1afeef0af131844e2edab9872662b854.ppt
- Количество слайдов: 42
Patient Assessment
Objectives • Students will: – Identify normal and abnormal V/S measurements. – Measure and record vital signs according to industry standards. – Measure and record height and weight according to industry standards. – Explain why urine, stool, and sputum specimens are collected. – Explain the rules for collecting different specimens – Describe the seven warning signs of cancer
Vital Signs • • Are important indicators of health Detect changes in normal body function May signal life-threatening conditions Provide information about responses to treatment
Vital Signs • Temperature • Pulse • Respirations • Blood Pressure
Vital Signs Are Measured: – Upon admission – As often as required by the person’s condition – Before & after surgery and other procedures – After a fall or accident – When prescribed drugs that affect the respiratory or circulatory system – When there are complaints of pain, dizziness, shortness of breath, chest pain – As stated on the care plan
When Measuring Vital Signs • Usually taken with the person sitting or lying • The person is at rest • Always report: – A change from a previous measurement – Vital signs above or below the normal range – If you are unable to measure the vital signs
Temperature • Measurement of balance between heat lost and produced by the body. – Heat is produced by: • Metabolism of food • Muscle and gland activity – Heat may be lost through: • Perspiration, Respiration, Excretion • Measured with the Fahrenheit (F) or Celsius or Centigrade (C) scales
Body Temperature • Factors that body temperature Illness Infection Exercise Excitement High temperatures in the environment • Temperature is usually higher in the evening • • • Starvation or fasting Sleep Decreased muscle activity Exposure to cold in the environment
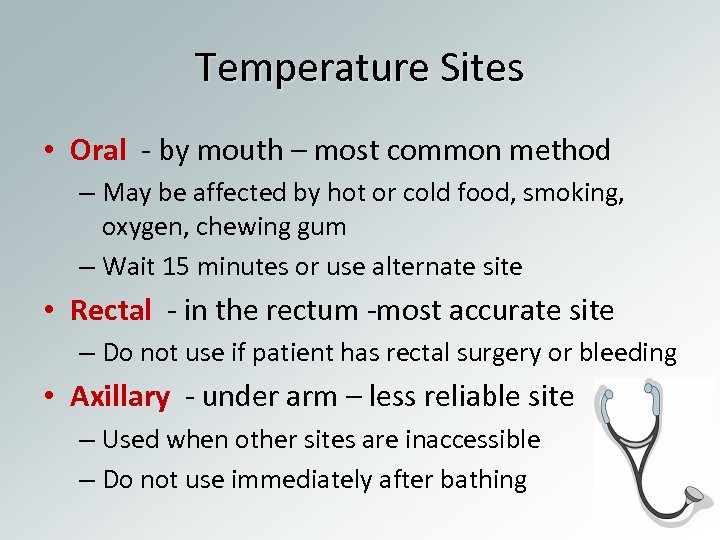
Temperature Sites • Oral - by mouth – most common method – May be affected by hot or cold food, smoking, oxygen, chewing gum – Wait 15 minutes or use alternate site • Rectal - in the rectum -most accurate site – Do not use if patient has rectal surgery or bleeding • Axillary - under arm – less reliable site – Used when other sites are inaccessible – Do not use immediately after bathing
