b4ed73fcb93e37b5248c152503d985fa.ppt
- Количество слайдов: 32
 PCRRT in HUS: Role of peritoneal dialysis Thomas J Neuhaus and GF Laube, JF Falger, EM Rüth, MJ Kemper, O Bänziger University Children’s Hospital, Zurich
PCRRT in HUS: Role of peritoneal dialysis Thomas J Neuhaus and GF Laube, JF Falger, EM Rüth, MJ Kemper, O Bänziger University Children’s Hospital, Zurich
 Zurich: Local History n 1955: Gasser et al: Hemolytic-Uremic Syndromes: HUS n 1964: Peritoneal dialysis for acute renal failure: HUS n 1970: Hemodialysis and renal transplantation n 1979: Continuous PD for chronic renal failure n 1995: Continuous veno-venous hemofiltration for ARF
Zurich: Local History n 1955: Gasser et al: Hemolytic-Uremic Syndromes: HUS n 1964: Peritoneal dialysis for acute renal failure: HUS n 1970: Hemodialysis and renal transplantation n 1979: Continuous PD for chronic renal failure n 1995: Continuous veno-venous hemofiltration for ARF
 HUS = Hemolytic-Uremic Syndromes n Hemolytic microangiopathic anemia: fragmentocytes, LDH , neg. Coombs n Thrombocytopenia n Uremia: acute renal failure n Further symptoms / complications: o Central nervous system (seizures, hemorrhages) o Hypertension and heart failure o Liver / Pancreas (with diabetes mellitus) o Eye: retinal bleedings
HUS = Hemolytic-Uremic Syndromes n Hemolytic microangiopathic anemia: fragmentocytes, LDH , neg. Coombs n Thrombocytopenia n Uremia: acute renal failure n Further symptoms / complications: o Central nervous system (seizures, hemorrhages) o Hypertension and heart failure o Liver / Pancreas (with diabetes mellitus) o Eye: retinal bleedings
 HUS: D+ and Dn D+ = Diarrhea-positive o Verotoxin (or Shigatoxin)-producing E. Coli o Other bacteria, e. g. Shigella …. („Big Mc disease“) o Hemorrhagic colitis: mild – severe, intussusception n D- = Diarrhea-negative o Pneumococcal infections (T-antigen positive) o Inherited and/or recurrent forms: e. g. complement (factor I/H) or v. WF-cleavage protease deficiency o Others: Pregnancy, drugs … o „Many“ cases of unknown cause
