55a181469928b00326964f5fc3894503.ppt
- Количество слайдов: 62
Perioperative Fluid and Blood Administration Jeffrey Groom, Ph. D, CRNA Associate Professor, Anesthesiology Nursing Florida International University
Fluid and Blood Administration Primary objective of perioperative fluid management is maintenance of adequate tissue perfusion and oxygen transport.
Clinical Indicators • • • Mental status Urine output Capillary refill Skin color & texture Pulse rate Blood pressure Temperature Frank Starling Curve Acid-base status BP, CVP, PA pressures Oxygen consumption Mixed Venous Oxygen Saturation Surgical patient who exhibits signs of low perfusion, such as oliguria or hypotension, the most common etiology is insufficient intravascular volume.
Quantitative Assessment • • Calculate fluid deficit Calculate fluid needs Calculate fluid losses “The amount of fluid to be administered is best quantitated by continuous evaluation of the response to that which is infused. ”
Physiologic Response to Hemodilution & Anemia • Increased cardiac output • Increased heart rate, stroke volume, contractility • Decreased peripheral vascular resistance • Increased release of oxygen by erythrocyte • Decreased blood viscosity • Increased O 2 consumption/demand
Hemostatic Mechanisms • Primary Hemostasis • Coagulation • Fibrinolysis
Hemostatic Mechanisms • • Primary Hemostasis Platelet adhesion (Factor VIII aka v. WF) Platelet activation (Thrombin aka IIa) Platelet aggregation (ADP, thromboxane A 2) Fibrin production (ex- in- trinsic & common pathways)
Hemostatic Mechanisms
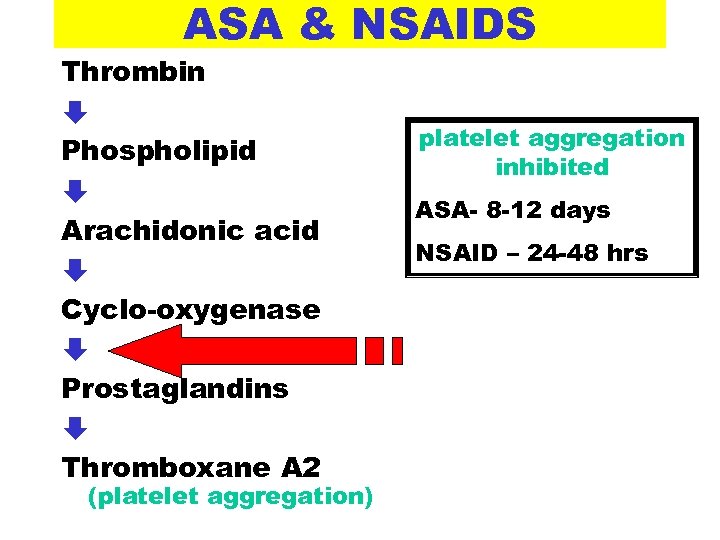
ASA & NSAIDS Thrombin È Phospholipid È Arachidonic acid È Cyclo-oxygenase È Prostaglandins È Thromboxane A 2 (platelet aggregation) platelet aggregation inhibited ASA- 8 -12 days NSAID – 24 -48 hrs
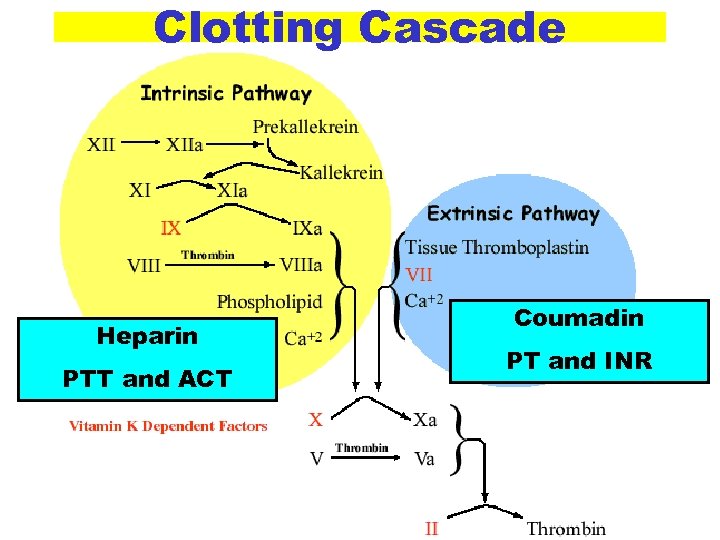
Clotting Cascade Heparin PTT and ACT Coumadin PT and INR
Coagulation Studies • History – ask about bleeding disorders or bleeding symptoms • Partial Prothrombin Time (PTT) • Prothrombin Time (PT) • Bleeding Time • Activated Clotting Time (ACT)
