d2d5aa27994557096025e16bfbede97a.ppt
- Количество слайдов: 90
Patient Safety in Primary Care Capacity Building Event
“Design and implement a Patient Safety Programme in Primary Care” Roll out March 2013 Start with GP Practices, Community Nurses and Pharmacy Extend to rest of primary care….
Patient Safety in Primary Care Programme - 3 Workstreams • Safer Medicines • Safe and reliable patient care across the interface and at home • Safety Culture and Leadership • • Not all at once Menu Build over time Organic spread
Current Activity SIPC Spread • • Dumfries and Galloway • Ayrshire and Arran • Lanarkshire Borders Lothian Tayside Grampian Highland Forth Valley Greater Glasgow &C
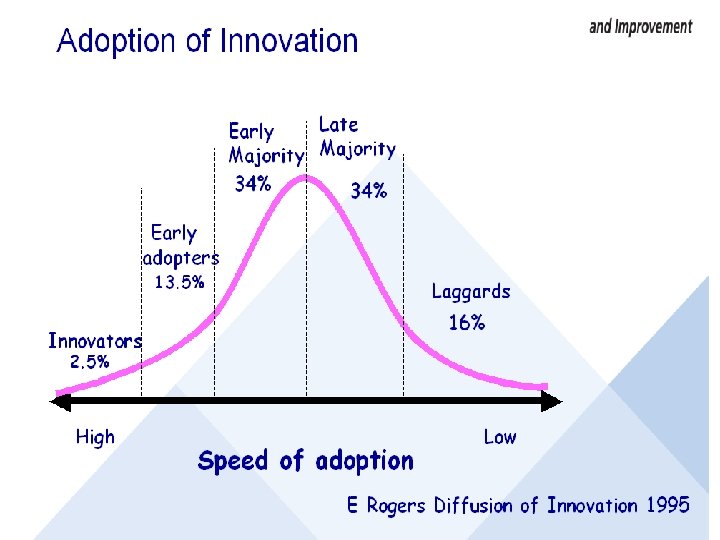
Innovation Adoption Curve .

Build Will • • “Houston we have a problem” Correct Areas of focus Safer care Confidence in systems – less waste Less things going wrong Less stress Improved interface working
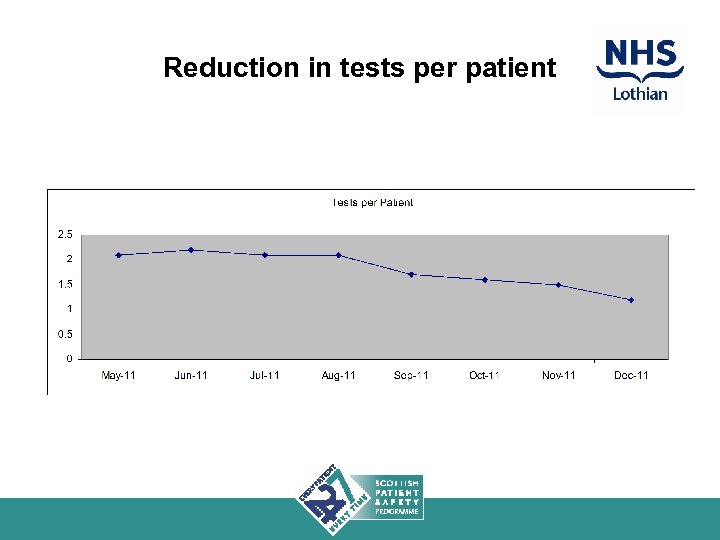
Reduction in tests per patient
Successful implementation needs. . • Build on the professionalism of front line staff • Prioritised within existing and adapted GMS contract • Alignment with GP Appraisal and Revalidation • Commitment of boards

Which way is your board looking…
Board Levers • • Measurable high quality care Reduce Admissions e. g 6% of admissions Link to SPSP: Med Rec – Warfarin – Pressure ulcers Less adverse events - harm- complaints Interface working Reducing Falls/ UTIs/Pressure ulcers

Boards need… • Executive buy in and championing • Prioritise this programme • Dedicated clinical leadership and QI support • Pharmacy support • Build knowledge and skills • Engagement with practices - PLT?

• Re focus • Re energise
Support Available • • Capacity Building Tools Experience Resources - education / interventions to build will • IT • Measurement • Productive General Practice
Going back to your board…. . • How aware is your Board of the safety programme for Primary Care? • Current knowledge /skills/ infrastructure/experience to support the programme? • What do you now need to do in your Board to prepare for it? • What support do you need?

Patient Safety in Primary Care Capacity Building Event
Using data to improve the reliability of care Bruce Guthrie Professor of Primary Care Medicine, University of Dundee GP NHS Fife With thanks to everyone in the Safety Improvement in Primary Care Programme (SIPC), and The Health Foundation for funding SIPC
Outline • Getting started with data • High-volume processes and sampling – What are we trying to improve? – How do you measure a nightmare? • Reliability and bundles – Examples from other contexts – Examples from SIPC • What to do in real life?