HUS: D+ and Dn D+ = Diarrhea-positive o Verotoxin (or Shigatoxin)-producing E. Coli o Other bacteria, e. g. Shigella …. („Big Mc disease“) o Hemorrhagic colitis: mild – severe, intussusception n D- = Diarrhea-negative o Pneumococcal infections (T-antigen positive) o Inherited and/or recurrent forms: e. g. complement (factor I/H) or v. WF-cleavage protease deficiency o Others: Pregnancy, drugs … o „Many“ cases of unknown cause
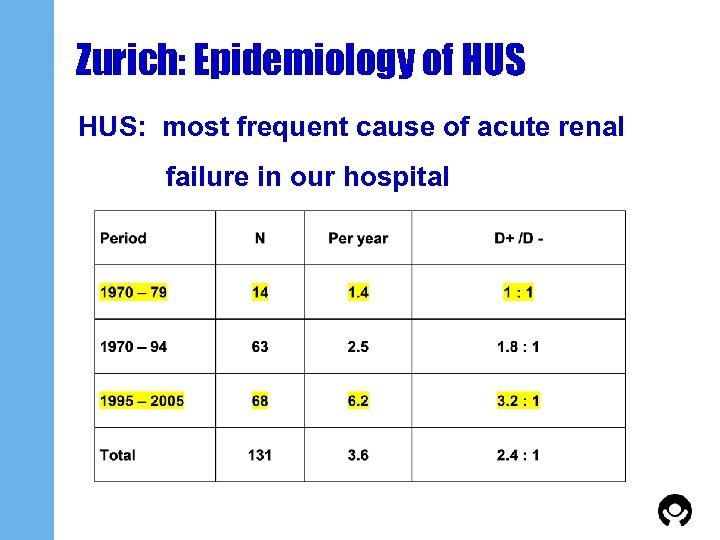 Zurich: Epidemiology of HUS: most frequent cause of acute renal failure in our hospital
Zurich: Epidemiology of HUS: most frequent cause of acute renal failure in our hospital
 HUS: Indications for dialysis modality since 1995 (1) n Peritoneal dialysis: „in general“ first choice o On ICU: CAPD o On ward: mainly automated PD n Hemodialysis if o „older“ patient in „good general condition“ not requiring care in intensive care unit o D-HUS and plasma-exchange (PEX) anticipated o life-threatening hyperkalemia
HUS: Indications for dialysis modality since 1995 (1) n Peritoneal dialysis: „in general“ first choice o On ICU: CAPD o On ward: mainly automated PD n Hemodialysis if o „older“ patient in „good general condition“ not requiring care in intensive care unit o D-HUS and plasma-exchange (PEX) anticipated o life-threatening hyperkalemia
 HUS: Indications for dialysis modality since 1995 (2) n Continuous veno-venous hemo(dia)filtration if o „in bad general condition“ (+/- PEX) o severe colitis n Plasma-exchange (PEX) or plasma infusion if o D-HUS and inherited type / complement deficiency suspected o D- or D+ HUS with severe central nervous system symptoms, e. g. impaired consciousness, neurological deficit
HUS: Indications for dialysis modality since 1995 (2) n Continuous veno-venous hemo(dia)filtration if o „in bad general condition“ (+/- PEX) o severe colitis n Plasma-exchange (PEX) or plasma infusion if o D-HUS and inherited type / complement deficiency suspected o D- or D+ HUS with severe central nervous system symptoms, e. g. impaired consciousness, neurological deficit
