76af9014dd379bb3e77a4156cd3a68af.ppt
- Количество слайдов: 40
 PERINATAL MOOD ANXIETY DISORDERS (PMADS)
PERINATAL MOOD ANXIETY DISORDERS (PMADS)
 2 Outline • PMADs Overview • Risk Factors • Types • Impact • Building Counseling Skills to Support Families • Considerations • Conversation tips • Sharing Resources & Information • Support for mom’s emotional health
2 Outline • PMADs Overview • Risk Factors • Types • Impact • Building Counseling Skills to Support Families • Considerations • Conversation tips • Sharing Resources & Information • Support for mom’s emotional health
 3 Objectives § Staff will identify 3 types of PMADs and their symptoms. § Staff will identify 2 ways in which PMADs impact pregnancy, birth outcomes, and the postpartum period. § Staff will describe 2 strategies to integrate the subject of maternal mental health into their work with women. § Staff will list 2 resources to support WIC participants who have or are at risk for perinatal mental health concerns.
3 Objectives § Staff will identify 3 types of PMADs and their symptoms. § Staff will identify 2 ways in which PMADs impact pregnancy, birth outcomes, and the postpartum period. § Staff will describe 2 strategies to integrate the subject of maternal mental health into their work with women. § Staff will list 2 resources to support WIC participants who have or are at risk for perinatal mental health concerns.
 4 PMAD Overview • Why do we say “Perinatal” Mood Disorders and not just “Postpartum Depression”? • Can occur during pregnancy • Can occur after pregnancy loss • Can occur up to one year postpartum • Why do we say “Mood & Anxiety” Disorders and not just “Depression? • Anxiety is a common characteristic • Sometimes women are more anxious than depressed • Depression is a separate illness
4 PMAD Overview • Why do we say “Perinatal” Mood Disorders and not just “Postpartum Depression”? • Can occur during pregnancy • Can occur after pregnancy loss • Can occur up to one year postpartum • Why do we say “Mood & Anxiety” Disorders and not just “Depression? • Anxiety is a common characteristic • Sometimes women are more anxious than depressed • Depression is a separate illness
 5 • What is the difference between PMADs and “Baby Blues”? • “Baby Blues” are short term. Many new moms feel weepy and anxious during the first few weeks after giving birth. • “Baby Blues” goes away with rest, support and time. • The symptoms of “Baby Blues” rarely get in the way of daily life or need intervention from a medical provider
5 • What is the difference between PMADs and “Baby Blues”? • “Baby Blues” are short term. Many new moms feel weepy and anxious during the first few weeks after giving birth. • “Baby Blues” goes away with rest, support and time. • The symptoms of “Baby Blues” rarely get in the way of daily life or need intervention from a medical provider
 Risk Factors for PMADs • Previous perinatal mood disorder • History of mood disorders • Sensitivity to hormonal changes • Poverty • Low social support • Under age 18
Risk Factors for PMADs • Previous perinatal mood disorder • History of mood disorders • Sensitivity to hormonal changes • Poverty • Low social support • Under age 18
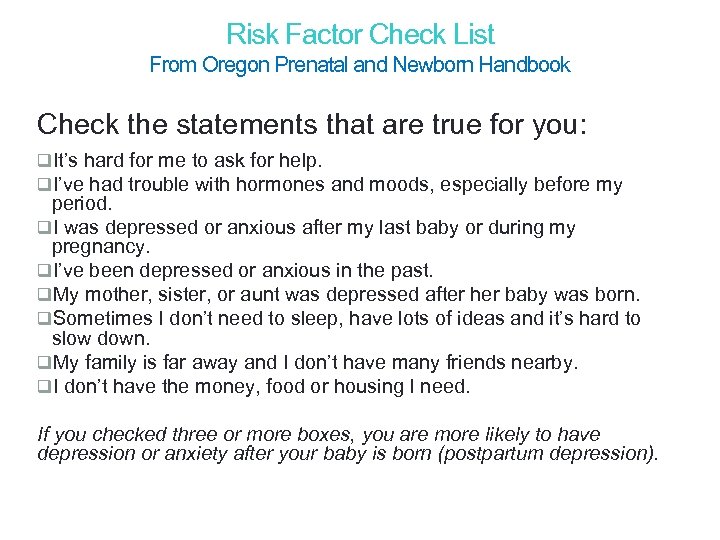 Risk Factor Check List 7 From Oregon Prenatal and Newborn Handbook Check the statements that are true for you: q. It’s hard for me to ask for help. q. I’ve had trouble with hormones and moods, especially before my period. q. I was depressed or anxious after my last baby or during my pregnancy. q. I’ve been depressed or anxious in the past. q. My mother, sister, or aunt was depressed after her baby was born. q. Sometimes I don’t need to sleep, have lots of ideas and it’s hard to slow down. q. My family is far away and I don’t have many friends nearby. q. I don’t have the money, food or housing I need. If you checked three or more boxes, you are more likely to have depression or anxiety after your baby is born (postpartum depression).