Coagulation Studies • • • Partial Prothrombin Time (PTT) Evaluates the INTRINSIC pathway of the clotting cascade system Normal range – 25 to 35 seconds Assumes normal clotting factors, will be elevated with heparin Not all abnormal PTT values equal Bleeding
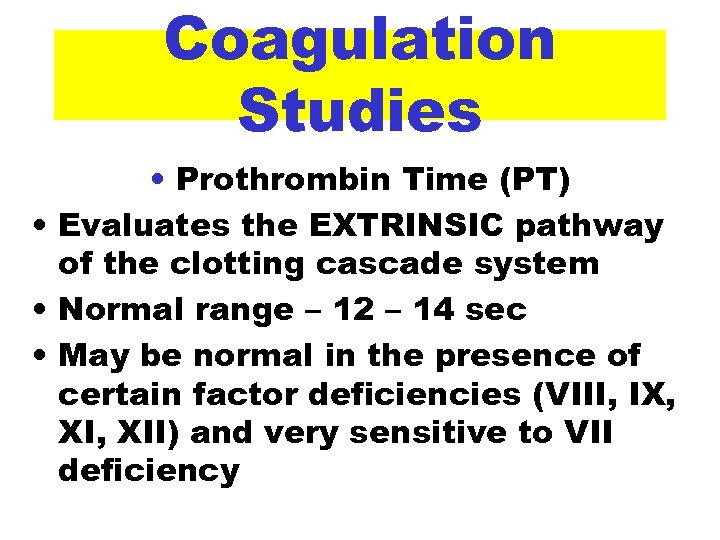
Coagulation Studies • Prothrombin Time (PT) • Evaluates the EXTRINSIC pathway of the clotting cascade system • Normal range – 12 – 14 sec • May be normal in the presence of certain factor deficiencies (VIII, IX, XII) and very sensitive to VII deficiency
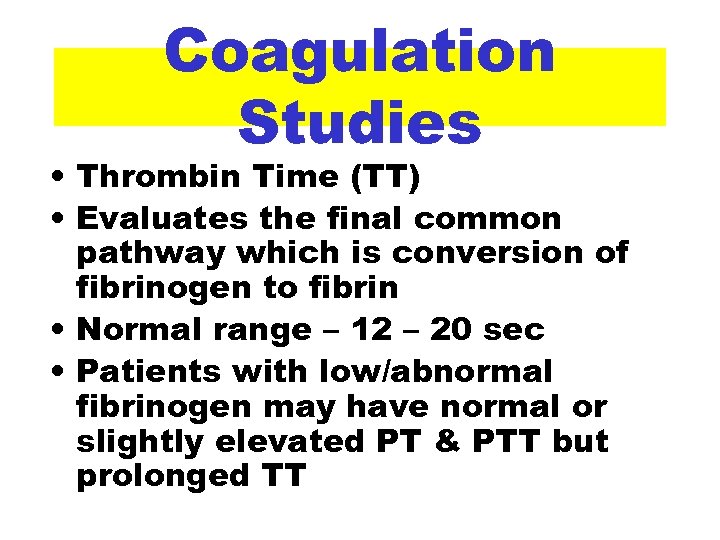
Coagulation Studies • Thrombin Time (TT) • Evaluates the final common pathway which is conversion of fibrinogen to fibrin • Normal range – 12 – 20 sec • Patients with low/abnormal fibrinogen may have normal or slightly elevated PT & PTT but prolonged TT
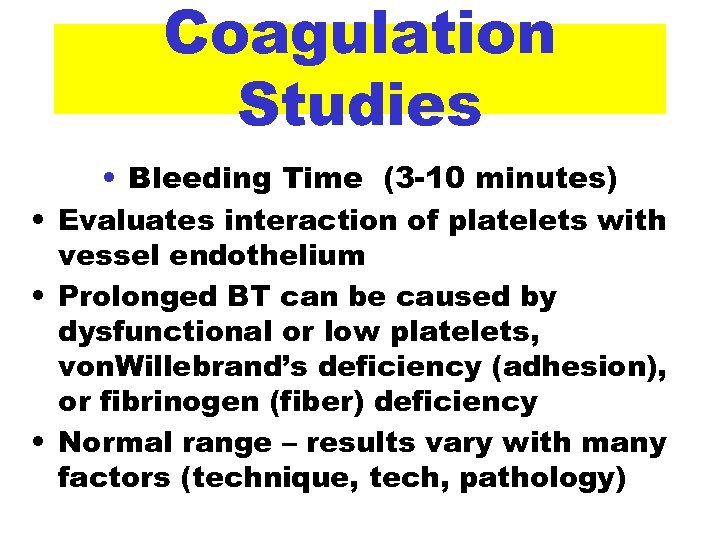
Coagulation Studies • Bleeding Time (3 -10 minutes) • Evaluates interaction of platelets with vessel endothelium • Prolonged BT can be caused by dysfunctional or low platelets, von. Willebrand’s deficiency (adhesion), or fibrinogen (fiber) deficiency • Normal range – results vary with many factors (technique, tech, pathology)
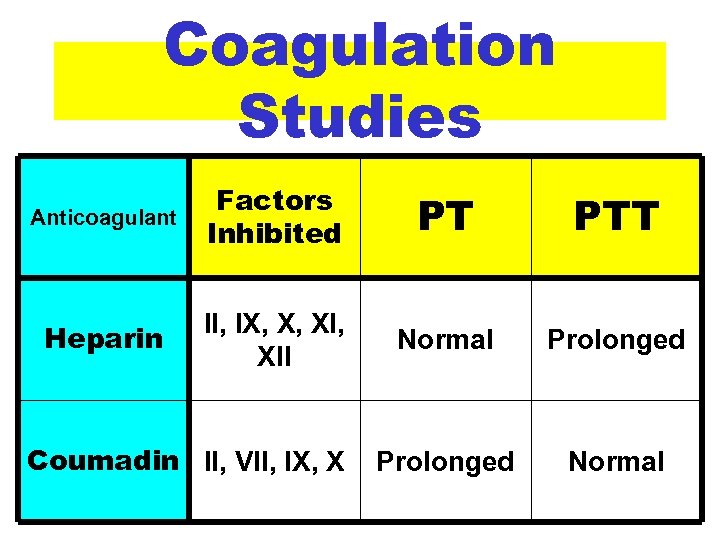
Coagulation Studies Anticoagulant Factors Inhibited PT PTT Heparin II, IX, X, XII Normal Prolonged Normal Coumadin II, VII, IX, X
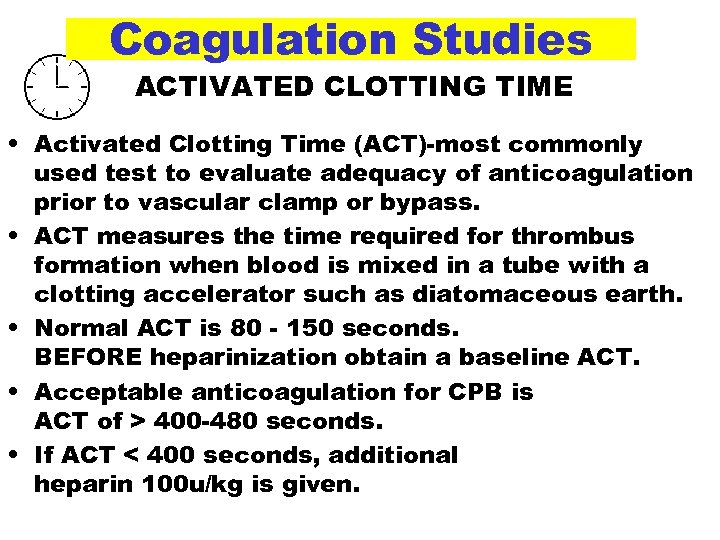
Coagulation Studies ACTIVATED CLOTTING TIME • Activated Clotting Time (ACT)-most commonly used test to evaluate adequacy of anticoagulation prior to vascular clamp or bypass. • ACT measures the time required for thrombus formation when blood is mixed in a tube with a clotting accelerator such as diatomaceous earth. • Normal ACT is 80 - 150 seconds. BEFORE heparinization obtain a baseline ACT. • Acceptable anticoagulation for CPB is ACT of > 400 -480 seconds. • If ACT < 400 seconds, additional heparin 100 u/kg is given.
