1024b0d8db196a5e728ee023a6aea9ea.ppt
- Количество слайдов: 47
 Patient Decision Aids as a Knowledge Translation Strategy: Opportunities and Barriers Annette O’Connor RN Ph. D Professor U Ottawa Nursing & Epidemiology Tier 1 Canada Research Chair
Patient Decision Aids as a Knowledge Translation Strategy: Opportunities and Barriers Annette O’Connor RN Ph. D Professor U Ottawa Nursing & Epidemiology Tier 1 Canada Research Chair
 Patient Decision Aids 1. Appreciate role in KT framework. 2. Understand evidence/gaps supporting their use. 3. Explore implementation strategies.
Patient Decision Aids 1. Appreciate role in KT framework. 2. Understand evidence/gaps supporting their use. 3. Explore implementation strategies.
 Objectives 1. Appreciate role in KT framework. 2. Understand evidence/gaps supporting their use. 3. Explore implementation strategies.
Objectives 1. Appreciate role in KT framework. 2. Understand evidence/gaps supporting their use. 3. Explore implementation strategies.
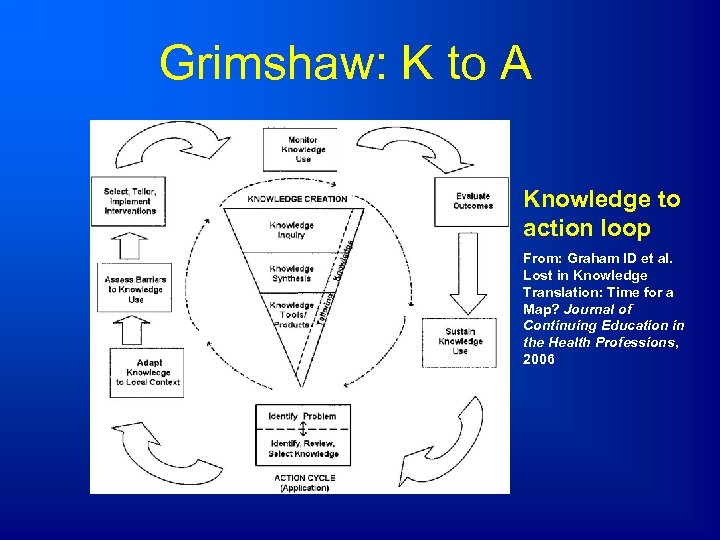 Grimshaw: K to A Knowledge to action loop From: Graham ID et al. Lost in Knowledge Translation: Time for a Map? Journal of Continuing Education in the Health Professions, 2006
Grimshaw: K to A Knowledge to action loop From: Graham ID et al. Lost in Knowledge Translation: Time for a Map? Journal of Continuing Education in the Health Professions, 2006
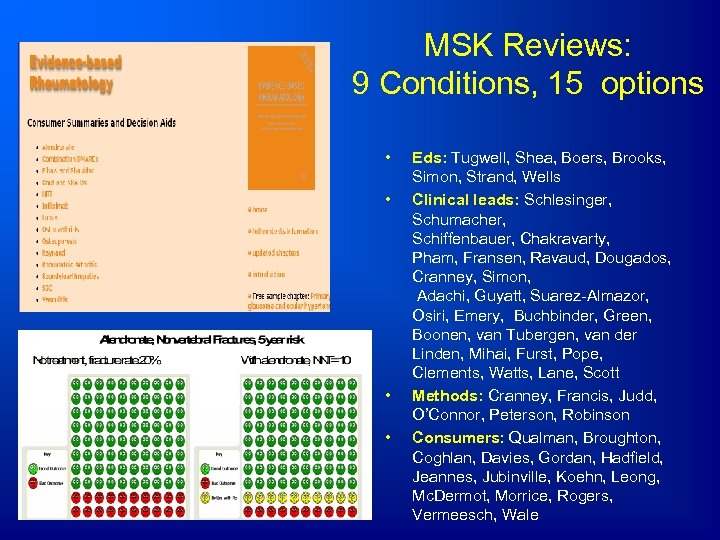 MSK Reviews: 9 Conditions, 15 options • • Eds: Tugwell, Shea, Boers, Brooks, Simon, Strand, Wells Clinical leads: Schlesinger, Schumacher, Schiffenbauer, Chakravarty, Pham, Fransen, Ravaud, Dougados, Cranney, Simon, Adachi, Guyatt, Suarez-Almazor, Osiri, Emery, Buchbinder, Green, Boonen, van Tubergen, van der Linden, Mihai, Furst, Pope, Clements, Watts, Lane, Scott Methods: Cranney, Francis, Judd, O’Connor, Peterson, Robinson Consumers: Qualman, Broughton, Coghlan, Davies, Gordan, Hadfield, Jeannes, Jubinville, Koehn, Leong, Mc. Dermot, Morrice, Rogers, Vermeesch, Wale
