86d4aea88951fd087a5ab00c01d3a616.ppt
- Количество слайдов: 54
 Pediatric Disaster Life Support (PDLS©): Scene Assessment & Triage Dr. Jim Courtney Assistant Professor of Emergency Medicine
Pediatric Disaster Life Support (PDLS©): Scene Assessment & Triage Dr. Jim Courtney Assistant Professor of Emergency Medicine
 Your homework got washed away with your house! A likely story young man! See me after class!
Your homework got washed away with your house! A likely story young man! See me after class!
 Triage Assessment, Stabilization, Resuscitation n Learning Objective n At the end of this lecture, the students should be able to: - describe differences in triage decision making for - children describe triage categories describe field triage assessment describe initial field stabilization methods for children
Triage Assessment, Stabilization, Resuscitation n Learning Objective n At the end of this lecture, the students should be able to: - describe differences in triage decision making for - children describe triage categories describe field triage assessment describe initial field stabilization methods for children
 General Principles of Disaster Care n Scene Assessment n Triage Assessment n Initial Stabilization n Resuscitation
General Principles of Disaster Care n Scene Assessment n Triage Assessment n Initial Stabilization n Resuscitation
 Scene Assessment n Ensure scene safety n Establish that disaster exists n Estimate number of victims: adults/children
Scene Assessment n Ensure scene safety n Establish that disaster exists n Estimate number of victims: adults/children


 Scene Assessment n Notification to medical control: regional communications, local emergency management / disaster authority - type of event - initial casualty estimate
Scene Assessment n Notification to medical control: regional communications, local emergency management / disaster authority - type of event - initial casualty estimate