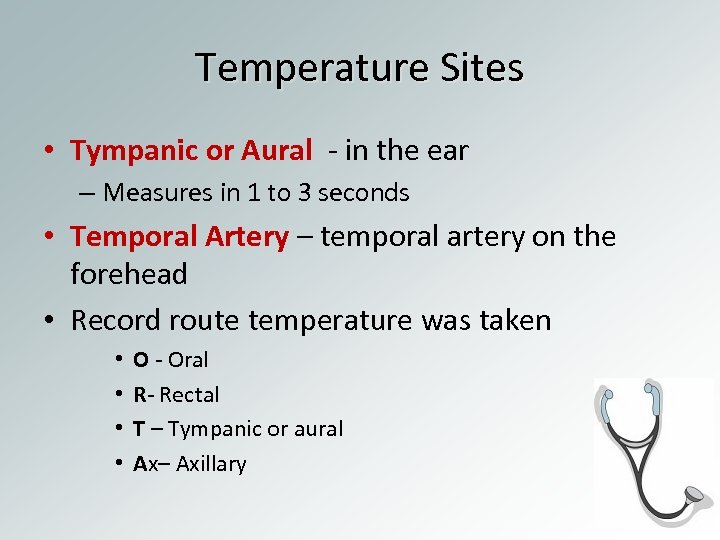
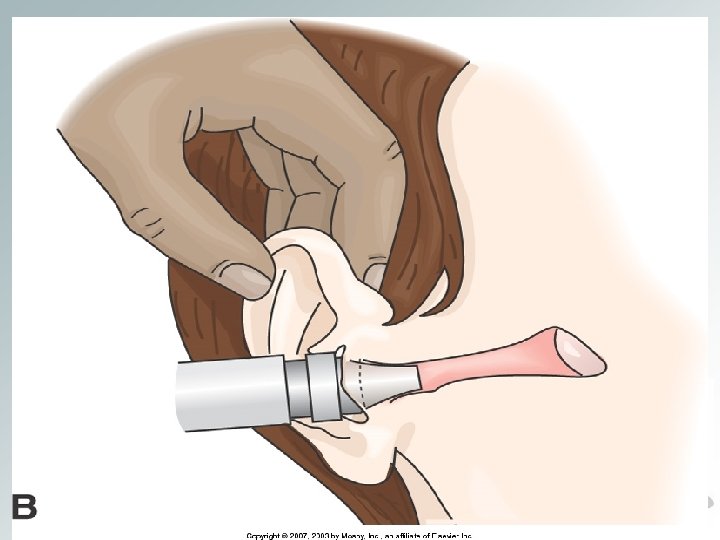
Temperature Sites • Tympanic or Aural - in the ear – Measures in 1 to 3 seconds • Temporal Artery – temporal artery on the forehead • Record route temperature was taken • • O - Oral R- Rectal T – Tympanic or aural Ax– Axillary
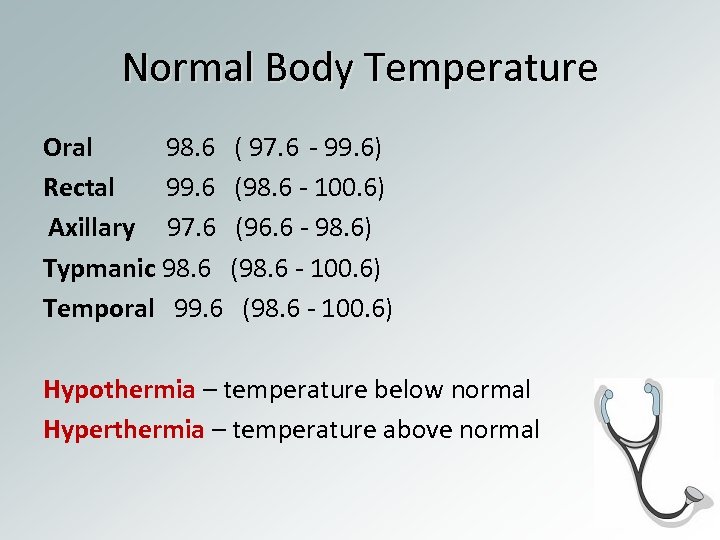
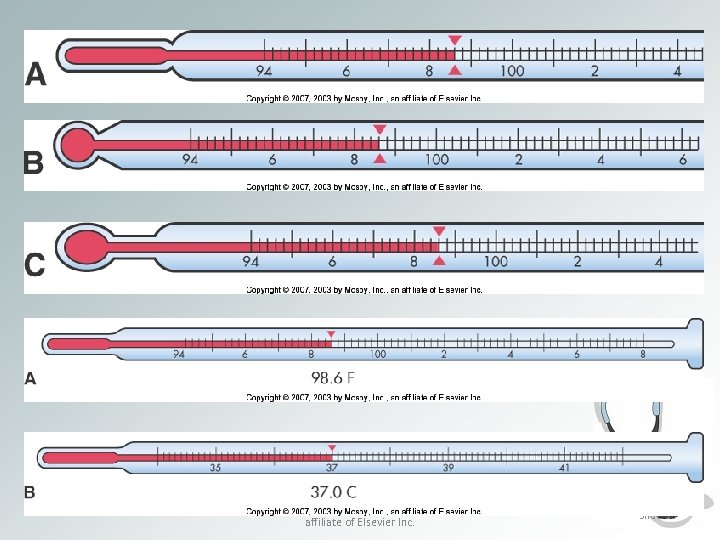
Normal Body Temperature Oral 98. 6 ( 97. 6 - 99. 6) Rectal 99. 6 (98. 6 - 100. 6) Axillary 97. 6 (96. 6 - 98. 6) Typmanic 98. 6 (98. 6 - 100. 6) Temporal 99. 6 (98. 6 - 100. 6) Hypothermia – temperature below normal Hyperthermia – temperature above normal
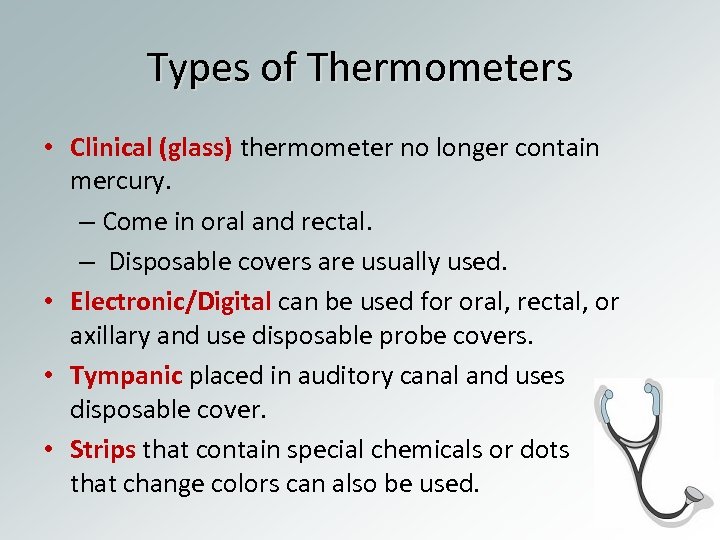
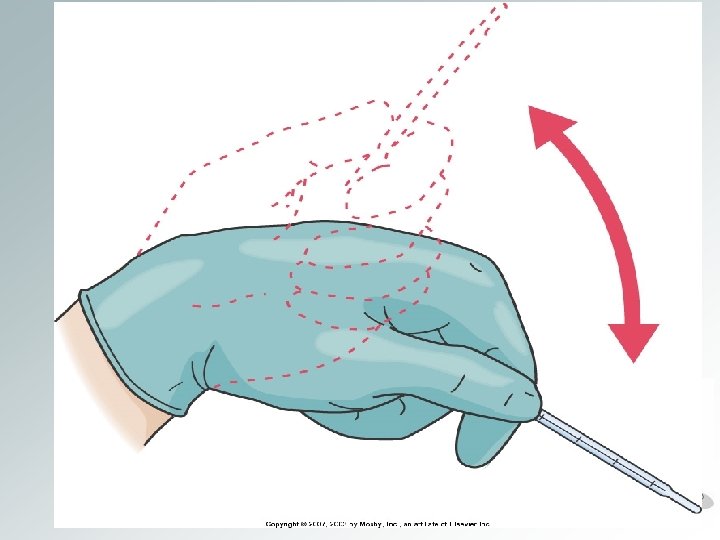
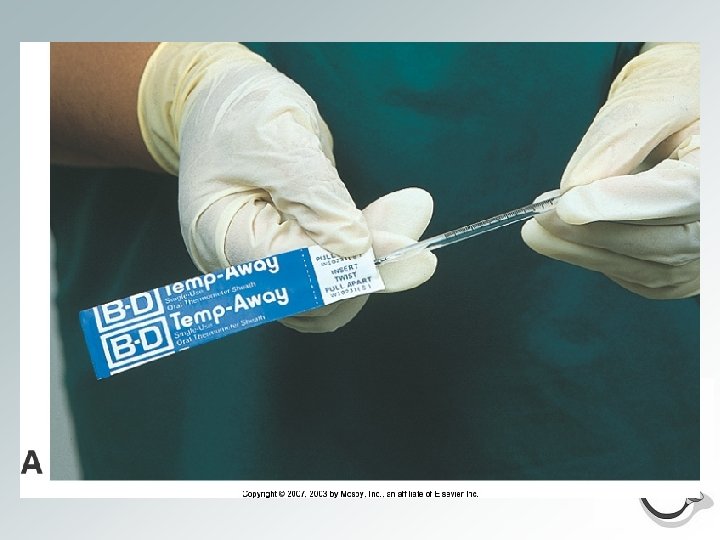
Types of Thermometers • Clinical (glass) thermometer no longer contain mercury. – Come in oral and rectal. – Disposable covers are usually used. • Electronic/Digital can be used for oral, rectal, or axillary and use disposable probe covers. • Tympanic placed in auditory canal and uses disposable cover. • Strips that contain special chemicals or dots that change colors can also be used.