MSK Reviews: 9 Conditions, 15 options • • Eds: Tugwell, Shea, Boers, Brooks, Simon, Strand, Wells Clinical leads: Schlesinger, Schumacher, Schiffenbauer, Chakravarty, Pham, Fransen, Ravaud, Dougados, Cranney, Simon, Adachi, Guyatt, Suarez-Almazor, Osiri, Emery, Buchbinder, Green, Boonen, van Tubergen, van der Linden, Mihai, Furst, Pope, Clements, Watts, Lane, Scott Methods: Cranney, Francis, Judd, O’Connor, Peterson, Robinson Consumers: Qualman, Broughton, Coghlan, Davies, Gordan, Hadfield, Jeannes, Jubinville, Koehn, Leong, Mc. Dermot, Morrice, Rogers, Vermeesch, Wale
 Decision Aids adjuncts to counseling Inform: facts, probabilities Clarify values: experience, ask Support: guide, worksheet
Decision Aids adjuncts to counseling Inform: facts, probabilities Clarify values: experience, ask Support: guide, worksheet
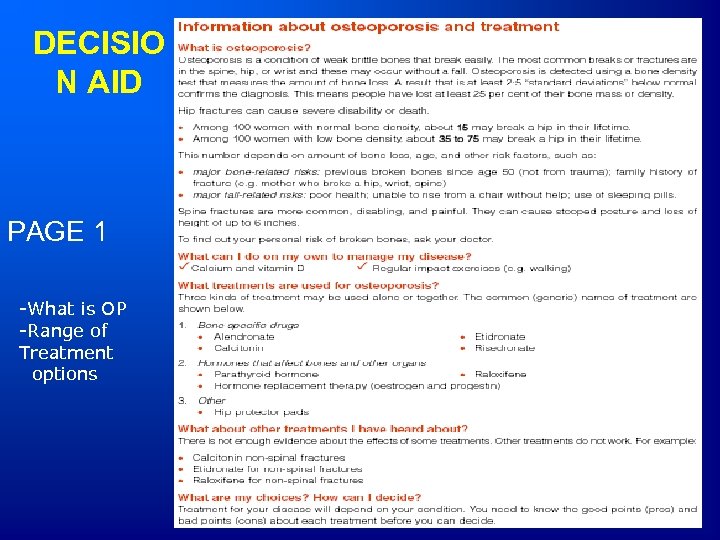 DECISIO N AID PAGE 1 -What is OP -Range of Treatment options
DECISIO N AID PAGE 1 -What is OP -Range of Treatment options
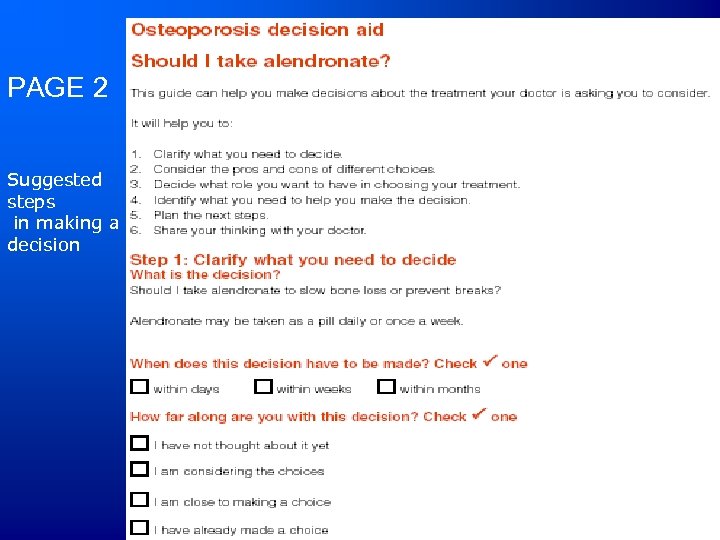 PAGE 2 Suggested steps in making a decision
PAGE 2 Suggested steps in making a decision
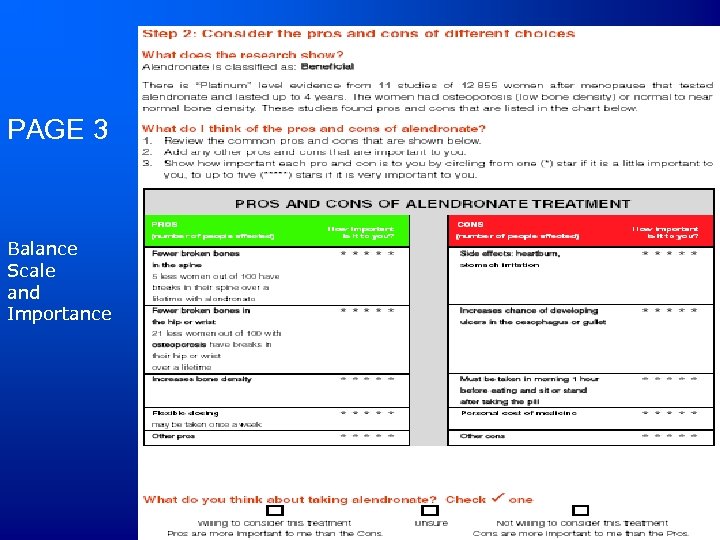 PAGE 3 Balance Scale and Importance
PAGE 3 Balance Scale and Importance
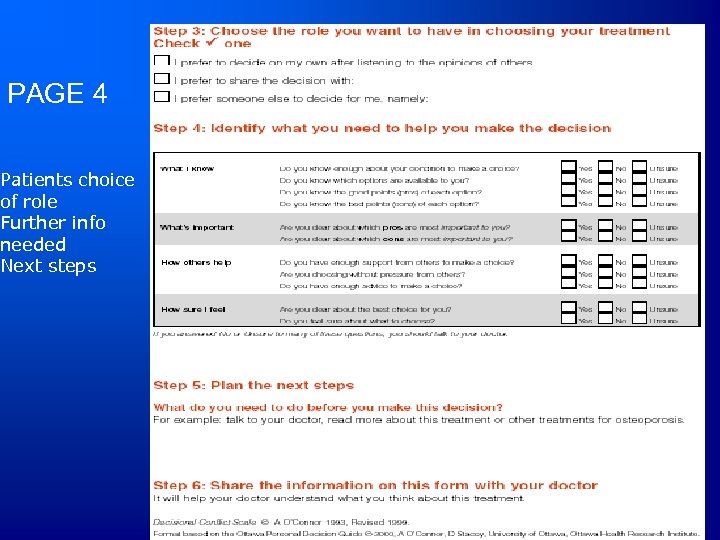 PAGE 4 Patients choice of role Further info needed Next steps
PAGE 4 Patients choice of role Further info needed Next steps
 When do you need one? 1. EBM class. • Patient uncertainty • Practice variation
When do you need one? 1. EBM class. • Patient uncertainty • Practice variation