 Acute renal failure and peritoneal dialyis among adults ? ! n Recent review on „Renal replacement therapy of acute renal failure in ICU adult patients“ n … Peritoneal dialysis is not further discussed … because of o missing data o no significant role o 1 study showing a very high mortality ….
Acute renal failure and peritoneal dialyis among adults ? ! n Recent review on „Renal replacement therapy of acute renal failure in ICU adult patients“ n … Peritoneal dialysis is not further discussed … because of o missing data o no significant role o 1 study showing a very high mortality ….
 HUS: 1995 – 2005 (1) n N = 68: 30 males, 38 females n Age: median 2. 3 years (2 months – 12 years) n D+: 52 = 76%: 5 months – 12 years n D- : 16 = 24%: 2 months – 10 years o 6: pneumoccocal infection, 5 with septicemia o 1: acute systemic lupus erythematodes o 1: complement I deficiency (Dg: 9 yrs after onset !) o 1: familial occurrence (mother / grandmother) o 7: unknown cause
HUS: 1995 – 2005 (1) n N = 68: 30 males, 38 females n Age: median 2. 3 years (2 months – 12 years) n D+: 52 = 76%: 5 months – 12 years n D- : 16 = 24%: 2 months – 10 years o 6: pneumoccocal infection, 5 with septicemia o 1: acute systemic lupus erythematodes o 1: complement I deficiency (Dg: 9 yrs after onset !) o 1: familial occurrence (mother / grandmother) o 7: unknown cause
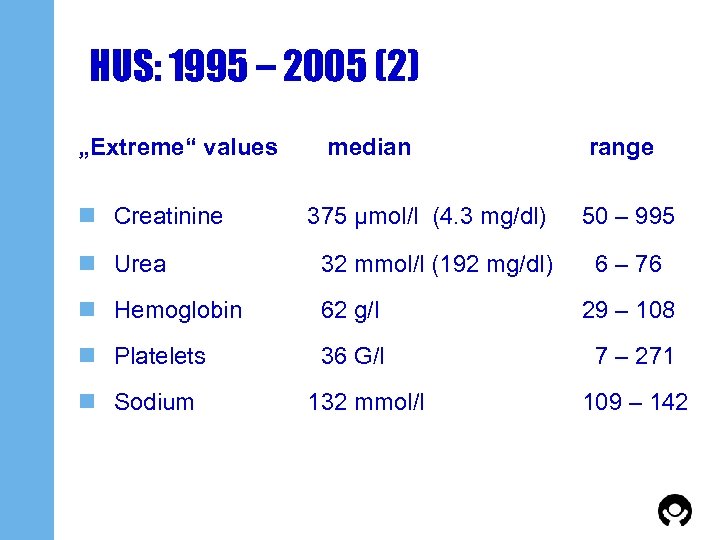 HUS: 1995 – 2005 (2) „Extreme“ values n Creatinine median 375 μmol/l (4. 3 mg/dl) range 50 – 995 n Urea 32 mmol/l (192 mg/dl) n Hemoglobin 62 g/l 29 – 108 n Platelets 36 G/l 7 – 271 n Sodium 132 mmol/l 6 – 76 109 – 142
HUS: 1995 – 2005 (2) „Extreme“ values n Creatinine median 375 μmol/l (4. 3 mg/dl) range 50 – 995 n Urea 32 mmol/l (192 mg/dl) n Hemoglobin 62 g/l 29 – 108 n Platelets 36 G/l 7 – 271 n Sodium 132 mmol/l 6 – 76 109 – 142