Risk Factor Check List 7 From Oregon Prenatal and Newborn Handbook Check the statements that are true for you: q. It’s hard for me to ask for help. q. I’ve had trouble with hormones and moods, especially before my period. q. I was depressed or anxious after my last baby or during my pregnancy. q. I’ve been depressed or anxious in the past. q. My mother, sister, or aunt was depressed after her baby was born. q. Sometimes I don’t need to sleep, have lots of ideas and it’s hard to slow down. q. My family is far away and I don’t have many friends nearby. q. I don’t have the money, food or housing I need. If you checked three or more boxes, you are more likely to have depression or anxiety after your baby is born (postpartum depression).
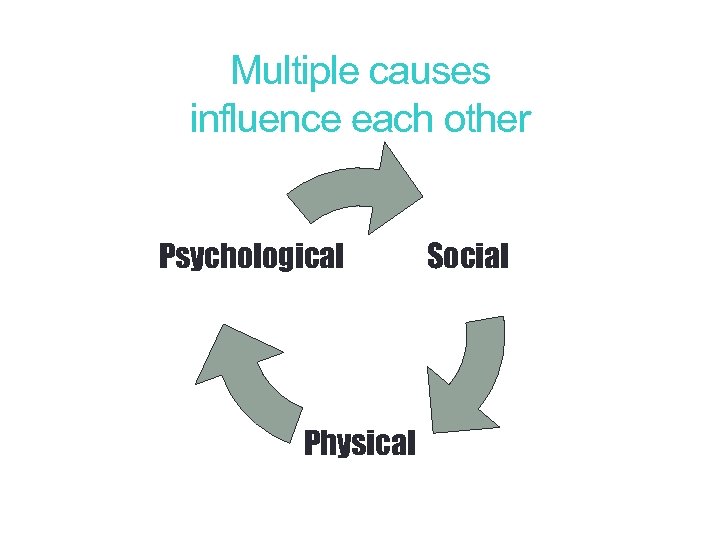 8 Multiple causes influence each other Psychological Physical Social
8 Multiple causes influence each other Psychological Physical Social
 Types of PMADs • Prenatal depression or anxiety • Postpartum depression (PPD) • Postpartum anxiety or panic disorder • Postpartum obsessive-compulsive disorder (OCD) • Postpartum Psychosis
Types of PMADs • Prenatal depression or anxiety • Postpartum depression (PPD) • Postpartum anxiety or panic disorder • Postpartum obsessive-compulsive disorder (OCD) • Postpartum Psychosis
 10 Prenatal Depression or Anxiety Prenatal Depression: …“I am going to act as though everything is fine but I am terrified of what lies ahead. ”
10 Prenatal Depression or Anxiety Prenatal Depression: …“I am going to act as though everything is fine but I am terrified of what lies ahead. ”
 11 Postpartum Depression (PPD) Incidence: Overall: 13. 6% Teen Moms: 26% Moms of Multiples: 25% Adoptive Moms: 8%
11 Postpartum Depression (PPD) Incidence: Overall: 13. 6% Teen Moms: 26% Moms of Multiples: 25% Adoptive Moms: 8%
 12 Postpartum Anxiety or Panic Disorder “I finally told my husband that he and my daughter would be better off without me—that I was not a good mother or wife. I felt like things were never going to get better—that I would never feel happy again. ”
12 Postpartum Anxiety or Panic Disorder “I finally told my husband that he and my daughter would be better off without me—that I was not a good mother or wife. I felt like things were never going to get better—that I would never feel happy again. ”
 13 Postpartum Obsessive-Compulsive Disorder PMADs can be present in any family. Existing mental health issues can be intensified with pregnancy and delivery.
13 Postpartum Obsessive-Compulsive Disorder PMADs can be present in any family. Existing mental health issues can be intensified with pregnancy and delivery.
