4e41b7cefd2f5debc9086764b72ec1ad.ppt
- Количество слайдов: 13
Pediatric Neurology Quick Talks Headache Michael Babcock Summer 2013
Scenario • • • 7 yo boy Headaches for 4 months Headaches last 90 minutes Grabs the front of his head when it hurts Has about 1 headache a week, vomits with some of the headaches Continues to do well in school, no vision complaints
Causes of headache • Primary – Migraine – Tension-type – Cluster – Paroxysmal hemicrania – SUNCT – Trigeminal neuralgia (not common in kids) – Chronic daily headache • Secondary – Medication overuse (rebound) – head/neck trauma – Vascular disorder – SAH, AVM, vasculitis, CSVT – High ICP / Low ICP – Tumor – Infection • CNS • Other infections
History • • • Headache – quality, severity, location, laterality, onset, time course – episodic and similar or progressive/changing Associated symptoms – systemic symptoms, fever, personality changes, seizures Preceding symptoms – aura, gradual/rapid onset Exacerbating features – migraines worse with activity; worse with laying or nocturnal or with cough/straining – signs of elevated ICP; worse with standing – signs of low ICP. Medical history – NF 1, Sturge-weber, connective tissue disorder, Sickle cell, immunocompromised.
Exam • • Vitals – fever, ICP signs Good neurologic exam – ? Altered mental status – Abnormal eye movements – Visual field testing – Fundoscopic exam – Focal weakness – UMN signs – Abnormal gait
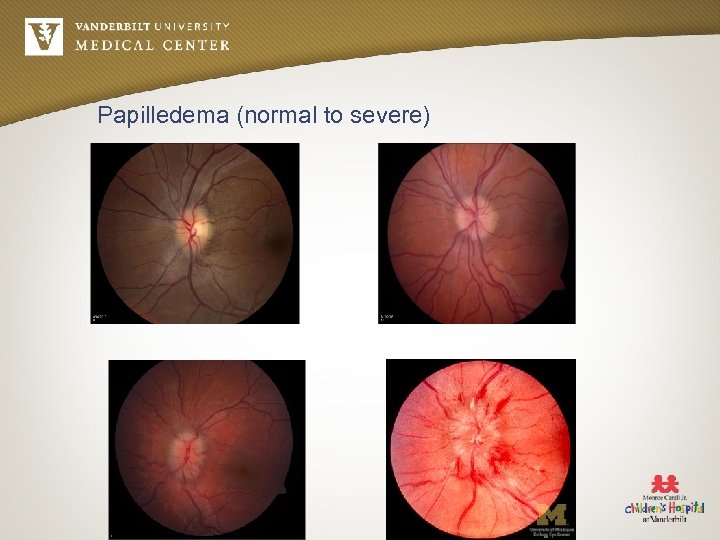
Papilledema (normal to severe)
Work-up • Imaging – Trauma – Associated seizures – AMS – Abnormal neurologic exam – Historical features – thunderclap headache, persistently lateralized, progressive course, shunt, change in pattern/type, occipital headache – Signs of elevated ICP – Considerations: • no family history of migraine • < 1 month of headache • Young age of onset – Prior to LP • CSF analysis – Pseudotumor (IIH) • Accurate recording of pressure, in lateral decub position must extend LE's. – Meningitis • Meningismus • Fever • New seizures • AMS • immunocompromised – SAH • Thunderclap headache
Migraine • • • Affects 7% of all children Causes $1 -17 billion in lost productivity Accounts for 10 million physician visits/year in U. S.
