15aa1b855c924b3455cc0508d8d7a6f4.ppt
- Количество слайдов: 38
Patient Centered Primary Care Collaborative Edwina Rogers Executive Director Patient Centered Primary Care Collaborative 601 Thirteenth St. , NW, Suite 400 North Washington, D. C. 20005 Direct: 202. 724. 3331 Mobile: 202. 674. 7800 erogers@pcpcc. net 1
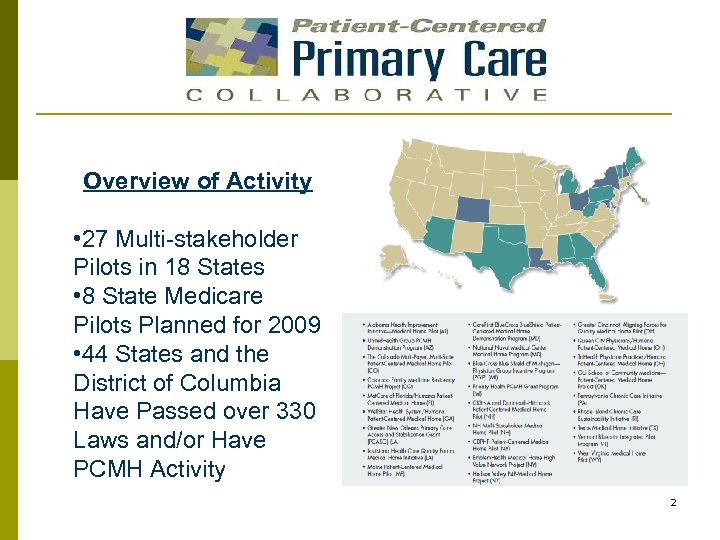
Overview of Activity • 27 Multi-stakeholder Pilots in 18 States • 8 State Medicare Pilots Planned for 2009 • 44 States and the District of Columbia Have Passed over 330 Laws and/or Have PCMH Activity 2
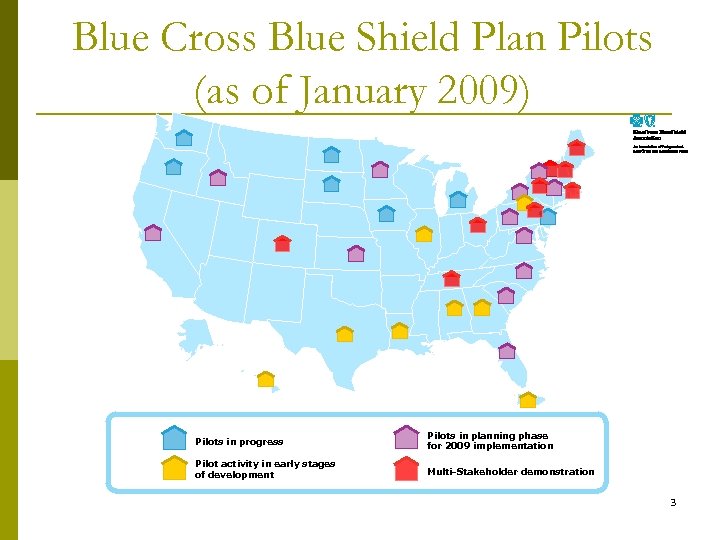
Blue Cross Blue Shield Plan Pilots (as of January 2009) Pilots in progress Pilots in planning phase for 2009 implementation Pilot activity in early stages of development Multi-Stakeholder demonstration 3
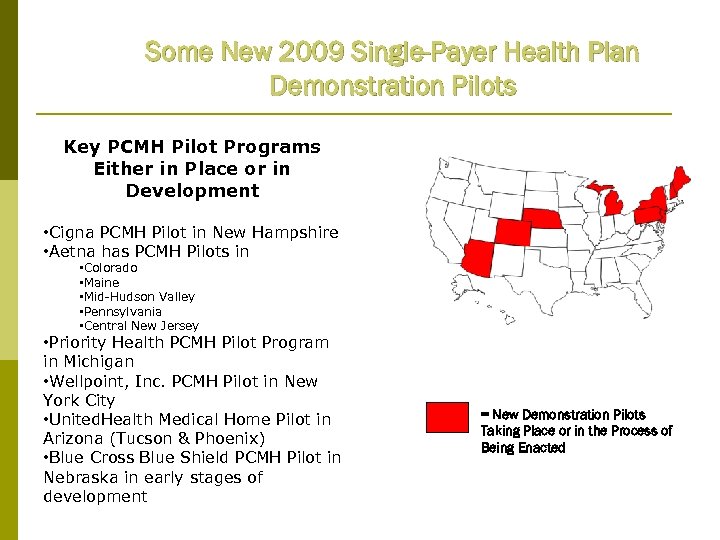
Some New 2009 Single-Payer Health Plan Demonstration Pilots Key PCMH Pilot Programs Either in Place or in Development • Cigna PCMH Pilot in New Hampshire • Aetna has PCMH Pilots in • Colorado • Maine • Mid-Hudson Valley • Pennsylvania • Central New Jersey • Priority Health PCMH Pilot Program in Michigan • Wellpoint, Inc. PCMH Pilot in New York City • United. Health Medical Home Pilot in Arizona (Tucson & Phoenix) • Blue Cross Blue Shield PCMH Pilot in Nebraska in early stages of development = New Demonstration Pilots Taking Place or in the Process of Being Enacted
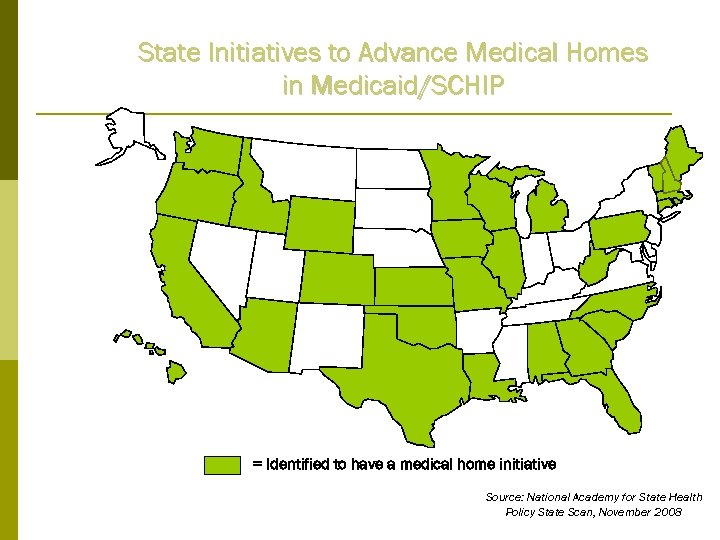
State Initiatives to Advance Medical Homes in Medicaid/SCHIP = Identified to have a medical home initiative Source: National Academy for State Health Policy State Scan, November 2008
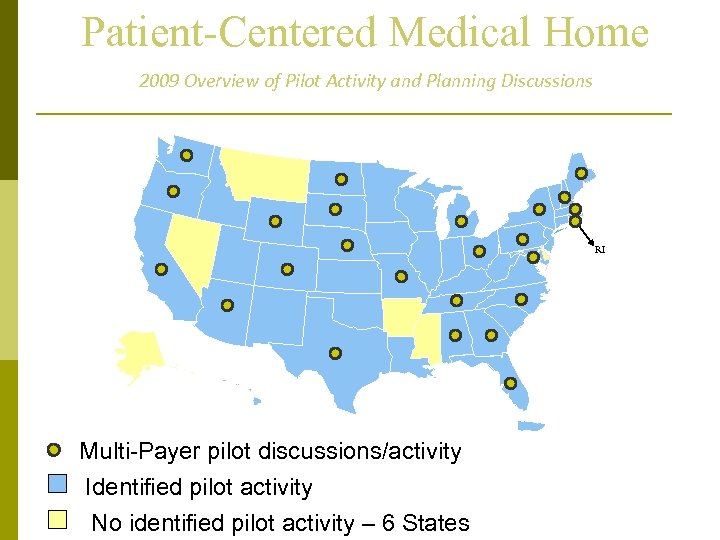
Patient-Centered Medical Home 2009 Overview of Pilot Activity and Planning Discussions RI Multi-Payer pilot discussions/activity Identified pilot activity No identified pilot activity – 6 States
Overview of the PCPCC p p p We are now in our 4 th year. Over 650 signing members Advancing the Patient Centered Medical Home (PCMH) concept in the public and private sectors Hosting Meetings, Summits and Congressional Briefings Weekly Call Thursday at 11: 00 AM EST n n p Call-in Number: 712. 432. 3900 Passcode: 471334# Weekly “Center” calls established to operationalize work of PCPCC 7
History of the Medical Home Concept p The first known documentation of the term “medical home” Standards of Child Health Care, AAP in 1967 by the AAP Council on Pediatric Practice -- “medical home -- one central source of a child’s pediatric records” History of the Medical Home Concept Calvin Sia, Thomas F. Tonniges, Elizabeth Osterhus and Sharon Taba Pediatrics 2004; 113; 14731478 p p p Patient Centered – IOM I would strongly urge the adoption of the Danish model of the Patient Centered Medical Home -- Karen Davis Commonwealth Fund 2009 Medical Home Wikipedia page: http: //en. wikipedia. org/wiki/Medical_home Henrik Jensen 8 Niels Rossing M. D.
Collaborative Principles The Patient Centered Primary Care Collaborative is a coalition of major employers, consumer groups, patient quality organizations, health plans, labor unions, hospitals, clinicians and many others who have joined together to develop and advance the patient centered medical home. The Collaborative believes that, if implemented, the patient centered medical home will improve the health of patients and the viability of the health care delivery system. In order to accomplish our goal, employers, consumers, patients, clinicians and payers have agreed that it is essential to support a better model of compensating clinicians. Compensation under the