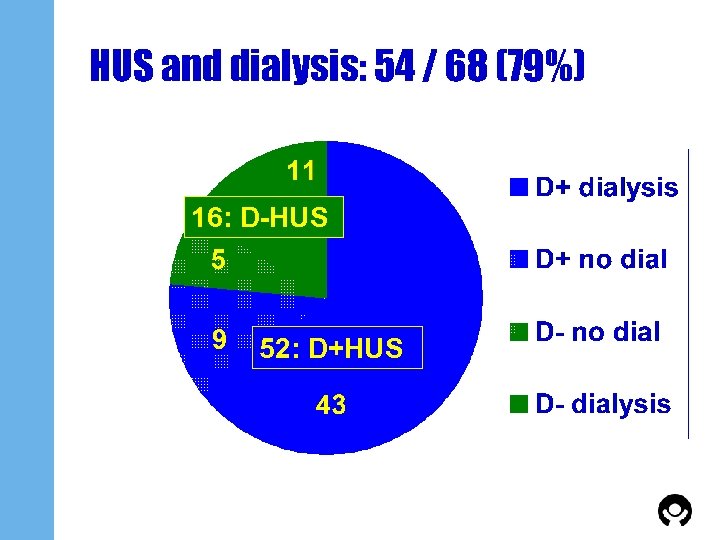 HUS and dialysis: 54 / 68 (79%) 16: D-HUS 52: D+HUS
HUS and dialysis: 54 / 68 (79%) 16: D-HUS 52: D+HUS
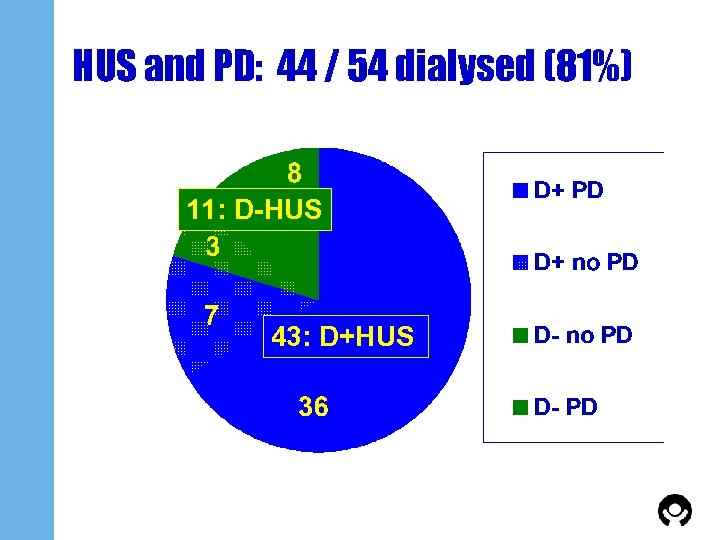 HUS and PD: 44 / 54 dialysed (81%) 11: D-HUS 43: D+HUS
HUS and PD: 44 / 54 dialysed (81%) 11: D-HUS 43: D+HUS
 Acute PD n before 1995: o „stiff“ Cook-catheter or o „soft“(„peel away“) catheter, inserted with trocar or o Tenckhoff n since 1995: o only Tenckhoff catheter o surgically placed by the surgeon (and the nephrologist also in theatre) under general anasthetic; at the same time insertion of central venous line
Acute PD n before 1995: o „stiff“ Cook-catheter or o „soft“(„peel away“) catheter, inserted with trocar or o Tenckhoff n since 1995: o only Tenckhoff catheter o surgically placed by the surgeon (and the nephrologist also in theatre) under general anasthetic; at the same time insertion of central venous line
 Acute and chronic PD n Tenckhoff catheter: o coil o 2 sizes: < / > 1 year o 1 cuff (glued by ourselves) o upward facing
Acute and chronic PD n Tenckhoff catheter: o coil o 2 sizes: < / > 1 year o 1 cuff (glued by ourselves) o upward facing
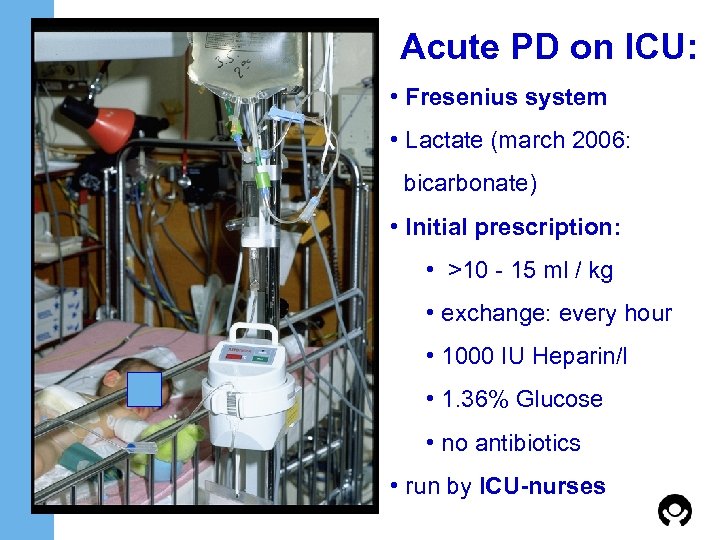 Acute PD on ICU: • Fresenius system • Lactate (march 2006: bicarbonate) • Initial prescription: • >10 - 15 ml / kg • exchange: every hour • 1000 IU Heparin/l • 1. 36% Glucose • no antibiotics • run by ICU-nurses
Acute PD on ICU: • Fresenius system • Lactate (march 2006: bicarbonate) • Initial prescription: • >10 - 15 ml / kg • exchange: every hour • 1000 IU Heparin/l • 1. 36% Glucose • no antibiotics • run by ICU-nurses
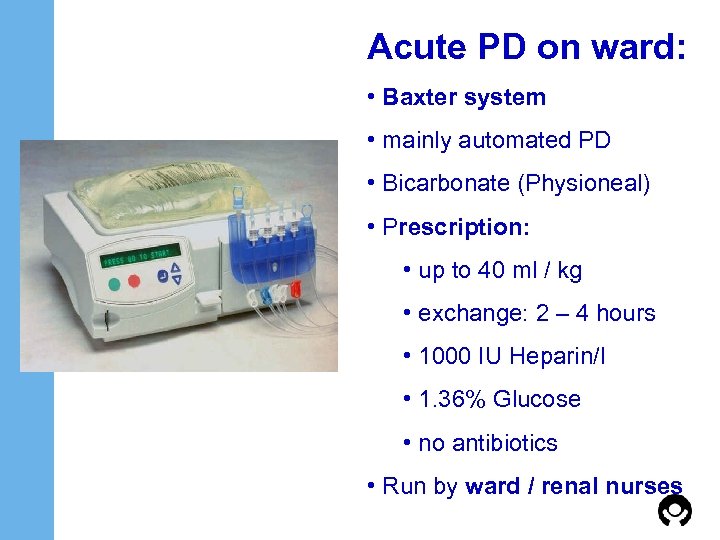 Acute PD on ward: • Baxter system • mainly automated PD • Bicarbonate (Physioneal) • Prescription: • up to 40 ml / kg • exchange: 2 – 4 hours • 1000 IU Heparin/l • 1. 36% Glucose • no antibiotics • Run by ward / renal nurses