Coagulation Studies Platelets • Normal range 150, 000 to 400, 000 cells/ml • Life span 8 to 12 days • Approximately 1/3 of platelets are sequestered in the spleen
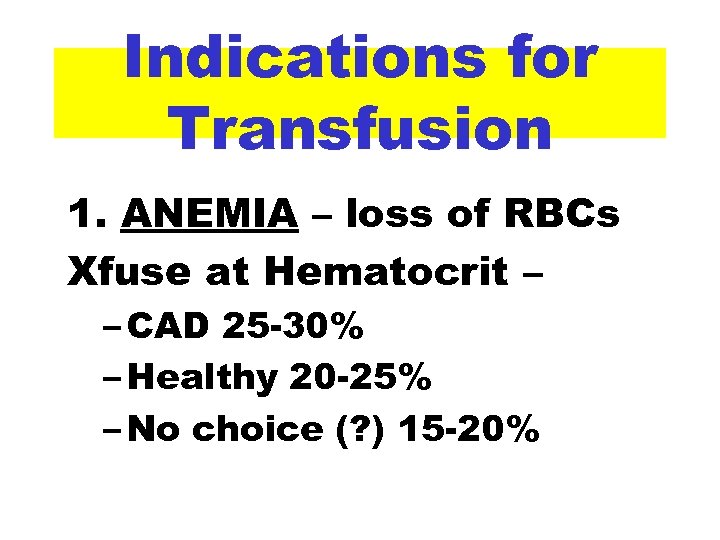
Indications for Transfusion 1. ANEMIA – loss of RBCs Xfuse at Hematocrit – – CAD 25 -30% – Healthy 20 -25% – No choice (? ) 15 -20%
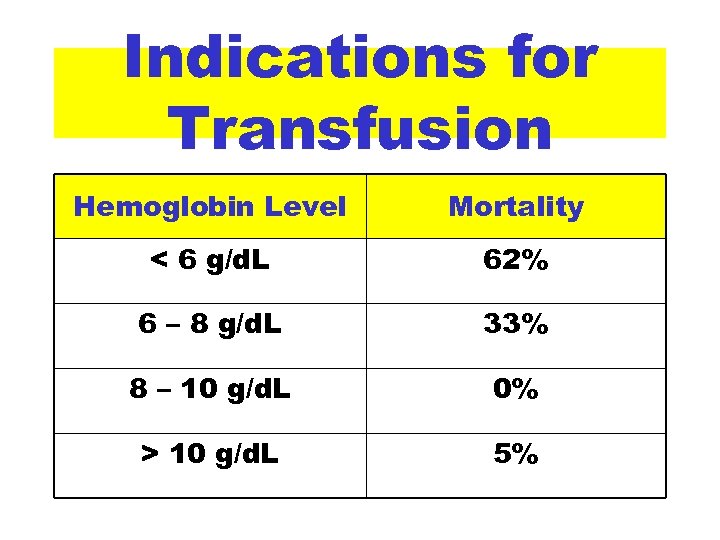
Indications for Transfusion Hemoglobin Level Mortality < 6 g/d. L 62% 6 – 8 g/d. L 33% 8 – 10 g/d. L 0% > 10 g/d. L 5%
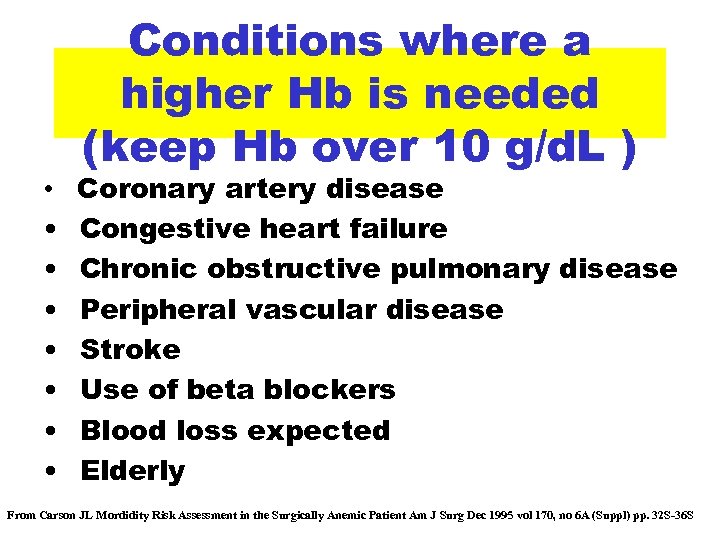
• • Conditions where a higher Hb is needed (keep Hb over 10 g/d. L ) Coronary artery disease Congestive heart failure Chronic obstructive pulmonary disease Peripheral vascular disease Stroke Use of beta blockers Blood loss expected Elderly From Carson JL Mordidity Risk Assessment in the Surgically Anemic Patient Am J Surg Dec 1995 vol 170, no 6 A (Suppl) pp. 32 S-36 S
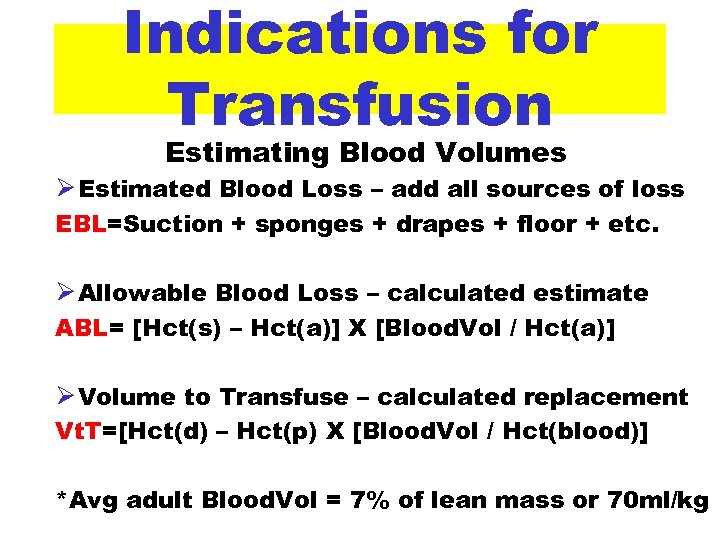
Indications for Transfusion Estimating Blood Volumes Ø Estimated Blood Loss – add all sources of loss EBL=Suction + sponges + drapes + floor + etc. Ø Allowable Blood Loss – calculated estimate ABL= [Hct(s) – Hct(a)] X [Blood. Vol / Hct(a)] Ø Volume to Transfuse – calculated replacement Vt. T=[Hct(d) – Hct(p) X [Blood. Vol / Hct(blood)] *Avg adult Blood. Vol = 7% of lean mass or 70 ml/kg
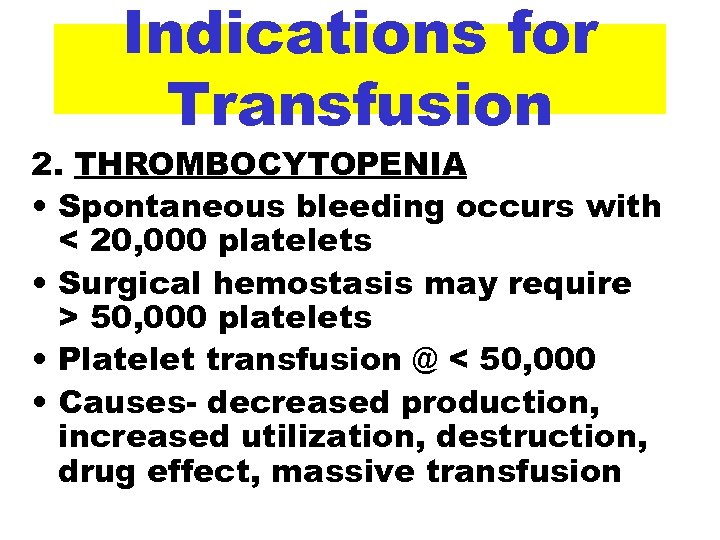
Indications for Transfusion 2. THROMBOCYTOPENIA • Spontaneous bleeding occurs with < 20, 000 platelets • Surgical hemostasis may require > 50, 000 platelets • Platelet transfusion @ < 50, 000 • Causes- decreased production, increased utilization, destruction, drug effect, massive transfusion
Indications for Transfusion 3. COAGULOPATHY – bleeding associated with Factor losses or prolonged clotting times (PT, PTT, BT, ACT)