Getting started with data • “Education, education” Tony Blair 1997 • “It’s the economy, stupid” Bill Clinton 1991 • No politician has yet said: – “Data, data” – “It’s the data, stupid”
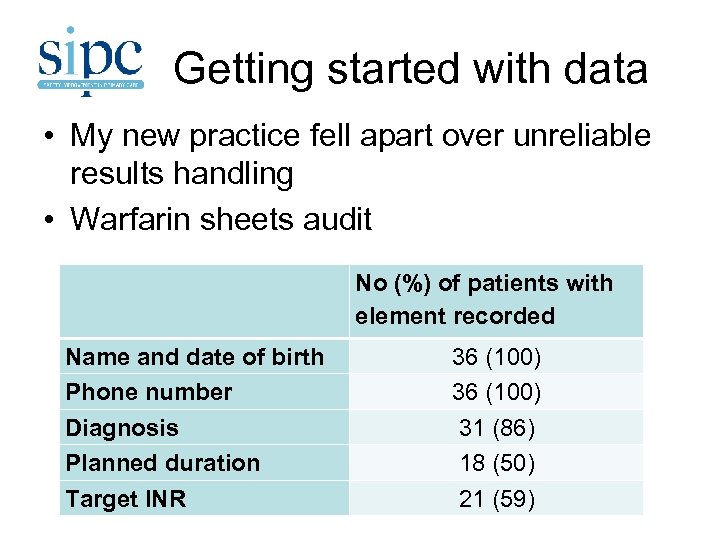
Getting started with data • My new practice fell apart over unreliable results handling • Warfarin sheets audit Name and date of birth Phone number Diagnosis Planned duration Target INR No (%) of patients with element recorded 36 (100) 31 (86) 18 (50) 21 (59)
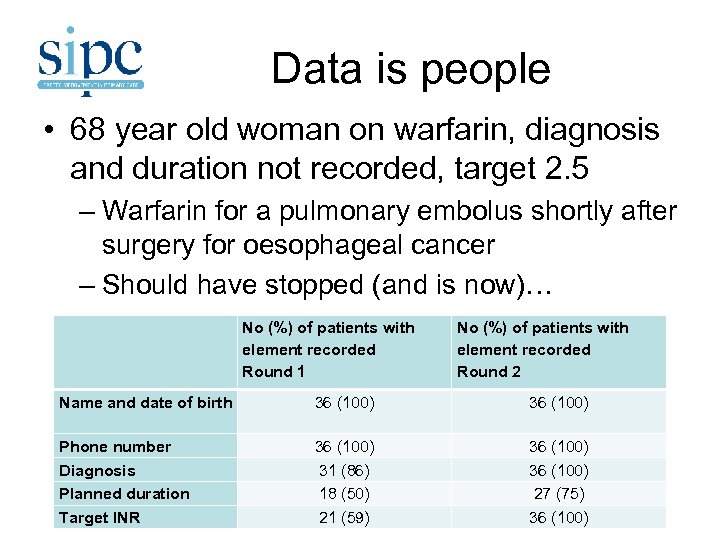
Data is people • 68 year old woman on warfarin, diagnosis and duration not recorded, target 2. 5 – Warfarin for a pulmonary embolus shortly after surgery for oesophageal cancer – Should have stopped (and is now)… No (%) of patients with element recorded Round 1 No (%) of patients with element recorded Round 2 Name and date of birth 36 (100) Phone number Diagnosis Planned duration Target INR 36 (100) 31 (86) 18 (50) 21 (59) 36 (100) 27 (75) 36 (100)
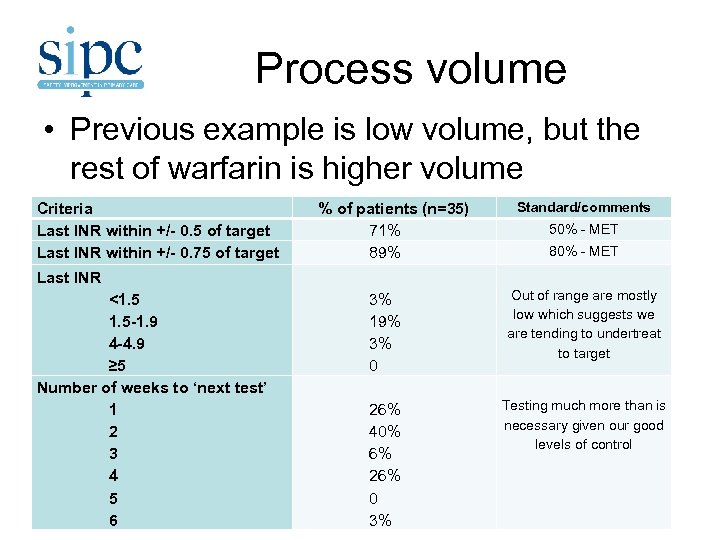
Process volume • Previous example is low volume, but the rest of warfarin is higher volume Criteria Last INR within +/- 0. 5 of target Last INR within +/- 0. 75 of target Last INR <1. 5 -1. 9 4 -4. 9 ≥ 5 Number of weeks to ‘next test’ 1 2 3 4 5 6 % of patients (n=35) 71% 89% 3% 19% 3% 0 26% 40% 6% 26% 0 3% Standard/comments 50% - MET 80% - MET Out of range are mostly low which suggests we are tending to undertreat to target Testing much more than is necessary given our good levels of control
Process volume • SIPC 1 projects vary in volume – Warfarin process is high volume – DMARDs and heart failure low volume • SIPC 2 projects are all high volume – Medicines reconciliation at discharge – Outpatient letters – Results handling • Exciting and innovative improvement work – “Solving some of the most important problems of healthcare” (Health Foundation) • Boring, boring work…
Safety systems • Learning from other industries • Error doesn’t usually cause harm. . . • . . . so should act on error and risk not harm
Safety systems • “It appears to me that there were significant flaws in the quality of Occidental’s management of safety which “Relying on the absence of any affected the circumstances of the events of the disaster. Senior management were too feedback of problems as easily satisfied that the Permit to Work indicating that all was well” system was being operated correctly, relying on the absence of any feedback of problems as indicating that all was well. ” (Lord Cullen)
Data is people • Letter comes in, a 64 year old woman just diagnosed with terminal lung cancer in 2010 – “In retrospect, the lesion is visible on a previous CXR” • Central Vision CXR report from 2005 – “Chest shows a well rounded opacity on the left side of the chest which is strongly suspicious of bronchial lesion. Referral to the chest physicians for further investigation is clearly appropriate. ” • A heartsink moment… • …but not our fault • What would stop it happening to us?
