4141a1a3c2e8b855d3bf0b1b1138dbdb.ppt
- Количество слайдов: 31
 Patient ID Caregiver ID Relaunch Christian Hay 10 th January 2011
Patient ID Caregiver ID Relaunch Christian Hay 10 th January 2011
 Overview As a JIC Project Pass through pre-existing Business Requirements Collect and evaluate usecases to support BR Adapt Glossary & consider ISO/DTS 22220 Discuss statements GS 1 is the most widely used supply chain standards system in the world © 2008 GS 1
Overview As a JIC Project Pass through pre-existing Business Requirements Collect and evaluate usecases to support BR Adapt Glossary & consider ISO/DTS 22220 Discuss statements GS 1 is the most widely used supply chain standards system in the world © 2008 GS 1
 PATIENT ID, CAREGIVER ID TO BECOME A JIC PROJECT © 2008 GS 1
PATIENT ID, CAREGIVER ID TO BECOME A JIC PROJECT © 2008 GS 1
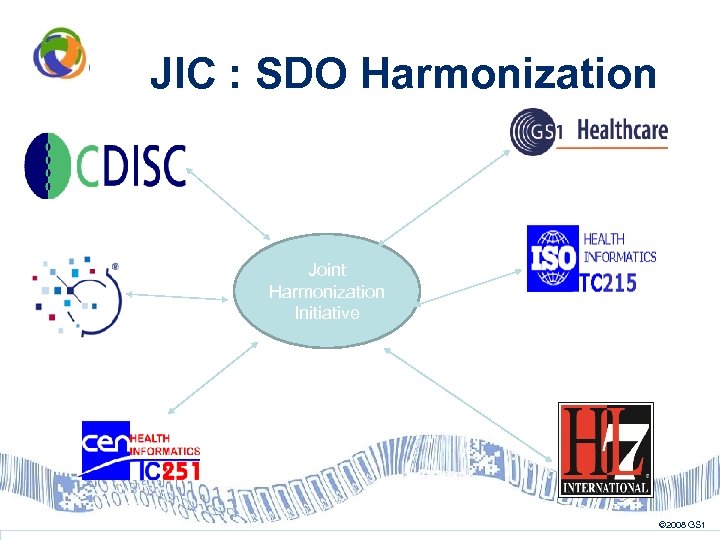 JIC : SDO Harmonization Joint Harmonization Initiative © 2008 GS 1
JIC : SDO Harmonization Joint Harmonization Initiative © 2008 GS 1
 Objectives Engage stakeholders, share communications between SDOs Encourage standards developed by one SDO to become harmonized to work with standards of other SDOs Support SDOs working together producing one harmonized standard fit for purpose Promote usability of standards © 2008 GS 1
Objectives Engage stakeholders, share communications between SDOs Encourage standards developed by one SDO to become harmonized to work with standards of other SDOs Support SDOs working together producing one harmonized standard fit for purpose Promote usability of standards © 2008 GS 1
 GS 1 and JIC GS 1 has been asked to become part of the Joint Initiative in Autumn 2009 As a new member of the Initiative, GS 1 has been asked to propose a joint work CEN representatives asked GS 1 to address Patient ID as a joint work item © 2008 GS 1
GS 1 and JIC GS 1 has been asked to become part of the Joint Initiative in Autumn 2009 As a new member of the Initiative, GS 1 has been asked to propose a joint work CEN representatives asked GS 1 to address Patient ID as a joint work item © 2008 GS 1
 New Work Item Proposal • NWIP Patient ID, Caregiver ID has been approved as a work item by all the SDOs. • For the first time, the work is concentrated into one single SDO (GS 1), following its rules (GSMP) • Experts from the other SDO are invited to join the GSMP WG – a special status has been adopted for them • Although work is done @ GSMP WG, each SDO can involve its appropriate working teams, to participate through their representative (inputs, comments in public review, etc. ) © 2008 GS 1
New Work Item Proposal • NWIP Patient ID, Caregiver ID has been approved as a work item by all the SDOs. • For the first time, the work is concentrated into one single SDO (GS 1), following its rules (GSMP) • Experts from the other SDO are invited to join the GSMP WG – a special status has been adopted for them • Although work is done @ GSMP WG, each SDO can involve its appropriate working teams, to participate through their representative (inputs, comments in public review, etc. ) © 2008 GS 1