Guidelines for Transfusion 1. Transfusion need should be assessed on a case-by-case basis. 2. Blood should be transfused one unit at a time, followed by an assessment of benefit and further need. 3. Exposure to allogeneic blood should be limited to appropriate need. • Does this pt need to be transfused? • Appropriate transfusion trigger for this pt • Donor-directed transfusion (? ) (H&H)
Guidelines for Transfusion 4. Perioperative blood loss should be prevented or controlled. • • Stop anticoagulant meds preop Assess/manage preop coagulopathy Restrict perioperative phlebotomy Consider regional anesthesia Consider hypotensive anesthesia Surgical technique options Antifibrinolytic drugs
Guidelines for Transfusion 5. Autologous blood should be considered for use as an alternative to allogeneic transfusion. • preoperative autologous blood • intraoperative acute normovolemic hemodilution • intraoperative autologous blood salvage and autotransfusion • postoperative autologous blood salvage and autotransfusion
Guidelines for Transfusion 6. Efforts should be made to maximize oxygen delivery in the surgical patient. 7. RBC mass should be increased or restored by means other than RBC transfusion. 8. The patient should be involved in the transfusion decision. 9. The reasons for and results of the transfusion decision should be documented contemporaneously in the patient's record. 10. Hospital transfusion policies and procedures should be developed as a cooperative effort that includes input from all those involved in the transfusion decision and reviewed annually. 11. ASA Guidelines – know professional standards
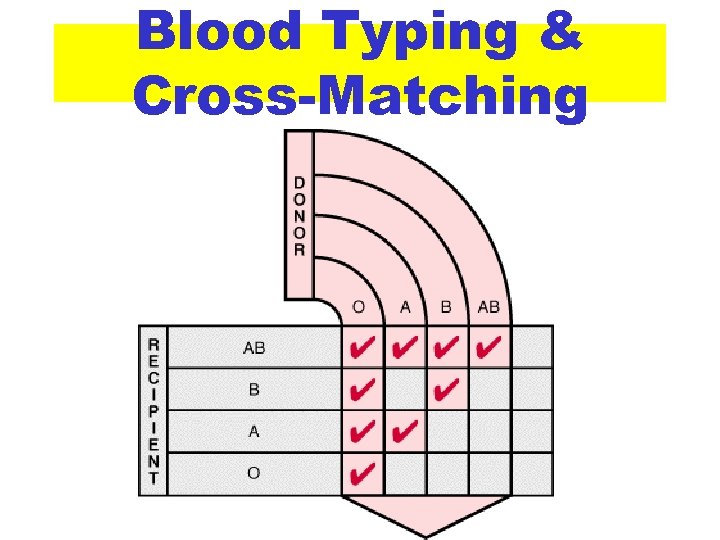
Blood Typing & Cross-Matching • ABO Blood Groups 1. Type A with A antigens on the red cells and anti B antibodies in the plasma 2. Type B with B antigens on the red cells and anti A antibodies in the plasma 3. Type AB with both A and B antigens on the red cells and no type antibodies in the plasma 4. Type O with no type antigens on the red cells and both anti A and anti B antibodies in the plasma