 Postpartum Psychosis Depression doesn’t turn into psychosis. Psychosis is a real break from reality and becomes a medical emergency Incidence of Postpartum Psychosis: 0. 1 to 0. 2% “…My children weren't righteous. They stumbled because I was evil. The way I was raising them they could never be saved. They were doomed to perish in the fires of hell. ”
Postpartum Psychosis Depression doesn’t turn into psychosis. Psychosis is a real break from reality and becomes a medical emergency Incidence of Postpartum Psychosis: 0. 1 to 0. 2% “…My children weren't righteous. They stumbled because I was evil. The way I was raising them they could never be saved. They were doomed to perish in the fires of hell. ”
 15 Impact of Untreated Perinatal Mood Disorders In Oregon, one in four new moms reports feeling depressed or anxious during or after pregnancy (PRAMS study)
15 Impact of Untreated Perinatal Mood Disorders In Oregon, one in four new moms reports feeling depressed or anxious during or after pregnancy (PRAMS study)
 Pregnancy Complications • Inadequate Prenatal Care • Poor Nutrition • Fears of Childbirth • Risk of Substance Abuse
Pregnancy Complications • Inadequate Prenatal Care • Poor Nutrition • Fears of Childbirth • Risk of Substance Abuse
 17 Birth Complications • Premature Labor • Low Birth Weight • Maternal Hypertension • Increased Rates of Miscarriage
17 Birth Complications • Premature Labor • Low Birth Weight • Maternal Hypertension • Increased Rates of Miscarriage
 18 Postpartum Impacts • Impaired mother-infant bonding, moms avoid connecting • Anxious mothering, moms can be over-sensitive and over- reactive • Negative maternal identity and low self esteem, moms can be highly self critical • Isolation from social support • Increased family conflicts
18 Postpartum Impacts • Impaired mother-infant bonding, moms avoid connecting • Anxious mothering, moms can be over-sensitive and over- reactive • Negative maternal identity and low self esteem, moms can be highly self critical • Isolation from social support • Increased family conflicts
 19 Effects on Toddlers and Older Children • Symptoms mimic mom’s depressed behavior • Higher risk for mood disorders • Poor peer relationships • Poor self-control • Neurological delays • Attention problems
19 Effects on Toddlers and Older Children • Symptoms mimic mom’s depressed behavior • Higher risk for mood disorders • Poor peer relationships • Poor self-control • Neurological delays • Attention problems
 Building Counseling Skills to Support Families • How can we help women when they don’t know what’s wrong? • How do we reassure women when they are afraid to disclose that they need help? • How can we reduce shame and normalize the new mother’s need for support?
Building Counseling Skills to Support Families • How can we help women when they don’t know what’s wrong? • How do we reassure women when they are afraid to disclose that they need help? • How can we reduce shame and normalize the new mother’s need for support?
 21 Counseling Goals • Utilize participant centered skills to create a safe, comfortable environment for conversation • Integrate subject naturally • Reduce fear of disclosure • Encourage small action steps • Support mother-baby bonding
21 Counseling Goals • Utilize participant centered skills to create a safe, comfortable environment for conversation • Integrate subject naturally • Reduce fear of disclosure • Encourage small action steps • Support mother-baby bonding
 22 Counseling Considerations • Primary focus on baby might miss mom’s distress • If mom is depressed or anxious, usual suggestions for new moms might not work well • Watch for signs that she is trying too hard to be agreeable or is overwhelmed • Break down suggestions into small, achievable steps
22 Counseling Considerations • Primary focus on baby might miss mom’s distress • If mom is depressed or anxious, usual suggestions for new moms might not work well • Watch for signs that she is trying too hard to be agreeable or is overwhelmed • Break down suggestions into small, achievable steps
 23 Picking Up On Cues • Depression • Withdrawn • Distant • Flatness of facial expression and voice • Anxiety • Repetitive fears and questions • Over-protective • Too well put-together
23 Picking Up On Cues • Depression • Withdrawn • Distant • Flatness of facial expression and voice • Anxiety • Repetitive fears and questions • Over-protective • Too well put-together
 24 Motherhood Myths • Social myths about joyous and selfless motherhood make depressed anxious moms feel worse. • Moms feel guilty and embarrassed about the feelings and thoughts that arise with maternal depression and anxiety. • Most depressed moms don’t recognize that what they are feeling is depression; they feel they are failing. • Counselors are challenged to reduce shame and normalize new mother’s need for support
24 Motherhood Myths • Social myths about joyous and selfless motherhood make depressed anxious moms feel worse. • Moms feel guilty and embarrassed about the feelings and thoughts that arise with maternal depression and anxiety. • Most depressed moms don’t recognize that what they are feeling is depression; they feel they are failing. • Counselors are challenged to reduce shame and normalize new mother’s need for support
 25 Conversation tips about motherhood myths • “Becoming a parent can be a tough transition. We talk to all our families about emotions and mental health. How you have been feeling? ” • “Lots of women tell us that being a new mom is harder than they expected. How has it been for you? ” • “You are not to blame for your feelings; this is a normal part of becoming a mother for many women. ”
25 Conversation tips about motherhood myths • “Becoming a parent can be a tough transition. We talk to all our families about emotions and mental health. How you have been feeling? ” • “Lots of women tell us that being a new mom is harder than they expected. How has it been for you? ” • “You are not to blame for your feelings; this is a normal part of becoming a mother for many women. ”
 26 Social Relationships • Depressed anxious moms are usually embarrassed and afraid of judgment. • A depressed or anxious mom might appear to be okay, but is truly feeling insecure and upset. She is working very hard to look good. • She needs reassurance that it is healthy to talk about difficulties and reach out for help.