Acute PD on ward: • Baxter system • mainly automated PD • Bicarbonate (Physioneal) • Prescription: • up to 40 ml / kg • exchange: 2 – 4 hours • 1000 IU Heparin/l • 1. 36% Glucose • no antibiotics • Run by ward / renal nurses
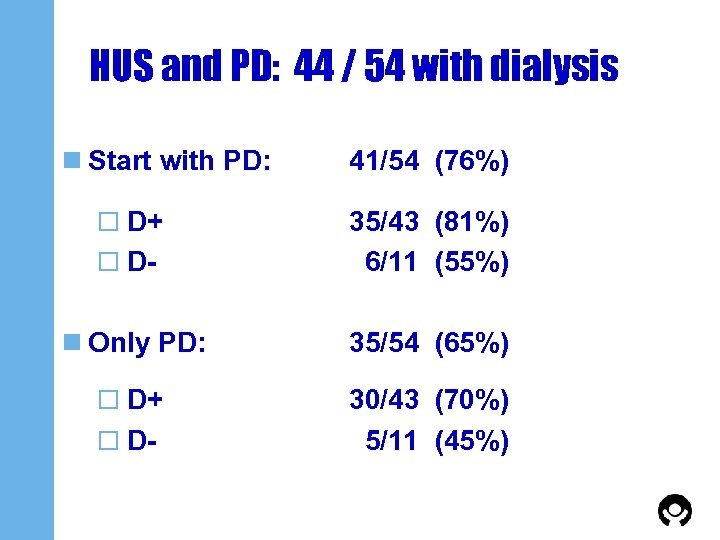 HUS and PD: 44 / 54 with dialysis n Start with PD: o D+ 41/54 (76%) o D- 35/43 (81%) 6/11 (55%) n Only PD: 35/54 (65%) o D+ 30/43 (70%) 5/11 (45%) o D-
HUS and PD: 44 / 54 with dialysis n Start with PD: o D+ 41/54 (76%) o D- 35/43 (81%) 6/11 (55%) n Only PD: 35/54 (65%) o D+ 30/43 (70%) 5/11 (45%) o D-
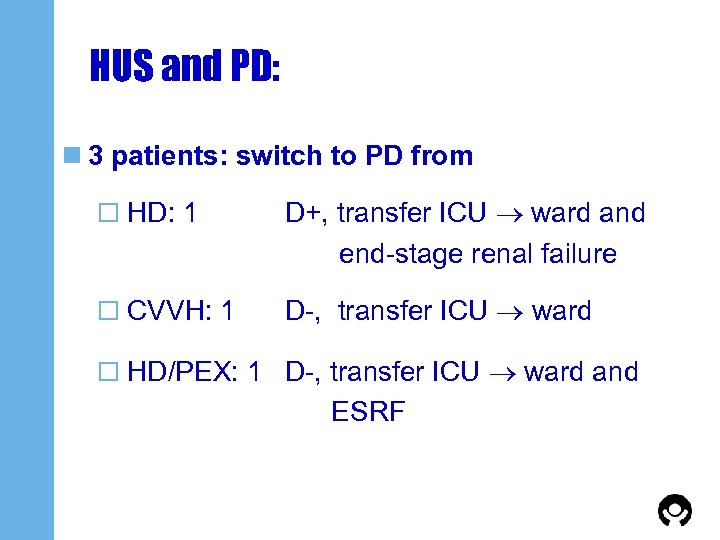 HUS and PD: n 3 patients: switch to PD from o HD: 1 D+, transfer ICU ward and end-stage renal failure o CVVH: 1 D-, transfer ICU ward o HD/PEX: 1 D-, transfer ICU ward and ESRF
HUS and PD: n 3 patients: switch to PD from o HD: 1 D+, transfer ICU ward and end-stage renal failure o CVVH: 1 D-, transfer ICU ward o HD/PEX: 1 D-, transfer ICU ward and ESRF
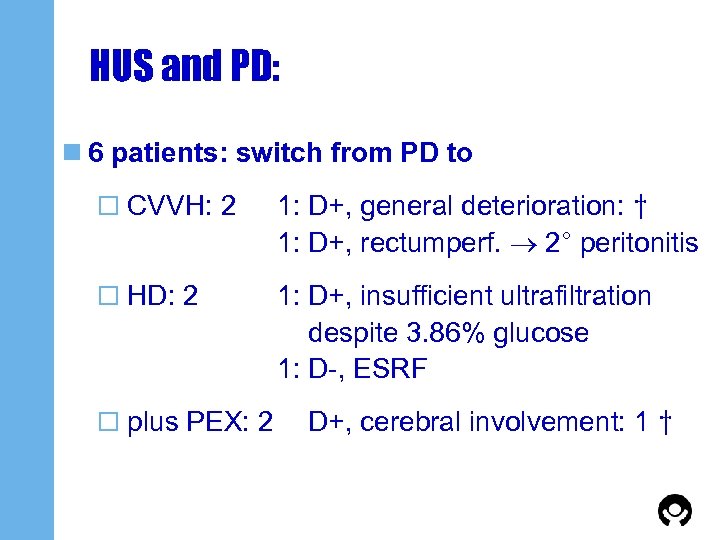 HUS and PD: n 6 patients: switch from PD to o CVVH: 2 1: D+, general deterioration: † 1: D+, rectumperf. 2° peritonitis o HD: 2 1: D+, insufficient ultrafiltration despite 3. 86% glucose 1: D-, ESRF o plus PEX: 2 D+, cerebral involvement: 1 †
HUS and PD: n 6 patients: switch from PD to o CVVH: 2 1: D+, general deterioration: † 1: D+, rectumperf. 2° peritonitis o HD: 2 1: D+, insufficient ultrafiltration despite 3. 86% glucose 1: D-, ESRF o plus PEX: 2 D+, cerebral involvement: 1 †
 HUS and PD: technical aspects n Time span between emergency room entry and onset of PD in ICU: o median 4 hours (2 – 20) n Duration of PD: o median 10 days (1 – 35)
HUS and PD: technical aspects n Time span between emergency room entry and onset of PD in ICU: o median 4 hours (2 – 20) n Duration of PD: o median 10 days (1 – 35)
 HUS and PD: technical complications n Peritonitis: n = 9 (all in ICU) n Exit-site infection n=3 n Insufficient ultrafiltration: n = 1 switch: HD n Catheter obstruction: n=0 n Insufficient dialysis: n=0 No catheter had to be replaced.
