(2)PUD 2rr.ppt
- Количество слайдов: 49
 PEPTIC ULCER DISEASE Dr. Mohammad Qasem Internist
PEPTIC ULCER DISEASE Dr. Mohammad Qasem Internist
 1 - Definition 2 - PREVALENCE 3 - Mucosal Defense 4 – Causes OF PUD 5 - Clinical Presentation 6 - Diagnosis 7 - Differential Diagnosis 8 - Complications 9 - Treatment
1 - Definition 2 - PREVALENCE 3 - Mucosal Defense 4 – Causes OF PUD 5 - Clinical Presentation 6 - Diagnosis 7 - Differential Diagnosis 8 - Complications 9 - Treatment
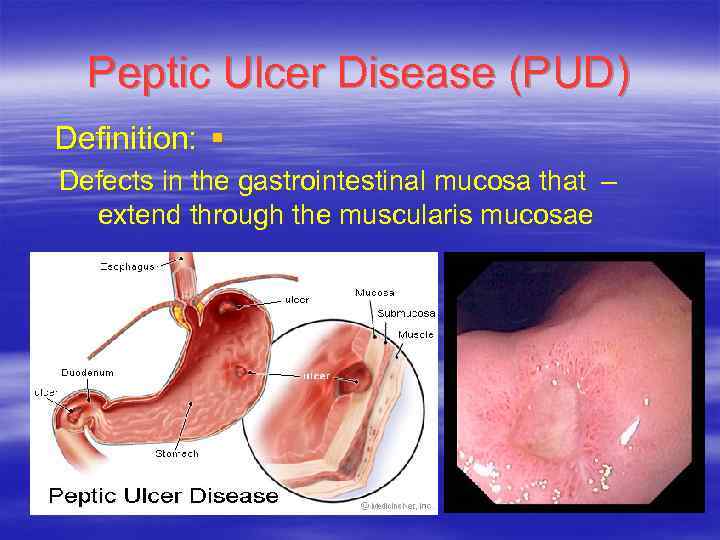 Peptic Ulcer Disease (PUD) Definition: § Defects in the gastrointestinal mucosa that – extend through the muscularis mucosae
Peptic Ulcer Disease (PUD) Definition: § Defects in the gastrointestinal mucosa that – extend through the muscularis mucosae
 Defination Mucosal ulceration near the acid bearing § reagions of the gastrointestinal tract. Duodenum § Stomach § Esophagus § Jejunum in Zollinger-Elison syndrome § Meckle s diverticulum(contain ectopic gastric § mucosa)
Defination Mucosal ulceration near the acid bearing § reagions of the gastrointestinal tract. Duodenum § Stomach § Esophagus § Jejunum in Zollinger-Elison syndrome § Meckle s diverticulum(contain ectopic gastric § mucosa)
 PREVALENCE 4 million new cases in the USA every year § Life time prevalence in males 12% and in § females 10%. 15000 deaths /year in the USA. § Health care coast more than 15 billion /year. §
PREVALENCE 4 million new cases in the USA every year § Life time prevalence in males 12% and in § females 10%. 15000 deaths /year in the USA. § Health care coast more than 15 billion /year. §
 Mucosal Defense Injurious Agents: § Endogenous: HCL, Pepsinogen, pepsine, Bile salts. Exogenous: Drugs, Alcohol, Bacteria The Barrier: § Pre-epithelial, Epithelial and sub-epithelial element
Mucosal Defense Injurious Agents: § Endogenous: HCL, Pepsinogen, pepsine, Bile salts. Exogenous: Drugs, Alcohol, Bacteria The Barrier: § Pre-epithelial, Epithelial and sub-epithelial element
 The Barrier Pre-epithelial: Mucus, Bicarbonate, Surface § phospholipids. Epithelial: Cellular resistance, Restitution, § Growth factors and prostaglandins, Cell proliferation. Sub-epithelial: Blood flow, Leukocytes §
The Barrier Pre-epithelial: Mucus, Bicarbonate, Surface § phospholipids. Epithelial: Cellular resistance, Restitution, § Growth factors and prostaglandins, Cell proliferation. Sub-epithelial: Blood flow, Leukocytes §
 Mucous: secreted by surface epithelial cells § consist of water with lipids and glycoproteins; This forms hydrophobic surface with fatty acids. Also forms a surface water layer that prevents diffusion of ions and substances like pepsin. Bicarbonate: secreted by the surface epithelial § cells to the mucous gel layer forming p. H gradient (lumen 1 -3, surface epithelium 6 -7), stimulated by Ca, prostaglandins, cholinergic input, and gastric p. H.