 New Work Item Proposal • End goal is that the deliverable adopted by the GSMP WG (thus, a possible change in the GS 1 General Specifications) becomes an ISO standard © 2008 GS 1
New Work Item Proposal • End goal is that the deliverable adopted by the GSMP WG (thus, a possible change in the GS 1 General Specifications) becomes an ISO standard © 2008 GS 1
 Status today • • • 2 Monthly conf calls since early October Good participation Participation fom various SDOs Co-chair election January 2011 On track regarding timeline © 2008 GS 1
Status today • • • 2 Monthly conf calls since early October Good participation Participation fom various SDOs Co-chair election January 2011 On track regarding timeline © 2008 GS 1
 PASS THROUGH PRE-EXISTING BUSINESS REQUIREMENTS © 2008 GS 1
PASS THROUGH PRE-EXISTING BUSINESS REQUIREMENTS © 2008 GS 1
 Gathering Business Requirements Over 60 business requirements have been gathered. Their source vary from ASTM Standard Guides, WHO (Patient Identification Solutions) and user expertise. © 2008 GS 1
Gathering Business Requirements Over 60 business requirements have been gathered. Their source vary from ASTM Standard Guides, WHO (Patient Identification Solutions) and user expertise. © 2008 GS 1
 COLLECT AND EVALUATE USECASES TO SUPPORT BR © 2008 GS 1
COLLECT AND EVALUATE USECASES TO SUPPORT BR © 2008 GS 1
 SCENARIO E © 2008 GS 1
SCENARIO E © 2008 GS 1
 Patient Identification in Sweden/1 • The personal identity number is the Swedish national identification number. • Issued by Swedish Tax Agency as part of the population register • The link between a person and the identity number is established • through Swedish identity documents, like ID cards • through the widespread use of the number in various contacts with authorities etc. • They are necessary for personal service at banks, authorities, health care • most people are familiar with their full number and those of e. g. family without hesitation, © 2008 GS 1
Patient Identification in Sweden/1 • The personal identity number is the Swedish national identification number. • Issued by Swedish Tax Agency as part of the population register • The link between a person and the identity number is established • through Swedish identity documents, like ID cards • through the widespread use of the number in various contacts with authorities etc. • They are necessary for personal service at banks, authorities, health care • most people are familiar with their full number and those of e. g. family without hesitation, © 2008 GS 1
 Patient Identification in Sweden/2 • The most important use of the PIN in Swedish health care is however to trace patients and their medical records. • enables efficient handling of referrals and referral letters, • Means of identifying patients handled by different health care staff such as physicians, nurses, occupational therapists, physiotherapists etc. • reduces the risk of duplication errors, © 2008 GS 1