Data is people • Home visit to a man with tenesmus in 2004 • Recently referred to colorectal with ? cancer (appointment tomorrow) • Had been seen with loose bowels 15 months ago – Short history, normal examination inc PR, “do some tests, come back if abnormal/persistent” – FBC and stool culture normal, FOB positive • Clinical care fine, results book failure
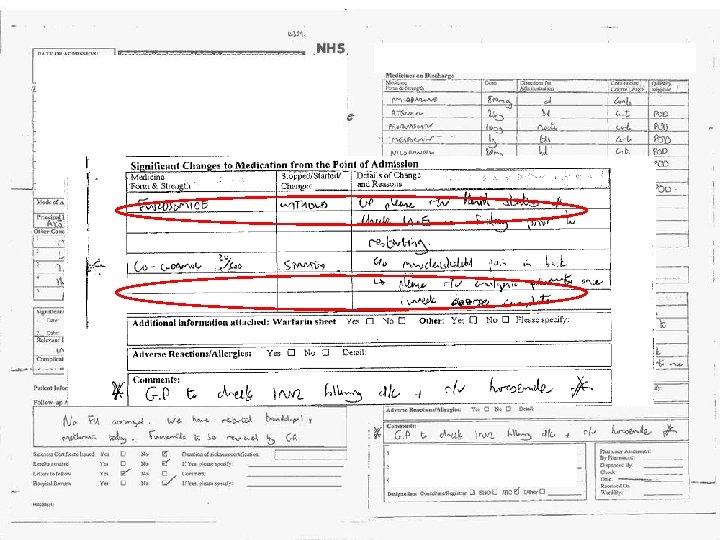
Data is people
Safety systems • Remember Lord Cullen’s criticism of Occidental management? – “Relying on the absence of any feedback of problems as indicating that all was well” • ‘Usual’ feedback isn’t reliable • Collecting data and measuring can be • Health care is more dangerous to patients than the oil industry is to employees – But we harm people one at a time
Process volume • SIPC topics – High risk medicines - warfarin, DMARDs – High risk conditions – heart failure – Medicines reconciliation at discharge – Outpatient letters – Results handling • Boring, boring work… • …but getting the paperwork wrong can kill people
How to measure? • Remember our warfarin audits? – Data is all in the warfarin book – Only 36 patients – All the measures were easily countable • Can’t always count everything every time – Volume may be too high, but high volume is an opportunity to sample – Take 5 or 10 results and check if actions done – Take 5 or 10 DC summaries or letters and check medications reconciled/actions done
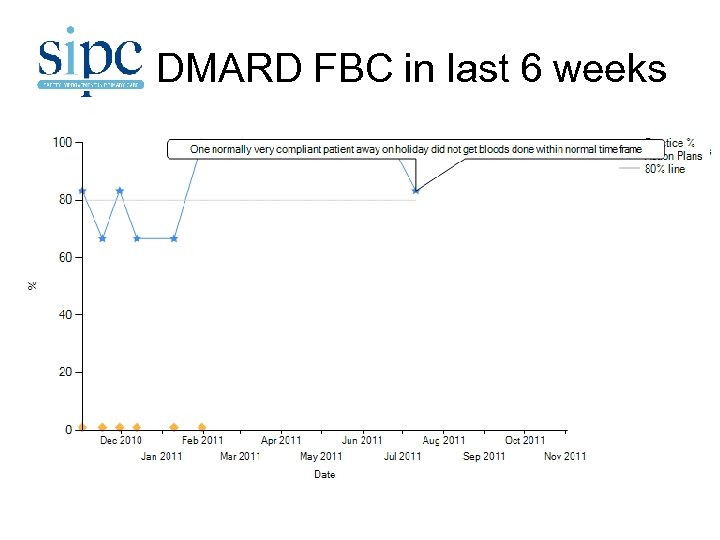
DMARD FBC in last 6 weeks
How to measure • There’s no right answer to: – How many to measure each time – Complete audit vs small sample – How often to sample – Depends on the context • Have to decide what to measure first…
Measures and bundles • Quality measures are hard to define well • Traditionally have usually been stand alone – % of patients with HT with controlled BP – % of patients on warfarin with INR in range – % of patients over 75 receiving a flu jag • Increasingly measures are ‘bundled’ in various ways – AKA composite measures
All or nothing measures • ‘Care bundles’ are all or nothing measures – The % of patients who achieve ALL individual measures/get all appropriate care • Appropriate when: – Each element is important in its own right – Patient outcome is improved by ALL measured care being received (the whole is greater than the sum of the parts) – Each element should be necessary every time
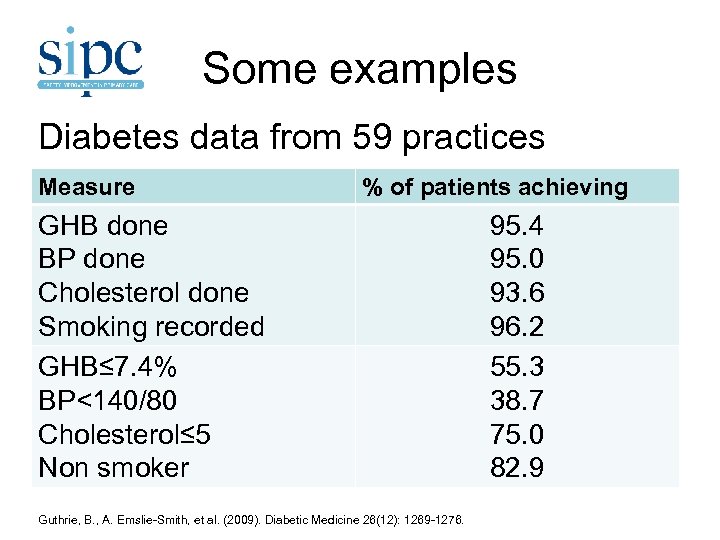
Some examples Diabetes data from 59 practices Measure % of patients achieving GHB done BP done Cholesterol done Smoking recorded GHB≤ 7. 4% BP<140/80 Cholesterol≤ 5 Non smoker Guthrie, B. , A. Emslie-Smith, et al. (2009). Diabetic Medicine 26(12): 1269 -1276. 95. 4 95. 0 93. 6 96. 2 55. 3 38. 7 75. 0 82. 9
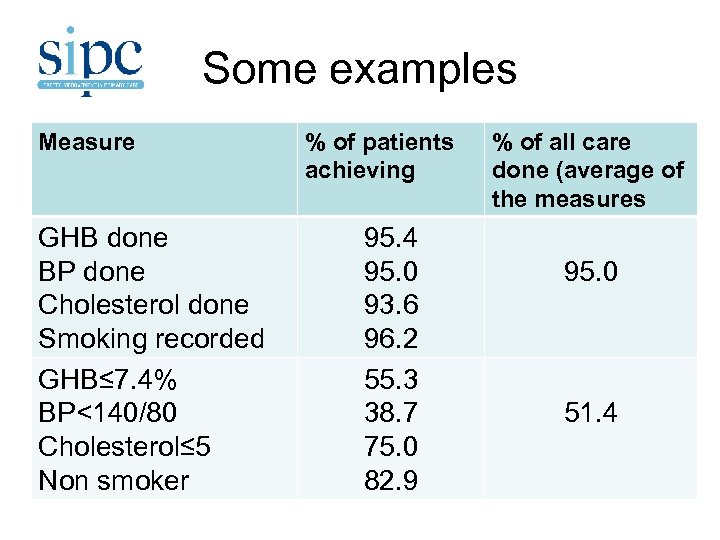
Some examples Measure GHB done BP done Cholesterol done Smoking recorded GHB≤ 7. 4% BP<140/80 Cholesterol≤ 5 Non smoker % of patients achieving 95. 4 95. 0 93. 6 96. 2 55. 3 38. 7 75. 0 82. 9 % of all care done (average of the measures 95. 0 51. 4
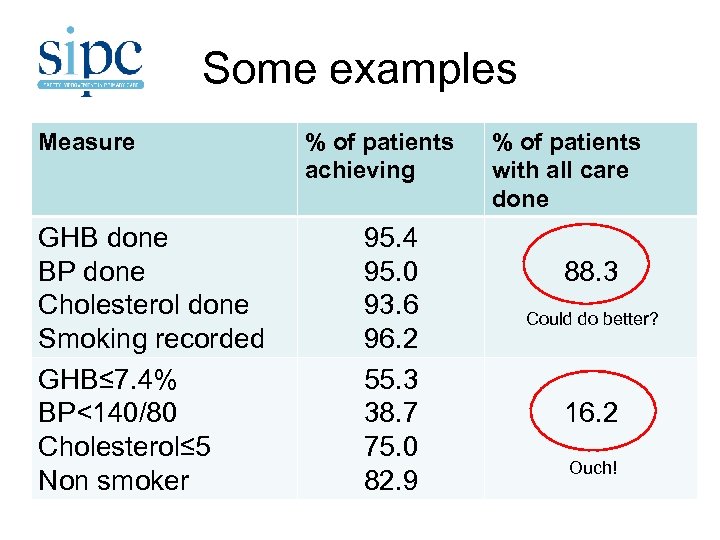
Some examples Measure GHB done BP done Cholesterol done Smoking recorded GHB≤ 7. 4% BP<140/80 Cholesterol≤ 5 Non smoker % of patients achieving 95. 4 95. 0 93. 6 96. 2 55. 3 38. 7 75. 0 82. 9 % of patients with all care done 88. 3 Could do better? 16. 2 Ouch!