Copyright © 2007, 2003 by Mosby, Inc. , an affiliate of Elsevier Inc. Slide 13



Electronic/ Digital Thermometer
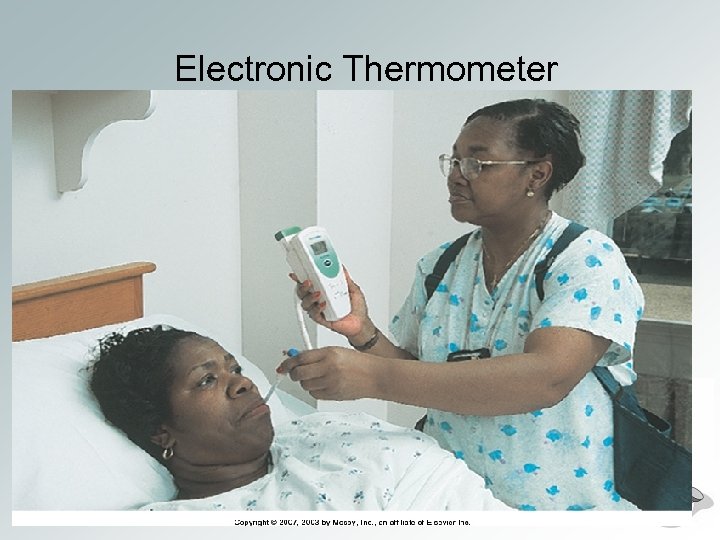
Electronic Thermometer
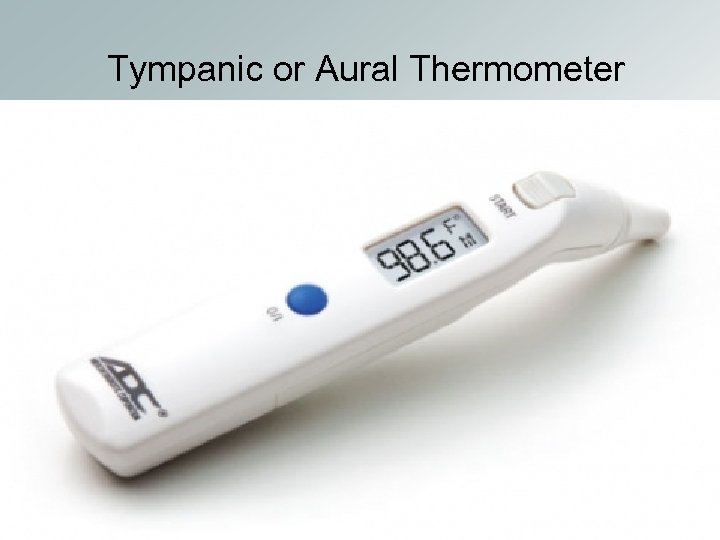
Tympanic or Aural Thermometer
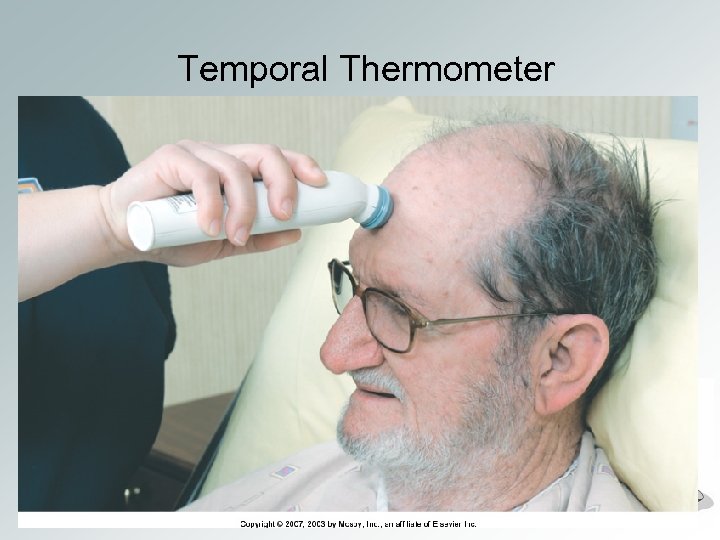
Temporal Thermometer
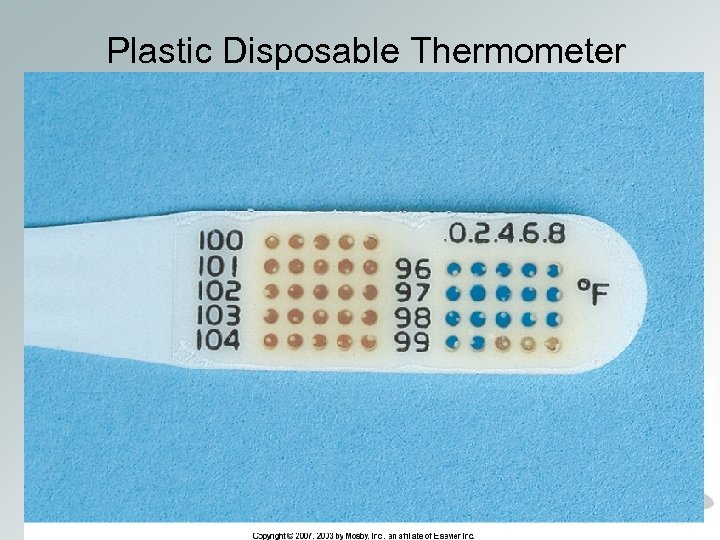
Plastic Disposable Thermometer
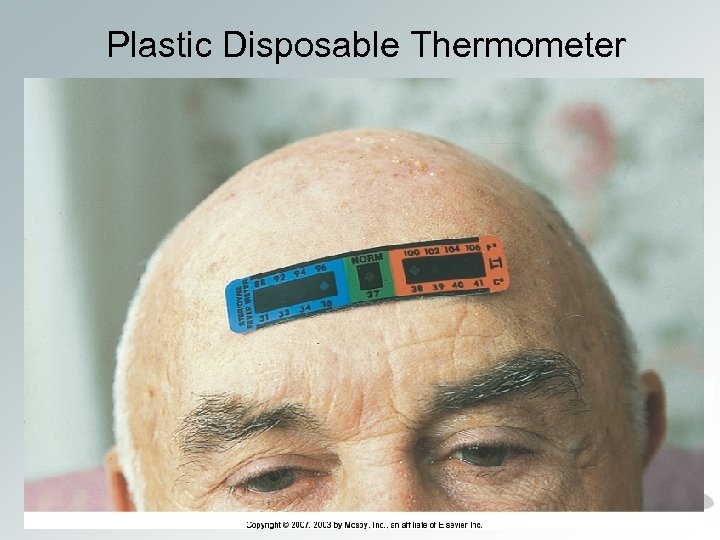
Plastic Disposable Thermometer
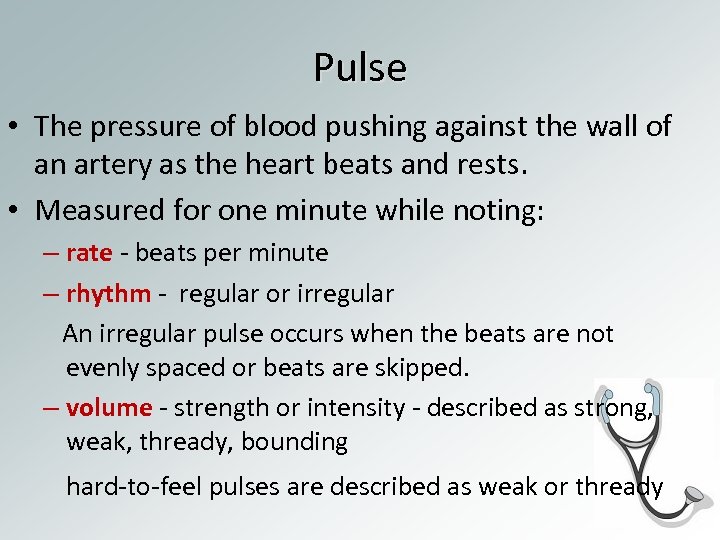
Pulse • The pressure of blood pushing against the wall of an artery as the heart beats and rests. • Measured for one minute while noting: – rate - beats per minute – rhythm - regular or irregular An irregular pulse occurs when the beats are not evenly spaced or beats are skipped. – volume - strength or intensity - described as strong, weak, thready, bounding hard-to-feel pulses are described as weak or thready
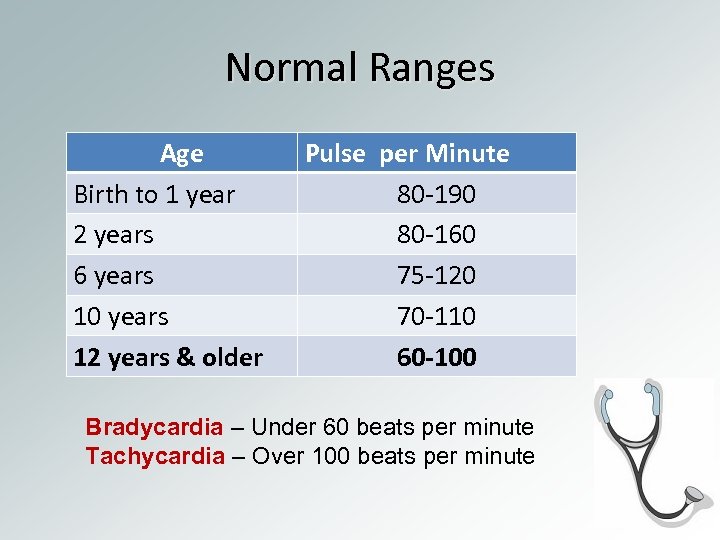
Normal Ranges Age Birth to 1 year 2 years 6 years 10 years 12 years & older Pulse per Minute 80 -190 80 -160 75 -120 70 -110 60 -100 Bradycardia – Under 60 beats per minute Tachycardia – Over 100 beats per minute