Patient Identification in Sweden/2 • The most important use of the PIN in Swedish health care is however to trace patients and their medical records. • enables efficient handling of referrals and referral letters, • Means of identifying patients handled by different health care staff such as physicians, nurses, occupational therapists, physiotherapists etc. • reduces the risk of duplication errors, © 2008 GS 1
 Patient Identification in Sweden/3 However: • This number is controversial at the moment because the advocates feel that it is the best way to identify a patient and all hospital systems are based on it. Some argue that a non significant number would be better so that unauthorized people cannot link the patient to e. g. a disease. E. g. housing for abused women now want to use a unique non-significant number such as GSRN • Many hospitals are starting bed side scanning and I guess we should investigate the dangers of just putting the 10 digit number in a bar code as it might collide with other numbers (since no qualifier that this is a patient id being scanned). © 2008 GS 1
Patient Identification in Sweden/3 However: • This number is controversial at the moment because the advocates feel that it is the best way to identify a patient and all hospital systems are based on it. Some argue that a non significant number would be better so that unauthorized people cannot link the patient to e. g. a disease. E. g. housing for abused women now want to use a unique non-significant number such as GSRN • Many hospitals are starting bed side scanning and I guess we should investigate the dangers of just putting the 10 digit number in a bar code as it might collide with other numbers (since no qualifier that this is a patient id being scanned). © 2008 GS 1
 ADAPT GLOSSARY & CONSIDER ISO/DTS 22220 © 2008 GS 1
ADAPT GLOSSARY & CONSIDER ISO/DTS 22220 © 2008 GS 1
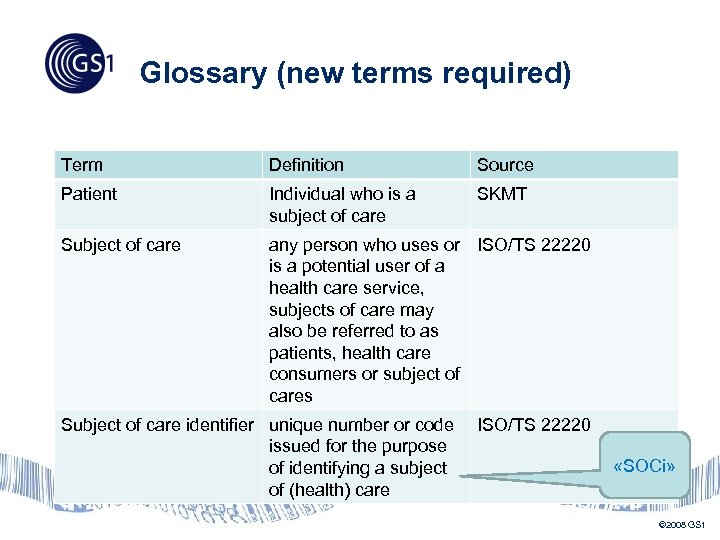 Glossary (new terms required) Term Definition Source Patient Individual who is a subject of care SKMT Subject of care any person who uses or ISO/TS 22220 is a potential user of a health care service, subjects of care may also be referred to as patients, health care consumers or subject of cares Subject of care identifier unique number or code issued for the purpose of identifying a subject of (health) care ISO/TS 22220 «SOCi» © 2008 GS 1
Glossary (new terms required) Term Definition Source Patient Individual who is a subject of care SKMT Subject of care any person who uses or ISO/TS 22220 is a potential user of a health care service, subjects of care may also be referred to as patients, health care consumers or subject of cares Subject of care identifier unique number or code issued for the purpose of identifying a subject of (health) care ISO/TS 22220 «SOCi» © 2008 GS 1
