f58cdf8f01a125282ce5491b1e159187.ppt
- Количество слайдов: 105
PHARMACOTHERAPY OF DRUGS USED IN BRONCHIAL ASTHMA & COPD By Prof. M. ABDELAZIZ
Disorders of Respiratory Function Main disorders of the respiratory system are : 1. Bronchial asthma 2. Cough 3. Allergic rhinitis 4. Chronic obstructive pulmonary disease (COPD, also called emphysema)
Asthma is a chronic inflammatory disorder of bronchial airways that result in airway obstruction in response to external stimuli (as pollen grains, cold air and tobacco smoke).
Characters of airways in asthmatic patients : Airway hyper-reactivity: abnormal sensitivity of the airways to wide range of external stimuli. Inflammation • Swelling • Thick mucus production. Bronchospasm (constriction of the bronchial muscles).
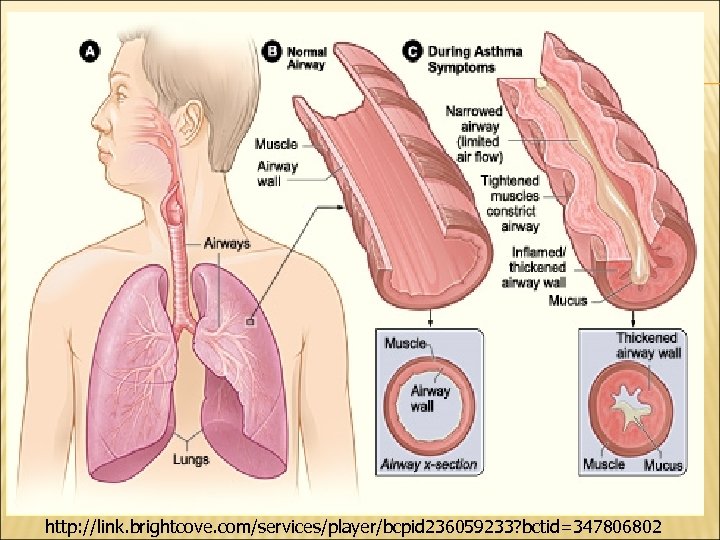
http: //link. brightcove. com/services/player/bcpid 236059233? bctid=347806802
Symptoms of asthma Asthma produces recurrent episodic attack of § Acute bronchoconstriction § Shortness of breath § Chest tightness § Wheezing § Rapid respiration § Cough Symptoms can happen each time the airways are irritated by inhaled irritants or allergens.
Causes § § § § Infection Emotional conditions Stress Exercise Pets Seasonal changes Some drugs as aspirin, β bockers
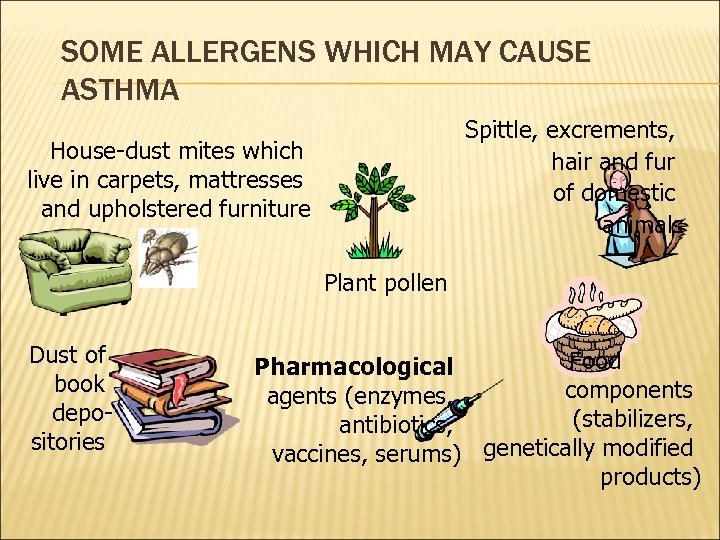
SOME ALLERGENS WHICH MAY CAUSE ASTHMA Spittle, excrements, hair and fur of domestic animals House-dust mites which live in carpets, mattresses and upholstered furniture Plant pollen Dust of book depositories Food Pharmacological components agents (enzymes, (stabilizers, antibiotics, vaccines, serums) genetically modified products)
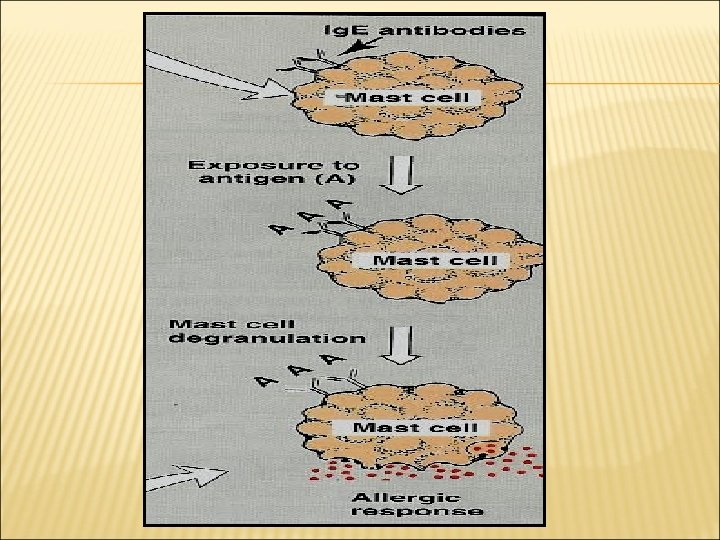
PATHOPHYSIOLOGY Asthma pathophysiology is quite difficult and insufficiently studied. Undoubtedly, in most cases the disease is based on 1 type hypersensitivity reaction. The genesis of any allergic reaction may be divided into immune, pathochemical and pathophysio-logic phases.
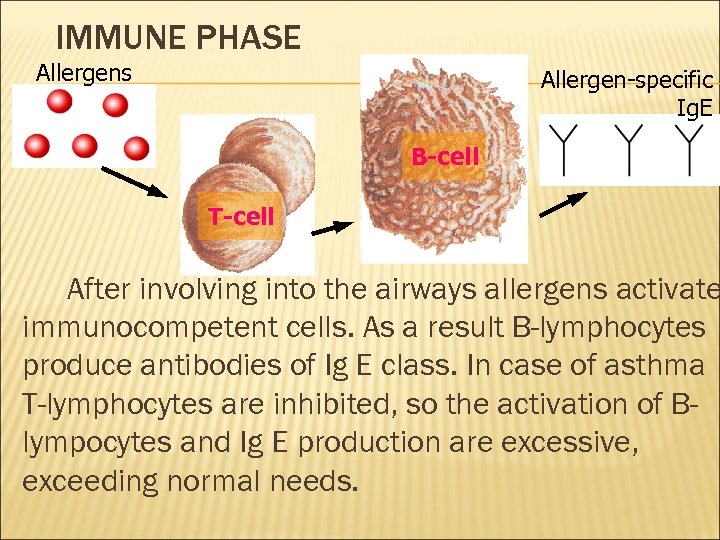
IMMUNE PHASE Allergens Allergen-specific Ig. E B-cell T-cell After involving into the airways allergens activate immunocompetent cells. As a result B-lymphocytes produce antibodies of Ig E class. In case of asthma T-lymphocytes are inhibited, so the activation of Blympocytes and Ig E production are excessive, exceeding normal needs.
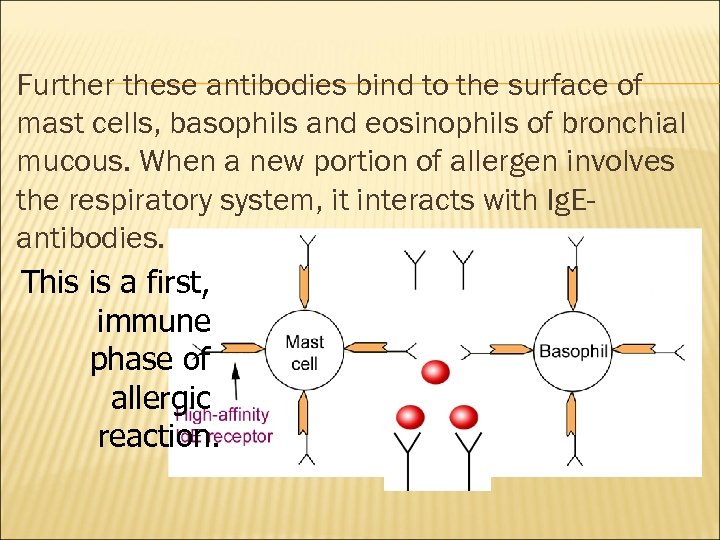
Further these antibodies bind to the surface of mast cells, basophils and eosinophils of bronchial mucous. When a new portion of allergen involves the respiratory system, it interacts with Ig. Eantibodies. This is a first, immune phase of allergic reaction.
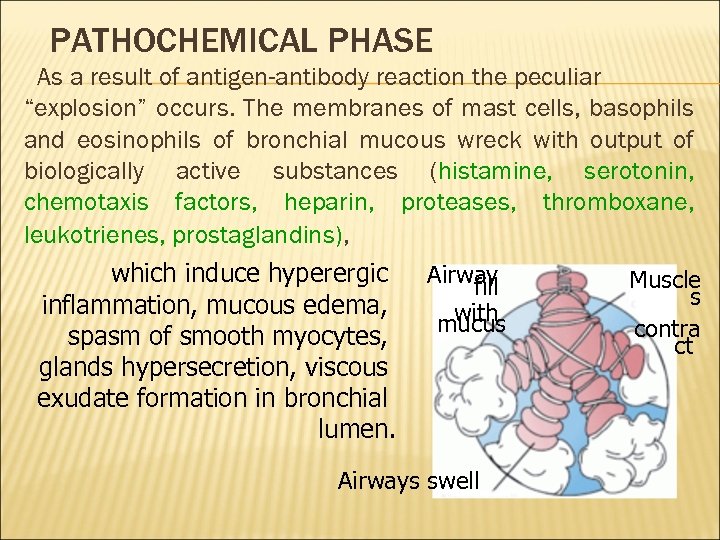
PATHOCHEMICAL PHASE As a result of antigen-antibody reaction the peculiar “explosion” occurs. The membranes of mast cells, basophils and eosinophils of bronchial mucous wreck with output of biologically active substances (histamine, serotonin, chemotaxis factors, heparin, proteases, thromboxane, leukotrienes, prostaglandins), which induce hyperergic inflammation, mucous edema, spasm of smooth myocytes, glands hypersecretion, viscous exudate formation in bronchial lumen. Airway fill with mucus Airways swell Muscle s contra ct
Asthma exacerbation, occurring as a result, is a clinical manifestation of the 3 rd, pathophysiolo-gical, phase of allergic reaction. The indicated mechanism is specific for atopic (exogenous) asthma genesis. In addition to this, autosensibilization of damaged pulmonary tissue, neuropsychic disturbances, corticoid insufficiency, adrenergic imbalance, impairment of arachidonic acid metabolism, genetic and some other factors probably play a certain role in genesis of nonatopic (endogenous) asthma.