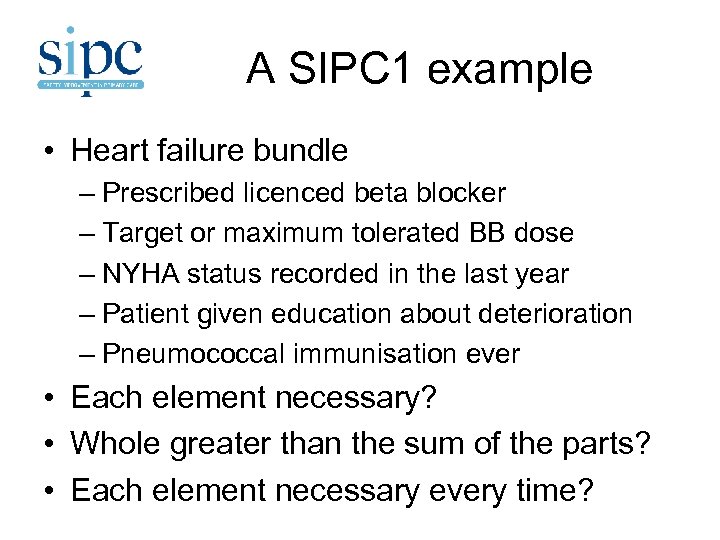
A SIPC 1 example • Heart failure bundle – Prescribed licenced beta blocker – Target or maximum tolerated BB dose – NYHA status recorded in the last year – Patient given education about deterioration – Pneumococcal immunisation ever • Each element necessary? • Whole greater than the sum of the parts? • Each element necessary every time?
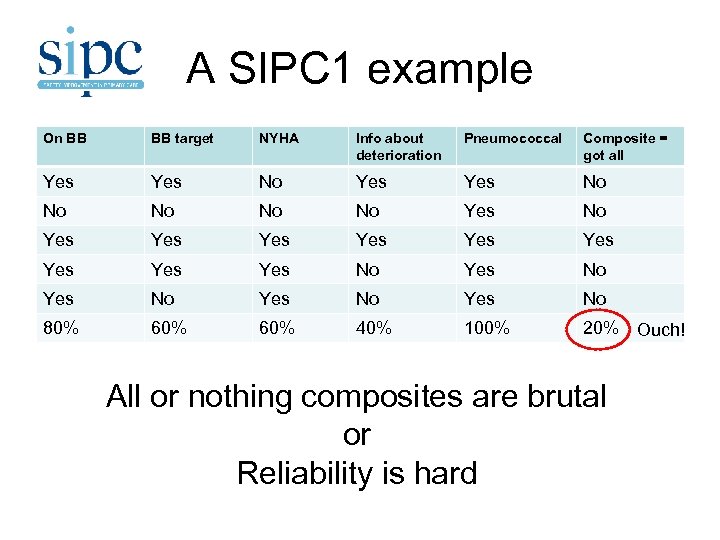
A SIPC 1 example On BB BB target NYHA Info about deterioration Pneumococcal Composite = got all Yes Yes No No No Yes Yes Yes No Yes No 80% 60% 40% 100% 20% Ouch! All or nothing composites are brutal or Reliability is hard
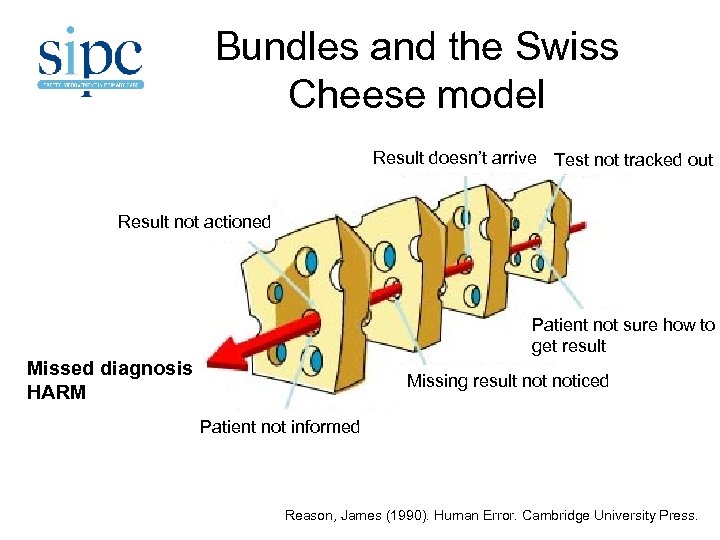
Bundles and the Swiss Cheese model Result doesn’t arrive Test not tracked out Test n Result not actioned ot tracked out Patient not sure how to get result Missed diagnosis Test n HARM Missing result noticed ot tracked out Patient not informed Reason, James (1990). Human Error. Cambridge University Press.
Choosing measures? • What are the individual measures? – For Boards and practices to decide – SIPC has a number of measures at various stages of development; other examples • Single measures or care bundle/all or nothing approaches? – Each element necessary? – Whole greater than the sum of the parts? – Each element necessary every time?
The SIPC approach • Make every measure count – 4 -5 measures in total – Measure what you need not just what you can – Processes plausibly ‘tightly linked’ to outcomes – Whole is plausibly more than the sum of its parts – Room for improvement – Suitable for repeated measurement in PDSAs • Be flexible (change, drop, add) • But there’s more to life than care bundles…
New political slogans? • Data, data (David Cameron 2012) • It is the data, stupid (Barack Obama 2012) – Because data is people – Because boring processes can kill people when they are unreliable – Because we can be better • Good luck!