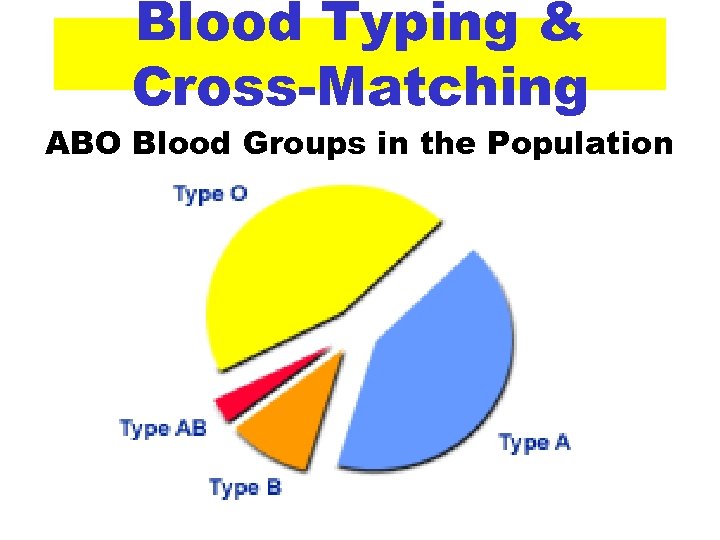
Blood Typing & Cross-Matching ABO Blood Groups in the Population
Blood Typing & Cross-Matching • Rh blood typing – test the presence (+) or absence (-) of the Rh antigen. If your red blood cells: • Contain the Rh antigen, your blood is Rh-positive. • Do not contain the Rh antigen, your blood is Rh-negative.
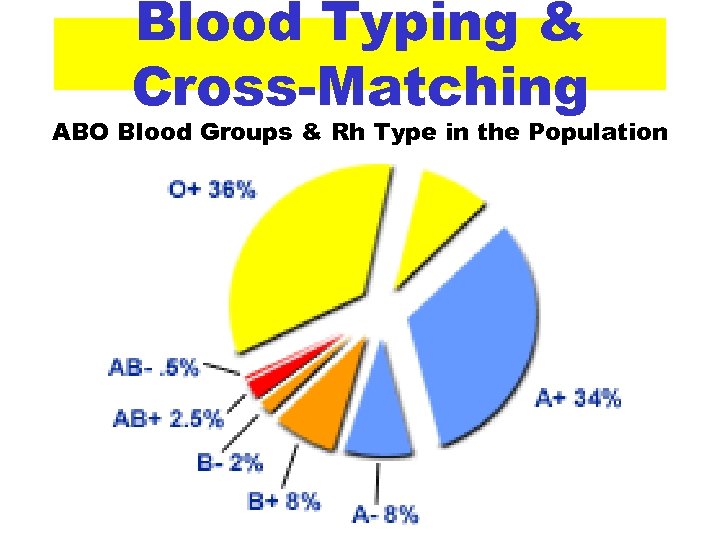
Blood Typing & Cross-Matching ABO Blood Groups & Rh Type in the Population
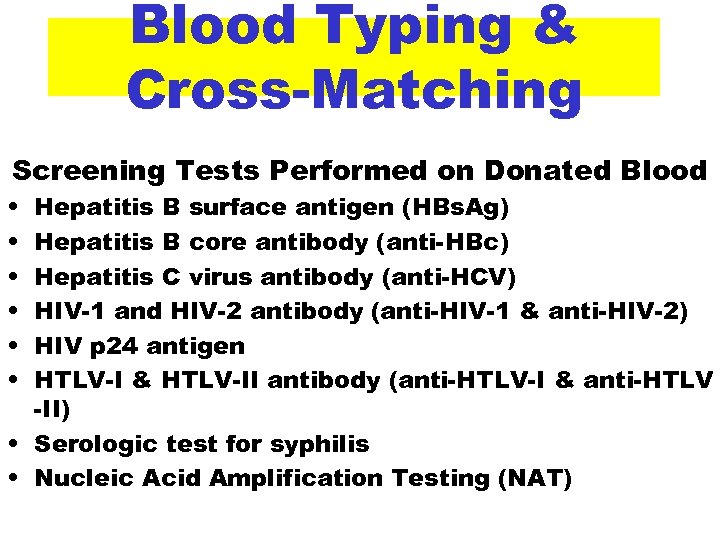
Blood Typing & Cross-Matching Screening Tests Performed on Donated Blood • • • Hepatitis B surface antigen (HBs. Ag) Hepatitis B core antibody (anti-HBc) Hepatitis C virus antibody (anti-HCV) HIV-1 and HIV-2 antibody (anti-HIV-1 & anti-HIV-2) HIV p 24 antigen HTLV-I & HTLV-II antibody (anti-HTLV-I & anti-HTLV -II) • Serologic test for syphilis • Nucleic Acid Amplification Testing (NAT)
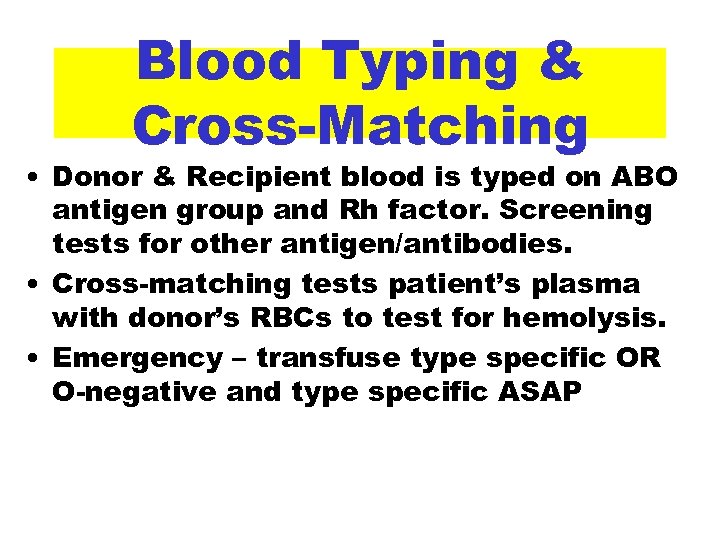
Blood Typing & Cross-Matching • Donor & Recipient blood is typed on ABO antigen group and Rh factor. Screening tests for other antigen/antibodies. • Cross-matching tests patient’s plasma with donor’s RBCs to test for hemolysis. • Emergency – transfuse type specific OR O-negative and type specific ASAP
Blood Typing & Cross-Matching
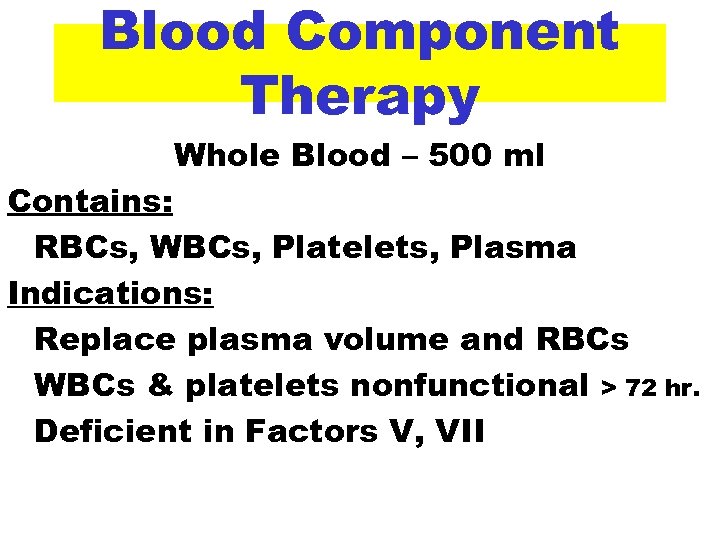
Blood Component Therapy Whole Blood – 500 ml Contains: RBCs, WBCs, Platelets, Plasma Indications: Replace plasma volume and RBCs WBCs & platelets nonfunctional > 72 hr. Deficient in Factors V, VII
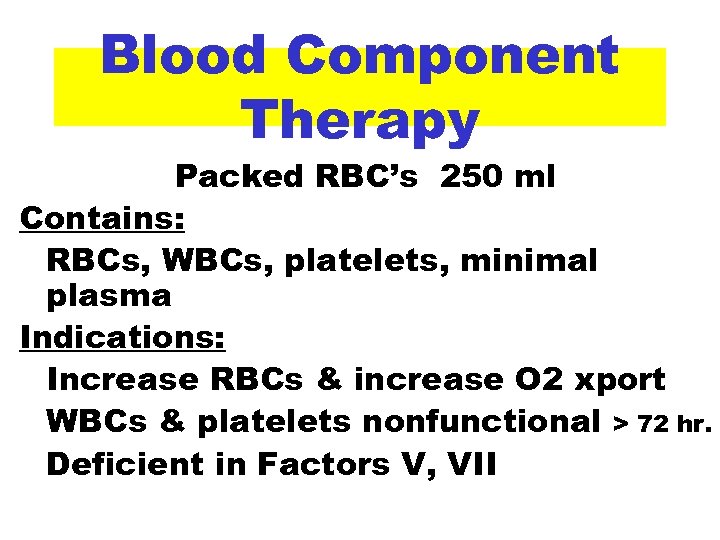
Blood Component Therapy Packed RBC’s 250 ml Contains: RBCs, WBCs, platelets, minimal plasma Indications: Increase RBCs & increase O 2 xport WBCs & platelets nonfunctional > 72 hr. Deficient in Factors V, VII
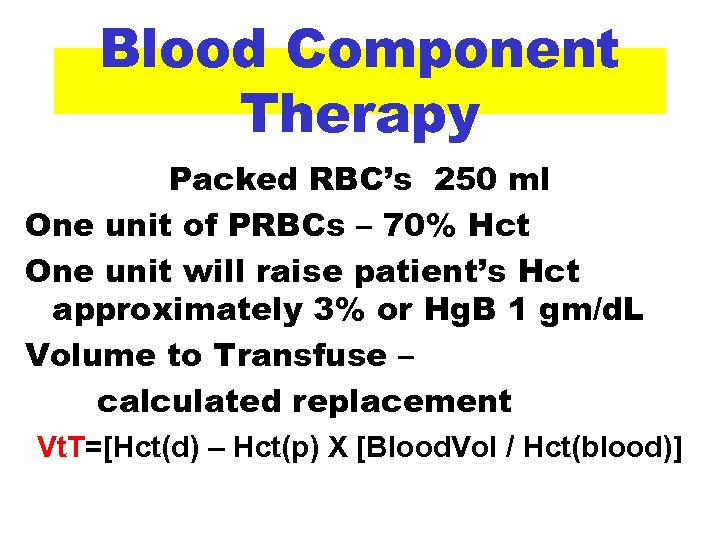