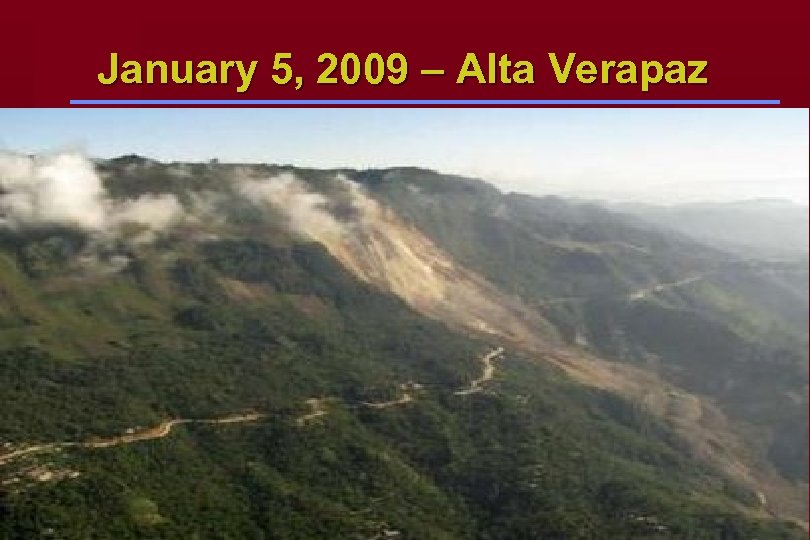 January 5, 2009 – Alta Verapaz
January 5, 2009 – Alta Verapaz
 n Make initial request for additional resources Then begin triage assessment of individual patients
n Make initial request for additional resources Then begin triage assessment of individual patients
 Triage Assessment n Derived from the French “trier” meaning to sort, it describes a medical decision making process n Guides decisions about allocating scarce resources and limited time n “greatest good for greatest number” n Protocol helps makes decisions n Appropriate performance crucial
Triage Assessment n Derived from the French “trier” meaning to sort, it describes a medical decision making process n Guides decisions about allocating scarce resources and limited time n “greatest good for greatest number” n Protocol helps makes decisions n Appropriate performance crucial
 Triage n ICS separates triage from treatment immediately - see everybody once briefly for overview n Dynamic process, re-triage / re-evaluate at several stages n Triage in disaster setting may be very difficult n Pediatric population unique challenge
Triage n ICS separates triage from treatment immediately - see everybody once briefly for overview n Dynamic process, re-triage / re-evaluate at several stages n Triage in disaster setting may be very difficult n Pediatric population unique challenge


 Initial Brief Assessment n Open airway n Control major hemorrhage n Categorize
Initial Brief Assessment n Open airway n Control major hemorrhage n Categorize
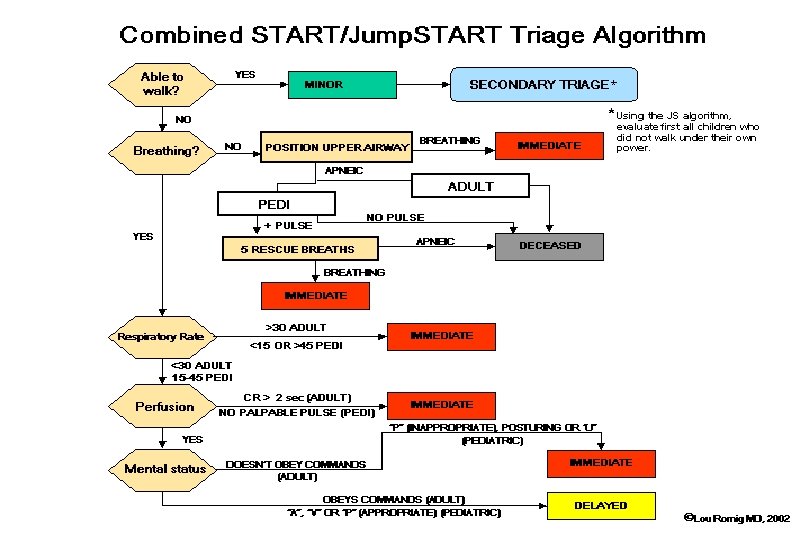
 Triage Classifications n Simple Triage And Rapid Treatment S. T. A. R. T. n Jump. START Tool for Rapid Pediatric Multicasualty Field Triage (children from 1 - 8 years of age)