Patient-Centered Medical Home model would incorporate enhanced access and communication, improve coordination of care, rewards for higher value, expand administrative and quality innovations and promote active patient and family involvement. The Patient-Centered Medical Home model will also engage patients and their families in positive ongoing relationships with their clinicians. Further, the Patient-Centered Medical Home will improve the quality of care delivered and help control the unsustainable rising costs of healthcare for both individuals and plan-sponsors. If you agree, please visit us at www. pcpcc. net and join today! 9
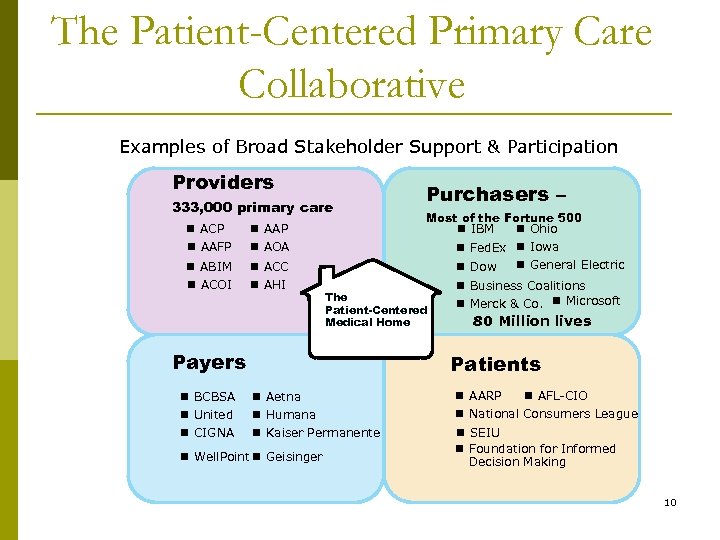
The Patient-Centered Primary Care Collaborative Examples of Broad Stakeholder Support & Participation Providers 333, 000 primary care n ACP n AAFP n AAP n AOA n ABIM n ACOI n ACC n AHI Most of the Fortune 500 n IBM n Ohio n Fed. Ex n Iowa n Dow The Patient-Centered Medical Home Payers n BCBSA n United n CIGNA Purchasers – n General Electric n Business Coalitions n Merck & Co. n Microsoft 80 Million lives Patients n Aetna n Humana n Kaiser Permanente n Well. Point n Geisinger n AARP n AFL-CIO n National Consumers League n SEIU n Foundation for Informed Decision Making 10
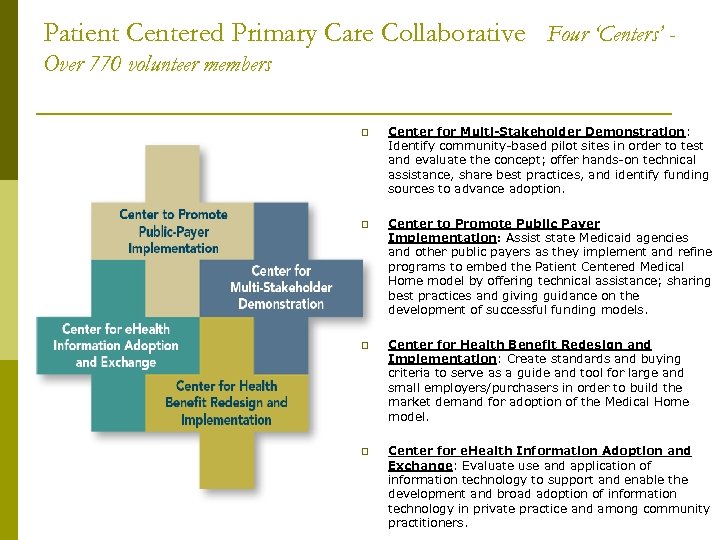
Patient Centered Primary Care Collaborative Four ‘Centers’ Over 770 volunteer members p Center for Multi-Stakeholder Demonstration: Identify community-based pilot sites in order to test and evaluate the concept; offer hands-on technical assistance, share best practices, and identify funding sources to advance adoption. p Center to Promote Public Payer Implementation: Assist state Medicaid agencies and other public payers as they implement and refine programs to embed the Patient Centered Medical Home model by offering technical assistance; sharing best practices and giving guidance on the development of successful funding models. p Center for Health Benefit Redesign and Implementation: Create standards and buying criteria to serve as a guide and tool for large and small employers/purchasers in order to build the market demand for adoption of the Medical Home model. p Center for e. Health Information Adoption and Exchange: Evaluate use and application of information technology to support and enable the development and broad adoption of information technology in private practice and among community practitioners. 9
JOINT PRINCIPLES OF THE PCMH (FEBRUARY 2007) The following principles were written and agreed upon by the four Primary Care Physician Organizations – the American Academy of Family Physicians, the American Academy of Pediatrics, the American College of Physicians, and the American Osteopathic Association. Principles: Ongoing relationship with personal physician Physician directed medical practice Whole person orientation Coordinated care across the health system Quality and safety Enhanced access to care Payment recognizes the value added 12
ENDORSEMENTS The PCMH Joint Principles have received endorsements from 18 specialty health care organizations: • The American Academy of Chest Physicians • The American Academy of Hospice and Palliative Medicine • The American Academy of Neurology • The American College of Cardiology • The American College of Osteopathic Family Physicians • The American College of Osteopathic Internists • The American Geriatrics Society • The American Medical Directors Association • The American Society of Addiction Medicine • The American Society of Clinical Oncology • The Society for Adolescent Medicine • The Society of Critical Care Medicine • The Society of General Internal Medicine • American Medical Association • Association of Professors of Medicine • Association of Program Directors in Internal Medicine • Clerkship Directors in Internal Medicine • Infectious Diseases Society of Medicine 13
