d1a3d2fe573aa84153ec0f75f3fe24c1.ppt
- Количество слайдов: 49
 PCCRT Conference London 2015 Fluid Resuscitation for Septic Shock Joseph A Carcillo MD University of Pittsburgh
PCCRT Conference London 2015 Fluid Resuscitation for Septic Shock Joseph A Carcillo MD University of Pittsburgh
![Energy metabolism provides ATP Lack of ATP = Shock Oxygen Delivery = [Oxygen Content] Energy metabolism provides ATP Lack of ATP = Shock Oxygen Delivery = [Oxygen Content]](https://present5.com/presentation/d1a3d2fe573aa84153ec0f75f3fe24c1/image-2.jpg) Energy metabolism provides ATP Lack of ATP = Shock Oxygen Delivery = [Oxygen Content] x Flow DO 2 = [1. 36 x %Hgb + O 2 sat + pa. O 2 x 0. 003] x [CO] O 2 diffusion Glucose Delivery Glucose + Insulin sensitivity Glucose Hypoxic Give Oxygen Anemic Give Blood Ischemic Fluid bolus if hypovolemic ATP Inotrope if Low Cardiac Shock Output Syndrome Lack of ATP = Shock Vasopressor if Hypotensive despite adequate fluid status Insulin sensitive Glucose transporter Glycopenic Shock Give glucose or Insulin + glucose
Energy metabolism provides ATP Lack of ATP = Shock Oxygen Delivery = [Oxygen Content] x Flow DO 2 = [1. 36 x %Hgb + O 2 sat + pa. O 2 x 0. 003] x [CO] O 2 diffusion Glucose Delivery Glucose + Insulin sensitivity Glucose Hypoxic Give Oxygen Anemic Give Blood Ischemic Fluid bolus if hypovolemic ATP Inotrope if Low Cardiac Shock Output Syndrome Lack of ATP = Shock Vasopressor if Hypotensive despite adequate fluid status Insulin sensitive Glucose transporter Glycopenic Shock Give glucose or Insulin + glucose
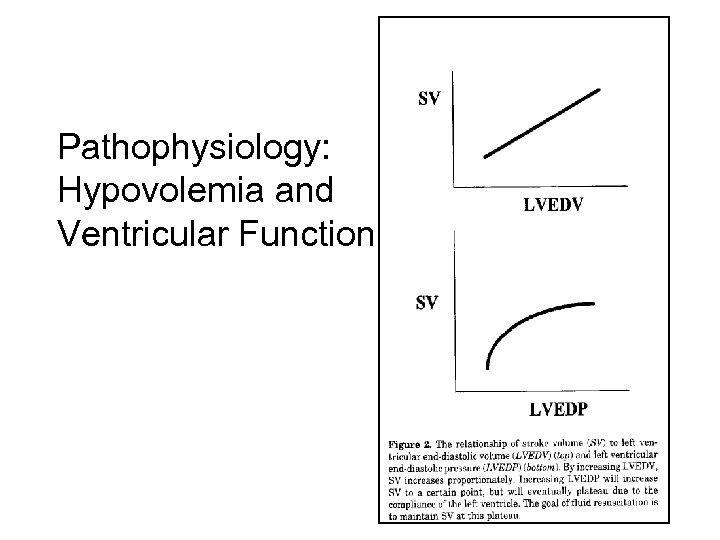 Pathophysiology: Hypovolemia and Ventricular Function
Pathophysiology: Hypovolemia and Ventricular Function
 Can I Give Too Much Fluid? You most certainly can! • • • Check for Hepatomegaly Check for Rales Evaluate MAP – CVP Evaluate SVV, or SBP variation Give diuretics Use Dialysis CRRT if unsucuccessful • You can definitely do harm if you do not attend to this! Some children need no 0 m. Ls / kg of fluid while others need up to 60 m. L/kg of fluid during resuscitation.
Can I Give Too Much Fluid? You most certainly can! • • • Check for Hepatomegaly Check for Rales Evaluate MAP – CVP Evaluate SVV, or SBP variation Give diuretics Use Dialysis CRRT if unsucuccessful • You can definitely do harm if you do not attend to this! Some children need no 0 m. Ls / kg of fluid while others need up to 60 m. L/kg of fluid during resuscitation.
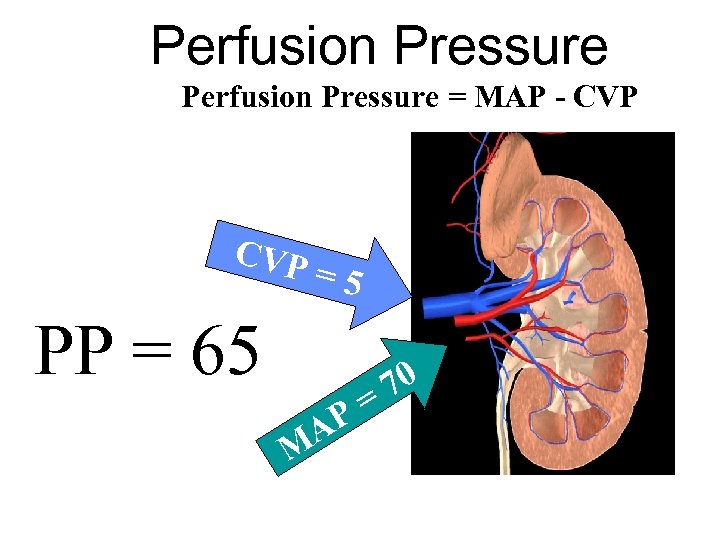 Perfusion Pressure = MAP - CVP =5 PP = 65 AP M 70 =
Perfusion Pressure = MAP - CVP =5 PP = 65 AP M 70 =
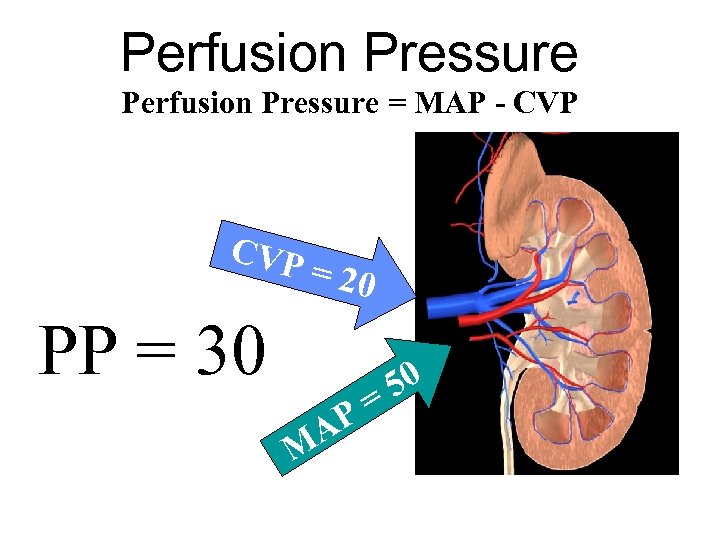 Perfusion Pressure = MAP - CVP = 20 PP = 30 AP M 50 =
Perfusion Pressure = MAP - CVP = 20 PP = 30 AP M 50 =
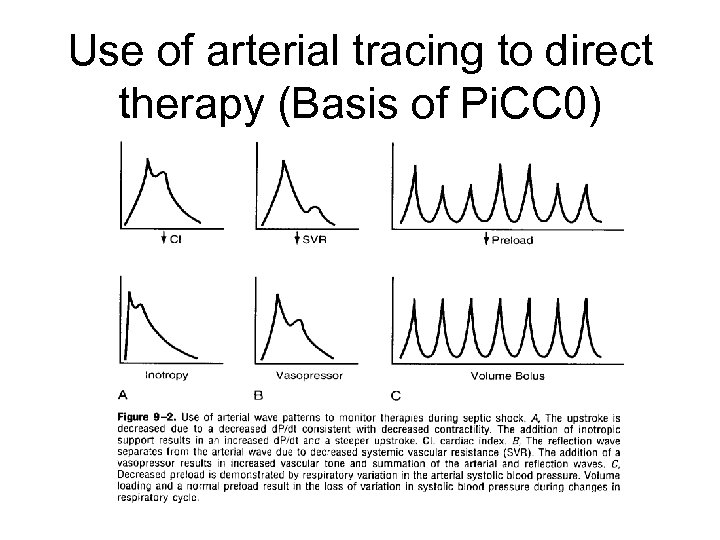 Use of arterial tracing to direct therapy (Basis of Pi. CC 0)
Use of arterial tracing to direct therapy (Basis of Pi. CC 0)
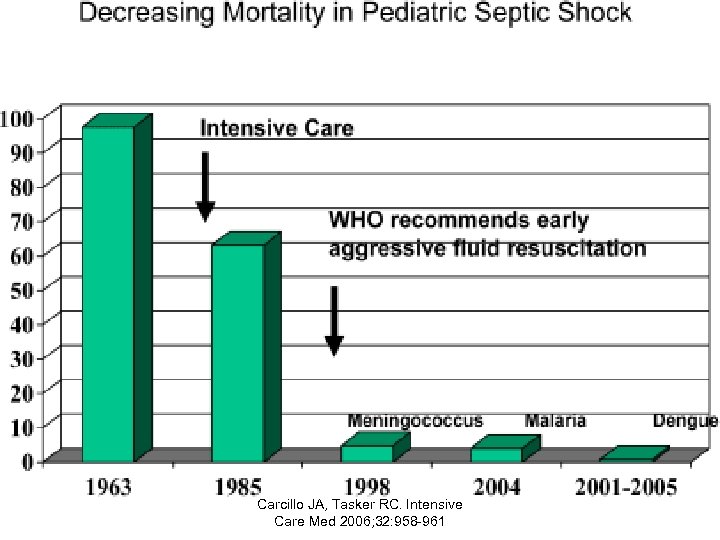 Carcillo JA, Tasker RC. Intensive Care Med 2006; 32: 958 -961
Carcillo JA, Tasker RC. Intensive Care Med 2006; 32: 958 -961