26 Social Relationships • Depressed anxious moms are usually embarrassed and afraid of judgment. • A depressed or anxious mom might appear to be okay, but is truly feeling insecure and upset. She is working very hard to look good. • She needs reassurance that it is healthy to talk about difficulties and reach out for help.
 27 Conversation tips about social relationships • “What are your questions about emotions and mental health? ” • “It looks like you’re taking good care of your baby. Motherhood can be hard work. How are you finding time to take care of yourself too? ” • “Thank you for telling me how you’re doing. It is really healthy to speak up. Have you told anyone else how you are feeling? ”
27 Conversation tips about social relationships • “What are your questions about emotions and mental health? ” • “It looks like you’re taking good care of your baby. Motherhood can be hard work. How are you finding time to take care of yourself too? ” • “Thank you for telling me how you’re doing. It is really healthy to speak up. Have you told anyone else how you are feeling? ”
 28 Attachment and Bonding • Bonding difficulties: − Moms might appear distant, over-anxious, controlling, − Moms might express negative perceptions of baby − Little physical contact or tentative/insecure contact − Mom might perceive herself negatively • It’s important to objectively assess mom and baby interactions − Mom might just be tired!
28 Attachment and Bonding • Bonding difficulties: − Moms might appear distant, over-anxious, controlling, − Moms might express negative perceptions of baby − Little physical contact or tentative/insecure contact − Mom might perceive herself negatively • It’s important to objectively assess mom and baby interactions − Mom might just be tired!
 29 Conversation tips about attachment and bonding • • • “Oh, look how that baby looks at you when s/he hears your voice. ” “How are you feeling when you're with your baby? ” “What questions do you have about ways to connect or play with your baby? ”
29 Conversation tips about attachment and bonding • • • “Oh, look how that baby looks at you when s/he hears your voice. ” “How are you feeling when you're with your baby? ” “What questions do you have about ways to connect or play with your baby? ”
 30 Importance of Self-Care Strategies • Moms need both support and self-care • Self-care is essential to health and recovery • How do we help a depressed parent feel empowered to initiate change? • What are some supportive ways we can help a mom put herself on her list of priorities?
30 Importance of Self-Care Strategies • Moms need both support and self-care • Self-care is essential to health and recovery • How do we help a depressed parent feel empowered to initiate change? • What are some supportive ways we can help a mom put herself on her list of priorities?