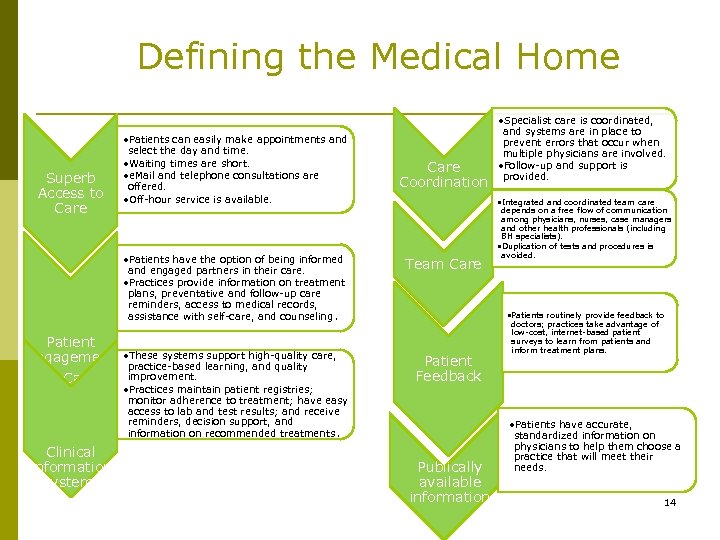
Defining the Medical Home Superb Access to Care • Patients can easily make appointments and select the day and time. • Waiting times are short. • e. Mail and telephone consultations are offered. • Off-hour service is available. • Patients have the option of being informed and engaged partners in their care. • Practices provide information on treatment plans, preventative and follow-up care reminders, access to medical records, assistance with self-care, and counseling. Patient Engagement • These systems support high-quality care, in Care practice-based learning, and quality improvement. • Practices maintain patient registries; monitor adherence to treatment; have easy access to lab and test results; and receive reminders, decision support, and information on recommended treatments. Clinical Information Systems Care Coordination • Integrated and coordinated team care Team Care depends on a free flow of communication among physicians, nurses, case managers and other health professionals (including BH specialists). • Duplication of tests and procedures is avoided. • Patients routinely provide feedback to Patient Feedback Publically available information Source: Health 2 Resources 9. 30. 08 • Specialist care is coordinated, and systems are in place to prevent errors that occur when multiple physicians are involved. • Follow-up and support is provided. doctors; practices take advantage of low-cost, internet-based patient surveys to learn from patients and inform treatment plans. • Patients have accurate, standardized information on physicians to help them choose a practice that will meet their needs. 14 8
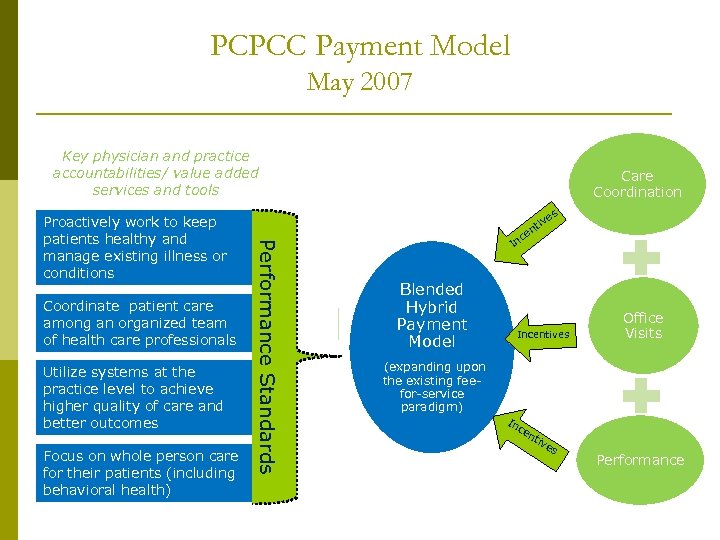
PCPCC Payment Model May 2007 Key physician and practice accountabilities/ value added services and tools Coordinate patient care among an organized team of health care professionals Utilize systems at the practice level to achieve higher quality of care and better outcomes Focus on whole person care for their patients (including behavioral health) es Performance Standards Proactively work to keep patients healthy and manage existing illness or conditions Care Coordination iv nt ce In Blended Hybrid Payment Model Incentives Office Visits (expanding upon the existing feefor-service paradigm) In ce nt ive s Performance 16
EVIDENCE OF COST SAVINGS & QUALITY IMPROVEMENT • Barbara Starfield of Johns Hopkins University • Within the United States, adults with a primary care physician rather than a specialist had 33 percent lower costs of care and were 19 percent less likely to die. • In both England the United States, each additional primary care physician per 10, 000 persons is associated with a decrease in mortality rate of 3 to 10 percent. • In the United States, an increase of just one primary care physician is associated with 1. 44 fewer deaths per 10, 000 persons. Commonwealth Fund has reported: • A medical home can reduce or even eliminate racial and ethnic disparities in access and quality for insured persons. Denmark has organized its entire health care system around patient-centered medical homes, achieving the highest patient satisfaction ratings in the world. Denmark has among the lowest per capita health expenditures and highest primary care rankings. Center for Evaluative Clinical Sciences at Dartmouth, states in the US relying more on primary care have: • lower Medicare spending, • lower resource inputs, • lower utilization, and • better quality of care. 16