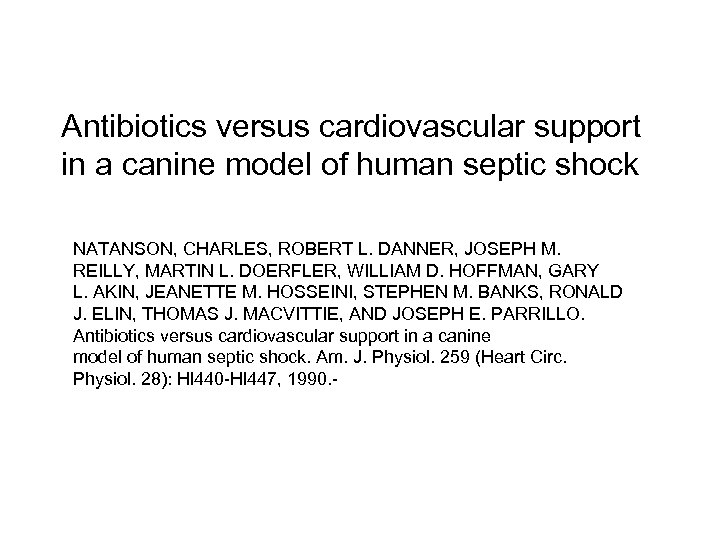 Antibiotics versus cardiovascular support in a canine model of human septic shock NATANSON, CHARLES, ROBERT L. DANNER, JOSEPH M. REILLY, MARTIN L. DOERFLER, WILLIAM D. HOFFMAN, GARY L. AKIN, JEANETTE M. HOSSEINI, STEPHEN M. BANKS, RONALD J. ELIN, THOMAS J. MACVITTIE, AND JOSEPH E. PARRILLO. Antibiotics versus cardiovascular support in a canine model of human septic shock. Am. J. Physiol. 259 (Heart Circ. Physiol. 28): Hl 440 -Hl 447, 1990. -
Antibiotics versus cardiovascular support in a canine model of human septic shock NATANSON, CHARLES, ROBERT L. DANNER, JOSEPH M. REILLY, MARTIN L. DOERFLER, WILLIAM D. HOFFMAN, GARY L. AKIN, JEANETTE M. HOSSEINI, STEPHEN M. BANKS, RONALD J. ELIN, THOMAS J. MACVITTIE, AND JOSEPH E. PARRILLO. Antibiotics versus cardiovascular support in a canine model of human septic shock. Am. J. Physiol. 259 (Heart Circ. Physiol. 28): Hl 440 -Hl 447, 1990. -
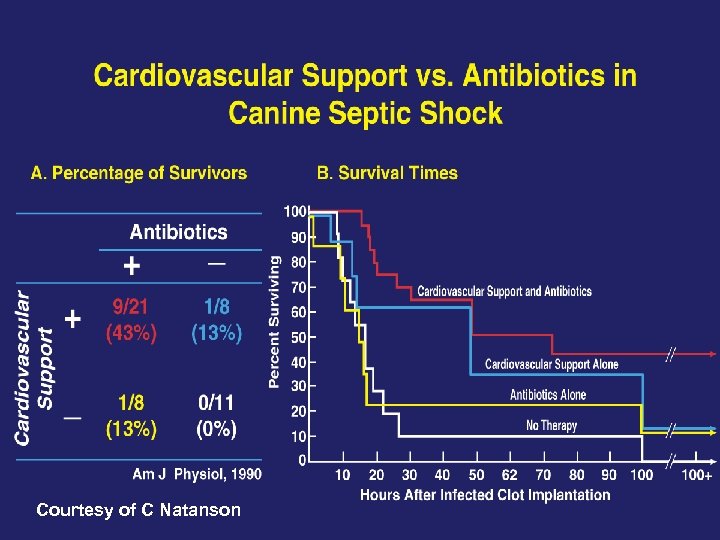 Courtesy of C Natanson
Courtesy of C Natanson
 Protective Antigen Antibody Augments Hemodynamic Support in Anthrax Lethal Toxin Shock in Canines Amisha V. Barochia, 1 Xizhong Cui, 1 Junfeng Sun, 1 Yan Li, 1 Steven B. Solomon, 1 Thi-Sau Migone, 2 G. Mani Subramanian, 2, a Sally D. Bolmer, 2 and Peter Q. Eichacker 1 1 Critical Care Medicine Department, Clinical Center, National Institutes of Health, Bethesda; and 2 Human Genome Sciences, Rockville, Maryland Journal of Infectious Diseases Advance Access published January 5, 2012
Protective Antigen Antibody Augments Hemodynamic Support in Anthrax Lethal Toxin Shock in Canines Amisha V. Barochia, 1 Xizhong Cui, 1 Junfeng Sun, 1 Yan Li, 1 Steven B. Solomon, 1 Thi-Sau Migone, 2 G. Mani Subramanian, 2, a Sally D. Bolmer, 2 and Peter Q. Eichacker 1 1 Critical Care Medicine Department, Clinical Center, National Institutes of Health, Bethesda; and 2 Human Genome Sciences, Rockville, Maryland Journal of Infectious Diseases Advance Access published January 5, 2012
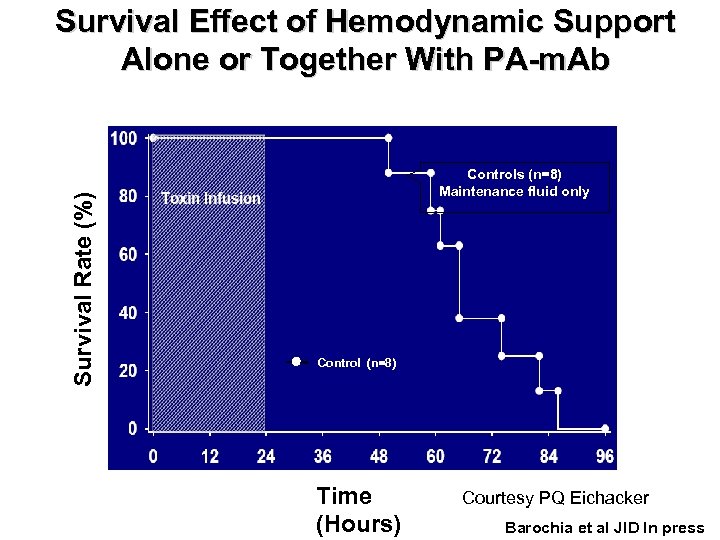 Survival Rate (%) Survival Effect of Hemodynamic Support Alone or Together With PA-m. Ab Controls (n=8) Maintenance fluid only Control (n=8) Time (Hours) Courtesy PQ Eichacker Barochia et al JID In press
Survival Rate (%) Survival Effect of Hemodynamic Support Alone or Together With PA-m. Ab Controls (n=8) Maintenance fluid only Control (n=8) Time (Hours) Courtesy PQ Eichacker Barochia et al JID In press
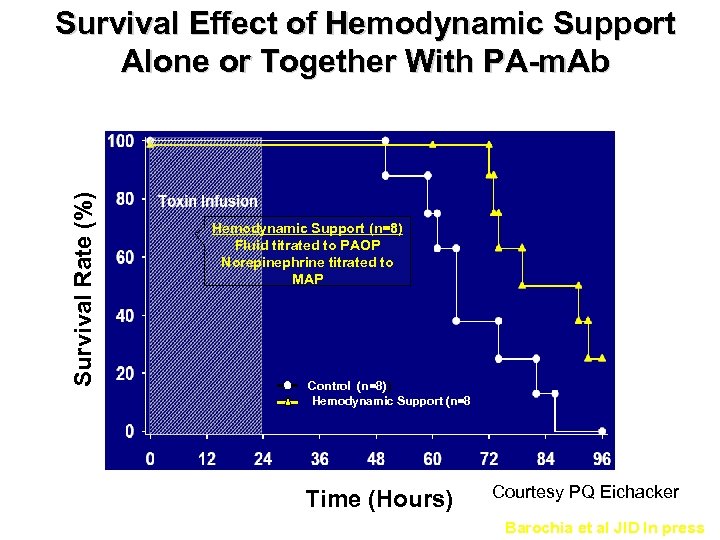 Survival Effect of Hemodynamic Support Alone or Together With PA-m. Ab Survival Rate (%) Hemodynamic Support (n=8) Fluid titrated to PAOP Norepinephrine titrated to MAP Control (n=8)) Hemodynamic Support (n=8 Time (Hours) Courtesy PQ Eichacker Barochia et al JID In press
Survival Effect of Hemodynamic Support Alone or Together With PA-m. Ab Survival Rate (%) Hemodynamic Support (n=8) Fluid titrated to PAOP Norepinephrine titrated to MAP Control (n=8)) Hemodynamic Support (n=8 Time (Hours) Courtesy PQ Eichacker Barochia et al JID In press
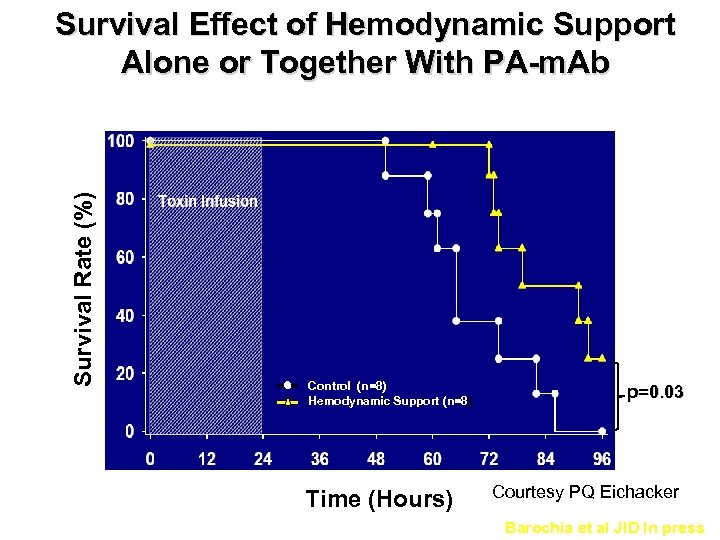 Survival Rate (%) Survival Effect of Hemodynamic Support Alone or Together With PA-m. Ab Control (n=8) Hemodynamic Support (n=8) Time (Hours) p=0. 03 Courtesy PQ Eichacker Barochia et al JID In press
Survival Rate (%) Survival Effect of Hemodynamic Support Alone or Together With PA-m. Ab Control (n=8) Hemodynamic Support (n=8) Time (Hours) p=0. 03 Courtesy PQ Eichacker Barochia et al JID In press