Mucous: secreted by surface epithelial cells § consist of water with lipids and glycoproteins; This forms hydrophobic surface with fatty acids. Also forms a surface water layer that prevents diffusion of ions and substances like pepsin. Bicarbonate: secreted by the surface epithelial § cells to the mucous gel layer forming p. H gradient (lumen 1 -3, surface epithelium 6 -7), stimulated by Ca, prostaglandins, cholinergic input, and gastric p. H.
 Restitution: migration of epithelial cells § bordering site of an injury to restore the damaged area. Epithelial cell regeneration: this regulated by § prostaglandins and occurs with angiogenesis Sub epithelial microvascular system. §
Restitution: migration of epithelial cells § bordering site of an injury to restore the damaged area. Epithelial cell regeneration: this regulated by § prostaglandins and occurs with angiogenesis Sub epithelial microvascular system. §
 Prostaglandine: § …. . regulate release of HCO 3, mucous. …. . Inhibit parietal cell secretion. …. . Maintaining the mucosal blood flow and cell restitution. COX 1: expressed in stomach, kidneys, platelets and endothelial cells. It has a role in mucosal integrity, platelet aggregation and renal function.
Prostaglandine: § …. . regulate release of HCO 3, mucous. …. . Inhibit parietal cell secretion. …. . Maintaining the mucosal blood flow and cell restitution. COX 1: expressed in stomach, kidneys, platelets and endothelial cells. It has a role in mucosal integrity, platelet aggregation and renal function.
 Causes PUD H Pylori § Nonsteroidal antiinflammatory drugs § Gastric acid hypersecretion § Familial aggregation §
Causes PUD H Pylori § Nonsteroidal antiinflammatory drugs § Gastric acid hypersecretion § Familial aggregation §
 PUD Causes H Pylori § Nonsteroidal antiinflammatory drugs § Gastric acid hypersecretion § Familial aggregation §
PUD Causes H Pylori § Nonsteroidal antiinflammatory drugs § Gastric acid hypersecretion § Familial aggregation §
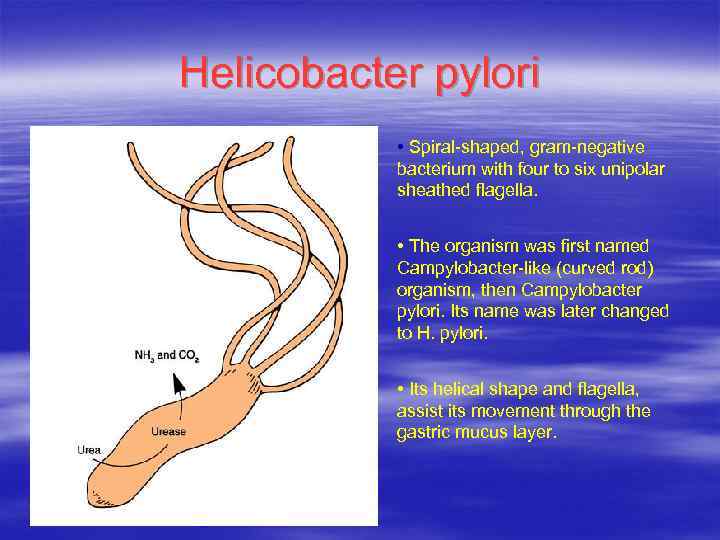 Helicobacter pylori • Spiral-shaped, gram-negative bacterium with four to six unipolar sheathed flagella. • The organism was first named Campylobacter-like (curved rod) organism, then Campylobacter pylori. Its name was later changed to H. pylori. • Its helical shape and flagella, assist its movement through the gastric mucus layer.
Helicobacter pylori • Spiral-shaped, gram-negative bacterium with four to six unipolar sheathed flagella. • The organism was first named Campylobacter-like (curved rod) organism, then Campylobacter pylori. Its name was later changed to H. pylori. • Its helical shape and flagella, assist its movement through the gastric mucus layer.