CLASSIFICATION asthma is divided into: Depending on etiology 1 - exogenous (atopic) 2 - and endogenous (non-atopic). By clinical course asthma is divided into 1 - intermittent (beginning, early) 2 -and persistent (chronic, late). Depending on frequency of exacerbations, limitations of patient’s physical activity and lung function persistent asthma is divided into: mild, moderate and severe (lung function is assessed by forced expiratory volume in 1 second (FEV 1) and peak expiratory flow (PEF) and daily variability of these parameters). There also remission phase and exacerbations.
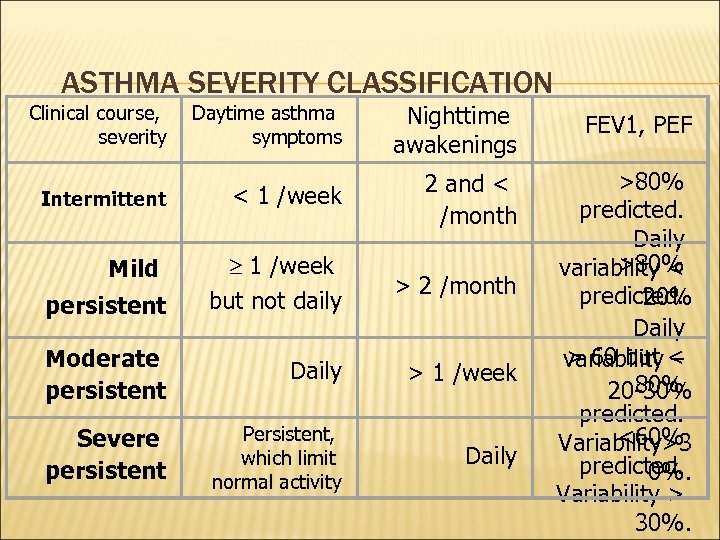
ASTHMA SEVERITY CLASSIFICATION Clinical course, severity Daytime asthma symptoms Nighttime awakenings FEV 1, PEF Intermittent < 1 /week 2 and < /month 1 /week but not daily > 2 /month Moderate persistent Daily > 1 /week Severe persistent Persistent, which limit normal activity Daily >80% predicted. Daily >80% variability < predicted. 20% Daily > 60 but – variability < 80% 20 -30% predicted. <60% Variability>3 predicted. 0%. Variability > 30%. Mild persistent
In recommendations of Global Initiative for Asthma (GINA) asthma is classified on the base of control assessment and is divided into well-controlled, partially controlled and uncontrolled. Asthma control is considered as: daytime symptoms 2 /week; ability to engage in normal daily activity; the absence of nighttime awakenings as a result of asthma symptoms; need in bronchodilators administration 2 /week; the absence of asthma exacerbations; normal or near normal lung function parameters.
CLINICAL MANIFESTATIONS Classic signs and symptoms of asthma are: attacks of expiratory dyspnea shortness of breath cough chest tightness wheezing (high-pitched whistling sounds when breathing out) sibilant rales
In typical cases in development of asthma exacerbation there are 3 periods – prodromal period, the height period and the period of reverse changes. At the prodromal period: vasomotoric nasal reaction with profuse watery discharge, sneezing, dryness in nasopharynx, paroxysmal cough with viscous sputum, emotional lability, excessive sweating, skin itch and other symptoms may occur.
At the peack of exacerbation there are: expiratory dyspnea forced position with supporting on arms poorly productive cough cyanotic skin and mucous tunics hyperexpansion of thorax with use of all accessory muscles during breathing at lung percussion: tympanitis, shifted downward lung borders at auscultation: diminished breath sounds, sibilant rales, prolonged breathing-out, tachycardia. in severe exacerbations: the signs of right-sided heart failure (swollen neck veins, hepatomegalia), overload of right heart chambers on ECG.
At the period of the reverse changes, which comes spontaneously or under pharmacologic therapy, dyspnea and breathlessness relieve or disappear, sputum becomes not so viscous, cough turns to be productive, patient breathes easier.
ASTHMATIC STATUS The severe and prolonged asthma exacerbation with intensive progressive respiratory failure, hypoxemia, hypercapnia, respiratory acidosis, increased blood viscosity and the most important sign is blockade of bronchial b 2 -receptors. Stages: 1 st - refractory response to b 2 -agonists (may be paradoxical reaction with bronchospasm aggravation) 2 nd - “silent” lung because of severe bronchial obstruction and collapse of small and intermediate bronchi; 3 rd stage – the hypercapnic coma.
In many cases asthma, particularly intermittent, manifests with few and atypical signs: episodic appearance of wheezing; cough, heavy breathing occurring at night; cough, hoarseness after physical activity; “seasonal” cough, wheezing, chest tightness (e. g. , during pollen period of ambrosia); the same symptoms occurring during contact with allergens, irritants; lingering course of acute respiratory infections.
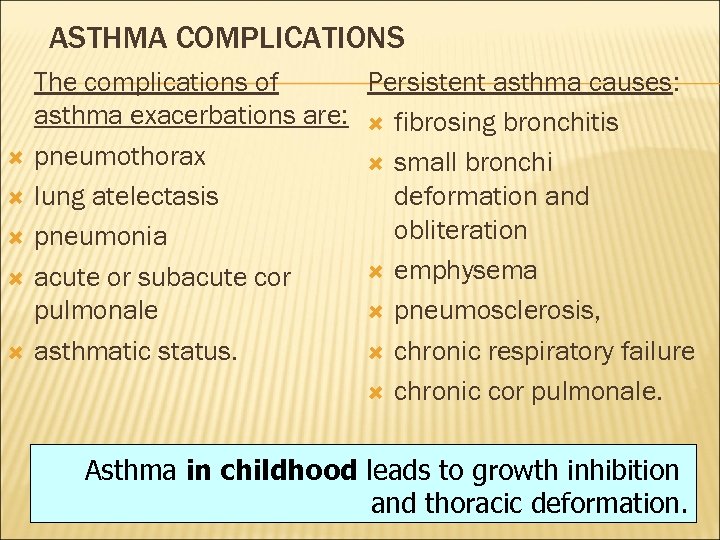
ASTHMA COMPLICATIONS The complications of Persistent asthma causes: asthma exacerbations are: fibrosing bronchitis pneumothorax small bronchi lung atelectasis deformation and obliteration pneumonia emphysema acute or subacute cor pulmonale pneumosclerosis, asthmatic status. chronic respiratory failure chronic cor pulmonale. Asthma in childhood leads to growth inhibition and thoracic deformation.
INVESTIGATIONS Lab Data Eosinophilia, moderate leukocytosis in blood count as well as increased serum level of Ig E can be found in patients with asthma, especially at asthma exacerbations. Inflammatory cells, Curschmann's spirals (viscous mucus which copies small bronchi) and Charcot-Leyden crystals (crystallized enzymes of eosinophils and mast cells) can be observed in sputum.
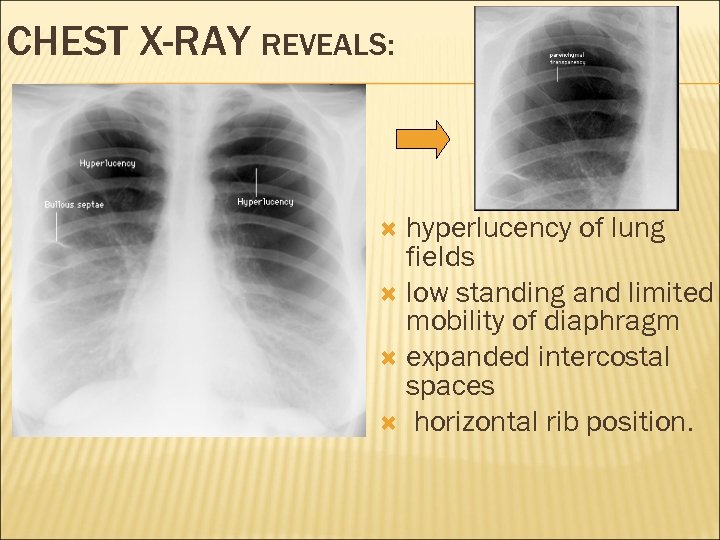
CHEST X-RAY REVEALS: hyperlucency of lung fields low standing and limited mobility of diaphragm expanded intercostal spaces horizontal rib position.
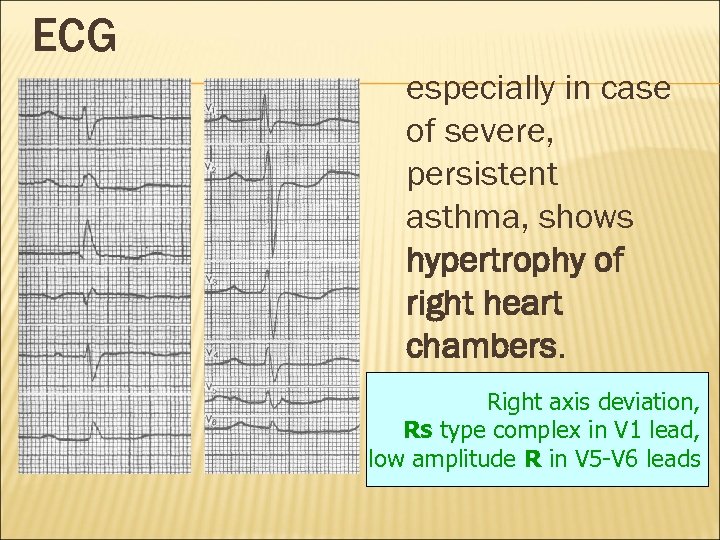
ECG especially in case of severe, persistent asthma, shows hypertrophy of right heart chambers. Right axis deviation, Rs type complex in V 1 lead, low amplitude R in V 5 -V 6 leads
CLASSIFICATION OF ASTHMA Mild Intermittent Asthma Mild Persistent Asthma Moderate Persistent Asthma Severe Persistent Asthma
LUNG FUNCTION ASSESSMENT The diagnosis and severity assessment of asthma is based mainly on parameters of lung function. The most important of them are: forced expiratory volume in 1 second (FEV 1) and peak expiratory flow (PEF), which are measured during spirometry at forced breathing-out.