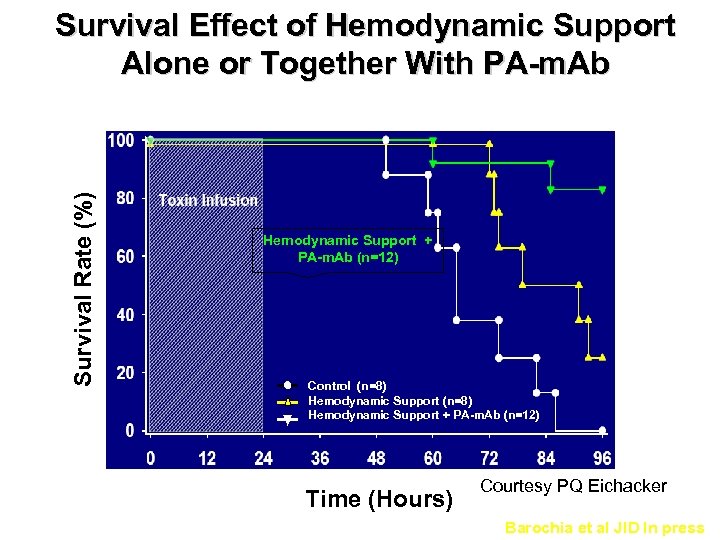 Survival Rate (%) Survival Effect of Hemodynamic Support Alone or Together With PA-m. Ab Hemodynamic Support + PA-m. Ab (n=12) Control (n=8) Hemodynamic Support + PA-m. Ab (n=12) Time (Hours) Courtesy PQ Eichacker Barochia et al JID In press
Survival Rate (%) Survival Effect of Hemodynamic Support Alone or Together With PA-m. Ab Hemodynamic Support + PA-m. Ab (n=12) Control (n=8) Hemodynamic Support + PA-m. Ab (n=12) Time (Hours) Courtesy PQ Eichacker Barochia et al JID In press
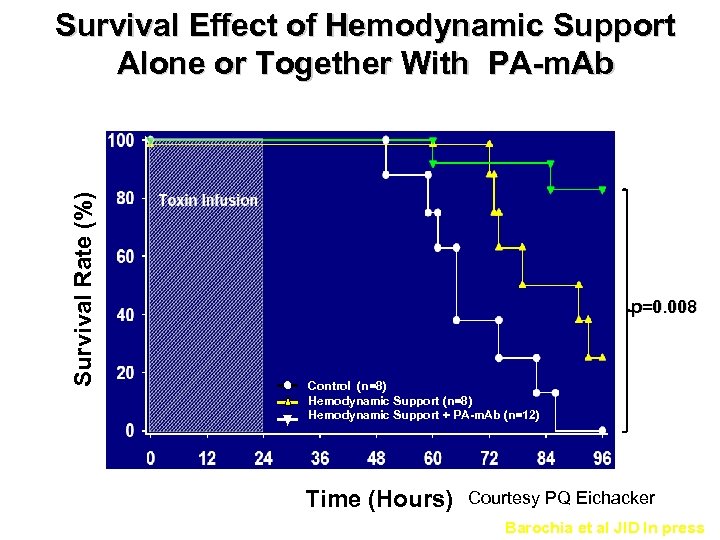 Survival Effect of Hemodynamic Support Alone or Together With PA-m. Ab Survival Rate (%) p=0. 008 Control (n=8) Hemodynamic Support + PA-m. Ab (n=12) Time (Hours) Courtesy PQ Eichacker Barochia et al JID In press
Survival Effect of Hemodynamic Support Alone or Together With PA-m. Ab Survival Rate (%) p=0. 008 Control (n=8) Hemodynamic Support + PA-m. Ab (n=12) Time (Hours) Courtesy PQ Eichacker Barochia et al JID In press
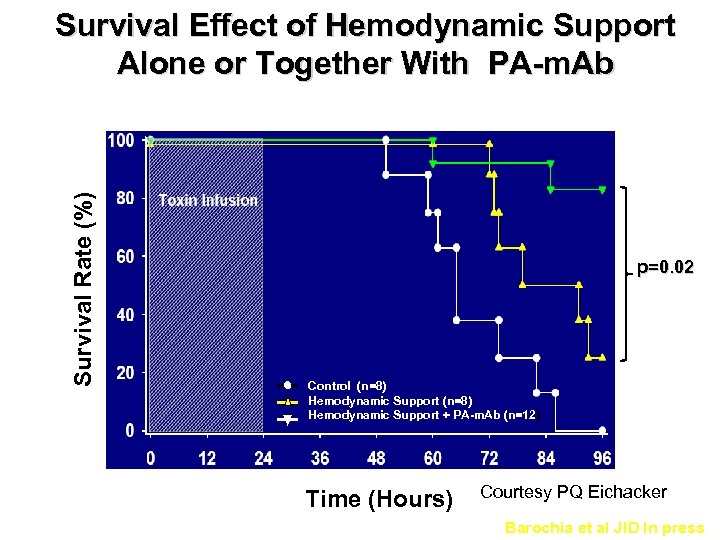 Survival Rate (%) Survival Effect of Hemodynamic Support Alone or Together With PA-m. Ab p=0. 02 Control (n=8) Hemodynamic Support + PA-m. Ab (n=12) Time (Hours) Courtesy PQ Eichacker Barochia et al JID In press
Survival Rate (%) Survival Effect of Hemodynamic Support Alone or Together With PA-m. Ab p=0. 02 Control (n=8) Hemodynamic Support + PA-m. Ab (n=12) Time (Hours) Courtesy PQ Eichacker Barochia et al JID In press
 Role of Early Fluid Resuscitation in Pediatric Septic Shock (Carcillo et al JAMA 266, 1991) • 34 patients in ED over 6 year period with septic shock and PAC at 6 hours. • Evaluated amount of fluid resuscitation and relation to following outcome variables: cardiogenic pulmonary edema, non-cardiogenic pulmonary edema, persistent hypovolemia, and survival
Role of Early Fluid Resuscitation in Pediatric Septic Shock (Carcillo et al JAMA 266, 1991) • 34 patients in ED over 6 year period with septic shock and PAC at 6 hours. • Evaluated amount of fluid resuscitation and relation to following outcome variables: cardiogenic pulmonary edema, non-cardiogenic pulmonary edema, persistent hypovolemia, and survival
 Epidemiology • • Overall mortality rate was 47% 82 % ventilator supported by 6 hrs 100% inotrope / vasopressor by 6 hrs 33 ml/kg volume (9 ml/kg colloid) at 1 hr 95 ml/kg volume (37 ml/kg colloid) at 6 hrs
Epidemiology • • Overall mortality rate was 47% 82 % ventilator supported by 6 hrs 100% inotrope / vasopressor by 6 hrs 33 ml/kg volume (9 ml/kg colloid) at 1 hr 95 ml/kg volume (37 ml/kg colloid) at 6 hrs
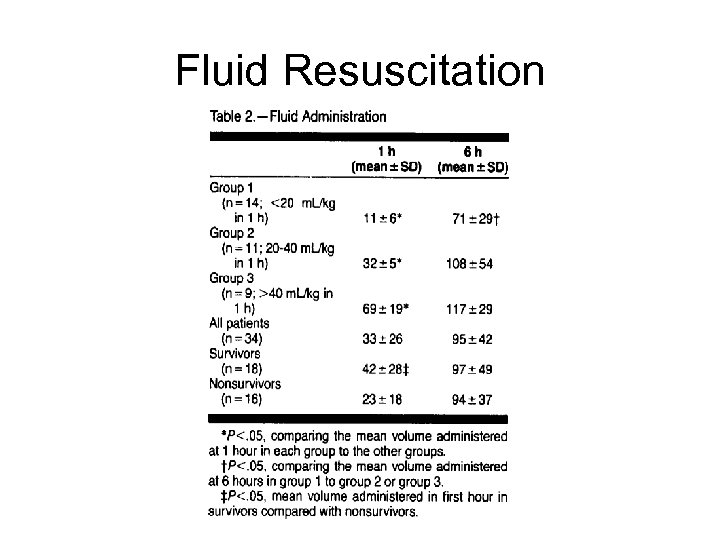 Fluid Resuscitation
Fluid Resuscitation
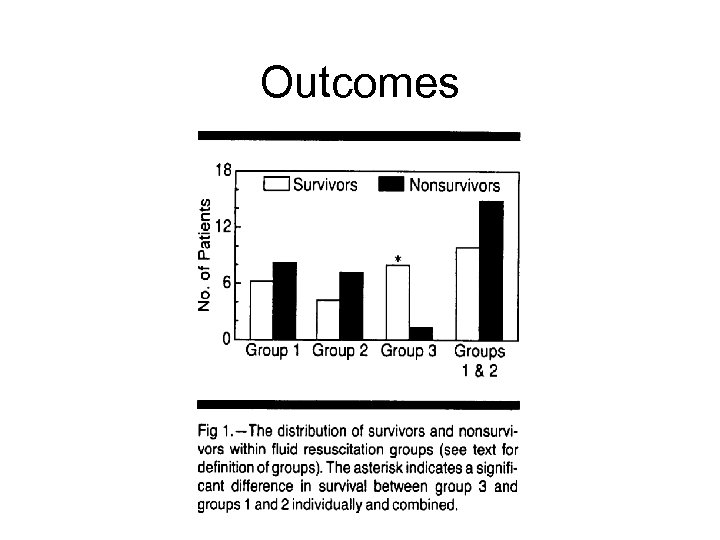 Outcomes
Outcomes
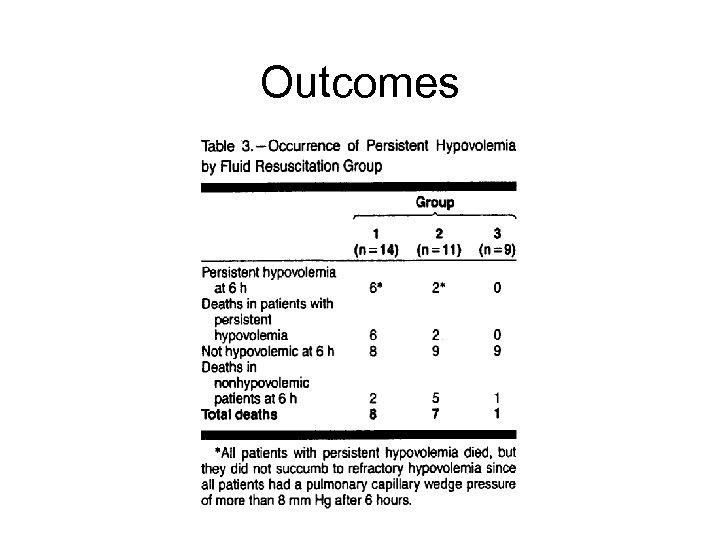 Outcomes
Outcomes
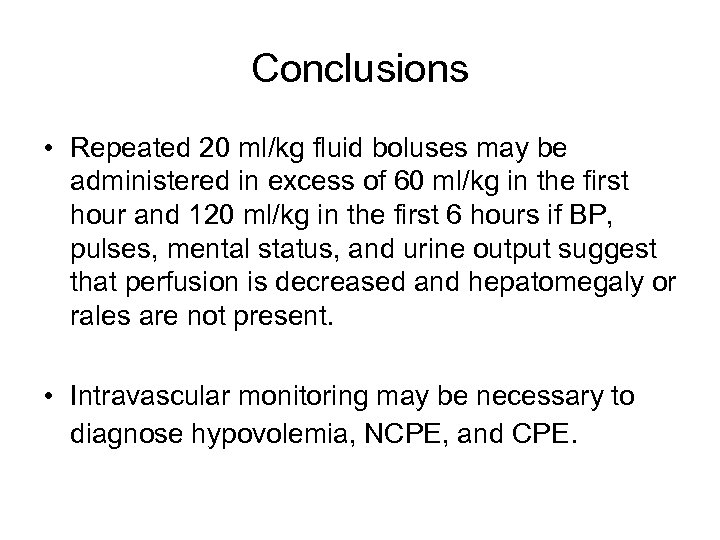 Conclusions • Repeated 20 ml/kg fluid boluses may be administered in excess of 60 ml/kg in the first hour and 120 ml/kg in the first 6 hours if BP, pulses, mental status, and urine output suggest that perfusion is decreased and hepatomegaly or rales are not present. • Intravascular monitoring may be necessary to diagnose hypovolemia, NCPE, and CPE.