HUS and PD: technical complications n Peritonitis: n = 9 (all in ICU) n Exit-site infection n=3 n Insufficient ultrafiltration: n = 1 switch: HD n Catheter obstruction: n=0 n Insufficient dialysis: n=0 No catheter had to be replaced.
 HUS and hemofiltration n Hemofiltration: 7 o Only CVVH: 2 o 1 D+: presentation with epileptic state o 1 D-: pneumoccocal septicemia o CVVH and PD: 3 o CVVH and HD: 2
HUS and hemofiltration n Hemofiltration: 7 o Only CVVH: 2 o 1 D+: presentation with epileptic state o 1 D-: pneumoccocal septicemia o CVVH and PD: 3 o CVVH and HD: 2
 HUS and hemodialysis / PEX n Only HD: 5, all D+ HUS o 3: older patients – 12 years – in „good condition“ o 1: recurrent intussusception and bowel resection before onset of ARF o 1: severe hemorrhagic colitis n Plus PEX: 4 o 2 D-, 2 D+
HUS and hemodialysis / PEX n Only HD: 5, all D+ HUS o 3: older patients – 12 years – in „good condition“ o 1: recurrent intussusception and bowel resection before onset of ARF o 1: severe hemorrhagic colitis n Plus PEX: 4 o 2 D-, 2 D+
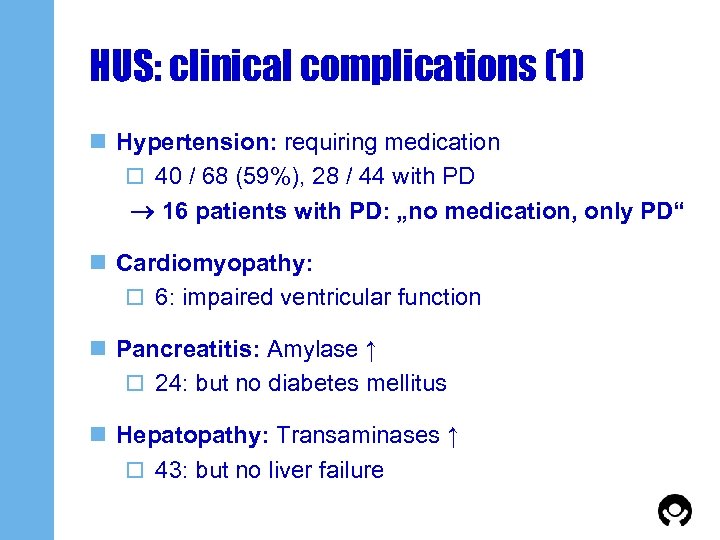 HUS: clinical complications (1) n Hypertension: requiring medication o 40 / 68 (59%), 28 / 44 with PD 16 patients with PD: „no medication, only PD“ n Cardiomyopathy: o 6: impaired ventricular function n Pancreatitis: Amylase ↑ o 24: but no diabetes mellitus n Hepatopathy: Transaminases ↑ o 43: but no liver failure