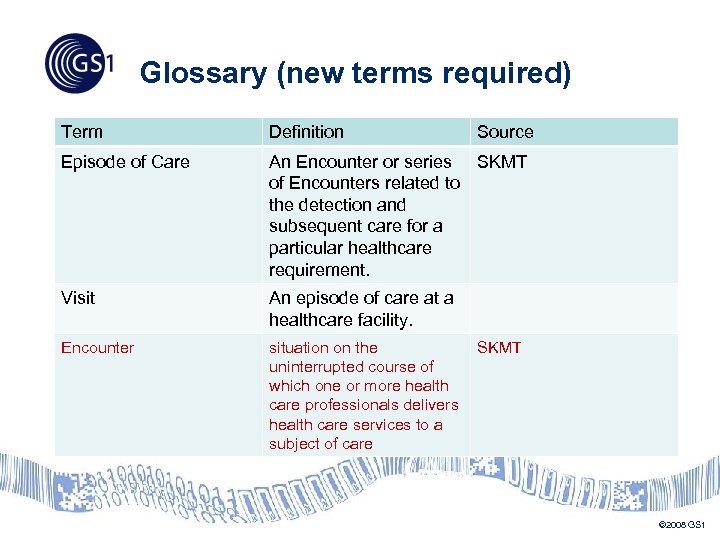 Glossary (new terms required) Term Definition Source Episode of Care An Encounter or series SKMT of Encounters related to the detection and subsequent care for a particular healthcare requirement. Visit An episode of care at a healthcare facility. Encounter situation on the uninterrupted course of which one or more health care professionals delivers health care services to a subject of care SKMT © 2008 GS 1
Glossary (new terms required) Term Definition Source Episode of Care An Encounter or series SKMT of Encounters related to the detection and subsequent care for a particular healthcare requirement. Visit An episode of care at a healthcare facility. Encounter situation on the uninterrupted course of which one or more health care professionals delivers health care services to a subject of care SKMT © 2008 GS 1
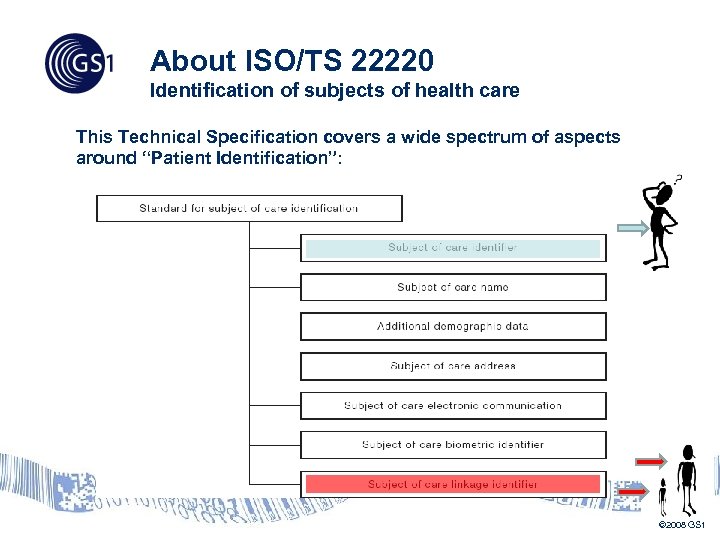 About ISO/TS 22220 Identification of subjects of health care This Technical Specification covers a wide spectrum of aspects around “Patient Identification”: © 2008 GS 1
About ISO/TS 22220 Identification of subjects of health care This Technical Specification covers a wide spectrum of aspects around “Patient Identification”: © 2008 GS 1
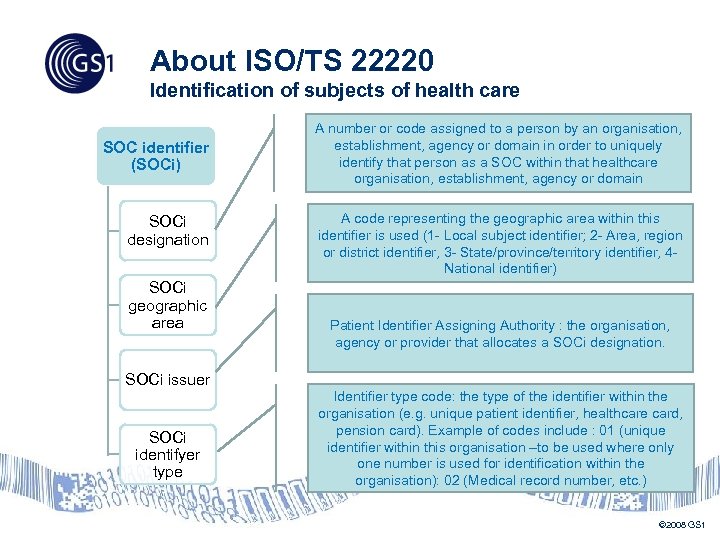 About ISO/TS 22220 Identification of subjects of health care SOC identifier (SOCi) SOCi designation SOCi geographic area SOCi issuer SOCi identifyer type A number or code assigned to a person by an organisation, establishment, agency or domain in order to uniquely identify that person as a SOC within that healthcare organisation, establishment, agency or domain A code representing the geographic area within this identifier is used (1 - Local subject identifier; 2 - Area, region or district identifier, 3 - State/province/territory identifier, 4 National identifier) Patient Identifier Assigning Authority : the organisation, agency or provider that allocates a SOCi designation. Identifier type code: the type of the identifier within the organisation (e. g. unique patient identifier, healthcare card, pension card). Example of codes include : 01 (unique identifier within this organisation –to be used where only one number is used for identification within the organisation): 02 (Medical record number, etc. ) © 2008 GS 1
About ISO/TS 22220 Identification of subjects of health care SOC identifier (SOCi) SOCi designation SOCi geographic area SOCi issuer SOCi identifyer type A number or code assigned to a person by an organisation, establishment, agency or domain in order to uniquely identify that person as a SOC within that healthcare organisation, establishment, agency or domain A code representing the geographic area within this identifier is used (1 - Local subject identifier; 2 - Area, region or district identifier, 3 - State/province/territory identifier, 4 National identifier) Patient Identifier Assigning Authority : the organisation, agency or provider that allocates a SOCi designation. Identifier type code: the type of the identifier within the organisation (e. g. unique patient identifier, healthcare card, pension card). Example of codes include : 01 (unique identifier within this organisation –to be used where only one number is used for identification within the organisation): 02 (Medical record number, etc. ) © 2008 GS 1