Conclusions • Repeated 20 ml/kg fluid boluses may be administered in excess of 60 ml/kg in the first hour and 120 ml/kg in the first 6 hours if BP, pulses, mental status, and urine output suggest that perfusion is decreased and hepatomegaly or rales are not present. • Intravascular monitoring may be necessary to diagnose hypovolemia, NCPE, and CPE.
 Implementation of goal-directed therapy for children with suspected sepsis in the emergency department. Cruz AT, Perry AM, Williams EA, Graf JM, Wuestner ER, Patel B. Pediatrics. 2011 Mar; 127(3): e 758 -66. doi: 10. 1542/peds. 2010 -2895. Epub 2011 Feb 21.
Implementation of goal-directed therapy for children with suspected sepsis in the emergency department. Cruz AT, Perry AM, Williams EA, Graf JM, Wuestner ER, Patel B. Pediatrics. 2011 Mar; 127(3): e 758 -66. doi: 10. 1542/peds. 2010 -2895. Epub 2011 Feb 21.
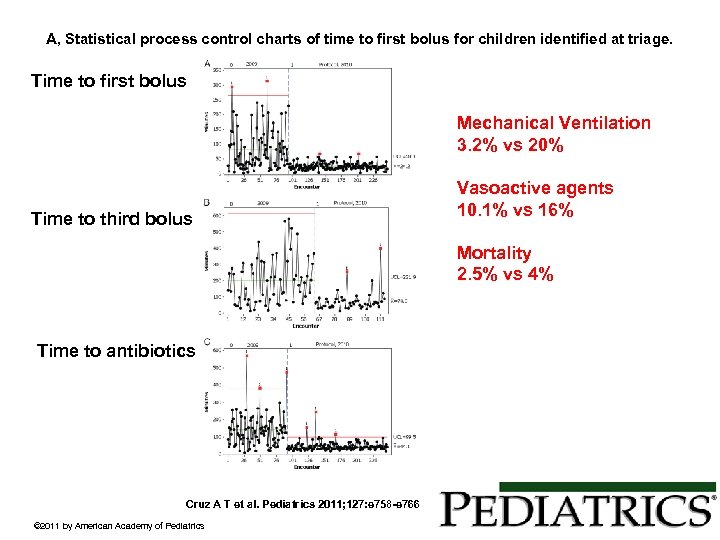 A, Statistical process control charts of time to first bolus for children identified at triage. Time to first bolus Mechanical Ventilation 3. 2% vs 20% Time to third bolus Vasoactive agents 10. 1% vs 16% Mortality 2. 5% vs 4% Time to antibiotics Cruz A T et al. Pediatrics 2011; 127: e 758 -e 766 © 2011 by American Academy of Pediatrics
A, Statistical process control charts of time to first bolus for children identified at triage. Time to first bolus Mechanical Ventilation 3. 2% vs 20% Time to third bolus Vasoactive agents 10. 1% vs 16% Mortality 2. 5% vs 4% Time to antibiotics Cruz A T et al. Pediatrics 2011; 127: e 758 -e 766 © 2011 by American Academy of Pediatrics
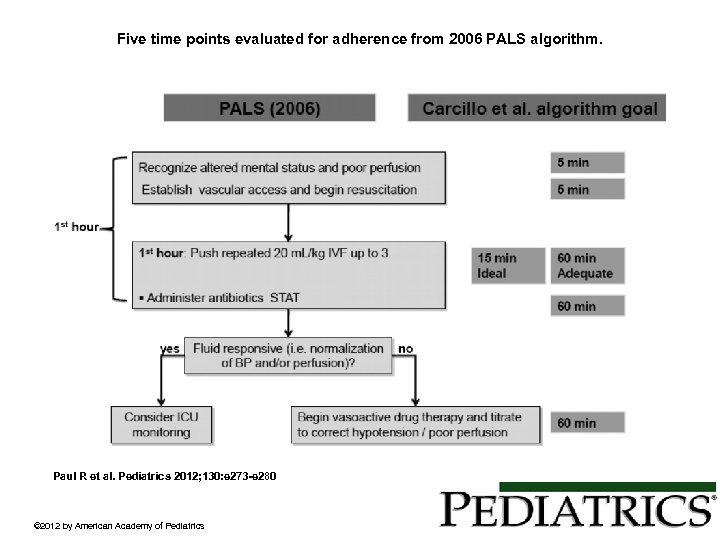 Five time points evaluated for adherence from 2006 PALS algorithm. Paul R et al. Pediatrics 2012; 130: e 273 -e 280 © 2012 by American Academy of Pediatrics
Five time points evaluated for adherence from 2006 PALS algorithm. Paul R et al. Pediatrics 2012; 130: e 273 -e 280 © 2012 by American Academy of Pediatrics
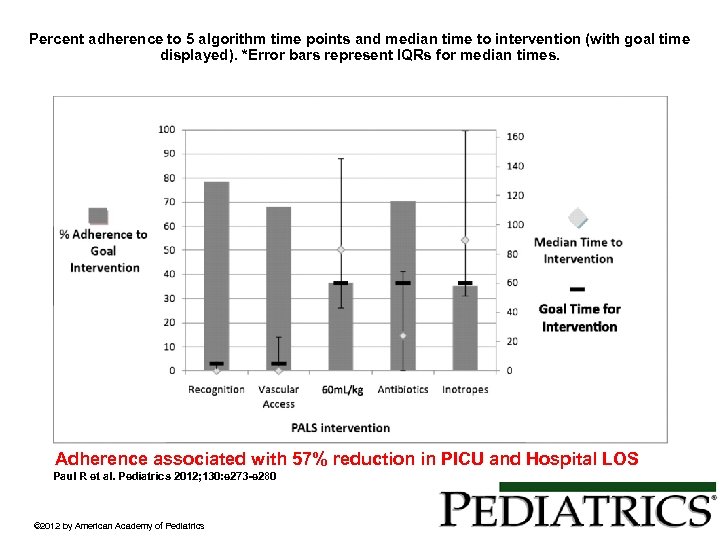 Percent adherence to 5 algorithm time points and median time to intervention (with goal time displayed). *Error bars represent IQRs for median times. Adherence associated with 57% reduction in PICU and Hospital LOS Paul R et al. Pediatrics 2012; 130: e 273 -e 280 © 2012 by American Academy of Pediatrics
Percent adherence to 5 algorithm time points and median time to intervention (with goal time displayed). *Error bars represent IQRs for median times. Adherence associated with 57% reduction in PICU and Hospital LOS Paul R et al. Pediatrics 2012; 130: e 273 -e 280 © 2012 by American Academy of Pediatrics
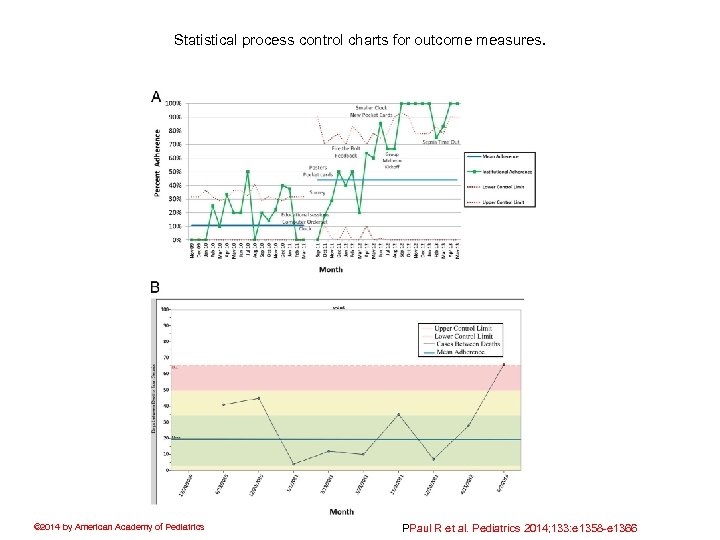 Statistical process control charts for outcome measures. © 2014 by American Academy of Pediatrics PPaul R et al. Pediatrics 2014; 133: e 1358 -e 1366
Statistical process control charts for outcome measures. © 2014 by American Academy of Pediatrics PPaul R et al. Pediatrics 2014; 133: e 1358 -e 1366
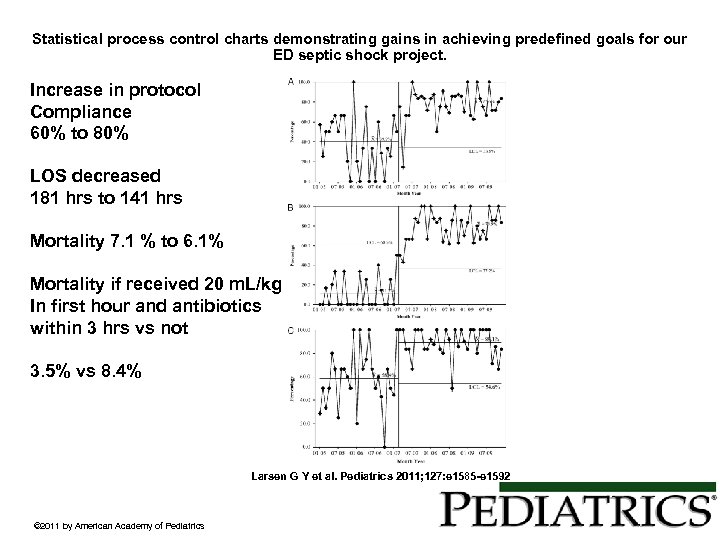 Statistical process control charts demonstrating gains in achieving predefined goals for our ED septic shock project. Increase in protocol Compliance 60% to 80% LOS decreased 181 hrs to 141 hrs Mortality 7. 1 % to 6. 1% Mortality if received 20 m. L/kg In first hour and antibiotics within 3 hrs vs not 3. 5% vs 8. 4% Larsen G Y et al. Pediatrics 2011; 127: e 1585 -e 1592 © 2011 by American Academy of Pediatrics
