1f6152a605e9d0ce1d3a5406722843b1.ppt
- Количество слайдов: 46
 PERCEPTION Dr. Fernandez OTR 615
PERCEPTION Dr. Fernandez OTR 615
 Key to Success Identify the Root of the problem Is the problem a auditory processing disorder Is the Problem a visual processing disorder Is the problem a timing, concentration/motor processing disorder
Key to Success Identify the Root of the problem Is the problem a auditory processing disorder Is the Problem a visual processing disorder Is the problem a timing, concentration/motor processing disorder
 Visual Attention Deficit Decrease ability to attend to , focus or discriminate for detail Focus on tangential elements of a task rather than on the main elements or goal
Visual Attention Deficit Decrease ability to attend to , focus or discriminate for detail Focus on tangential elements of a task rather than on the main elements or goal
 Functional treatment for Visual Attention Deficits Work in a quiet area and start having them focus for short periods of time. Have patient set goals of time if possible Start with patient attending to large objects first, then add on, moving to smaller and increase numbers of items to work with Add variables of color, size, speed
Functional treatment for Visual Attention Deficits Work in a quiet area and start having them focus for short periods of time. Have patient set goals of time if possible Start with patient attending to large objects first, then add on, moving to smaller and increase numbers of items to work with Add variables of color, size, speed
 Visual Tracking Deficit Decrease ability to read without skipping lines and losing ones place. Squinting, rubbing eye Double vision Difficulty tracking moving objects Writes crooked or poorly spaced Avoidance of reading.
Visual Tracking Deficit Decrease ability to read without skipping lines and losing ones place. Squinting, rubbing eye Double vision Difficulty tracking moving objects Writes crooked or poorly spaced Avoidance of reading.
 Functional treatments for Visual Tracking Deficits Vision therapy Eye exercises/orthoptics/visual training Utilize the Amsler Grid Vision tracking Goggles (Visagraph II) Symmetrical pursuit training
Functional treatments for Visual Tracking Deficits Vision therapy Eye exercises/orthoptics/visual training Utilize the Amsler Grid Vision tracking Goggles (Visagraph II) Symmetrical pursuit training
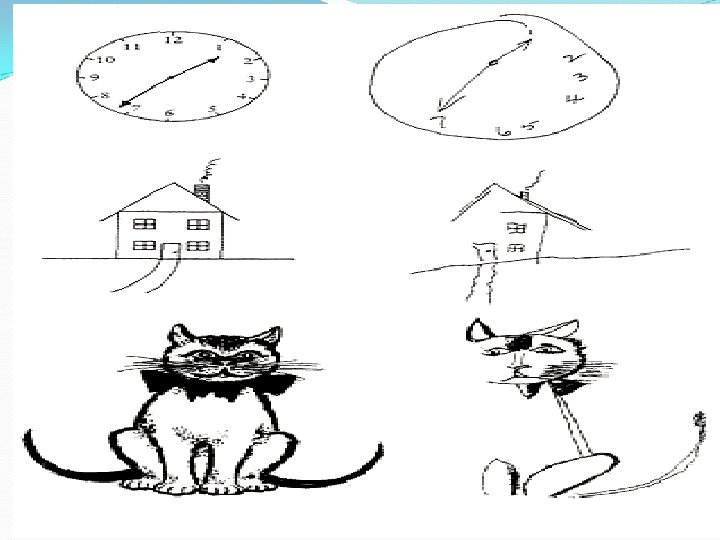
 Unilateral Neglect Inferior parietal lobe/no dominant hemisphere Inability to integrate sensory input from one side of the body (usually the left) and from one side of the environment Patient neglects to wash one side of the body/shave/eat food from one half of his plate Reading from the middle of the line/article Bumping into furniture on one side Applies make-up on one side of the face combs, hair on one side only
Unilateral Neglect Inferior parietal lobe/no dominant hemisphere Inability to integrate sensory input from one side of the body (usually the left) and from one side of the environment Patient neglects to wash one side of the body/shave/eat food from one half of his plate Reading from the middle of the line/article Bumping into furniture on one side Applies make-up on one side of the face combs, hair on one side only
 Functional treatment for Unilateral Neglect Activities to stimulate the neglected side(brushing, rubbing, ice, vibration) while patient watching Movement of neglected side(while patient watches) either actively or passively Activities that force the patient to look to the neglected side For the patient having trouble reading/writing utilize a red line down the side of the page on the neglected side as a cue Teaching the patient to monitor visually both the position and movement of the neglected side
