familial effects COA
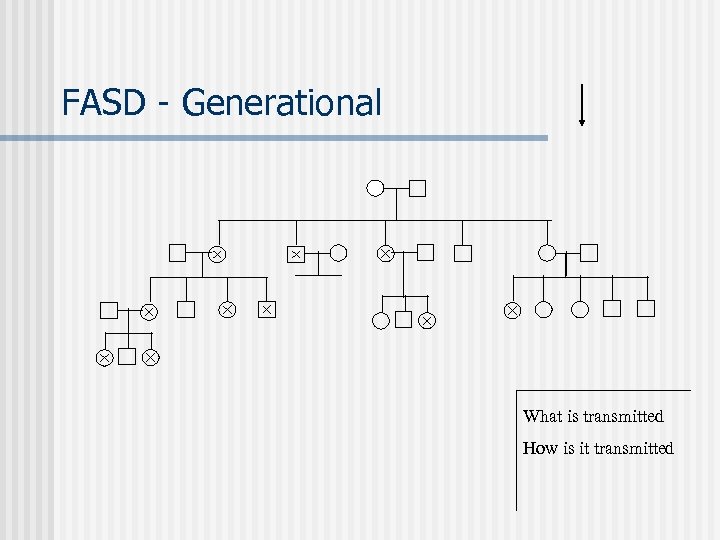
FASD - Generational What is transmitted How is it transmitted
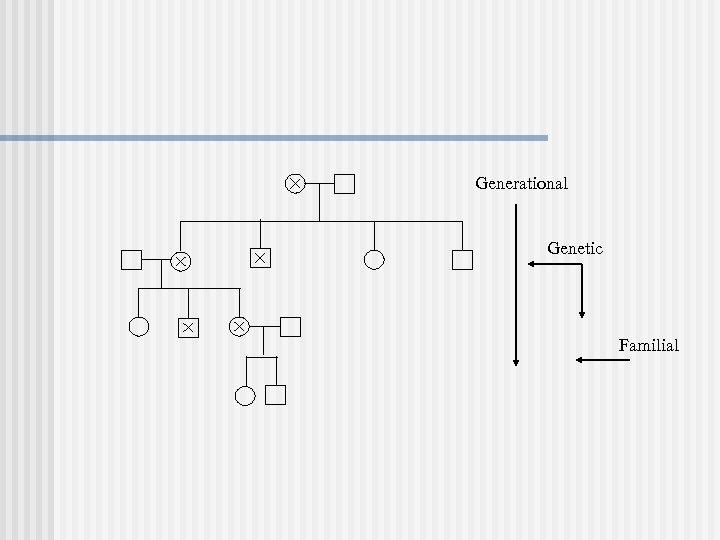
Generational Genetic Familial
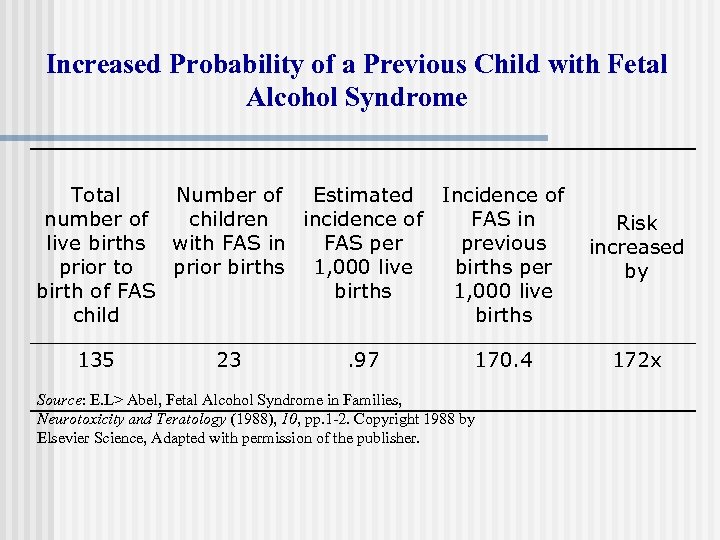
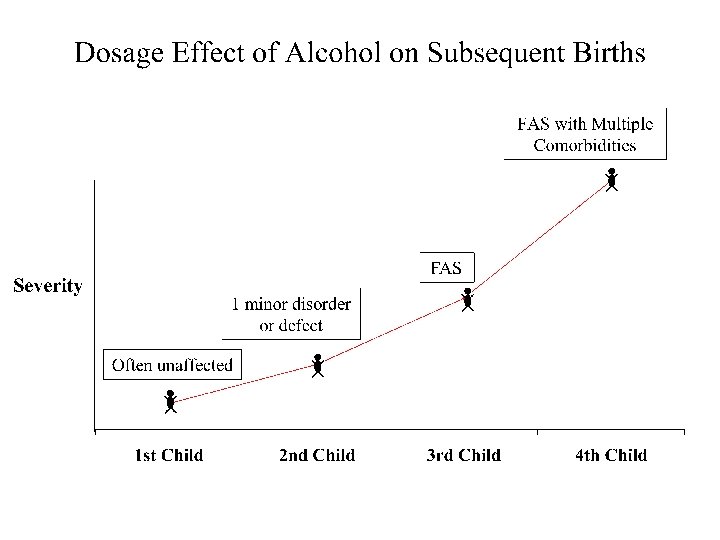
Increased Probability of a Previous Child with Fetal Alcohol Syndrome Total Number of Estimated Incidence of number of children incidence of FAS in live births with FAS in FAS per previous prior to prior births 1, 000 live births per birth of FAS births 1, 000 live child births 135 23 . 97 170. 4 Source: E. L> Abel, Fetal Alcohol Syndrome in Families, Neurotoxicity and Teratology (1988), 10, pp. 1 -2. Copyright 1988 by Elsevier Science, Adapted with permission of the publisher. Risk increased by 172 x
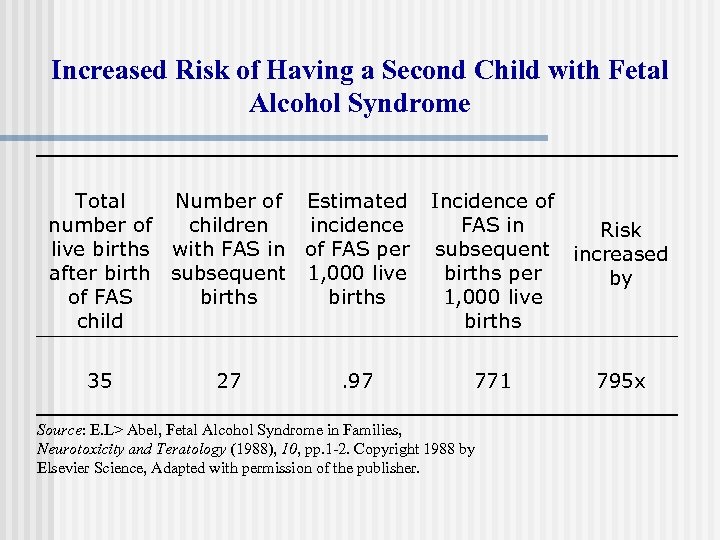
Increased Risk of Having a Second Child with Fetal Alcohol Syndrome Total Number of Estimated number of children incidence live births with FAS in of FAS per after birth subsequent 1, 000 live of FAS births child 35 27 . 97 Incidence of FAS in Risk subsequent increased births per by 1, 000 live births 771 Source: E. L> Abel, Fetal Alcohol Syndrome in Families, Neurotoxicity and Teratology (1988), 10, pp. 1 -2. Copyright 1988 by Elsevier Science, Adapted with permission of the publisher. 795 x
Mortality
Mortality in a Ten-Year Follow. Up of FAS Children 18% cases 27% of the Mothers (Streissguth, 1985)
Diagnosis of People with Adverse Outcome from Prenatal Alcohol Exposure Specific Pattern of Malformations. Confirmed History of Maternal Alcohol Use-Abuse. Specific Pattern of Neurocognitive Deficits.