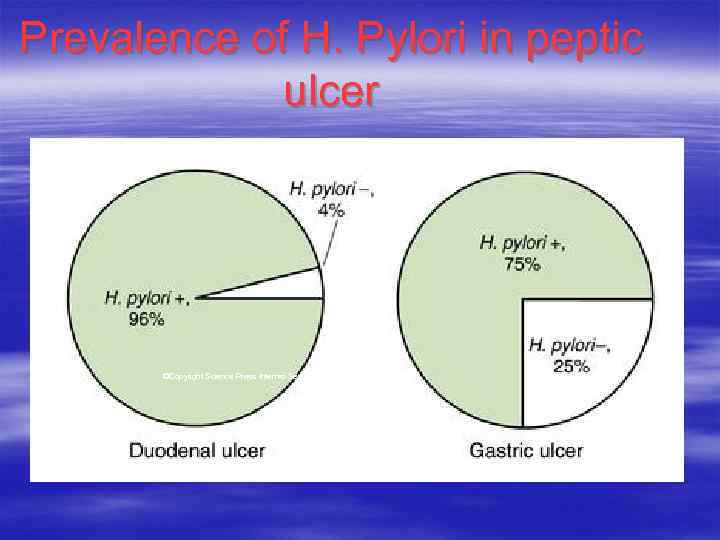 Prevalence of H. Pylori in peptic ulcer ©Copyright Science Press Internet Services
Prevalence of H. Pylori in peptic ulcer ©Copyright Science Press Internet Services
 PUD Causes H Pylori § Nonsteroidal antiinflammatory drugs § Gastric acid hypersecretion § Familial aggregation §
PUD Causes H Pylori § Nonsteroidal antiinflammatory drugs § Gastric acid hypersecretion § Familial aggregation §
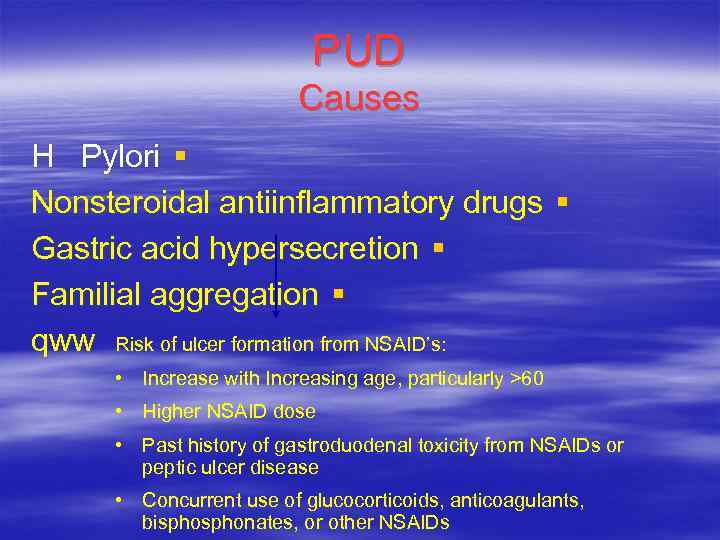 PUD Causes H Pylori § Nonsteroidal antiinflammatory drugs § Gastric acid hypersecretion § Familial aggregation § qww Risk of ulcer formation from NSAID’s: • Increase with Increasing age, particularly >60 • Higher NSAID dose • Past history of gastroduodenal toxicity from NSAIDs or peptic ulcer disease • Concurrent use of glucocorticoids, anticoagulants, bisphonates, or other NSAIDs
PUD Causes H Pylori § Nonsteroidal antiinflammatory drugs § Gastric acid hypersecretion § Familial aggregation § qww Risk of ulcer formation from NSAID’s: • Increase with Increasing age, particularly >60 • Higher NSAID dose • Past history of gastroduodenal toxicity from NSAIDs or peptic ulcer disease • Concurrent use of glucocorticoids, anticoagulants, bisphonates, or other NSAIDs
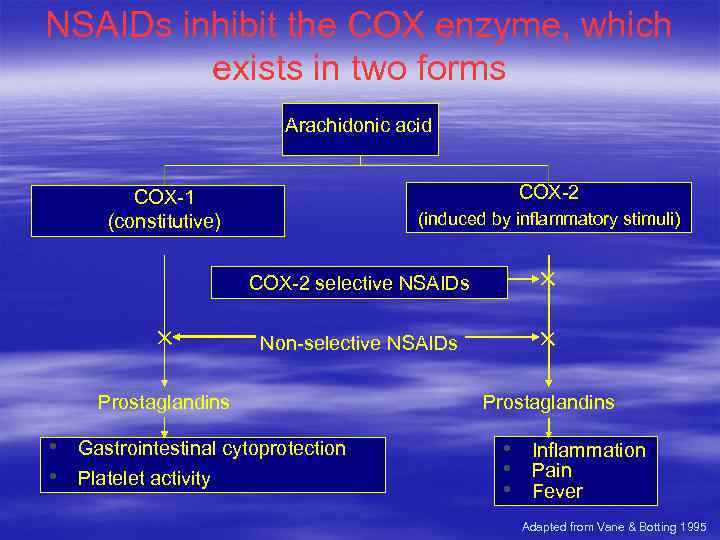 NSAIDs inhibit the COX enzyme, which exists in two forms Arachidonic acid COX-2 COX-1 (constitutive) (induced by inflammatory stimuli) COX-2 selective NSAIDs Non-selective NSAIDs Prostaglandins • • Gastrointestinal cytoprotection Platelet activity Prostaglandins • • • Inflammation Pain Fever Adapted from Vane & Botting 1995
NSAIDs inhibit the COX enzyme, which exists in two forms Arachidonic acid COX-2 COX-1 (constitutive) (induced by inflammatory stimuli) COX-2 selective NSAIDs Non-selective NSAIDs Prostaglandins • • Gastrointestinal cytoprotection Platelet activity Prostaglandins • • • Inflammation Pain Fever Adapted from Vane & Botting 1995
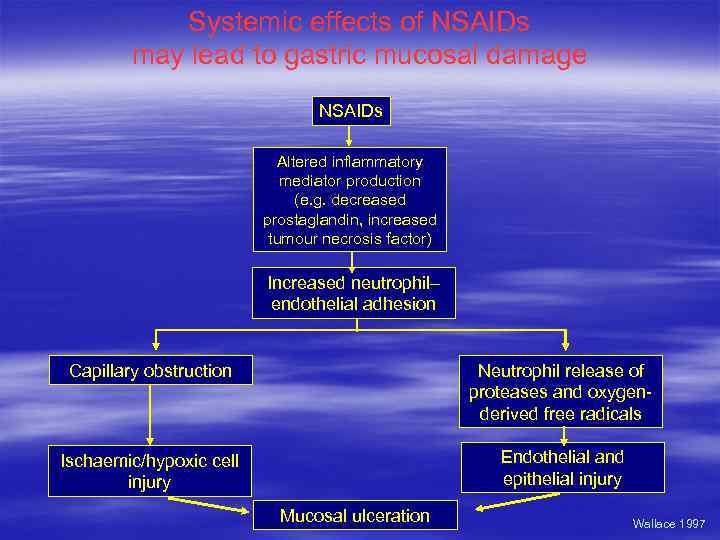 Systemic effects of NSAIDs may lead to gastric mucosal damage NSAIDs Altered inflammatory mediator production (e. g. decreased prostaglandin, increased tumour necrosis factor) Increased neutrophil– endothelial adhesion Capillary obstruction Neutrophil release of proteases and oxygenderived free radicals Ischaemic/hypoxic cell injury Endothelial and epithelial injury Mucosal ulceration Wallace 1997