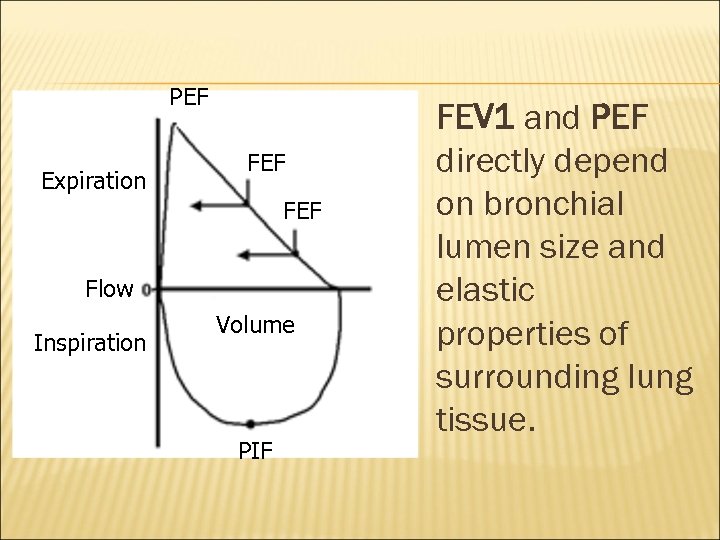
PEF Expiration FEF Flow Inspiration Volume PIF FEV 1 and PEF directly depend on bronchial lumen size and elastic properties of surrounding lung tissue.
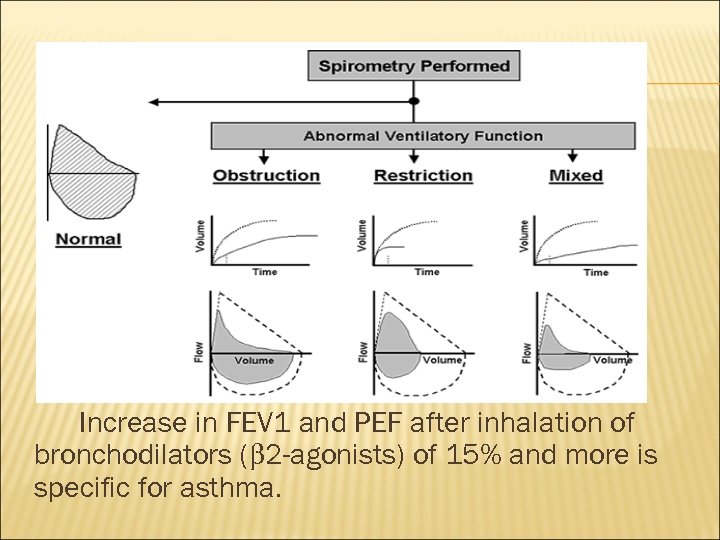
Increase in FEV 1 and PEF after inhalation of bronchodilators (b 2 -agonists) of 15% and more is specific for asthma.
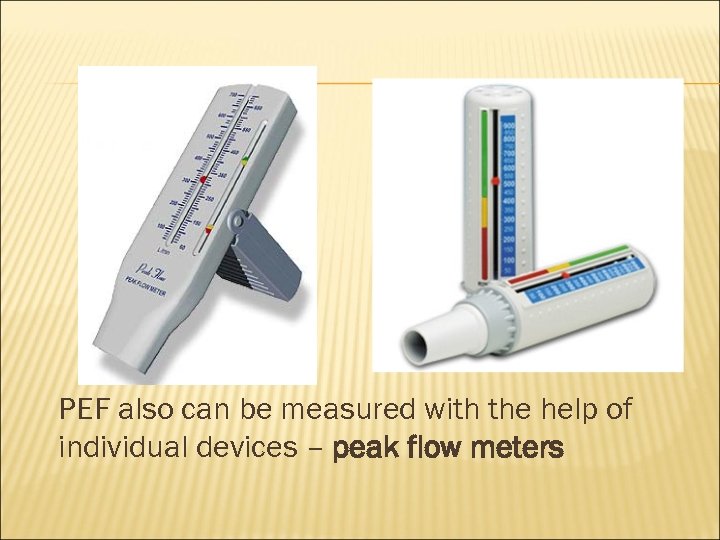
PEF also can be measured with the help of individual devices – peak flow meters
DIAGNOSIS Typical clinical manifestations and lung function assessment are sufficient for diagnosis of asthma.
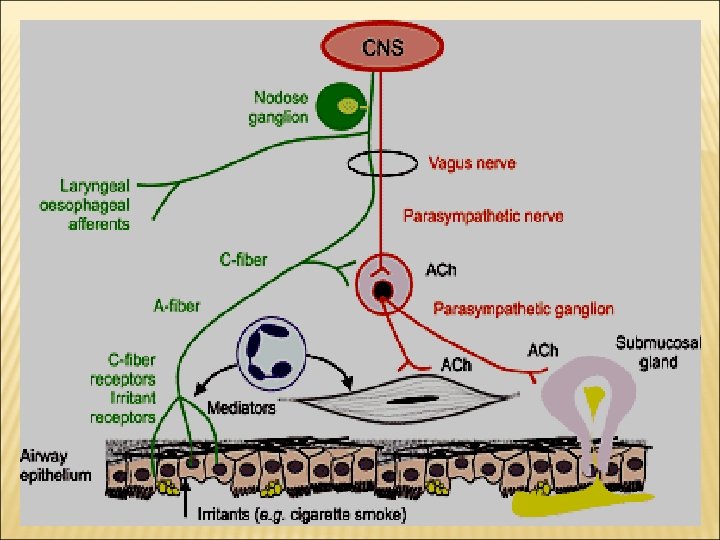
Airways Innervations Afferent nerves (sensory) Ø Ø Irritant receptors in upper airways. C-fiber receptors in lower airways. Stimulated by : Exogenous chemicals Physical stimuli (cold air) Endogenous inflammatory mediators
Efferent nerves (motor) Ø Parasympathetic supply M 3 receptors in smooth muscles and glands. Ø No sympathetic supply but B 2 receptors in smooth muscles and glands
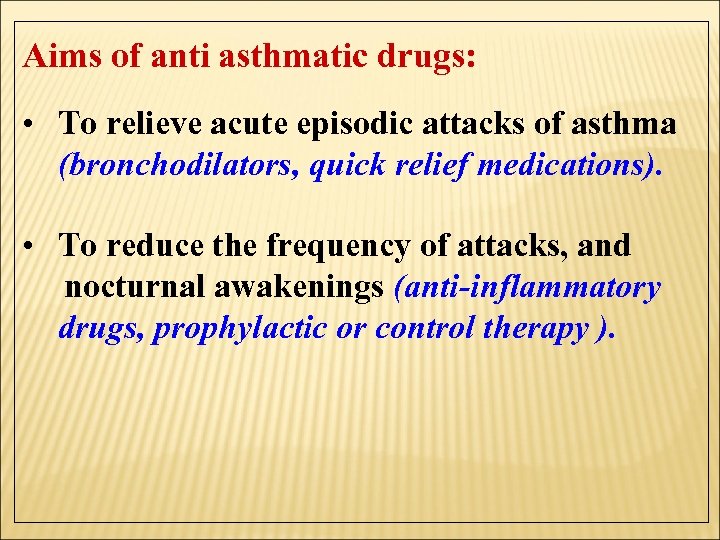
Aims of anti asthmatic drugs: • To relieve acute episodic attacks of asthma (bronchodilators, quick relief medications). • To reduce the frequency of attacks, and nocturnal awakenings (anti-inflammatory drugs, prophylactic or control therapy ).
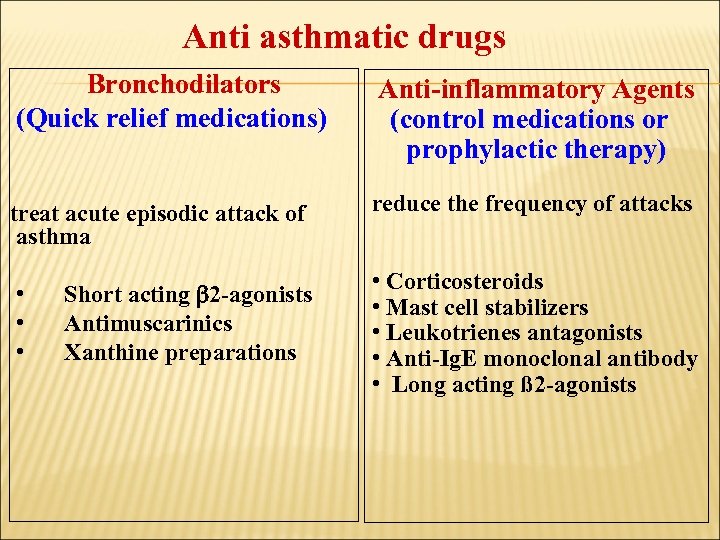
Anti asthmatic drugs Bronchodilators (Quick relief medications) treat acute episodic attack of asthma • • • Short acting 2 -agonists Antimuscarinics Xanthine preparations Anti-inflammatory Agents (control medications or prophylactic therapy) reduce the frequency of attacks • Corticosteroids • Mast cell stabilizers • Leukotrienes antagonists • Anti-Ig. E monoclonal antibody • Long acting ß 2 -agonists
Anti asthmatic drugs Bronchodilators : (Quick relief medications) are used to relieve acute attack of bronchoconstriction 1. 2 - adrenoreceptor agonists 2. Antimuscarinics 3. Xanthine preparations
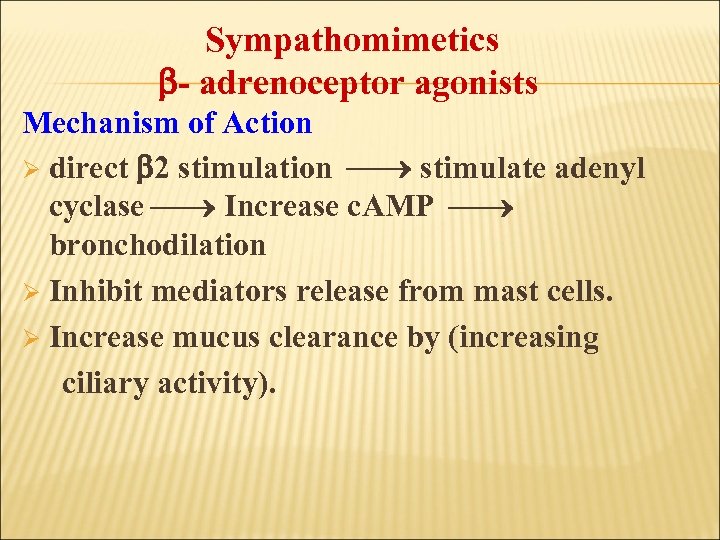
Sympathomimetics - adrenoceptor agonists Mechanism of Action Ø direct 2 stimulation stimulate adenyl cyclase Increase c. AMP bronchodilation Ø Inhibit mediators release from mast cells. Ø Increase mucus clearance by (increasing ciliary activity).
