35b1966b5862736bec8636d452faacf3.ppt
- Количество слайдов: 44

PERIOPERATIVE CARE
OBJECTIVES Know and understand: • How age-related physiologic changes influence perioperative care • Risk factors for cardiovascular, pulmonary, renal, and neurologic complications • Elements of perioperative management of selected medical problems • How to avoid iatrogenic complications Slide 2
TOPICS COVERED • Overview of Operative Therapy for Older People • Preoperative Assessment and Management • Perioperative Management of Selected Medical Problems • Avoiding Iatrogenic Complications Slide 3
SURGERY IS A COMMON TREATMENT FOR OLDER PATIENTS • More than 55% of all surgeries are done in patients ≥ 65 years old • Advances in care have lowered surgical risks and shifted the risk-benefit ratio to favor surgery in increasingly older patients with more complex conditions Slide 4

AGE-RELATED CHANGES INFLUENCE PERIOPERATIVE CARE • As a result of normal aging, multiple organ systems may have limited physiologic reserve Examples: Ø Cardiac and vascular stiffening complicate fluid management Ø Decreased thermoregulation increased risk of perioperative hypothermia • The resulting “homeostenosis” greatly increases the risk of iatrogenic events Slide 5
PREOPERATIVE CARE SHOULD BE INDIVIDUALIZED • Not all organ systems age at the same rate, even within an individual • Most older people have one or more chronic conditions that influence perioperative care, either directly or through the drugs they use • Thus, older patients require thorough and individualized preoperative care, and often benefit from a multidisciplinary approach Slide 6
PREOPERATIVE ASSESSMENT: CARDIOVASCULAR SYSTEM • The risk of postoperative cardiac events is directly related to age • To calculate cardiac risk: Ø ASA classification http: /www. asahq. org/clinical/physicalstatus. htm Ø ACC/AHA guideline http: //www. acc. org/clinical/guidelines/perio/ update/periupdate_index. htm Slide 7
PREOPERATIVE CARDIAC ASSESSMENT GUIDELINE • Urgency of surgery • Presence of active major cardiac risk factors • Type of surgery • Patient’s functional capacity • Presence of other clinical risk factors Slide 8
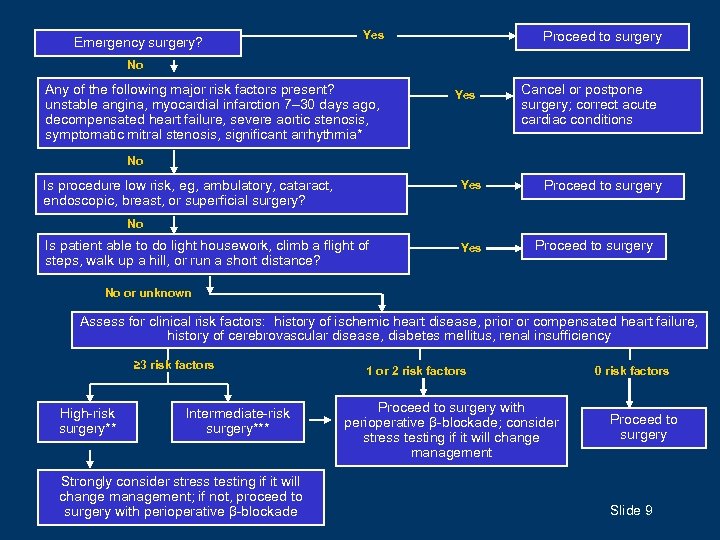
Emergency surgery? Yes Proceed to surgery No Any of the following major risk factors present? unstable angina, myocardial infarction 7– 30 days ago, decompensated heart failure, severe aortic stenosis, symptomatic mitral stenosis, significant arrhythmia* Yes Cancel or postpone surgery; correct acute cardiac conditions No Is procedure low risk, eg, ambulatory, cataract, endoscopic, breast, or superficial surgery? Yes Proceed to surgery No Is patient able to do light housework, climb a flight of steps, walk up a hill, or run a short distance? Yes Proceed to surgery No or unknown Assess for clinical risk factors: history of ischemic heart disease, prior or compensated heart failure, history of cerebrovascular disease, diabetes mellitus, renal insufficiency ≥ 3 risk factors High-risk surgery** Intermediate-risk surgery*** Strongly consider stress testing if it will change management; if not, proceed to surgery with perioperative β-blockade 1 or 2 risk factors Proceed to surgery with perioperative β-blockade; consider stress testing if it will change management 0 risk factors Proceed to surgery Slide 9