Systemic effects of NSAIDs may lead to gastric mucosal damage NSAIDs Altered inflammatory mediator production (e. g. decreased prostaglandin, increased tumour necrosis factor) Increased neutrophil– endothelial adhesion Capillary obstruction Neutrophil release of proteases and oxygenderived free radicals Ischaemic/hypoxic cell injury Endothelial and epithelial injury Mucosal ulceration Wallace 1997
 PUD Causes H Pylori § Nonsteroidal antiinflammatory drugs § Gastric acid hypersecretion Zollinger-Ellison § syndrome Familial aggregation § • DU and no Helicobacter pylori present • • Presence of diarrhea Failure of the ulcer to heal with H. pylori eradication Multiple ulcers or ulcers in unusual locations Severe peptic ulcer disease leading to a complication (eg, bleeding perforation, intractability) Severe or resistant peptic esophageal disease History of nephrolithiasis or endocrinopathies Family history of nephrolithiasis, endocrinopathies, or peptic ulcer disease
PUD Causes H Pylori § Nonsteroidal antiinflammatory drugs § Gastric acid hypersecretion Zollinger-Ellison § syndrome Familial aggregation § • DU and no Helicobacter pylori present • • Presence of diarrhea Failure of the ulcer to heal with H. pylori eradication Multiple ulcers or ulcers in unusual locations Severe peptic ulcer disease leading to a complication (eg, bleeding perforation, intractability) Severe or resistant peptic esophageal disease History of nephrolithiasis or endocrinopathies Family history of nephrolithiasis, endocrinopathies, or peptic ulcer disease
 PUD Causes H Pylori § Nonsteroidal antiinflammatory drugs § Gastric acid hypersecretion § Familial aggregation § • • • First-degree relatives of patients with DU have a threefold increase in the prevalence of DU but not GU Relatives of patients with GU have a threefold increase in the prevalence of GU but not DU. Hyperpepsinogenemia was proposed as a marker of autosomal dominant inheritance.