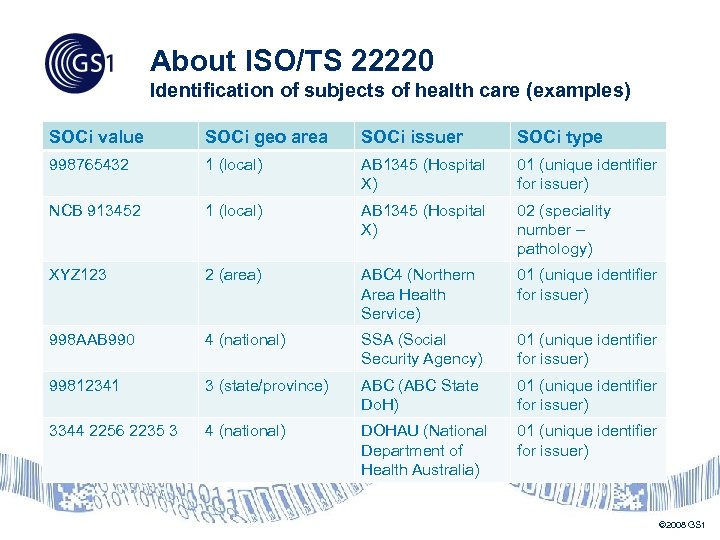 About ISO/TS 22220 Identification of subjects of health care (examples) SOCi value SOCi geo area SOCi issuer SOCi type 998765432 1 (local) AB 1345 (Hospital X) 01 (unique identifier for issuer) NCB 913452 1 (local) AB 1345 (Hospital X) 02 (speciality number – pathology) XYZ 123 2 (area) ABC 4 (Northern Area Health Service) 01 (unique identifier for issuer) 998 AAB 990 4 (national) SSA (Social Security Agency) 01 (unique identifier for issuer) 99812341 3 (state/province) ABC (ABC State Do. H) 01 (unique identifier for issuer) 3344 2256 2235 3 4 (national) DOHAU (National Department of Health Australia) 01 (unique identifier for issuer) © 2008 GS 1
About ISO/TS 22220 Identification of subjects of health care (examples) SOCi value SOCi geo area SOCi issuer SOCi type 998765432 1 (local) AB 1345 (Hospital X) 01 (unique identifier for issuer) NCB 913452 1 (local) AB 1345 (Hospital X) 02 (speciality number – pathology) XYZ 123 2 (area) ABC 4 (Northern Area Health Service) 01 (unique identifier for issuer) 998 AAB 990 4 (national) SSA (Social Security Agency) 01 (unique identifier for issuer) 99812341 3 (state/province) ABC (ABC State Do. H) 01 (unique identifier for issuer) 3344 2256 2235 3 4 (national) DOHAU (National Department of Health Australia) 01 (unique identifier for issuer) © 2008 GS 1
 REVIEW OF STATEMENTS CONFIRM – REVIEW – DISCUSS (ADOPT? ) © 2008 GS 1
REVIEW OF STATEMENTS CONFIRM – REVIEW – DISCUSS (ADOPT? ) © 2008 GS 1
 The 3 pillars (to be used in BRAD’s introduction) There are three pillars that need the establishment of a solid link between objects, Subject of Care, Individual Provider and Healthcare Provider. The three pillars are not of the same importance, but they all need to refer to unique (master) ID in order to function. • Safety: correct patient and care giver identification is an essential step in the safe delivery of care; accurate documentation about care provided (as EHR) is part of this requirement • Efficiency: efficiency aims at providing the best quality of care at the best cost. • Finance and governance: this area covers healthcare governance, whiteboards and billing, such as fee-for-services and DRG’s. © 2008 GS 1
The 3 pillars (to be used in BRAD’s introduction) There are three pillars that need the establishment of a solid link between objects, Subject of Care, Individual Provider and Healthcare Provider. The three pillars are not of the same importance, but they all need to refer to unique (master) ID in order to function. • Safety: correct patient and care giver identification is an essential step in the safe delivery of care; accurate documentation about care provided (as EHR) is part of this requirement • Efficiency: efficiency aims at providing the best quality of care at the best cost. • Finance and governance: this area covers healthcare governance, whiteboards and billing, such as fee-for-services and DRG’s. © 2008 GS 1