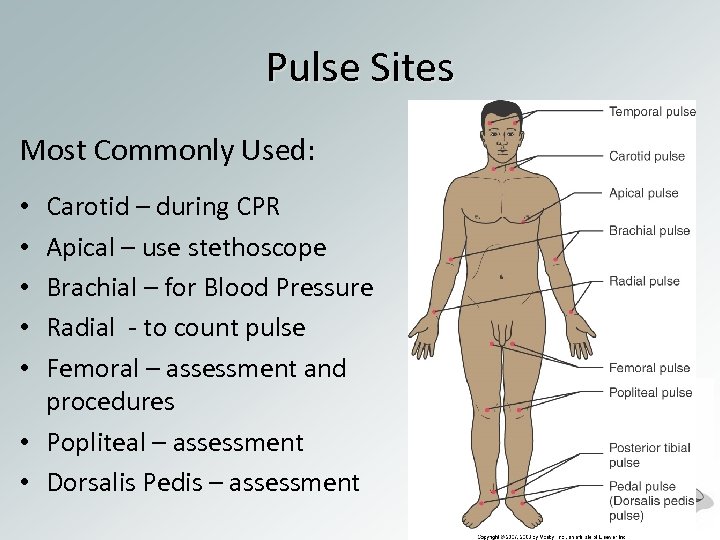
Pulse Sites Most Commonly Used: Carotid – during CPR Apical – use stethoscope Brachial – for Blood Pressure Radial - to count pulse Femoral – assessment and procedures • Popliteal – assessment • Dorsalis Pedis – assessment • • •
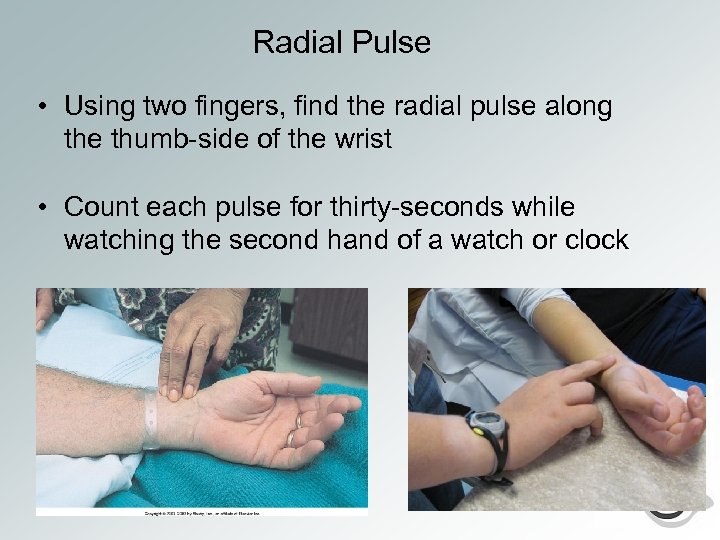
Radial Pulse • Using two fingers, find the radial pulse along the thumb-side of the wrist • Count each pulse for thirty-seconds while watching the second hand of a watch or clock
– The apical pulse is on the left side of the chest slightly below the nipple. • It is taken with a stethoscope. • Count the apical pulse for 1 minute. • Count each lub-dub as one beat. – The apical and radial pulses should be equal. • To see if the apical and radial pulses are equal, two staff members are needed. • The pulse deficit is the difference between the apical and radial pulse rates. Copyright © 2007, 2003 by Mosby, Inc. , an affiliate of Elsevier Inc. Slide 30