Triage Classifications n Simple Triage And Rapid Treatment S. T. A. R. T. n Jump. START Tool for Rapid Pediatric Multicasualty Field Triage (children from 1 - 8 years of age)
 Triage Categories n Red / Immediate / Emergent n Yellow / Urgent n Green / Non-Urgent / Walking Wounded n Black / Deceased or soon to be
Triage Categories n Red / Immediate / Emergent n Yellow / Urgent n Green / Non-Urgent / Walking Wounded n Black / Deceased or soon to be
 Triage Classifications and Examples n Red - tension pneumothorax, rib fractures, upper airway obstruction, hemorrhage, femur fracture, asthmatic n Yellow - humerus fracture, scalp lacerations, shoulder dislocation n Green - ankle sprain, simple laceration, orphaned child, subluxed radial head n Black/Blue - cardiopulmonary arrest, severe open head injury
Triage Classifications and Examples n Red - tension pneumothorax, rib fractures, upper airway obstruction, hemorrhage, femur fracture, asthmatic n Yellow - humerus fracture, scalp lacerations, shoulder dislocation n Green - ankle sprain, simple laceration, orphaned child, subluxed radial head n Black/Blue - cardiopulmonary arrest, severe open head injury
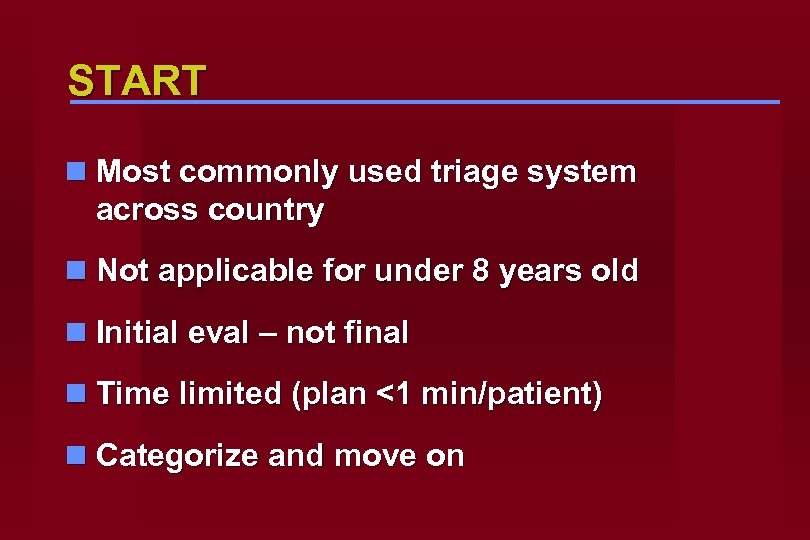 START n Most commonly used triage system across country n Not applicable for under 8 years old n Initial eval – not final n Time limited (plan <1 min/patient) n Categorize and move on
START n Most commonly used triage system across country n Not applicable for under 8 years old n Initial eval – not final n Time limited (plan <1 min/patient) n Categorize and move on
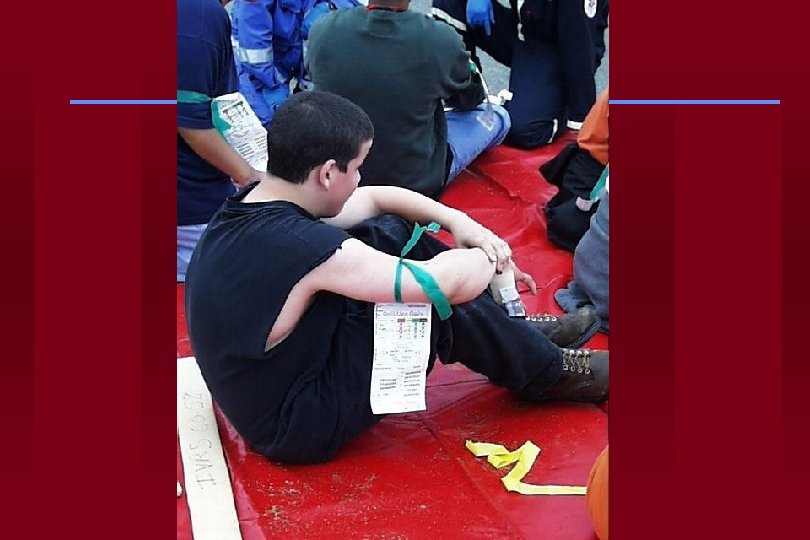
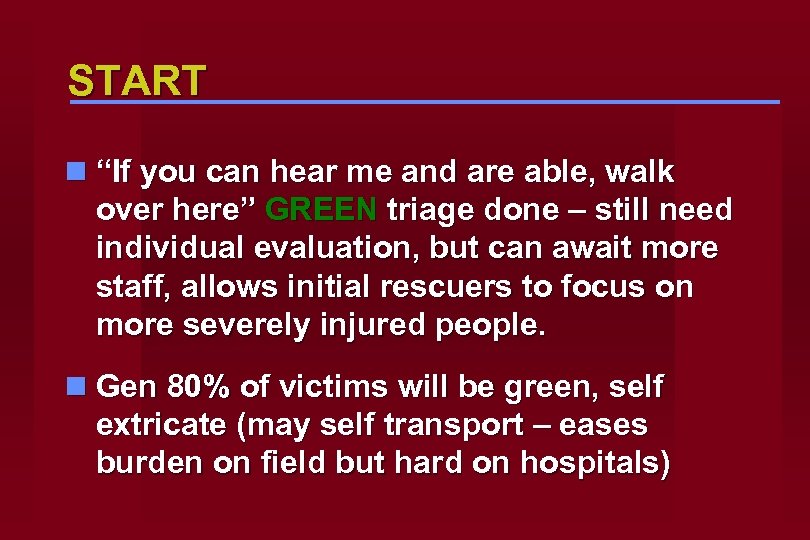 START n “If you can hear me and are able, walk over here” GREEN triage done – still need individual evaluation, but can await more staff, allows initial rescuers to focus on more severely injured people. n Gen 80% of victims will be green, self extricate (may self transport – eases burden on field but hard on hospitals)