Functional treatment for Unilateral Neglect Activities to stimulate the neglected side(brushing, rubbing, ice, vibration) while patient watching Movement of neglected side(while patient watches) either actively or passively Activities that force the patient to look to the neglected side For the patient having trouble reading/writing utilize a red line down the side of the page on the neglected side as a cue Teaching the patient to monitor visually both the position and movement of the neglected side
 Continued…Unilateral neglect For the patient that turns to the uninvolved side when operating a wheelchair, placement of a tape on the floor as a guide For the patient who has not yet learned to compensate for his deficits, placement of food, telephone, call light, etc. On the uninvolved side Keep the affected side in visual field, lap tray/pillow
Continued…Unilateral neglect For the patient that turns to the uninvolved side when operating a wheelchair, placement of a tape on the floor as a guide For the patient who has not yet learned to compensate for his deficits, placement of food, telephone, call light, etc. On the uninvolved side Keep the affected side in visual field, lap tray/pillow
 Body Scheme Deficits (somatognosia) Parietal lobe/dominant hemisphere Lack of awareness of body structure Patient fails to recognize his/her own body parts Inability to recognize the relations between his/her body parts Difficulty in orientation of his body to the environment to the outside world Confusion to his /her side of the body Difficulty in contra lateral movements Inability to distinguish between therapist extremities and his own
Body Scheme Deficits (somatognosia) Parietal lobe/dominant hemisphere Lack of awareness of body structure Patient fails to recognize his/her own body parts Inability to recognize the relations between his/her body parts Difficulty in orientation of his body to the environment to the outside world Confusion to his /her side of the body Difficulty in contra lateral movements Inability to distinguish between therapist extremities and his own

 Functional treatment for Body Scheme Deficits Practice of activities that require patient to name body parts Practice of activities that require patient to explore the relations between body parts( eg. , puzzles of human body, imitating postures) Reinforcement of awareness of body parts by having patient tactilely stimulate parts of the body as they are named by therapist(e. g. , patient rubs, brushes, strokes , or washes part named by therapist
Functional treatment for Body Scheme Deficits Practice of activities that require patient to name body parts Practice of activities that require patient to explore the relations between body parts( eg. , puzzles of human body, imitating postures) Reinforcement of awareness of body parts by having patient tactilely stimulate parts of the body as they are named by therapist(e. g. , patient rubs, brushes, strokes , or washes part named by therapist
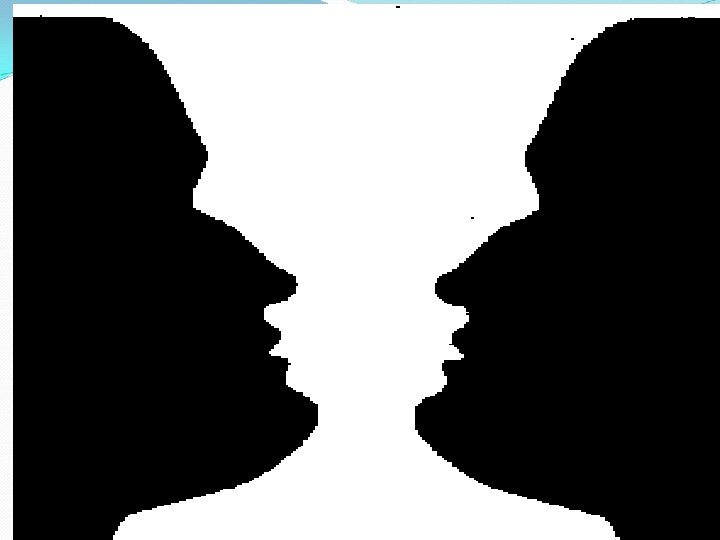
 Figure Ground Deficit Parietal lobe Difficulty in differentiating foreground from back ground Difficulty finding items/ things in especially cluttered areas Difficulty in finding sleeves/opening in sleeve or leg opening in pants Difficulty finding the brakes on the wheelchair/difference finding the wheels from the arm rest Difficulty finding hidden pictures, picking one line of prints from another while reading
Figure Ground Deficit Parietal lobe Difficulty in differentiating foreground from back ground Difficulty finding items/ things in especially cluttered areas Difficulty in finding sleeves/opening in sleeve or leg opening in pants Difficulty finding the brakes on the wheelchair/difference finding the wheels from the arm rest Difficulty finding hidden pictures, picking one line of prints from another while reading