PREOPERATIVE CARE: CARDIOVASCULAR SYSTEM • Older patients with known CAD or more than one risk factor for CAD may benefit from perioperative β-blockers titrated to HR of 60 -80, particularly if they are undergoing vascular surgery or major surgery. If β-blockade is decided, it should be performed in the weeks prior to surgery rather than perioperatively. • Aspirin and statins have been beneficial in nonrandomized studies of high-risk patients • Choose DVT prophylaxis based upon DVT/PE risk and type of surgery • Prophylactic antibiotics are recommended for selected patients to prevent bacterial endocarditis Slide 10
CESSATION OF ANTICOAGULATION BEFORE SURGERY IN OLDER ADULTS • Weigh protective benefit versus bleeding risk in patients already on anticoagulation • Do not withhold for cutaneous surgery, dental extractions, minor oral procedures, or cataract surgery • For other procedures, cessation of warfarin, with or without low-molecular-weight heparin bridge therapy, is based on patient’s risk of thromboembolism Slide 11
PREOPERATIVE ASSESSMENT: RESPIRATORY SYSTEM Risk factors for pulmonary complications: • Patient-related: age, COPD, ASA class II or greater, heart failure, ADL deficit, low albumin • Procedure-related: emergency surgery; prolonged surgery; AAA repair; neurosurgery; or thoracic, abdominal, head and neck, or vascular surgery Slide 12
2007 ACP GUIDELINE FOR RISK ASSESSMENT AND PERIOPERATIVE MANAGEMENT OF PULMONARY COMPLICATIONS • Appraise risk factors • Routine chest x-ray not recommended except for known cardiac or pulmonary disease • Spirometry reserved for patients with suspected COPD • Post-op lung expansion therapy recommended Slide 13

PREOPERATIVE ASSESSMENT: KIDNEY FUNCTION Accurate estimation of GFR is important • Renal and glomerular blood flow decrease with age, and muscle mass declines, so serum creatinine may appear normal even when kidney function is not • Many drugs used perioperatively may require dosage adjustment if renal function is impaired Slide 14
PREOPERATIVE ASSESSMENT: RISK OF DELIRIUM • Preoperative risk factors in noncardiac surgery: Ø Age ≥ 70 years Ø Cognitive impairment Ø Limited physical function Ø History of alcohol abuse Ø Abnormal serum sodium, potassium, or glucose Ø Intrathoracic surgery or abdominal aneurysm surgery • The most important intraoperative risk factor for delirium is blood loss Slide 15
AVOIDING IATROGENIC COMPLICATIONS • Encourage time out of bed and avoid restraints, to maintain mobility and function • Remove indwelling catheters as soon as possible, to reduce the risk of infection and the effects of restricted mobility • Stop IV fluids, and lift restrictions on diet, as soon as possible • Review medications regularly Slide 16
POSTOPERATIVE CARE: HYPERTENSION • Search for a non-cardiovascular cause, such as pain or urinary retention • Assess volume status, review fluid administration, and note whether antihypertensives were omitted • Consider a parenteral antihypertensive for treating uncontrolled essential hypertension • Topical agents, such as topical nitroglycerin, may also be useful postoperatively if patient is unable to take oral medications Slide 17
POSTOPERATIVE CARE: ARRHYTHMIA • Supraventricular tachycardia: Attempt to restore sinus rhythm, or at least control the ventricular rate, by infusing adenosine, a β-blocker, or a calcium-channel blocker • Atrial fibrillation: Ø Attempt conversion to sinus rhythm with electrical cardioversion or infusion of amiodarone if poorly tolerated Ø Spontaneous reversion to sinus rhythm often occurs within 6 weeks after surgery Ø Persistent a-fib (beyond 24– 48 hours) increases the risk of thromboembolism, so consider anticoagulation Slide 18