Classification of agonists Ø Non selective agonists: epinephrine - isoprenaline Selective 2 – agonists (Preferable). Salbutamol (albuterol) Terbutaline Salmeterol Formeterol Ø
Non selective -agonists. Epinephrine Potent bronchodilator rapid action (maximum effect within 15 min). S. C. or by inhalation (aerosol or nebulizer). Has short duration of action (60 -90 min) Drug of choice for acute anaphylaxis (hypersensitivity reactions).

Nebulizer Inhaler
Disadvantages Not effective orally. Ø Hyperglycemia Ø CVS side effects: tachycardia, arrhythmia, hypertension Ø Skeletal muscle tremor Ø Not suitable for asthmatic patients with hypertension or heart failure. Ø Contraindication: CVS patients, diabetic patients
Selective 2 –agonists Ø Ø Ø drugs of choice for acute attack of asthma Are mainly given by inhalation (metered dose inhaler or nebulizer). Can be given orally, parenterally. Short acting ß 2 agonists e. g. salbutamol, terbutaline Long acting ß 2 agonists e. g. salmeterol, formeterol
Short acting ß 2 agonists Salbutamol, inhalation, orally, i. v. Terbutaline, inhalation, orally, s. c. Ø Have rapid onset of action (15 -30 min). Ø short duration of action (4 -6 hr) Ø used for symptomatic treatment of acute episodic attack of asthma.
Long acting selective ß 2 agonists Salmeterol & formoterol: Ø Long acting bronchodilators (12 hours) Ø have high lipid solubility (creates depot effect) Ø are given by inhalation Ø are not used to relieve acute episodes of asthma Ø used for nocturnal asthma (long acting relievers). Ø combined with inhaled corticosteroids to control asthma (decreases the number and severity of asthma attacks). Ø
Advantages of ß 2 agonists Ø Minimal CVS side effects Ø suitable for asthmatic patients with hypertension or heart failure. Disadvantages of ß 2 agonists Ø Skeletal muscle tremors. Ø Nervousness Ø Tolerance (B-receptors down regulation). Ø Tachycardia over dose (B 1 -stimulation).
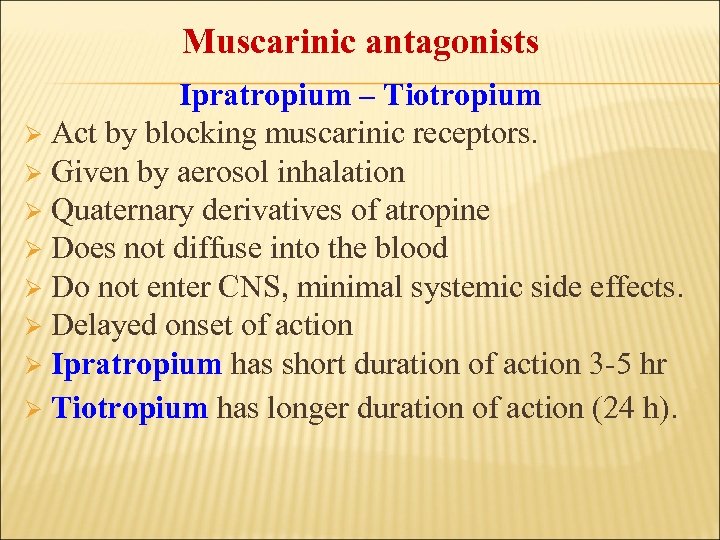
Muscarinic antagonists Ipratropium – Tiotropium Ø Act by blocking muscarinic receptors. Ø Given by aerosol inhalation Ø Quaternary derivatives of atropine Ø Does not diffuse into the blood Ø Do not enter CNS, minimal systemic side effects. Ø Delayed onset of action Ø Ipratropium has short duration of action 3 -5 hr Ø Tiotropium has longer duration of action (24 h).
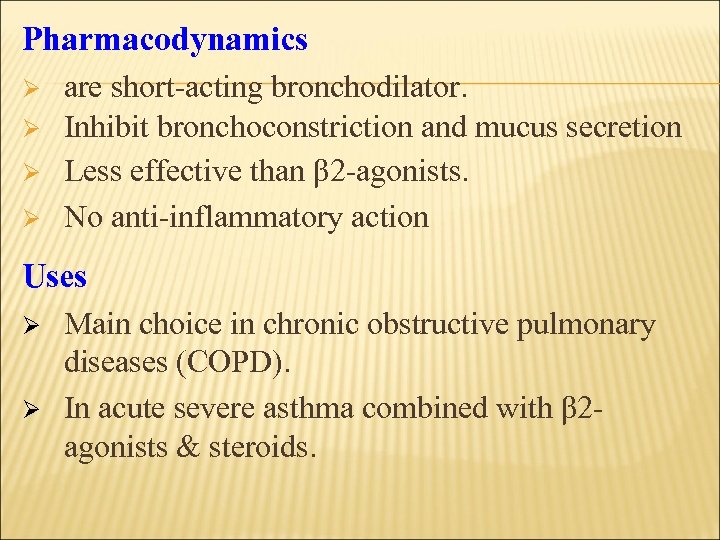
Pharmacodynamics Ø Ø are short-acting bronchodilator. Inhibit bronchoconstriction and mucus secretion Less effective than β 2 -agonists. No anti-inflammatory action Uses Ø Ø Main choice in chronic obstructive pulmonary diseases (COPD). In acute severe asthma combined with β 2 agonists & steroids.
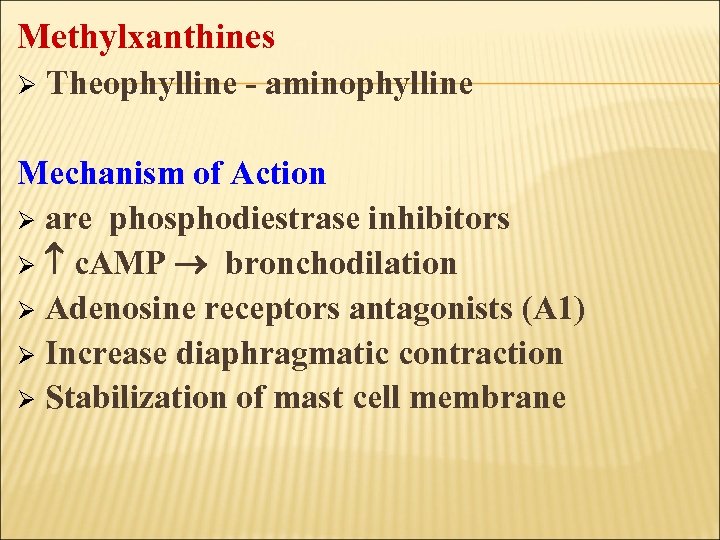
Methylxanthines Ø Theophylline - aminophylline Mechanism of Action Ø are phosphodiestrase inhibitors Ø c. AMP bronchodilation Ø Adenosine receptors antagonists (A 1) Ø Increase diaphragmatic contraction Ø Stabilization of mast cell membrane
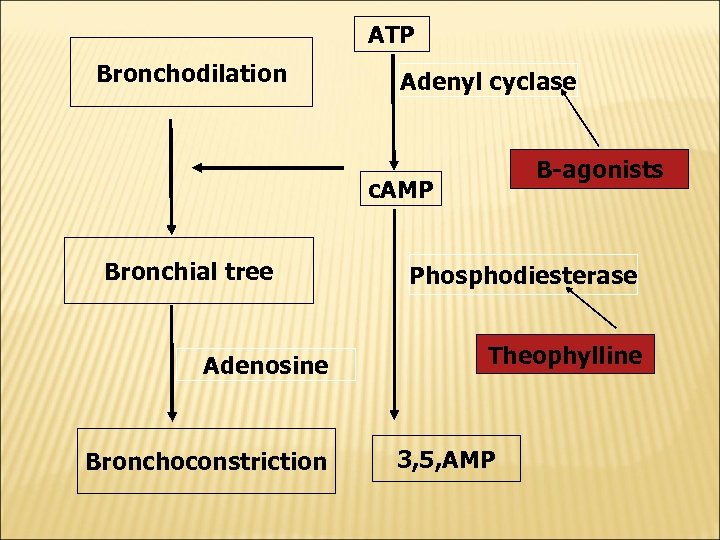
ATP Bronchodilation Adenyl cyclase B-agonists c. AMP Bronchial tree Adenosine Bronchoconstriction Phosphodiesterase Theophylline 3, 5, AMP
Pharmacological effects : ØBronchial muscle relaxation Ø contraction of diaphragm improve ventilation CVS: ↑ heart rate, ↑ force of contraction GIT: ↑ gastric acid secretions Kidney: ↑renal blood flow, weak diuretic action CNS stimulation * stimulant effect on respiratory center. * decrease fatigue & elevate mood. * overdose (tremors, nervousness, insomnia, convulsion)
Pharmacokinetics Ø metabolized by Cyt P 450 enzymes in liver ØT ½= 8 hours Øhas many drug interactions Ø Enzyme inducers: as phenobarbitone- rifampicin → ↑metabolism of theophylline → ↓ T ½. Ø Enzyme inhibitors: as erythromycin→ ↓ metabolism of theophylline → ↑T ½.
Uses Ø Second line drug in asthma (theophylline) Ø For status asthmatics (aminophylline, is given as slow infusion). Side Effects Ø Low therapeutic index narrow safety margin monitoring of theophylline blood level is necessary. Ø CVS effects: hypotension, arrhythmia. Ø GIT effects: nausea & vomiting Ø CNS side effects: tremors, nervousness, insomnia, convulsion
Anti - inflammatory agents include: Glucocorticoids Ø Leukotrienes antagonists Ø Mast cell stabilizers Ø Anti-Ig. E monoclonal antibody (omalizumab) Ø
Anti - inflammatory Agents: (control medications / prophylactic therapy) reduce the number of inflammatory cells in the airways and prevent blood vessels from leaking fluid into the airway tissues. By reducing inflammation, they reduce the spasm of airways & bronchial hyper-reactivity.