START n “If you can hear me and are able, walk over here” GREEN triage done – still need individual evaluation, but can await more staff, allows initial rescuers to focus on more severely injured people. n Gen 80% of victims will be green, self extricate (may self transport – eases burden on field but hard on hospitals)
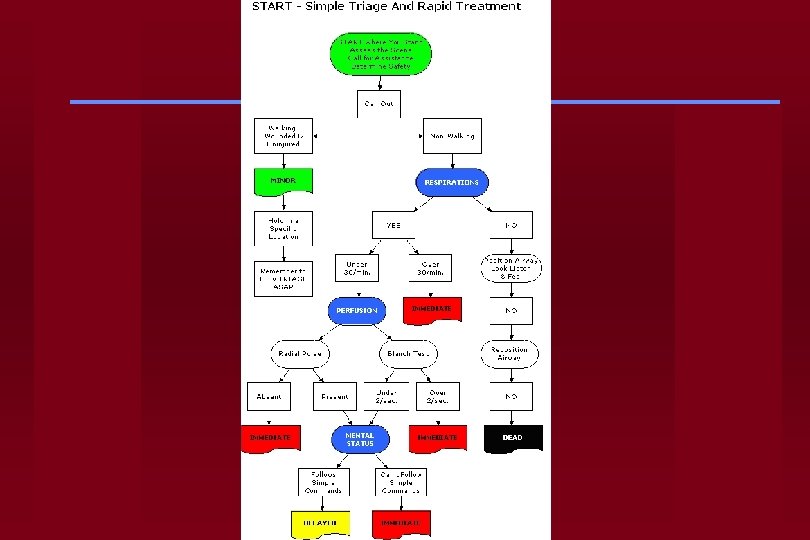
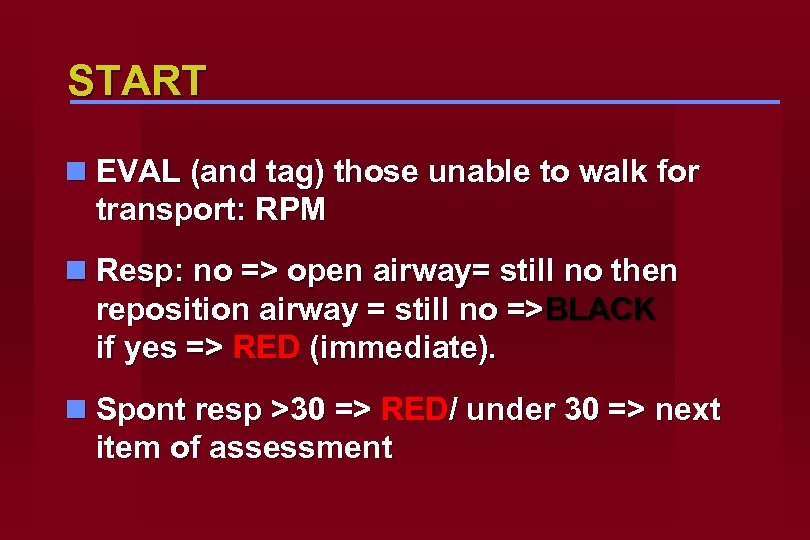 START n EVAL (and tag) those unable to walk for transport: RPM n Resp: no => open airway= still no then reposition airway = still no =>BLACK if yes => RED (immediate). n Spont resp >30 => RED/ under 30 => next item of assessment
START n EVAL (and tag) those unable to walk for transport: RPM n Resp: no => open airway= still no then reposition airway = still no =>BLACK if yes => RED (immediate). n Spont resp >30 => RED/ under 30 => next item of assessment
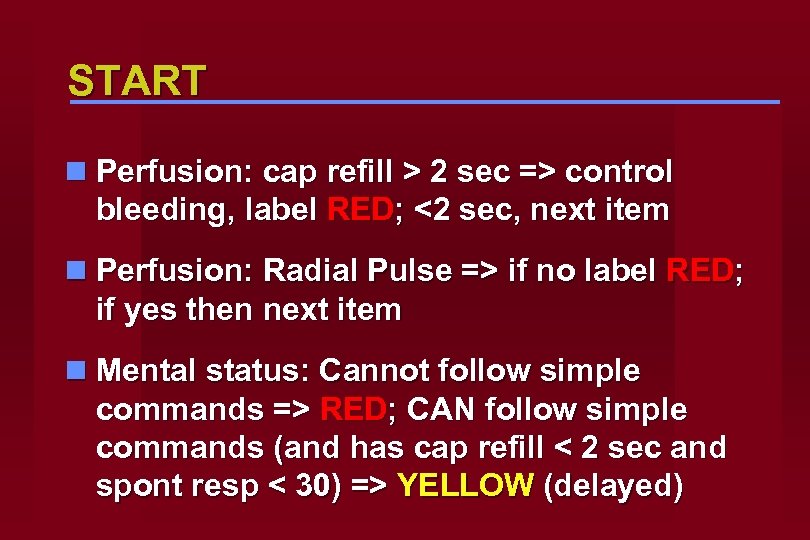 START n Perfusion: cap refill > 2 sec => control bleeding, label RED; <2 sec, next item n Perfusion: Radial Pulse => if no label RED; if yes then next item n Mental status: Cannot follow simple commands => RED; CAN follow simple commands (and has cap refill < 2 sec and spont resp < 30) => YELLOW (delayed)
START n Perfusion: cap refill > 2 sec => control bleeding, label RED; <2 sec, next item n Perfusion: Radial Pulse => if no label RED; if yes then next item n Mental status: Cannot follow simple commands => RED; CAN follow simple commands (and has cap refill < 2 sec and spont resp < 30) => YELLOW (delayed)
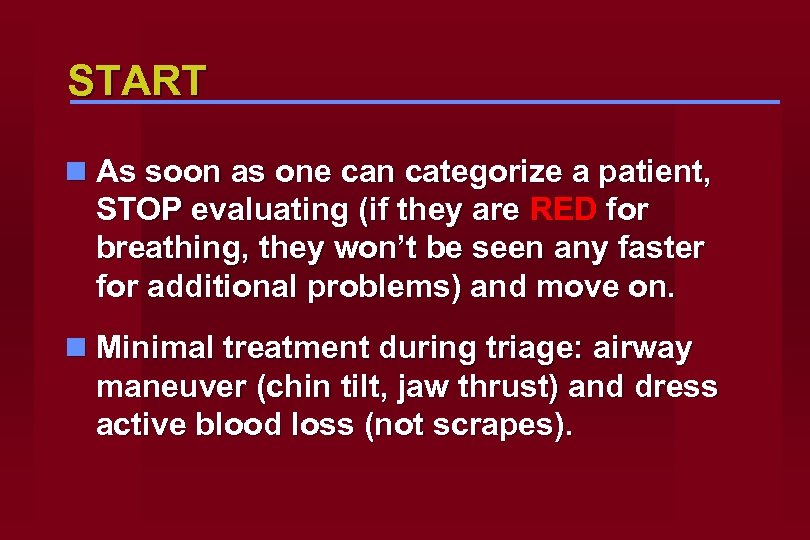 START n As soon as one can categorize a patient, STOP evaluating (if they are RED for breathing, they won’t be seen any faster for additional problems) and move on. n Minimal treatment during triage: airway maneuver (chin tilt, jaw thrust) and dress active blood loss (not scrapes).