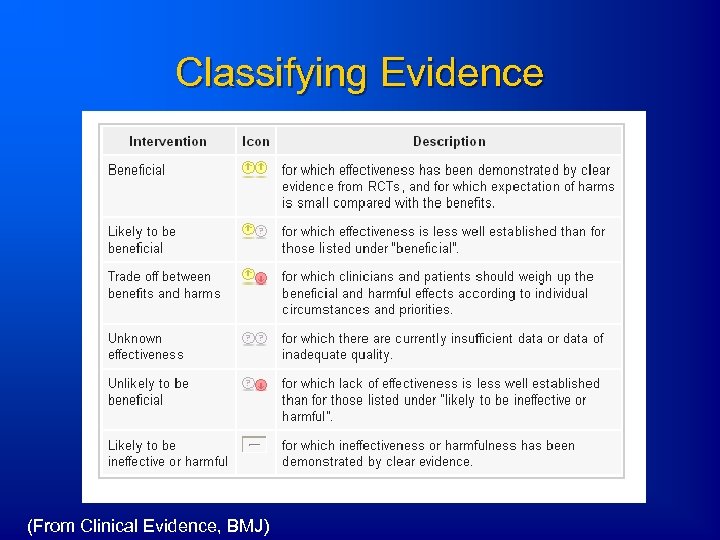 Classifying Evidence (From Clinical Evidence, BMJ)
Classifying Evidence (From Clinical Evidence, BMJ)
 Need for Total Joint Replacement Random sample 48, 000+ Canadians >= 55 yrs Hawker et al. MEDICAL CARE 2001; 39 (3): 206– 216
Need for Total Joint Replacement Random sample 48, 000+ Canadians >= 55 yrs Hawker et al. MEDICAL CARE 2001; 39 (3): 206– 216
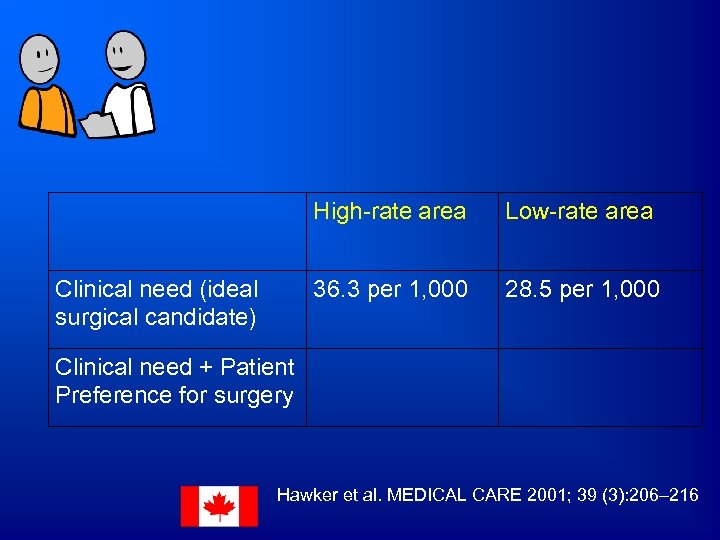 High-rate area 36. 3 per 1, 000 Clinical need (ideal surgical candidate) Low-rate area 28. 5 per 1, 000 Clinical need + Patient Preference for surgery Hawker et al. MEDICAL CARE 2001; 39 (3): 206– 216
High-rate area 36. 3 per 1, 000 Clinical need (ideal surgical candidate) Low-rate area 28. 5 per 1, 000 Clinical need + Patient Preference for surgery Hawker et al. MEDICAL CARE 2001; 39 (3): 206– 216
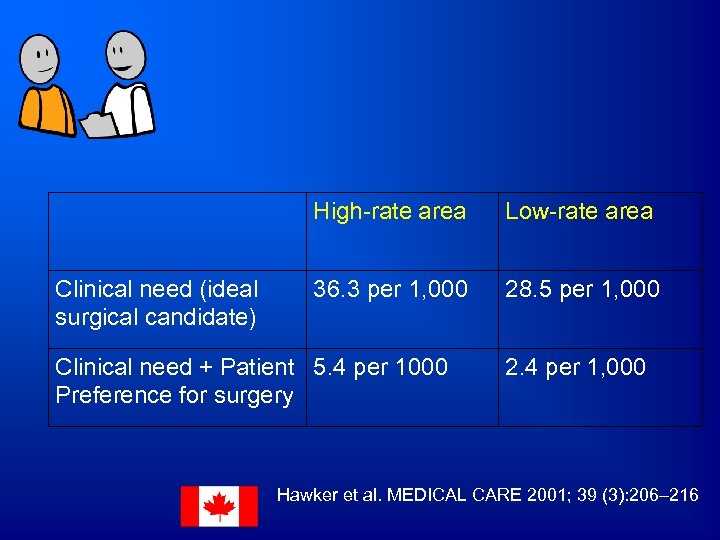 High-rate area Clinical need (ideal surgical candidate) Low-rate area 36. 3 per 1, 000 28. 5 per 1, 000 Clinical need + Patient 5. 4 per 1000 Preference for surgery 2. 4 per 1, 000 Hawker et al. MEDICAL CARE 2001; 39 (3): 206– 216
High-rate area Clinical need (ideal surgical candidate) Low-rate area 36. 3 per 1, 000 28. 5 per 1, 000 Clinical need + Patient 5. 4 per 1000 Preference for surgery 2. 4 per 1, 000 Hawker et al. MEDICAL CARE 2001; 39 (3): 206– 216
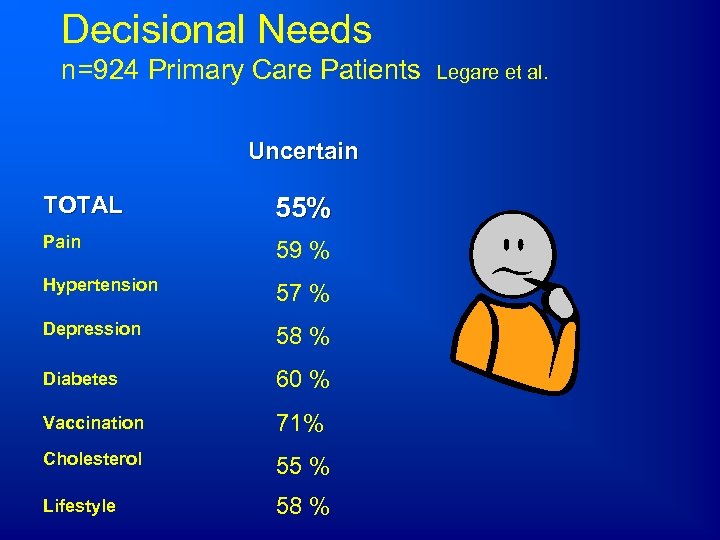 Decisional Needs n=924 Primary Care Patients Uncertain TOTAL 55% Pain 59 % Hypertension 57 % Depression 58 % Diabetes 60 % Vaccination 71% Cholesterol 55 % Lifestyle 58 % Legare et al.
Decisional Needs n=924 Primary Care Patients Uncertain TOTAL 55% Pain 59 % Hypertension 57 % Depression 58 % Diabetes 60 % Vaccination 71% Cholesterol 55 % Lifestyle 58 % Legare et al.