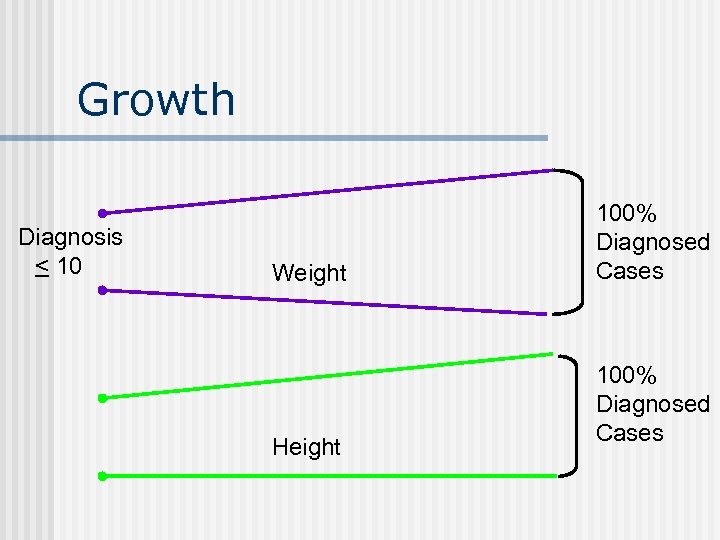
Growth Diagnosis < 10 Weight Height 100% Diagnosed Cases
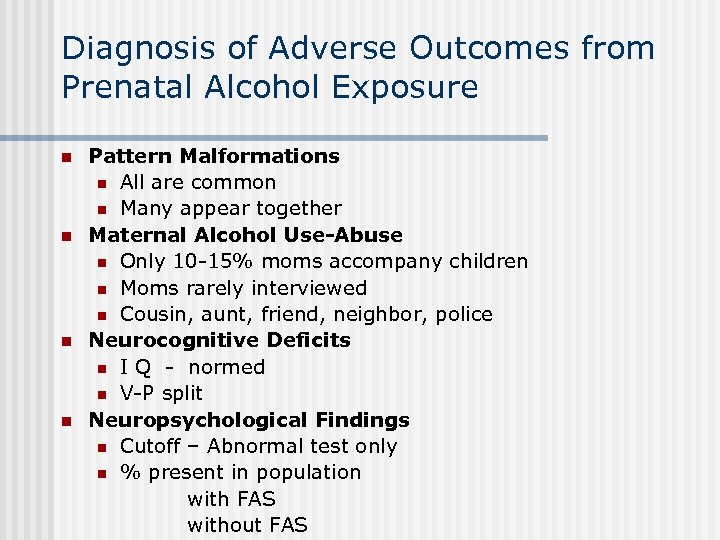
Diagnosis of Adverse Outcomes from Prenatal Alcohol Exposure n n Pattern Malformations n All are common n Many appear together Maternal Alcohol Use-Abuse n Only 10 -15% moms accompany children n Moms rarely interviewed n Cousin, aunt, friend, neighbor, police Neurocognitive Deficits n I Q - normed n V-P split Neuropsychological Findings n Cutoff – Abnormal test only n % present in population with FAS without FAS
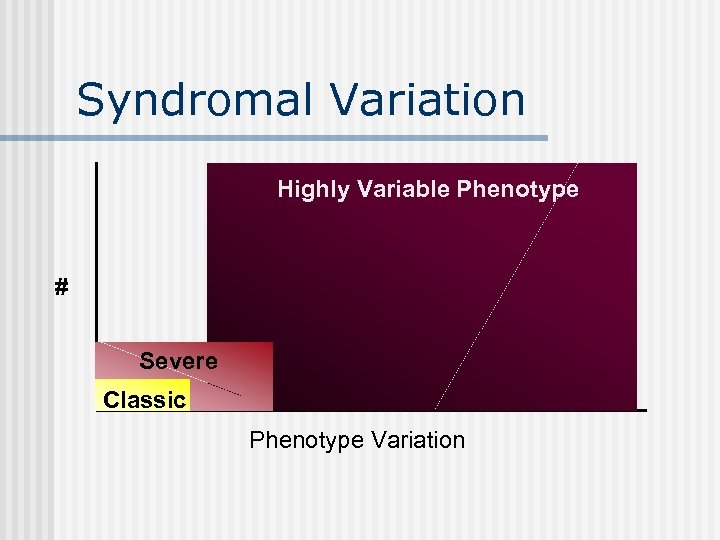
Syndromal Variation Highly Variable Phenotype # Severe Classic Phenotype Variation
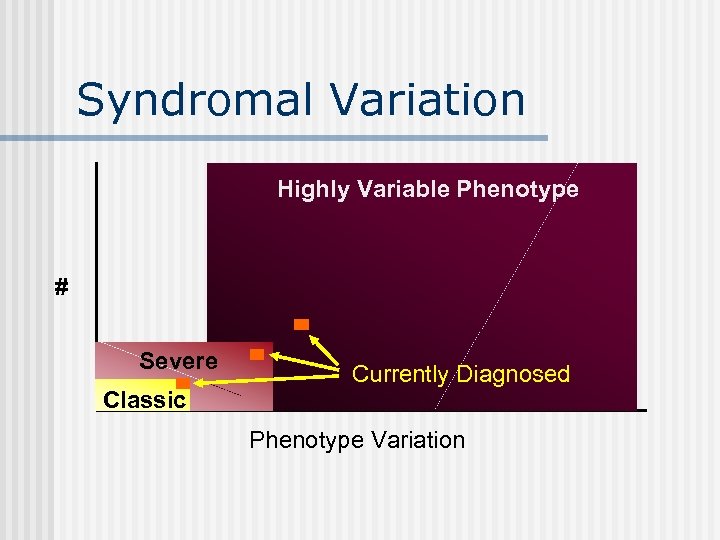
Syndromal Variation Highly Variable Phenotype # Severe Classic Currently Diagnosed Phenotype Variation
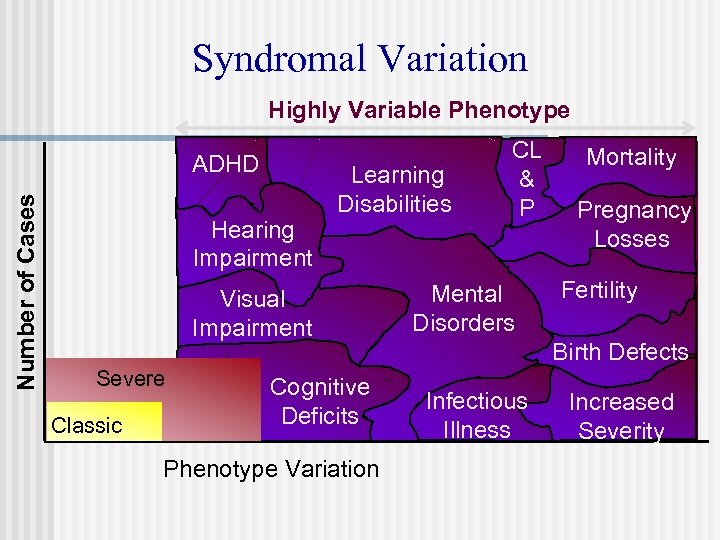