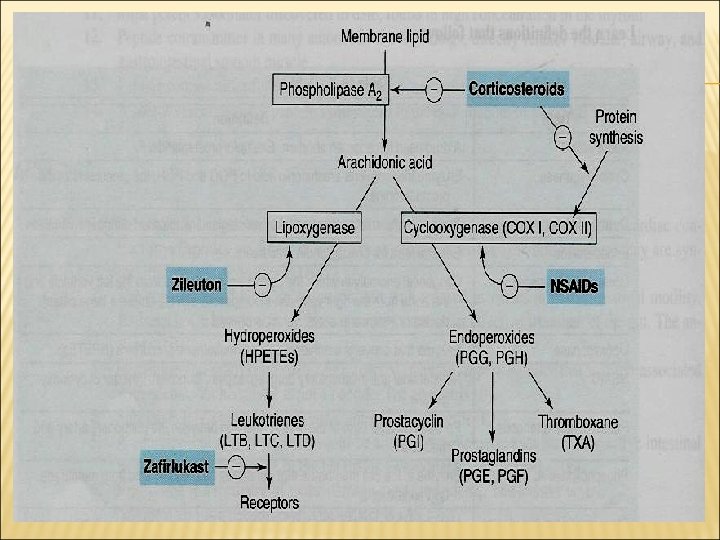
Glucocorticoids Mechanism of action Ø Ø Ø Ø Inhibition of phospholipase A 2 ↓ prostaglandin and leukotrienes ↓ Number of inflammatory cells in airways. Mast cell stabilization →↓ histamine release. ↓ capillary permeability and mucosal edema. Inhibition of antigen-antibody reaction. Upregulate β 2 receptors (have additive effect to B 2 agonists).
Pharmacological actions of glucocorticoids Ø Ø Ø Anti-inflammatory actions Immunosuppressant effects Metabolic effects – – – Ø Hyperglycemia ↑ protein catabolism, ↓ protein anabolism Stimulation of lipolysis - fat redistribution Mineralocorticoid effects: sodium/fluid retention – Increase potassium excretion (hypokalemia) – Increase blood volume (hypertension) –
Ø Ø Behavioral changes: depression Bone loss (osteoporosis) due to Inhibit bone formation ↓ calcium absorption.
Routes of administration Inhalation: e. g. Budesonide & Fluticasone, beclometasone Ø Given by inhalation, given by metered-dose inhaler Have first pass metabolism Best choice in asthma, less side effects Ø Ø Orally: Prednisone, methyl prednisolone Injection: Hydrocortisone, dexamethasone
Glucocorticoids in asthma § Are not bronchodilators § Reduce bronchial inflammation § Reduce bronchial hyper-reactivity to stimuli § Have delayed onset of action (effect usually attained after 2 -4 weeks). § Maximum action at 9 -12 months. § Given as prophylactic medications, used alone or combined with beta-agonists. § Effective in allergic, exercise, antigen and irritant -induced asthma,
Systemic corticosteroids are reserved for: Status asthmaticus (i. v. ). Inhaled steroids should be considered for adults, children with any of the following features using inhaled β 2 agonists three times/week symptomatic three times/ week or more; or waking one night/week.
Clinical Uses of glucocorticoids 1. Treatment of inflammatory disorders (asthma, rheumatoid arthritis). 2. Treatment of autoimmune disorders (ulcerative colitis, psoriasis) and after organ or bone marrow transplantation. 3. Antiemetics in cancer chemotherapy
Side effects due to systemic corticosteroids Adrenal suppression Growth retardation in children Osteoporosis Fluid retention, weight gain, hypertension Hyperglycemia Susceptibility to infections Glaucoma Cataract Fat distribution, wasting of the muscles Psychosis
Inhalation has very less side effects: Oropharyngeal candidiasis (thrush). Dysphonia (voice hoarseness). Withdrawal Abrupt stop of corticosteroids should be avoided and dose should be tapered (adrenal insufficiency syndrome).
Mast cell stabilizers e. g. Cromolyn (cromoglycate) - Nedocromil Ø act by stabilization of mast cell membrane. Ø given by inhalation (aerosol, microfine powder, nebulizer). ØHave poor oral absorption (10%)
Pharmacodynamics § are Not bronchodilators § Not effective in acute attack of asthma. § Prophylactic anti-inflammatory drug § Reduce bronchial hyper-reactivity. § Effective in exercise, antigen and irritant-induced asthma. § Children respond better than adults
Uses Ø Ø Ø Prophylactic therapy in asthma especially in children. Allergic rhinitis. Conjunctivitis. Side effects Ø Ø Bitter taste minor upper respiratory tract irritation (burning sensation, nasal congestion)
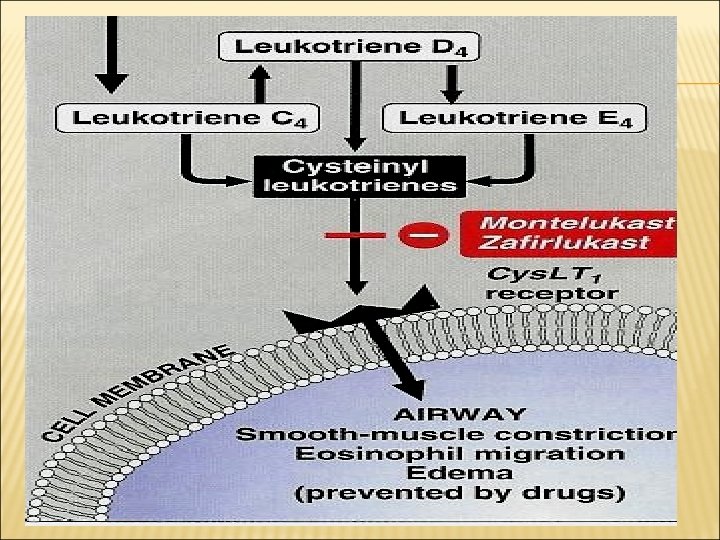
Leukotrienes antagonists Leukotrienes Ø produced by the action of 5 -lipoxygenase on arachidonic acid. Ø Synthesized by inflammatory cells found in the airways (eosinophils, macrophages, mast cells). Ø Leukotriene B 4: chemotaxis of neutrophils Ø Cysteinyl leukotrienes C 4, D 4 & E 4: bronchoconstriction increase bronchial hyper-reactivity mucosal edema, mucus hyper-secretion
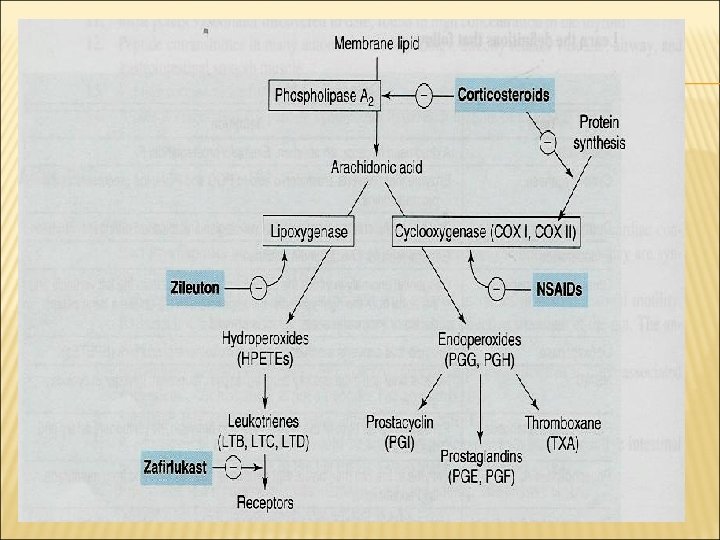
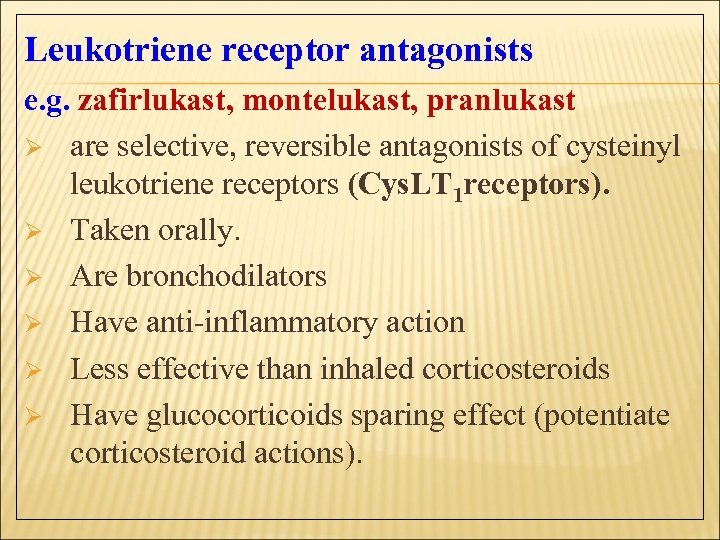
Leukotriene receptor antagonists e. g. zafirlukast, montelukast, pranlukast Ø are selective, reversible antagonists of cysteinyl leukotriene receptors (Cys. LT 1 receptors). Ø Taken orally. Ø Are bronchodilators Ø Have anti-inflammatory action Ø Less effective than inhaled corticosteroids Ø Have glucocorticoids sparing effect (potentiate corticosteroid actions).
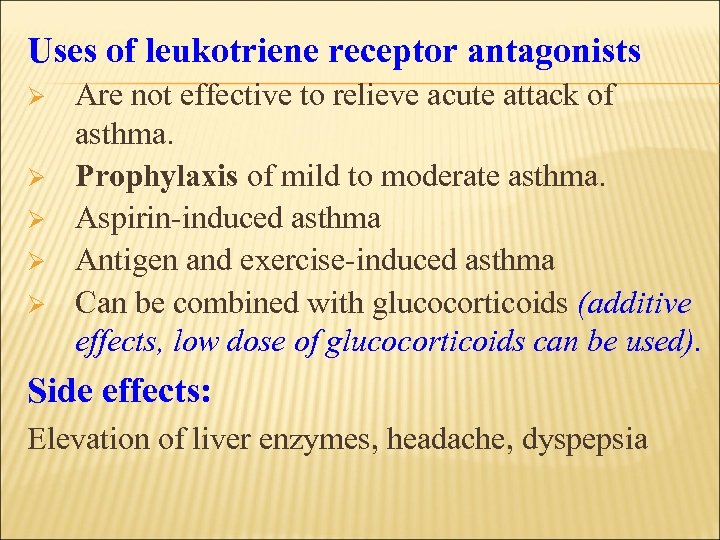
Uses of leukotriene receptor antagonists Ø Ø Ø Are not effective to relieve acute attack of asthma. Prophylaxis of mild to moderate asthma. Aspirin-induced asthma Antigen and exercise-induced asthma Can be combined with glucocorticoids (additive effects, low dose of glucocorticoids can be used). Side effects: Elevation of liver enzymes, headache, dyspepsia
Omalizumab § § § is a monoclonal antibody directed against human Ig. E. prevents Ig. E binding with its receptors on mast cells & basophiles. ↓ release of allergic mediators. used for treatment of allergic asthma. Expensive-not first line therapy.