Statistical process control charts demonstrating gains in achieving predefined goals for our ED septic shock project. Increase in protocol Compliance 60% to 80% LOS decreased 181 hrs to 141 hrs Mortality 7. 1 % to 6. 1% Mortality if received 20 m. L/kg In first hour and antibiotics within 3 hrs vs not 3. 5% vs 8. 4% Larsen G Y et al. Pediatrics 2011; 127: e 1585 -e 1592 © 2011 by American Academy of Pediatrics
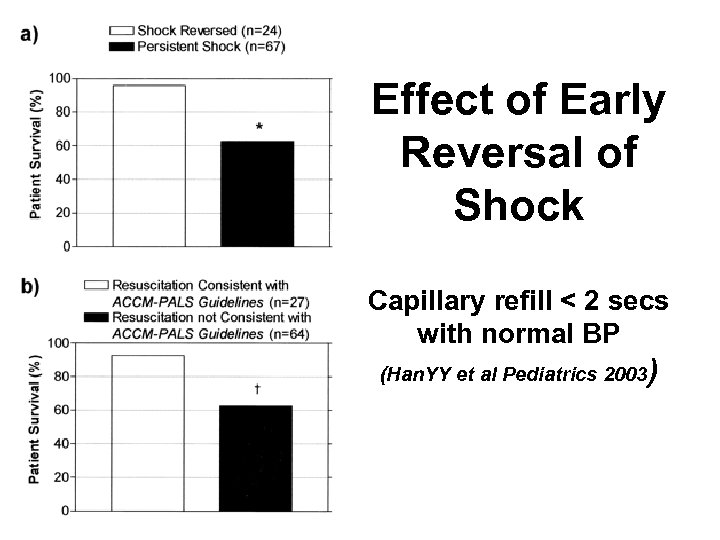 Effect of Early Reversal of Shock Capillary refill < 2 secs with normal BP (Han. YY et al Pediatrics 2003 )
Effect of Early Reversal of Shock Capillary refill < 2 secs with normal BP (Han. YY et al Pediatrics 2003 )
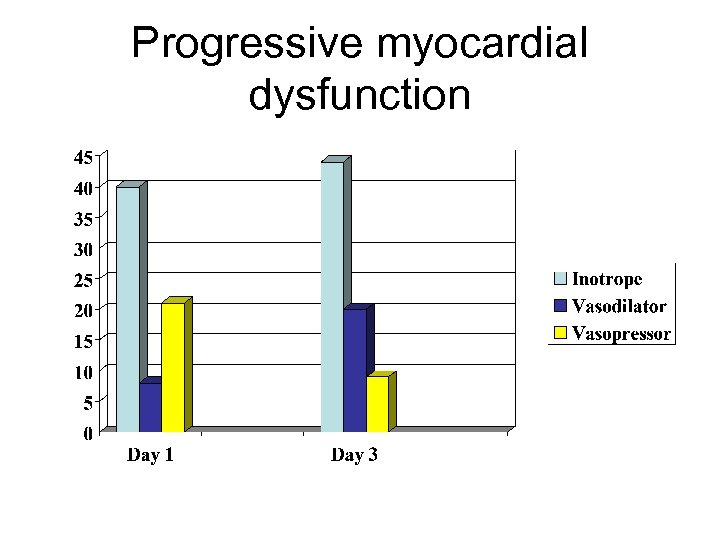 Progressive myocardial dysfunction
Progressive myocardial dysfunction
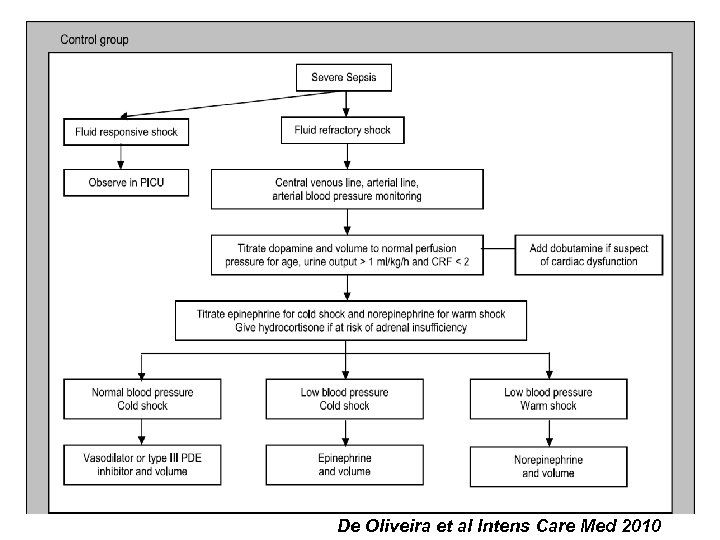 De Oliveira et al Intens Care Med 2010
De Oliveira et al Intens Care Med 2010
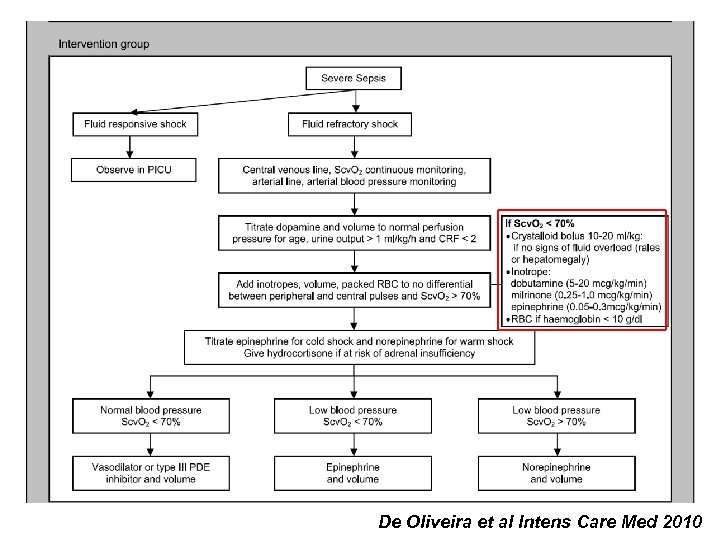 De Oliveira et al Intens Care Med 2010
De Oliveira et al Intens Care Med 2010
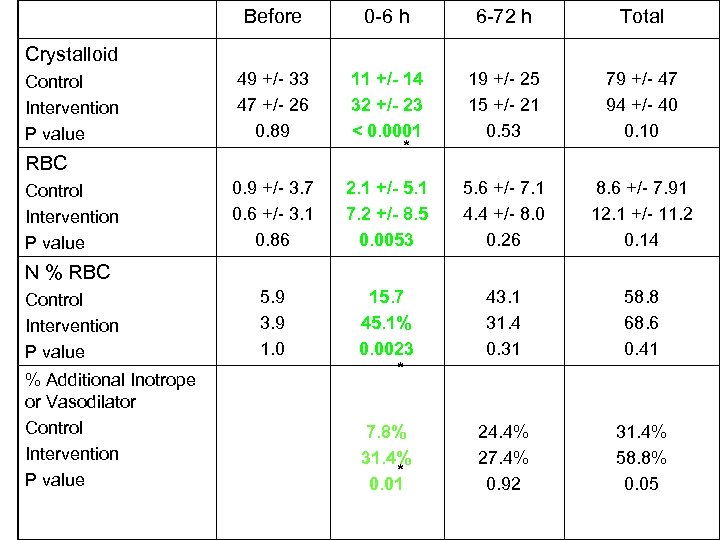 Before 0 -6 h 6 -72 h Total 49 +/- 33 47 +/- 26 0. 89 11 +/- 14 32 +/- 23 < 0. 0001 * 19 +/- 25 15 +/- 21 0. 53 79 +/- 47 94 +/- 40 0. 10 0. 9 +/- 3. 7 0. 6 +/- 3. 1 0. 86 2. 1 +/- 5. 1 7. 2 +/- 8. 5 0. 0053 5. 6 +/- 7. 1 4. 4 +/- 8. 0 0. 26 8. 6 +/- 7. 91 12. 1 +/- 11. 2 0. 14 5. 9 3. 9 1. 0 15. 7 45. 1% 0. 0023 * 43. 1 31. 4 0. 31 58. 8 68. 6 0. 41 7. 8% 31. 4% * 0. 01 24. 4% 27. 4% 0. 92 31. 4% 58. 8% 0. 05 Crystalloid Control Intervention P value RBC Control Intervention P value N % RBC Control Intervention P value % Additional Inotrope or Vasodilator Control Intervention P value
Before 0 -6 h 6 -72 h Total 49 +/- 33 47 +/- 26 0. 89 11 +/- 14 32 +/- 23 < 0. 0001 * 19 +/- 25 15 +/- 21 0. 53 79 +/- 47 94 +/- 40 0. 10 0. 9 +/- 3. 7 0. 6 +/- 3. 1 0. 86 2. 1 +/- 5. 1 7. 2 +/- 8. 5 0. 0053 5. 6 +/- 7. 1 4. 4 +/- 8. 0 0. 26 8. 6 +/- 7. 91 12. 1 +/- 11. 2 0. 14 5. 9 3. 9 1. 0 15. 7 45. 1% 0. 0023 * 43. 1 31. 4 0. 31 58. 8 68. 6 0. 41 7. 8% 31. 4% * 0. 01 24. 4% 27. 4% 0. 92 31. 4% 58. 8% 0. 05 Crystalloid Control Intervention P value RBC Control Intervention P value N % RBC Control Intervention P value % Additional Inotrope or Vasodilator Control Intervention P value
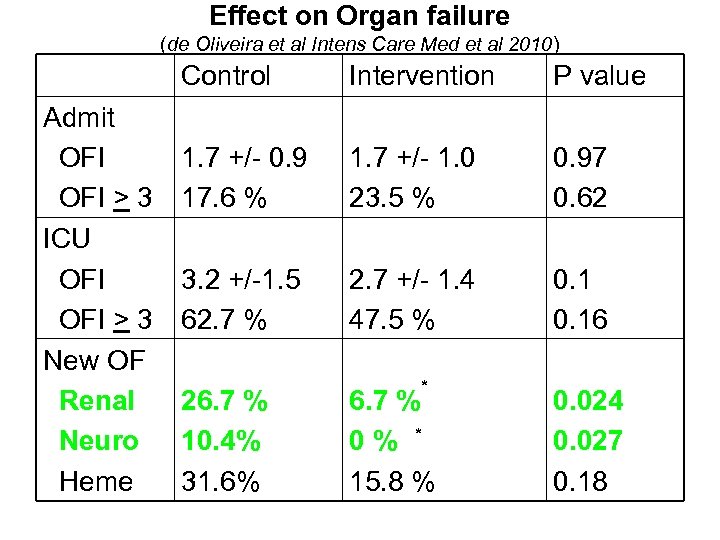 Effect on Organ failure (de Oliveira et al Intens Care Med et al 2010) Control Admit OFI > 3 ICU OFI > 3 New OF Renal Neuro Heme Intervention P value 1. 7 +/- 0. 9 17. 6 % 1. 7 +/- 1. 0 23. 5 % 0. 97 0. 62 3. 2 +/-1. 5 62. 7 % 2. 7 +/- 1. 4 47. 5 % 0. 16 26. 7 % 10. 4% 31. 6% * 6. 7 % 0 % * 15. 8 % 0. 024 0. 027 0. 18
Effect on Organ failure (de Oliveira et al Intens Care Med et al 2010) Control Admit OFI > 3 ICU OFI > 3 New OF Renal Neuro Heme Intervention P value 1. 7 +/- 0. 9 17. 6 % 1. 7 +/- 1. 0 23. 5 % 0. 97 0. 62 3. 2 +/-1. 5 62. 7 % 2. 7 +/- 1. 4 47. 5 % 0. 16 26. 7 % 10. 4% 31. 6% * 6. 7 % 0 % * 15. 8 % 0. 024 0. 027 0. 18
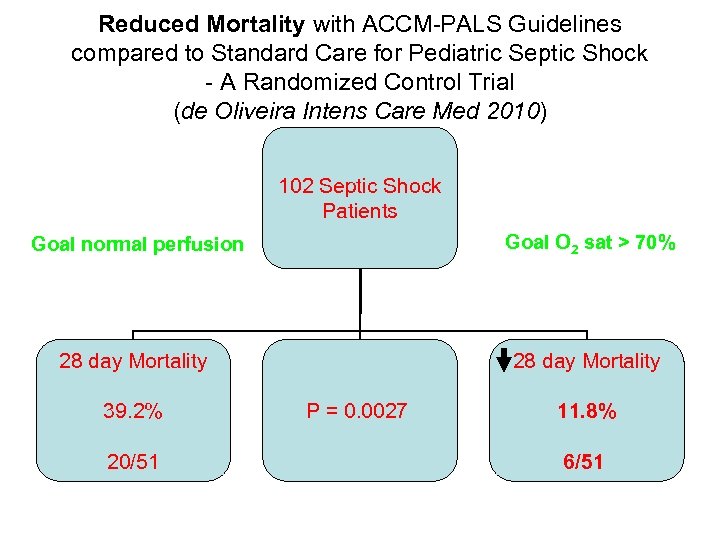 Reduced Mortality with ACCM-PALS Guidelines compared to Standard Care for Pediatric Septic Shock - A Randomized Control Trial (de Oliveira Intens Care Med 2010) 102 Septic Shock Patients Goal O 2 sat > 70% Goal normal perfusion 28 day Mortality 39. 2% 20/51 28 day Mortality P = 0. 0027 11. 8% 6/51
Reduced Mortality with ACCM-PALS Guidelines compared to Standard Care for Pediatric Septic Shock - A Randomized Control Trial (de Oliveira Intens Care Med 2010) 102 Septic Shock Patients Goal O 2 sat > 70% Goal normal perfusion 28 day Mortality 39. 2% 20/51 28 day Mortality P = 0. 0027 11. 8% 6/51