Syndromal Variation Highly Variable Phenotype Number of Cases ADHD Hearing Impairment Learning Disabilities Visual Impairment Severe Classic Cognitive Deficits Phenotype Variation CL & P Mental Disorders Mortality Pregnancy Losses Fertility Birth Defects Infectious Illness Increased Severity
No leaves Smooth bark “I found one! It’s the only tree here, but I expected to find a whole forest. . ” FAS Too big Too small House, not tree Trunk too Looks like thick Family Has fruit Has needles Poor soil
We have exact standards for trees. We do not want to label or stigmatize.

Inaccurate Diagnosis: Stigmatization of Mother Labeling of Child Diagnostic Imprecision • Parents • Schools • Doctors • Epidemiologist • Apathy
Consequences of Misdiagnosis Public Health § Inaccurate Prevalence Outcome § Causal Factors § Cost Estimates § Service Systems
Consequences of Misdiagnosis Mothers § Recurrence § Health § Death § Guilt § Search for what’s wrong

Consequences of Misdiagnosis Child § Misunderstood Behavior § Inappropriate Treatment § Secondary Disabilities § Jail § Substance Abuse § Multiple Foster Homes § Unnecessary testing
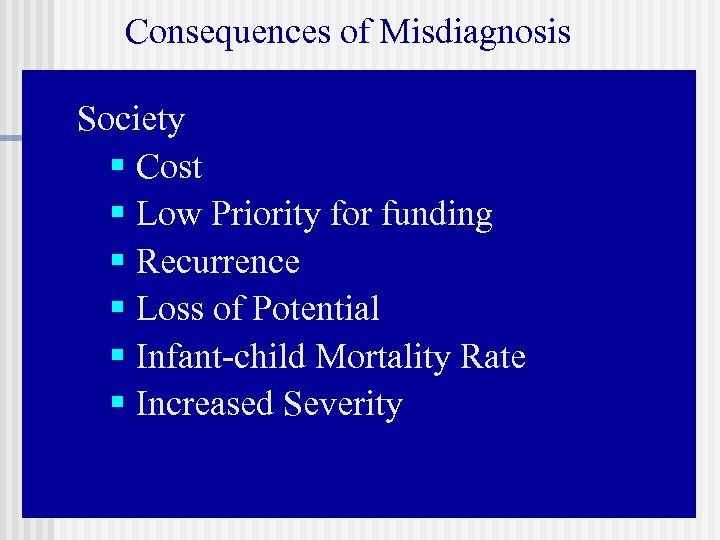
Consequences of Misdiagnosis Society § Cost § Low Priority for funding § Recurrence § Loss of Potential § Infant-child Mortality Rate § Increased Severity
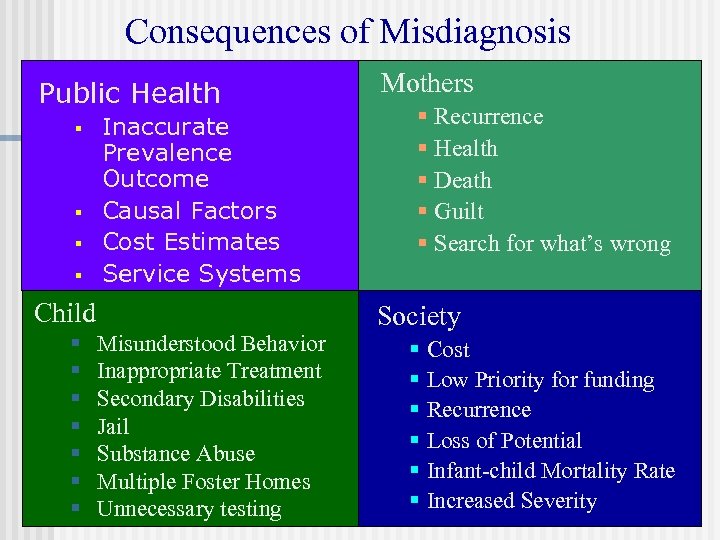
Consequences of Misdiagnosis Public Health § § Inaccurate Prevalence Outcome Causal Factors Cost Estimates Service Systems Child § § § § Misunderstood Behavior Inappropriate Treatment Secondary Disabilities Jail Substance Abuse Multiple Foster Homes Unnecessary testing Mothers § Recurrence § Health § Death § Guilt § Search for what’s wrong Society § § § Cost Low Priority for funding Recurrence Loss of Potential Infant-child Mortality Rate Increased Severity
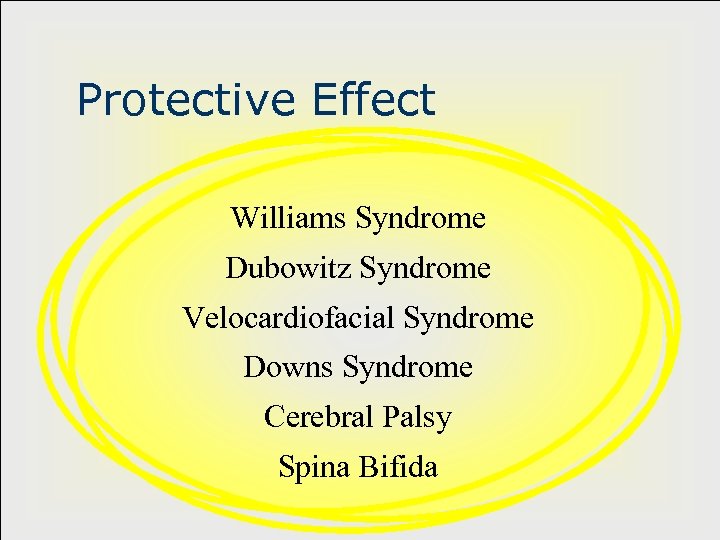
Protective Effect Williams Syndrome Dubowitz Syndrome Velocardiofacial Syndrome Downs Syndrome Cerebral Palsy Spina Bifida
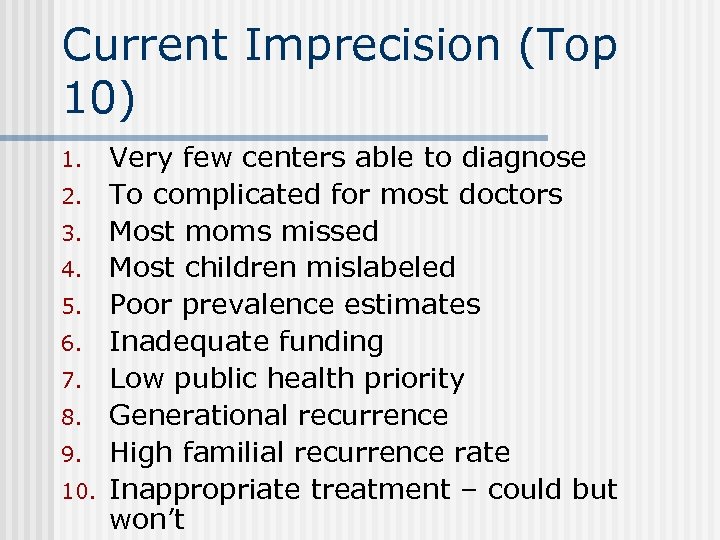