PUD Causes H Pylori § Nonsteroidal antiinflammatory drugs § Gastric acid hypersecretion § Familial aggregation § • • • First-degree relatives of patients with DU have a threefold increase in the prevalence of DU but not GU Relatives of patients with GU have a threefold increase in the prevalence of GU but not DU. Hyperpepsinogenemia was proposed as a marker of autosomal dominant inheritance.
 PUD Clinical Presentation Dyspepsia § DU: The "classic" symptoms occur when – acid is secreted in the absence of a food buffer. symptoms occur two to five hours after meals or § on an empty stomach. Symptoms also occur at night, between 11 PM § and 2 AM, when the circadian stimulation of acid secretion is maximal. GU: Has classically been associated with – more severe pain occurring soon after meals, with less frequent relief by antacids or food.
PUD Clinical Presentation Dyspepsia § DU: The "classic" symptoms occur when – acid is secreted in the absence of a food buffer. symptoms occur two to five hours after meals or § on an empty stomach. Symptoms also occur at night, between 11 PM § and 2 AM, when the circadian stimulation of acid secretion is maximal. GU: Has classically been associated with – more severe pain occurring soon after meals, with less frequent relief by antacids or food.
 PUD Clinical Presentation Postprandial belching § Bloating § Epigastric fullness § Anorexia § Early satiety § Nausea and occasional vomiting § Silent Ulcers in 1 -2% of asymptomatic population
PUD Clinical Presentation Postprandial belching § Bloating § Epigastric fullness § Anorexia § Early satiety § Nausea and occasional vomiting § Silent Ulcers in 1 -2% of asymptomatic population
 Presentation of more complicated cases Penetrating ulcers: § a shift from the typical vague visceral – discomfort to a more localized and intense pain that radiates to the back and is not relieved by food or antacids. Perforation: § sudden development of severe, diffuse – abdominal pain. Pyloric outlet obstruction: § Vomiting is the cardinal feature present in – most cases. Hemorrhage: §
Presentation of more complicated cases Penetrating ulcers: § a shift from the typical vague visceral – discomfort to a more localized and intense pain that radiates to the back and is not relieved by food or antacids. Perforation: § sudden development of severe, diffuse – abdominal pain. Pyloric outlet obstruction: § Vomiting is the cardinal feature present in – most cases. Hemorrhage: §