EVIDENCE OF COST SAVINGS & QUALITY IMPROVEMENT This briefing document summarizes key findings from recent PCMH evaluation studies. Across these diverse settings and patient populations, evaluation findings consistently indicate that investments to redesign the delivery of care around a primary care PCMH yield an excellent return on investment: • Quality of care, patient experiences, care coordination, and access are demonstrably better. • Investments to strengthen primary care result within a relatively short time in reductions in emergency department visits and inpatient hospitalizations that produce savings in total costs. These savings at a minimum offset the new investments in primary care in a cost-neutral manner, and in many cases appear to produce a reduction in total costs per patient. 17
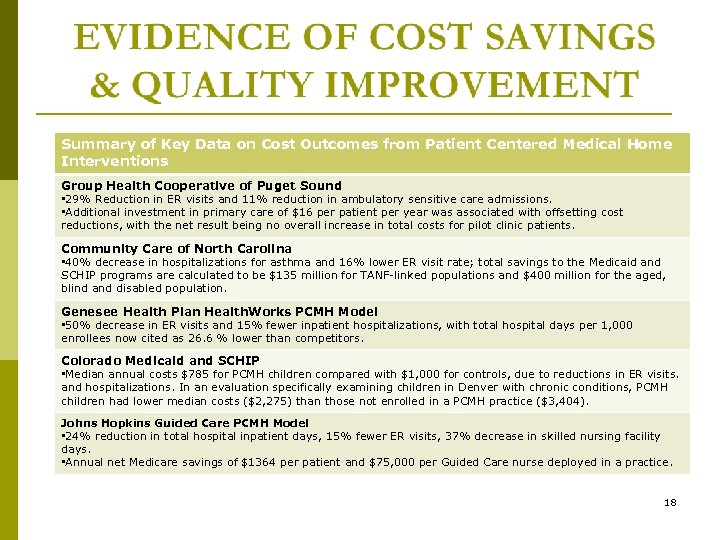
Summary of Key Data on Cost Outcomes from Patient Centered Medical Home Interventions Group Health Cooperative of Puget Sound • 29% Reduction in ER visits and 11% reduction in ambulatory sensitive care admissions. • Additional investment in primary care of $16 per patient per year was associated with offsetting cost reductions, with the net result being no overall increase in total costs for pilot clinic patients. Community Care of North Carolina • 40% decrease in hospitalizations for asthma and 16% lower ER visit rate; total savings to the Medicaid and SCHIP programs are calculated to be $135 million for TANF-linked populations and $400 million for the aged, blind and disabled population. Genesee Health Plan Health. Works PCMH Model • 50% decrease in ER visits and 15% fewer inpatient hospitalizations, with total hospital days per 1, 000 enrollees now cited as 26. 6 % lower than competitors. Colorado Medicaid and SCHIP • Median annual costs $785 for PCMH children compared with $1, 000 for controls, due to reductions in ER visits. and hospitalizations. In an evaluation specifically examining children in Denver with chronic conditions, PCMH children had lower median costs ($2, 275) than those not enrolled in a PCMH practice ($3, 404). Johns Hopkins Guided Care PCMH Model • 24% reduction in total hospital inpatient days, 15% fewer ER visits, 37% decrease in skilled nursing facility days. • Annual net Medicare savings of $1364 per patient and $75, 000 per Guided Care nurse deployed in a practice. 18
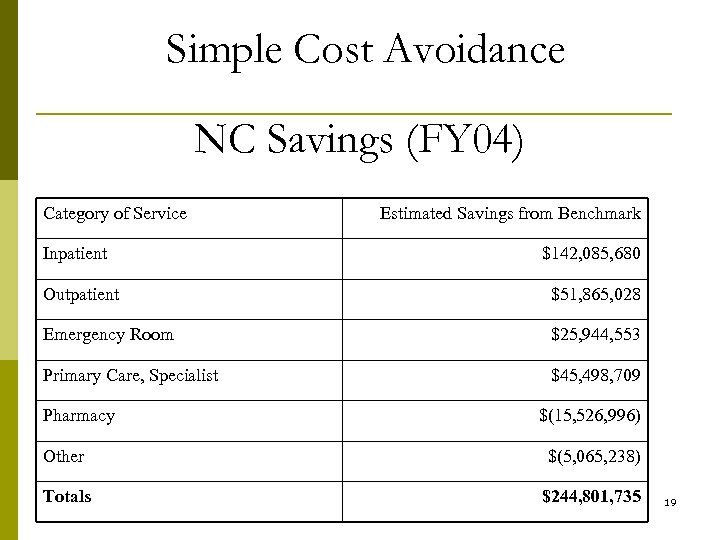
Simple Cost Avoidance NC Savings (FY 04) Category of Service Inpatient Estimated Savings from Benchmark $142, 085, 680 Outpatient $51, 865, 028 Emergency Room $25, 944, 553 Primary Care, Specialist $45, 498, 709 Pharmacy $(15, 526, 996) Other $(5, 065, 238) Totals $244, 801, 735 19
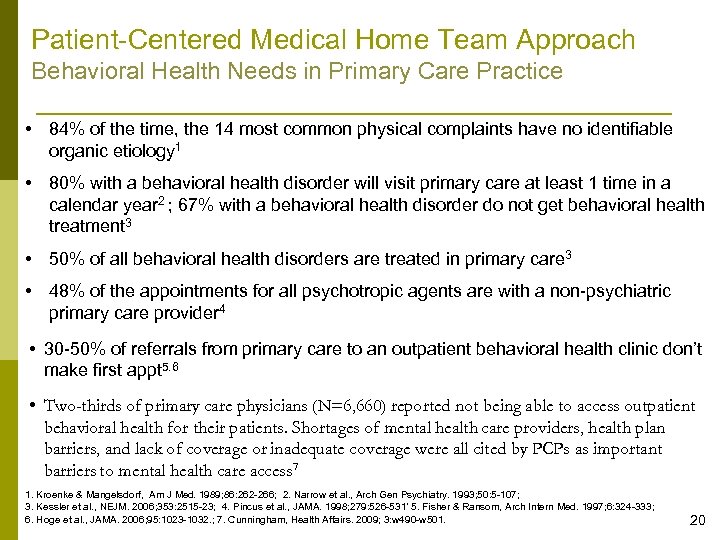
Patient-Centered Medical Home Team Approach Behavioral Health Needs in Primary Care Practice • 84% of the time, the 14 most common physical complaints have no identifiable organic etiology 1 • 80% with a behavioral health disorder will visit primary care at least 1 time in a calendar year 2 ; 67% with a behavioral health disorder do not get behavioral health treatment 3 • 50% of all behavioral health disorders are treated in primary care 3 • 48% of the appointments for all psychotropic agents are with a non-psychiatric primary care provider 4 • 30 -50% of referrals from primary care to an outpatient behavioral health clinic don’t make first appt 5. 