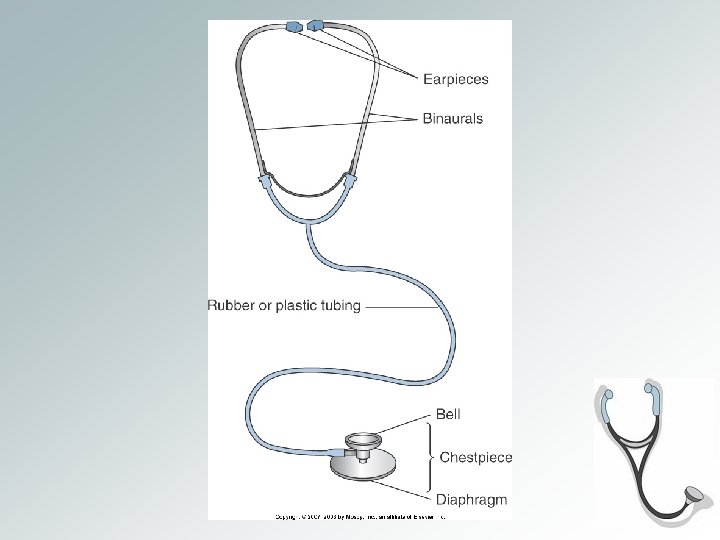
• To use a stethoscope: q. Wipe the earpieces and diaphragm with antiseptic wipes before and after use. • Place the earpiece tips in your ears. • Place the diaphragm over the artery. • Prevent noise. Copyright © 2007, 2003 by Mosby, Inc. , an affiliate of Elsevier Inc. Slide 32

Factors that Affect Pulse • • Factors that pulse Exercise Stimulant drugs Excitement Fever Shock Nervous tension • • • Factors that pulse Sleep Depressant drugs Heart disease Coma
Respirations • Process of breathing air into (inhalation) and out of (exhalation) the lungs. • Oxygen enters the lungs during inhalation. • Carbon dioxide leaves the lungs during exhalation. • The chest rises during inhalation and falls during exhalation. • Normal rate 12 -20 breaths per minute
Assessing Respiration • Respirations are normally quiet, effortless, and regular • Respirations is measured when the person is at rest. • Rate may change is patient is aware that it is being counted. • To prevent this, count respirations right after taking a pulse. q. Keep your