START n As soon as one can categorize a patient, STOP evaluating (if they are RED for breathing, they won’t be seen any faster for additional problems) and move on. n Minimal treatment during triage: airway maneuver (chin tilt, jaw thrust) and dress active blood loss (not scrapes).
 Pediatric Triage
Pediatric Triage
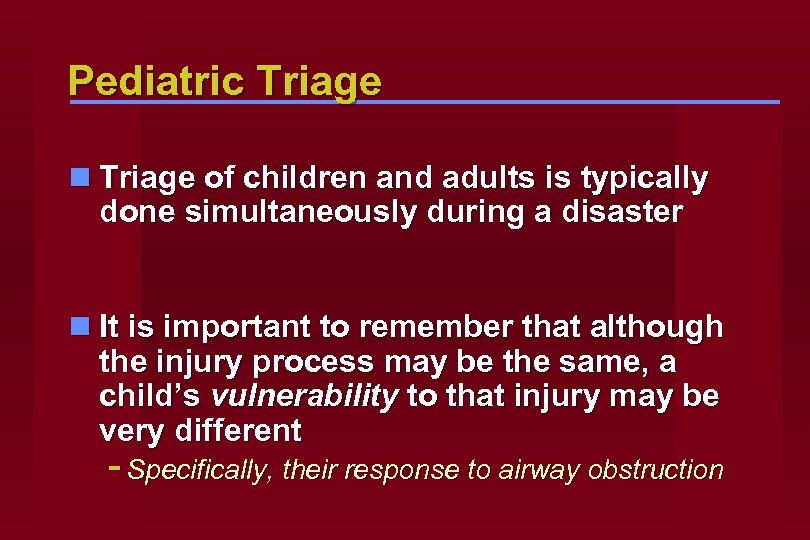 Pediatric Triage n Triage of children and adults is typically done simultaneously during a disaster n It is important to remember that although the injury process may be the same, a child’s vulnerability to that injury may be very different - Specifically, their response to airway obstruction
Pediatric Triage n Triage of children and adults is typically done simultaneously during a disaster n It is important to remember that although the injury process may be the same, a child’s vulnerability to that injury may be very different - Specifically, their response to airway obstruction
 Pediatric Triage n The standard adult triage tools do not take into account the specific vulnerability that children have to dying from airway obstruction n Children may have a reversible period of respiratory arrest from which they may recover if treated promptly
Pediatric Triage n The standard adult triage tools do not take into account the specific vulnerability that children have to dying from airway obstruction n Children may have a reversible period of respiratory arrest from which they may recover if treated promptly
 Pediatric Triage n Due to this, a specific pediatric triage tool was developed and tested - Jump. START n Builds from the concepts of triage taught in START triage, which is commonly utilized
Pediatric Triage n Due to this, a specific pediatric triage tool was developed and tested - Jump. START n Builds from the concepts of triage taught in START triage, which is commonly utilized
 Confused? n If you remember the specific vulnerability children have to airway compromise, this makes sense n The “Jumpstart” term refers to the extra chance we give a child to breathe before we declare them a BLACK TAG
Confused? n If you remember the specific vulnerability children have to airway compromise, this makes sense n The “Jumpstart” term refers to the extra chance we give a child to breathe before we declare them a BLACK TAG