POSTOPERATIVE CARE: HEART FAILURE • May develop as a result of excessive fluid administration, new cardiac ischemia, or arrhythmia • It can be extremely challenging to ensure optimal ventricular filling pressures by basing the assessment of volume status on physical examination and standard laboratory parameters alone • Pulmonary artery catheters have been recommended for high-risk patients, but studies have not shown a mortality benefit Slide 19
POSTOPERATIVE CARE: RESPIRATORY SYSTEM Measures that may reduce the risk of postoperative pulmonary complications: • Encouragement of coughing • Deep breathing exercises • Incentive spirometry • Early mobility Slide 20
POSTOPERATIVE CARE: KIDNEY DAMAGE (1 of 2) • Early signs of postoperative kidney damage: oliguria, isosthenuria, increase in serum creatinine • Mechanisms of postoperative kidney damage: Ø Impaired renal blood flow: signaled by urine sodium <40 m. Eq/L, ratio of urine to plasma creatinine >10: 1 Ø Acute tubular necrosis: signaled by urine sodium >40 m. Eq/L, ratio of urine to plasma creatinine <10: 1; urine sediment may have granular or epithelial cell casts Ø Obstructive nephropathy, especially in men with prostatic hyperplasia: bladder typically distended, palpable Slide 21
POSTOPERATIVE CARE: KIDNEY DAMAGE (2 of 2) • Acute tubular necrosis: Hold all potentially nephrotoxic medications and meticulously maintain a euvolemic state • Obstructive nephropathy: Insert a bladder catheter to reduce the risk of hydronephrosis and impaired kidney function • Indications for dialysis are no different in the perioperative period and include hypervolemia, hyperkalemia, metabolic acidosis, or encephalopathy Slide 22
POSTOPERATIVE CARE: GASTROINTESTINAL CONCERNS Constipation • Order a laxative and a stool softener when a narcotic medication is ordered • Consider suggesting prunes, prune juice, applesauce, or bran Diarrhea • Check manually for fecal impaction, and consider having stool specimen checked for leukocytes or Clostridium difficile • Focus carefully on volume resuscitation and treating the underlying cause Slide 23
PERIOPERATIVE CARE: TYPE 2 DIABETES MELLITUS (1 of 2) • Oral drugs are usually held the day of surgery, especially metformin, which increases the risk of metabolic acidosis during times of stress • An option for optimizing glucose control: Ø Administer an IV glucose-containing solution at a constant rate while closely monitoring blood glucose by fingerstick assay Ø Administer SC insulin as needed to control glucose until the patient can resume eating Slide 24
PERIOPERATIVE CARE: TYPE 2 DIABETES MELLITUS (2 of 2) • Insulin-using patients with type 2 diabetes: Ø Day of surgery: Hold the outpatient dose of insulin and give “sliding-scale” insulin as needed Ø First day of eating by mouth: A general rule is to give half the outpatient dose of diabetes drugs, with slidingscale insulin as needed Ø When patient can consume a usual diet: Resume full doses of diabetes drugs Slide 25
PERIOPERATIVE CARE: PATIENTS USING CORTICOSTEROIDS • Perioperative administration of “stress doses” of steroids is appropriate for: Ø Patients on prednisone >20 mg/day for >1 week Ø Patients with known adrenal insufficiency • If HPA axis function is in question: Ø Measure cortisol Ø Cortisol not elevated: Consider 30 -minute ACTH test Slide 26