 Diagnosis Barium studies § Endoscopy § Serological test §
Diagnosis Barium studies § Endoscopy § Serological test §
 Barium Study Folds radiating to the crater and deformities in the region secondary to spasm, edema, and scarring Barium within an ulcer niche, which is generally round or oval
Barium Study Folds radiating to the crater and deformities in the region secondary to spasm, edema, and scarring Barium within an ulcer niche, which is generally round or oval
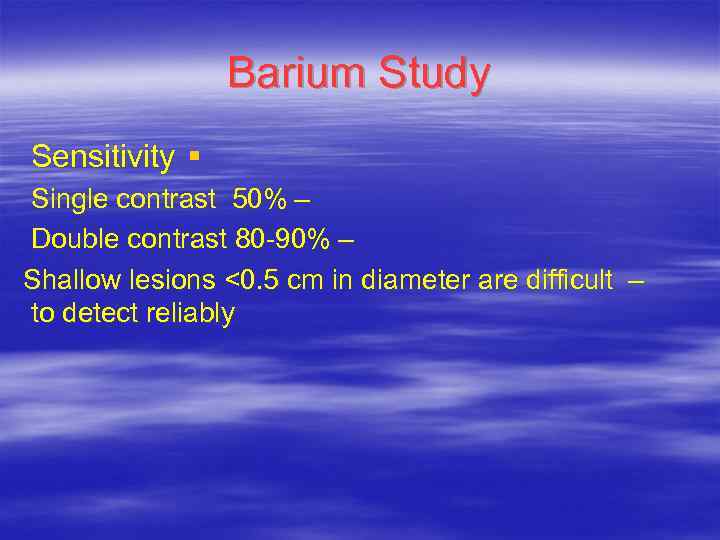 Barium Study Sensitivity § Single contrast 50% – Double contrast 80 -90% – Shallow lesions <0. 5 cm in diameter are difficult – to detect reliably
Barium Study Sensitivity § Single contrast 50% – Double contrast 80 -90% – Shallow lesions <0. 5 cm in diameter are difficult – to detect reliably
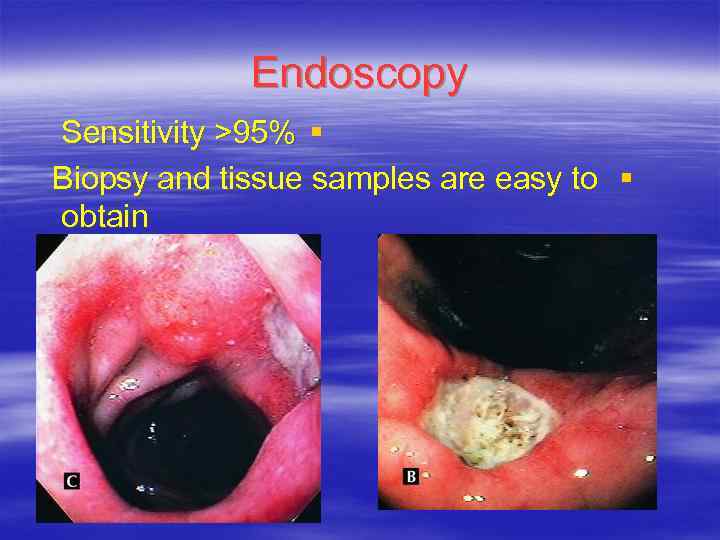 Endoscopy Sensitivity >95% § Biopsy and tissue samples are easy to § obtain
Endoscopy Sensitivity >95% § Biopsy and tissue samples are easy to § obtain
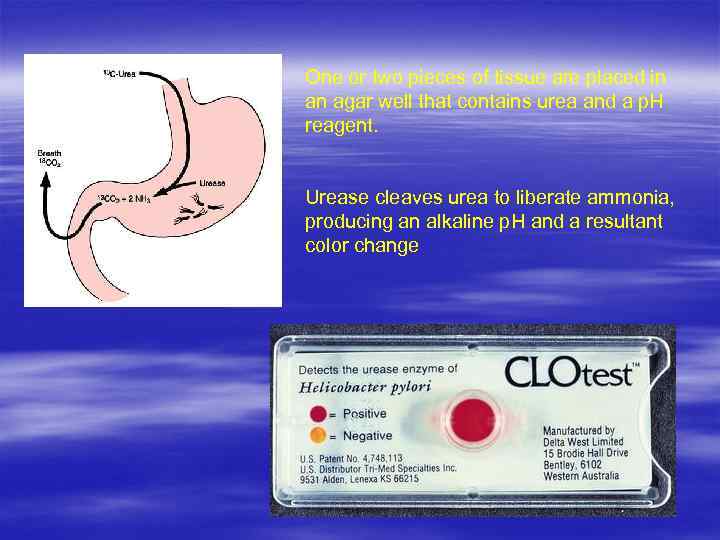 One or two pieces of tissue are placed in an agar well that contains urea and a p. H reagent. Urease cleaves urea to liberate ammonia, producing an alkaline p. H and a resultant color change
One or two pieces of tissue are placed in an agar well that contains urea and a p. H reagent. Urease cleaves urea to liberate ammonia, producing an alkaline p. H and a resultant color change
 Serological test ELISA technology to detect Ig. G or Ig. A § antibodies Inexpensive §
Serological test ELISA technology to detect Ig. G or Ig. A § antibodies Inexpensive §
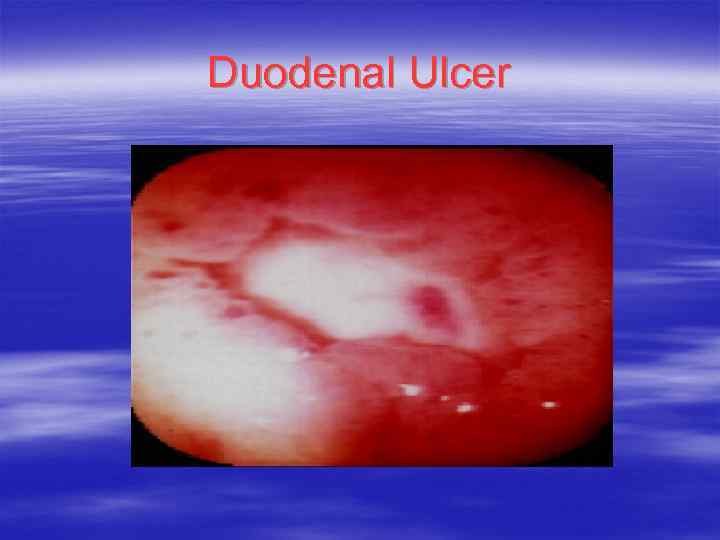 Duodenal Ulcer
Duodenal Ulcer
 Gastric Ulcer
Gastric Ulcer
 Malignant Gastric Ulcer
Malignant Gastric Ulcer
 Differential Diagnosis NUD § Pancreatic § Biliary § GERD §
Differential Diagnosis NUD § Pancreatic § Biliary § GERD §
 Complications GI bleeding. § Perforation & penetration. § Gastric outlet obstruction. §
Complications GI bleeding. § Perforation & penetration. § Gastric outlet obstruction. §
 Bleeding
Bleeding
 Gastric Outlet Obstruction
Gastric Outlet Obstruction