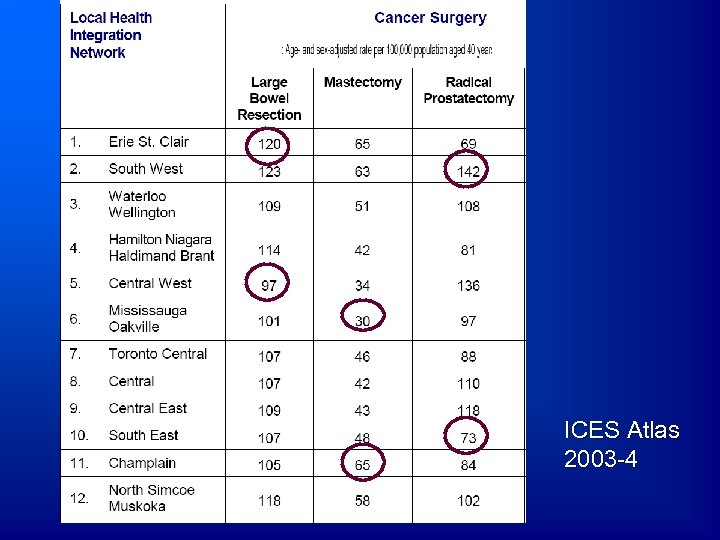 ICES Atlas 2003 -4
ICES Atlas 2003 -4
 Objectives 1. Appreciate role in KT framework. 2. Understand evidence/gaps supporting their use. 3. Explore implementation strategies.
Objectives 1. Appreciate role in KT framework. 2. Understand evidence/gaps supporting their use. 3. Explore implementation strategies.
 International Cochrane Collaboration • Systematic review of 55 randomized trials of patient decision aids O’Connor et al. , Cochrane Library, 2009
International Cochrane Collaboration • Systematic review of 55 randomized trials of patient decision aids O’Connor et al. , Cochrane Library, 2009
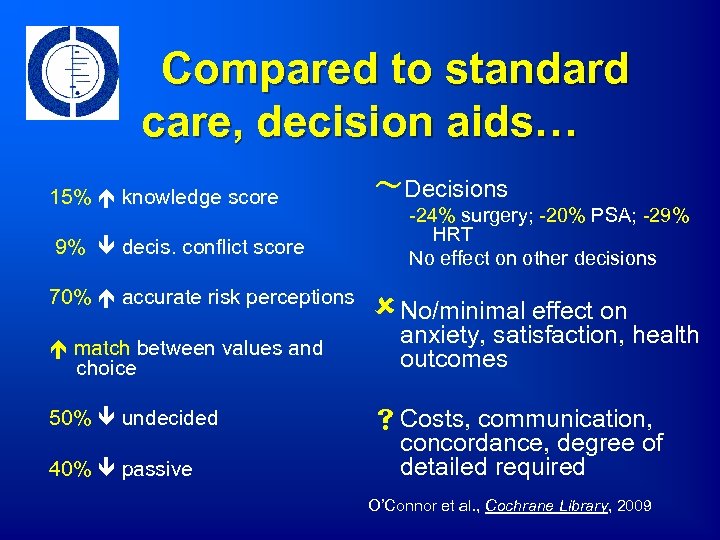 Compared to standard care, decision aids… ~Decisions 15% knowledge score 9% decis. conflict score 70% accurate risk perceptions match between values and choice 50% undecided 40% passive -24% surgery; -20% PSA; -29% HRT No effect on other decisions û No/minimal effect on anxiety, satisfaction, health outcomes s Costs, communication, concordance, degree of detailed required O’Connor et al. , Cochrane Library, 2009
Compared to standard care, decision aids… ~Decisions 15% knowledge score 9% decis. conflict score 70% accurate risk perceptions match between values and choice 50% undecided 40% passive -24% surgery; -20% PSA; -29% HRT No effect on other decisions û No/minimal effect on anxiety, satisfaction, health outcomes s Costs, communication, concordance, degree of detailed required O’Connor et al. , Cochrane Library, 2009
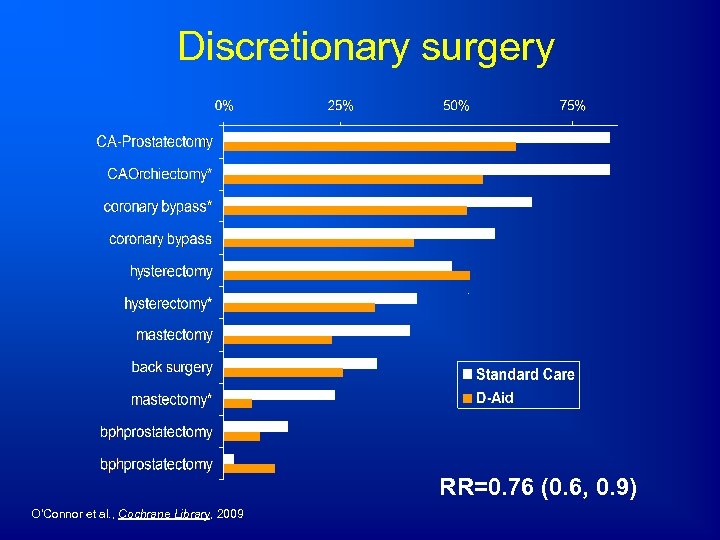 Discretionary surgery RR=0. 76 (0. 6, 0. 9) O’Connor et al. , Cochrane Library, 2009
Discretionary surgery RR=0. 76 (0. 6, 0. 9) O’Connor et al. , Cochrane Library, 2009
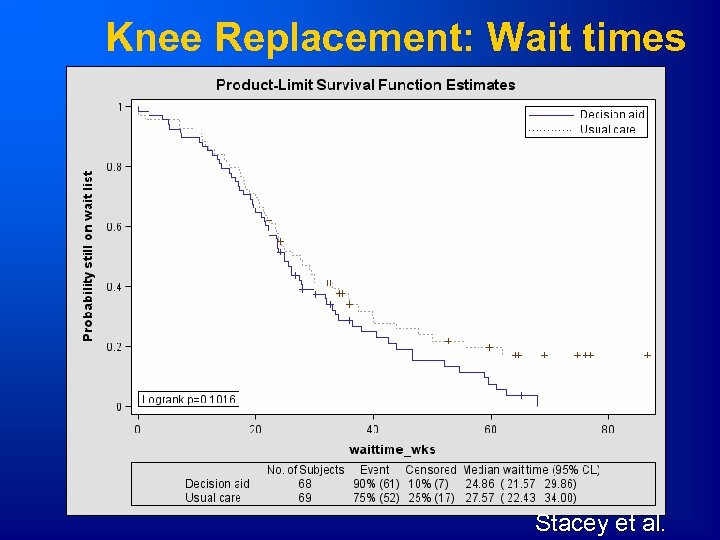 Knee Replacement: Wait times Stacey et al.