PERIOPERATIVE CARE: REDUCING RISK OF DELIRIUM When preoperative risk factors are present, clinicians should be especially vigilant about: Ø Correcting fluid, electrolyte, metabolic derangements Ø Optimizing replacement of blood loss Ø Encouraging mobility, avoiding restraints Ø Maintaining circadian rhythms Ø Enhancing sensory input Ø Prescribing medications cautiously Slide 27
POSTOPERATIVE CARE: COGNITIVE DECLINE • A syndrome distinct from delirium, characterized by abnormalities in learning and memory • Most common after cardiac surgery • Persists for many months in 10%– 30% of patients • No demonstrated link to hypotension, hypoxemia, or type of anesthesia • Treatment is supportive Slide 28
POSTOPERATIVE CARE: PAIN (1 of 2) • The oldest-old and cognitively impaired patients are at highest risk for undertreatment of pain • Most postsurgical pain requires narcotic analgesia • For cognitively intact patients, consider a patientcontrolled analgesia (PCA) pump to improve pain relief and lower use of narcotics Slide 29

POSTOPERATIVE CARE: PAIN (2 of 2) • Less severe pain: Patient may tolerate acetaminophen (≤ 4 g/day) with narcotic analgesic as needed, if able to request pain relief • Patient unable to communicate effectively: Standing orders for narcotic analgesic, with frequent assessment of medication effect • Useful adjuncts: ice packs, heating pads, massage, relaxation techniques • Avoid NSAIDS Slide 30
SUMMARY • Surgery is an important therapeutic option for many older people • Preoperative assessment should be individualized, comprehensive, and, often, multidisciplinary • Attentive perioperative management minimizes complications in older patients, especially those with chronic medical problems and functional impairments Slide 31
CASE 1 (1 of 4) • A 72 -year-old woman comes to the office for evaluation before left total-knee replacement. • Despite the worsening pain in her left knee, she remains active; she gardens and plays golf 4 days a week. • She has no known allergies and has never smoked. • Both her parents lived into their nineties. • Her history includes mild hypertension, for which she takes atenolol 25 mg/day. Slide 32

CASE 1 (2 of 4) • On physical examination, blood pressure is 121/82 mm. Hg and resting heart rate is 70 beats per minute. • Serum chemistries and CBC are within normal limits. • ECG shows no conduction delays and no ischemic changes. • Other than osteoarthritic changes in both knees, left worse than right, her examination is unremarkable. Slide 33
CASE 1 (3 of 4) Which of the following is most appropriate for perioperative management of this patient? A. Increase atenolol dosage to 50 mg/d; continue perioperatively. B. Discontinue atenolol immediately before surgery; restart 48 hours after surgery. C. Continue atenolol at the current dosage. D. Discontinue atenolol; begin an ACE inhibitor plus a statin. Slide 34
CASE 1 (4 of 4) Which of the following is most appropriate for perioperative management of this patient? A. Increase atenolol dosage to 50 mg/d; continue perioperatively. B. Discontinue atenolol immediately before surgery; restart 48 hours after surgery. C. Continue atenolol at the current dosage. D. Discontinue atenolol; begin an ACE inhibitor plus a statin. Slide 35