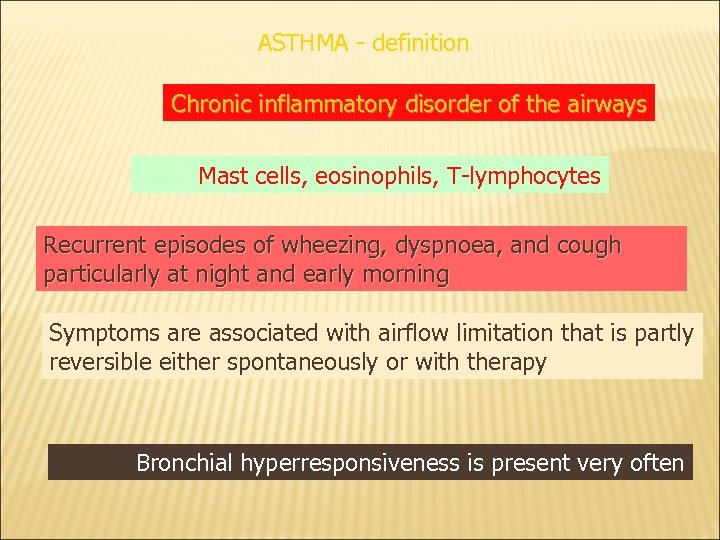
ASTHMA - definition Chronic inflammatory disorder of the airways Mast cells, eosinophils, T-lymphocytes Recurrent episodes of wheezing, dyspnoea, and cough particularly at night and early morning Symptoms are associated with airflow limitation that is partly reversible either spontaneously or with therapy Bronchial hyperresponsiveness is present very often
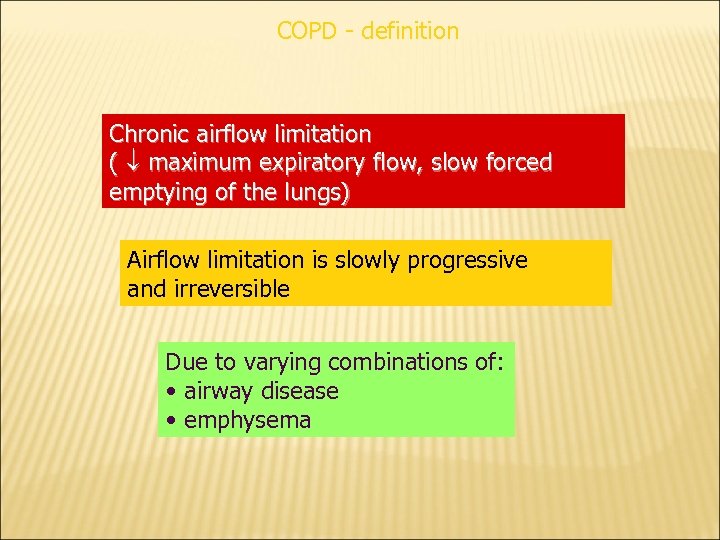
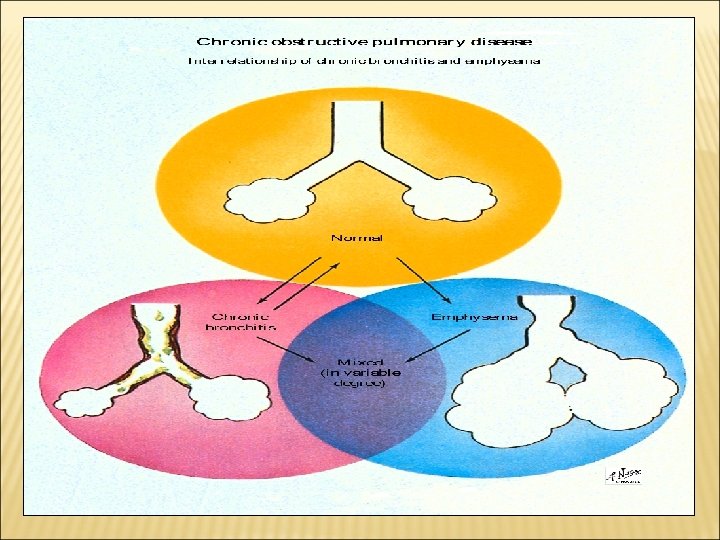
COPD - definition Chronic airflow limitation ( maximum expiratory flow, slow forced emptying of the lungs) Airflow limitation is slowly progressive and irreversible Due to varying combinations of: • airway disease • emphysema
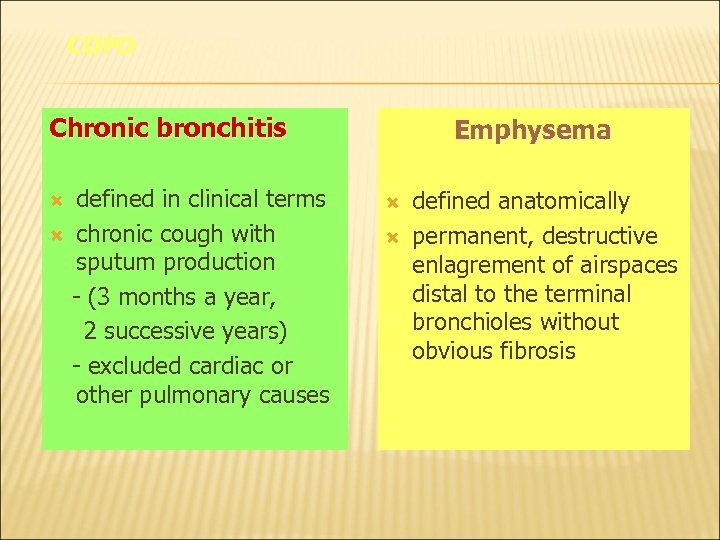
COPD Chronic bronchitis defined in clinical terms chronic cough with sputum production - (3 months a year, 2 successive years) - excluded cardiac or other pulmonary causes Emphysema defined anatomically permanent, destructive enlagrement of airspaces distal to the terminal bronchioles without obvious fibrosis
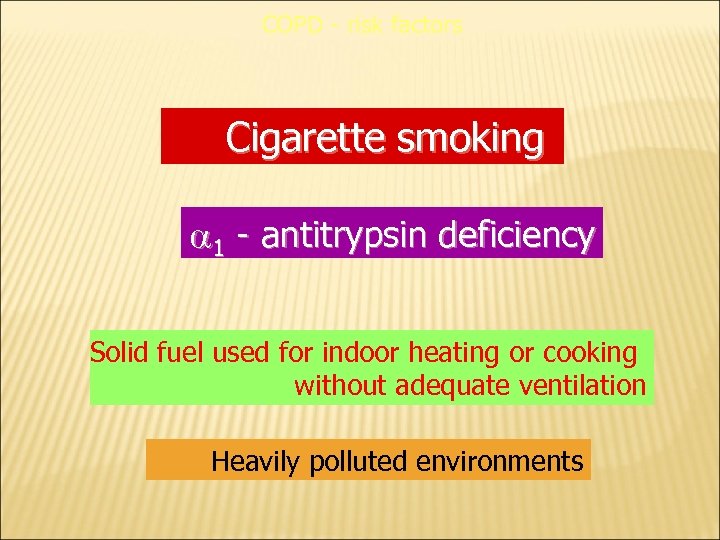
COPD - risk factors Cigarette smoking 1 - antitrypsin deficiency Solid fuel used for indoor heating or cooking without adequate ventilation Heavily polluted environments
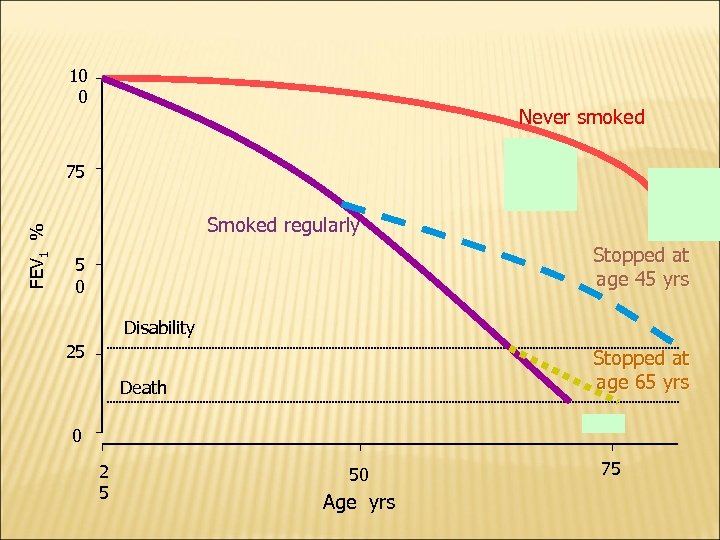
10 0 Never smoked FEV 1 % 75 Smoked regularly Stopped at age 45 yrs 5 0 Disability 25 Stopped at age 65 yrs Death 0 2 5 50 Age yrs 75
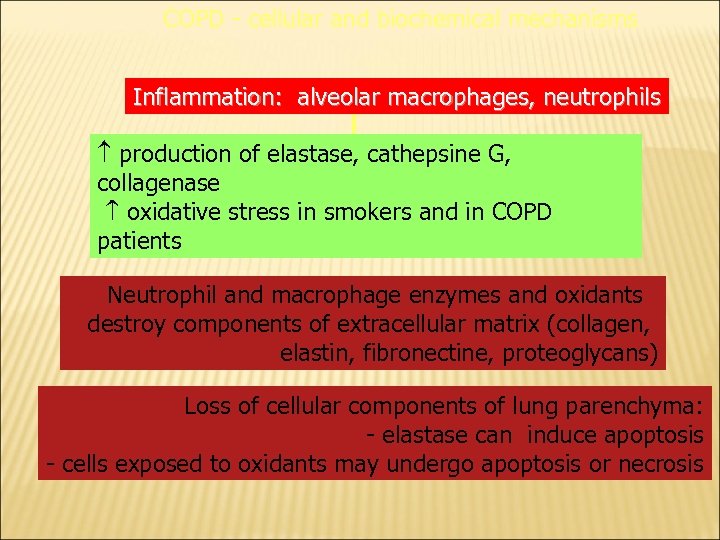
COPD - cellular and biochemical mechanisms Inflammation: alveolar macrophages, neutrophils production of elastase, cathepsine G, collagenase oxidative stress in smokers and in COPD patients Neutrophil and macrophage enzymes and oxidants destroy components of extracellular matrix (collagen, elastin, fibronectine, proteoglycans) Loss of cellular components of lung parenchyma: - elastase can induce apoptosis - cells exposed to oxidants may undergo apoptosis or necrosis
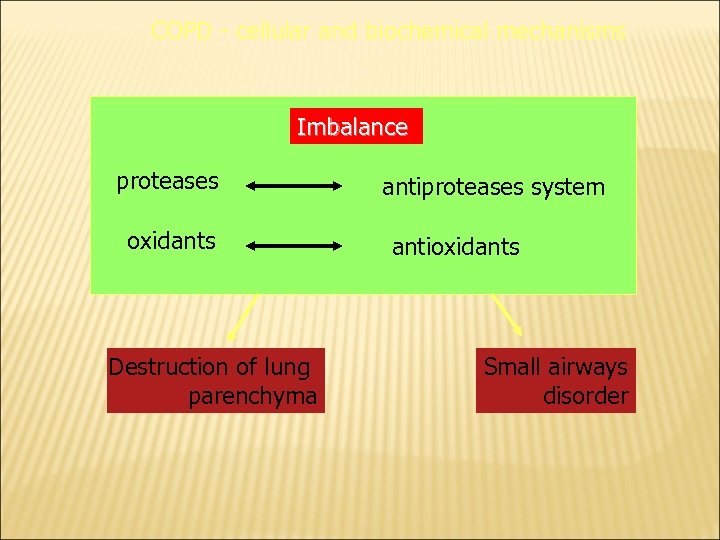
COPD - cellular and biochemical mechanisms Imbalance proteases oxidants Destruction of lung parenchyma antiproteases system antioxidants Small airways disorder
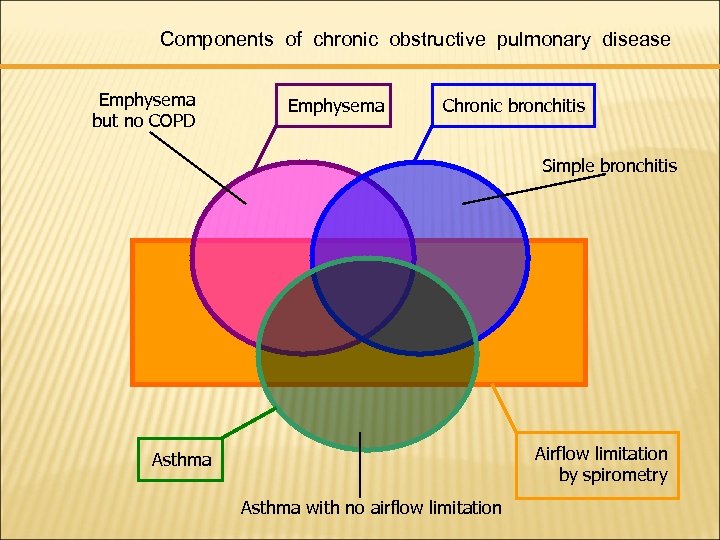
Components of chronic obstructive pulmonary disease Emphysema but no COPD Emphysema Chronic bronchitis Simple bronchitis Airflow limitation by spirometry Asthma with no airflow limitation
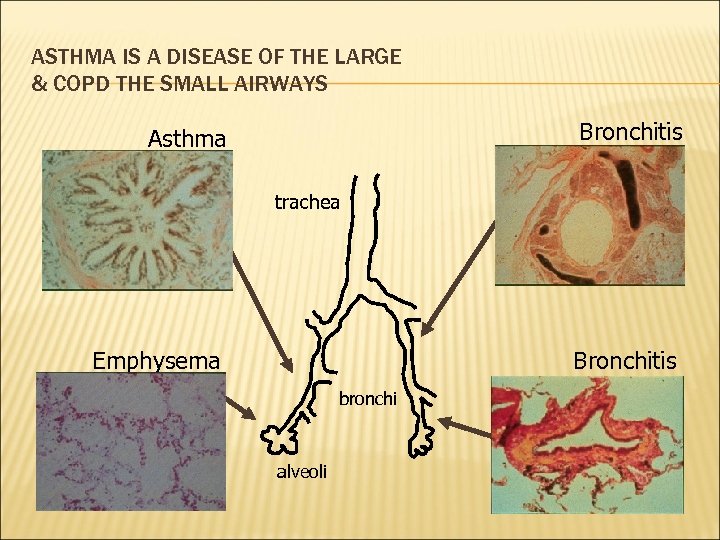
ASTHMA IS A DISEASE OF THE LARGE & COPD THE SMALL AIRWAYS Bronchitis Asthma trachea Emphysema Bronchitis bronchi alveoli
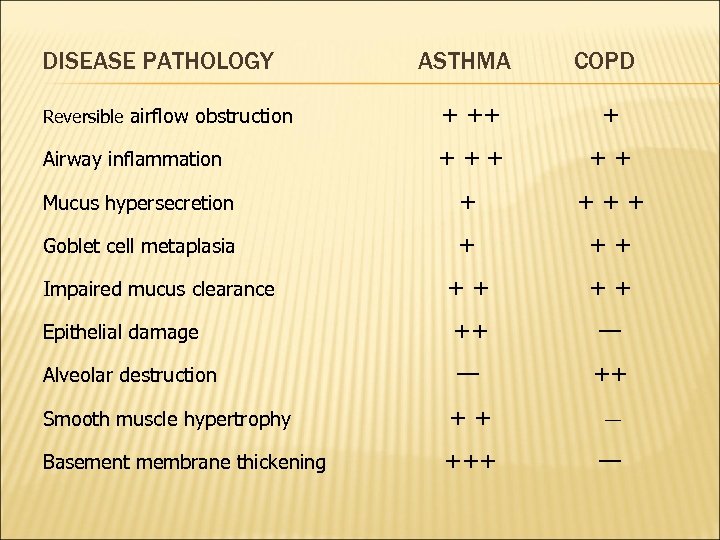