 Jump. START (under 8) n Kids more airway dependent – rescue breaths attempted if pulse present (unlike adults) Resp 15 -45 instead of <30 n Vascular system clamps down sooner, so cap refill less reliable. Use peripheral pulse instead. n Mental status AVPU instead of following simple commands
Jump. START (under 8) n Kids more airway dependent – rescue breaths attempted if pulse present (unlike adults) Resp 15 -45 instead of <30 n Vascular system clamps down sooner, so cap refill less reliable. Use peripheral pulse instead. n Mental status AVPU instead of following simple commands
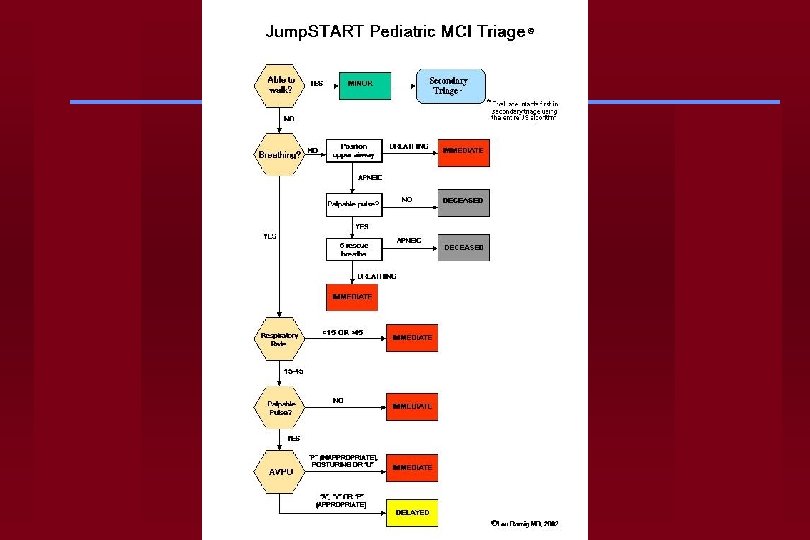
 Jump. START n “If you can hear me and you are able, walk over here for help. ” n Probably won’t work for children n If they are ambulatory, then they are GREEN n Use adults on scene to help corral the GREEN children
Jump. START n “If you can hear me and you are able, walk over here for help. ” n Probably won’t work for children n If they are ambulatory, then they are GREEN n Use adults on scene to help corral the GREEN children

 Jump. START n Respirations: NO open airway => yes RED; no -> check peripheral pulse. n NO pulse = BLACK n Pulse 15 sec mask to mouth ventilation n Spont resp: NO BLACK; YES RED
Jump. START n Respirations: NO open airway => yes RED; no -> check peripheral pulse. n NO pulse = BLACK n Pulse 15 sec mask to mouth ventilation n Spont resp: NO BLACK; YES RED
 Jump. START n Breathing: RR <15, >40 or irregular =RED n RR 15 -40, regular – check pulse n No peripheral pulse: RED n Peripheral pulse: check mental status n AV (appropriate) YELLOW n PU (inappropriate) RED
Jump. START n Breathing: RR <15, >40 or irregular =RED n RR 15 -40, regular – check pulse n No peripheral pulse: RED n Peripheral pulse: check mental status n AV (appropriate) YELLOW n PU (inappropriate) RED
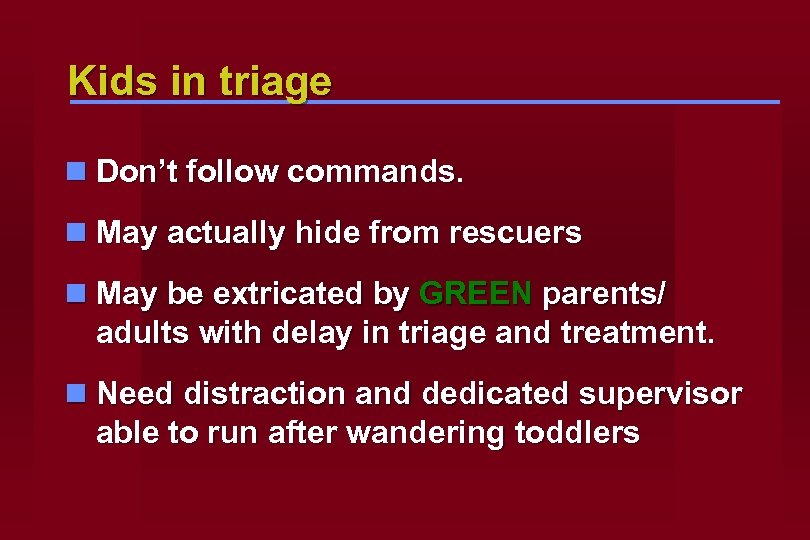 Kids in triage n Don’t follow commands. n May actually hide from rescuers n May be extricated by GREEN parents/ adults with delay in triage and treatment. n Need distraction and dedicated supervisor able to run after wandering toddlers
Kids in triage n Don’t follow commands. n May actually hide from rescuers n May be extricated by GREEN parents/ adults with delay in triage and treatment. n Need distraction and dedicated supervisor able to run after wandering toddlers


 Examples n Awake 8 yr old child brought in 3 days after earthquake with 20 others n Can not walk n Responds to voice n Respiratory Rate 50 IMMEDIATE n No obvious injuries