Knee Replacement: Wait times Stacey et al.
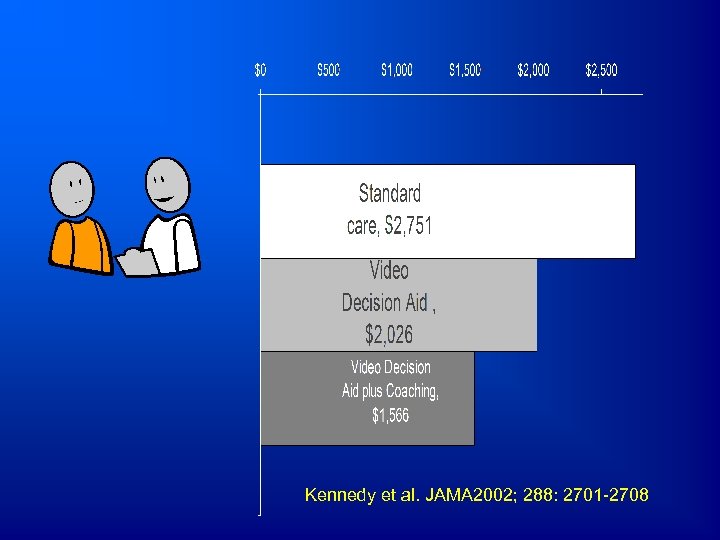 Kennedy et al. JAMA 2002; 288: 2701 -2708
Kennedy et al. JAMA 2002; 288: 2701 -2708
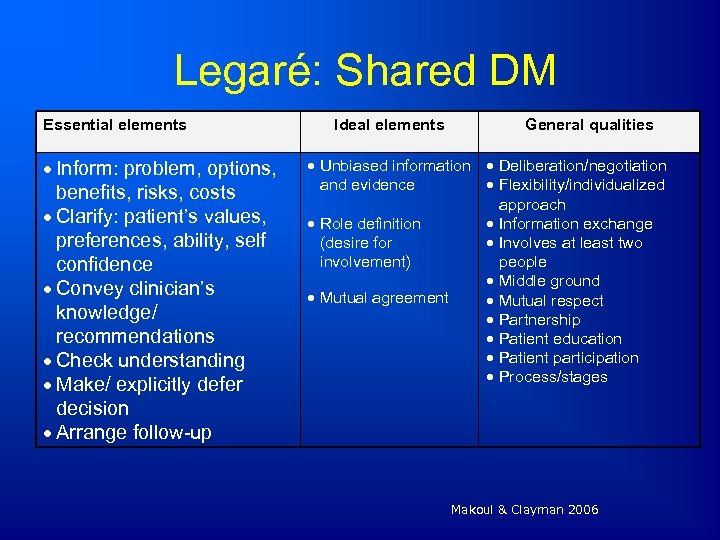 Legaré: Shared DM Essential elements Inform: problem, options, benefits, risks, costs Clarify: patient’s values, preferences, ability, self confidence Convey clinician’s knowledge/ recommendations Check understanding Make/ explicitly defer decision Arrange follow-up Ideal elements General qualities Unbiased information Deliberation/negotiation and evidence Flexibility/individualized approach Role definition Information exchange (desire for Involves at least two involvement) people Middle ground Mutual agreement Mutual respect Partnership Patient education Patient participation Process/stages Makoul & Clayman 2006
Legaré: Shared DM Essential elements Inform: problem, options, benefits, risks, costs Clarify: patient’s values, preferences, ability, self confidence Convey clinician’s knowledge/ recommendations Check understanding Make/ explicitly defer decision Arrange follow-up Ideal elements General qualities Unbiased information Deliberation/negotiation and evidence Flexibility/individualized approach Role definition Information exchange (desire for Involves at least two involvement) people Middle ground Mutual agreement Mutual respect Partnership Patient education Patient participation Process/stages Makoul & Clayman 2006
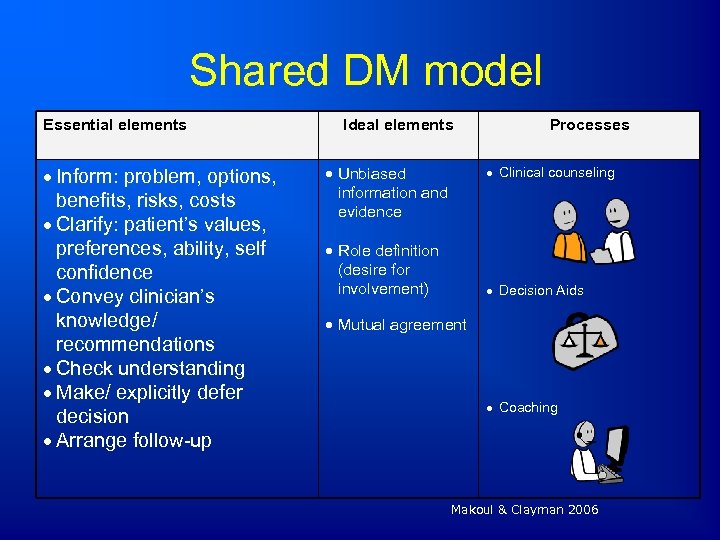 Shared DM model Essential elements Inform: problem, options, benefits, risks, costs Clarify: patient’s values, preferences, ability, self confidence Convey clinician’s knowledge/ recommendations Check understanding Make/ explicitly defer decision Arrange follow-up Ideal elements Unbiased information and evidence Processes Clinical counseling Role definition (desire for involvement) Decision Aids Mutual agreement Coaching Makoul & Clayman 2006
Shared DM model Essential elements Inform: problem, options, benefits, risks, costs Clarify: patient’s values, preferences, ability, self confidence Convey clinician’s knowledge/ recommendations Check understanding Make/ explicitly defer decision Arrange follow-up Ideal elements Unbiased information and evidence Processes Clinical counseling Role definition (desire for involvement) Decision Aids Mutual agreement Coaching Makoul & Clayman 2006
 Objectives 1. Appreciate role in KT framework. 2. Understand evidence/gaps supporting their use. 3. Explore implementation strategies.
Objectives 1. Appreciate role in KT framework. 2. Understand evidence/gaps supporting their use. 3. Explore implementation strategies.