DISEASE PATHOLOGY ASTHMA COPD Reversible airflow obstruction + ++ + Airway inflammation + ++ ++ Mucus hypersecretion + +++ Goblet cell metaplasia + ++ ++ ++ Epithelial damage ++ — Alveolar destruction — ++ Smooth muscle hypertrophy ++ — Basement membrane thickening +++ — Impaired mucus clearance
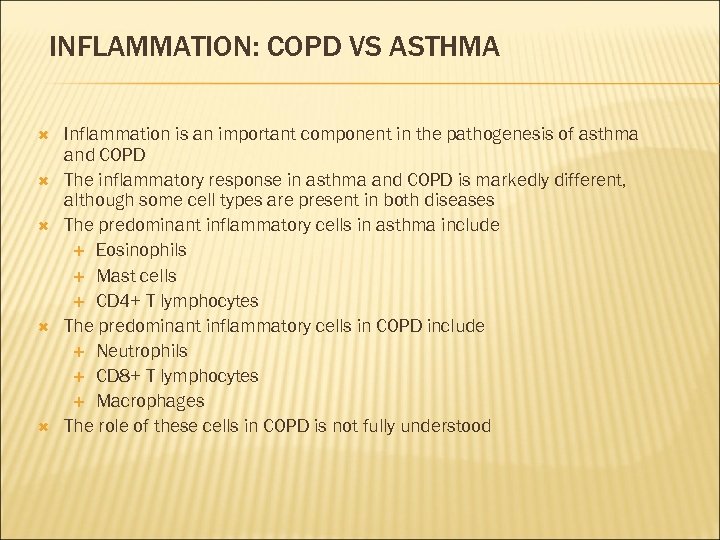
INFLAMMATION: COPD VS ASTHMA Inflammation is an important component in the pathogenesis of asthma and COPD The inflammatory response in asthma and COPD is markedly different, although some cell types are present in both diseases The predominant inflammatory cells in asthma include Eosinophils Mast cells CD 4+ T lymphocytes The predominant inflammatory cells in COPD include Neutrophils CD 8+ T lymphocytes Macrophages The role of these cells in COPD is not fully understood
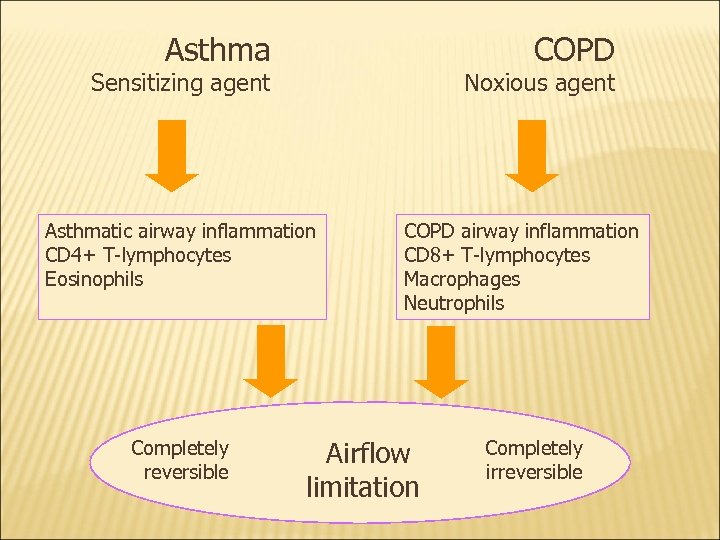
Asthma COPD Sensitizing agent Noxious agent Asthmatic airway inflammation CD 4+ T-lymphocytes Eosinophils Completely reversible COPD airway inflammation CD 8+ T-lymphocytes Macrophages Neutrophils Airflow limitation Completely irreversible
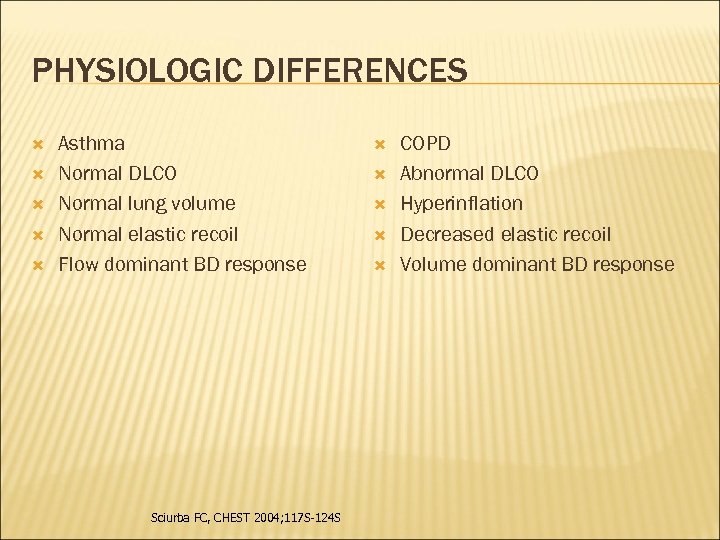
PHYSIOLOGIC DIFFERENCES Asthma Normal DLCO Normal lung volume Normal elastic recoil Flow dominant BD response Sciurba FC, CHEST 2004; 117 S-124 S COPD Abnormal DLCO Hyperinflation Decreased elastic recoil Volume dominant BD response
DRUGS USED IN COPD is a chronic irreversible airflow obstruction, lung damage and inflammation of the air sacs (alveoli). Smoking is a high risk factor Treatment: Inhaled bronchodilators Inhaled glucocorticoids Oxygen therapy
Antibiotics specifically macrolides such as azithromycin to reduce the number of exacerbations. Lung transplantation
Smoking Cessation q. Nicotinic receptor partial agonists such as varenicline q. Nicotine vaccine , when nicotine is coupled to a carrier protein, it is possible to induce antibody formation to nicotine q. The antibodies in the circulation then bind nicotine reversibly q. The binding, however, greatly slows delivery of nicotine to the brain, reducing its addiction potential. Clinical trials with nicotine vaccine are currently underway, and early studies show promise Rennard, 2011
Rimonabant q. It is a canabinoid receptor antagonist that alters release of gamma amino butyric acid release which, in turn, modulates the release of dopamine that is the main downstream mediator of nicotine effects q. FDA declined to approve rimonabant because of concerns for potential suicide risk Rennard, 2011
TREATMENT OF COPD Inhaled bronchodilators Ø Inhaled antimuscarinics (are superior to β 2 agonists in COPD) Ø β 2 agonists Ø these drugs can be used either alone or combined salbutamol + ipratropium salmeterol + Tiotropium (long acting-less dose frequency).