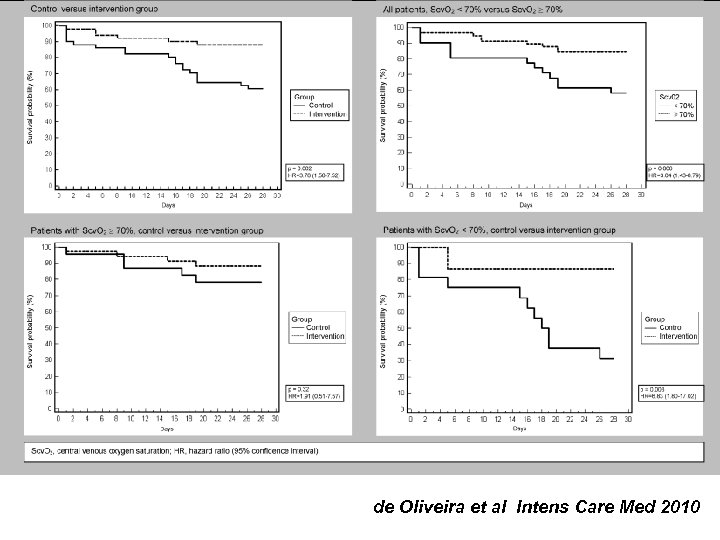 Fig. 3 Kaplan–Meier estimates of mortality (28 days) de Oliveira et al Intens Care Med 2010
Fig. 3 Kaplan–Meier estimates of mortality (28 days) de Oliveira et al Intens Care Med 2010
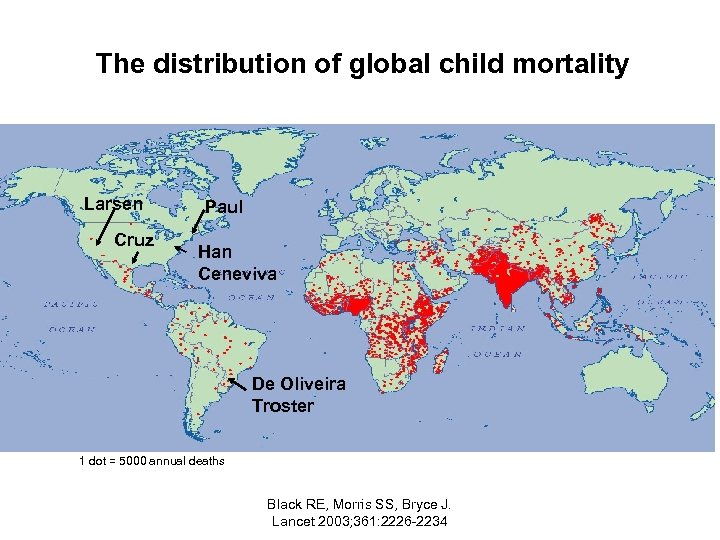 The distribution of global child mortality Larsen Cruz Paul Han Ceneviva De Oliveira Troster 1 dot = 5000 annual deaths Black RE, Morris SS, Bryce J. Lancet 2003; 361: 2226 -2234
The distribution of global child mortality Larsen Cruz Paul Han Ceneviva De Oliveira Troster 1 dot = 5000 annual deaths Black RE, Morris SS, Bryce J. Lancet 2003; 361: 2226 -2234
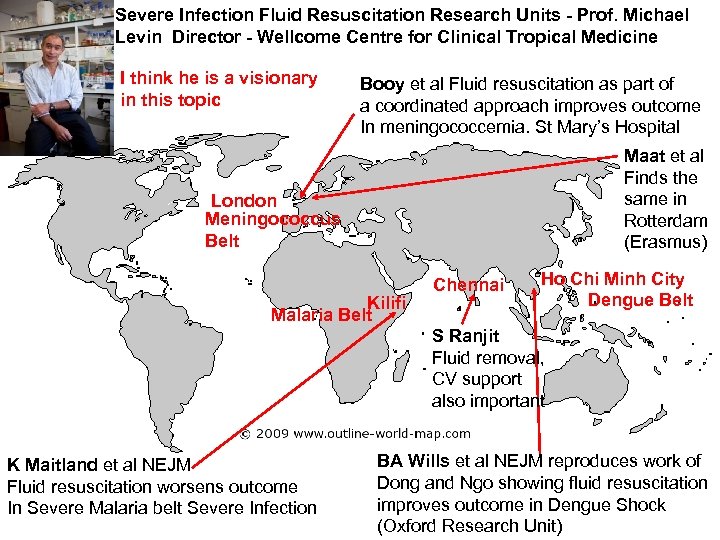 Severe Infection Fluid Resuscitation Research Units - Prof. Michael Levin Director - Wellcome Centre for Clinical Tropical Medicine I think he is a visionary in this topic Booy et al Fluid resuscitation as part of a coordinated approach improves outcome In meningococcemia. St Mary’s Hospital Maat et al Finds the same in Rotterdam (Erasmus) London Meningococcus Belt Kilifi Malaria Belt Chennai Ho Chi Minh City Dengue Belt S Ranjit Fluid removal, CV support also important K Maitland et al NEJM Fluid resuscitation worsens outcome In Severe Malaria belt Severe Infection BA Wills et al NEJM reproduces work of Dong and Ngo showing fluid resuscitation improves outcome in Dengue Shock (Oxford Research Unit)
Severe Infection Fluid Resuscitation Research Units - Prof. Michael Levin Director - Wellcome Centre for Clinical Tropical Medicine I think he is a visionary in this topic Booy et al Fluid resuscitation as part of a coordinated approach improves outcome In meningococcemia. St Mary’s Hospital Maat et al Finds the same in Rotterdam (Erasmus) London Meningococcus Belt Kilifi Malaria Belt Chennai Ho Chi Minh City Dengue Belt S Ranjit Fluid removal, CV support also important K Maitland et al NEJM Fluid resuscitation worsens outcome In Severe Malaria belt Severe Infection BA Wills et al NEJM reproduces work of Dong and Ngo showing fluid resuscitation improves outcome in Dengue Shock (Oxford Research Unit)
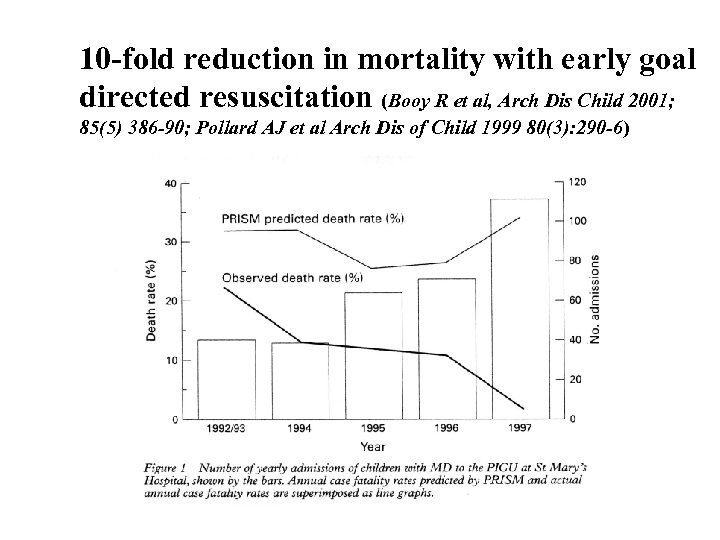 10 -fold reduction in mortality with early goal directed resuscitation (Booy R et al, Arch Dis Child 2001; 85(5) 386 -90; Pollard AJ et al Arch Dis of Child 1999 80(3): 290 -6)
10 -fold reduction in mortality with early goal directed resuscitation (Booy R et al, Arch Dis Child 2001; 85(5) 386 -90; Pollard AJ et al Arch Dis of Child 1999 80(3): 290 -6)
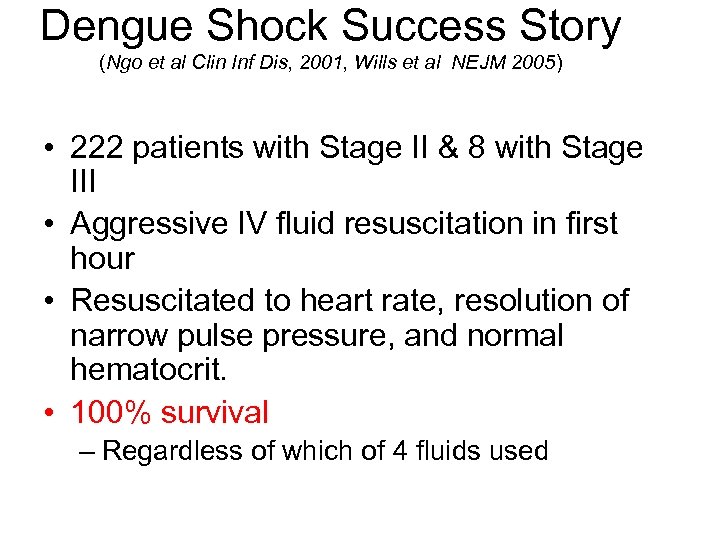 Dengue Shock Success Story (Ngo et al Clin Inf Dis, 2001, Wills et al NEJM 2005) • 222 patients with Stage II & 8 with Stage III • Aggressive IV fluid resuscitation in first hour • Resuscitated to heart rate, resolution of narrow pulse pressure, and normal hematocrit. • 100% survival – Regardless of which of 4 fluids used
Dengue Shock Success Story (Ngo et al Clin Inf Dis, 2001, Wills et al NEJM 2005) • 222 patients with Stage II & 8 with Stage III • Aggressive IV fluid resuscitation in first hour • Resuscitated to heart rate, resolution of narrow pulse pressure, and normal hematocrit. • 100% survival – Regardless of which of 4 fluids used