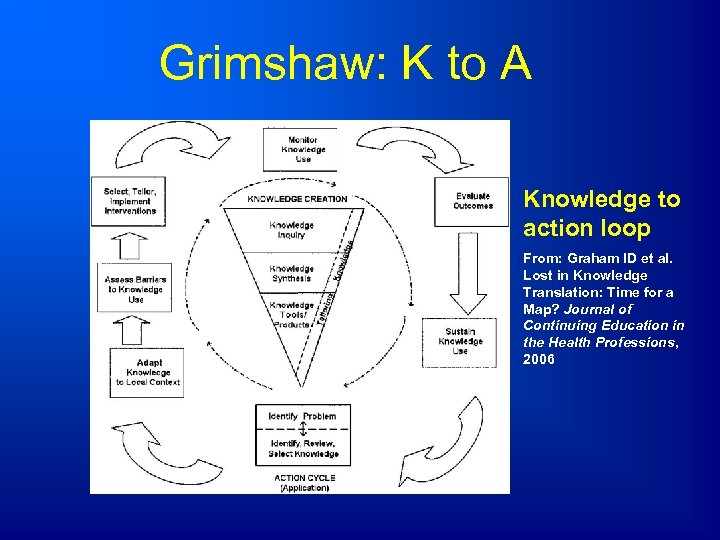 Grimshaw: K to A Knowledge to action loop From: Graham ID et al. Lost in Knowledge Translation: Time for a Map? Journal of Continuing Education in the Health Professions, 2006
Grimshaw: K to A Knowledge to action loop From: Graham ID et al. Lost in Knowledge Translation: Time for a Map? Journal of Continuing Education in the Health Professions, 2006
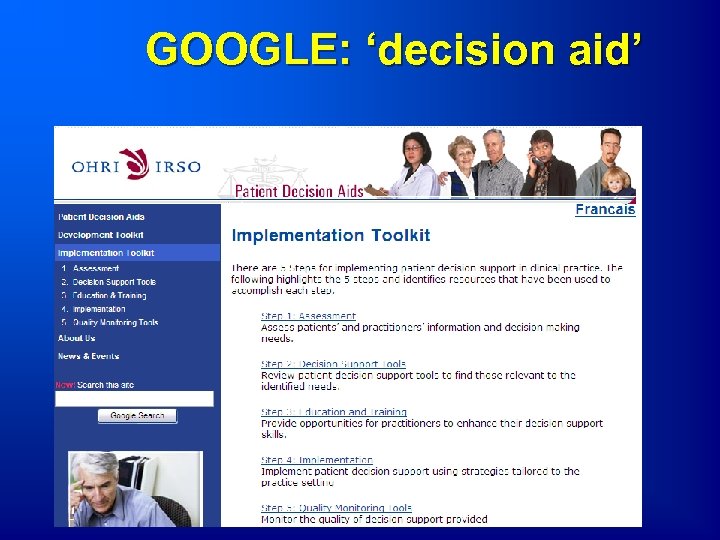 GOOGLE: ‘decision aid’
GOOGLE: ‘decision aid’
![Delivery Models 1. Internet [8 million in 2006] 2. Call Center 3. Practice Centers Delivery Models 1. Internet [8 million in 2006] 2. Call Center 3. Practice Centers](https://present5.com/presentation/1024b0d8db196a5e728ee023a6aea9ea/image-31.jpg) Delivery Models 1. Internet [8 million in 2006] 2. Call Center 3. Practice Centers or Shared DM Center
Delivery Models 1. Internet [8 million in 2006] 2. Call Center 3. Practice Centers or Shared DM Center
 Challenge #1 • Need to train potential users: – High school students – Post 2 ndary students – Health science students day 1 of training – New mothers – Health departments – Call centers and helplines
Challenge #1 • Need to train potential users: – High school students – Post 2 ndary students – Health science students day 1 of training – New mothers – Health departments – Call centers and helplines
 BIG Challenge #2 • Embed ‘just in time’ information for an individual as part of the process of care
BIG Challenge #2 • Embed ‘just in time’ information for an individual as part of the process of care
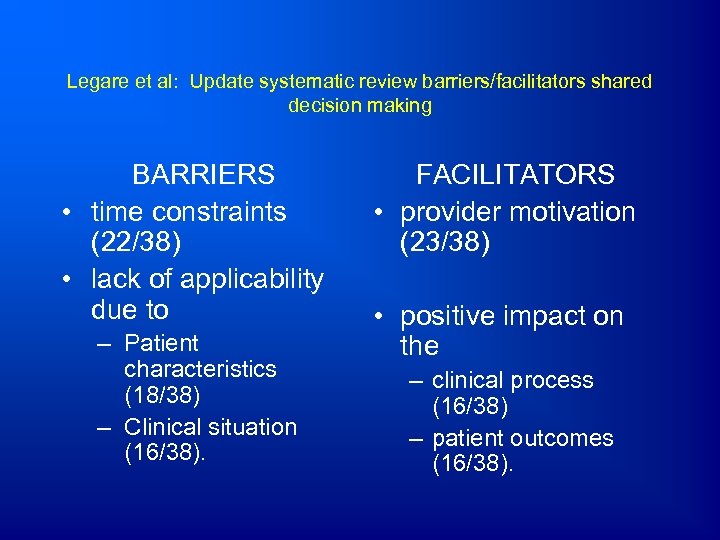 Legare et al: Update systematic review barriers/facilitators shared decision making BARRIERS • time constraints (22/38) • lack of applicability due to – Patient characteristics (18/38) – Clinical situation (16/38). FACILITATORS • provider motivation (23/38) • positive impact on the – clinical process (16/38) – patient outcomes (16/38).
Legare et al: Update systematic review barriers/facilitators shared decision making BARRIERS • time constraints (22/38) • lack of applicability due to – Patient characteristics (18/38) – Clinical situation (16/38). FACILITATORS • provider motivation (23/38) • positive impact on the – clinical process (16/38) – patient outcomes (16/38).