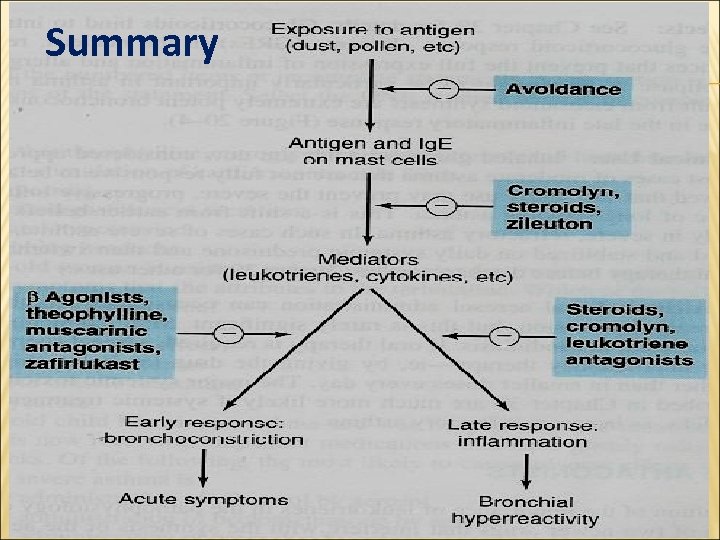
Summary
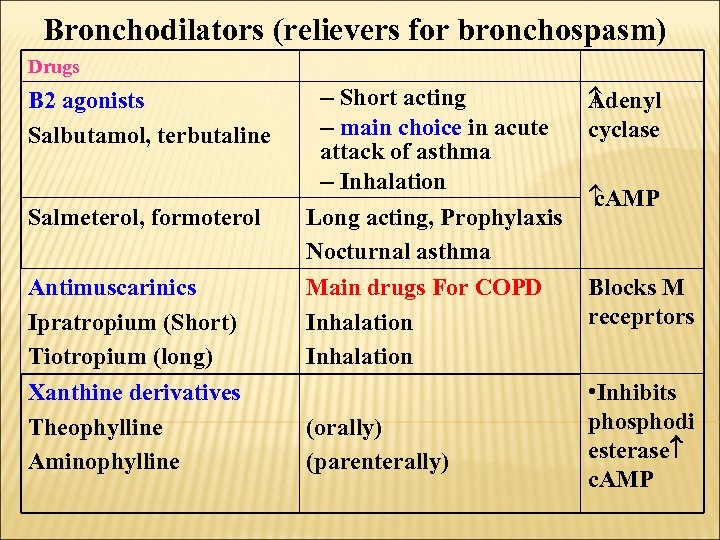
Bronchodilators (relievers for bronchospasm) Drugs B 2 agonists Salbutamol, terbutaline Salmeterol, formoterol Antimuscarinics Ipratropium (Short) Tiotropium (long) Xanthine derivatives Theophylline Aminophylline – Short acting – main choice in acute attack of asthma – Inhalation Long acting, Prophylaxis Nocturnal asthma Main drugs For COPD Inhalation (orally) (parenterally) A denyl cyclase c. AMP Blocks M receprtors • Inhibits phosphodi esterase c. AMP
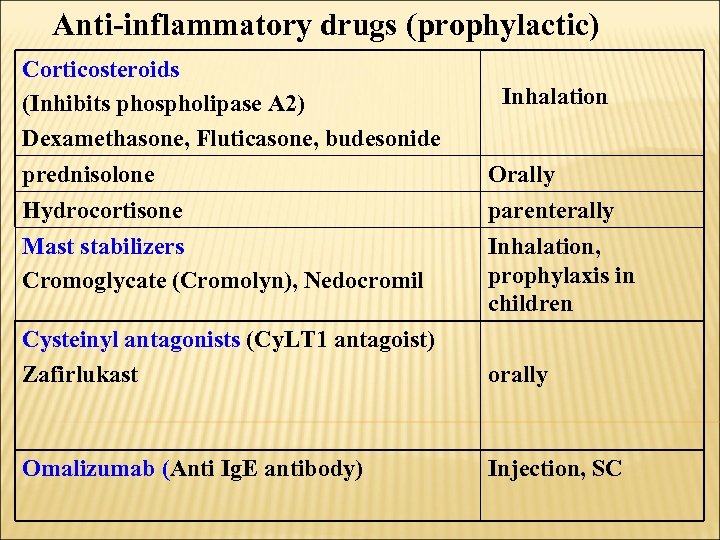
Anti-inflammatory drugs (prophylactic) Corticosteroids (Inhibits phospholipase A 2) Dexamethasone, Fluticasone, budesonide prednisolone Hydrocortisone Mast stabilizers Cromoglycate (Cromolyn), Nedocromil Inhalation Orally parenterally Inhalation, prophylaxis in children Cysteinyl antagonists (Cy. LT 1 antagoist) Zafirlukast orally Omalizumab (Anti Ig. E antibody) Injection, SC
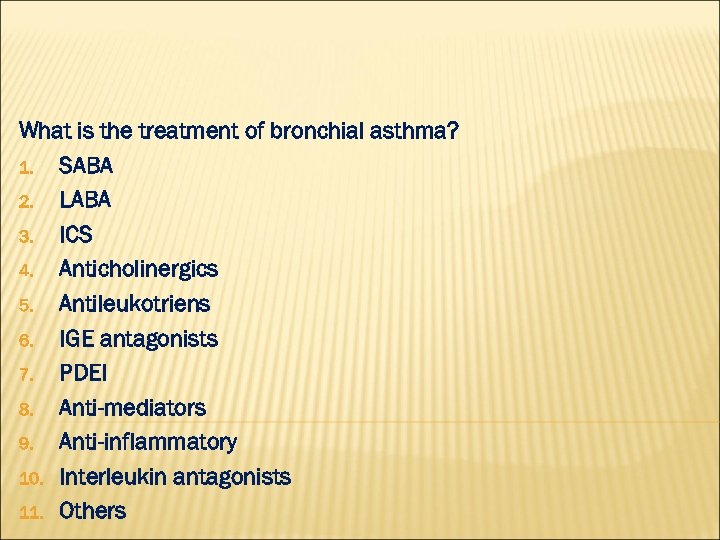
What is the treatment of bronchial asthma? 1. SABA 2. LABA 3. ICS 4. Anticholinergics 5. Antileukotriens 6. IGE antagonists 7. PDEI 8. Anti-mediators 9. Anti-inflammatory 10. Interleukin antagonists 11. Others
What is the treatment of COPD? 1. SABA 2. LABA 3. ICS 4. Anticholinergics 5. Antileukotriens!!!!!!! 6. IGE antagonists!!!!!!! 7. PDEI 8. Anti-mediators 9. Anti-inflammatory 10. Interleukin antagonists!!!! 11. Others
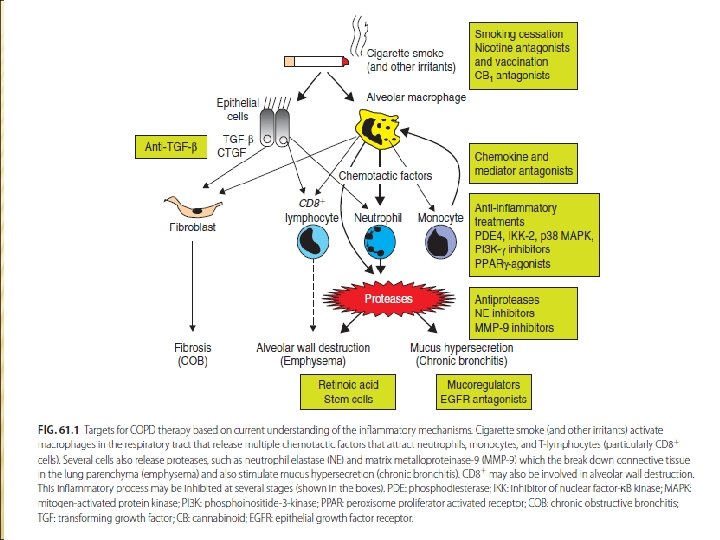
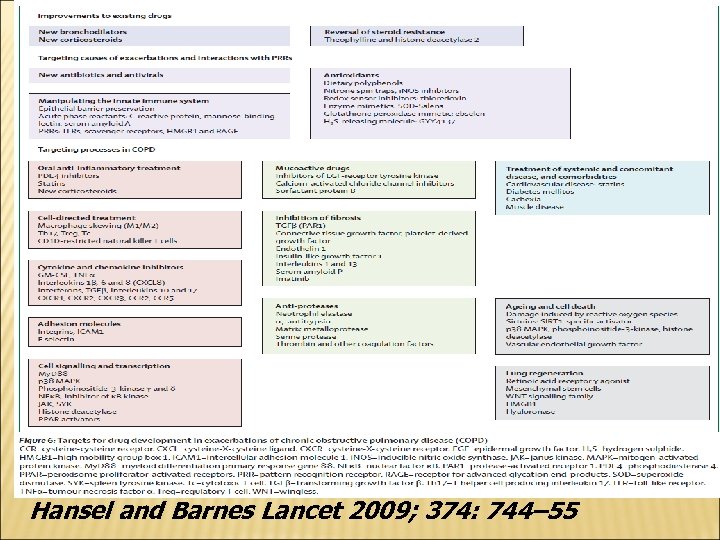
Hansel and Barnes Lancet 2009; 374: 744– 55
ﺍﻟﻠﻬﻢ ﺭﺏ ﺍﻟﻨﺎﺱ ﺃﺬﻫﺐ ﺍﻟﺒﺄﺲ ﺍﺷ ﺃﻨﺖ ﺍﻟﺸﺎﻓﻲ ﻻ ﺷﻔﺎﺀ ﺇﻻ ﺷﻔﺎﺅﻚ ، ﺷﻔﺎﺀ ﻻ ﻳﻐﺎﺩﺭ ﺳﻘﻤﺎ
f58cdf8f01a125282ce5491b1e159187.ppt