Examples n Awake 8 yr old child brought in 3 days after earthquake with 20 others n Can not walk n Responds to voice n Respiratory Rate 50 IMMEDIATE n No obvious injuries
 Examples n Unconscious 4 year old hit in head by debris moments ago n In a room full of injured children n Not breathing n Obvious head injury
Examples n Unconscious 4 year old hit in head by debris moments ago n In a room full of injured children n Not breathing n Obvious head injury
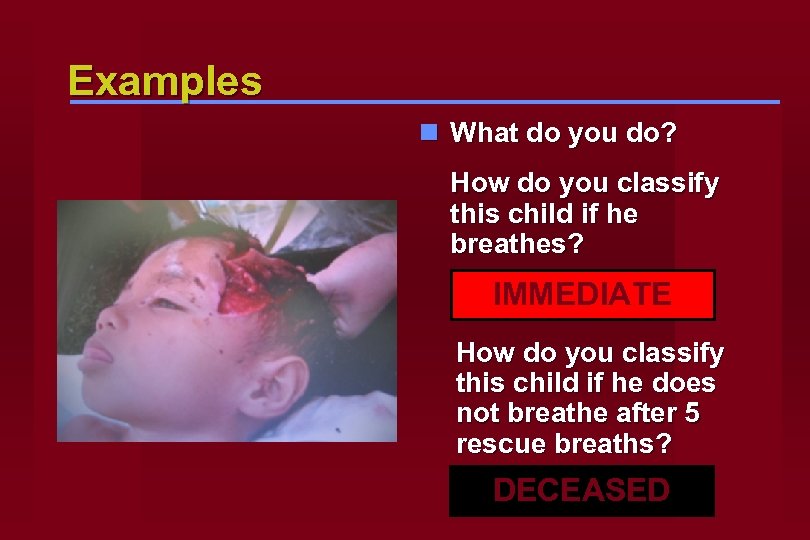 Examples n What do you do? How do you classify this child if he breathes? IMMEDIATE How do you classify this child if he does not breathe after 5 rescue breaths? DECEASED
Examples n What do you do? How do you classify this child if he breathes? IMMEDIATE How do you classify this child if he does not breathe after 5 rescue breaths? DECEASED
 Examples n Young child found breathing but sleepy n Respiratory Rate 30 n Has a palpable pulse n Arouses to touch and loud voice DELAYED
Examples n Young child found breathing but sleepy n Respiratory Rate 30 n Has a palpable pulse n Arouses to touch and loud voice DELAYED
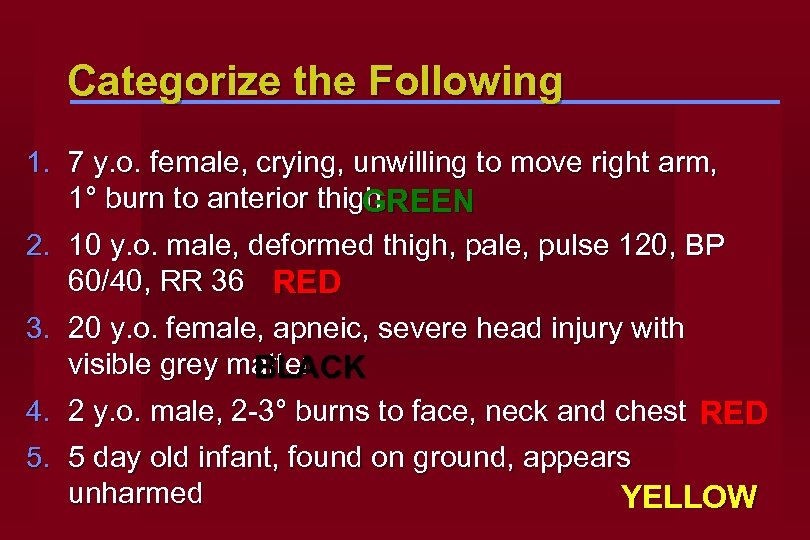 Categorize the Following 1. 7 y. o. female, crying, unwilling to move right arm, 1° burn to anterior thigh GREEN 2. 10 y. o. male, deformed thigh, pale, pulse 120, BP 60/40, RR 36 RED 3. 20 y. o. female, apneic, severe head injury with visible grey matter BLACK 4. 2 y. o. male, 2 -3° burns to face, neck and chest RED 5. 5 day old infant, found on ground, appears unharmed YELLOW
Categorize the Following 1. 7 y. o. female, crying, unwilling to move right arm, 1° burn to anterior thigh GREEN 2. 10 y. o. male, deformed thigh, pale, pulse 120, BP 60/40, RR 36 RED 3. 20 y. o. female, apneic, severe head injury with visible grey matter BLACK 4. 2 y. o. male, 2 -3° burns to face, neck and chest RED 5. 5 day old infant, found on ground, appears unharmed YELLOW
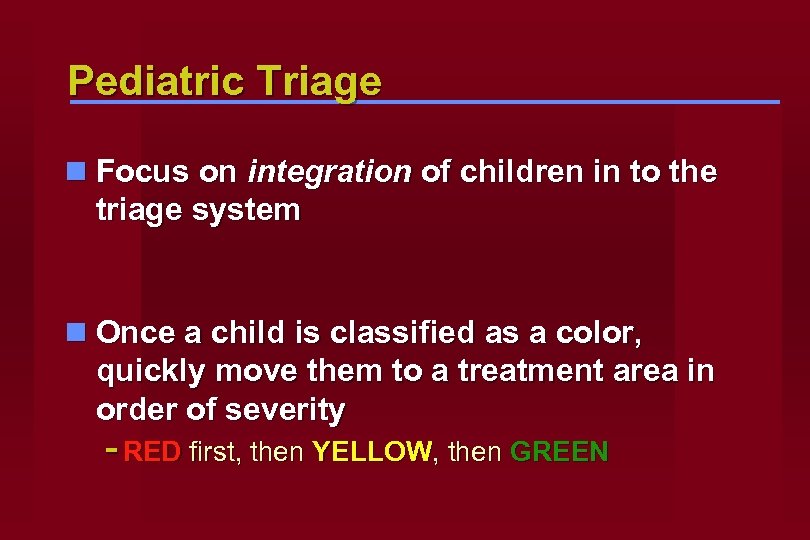 Pediatric Triage n Focus on integration of children in to the triage system n Once a child is classified as a color, quickly move them to a treatment area in order of severity - RED first, then YELLOW, then GREEN
Pediatric Triage n Focus on integration of children in to the triage system n Once a child is classified as a color, quickly move them to a treatment area in order of severity - RED first, then YELLOW, then GREEN
 Resources n PDLS is a start n Much information exists to guide the preparation and care for children in disasters