 Functional treatment for Figure Ground Deficits to outline/highlight the object 9 e. g. , ribbon Color cues around brake of wheelchair, colored tape/tread around sleeve of shirt or pant leg. Adaptation of the environment to make it simple and uncluttered Use of dividers to separate items in drawers Placement of only a few things on bedside table Organization of meal tray so that it has only a few items on it(I. e, meals served in courses Compensation for deficits by very systematic examination of each small area, both visually and tactilely Practice of functional activity until the patient can do the automatically Random scattering of a few objects for patient to name
Functional treatment for Figure Ground Deficits to outline/highlight the object 9 e. g. , ribbon Color cues around brake of wheelchair, colored tape/tread around sleeve of shirt or pant leg. Adaptation of the environment to make it simple and uncluttered Use of dividers to separate items in drawers Placement of only a few things on bedside table Organization of meal tray so that it has only a few items on it(I. e, meals served in courses Compensation for deficits by very systematic examination of each small area, both visually and tactilely Practice of functional activity until the patient can do the automatically Random scattering of a few objects for patient to name
 Depth Perception Deficit Parietal lobe of either hemisphere Difficulty in perceiving spatial relationships between objects or between objects and self
Depth Perception Deficit Parietal lobe of either hemisphere Difficulty in perceiving spatial relationships between objects or between objects and self
 Functional treatment of Depth Perception Deficits Have patient practice functional tasks that require him/her to judge distance and depth(e. g. , walking up and down steps of varying height, walking through a furniture maze Have patient try to determine distance to objects visually and verify his judgment by pacing out distance to see which objects actually are farther away or closer Have patient verify visual space determinations by tactile sensation(e. g. , pour a cup of water to what seems full and verify by putting his finger inside the top of the glass Have patient follow maps to navigate between points A and B
Functional treatment of Depth Perception Deficits Have patient practice functional tasks that require him/her to judge distance and depth(e. g. , walking up and down steps of varying height, walking through a furniture maze Have patient try to determine distance to objects visually and verify his judgment by pacing out distance to see which objects actually are farther away or closer Have patient verify visual space determinations by tactile sensation(e. g. , pour a cup of water to what seems full and verify by putting his finger inside the top of the glass Have patient follow maps to navigate between points A and B

 Form Constancy Deficit Parietal lobe lesion Inability to attend to subtle variation in form: inability to differentiate objects of similar shapes( water pitcher/urinal) Difficulty sorting task Difficulty sorting R from L sleeve
Form Constancy Deficit Parietal lobe lesion Inability to attend to subtle variation in form: inability to differentiate objects of similar shapes( water pitcher/urinal) Difficulty sorting task Difficulty sorting R from L sleeve
 Functional treatment of Form Constancy Matching activities, sorting activities, and activities to duplicate printed patterns Presentation of an object in various position and sizes for patient to identify it.
Functional treatment of Form Constancy Matching activities, sorting activities, and activities to duplicate printed patterns Presentation of an object in various position and sizes for patient to identify it.