 Treatment of H. Pylori § Prevention & Treatment of NSAIDS related § Ulcers. Antacids : For symptomatic relief if any at all. § H 2 receptors antagonists: Cimitidine, § ranitidine, Famotidine, Nizatidine. PPI: Omeprazole, Lansoprazole, § Rabeprazole, Pantoprazole, Esomeprazole.
Treatment of H. Pylori § Prevention & Treatment of NSAIDS related § Ulcers. Antacids : For symptomatic relief if any at all. § H 2 receptors antagonists: Cimitidine, § ranitidine, Famotidine, Nizatidine. PPI: Omeprazole, Lansoprazole, § Rabeprazole, Pantoprazole, Esomeprazole.
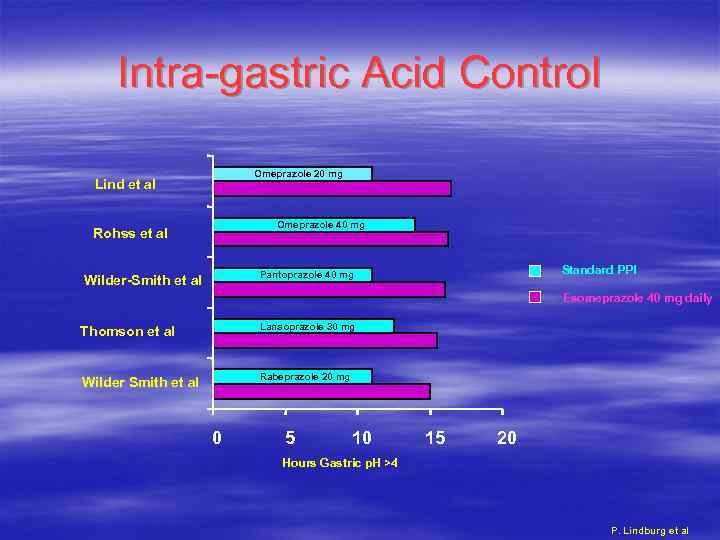 Intra-gastric Acid Control Omeprazole 20 mg Lind et al Omeprazole 40 mg Rohss et al Standard PPI Pantoprazole 40 mg Wilder-Smith et al Esomeprazole 40 mg daily Thomson et al Lansoprazole 30 mg Wilder Smith et al Rabeprazole 20 mg 0 5 10 15 20 Hours Gastric p. H >4 P. Lindburg et al
Intra-gastric Acid Control Omeprazole 20 mg Lind et al Omeprazole 40 mg Rohss et al Standard PPI Pantoprazole 40 mg Wilder-Smith et al Esomeprazole 40 mg daily Thomson et al Lansoprazole 30 mg Wilder Smith et al Rabeprazole 20 mg 0 5 10 15 20 Hours Gastric p. H >4 P. Lindburg et al
 Treatment Sucralfate: water insoluble that binds to site § of ulceration Bismuth § Prostaglandin analogue: Misoprostal §
Treatment Sucralfate: water insoluble that binds to site § of ulceration Bismuth § Prostaglandin analogue: Misoprostal §
 H. Pylori Treatment All patients with H pylori infection and § documented PUD either active or previous should have eradication therapy. Patients with MALT lymphoma has § significant response rate to H. Pylori treatment. Role in treating NUD? ? !! § Role in prevention gastric cancer? ? !! §
H. Pylori Treatment All patients with H pylori infection and § documented PUD either active or previous should have eradication therapy. Patients with MALT lymphoma has § significant response rate to H. Pylori treatment. Role in treating NUD? ? !! § Role in prevention gastric cancer? ? !! §
 Treatment of H. Pylori Amoxicillin, Metronidazole, § Clarithromycin, Omeprazole Clarithromycin, Metronidazole, Tetracycline, § Ranitidine- Bismuth Omeprazole, Bismuth subsalicylate, § Metronidazole, Tetracycline Eradication of H. Pylori result in decrease § recurrence of PUD 4%, 6%, -59%, 67% for GU, DU.