 31 Examples of Self-Care Strategies • supportive relationships • peer support • healthy nutrition • physical activity • sleep/rest • taking breaks • positive coping strategies • stress-reduction techniques • reaching out for help (practical and supportive)
31 Examples of Self-Care Strategies • supportive relationships • peer support • healthy nutrition • physical activity • sleep/rest • taking breaks • positive coping strategies • stress-reduction techniques • reaching out for help (practical and supportive)
 32 Conversation tips about small steps toward healthy goals • “Remember that you will feel better, one step at a time. It helps to start with small steps, and build from there. ” • “Yes, they say what you need to do but they might forget how hard it can be to get going. Some moms find it helpful to start small. For example, if you wanted to exercise more, you can just step outside for a few minutes each day, then you can add a little walk, then build up from there”
32 Conversation tips about small steps toward healthy goals • “Remember that you will feel better, one step at a time. It helps to start with small steps, and build from there. ” • “Yes, they say what you need to do but they might forget how hard it can be to get going. Some moms find it helpful to start small. For example, if you wanted to exercise more, you can just step outside for a few minutes each day, then you can add a little walk, then build up from there”
 33 Helping Mom Reach Out • Listen without judgment • Encourage or help her talk to her healthcare and mental health provider • She can reach out to resources for any question related to support/stress during or after pregnancy. No diagnosis is needed to seek help • Help her find Oregon support at www. postpartum. net/gethelp • Encourage or help her call the Support Warmline • Offer referral to a public health nurse
33 Helping Mom Reach Out • Listen without judgment • Encourage or help her talk to her healthcare and mental health provider • She can reach out to resources for any question related to support/stress during or after pregnancy. No diagnosis is needed to seek help • Help her find Oregon support at www. postpartum. net/gethelp • Encourage or help her call the Support Warmline • Offer referral to a public health nurse
 34 Sharing Resources & Information • What is your role in sharing resources? • Practicing PCE skills • Use Active Listening Skills • Normalize the subject • Find out what she already knows • Avoid judgment • Offer menu of options for follow up • Share resources and offer referrals
34 Sharing Resources & Information • What is your role in sharing resources? • Practicing PCE skills • Use Active Listening Skills • Normalize the subject • Find out what she already knows • Avoid judgment • Offer menu of options for follow up • Share resources and offer referrals
 35 Oregon Resources • Postpartum Support International, Oregon 1 -800 -944 -4 PPD (800 -944 -4773) • English & Spanish • Telephone Help Line for support & resources • Connects with support volunteers • www. postpartum. net • Oregon Health Authority Website • www. healthoregon. org/perinatalmentalhealth • 211
35 Oregon Resources • Postpartum Support International, Oregon 1 -800 -944 -4 PPD (800 -944 -4773) • English & Spanish • Telephone Help Line for support & resources • Connects with support volunteers • www. postpartum. net • Oregon Health Authority Website • www. healthoregon. org/perinatalmentalhealth • 211
 36 Parent Education Materials • OHA Website www. healthoregon. org/perinatalmentalhealth • Parent Brochure from OHA • HRSA brochure – in English and Spanish (Health Resources and Services Administration) http: //mchb. hrsa. gov/pregnancyandbeyond/depression/morethanbl ues. htm
36 Parent Education Materials • OHA Website www. healthoregon. org/perinatalmentalhealth • Parent Brochure from OHA • HRSA brochure – in English and Spanish (Health Resources and Services Administration) http: //mchb. hrsa. gov/pregnancyandbeyond/depression/morethanbl ues. htm
 37 Online Resources for Families • www. postpartumprogress. com • www. ppdsupportpage. com • www. mededppd. org/mothers • www. postpartumdads. org • www. postpartum. net
37 Online Resources for Families • www. postpartumprogress. com • www. ppdsupportpage. com • www. mededppd. org/mothers • www. postpartumdads. org • www. postpartum. net
 38 Emergency Resources • In an emergency, call 911 or go to your nearest emergency room • Local or Regional Mental Health Crisis Hotlines • National Suicide Hotline v 1 -800 -273 -TALK (800 -273 -8255)
38 Emergency Resources • In an emergency, call 911 or go to your nearest emergency room • Local or Regional Mental Health Crisis Hotlines • National Suicide Hotline v 1 -800 -273 -TALK (800 -273 -8255)
 39 Food for Thought… • If you were a depressed or anxious mom, what would you want the WIC staff to say? How should they say it? What would you want them to ask? • What resources in our community might be the most helpful to WIC moms with perinatal depression and anxiety? • What other questions do you have about PMADs? Your state nutrition consultant can be a resource.
39 Food for Thought… • If you were a depressed or anxious mom, what would you want the WIC staff to say? How should they say it? What would you want them to ask? • What resources in our community might be the most helpful to WIC moms with perinatal depression and anxiety? • What other questions do you have about PMADs? Your state nutrition consultant can be a resource.
 40 This presentation is based on work done by : Perinatal Mood Disorders Trainer Wendy N. Davis, Ph. D Postpartum Support International, Executive Director wdavis@postpartum. net 503 -246 -0941
40 This presentation is based on work done by : Perinatal Mood Disorders Trainer Wendy N. Davis, Ph. D Postpartum Support International, Executive Director wdavis@postpartum. net 503 -246 -0941