Resources n PDLS is a start n Much information exists to guide the preparation and care for children in disasters
 Resources n U. S. Center for Disease Control - www. cdc. gov n National Center for Disaster Preparedness - http: //www. ncdp. mailman. columbia. edu/ n American Psychological Association - www. apa. org
Resources n U. S. Center for Disease Control - www. cdc. gov n National Center for Disaster Preparedness - http: //www. ncdp. mailman. columbia. edu/ n American Psychological Association - www. apa. org
 Resources n Jump. START Triage Tool - www. jumpstarttriage. org n American Academy of Pediatrics - http: //www. aap. org/terrorism/topics/disaster_planning. html n Pediatric Disaster Preparedness Consensus Conference Summary - http: //www. bt. cdc. gov/children/pdf/working/execsumm 03. pdf n U. S. Department of Homeland Security - www. dhs. gov
Resources n Jump. START Triage Tool - www. jumpstarttriage. org n American Academy of Pediatrics - http: //www. aap. org/terrorism/topics/disaster_planning. html n Pediatric Disaster Preparedness Consensus Conference Summary - http: //www. bt. cdc. gov/children/pdf/working/execsumm 03. pdf n U. S. Department of Homeland Security - www. dhs. gov
 PDLS Content Revision - Richard V. Aghababian, MD, FACEP - Mark X. Cicero, MD, FAAP - James M. Courtney, DO, FAAEM - Andrew L. Garrett MD, FAAP - Eric J. Goedecke, DO, FACEP
PDLS Content Revision - Richard V. Aghababian, MD, FACEP - Mark X. Cicero, MD, FAAP - James M. Courtney, DO, FAAEM - Andrew L. Garrett MD, FAAP - Eric J. Goedecke, DO, FACEP
 Original Contributors n Gregory Ciottone, MD n Lucille Gans, MD n Patricia Hughes, RN n Frank Jehle, MD n Taryn Kennedy, MD n Gretchen Lipke, MD n Mariann Manno, MD n Robert Mc. Grath, M. Ed. n W. Peter Metz, MD n John A. Paraskos, MD n Carol Shustak, RN n Elizabeth Shilale, RN n A. Richard Starzyk n Gina Smith, RN n Michael Weinstock, MD n Fred Henretig, MD n Sharon Welsh, RN n Theodore Cieslak, MD n Lou Romig, MD
Original Contributors n Gregory Ciottone, MD n Lucille Gans, MD n Patricia Hughes, RN n Frank Jehle, MD n Taryn Kennedy, MD n Gretchen Lipke, MD n Mariann Manno, MD n Robert Mc. Grath, M. Ed. n W. Peter Metz, MD n John A. Paraskos, MD n Carol Shustak, RN n Elizabeth Shilale, RN n A. Richard Starzyk n Gina Smith, RN n Michael Weinstock, MD n Fred Henretig, MD n Sharon Welsh, RN n Theodore Cieslak, MD n Lou Romig, MD