Treatment of H. Pylori Amoxicillin, Metronidazole, § Clarithromycin, Omeprazole Clarithromycin, Metronidazole, Tetracycline, § Ranitidine- Bismuth Omeprazole, Bismuth subsalicylate, § Metronidazole, Tetracycline Eradication of H. Pylori result in decrease § recurrence of PUD 4%, 6%, -59%, 67% for GU, DU.
 Treatment of NSAIDS Related Ulcers Stop NSAIDS if possible. PPI or H 2 blocker. Prevention of NSAIDS related ulcer: Use of PPI, H 2 blockers, Misoprostol. Use of selective COX 2 inhibitors.
Treatment of NSAIDS Related Ulcers Stop NSAIDS if possible. PPI or H 2 blocker. Prevention of NSAIDS related ulcer: Use of PPI, H 2 blockers, Misoprostol. Use of selective COX 2 inhibitors.
 Treatment of PUD Repeat endoscopy for GU but not DUs. Increase the dose of PPI and exclude other causes in refractory cases Surgical therapy should be limited to complicated cases and cases refractory to treatment.
Treatment of PUD Repeat endoscopy for GU but not DUs. Increase the dose of PPI and exclude other causes in refractory cases Surgical therapy should be limited to complicated cases and cases refractory to treatment.
 Surgical treatment FOR DU: Vagotomy with Pyloroplasty (gastrodudenostomy, gastrojejunostomy) Highly selective Vagotomy with Antrectomy.
Surgical treatment FOR DU: Vagotomy with Pyloroplasty (gastrodudenostomy, gastrojejunostomy) Highly selective Vagotomy with Antrectomy.
 Surgical Treatment for GU Antrectomy with Biliroth 1 For Antral ulcers. Vagotomy if concomitant DU is present. Sub total gastrectomy with Jejunostomy for proximal ulcers
Surgical Treatment for GU Antrectomy with Biliroth 1 For Antral ulcers. Vagotomy if concomitant DU is present. Sub total gastrectomy with Jejunostomy for proximal ulcers
 Stress ulcers Underlying conditions for stress ulcer : trauma’, sepsis, serious illness Hemorrhaging occurs 3 -7 days after traumatic event Burns involving more than 35% of the body mass Occur in 50 % to 75% of pt with head injury
Stress ulcers Underlying conditions for stress ulcer : trauma’, sepsis, serious illness Hemorrhaging occurs 3 -7 days after traumatic event Burns involving more than 35% of the body mass Occur in 50 % to 75% of pt with head injury
 H. pylori releated disease PUD Gastric adenocarcinoma Gastric B –Cell lymphoma gastritis
H. pylori releated disease PUD Gastric adenocarcinoma Gastric B –Cell lymphoma gastritis
 H. Pylori testing A- INVASIVE(antral biopsy) 1 - rapid urase test 2 - culture 3 - histology B- Noninvasive 1 -Urea breath test 2 -Fecal antigen tests 3 -Serologic tests (ELISA-Ig. G)
H. Pylori testing A- INVASIVE(antral biopsy) 1 - rapid urase test 2 - culture 3 - histology B- Noninvasive 1 -Urea breath test 2 -Fecal antigen tests 3 -Serologic tests (ELISA-Ig. G)
 THANK YOU
THANK YOU