Blood Component Therapy Packed RBC’s 250 ml One unit of PRBCs – 70% Hct One unit will raise patient’s Hct approximately 3% or Hg. B 1 gm/d. L Volume to Transfuse – calculated replacement Vt. T=[Hct(d) – Hct(p) X [Blood. Vol / Hct(blood)]
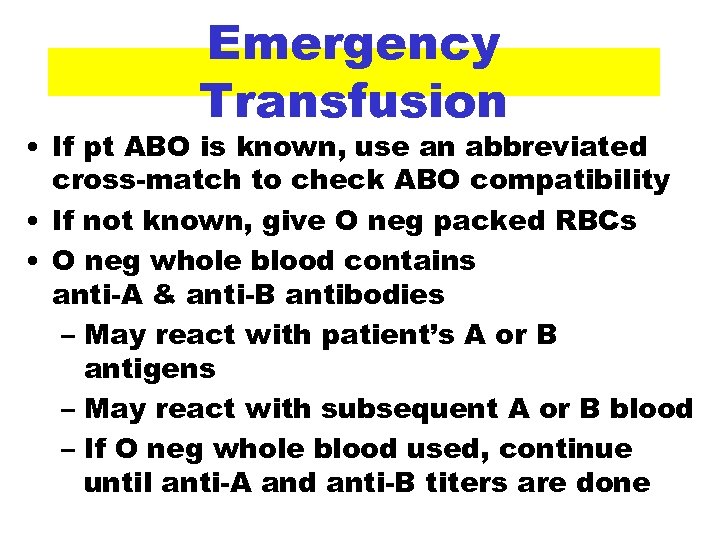
Emergency Transfusion • If pt ABO is known, use an abbreviated cross-match to check ABO compatibility • If not known, give O neg packed RBCs • O neg whole blood contains anti-A & anti-B antibodies – May react with patient’s A or B antigens – May react with subsequent A or B blood – If O neg whole blood used, continue until anti-A and anti-B titers are done
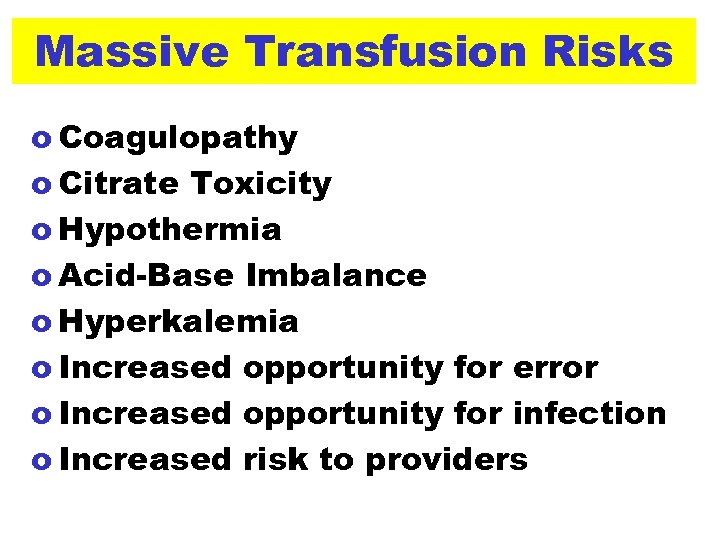
Massive Transfusion Risks o Coagulopathy o Citrate Toxicity o Hypothermia o Acid-Base Imbalance o Hyperkalemia o Increased opportunity for error o Increased opportunity for infection o Increased risk to providers
Blood Component Therapy Platelet Concentrate 50 ml Contains: > 5 x 1010 platelets, RBCs, WBCs, platelets, minimal plasma Indications: Bleeding from thrombocytopenia or thrombocytopathy
Blood Component Therapy Platelet Concentrate 50 ml One unit of PC increases platelet count 5000 – 10, 000 cells/mm
Blood Component Therapy Fresh Frozen Plasma 220 ml Contains: Contains plasma with coagulation factors but no platelets Indications: Correction of coagulopathy
Blood Component Therapy Fresh Frozen Plasma 220 ml Dose of 10 -15 ml/kg increases coagulation factors by 30% Fibrinogen increases 1 mg/ml of FFP Rapid reversal of warfarin usually requires 5 – 10 ml/kg of FFP
Blood Component Therapy Cryoprecipitate 15 - 25 ml Contains: Fibrinogen, Factors VIII, XIII, von Willebrand’s Indications: Correction of coagulopathy where Fibrinogen, Factors VIII, XIII, or von Willebrand’s are deficient

Blood Component Therapy Cryoprecipitate 15 - 25 ml Dose of 1 unit per 10 kg raises fibrinogen level 50 mg/d. L