6 • Two-thirds of primary care physicians (N=6, 660) reported not being able to access outpatient behavioral health for their patients. Shortages of mental health care providers, health plan barriers, and lack of coverage or inadequate coverage were all cited by PCPs as important barriers to mental health care access 7 1. Kroenke & Mangelsdorf, Am J Med. 1989; 86: 262 -266; 2. Narrow et al. , Arch Gen Psychiatry. 1993; 50: 5 -107; 3. Kessler et al. , NEJM. 2006; 353: 2515 -23; 4. Pincus et al. , JAMA. 1998; 279: 526 -531’ 5. Fisher & Ransom, Arch Intern Med. 1997; 6: 324 -333; 6. Hoge et al. , JAMA. 2006; 95: 1023 -1032. ; 7. Cunningham, Health Affairs. 2009; 3: w 490 -w 501. 20
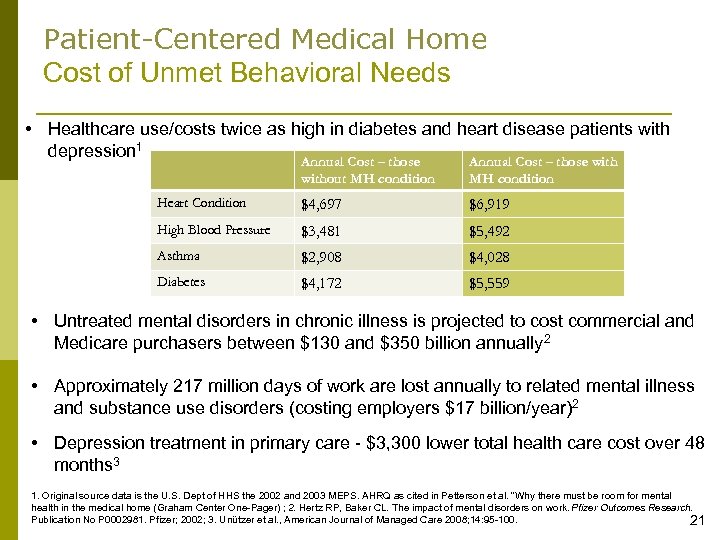
Patient-Centered Medical Home Cost of Unmet Behavioral Needs • Healthcare use/costs twice as high in diabetes and heart disease patients with depression 1 Annual Cost – those without MH condition Annual Cost – those with MH condition Heart Condition $4, 697 $6, 919 High Blood Pressure $3, 481 $5, 492 Asthma $2, 908 $4, 028 Diabetes $4, 172 $5, 559 • Untreated mental disorders in chronic illness is projected to cost commercial and Medicare purchasers between $130 and $350 billion annually 2 • Approximately 217 million days of work are lost annually to related mental illness and substance use disorders (costing employers $17 billion/year)2 • Depression treatment in primary care - $3, 300 lower total health care cost over 48 months 3 1. Original source data is the U. S. Dept of HHS the 2002 and 2003 MEPS. AHRQ as cited in Petterson et al. “Why there must be room for mental health in the medical home (Graham Center One-Pager) ; 2. Hertz RP, Baker CL. The impact of mental disorders on work. Pfizer Outcomes Research. Publication No P 0002981. Pfizer; 2002; 3. Unützer et al. , American Journal of Managed Care 2008; 14: 95 -100. 21
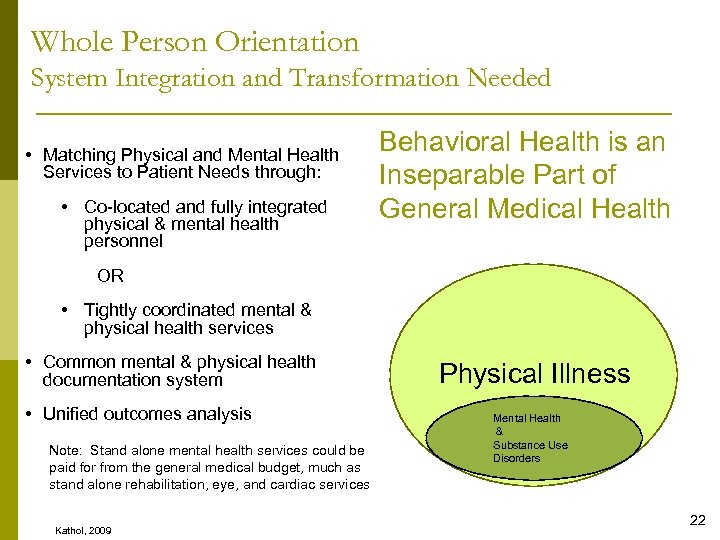
Whole Person Orientation System Integration and Transformation Needed • Matching Physical and Mental Health Services to Patient Needs through: • Co-located and fully integrated physical & mental health personnel Behavioral Health is an Inseparable Part of General Medical Health OR • Tightly coordinated mental & physical health services • Common mental & physical health documentation system • Unified outcomes analysis Note: Stand alone mental health services could be paid for from the general medical budget, much as stand alone rehabilitation, eye, and cardiac services Kathol, 2009 Physical Illness Mental Health & Substance Use Disorders 22
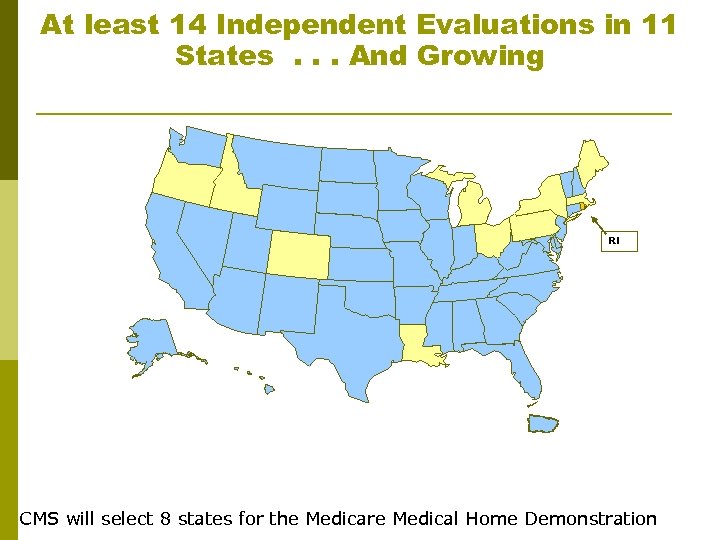
At least 14 Independent Evaluations in 11 States. . . And Growing RI CMS will select 8 states for the Medicare Medical Home Demonstration
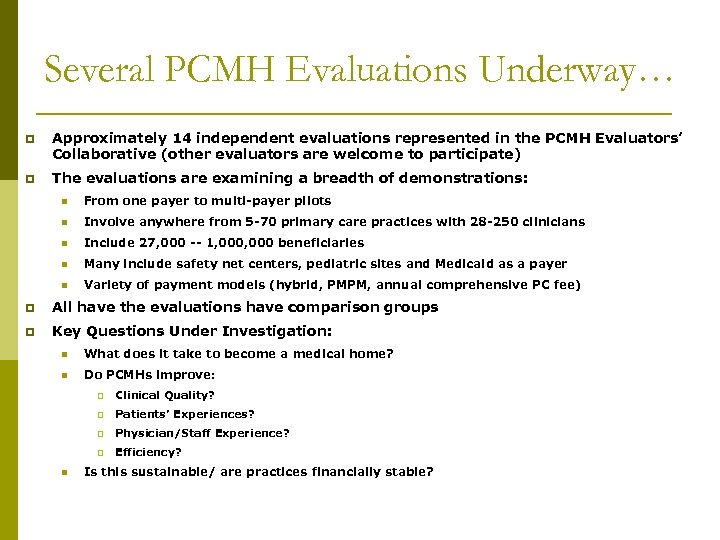
Several PCMH Evaluations Underway… p Approximately 14 independent evaluations represented in the PCMH Evaluators’ Collaborative (other evaluators are welcome to participate) p The evaluations are examining a breadth of demonstrations: n From one payer to multi-payer pilots n Involve anywhere from 5 -70 primary care practices with 28 -250 clinicians n Include 27, 000 -- 1, 000 beneficiaries n Many include safety net centers, pediatric sites and Medicaid as a payer n Variety of payment models (hybrid, PMPM, annual comprehensive PC fee) p All have the evaluations have comparison groups p Key Questions Under Investigation: n What does it take to become a medical home? n Do PCMHs improve: p p Patients’ Experiences? p Physician/Staff Experience? p n Clinical Quality? Efficiency? Is this sustainable/ are practices financially stable?