CASE 2 (1 of 4) • An 80 -year-old man is brought to the ER because his cognition is rapidly deteriorating, his temperature is 39. 4°C (103 o. F), and he has upper abdominal pain. • His family reports that he has steroid-dependent COPD. • He smokes one-half pack of cigarettes daily. • He has not been eating well and has lost 4. 5 kg (10 lb) over the last 4 months. Slide 36
CASE 2 (2 of 4) • The patient uses a walker to ambulate short distances within the house and is dependent on his family for all IADLs. • Surgical evaluation and ultrasound study are highly suggestive of cholecystitis and possible abscess. • Admission laboratory data show a WBC count of 19 × 103/mm 3 and a BUN of 32 mg/d. L. • He is vigorously rehydrated before undergoing emergent cholecystectomy under general anesthesia. Slide 37
CASE 2 (3 of 4) Which of the following is most likely to reduce the patient’s risk of postoperative pulmonary complications? A. Incentive spirometry B. Total parenteral hyperalimentation C. Postoperative epidural analgesia D. Routine nasogastric decompression Slide 38
CASE 2 (4 of 4) Which of the following is most likely to reduce the patient’s risk of postoperative pulmonary complications? A. Incentive spirometry B. Total parenteral hyperalimentation C. Postoperative epidural analgesia D. Routine nasogastric decompression Slide 39
CASE 3 (1 of 4) • A 76 -year-old woman comes from a rehabilitation facility to the hospital after she falls and fractures her right hip. • She was recovering from a recent hospitalization for pneumonia and exacerbation of COPD that left her profoundly deconditioned. • She uses a combined steroid and long-acting β-agonist inhaler and takes oral steroids for exacerbations. She is not oxygen-dependent. • She has no history of dementia but believes she has been more forgetful over the past year. Slide 40
CASE 3 (2 of 4) • The patient is vigorously hydrated, her pain is controlled with narcotics, and surgery is planned for the next morning under general anesthesia. Slide 41
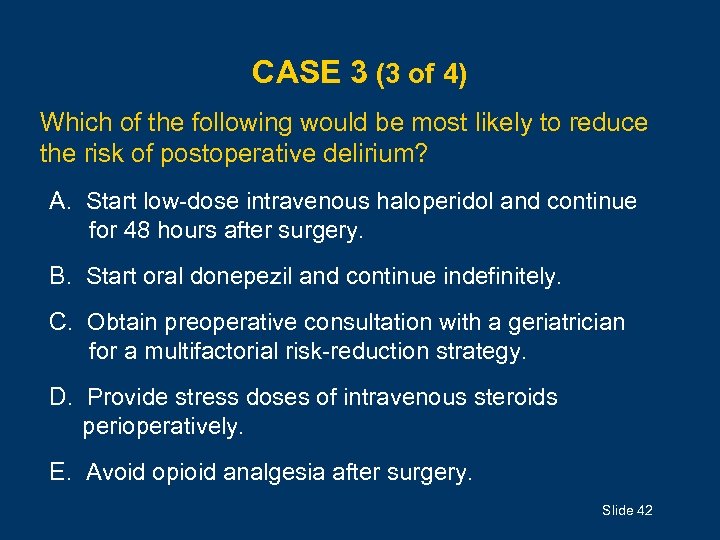
CASE 3 (3 of 4) Which of the following would be most likely to reduce the risk of postoperative delirium? A. Start low-dose intravenous haloperidol and continue for 48 hours after surgery. B. Start oral donepezil and continue indefinitely. C. Obtain preoperative consultation with a geriatrician for a multifactorial risk-reduction strategy. D. Provide stress doses of intravenous steroids perioperatively. E. Avoid opioid analgesia after surgery. Slide 42

CASE 3 (4 of 4) Which of the following would be most likely to reduce the risk of postoperative delirium? A. Start low-dose intravenous haloperidol and continue for 48 hours after surgery. B. Start oral donepezil and continue indefinitely. C. Obtain preoperative consultation with a geriatrician for a multifactorial risk-reduction strategy. D. Provide stress doses of intravenous steroids perioperatively. E. Avoid opioid analgesia after surgery. Slide 43
ACKNOWLEDGMENTS Editor: Annie Medina-Walpole, MD GRS 7 Chapter Authors: Colleen Christmas, MD James T. Pacala, MD, MS GRS 7 Question Writer: Michael C. Lindberg, MD Pharmacotherapy Editor: Judith L. Beizer, Pharm. D Medical Writers: Beverly A. Caley Faith Reidenbach Managing Editor: Andrea N. Sherman, MS Copyright © 2010 American Geriatrics Society Slide 44
35b1966b5862736bec8636d452faacf3.ppt