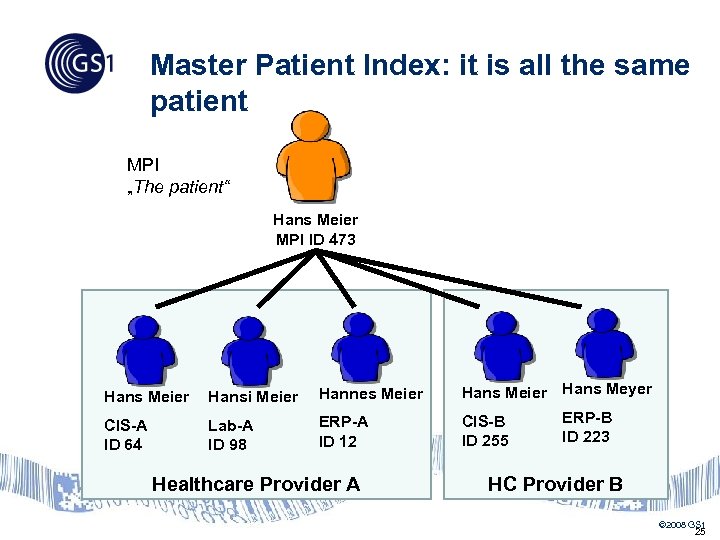 Master Patient Index: it is all the same patient MPI „The patient“ Hans Meier MPI ID 473 Hans Meier Hansi Meier Hannes Meier Hans Meyer CIS-A ID 64 Lab-A ID 98 ERP-A ID 12 CIS-B ID 255 Healthcare Provider A ERP-B ID 223 HC Provider B © 2008 GS 1 25
Master Patient Index: it is all the same patient MPI „The patient“ Hans Meier MPI ID 473 Hans Meier Hansi Meier Hannes Meier Hans Meyer CIS-A ID 64 Lab-A ID 98 ERP-A ID 12 CIS-B ID 255 Healthcare Provider A ERP-B ID 223 HC Provider B © 2008 GS 1 25
 Requirements for successful AIDC 1. Patient ID captured from identification band must be unique in the activity domain (i. e. within Healthcare Provider X) • the aim is to have a single identifier for the Healthcare Provider, ultimately for the region / country 2. Patient ID captured from identification band issued by Healthcare Provider A, must be readable and its origin linked to A, when Healthcare provider B is capturing it • • Using a kind of a filter (some sort of international identifier for the issuer); or append a 2 nd field for issuer identification AIDC solution is not related to MPI (Master Patient Index). MPI is useless in AIDC process. Discuss what these statements imply © 2008 GS 1
Requirements for successful AIDC 1. Patient ID captured from identification band must be unique in the activity domain (i. e. within Healthcare Provider X) • the aim is to have a single identifier for the Healthcare Provider, ultimately for the region / country 2. Patient ID captured from identification band issued by Healthcare Provider A, must be readable and its origin linked to A, when Healthcare provider B is capturing it • • Using a kind of a filter (some sort of international identifier for the issuer); or append a 2 nd field for issuer identification AIDC solution is not related to MPI (Master Patient Index). MPI is useless in AIDC process. Discuss what these statements imply © 2008 GS 1
 Requirements for successful AIDC 1. Subject of Care identification requires distinction: • • between an attribute (Diabetic i. e. one who suffers from diabetes. . , haemophiliac) -fix relationship and an episode (broken leg) – relationship limited in time 2. Example: NHS number identifies as a person • • fix relation to diabetes, etc. It is dangerous to use condition-specific identifiers (because identification is meaningful; the patient may be cured; privacy issues) • Ex. Pregnancy is a temporary condition – attributes to Subject of Care Identification is preferable © 2008 GS 1
Requirements for successful AIDC 1. Subject of Care identification requires distinction: • • between an attribute (Diabetic i. e. one who suffers from diabetes. . , haemophiliac) -fix relationship and an episode (broken leg) – relationship limited in time 2. Example: NHS number identifies as a person • • fix relation to diabetes, etc. It is dangerous to use condition-specific identifiers (because identification is meaningful; the patient may be cured; privacy issues) • Ex. Pregnancy is a temporary condition – attributes to Subject of Care Identification is preferable © 2008 GS 1