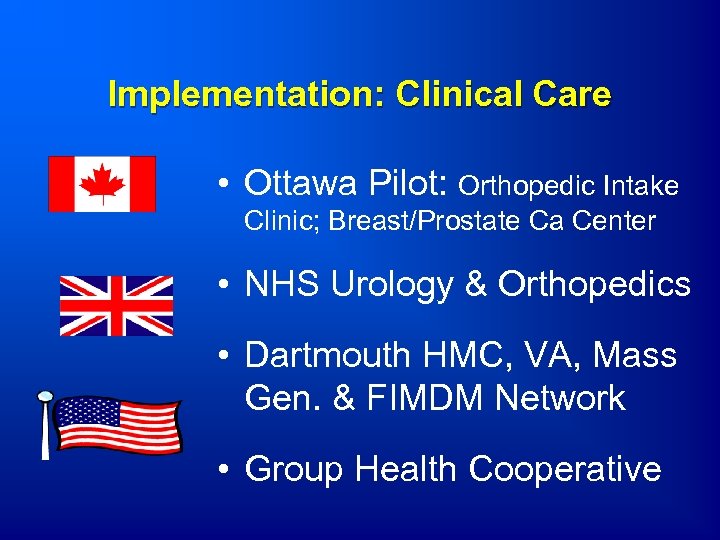 Implementation: Clinical Care • Ottawa Pilot: Orthopedic Intake Clinic; Breast/Prostate Ca Center • NHS Urology & Orthopedics • Dartmouth HMC, VA, Mass Gen. & FIMDM Network • Group Health Cooperative
Implementation: Clinical Care • Ottawa Pilot: Orthopedic Intake Clinic; Breast/Prostate Ca Center • NHS Urology & Orthopedics • Dartmouth HMC, VA, Mass Gen. & FIMDM Network • Group Health Cooperative
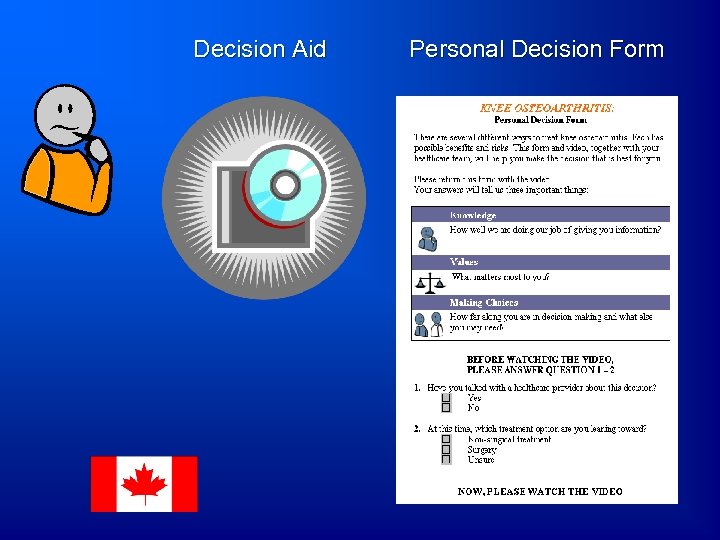 Decision Aid Personal Decision Form
Decision Aid Personal Decision Form
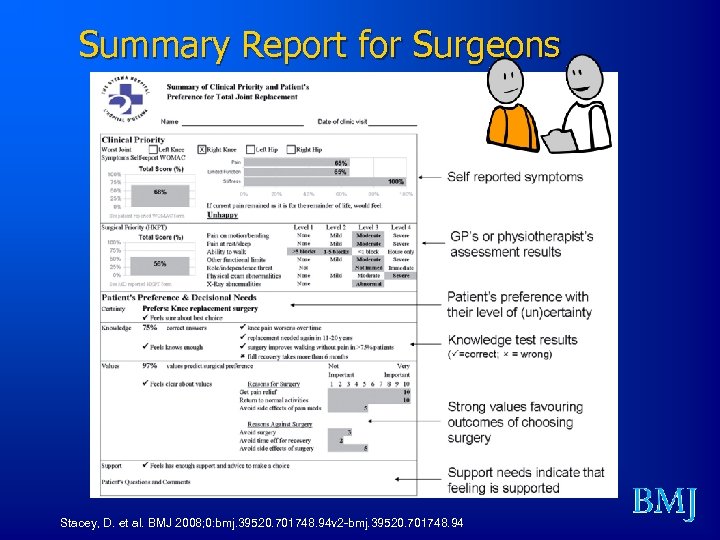 Summary Report for Surgeons Stacey, D. et al. BMJ 2008; 0: bmj. 39520. 701748. 94 v 2 -bmj. 39520. 701748. 94
Summary Report for Surgeons Stacey, D. et al. BMJ 2008; 0: bmj. 39520. 701748. 94 v 2 -bmj. 39520. 701748. 94
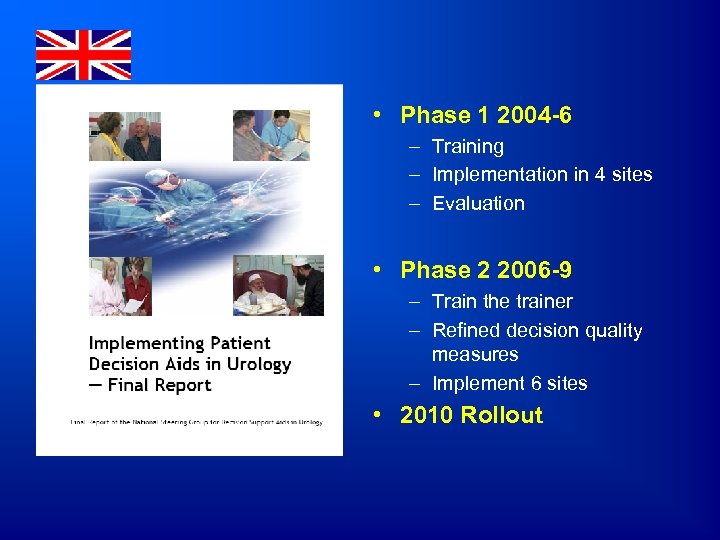 • Phase 1 2004 -6 – Training – Implementation in 4 sites – Evaluation • Phase 2 2006 -9 – Train the trainer – Refined decision quality measures – Implement 6 sites • 2010 Rollout
• Phase 1 2004 -6 – Training – Implementation in 4 sites – Evaluation • Phase 2 2006 -9 – Train the trainer – Refined decision quality measures – Implement 6 sites • 2010 Rollout
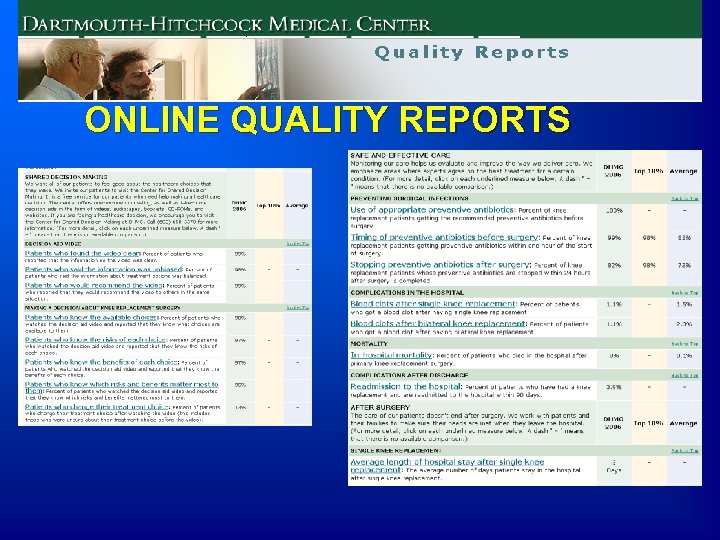 ONLINE QUALITY REPORTS
ONLINE QUALITY REPORTS
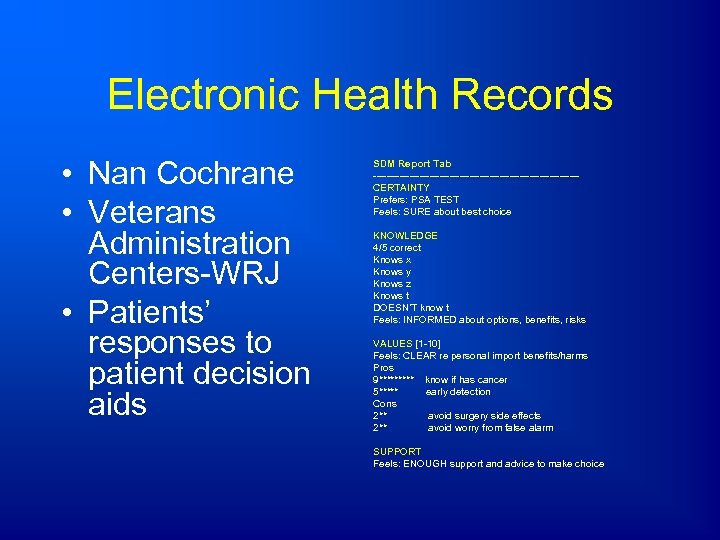 Electronic Health Records • Nan Cochrane • Veterans Administration Centers-WRJ • Patients’ responses to patient decision aids SDM Report Tab -------------------------------CERTAINTY Prefers: PSA TEST Feels: SURE about best choice KNOWLEDGE 4/5 correct Knows x Knows y Knows z Knows t DOESN’T know t Feels: INFORMED about options, benefits, risks VALUES [1 -10] Feels: CLEAR re personal import benefits/harms Pros 9***** know if has cancer 5***** early detection Cons 2** avoid surgery side effects 2** avoid worry from false alarm SUPPORT Feels: ENOUGH support and advice to make choice
Electronic Health Records • Nan Cochrane • Veterans Administration Centers-WRJ • Patients’ responses to patient decision aids SDM Report Tab -------------------------------CERTAINTY Prefers: PSA TEST Feels: SURE about best choice KNOWLEDGE 4/5 correct Knows x Knows y Knows z Knows t DOESN’T know t Feels: INFORMED about options, benefits, risks VALUES [1 -10] Feels: CLEAR re personal import benefits/harms Pros 9***** know if has cancer 5***** early detection Cons 2** avoid surgery side effects 2** avoid worry from false alarm SUPPORT Feels: ENOUGH support and advice to make choice
 Washington State New Legislation Bill 5930 (May 2007) An act relating to providing high quality, affordable healthcare to Washingtonians based on the recommendations of the blue ribbon commission on health care costs and access • • if a patient/delegate signs an acknowledgement of shared decision making, such acknowledgement shall constitute evidence that the patient gave his or her informed consent to the treatment administered Acknowledgement of SDM includes: – Statement that patient and health care provider have engaged in SDM – Brief description of the services the patient and provider have jointly have agreed to – Brief description of the patient decision aid used – Statement that patient understands risks or