Patient Safety in Primary Care Capacity Building Event
The Case for Quality Improvement Jane Murkin 12 th March 2012

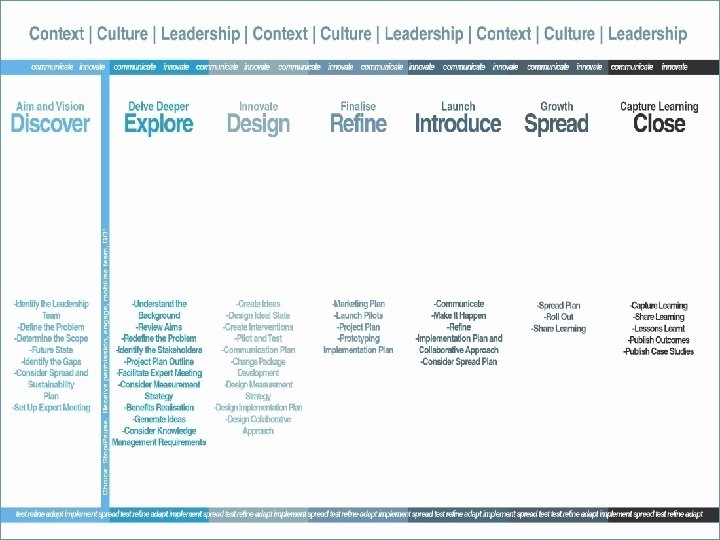
Quality Improvement Hub Session Aims • Context of healthcare today and its relationship with quality improvement • Outlining the improvement approach, journey and measurement plan • Consider the application of improvement science and methodologies in relation to Primary Care Patient Safety Improvement • Learning from others - collaboration – a network and community
Quality Improvement Hub Lets take a moment to…… • Thank you and celebrate your successes • Building on work to date – acknowledge the need to focus on demonstrable measurement for improvement • Quality strategy – safe, effective & person centred care • 20: 20 vision – Sustainable high quality healthcare • Focus – what has been achieved, where are our gaps, priority areas for focus -testing, implementation and improvement • Achieving reliability : Communication, transitions, results handling, medicines reconciliation • Developing your local aims and your first pdsas,
Context
Quality Improvement Hub Care is not safe – Institute of Medicine report “Between the care we have and the care we could have, lies not a gap, but a chasm”
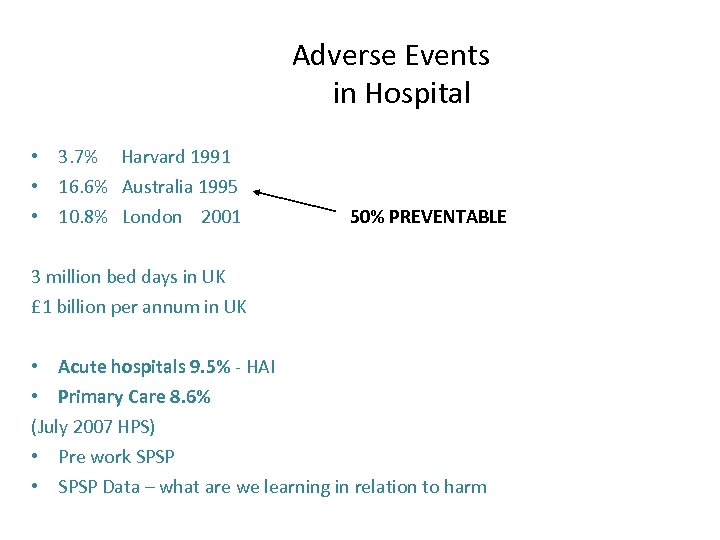
Adverse Events in Hospital • 3. 7% Harvard 1991 • 16. 6% Australia 1995 • 10. 8% London 2001 50% PREVENTABLE 3 million bed days in UK £ 1 billion per annum in UK • Acute hospitals 9. 5% - HAI • Primary Care 8. 6% (July 2007 HPS) • Pre work SPSP • SPSP Data – what are we learning in relation to harm
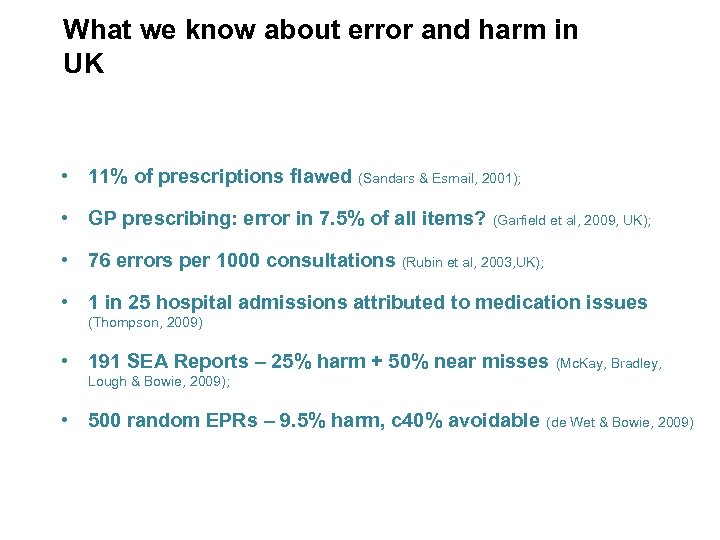
What we know about error and harm in UK • 11% of prescriptions flawed (Sandars & Esmail, 2001); • GP prescribing: error in 7. 5% of all items? (Garfield et al, 2009, UK); • 76 errors per 1000 consultations (Rubin et al, 2003, UK); • 1 in 25 hospital admissions attributed to medication issues (Thompson, 2009) • 191 SEA Reports – 25% harm + 50% near misses (Mc. Kay, Bradley, Lough & Bowie, 2009); • 500 random EPRs – 9. 5% harm, c 40% avoidable (de Wet & Bowie, 2009)
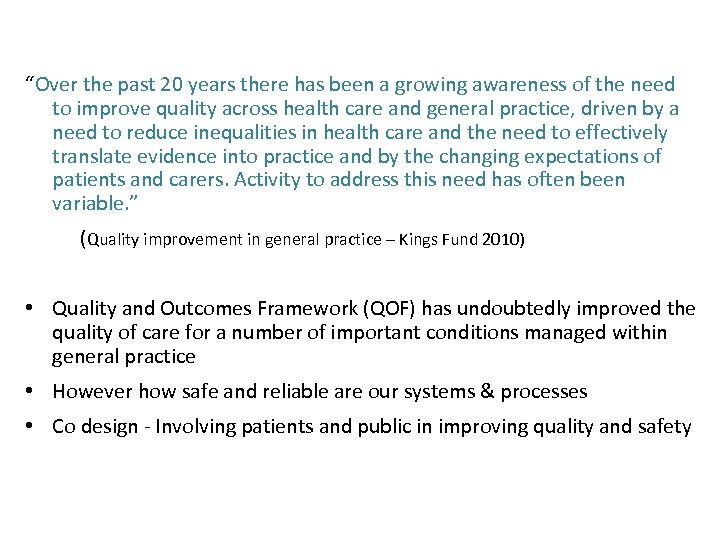
“Over the past 20 years there has been a growing awareness of the need to improve quality across health care and general practice, driven by a need to reduce inequalities in health care and the need to effectively translate evidence into practice and by the changing expectations of patients and carers. Activity to address this need has often been variable. ” (Quality improvement in general practice – Kings Fund 2010) • Quality and Outcomes Framework (QOF) has undoubtedly improved the quality of care for a number of important conditions managed within general practice • However how safe and reliable are our systems & processes • Co design - Involving patients and public in improving quality and safety