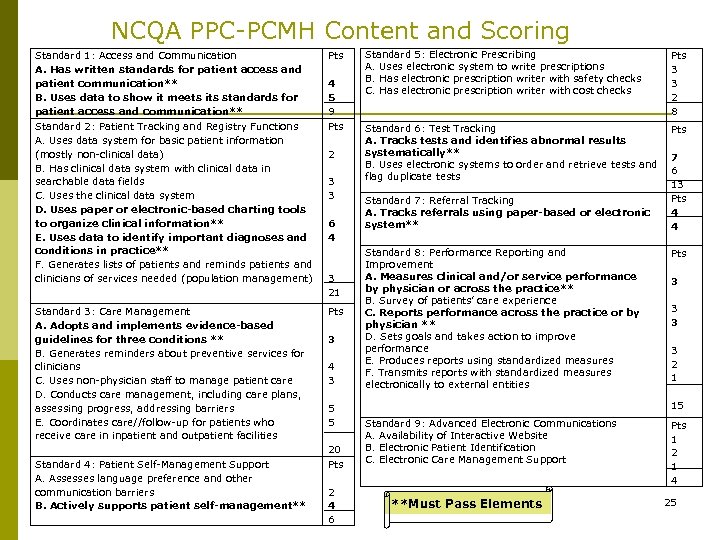
NCQA PPC-PCMH Content and Scoring Standard 1: Access and Communication A. Has written standards for patient access and patient communication** B. Uses data to show it meets its standards for patient access and communication** Pts Standard 2: Patient Tracking and Registry Functions A. Uses data system for basic patient information (mostly non-clinical data) B. Has clinical data system with clinical data in searchable data fields C. Uses the clinical data system D. Uses paper or electronic-based charting tools to organize clinical information** E. Uses data to identify important diagnoses and conditions in practice** F. Generates lists of patients and reminds patients and clinicians of services needed (population management) Pts Standard 3: Care Management A. Adopts and implements evidence-based guidelines for three conditions ** B. Generates reminders about preventive services for clinicians C. Uses non-physician staff to manage patient care D. Conducts care management, including care plans, assessing progress, addressing barriers E. Coordinates care//follow-up for patients who receive care in inpatient and outpatient facilities Pts Standard 4: Patient Self-Management Support A. Assesses language preference and other communication barriers B. Actively supports patient self-management** 4 5 9 2 3 3 6 4 3 21 3 4 3 5 5 20 Pts 2 4 6 Standard 5: Electronic Prescribing A. Uses electronic system to write prescriptions B. Has electronic prescription writer with safety checks C. Has electronic prescription writer with cost checks Pts 3 3 2 8 Standard 6: Test Tracking A. Tracks tests and identifies abnormal results systematically** B. Uses electronic systems to order and retrieve tests and flag duplicate tests Pts Standard 7: Referral Tracking A. Tracks referrals using paper-based or electronic system** Standard 8: Performance Reporting and Improvement A. Measures clinical and/or service performance by physician or across the practice** B. Survey of patients’ care experience C. Reports performance across the practice or by physician ** D. Sets goals and takes action to improve performance E. Produces reports using standardized measures F. Transmits reports with standardized measures electronically to external entities 7 6 13 Pts 4 4 Pts 3 3 2 1 15 Standard 9: Advanced Electronic Communications A. Availability of Interactive Website B. Electronic Patient Identification C. Electronic Care Management Support **Must Pass Elements Pts 1 2 1 4 25
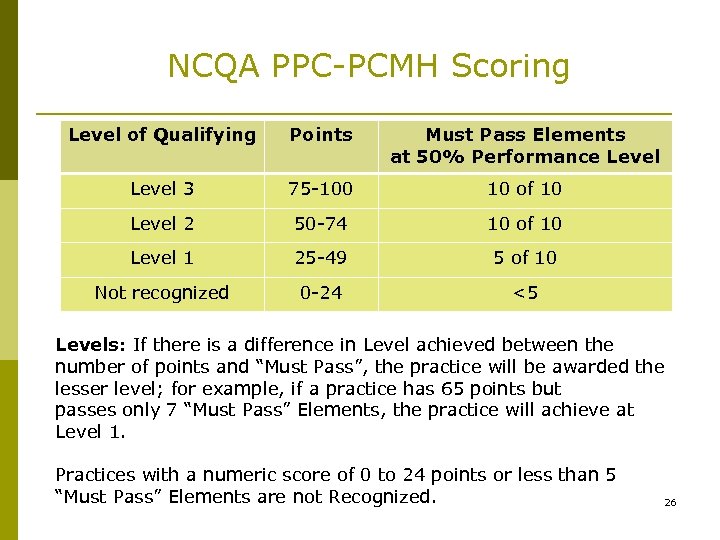
NCQA PPC-PCMH Scoring Level of Qualifying Points Must Pass Elements at 50% Performance Level 3 75 -100 10 of 10 Level 2 50 -74 10 of 10 Level 1 25 -49 5 of 10 Not recognized 0 -24 <5 Levels: If there is a difference in Level achieved between the number of points and “Must Pass”, the practice will be awarded the lesser level; for example, if a practice has 65 points but passes only 7 “Must Pass” Elements, the practice will achieve at Level 1. Practices with a numeric score of 0 to 24 points or less than 5 “Must Pass” Elements are not Recognized. 26
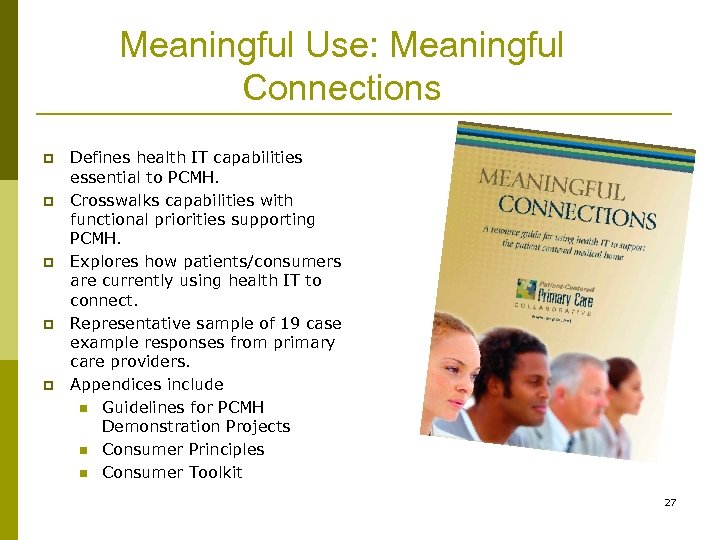
Meaningful Use: Meaningful Connections p p p Defines health IT capabilities essential to PCMH. Crosswalks capabilities with functional priorities supporting PCMH. Explores how patients/consumers are currently using health IT to connect. Representative sample of 19 case example responses from primary care providers. Appendices include n Guidelines for PCMH Demonstration Projects n Consumer Principles n Consumer Toolkit 27