seriousness of disease, available treatment alternatives (including non-tx), risks, benefits and uncertainties of treatment alternatives – Statement that patient had opportunity to ask the provider questions and have questions answered to patients’ satisfaction • SDM Def’n: process in which the physician or other health care practitioner discusses with the patient or his/her representative the information specified above with the use of a patient decision aid and the patient shares with the provider such relevant personal info as might make one treatment or side effect more or less tolerable than others
Washington State New Legislation Bill 5930 (May 2007) An act relating to providing high quality, affordable healthcare to Washingtonians based on the recommendations of the blue ribbon commission on health care costs and access • • if a patient/delegate signs an acknowledgement of shared decision making, such acknowledgement shall constitute evidence that the patient gave his or her informed consent to the treatment administered Acknowledgement of SDM includes: – Statement that patient and health care provider have engaged in SDM – Brief description of the services the patient and provider have jointly have agreed to – Brief description of the patient decision aid used – Statement that patient understands risks or seriousness of disease, available treatment alternatives (including non-tx), risks, benefits and uncertainties of treatment alternatives – Statement that patient had opportunity to ask the provider questions and have questions answered to patients’ satisfaction • SDM Def’n: process in which the physician or other health care practitioner discusses with the patient or his/her representative the information specified above with the use of a patient decision aid and the patient shares with the provider such relevant personal info as might make one treatment or side effect more or less tolerable than others
 Re-imbursement • Stop rewarding providers for utilization • Reward for shared decision making – Provider: pay for decision quality performance – Consumer: medical savings accounts; eliminating co-pay if Pt. DA used
Re-imbursement • Stop rewarding providers for utilization • Reward for shared decision making – Provider: pay for decision quality performance – Consumer: medical savings accounts; eliminating co-pay if Pt. DA used
 Achilles Heels shelf life of scientific evidence rapid response tools options clinically tailored, values-based matching strategies ‘face time’ plus competing demands ‘Ix’ solutions; Web 2. 0; automated coaching integrated in care pathways; preference diagnostic labs
Achilles Heels shelf life of scientific evidence rapid response tools options clinically tailored, values-based matching strategies ‘face time’ plus competing demands ‘Ix’ solutions; Web 2. 0; automated coaching integrated in care pathways; preference diagnostic labs
 Key Messages: Patient Decision Aids ñInformed decision making òOver-use of options that informed patients don’t value Challenge: implementation
Key Messages: Patient Decision Aids ñInformed decision making òOver-use of options that informed patients don’t value Challenge: implementation
 GOOGLE: ‘decision aid’
GOOGLE: ‘decision aid’