Blood Administration ü Check and double check IDs & Labels. ü Blood should not be infused with D 5 W hemolysis ü Blood should not be infused with LR Ca++ in LR may induce clot formation ü RBCs are compatible with: Normal saline, 5% albumin, FFP
Blood Administration Blood Filters ü 80 mcm filters should be used for all blood components ü 170 mcm filters should be used to administer platelets ü Leukocyte filters for patients with febrile rxn history, maybe for all to prevent alloimmunization to foreign leukocyte antigens
Blood Administration Future Blood Substitutes • Fluosol-DA 20% • Free hemoglobin solutions
Plasma Substitutes Albumin • Isotonic Albumin 5% • Hypertonic Albumin 20 & 25% • Intravascular half-life = 10 to 15 days
Plasma Substitutes • • • Dextran 70 – Macrodex and Dextran 40 – Rheomacrodex Intravascular half life = 2 to 8 hours Decreases platelet adhesion and VIII Coag changes > 1. 5 g/kg 1% incidence of anaphylactoid reactions Give 20 ml Promit to inhibit dextran binding antibodies
Plasma Substitutes Hespan ( Hydroxyethyl starch ) - small molecules broken down by kidneys, large molecules by amylase - Nonantigenic, anaphylactoid reactions are rare - Coag studies not impaired - Half-life – 24 -36 hours
Blood Conservation Techniques Autologous Donation • Donation 5 weeks pre-op, must have Hg. B > 11 g/d. L, can donate Q 3 days, last donation > 72 hr pre-op • Not all patients tolerate donation • Transfusion reaction risk is reduced but human error component is still present – transfuse with same criteria & precautions
Blood Conservation Techniques • • Hemodilution Techniques (? ) Remove 1 to 2 units of whole blood (Hct 25 -30%) Replace volume with LR or colloids Intraop loss then is greater plasma loss and less RBC loss Reinfuse fresh autologous blood (Hct will be the same as pre-op, not PRBC)