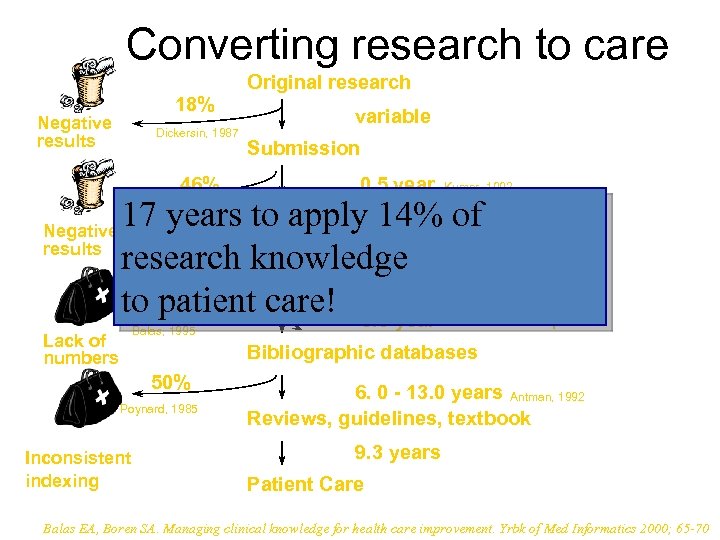
Converting research to care 18% Original research variable Negative Dickersin, 1987 results Submission 46% 0. 5 year Kumar, 1992 17 years Acceptance 14% of to apply Negative 0. 6 year results research Publication knowledge 17: 14 to 35% patient care! 0. 3 year Koren, 1989 Kumar, 1992 Poyer, 1982 Balas, 1995 Lack of numbers Bibliographic databases 50% Poynard, 1985 Inconsistent indexing Expert opinion 6. 0 - 13. 0 years Antman, 1992 Reviews, guidelines, textbook 9. 3 years Patient Care Balas EA, Boren SA. Managing clinical knowledge for health care improvement. Yrbk of Med Informatics 2000; 65 -70
How safe are clinical systems? Primary research into the reliability of systems within 7 NHS organisations and ideas for improvement ( Health Foundation May 2010) Reliability in healthcare – This is not simply a matter of putting in place proper guidelines and expecting practitioners to follow them. It involves identifying in advance the points at which those mistakes can happen, the different elements that contribute to those mistakes and the systems that practitioners should follow in order to ensure pt safety

In aviation 75% of accidents are caused by human factors… …what’s the figure in healthcare?
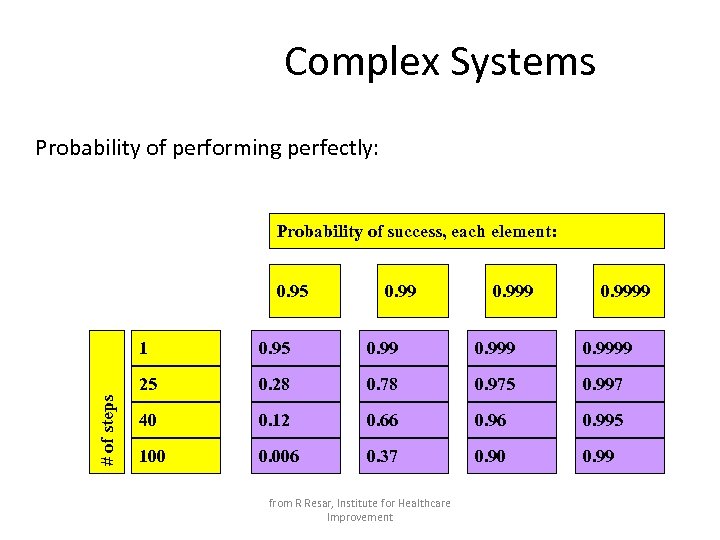
Complex Systems Probability of performing perfectly: Probability of success, each element: 0. 95 0. 999 0. 9999 25 # of steps 1 0. 28 0. 78 0. 975 0. 997 40 0. 12 0. 66 0. 995 100 0. 006 0. 37 0. 90 0. 99 from R Resar, Institute for Healthcare Improvement
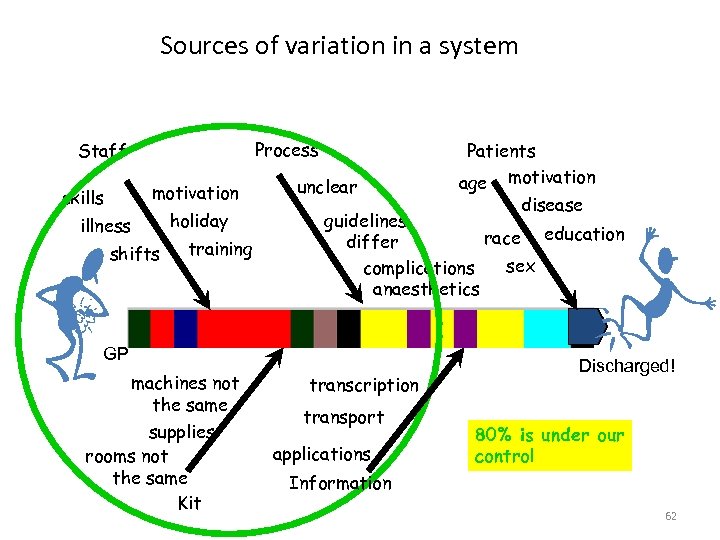
Sources of variation in a system Process Staff motivation skills illness shifts holiday training unclear disease guidelines race education differ sex complications anaesthetics GP machines not the same supplies rooms not the same Kit Patients age motivation transcription transport applications Discharged! 80% is under our control Information 62
So, how is our business changing? Demography – 25 % increase over 75 ( nxt 10 yrs) Finance – Falling public expenditure Technology Inequality Epidemiology/ Morbidity- Shift long term care and complex needs Expectations growing/ Quality Mutuality