 Requirements for successful AIDC Successful AIDC is challenged by inappropriate practice, as : 1. Within a single Healthcare Provider, identification bands may carry different IDs for the same patient, depending on the Department 2. At the same Healthcare Provider, an identification band issued by Department A should be readable and its origin linked to A, when Department B is capturing it • Healthcare Provider should strongly adopt single Subject of Care identification for all its Departments Discuss what these statements imply © 2008 GS 1
Requirements for successful AIDC Successful AIDC is challenged by inappropriate practice, as : 1. Within a single Healthcare Provider, identification bands may carry different IDs for the same patient, depending on the Department 2. At the same Healthcare Provider, an identification band issued by Department A should be readable and its origin linked to A, when Department B is capturing it • Healthcare Provider should strongly adopt single Subject of Care identification for all its Departments Discuss what these statements imply © 2008 GS 1
 Requirements for successful AIDC In a data capture process, the system must be able to document that the ID has been captured from an identification band, or from an order form, sample tube, etc. (source : ISBT 128 technical specifications § 4. 2. 25; would be great to find examples of implementation) Discuss what this statements implies © 2008 GS 1
Requirements for successful AIDC In a data capture process, the system must be able to document that the ID has been captured from an identification band, or from an order form, sample tube, etc. (source : ISBT 128 technical specifications § 4. 2. 25; would be great to find examples of implementation) Discuss what this statements implies © 2008 GS 1
 Requirements for successful AIDC When an identification band has to be replaced (damaged, incompatible with radiology, etc. ), the system must document if the ID has been captured from the first or from the following identification band We need more to document about this requirement Discuss what this statements implies © 2008 GS 1
Requirements for successful AIDC When an identification band has to be replaced (damaged, incompatible with radiology, etc. ), the system must document if the ID has been captured from the first or from the following identification band We need more to document about this requirement Discuss what this statements implies © 2008 GS 1
 Contact Christian Hay Sr Consultant Healthcare Tel +41 (0) 21 825 32 19 Mob +41 (0) 76 369 10 54 christian. hay@gs 1. org 31 © GS 1 Switzerland 19. 03. 2018 Where industries meet for global solutions © 2010 GS 1 31
Contact Christian Hay Sr Consultant Healthcare Tel +41 (0) 21 825 32 19 Mob +41 (0) 76 369 10 54 christian. hay@gs 1. org 31 © GS 1 Switzerland 19. 03. 2018 Where industries meet for global solutions © 2010 GS 1 31