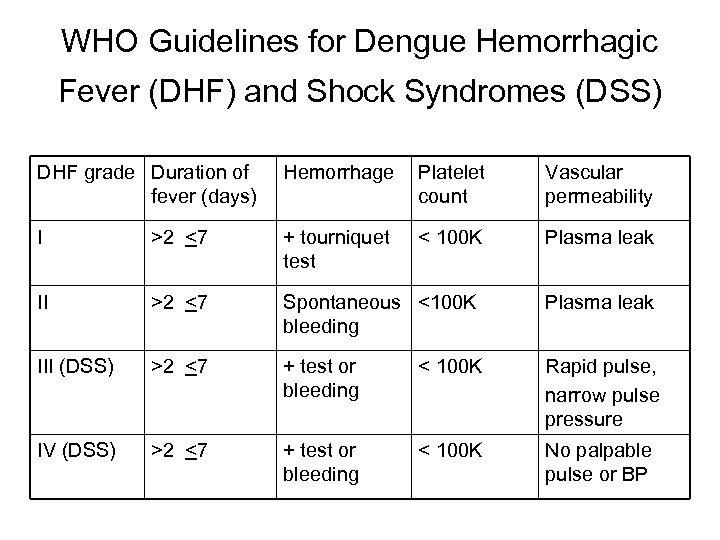 WHO Guidelines for Dengue Hemorrhagic Fever (DHF) and Shock Syndromes (DSS) DHF grade Duration of fever (days) Hemorrhage Platelet count Vascular permeability I >2 <7 + tourniquet test < 100 K Plasma leak II >2 <7 Spontaneous <100 K bleeding Plasma leak III (DSS) >2 <7 + test or bleeding < 100 K Rapid pulse, narrow pulse pressure IV (DSS) >2 <7 + test or bleeding < 100 K No palpable pulse or BP
WHO Guidelines for Dengue Hemorrhagic Fever (DHF) and Shock Syndromes (DSS) DHF grade Duration of fever (days) Hemorrhage Platelet count Vascular permeability I >2 <7 + tourniquet test < 100 K Plasma leak II >2 <7 Spontaneous <100 K bleeding Plasma leak III (DSS) >2 <7 + test or bleeding < 100 K Rapid pulse, narrow pulse pressure IV (DSS) >2 <7 + test or bleeding < 100 K No palpable pulse or BP
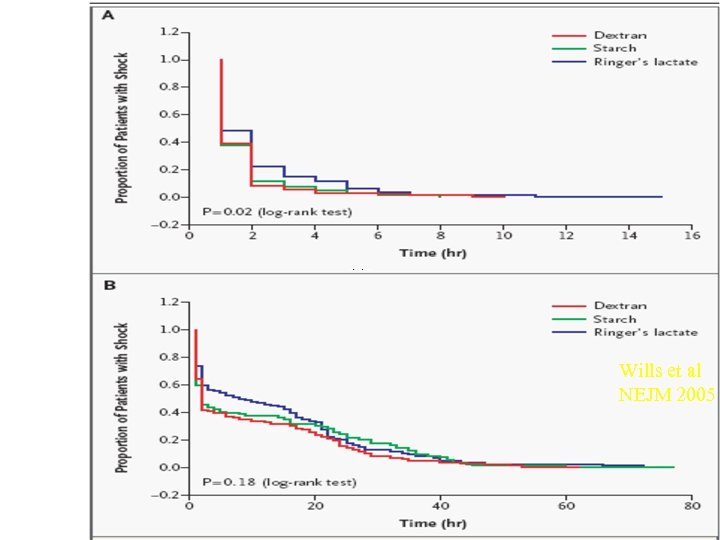 Wills et al NEJM 2005
Wills et al NEJM 2005
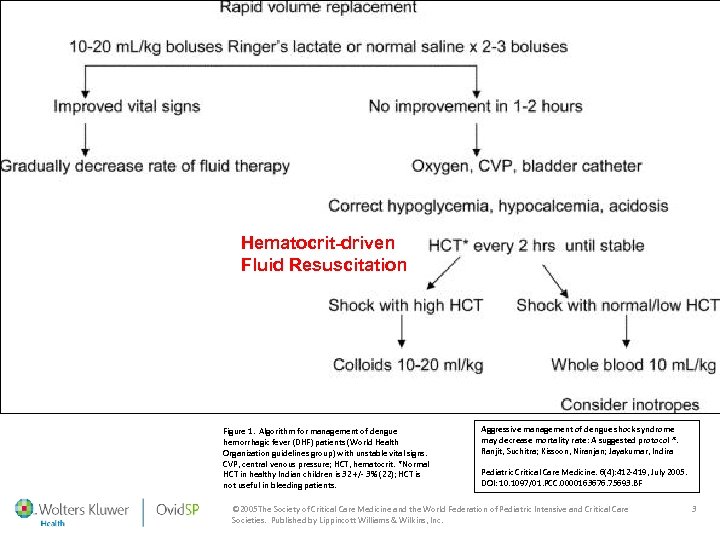 Hematocrit-driven Fluid Resuscitation Figure 1. Algorithm for management of dengue hemorrhagic fever (DHF) patients (World Health Organization guidelines group) with unstable vital signs. CVP, central venous pressure; HCT, hematocrit. *Normal HCT in healthy Indian children is 32 +/- 3% (22); HCT is not useful in bleeding patients. Aggressive management of dengue shock syndrome may decrease mortality rate: A suggested protocol *. Ranjit, Suchitra; Kissoon, Niranjan; Jayakumar, Indira Pediatric Critical Care Medicine. 6(4): 412 -419, July 2005. DOI: 10. 1097/01. PCC. 0000163676. 75693. BF © 2005 The Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies. Published by Lippincott Williams & Wilkins, Inc. 3
Hematocrit-driven Fluid Resuscitation Figure 1. Algorithm for management of dengue hemorrhagic fever (DHF) patients (World Health Organization guidelines group) with unstable vital signs. CVP, central venous pressure; HCT, hematocrit. *Normal HCT in healthy Indian children is 32 +/- 3% (22); HCT is not useful in bleeding patients. Aggressive management of dengue shock syndrome may decrease mortality rate: A suggested protocol *. Ranjit, Suchitra; Kissoon, Niranjan; Jayakumar, Indira Pediatric Critical Care Medicine. 6(4): 412 -419, July 2005. DOI: 10. 1097/01. PCC. 0000163676. 75693. BF © 2005 The Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies. Published by Lippincott Williams & Wilkins, Inc. 3
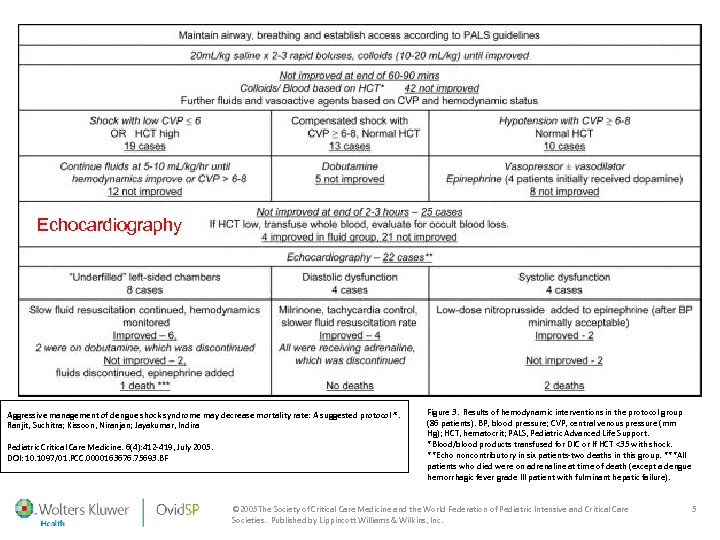 Echocardiography Aggressive management of dengue shock syndrome may decrease mortality rate: A suggested protocol *. Ranjit, Suchitra; Kissoon, Niranjan; Jayakumar, Indira Pediatric Critical Care Medicine. 6(4): 412 -419, July 2005. DOI: 10. 1097/01. PCC. 0000163676. 75693. BF Figure 3. Results of hemodynamic interventions in the protocol group (86 patients). BP, blood pressure; CVP, central venous pressure (mm Hg); HCT, hematocrit; PALS, Pediatric Advanced Life Support. *Blood/blood products transfused for DIC or If HCT <35 with shock. **Echo noncontributory in six patients-two deaths in this group. ***All patients who died were on adrenaline at time of death (except a dengue hemorrhagic fever grade III patient with fulminant hepatic failure). © 2005 The Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies. Published by Lippincott Williams & Wilkins, Inc. 5