Why Quality Improvement? Context in relation to Healthcare • • What is the problem? Unacceptable variation in our systems Delays - for patients and staff Unpredictable process and outcomes Waste Preventable harm Chaos and complexity Innovation is recognised by leading commercial organisations as being essential for success • We have innovative approaches within healthcare, but these are not systematically applied • The current rate of improvement is not likely to achieve the change we want and need

you do gap How the ge ese brid een th e! to b t betw two wan s? ere we ition Wh d con here W ! are we
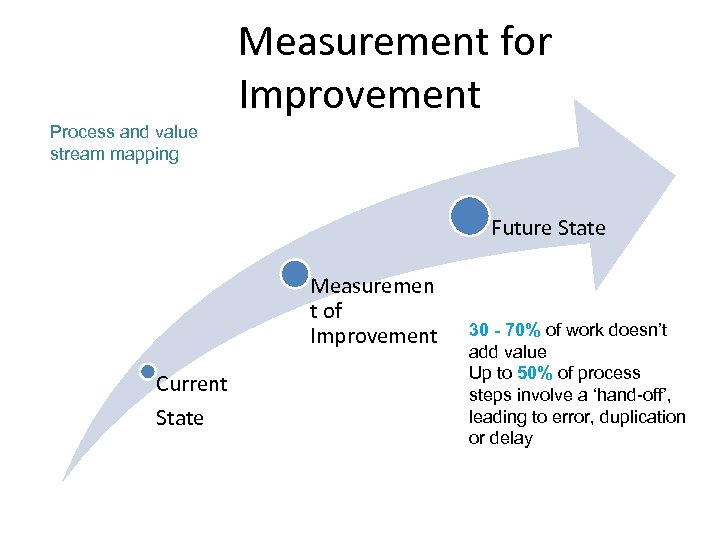
Measurement for Improvement Process and value stream mapping Future State Measuremen t of Improvement Current State 30 - 70% of work doesn’t add value Up to 50% of process steps involve a ‘hand-off’, leading to error, duplication or delay
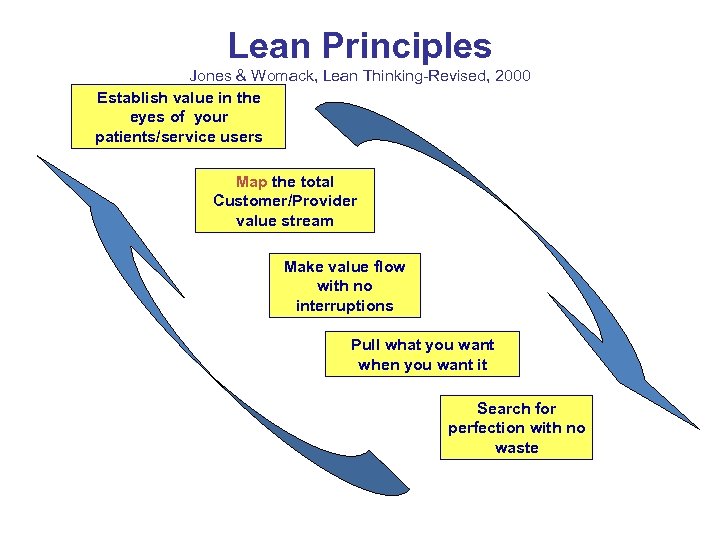
Lean Principles Jones & Womack, Lean Thinking-Revised, 2000 Establish value in the eyes of your patients/service users Map the total Customer/Provider value stream Make value flow with no interruptions Pull what you want when you want it Search for perfection with no waste
Developing an Aim Statement Team name: Aim statement (What’s the problem? Why is it important? What are we going to do about it? ) You should review your Aim Statement frequently to make sure it is consistent and that everyone involved with the initiative has a common understanding of what is to achieved. How good? By when? 69
Quality Improvement Hub • Improvement comes from the application of knowledge • Five fundamental principles of improvement: 1. Knowing why you need to improve 2. Having a feedback mechanism to tell you if the improvement is happening 3. Developing an effective change that will result in improvement 4. Testing a change prior to implementation 5. Knowing when and how to make the change permanent – implementation
The Quality Pioneers Walter Shewhart W. Edwards Deming (1900 - 1993) 72 (1891 – 1967) Joseph Juran (1904 - 2008)
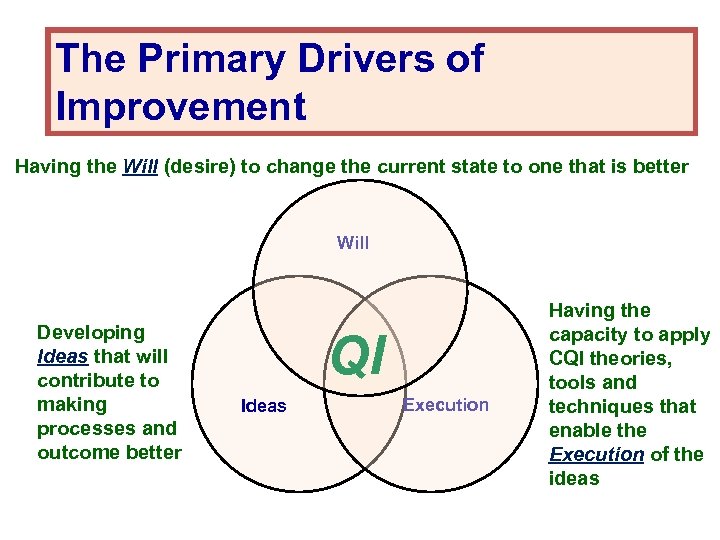
The Primary Drivers of Improvement Having the Will (desire) to change the current state to one that is better Will Developing Ideas that will contribute to making processes and outcome better QI Ideas Execution Having the capacity to apply CQI theories, tools and techniques that enable the Execution of the ideas
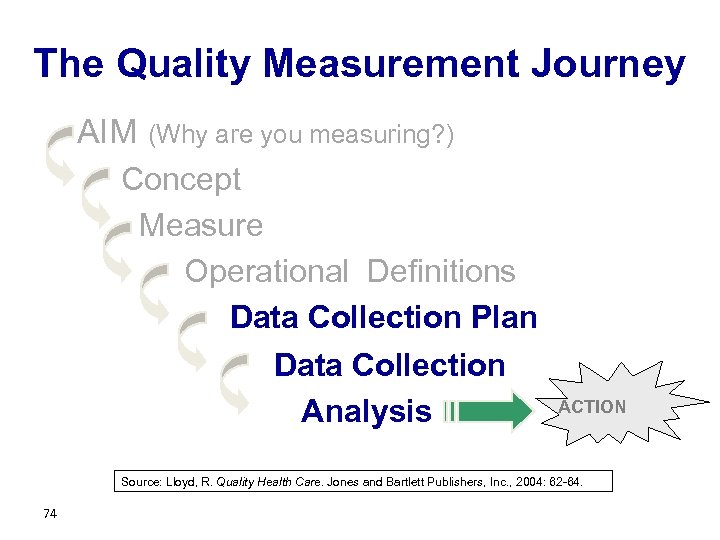
The Quality Measurement Journey AIM (Why are you measuring? ) Concept Measure Operational Definitions Data Collection Plan Data Collection Analysis ACTION Source: Lloyd, R. Quality Health Care. Jones and Bartlett Publishers, Inc. , 2004: 62 -64. 74
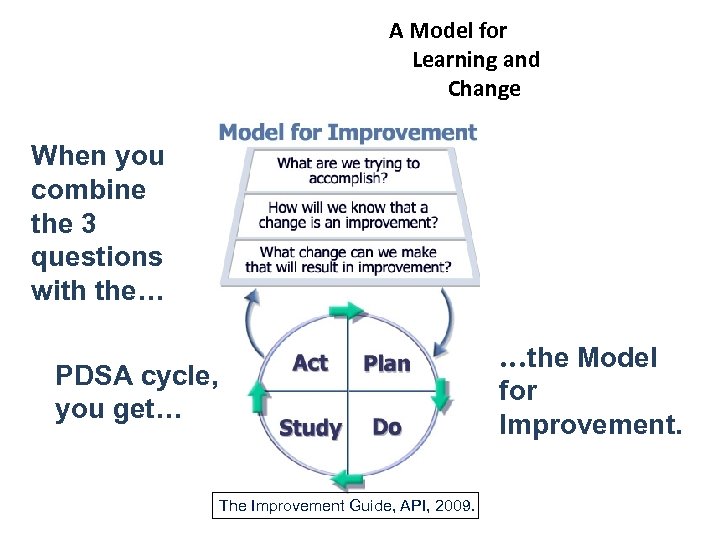
A Model for Learning and Change When you combine the 3 questions with the… PDSA cycle, you get… The Improvement Guide, API, 2009. …the Model for Improvement.