 Position in Space Deficit Parietal lobe non-dominant hemisphere Difficulty in interpreting position in space (up -down, in-out, front- behind) Difficulty in navigating both in w/c and upright Failure to look under or behind Decrease midline orientation
Position in Space Deficit Parietal lobe non-dominant hemisphere Difficulty in interpreting position in space (up -down, in-out, front- behind) Difficulty in navigating both in w/c and upright Failure to look under or behind Decrease midline orientation
 Functional treatments for Position in Space Deficits Practice of functional tasks that require the patient to use the concept of position in space (e. g. , stacking cans, organizing food pantry, organizing closets) Work with building blocks, following verbal or written instructions Obstacle courses, maze
Functional treatments for Position in Space Deficits Practice of functional tasks that require the patient to use the concept of position in space (e. g. , stacking cans, organizing food pantry, organizing closets) Work with building blocks, following verbal or written instructions Obstacle courses, maze
 Spatial Relationship Deficit Parietal lobe non-dominant hemisphere Problems perceiving the position of two or more objects in relations with self Problems perceiving the position of two objects in relations to each other Difficulty in processing mirror images Difficulty in judging the relative position of one object to another(directionality) and the internal awareness of the two sides of the body(laterality. )
Spatial Relationship Deficit Parietal lobe non-dominant hemisphere Problems perceiving the position of two or more objects in relations with self Problems perceiving the position of two objects in relations to each other Difficulty in processing mirror images Difficulty in judging the relative position of one object to another(directionality) and the internal awareness of the two sides of the body(laterality. )
 Functional treatments for Spatial Relationship Deficits Practice of task in which patient must orient himself in space (e. g. , navigating around furniture, maze) either following verbal instructions or following a map Practice of task in which patient must orient object to object (e. g. , copying tasks, making blocks and peg boards designs, connecting dots, converting 2 D drawings to 3 D ones with blocks
Functional treatments for Spatial Relationship Deficits Practice of task in which patient must orient himself in space (e. g. , navigating around furniture, maze) either following verbal instructions or following a map Practice of task in which patient must orient object to object (e. g. , copying tasks, making blocks and peg boards designs, connecting dots, converting 2 D drawings to 3 D ones with blocks
 Visual Discrimination Deficit Left-Right Inability to differentiate between R-L sides of the body either own body or another persons Decrease ability to differentiate between two similar objects ( letter m/n)
Visual Discrimination Deficit Left-Right Inability to differentiate between R-L sides of the body either own body or another persons Decrease ability to differentiate between two similar objects ( letter m/n)
 Functional treatments for Visual Discrimination Deficits Giving on side of the body augmented tactile and proprioceptive input (e. g. , have patient wear weighted cuff on one side extremities Quizzing patient on right versus left discrimination (e. g. , show me your right hand) Including the terms right and left when practicing functional skills (e. g. , you are putting on your right shoe, you wear your watch on your left arm)
Functional treatments for Visual Discrimination Deficits Giving on side of the body augmented tactile and proprioceptive input (e. g. , have patient wear weighted cuff on one side extremities Quizzing patient on right versus left discrimination (e. g. , show me your right hand) Including the terms right and left when practicing functional skills (e. g. , you are putting on your right shoe, you wear your watch on your left arm)
 Visual Closure Deficit Decrease ability to visualize the whole of something when only part of it is visible Difficulties in recognizing a picture of someone with a facial feature covered
Visual Closure Deficit Decrease ability to visualize the whole of something when only part of it is visible Difficulties in recognizing a picture of someone with a facial feature covered
 Functional treatments for Visual Closure Deficits Provide matching pictures/items labeled Review whole picture vs incomplete labeled Puzzles of various items Newspaper clipping of item match with name of item Cut pictures of items in half and match halves together
Functional treatments for Visual Closure Deficits Provide matching pictures/items labeled Review whole picture vs incomplete labeled Puzzles of various items Newspaper clipping of item match with name of item Cut pictures of items in half and match halves together