Echocardiography Aggressive management of dengue shock syndrome may decrease mortality rate: A suggested protocol *. Ranjit, Suchitra; Kissoon, Niranjan; Jayakumar, Indira Pediatric Critical Care Medicine. 6(4): 412 -419, July 2005. DOI: 10. 1097/01. PCC. 0000163676. 75693. BF Figure 3. Results of hemodynamic interventions in the protocol group (86 patients). BP, blood pressure; CVP, central venous pressure (mm Hg); HCT, hematocrit; PALS, Pediatric Advanced Life Support. *Blood/blood products transfused for DIC or If HCT <35 with shock. **Echo noncontributory in six patients-two deaths in this group. ***All patients who died were on adrenaline at time of death (except a dengue hemorrhagic fever grade III patient with fulminant hepatic failure). © 2005 The Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies. Published by Lippincott Williams & Wilkins, Inc. 5
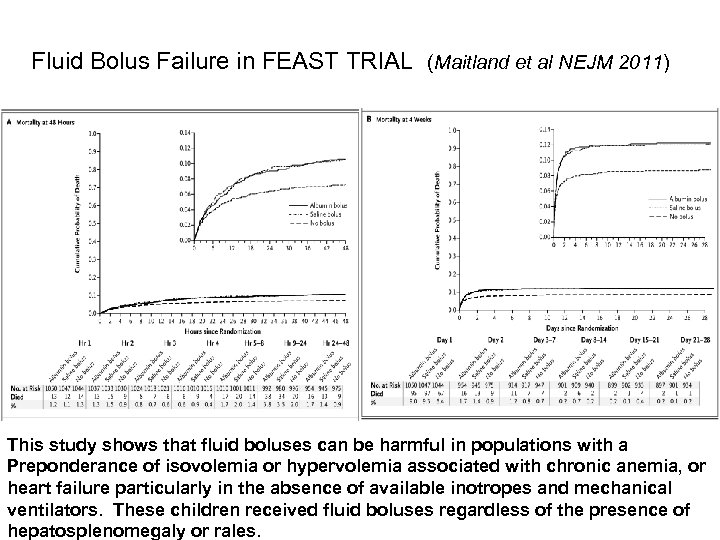 Fluid Bolus Failure in FEAST TRIAL (Maitland et al NEJM 2011) This study shows that fluid boluses can be harmful in populations with a Preponderance of isovolemia or hypervolemia associated with chronic anemia, or heart failure particularly in the absence of available inotropes and mechanical ventilators. These children received fluid boluses regardless of the presence of hepatosplenomegaly or rales.
Fluid Bolus Failure in FEAST TRIAL (Maitland et al NEJM 2011) This study shows that fluid boluses can be harmful in populations with a Preponderance of isovolemia or hypervolemia associated with chronic anemia, or heart failure particularly in the absence of available inotropes and mechanical ventilators. These children received fluid boluses regardless of the presence of hepatosplenomegaly or rales.
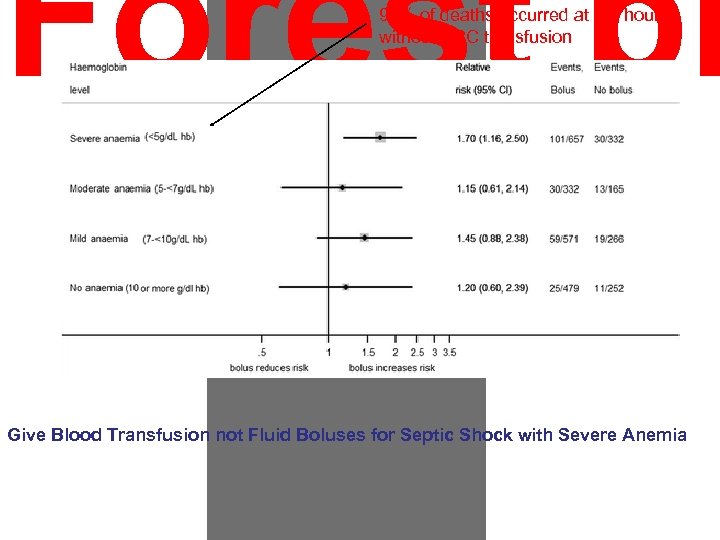 Forest pl 90% of deaths occurred at 2. 5 hours without RBC transfusion Give Blood Transfusion not Fluid Boluses for Septic Shock with Severe Anemia
Forest pl 90% of deaths occurred at 2. 5 hours without RBC transfusion Give Blood Transfusion not Fluid Boluses for Septic Shock with Severe Anemia
 Hematocrit = 34 Mortality 2% With Fluid Bolus Appropriate timely Abx Inotropes Previously Healthy Hematocrit = 50 Mortality 0% With Fluid Boluses Previously Healthy Chronic High Output Anemia Hematocrit = 18 Mortality 7% with Blood Maintenance IVF Antimalarials
Hematocrit = 34 Mortality 2% With Fluid Bolus Appropriate timely Abx Inotropes Previously Healthy Hematocrit = 50 Mortality 0% With Fluid Boluses Previously Healthy Chronic High Output Anemia Hematocrit = 18 Mortality 7% with Blood Maintenance IVF Antimalarials
 And so I remain decidedly PRO - Fluid resuscitation for pediatric septic shock duly noting the following caveats framed below by famed Professors (Guess who was not my teacher) The First Law of Sociology - Some Do The Second Law of Sociology - Some Don’t Professor Vernon K Dibble Wesleyan University Sociology Seminar 1973 To know Syphilis is to know Medicine Sir William Osler (He was not my teacher) To know Sepsis is to know Critical Care Medicine Professor Jerry Zimmerman Thank You for listening
And so I remain decidedly PRO - Fluid resuscitation for pediatric septic shock duly noting the following caveats framed below by famed Professors (Guess who was not my teacher) The First Law of Sociology - Some Do The Second Law of Sociology - Some Don’t Professor Vernon K Dibble Wesleyan University Sociology Seminar 1973 To know Syphilis is to know Medicine Sir William Osler (He was not my teacher) To know Sepsis is to know Critical Care Medicine Professor Jerry Zimmerman Thank You for listening