Patient Centered Primary Care Collaborative “Purchaser Guide” Released July, 2008 p p p Developed by the PCPCC Center for Benefit Redesign and Implementation in partnership with NBCH and the Center’s multi-stakeholder advisory panel. Guide offers employers and buyers actionable steps as they work with health plans in local markets - over 6000 copies downloaded and/or distributed. Includes contract language, RFP language and overview of national pilots. Includes steps employers can take to involve themselves now in local market efforts. The PCPCC is holding a series of Webinars, sponsored by Pfizer, on the Purchaser Guide. 28 11
Patient Centered Primary Care Collaborative “Proof in Practice– A Compilation of Patient Centered Medical Home Pilot and Demonstration Projects” Released October 2009 p p Developed by the PCPCC Center for Multi-stakeholder Demonstration through a grant from AAFP offering a state-by-state sample of key pilot initiatives. Offers key contacts, project status, participating practices and market scan of covered lives; physicians. Inventory of : recognition program used, practice support (technology), project evaluation, and key resources. Begins to establish framework for program evaluation/ market tracking. 29 12
COLLABORATIVE “A COLLABORATIVE PARTNERSHIP – RESOURCES TO HELP CONSUMERS THRIVE IN THE MEDICAL HOME” RELEASED OCTOBER 2009 Included in the Guide: 1. PCPCC activities and initiatives supporting consumer engagement; 2. Research and examples surrounding consumer engagement in PCMH demonstrations; 3. Tools for consumers and other stakeholders to assist with PCMH education, engagement and partnerships; and 4. A catalogue of resources that provides descriptions of and the means to obtain potential resources for consumers, providers and purchasers seeking to better engage consumers. 30
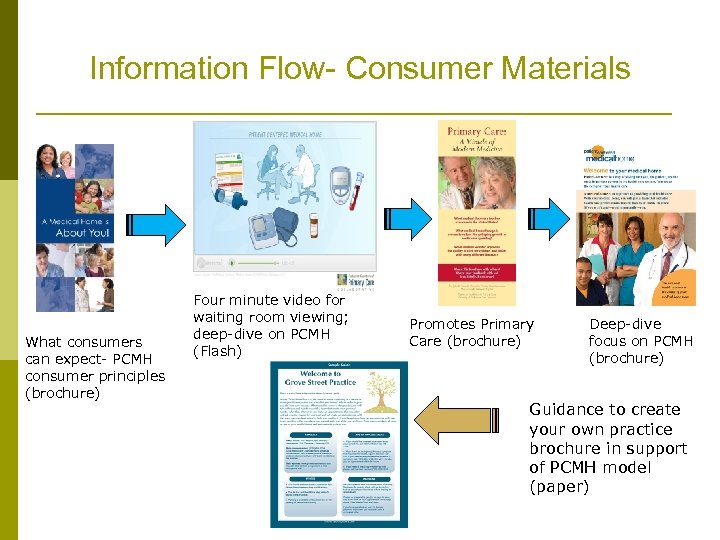
Information Flow- Consumer Materials What consumers can expect- PCMH consumer principles (brochure) Four minute video for waiting room viewing; deep-dive on PCMH (Flash) Promotes Primary Care (brochure) Deep-dive focus on PCMH (brochure) Guidance to create your own practice brochure in support of PCMH model (paper)
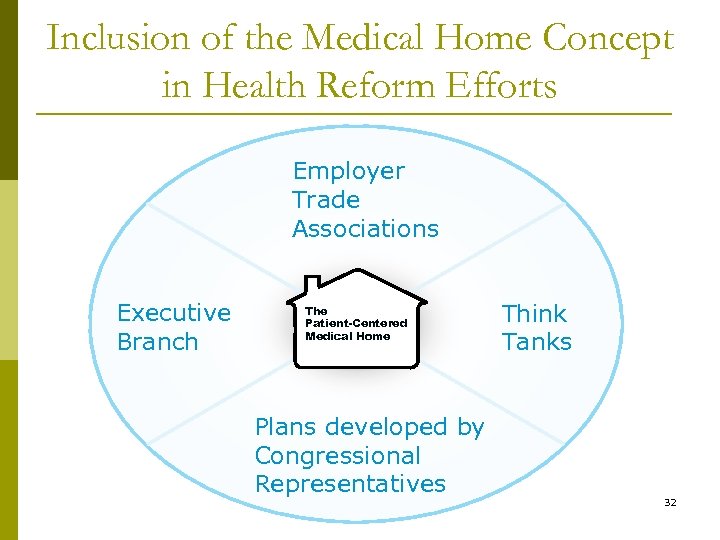
Inclusion of the Medical Home Concept in Health Reform Efforts Employer Trade Associations Executive Branch The Patient-Centered Medical Home Plans developed by Congressional Representatives Think Tanks 32
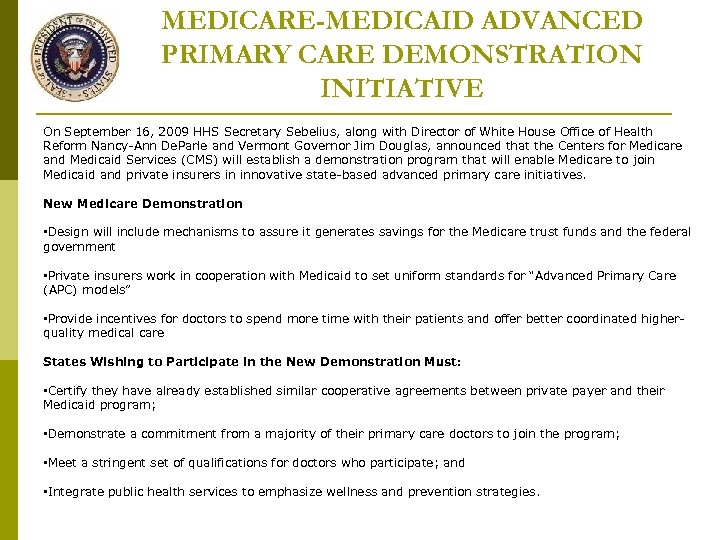
MEDICARE-MEDICAID ADVANCED PRIMARY CARE DEMONSTRATION INITIATIVE On September 16, 2009 HHS Secretary Sebelius, along with Director of White House Office of Health Reform Nancy-Ann De. Parle and Vermont Governor Jim Douglas, announced that the Centers for Medicare and Medicaid Services (CMS) will establish a demonstration program that will enable Medicare to join Medicaid and private insurers in innovative state-based advanced primary care initiatives. New Medicare Demonstration • Design will include mechanisms to assure it generates savings for the Medicare trust funds and the federal government • Private insurers work in cooperation with Medicaid to set uniform standards for “Advanced Primary Care (APC) models” • Provide incentives for doctors to spend more time with their patients and offer better coordinated higherquality medical care States Wishing to Participate in the New Demonstration Must: • Certify they have already established similar cooperative agreements between private payer and their Medicaid program; • Demonstrate a commitment from a majority of their primary care doctors to join the program; • Meet a stringent set of qualifications for doctors who participate; and • Integrate public health services to emphasize wellness and prevention strategies.