 Visual Memory Deficit Problems in remembering objects Unable to store visual material Unable to recall visually presented material Simultaneously or sequential Individual can not retrieve the mental representation of the object being viewed or make a connection between the mental representation and the object itself Unable to recall and use visual information from the past
Visual Memory Deficit Problems in remembering objects Unable to store visual material Unable to recall visually presented material Simultaneously or sequential Individual can not retrieve the mental representation of the object being viewed or make a connection between the mental representation and the object itself Unable to recall and use visual information from the past
 Functional treatment for Visual Memory Deficits Utilize techniques of repetition Utilize pictures of family/pets/home Utilize memory book with familiar items titled Have familiar items of ADL labeled with picture/ have the sort/categorize items Behavior compensation using external aids Repeat, Repeat
Functional treatment for Visual Memory Deficits Utilize techniques of repetition Utilize pictures of family/pets/home Utilize memory book with familiar items titled Have familiar items of ADL labeled with picture/ have the sort/categorize items Behavior compensation using external aids Repeat, Repeat
 Topographical Orientation Deficit Occipital parietal lobe non-dominant hemisphere Difficulty understanding the relationship of places to one another Difficulty finding way in space Unreliable in transporting self to and from treatment or from room to room or around house
Topographical Orientation Deficit Occipital parietal lobe non-dominant hemisphere Difficulty understanding the relationship of places to one another Difficulty finding way in space Unreliable in transporting self to and from treatment or from room to room or around house
 Functional treatments for Topographical Orientation Use of markers (e. g. , colored dots) to mark the patient’s route between locations, gradual removal of cues Practice of tasks in which patient must go from one place to another Review local maps/ facility map and location
Functional treatments for Topographical Orientation Use of markers (e. g. , colored dots) to mark the patient’s route between locations, gradual removal of cues Practice of tasks in which patient must go from one place to another Review local maps/ facility map and location
 APRAXIA Caused by a lesion in the neural pathways of the brain that contain the learned patterns of movement
APRAXIA Caused by a lesion in the neural pathways of the brain that contain the learned patterns of movement
 Motor Apraxia Loss of kinesthetic memory pattern so that purposeful movement patterns so that purposeful movement cannot be achieved, even though the idea and purpose of the task is understood Defect in execution Inability to carry out a complicated sequence, although simple tasks performed automatically
Motor Apraxia Loss of kinesthetic memory pattern so that purposeful movement patterns so that purposeful movement cannot be achieved, even though the idea and purpose of the task is understood Defect in execution Inability to carry out a complicated sequence, although simple tasks performed automatically

 Constructional Apraxia Difficulty in producing 2 Dor 3 D designs by coping, drawing, or constructing, both on command or spontaneously. Difficulty in performing purposeful acts while using objects in his environment Affects person’s ability to draw or copy simple diagrams or to construct simple figures
Constructional Apraxia Difficulty in producing 2 Dor 3 D designs by coping, drawing, or constructing, both on command or spontaneously. Difficulty in performing purposeful acts while using objects in his environment Affects person’s ability to draw or copy simple diagrams or to construct simple figures
 Ideomotor Apraxia Inability to imitate features or perform a purposeful motor task on command, even though the patient understands the idea or concepts of the task Retained ability to carry out old habitual tasks automatically Motor planning problems Loss of skilled sequence of movement Perseveration of movement
Ideomotor Apraxia Inability to imitate features or perform a purposeful motor task on command, even though the patient understands the idea or concepts of the task Retained ability to carry out old habitual tasks automatically Motor planning problems Loss of skilled sequence of movement Perseveration of movement
 Ideational Apraxia Conceptual Since aphasia can occur concomitantly with apraxia it may be necessary to give short directions and to speak slowly and clearly Component parts of tasks to be taught separately then slowly combined Inability to create a plan for a specific movement Loss of knowledge about the idea of the movements
Ideational Apraxia Conceptual Since aphasia can occur concomitantly with apraxia it may be necessary to give short directions and to speak slowly and clearly Component parts of tasks to be taught separately then slowly combined Inability to create a plan for a specific movement Loss of knowledge about the idea of the movements