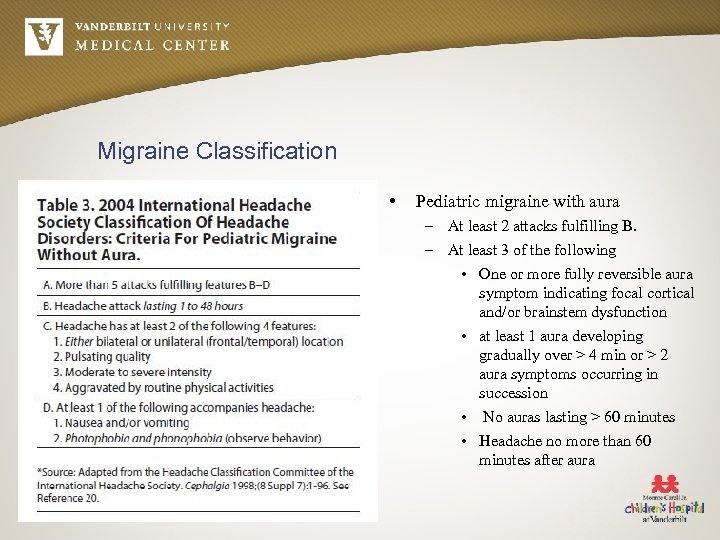
Migraine Classification • Pediatric migraine with aura – At least 2 attacks fulfilling B. – At least 3 of the following • One or more fully reversible aura symptom indicating focal cortical and/or brainstem dysfunction • at least 1 aura developing gradually over > 4 min or > 2 aura symptoms occurring in succession • No auras lasting > 60 minutes • Headache no more than 60 minutes after aura
Migraine treatment – Life-style modification • • Sleep – don't vary by more than one hour on school/weekend nights Exercise – regular exercise, but over-exercise can cause headache Mealtimes – 3 meals daily, don't skip meals Hydration – carry water bottle – school excuse to carry and go to bathroom Stress – stress reduction techniques Caffeine – moderation or stop Analgesic overuse – Don't use OTC pain relievers more than two-three times weekly – Opiates can also cause this – To relieve headache – have to break cycle, stop medication, headache worse for 2 -3 weeks, then better.
Migraine Medications - Preventative • • • Cyproheptadine – AAN PP – insufficient evidence – histamine and serotonin antagonist with Ca-channel blocking properties; SE – weightgain and sedation. Can be OK for younger, non-overweight children. Beta-blockers – conflicting evidence. SE – asthma, DM, orthostatic hypotension, depression, not good for athletes Amitryptaline (TCA's) – depressino/affective disorder often co-morbid with migraines. SE – QT prolongation – get EKG, behavior change Ca-channel blockers – Verapamil – good for hemiplegic migraine AED's – Topamax – SE – weight loss, cognitive change, sedation – Depakote – SE – weight gain, PCOS, teratogenic; need CBC/LFT monitoring – Keppra – consider because low SE profile – Gabapentin – SE – sedation
Migraine Medications – Abortive • • Naproxen (Aleve) – 10 -20 mg/kg/d div Q 8 H. For patients over 30 kg. Can give 1 -2 tabs at onset, 1 more tab in 8 hours. Motrin Fioricet (acetaminophen/butalbital/caffeine) or fiorinal – good for rescue but risk of dependance, overuse – probably best not to give outside ED. Anti-emetics – Phenergan, Reglan, Compazine – can give benadryl to help with sleep/extrapyramidal effects Triptans – Sumatriptan (PO, SC, IN) – Adult oral PO dose is 25 -100 mg at onset, max 200 mg/day PO. No dosage recommendations for children in packet. SE-- heart – vasospasm, MI, arrhythmias, HTN, stroke, seizure, rebound headaches; chest/jaw/neck pain. Ergots – nasal DHE (Migrinal nasal spray) – 1 squirt in each nostril – SE—chest pain, nausea, cannot use within 24 hours of triptan In ED – hydration with NS, Magnesium, Depakote, Ketorolac if not medication overuse, compazine, benadryl, steroid
References • • http: //eyewiki. aao. org/Papilledema http: //www. kellogg. umich. edu/theeyeshaveit/acquired/papilledema. html AAN Practice parameter – migraines Maria, B. 2009. Current management in child neurology. People's medical publishing house.
4e41b7cefd2f5debc9086764b72ec1ad.ppt