HUS: clinical complications (1) n Hypertension: requiring medication o 40 / 68 (59%), 28 / 44 with PD 16 patients with PD: „no medication, only PD“ n Cardiomyopathy: o 6: impaired ventricular function n Pancreatitis: Amylase ↑ o 24: but no diabetes mellitus n Hepatopathy: Transaminases ↑ o 43: but no liver failure
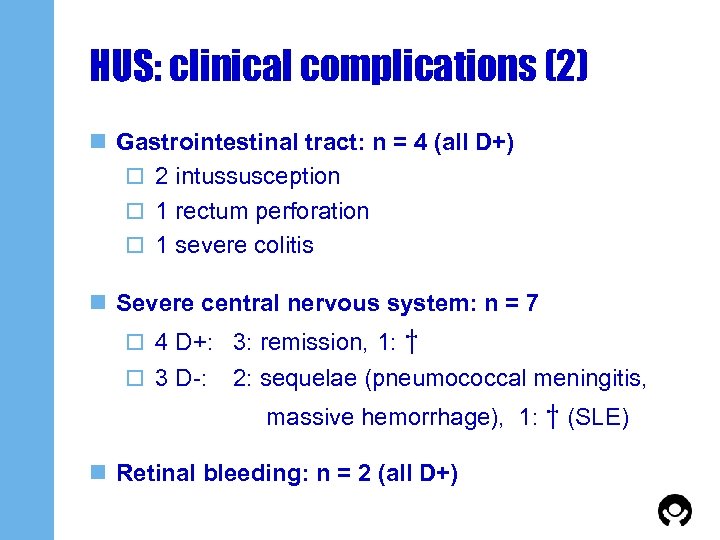 HUS: clinical complications (2) n Gastrointestinal tract: n = 4 (all D+) o 2 intussusception o 1 rectum perforation o 1 severe colitis n Severe central nervous system: n = 7 o 4 D+: 3: remission, 1: o 3 D-: † 2: sequelae (pneumococcal meningitis, massive hemorrhage), 1: † (SLE) n Retinal bleeding: n = 2 (all D+)
HUS: clinical complications (2) n Gastrointestinal tract: n = 4 (all D+) o 2 intussusception o 1 rectum perforation o 1 severe colitis n Severe central nervous system: n = 7 o 4 D+: 3: remission, 1: o 3 D-: † 2: sequelae (pneumococcal meningitis, massive hemorrhage), 1: † (SLE) n Retinal bleeding: n = 2 (all D+)
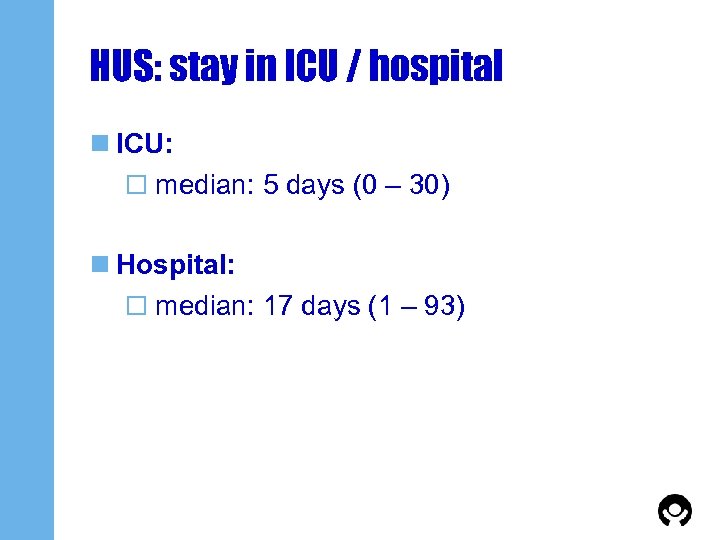 HUS: stay in ICU / hospital n ICU: o median: 5 days (0 – 30) n Hospital: o median: 17 days (1 – 93)
HUS: stay in ICU / hospital n ICU: o median: 5 days (0 – 30) n Hospital: o median: 17 days (1 – 93)