Blood Conservation Techniques Cell Saver • Intraop autotransfusion • Double lumen suction aspirates blood from clean field (heparin + saline + blood) • Collected blood is filtered and washed prior to reinfusion • RBC’s in saline Hct ~ 50% • No plasma, clotting factors or platelets
Complications of Transfusion • • Acute Hemolytic Reactions ABO-incompatiability Occur ~ 1 in 33, 000 most due to human error, fatal in 1: 300 k to 700 k Symptoms may be masked by anesthesia (agitation, chest or flank pain, headache, dyspnea, chills) Signs include: fever, tachycardia, hypotension, DIC, hemoglobinuria
Complications of Transfusion Acute Hemolytic Reactions • STOP the infusion • Establish a noncontaminated IV • Send unused donor blood to lab with blood sample from patient for rematch • Send blood for: Hgb, haptoglobin, Coomb’s and DIC screening • Rx hypotension – fluids & vasopressors prn • May give corticosteroids • Preserve renal function – fluids, dopamine, diuertic – maintain UO 1 -2 ml/kg/hr • R/O DIC
Complications of Transfusion Non-Hemolytic Reactions • Allergic or febrile rxn to antibodies to donor WBCs or platelets • Transfused allergens in plasma interact with the patient's tissue mast cells, causing them to degranulate and release inflammatory mediators (histamine, tryines, etc. )
Complications of Transfusion Non-Hemolytic Reactions • STOP the transfusion, establish clean IV and send labs • Mild rxn – diphenhydramine 25 -50 mg IV & hydrocortisone 50 -100 mg IV, acetaminophen 650 mg • May resume transfusion slowly (? ) • Rx other symptoms prn
Complications of Transfusion Infection Risk
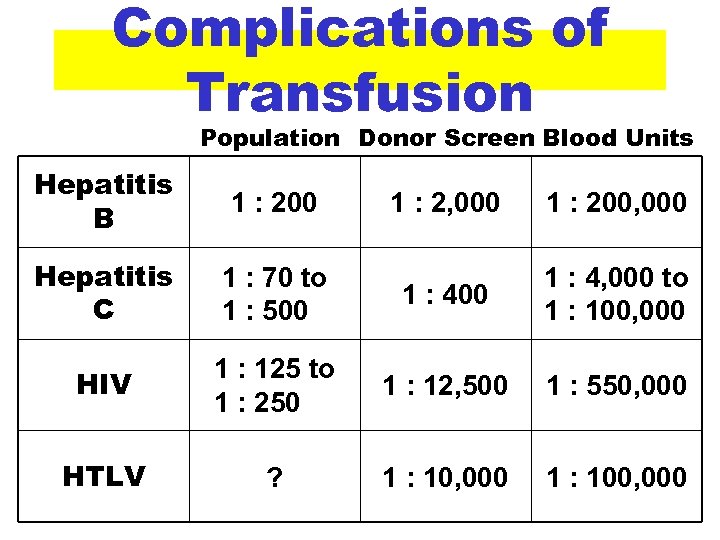
Complications of Transfusion Population Donor Screen Blood Units Hepatitis B 1 : 200 Hepatitis C 1 : 2, 000 1 : 200, 000 1 : 70 to 1 : 500 1 : 4, 000 to 1 : 100, 000 HIV 1 : 125 to 1 : 250 1 : 12, 500 1 : 550, 000 HTLV ? 1 : 10, 000 1 : 100, 000
SUMMARY • Blood components • Coagulation system and tests • Blood and fluid administration
55a181469928b00326964f5fc3894503.ppt