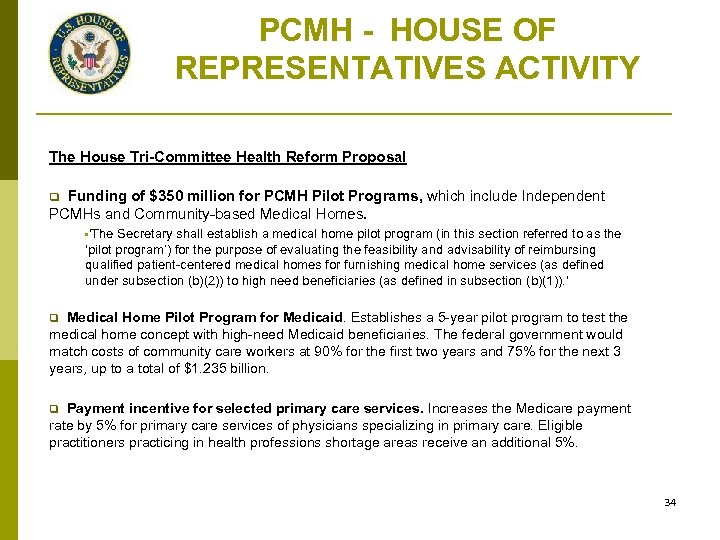
PCMH - HOUSE OF REPRESENTATIVES ACTIVITY The House Tri-Committee Health Reform Proposal Funding of $350 million for PCMH Pilot Programs, which include Independent PCMHs and Community-based Medical Homes. q • 'The Secretary shall establish a medical home pilot program (in this section referred to as the ‘pilot program’) for the purpose of evaluating the feasibility and advisability of reimbursing qualified patient-centered medical homes for furnishing medical home services (as defined under subsection (b)(2)) to high need beneficiaries (as defined in subsection (b)(1)). ' Medical Home Pilot Program for Medicaid. Establishes a 5 -year pilot program to test the medical home concept with high-need Medicaid beneficiaries. The federal government would match costs of community care workers at 90% for the first two years and 75% for the next 3 years, up to a total of $1. 235 billion. q Payment incentive for selected primary care services. Increases the Medicare payment rate by 5% for primary care services of physicians specializing in primary care. Eligible practitioners practicing in health professions shortage areas receive an additional 5%. q 34
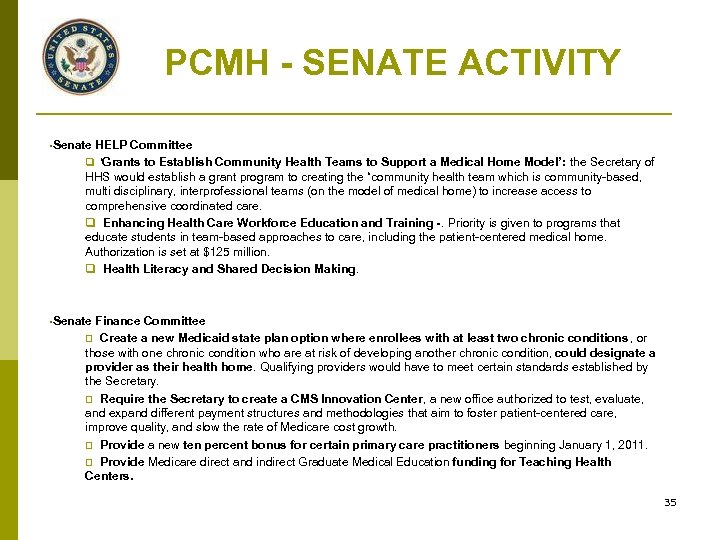
PCMH - SENATE ACTIVITY • Senate HELP Committee q ‘Grants to Establish Community Health Teams to Support a Medical Home Model’: the Secretary of HHS would establish a grant program to creating the “community health team which is community-based, multi disciplinary, interprofessional teams (on the model of medical home) to increase access to comprehensive coordinated care. q Enhancing Health Care Workforce Education and Training -. Priority is given to programs that educate students in team-based approaches to care, including the patient-centered medical home. Authorization is set at $125 million. q Health Literacy and Shared Decision Making. • Senate Finance Committee q Create a new Medicaid state plan option where enrollees with at least two chronic conditions , or those with one chronic condition who are at risk of developing another chronic condition, could designate a provider as their health home. Qualifying providers would have to meet certain standards established by the Secretary. q Require the Secretary to create a CMS Innovation Center, a new office authorized to test, evaluate, and expand different payment structures and methodologies that aim to foster patient-centered care, improve quality, and slow the rate of Medicare cost growth. q Provide a new ten percent bonus for certain primary care practitioners beginning January 1, 2011. q Provide Medicare direct and indirect Graduate Medical Education funding for Teaching Health Centers. 35
UPCOMING COLLABORATIVE EVENTS Tuesday, March 30, 2010 - Washington D. C. , Stakeholder Meeting - Ronald Reagan Building and International Trade Center Thursday, July 22, 2010 - Washington D. C. , Stakeholder Meeting - Ronald Reagan Building and International Trade Center Thursday, October 21, 2010 - Washington D. C. , Annual Summit - Ronald Reagan Building and International Trade Center 36
p www. pcpcc. net p About the PCPCC n n n n p History Members Brochure Executive Committee Advisory Board Officers Executive Bios The Patient Centered Medical Home n n n p Joint Principles Endorsements by Specialists Employer Perspectives Evidence of Quality Health Reform Proposal Reimbursement Model Collaborative Centers n n p Other PCMH Resources n n n p Center to Promote Public Payer Implementation Center for Multi-Stakeholder Demonstration Center for Benefits Redesign and Implementation Center for e. Health Information Exchange and Adoption Pilot Project Guide Purchasers Guide Evidence Documents Consumer Materials Events National Weekly Call n Thursday, 11: 00 AM EST 37
CONTACT INFORMATION Visit our website – http: //www. pcpcc. net To request any additional information on the PCMH or the Patient Centered Primary Care Collaborative please contact: Edwina Rogers Patient Centered Primary Care Collaborative Executive Director 202. 724. 3331 202. 674. 7800 (cell) erogers@pcpcc. net The Homer Building 601 Thirteenth St. , NW, Suite 400 North Washington, DC 20005 38
15aa1b855c924b3455cc0508d8d7a6f4.ppt