The basics • • Aims Measures Changes Testing What are yours in relation to reliable and safe systems for primary care interfaces and transitions ?
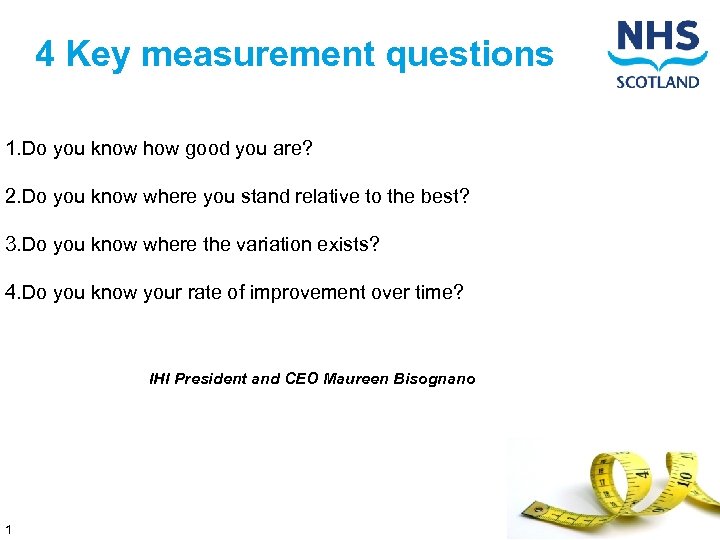
4 Key measurement questions 1. Do you know how good you are? 2. Do you know where you stand relative to the best? 3. Do you know where the variation exists? 4. Do you know your rate of improvement over time? IHI President and CEO Maureen Bisognano 1
Developing an Aim Statement Team name: Aim statement (What’s the problem? Why is it important? What are we going to do about it? ) You should review your Aim Statement frequently to make sure it is consistent and that everyone involved with the initiative has a common understanding of what is to achieved. How good? By when? 78

Exercise At your table individually or with your Colleague spend 5 minutes drafting your aim and your first PDSA Something you will commit to do next Monday! PDSA Worksheet
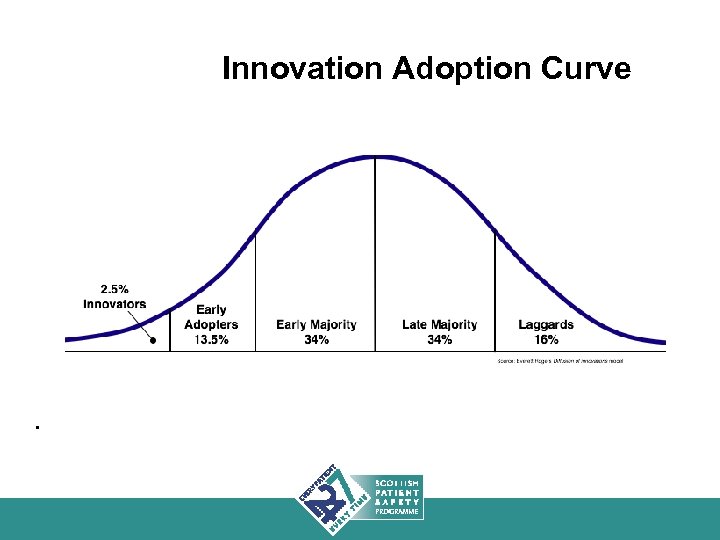
Closing the Gap Between best practice and common practice: is based on the ability of health care providers and their organizations to rapidly spread innovations and new ideas. 80
Challenges in Spreading New Ideas • Characteristics of the innovation itself • Willingness or ability of those making the adoption to try new ideas • Characteristics of the culture and infrastructure of the organization to support change 81

Expectations will always exceed capacity. The service must always be changing, growing and improving…”. “ Aneurin Bevan, 1948
Quality Improvement Hub What will it take to improve quality ? • • • Winning the hearts and minds of the staff A clear, defined and executable aim. Communication Linked with the overall strategy of the organization- Leadership Tempo-momentum monthly reviews for on track status, quarterly by chief executives Transparency- visibility Focus- less is more Change at the local level local Integration Making it daily work Creating capability and capacity Measurement that has meaning Understanding context and culture

Patient Safety in Primary Care Capacity Building Event
Breakout Rooms 1. Shuna (upstairs) – Warfarin 2. Bara & Jurra (upstairs) – Human Factors 3. Argyll (next door) – Near Patient Testing
Questions for Consideration 1. How aware is your board of the Safety Programme in Primary Care? 2. What is the current infrastructure to support the implementation of the programme? 3. What do you need to do in your board to prepare for it?

Patient Safety in Primary Care Capacity Building Event
Patient Safety in Primary Care Capacity Building Event
Patient Safety in Primary Care Capacity Building Event
d2d5aa27994557096025e16bfbede97a.ppt