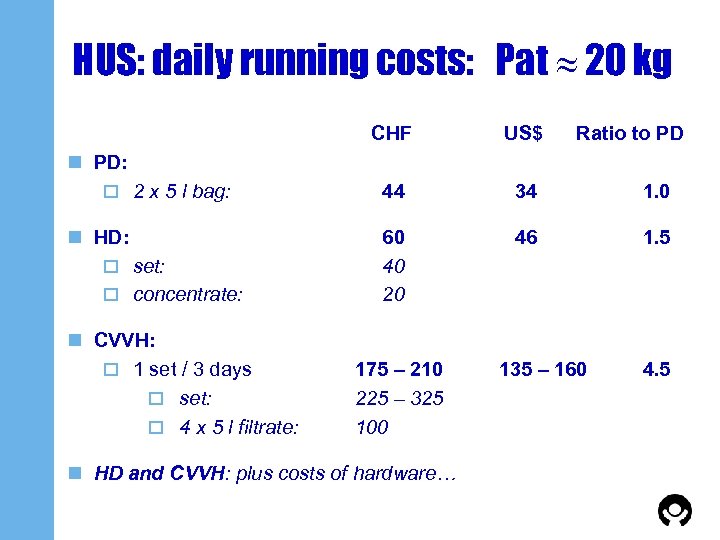 HUS: daily running costs: Pat 20 kg CHF US$ Ratio to PD 44 34 1. 0 60 40 20 46 1. 5 n PD: o 2 x 5 l bag: n HD: o set: o concentrate: n CVVH: o 1 set / 3 days o set: o 4 x 5 l filtrate: 175 – 210 225 – 325 100 n HD and CVVH: plus costs of hardware… 135 – 160 4. 5
HUS: daily running costs: Pat 20 kg CHF US$ Ratio to PD 44 34 1. 0 60 40 20 46 1. 5 n PD: o 2 x 5 l bag: n HD: o set: o concentrate: n CVVH: o 1 set / 3 days o set: o 4 x 5 l filtrate: 175 – 210 225 – 325 100 n HD and CVVH: plus costs of hardware… 135 – 160 4. 5
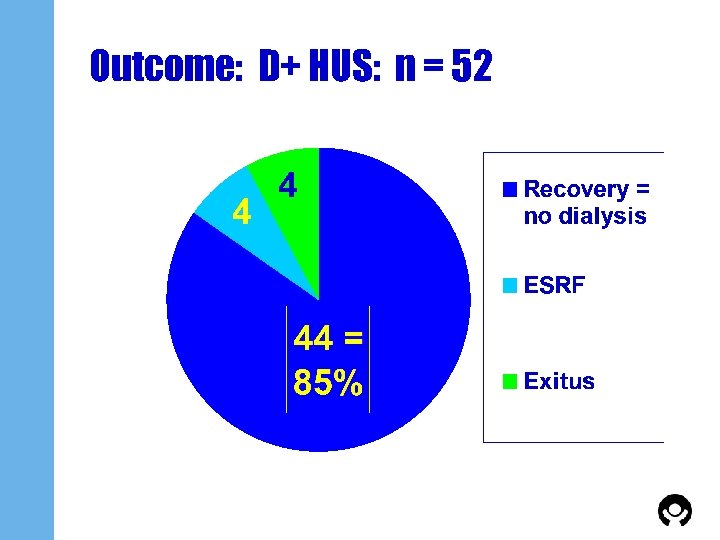 Outcome: D+ HUS: n = 52
Outcome: D+ HUS: n = 52
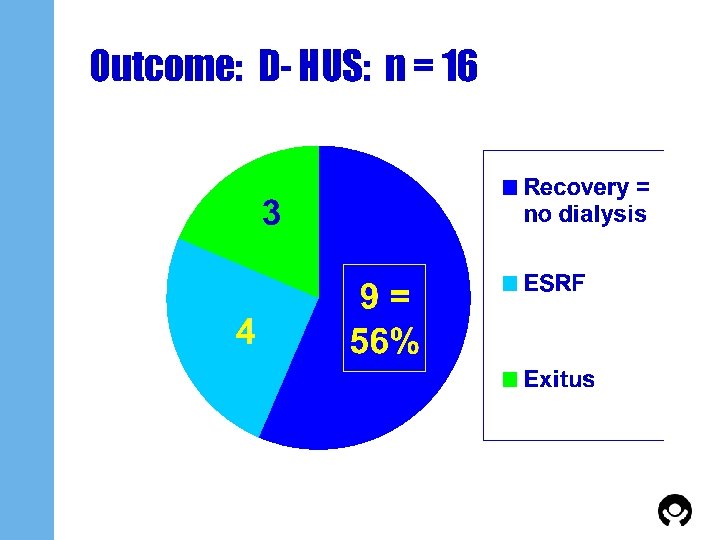 Outcome: D- HUS: n = 16
Outcome: D- HUS: n = 16
 Conclusions (1): HUS n Incidence: o D+ >>> D- (over the last 35 years) n 80% require dialysis n Outcome: D+ >> Do Patient survival o Recovery of renal function
Conclusions (1): HUS n Incidence: o D+ >>> D- (over the last 35 years) n 80% require dialysis n Outcome: D+ >> Do Patient survival o Recovery of renal function
 Conclusions (2): HUS – PD n Surgically placed Tenckhoff-catheter: o Simple technique o High efficacy o Low frequency of side effects / complications n PD in HUS is o safe o efficient o convenient o economic
Conclusions (2): HUS – PD n Surgically placed Tenckhoff-catheter: o Simple technique o High efficacy o Low frequency of side effects / complications n PD in HUS is o safe o efficient o convenient o economic