fingers or stethoscope over the pulse site. q. Do not tell the patient that you are counting respirations • One respiration equals one inspiration (rise of the chest) and one exhalation (fall of the chest)
Assessing Respiration • Character and quality of respirations is also assessed: – – – Deep Shallow Labored or difficult Noises – wheezing, stertorous (a heavy, snoring type of sound) Moist or rattling sounds • Dyspnea – difficult or labored breathing • Apnea – absence of respirations • Cheyne-Stokes – periods of dyspnea followed by periods of apnea; often noted in the dying patient • Rales – bubbling or noisy sounds caused by fluids or mucus in the air passages
Blood Pressure • Measure of the pressure blood exerts on the walls of arteries • Blood pressure is controlled by: – The force of heart contractions • weakened heart drop in BP – The amount of blood pumped with each heartbeat • loss of blood drop in BP – How easily the blood flows through the blood vessels • Narrowing of vessels increase in BP • Dilatation of vessels decrease in BP
Factors that Affect Blood Pressure Factors that blood pressure • Excitement, anxiety, nervous tension • Stimulant drugs • Exercise and eating Factors that blood pressure • Rest or sleep • Depressant drugs • Shock • Excessive loss of blood
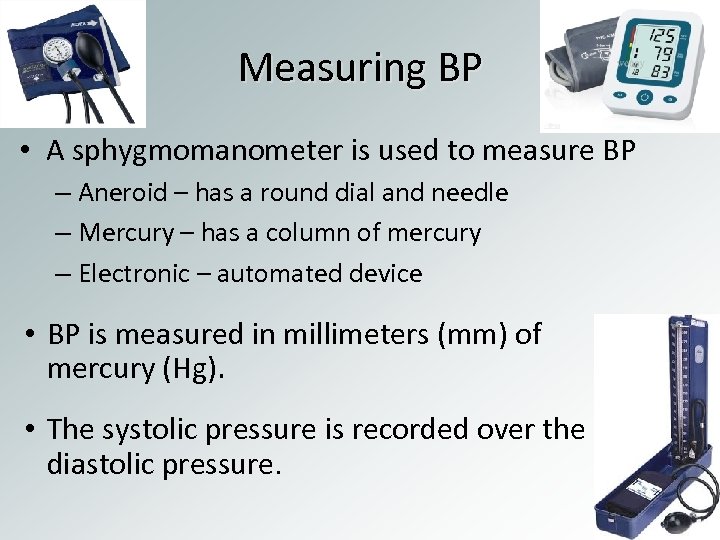
Measuring BP • A sphygmomanometer is used to measure BP – Aneroid – has a round dial and needle – Mercury – has a column of mercury – Electronic – automated device • BP is measured in millimeters (mm) of mercury (Hg). • The systolic pressure is recorded over the diastolic pressure.
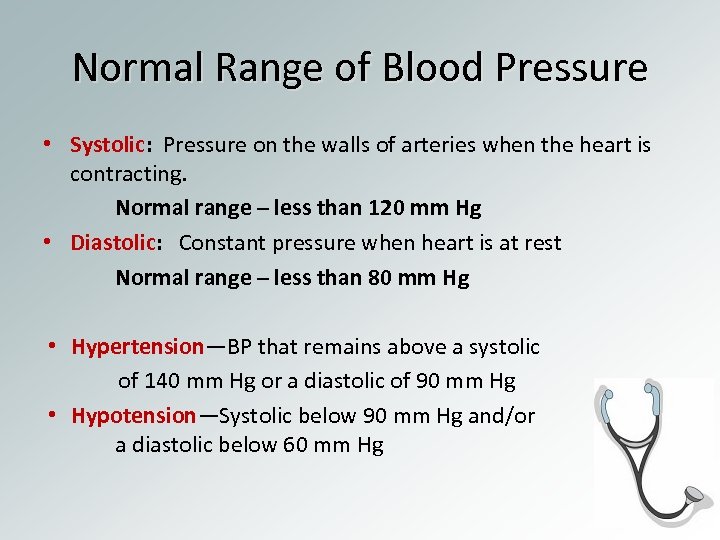
Normal Range of Blood Pressure • Systolic: Pressure on the walls of arteries when the heart is contracting. Normal range – less than 120 mm Hg • Diastolic: Constant pressure when heart is at rest Normal range – less than 80 mm Hg • Hypertension—BP that remains above a systolic of 140 mm Hg or a diastolic of 90 mm Hg • Hypotension—Systolic below 90 mm Hg and/or a diastolic below 60 mm Hg
https: //www. youtube. com/watch? v=RAGxm 32 f tb. U
1afeef0af131844e2edab9872662b854.ppt