Current Imprecision (Top 10) 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Very few centers able to diagnose To complicated for most doctors Most moms missed Most children mislabeled Poor prevalence estimates Inadequate funding Low public health priority Generational recurrence High familial recurrence rate Inappropriate treatment – could but won’t
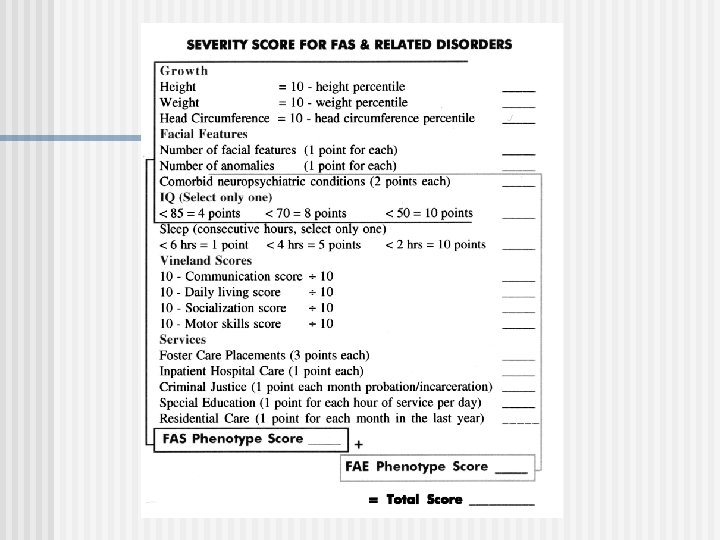
Co-Morbidity Weighting n Multiple Events n Impact assessment n
Preferred Performance Characteristics 1. 2. 3. 4. 5. 6. 7. 8. Captures many – most cases Reflects understanding of comorbidity Does not exert a protective effect Easy to implement Leads to prevention of recurrence Protects mother Decreases secondary disability Leads to appropriate interventions
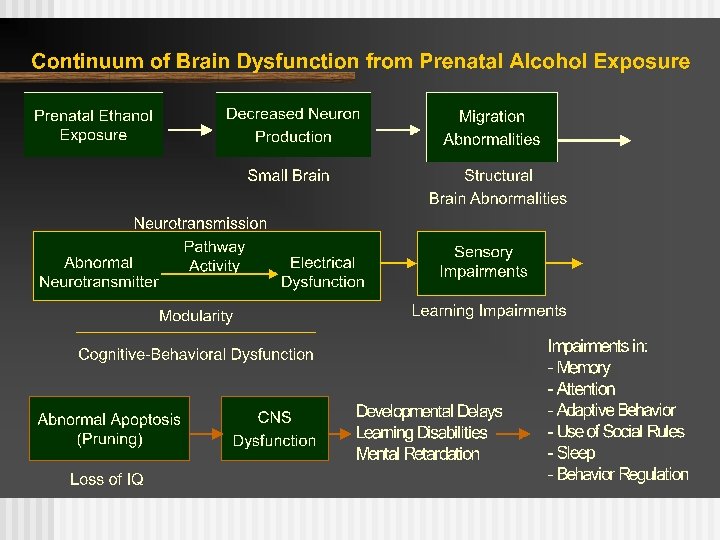
Impairments in: • Memory • Attention • Adaptive behavior • Use of social rules • Sleep • Behavior regulation
3f6525a0b165f4aa17561b030bc90a75.ppt