8785ac2f7abdc499a45c0bb96f30beee.ppt
- Количество слайдов: 70
 Parent / Carer Mental Illness and the potential impact for dependant children Vicky Finch Jo Farthing-Bell
Parent / Carer Mental Illness and the potential impact for dependant children Vicky Finch Jo Farthing-Bell
 Ground Rules Respect Confidentiality responsibility
Ground Rules Respect Confidentiality responsibility
 Aims and Objectives Aim: To be introduced to the key features associated with common mental health problems and consider how parent/carer mental health problems may impact on the child and family. By the end of the training participants will: Have a basic understanding of common mental health problems and be able to describe some of the associated features. Have an opportunity to explore the impact of parental/carer mental illness on children through the use of practical activities and case scenarios. Consider their role in supporting and working in partnership with families and agencies to promote good outcomes for children living in families where parent /carer mental illness is present. Be able to identify factors associated with parent /carer mental illness that indicate a child or young person may be at risk of significant harm and know what procedures to follow.
Aims and Objectives Aim: To be introduced to the key features associated with common mental health problems and consider how parent/carer mental health problems may impact on the child and family. By the end of the training participants will: Have a basic understanding of common mental health problems and be able to describe some of the associated features. Have an opportunity to explore the impact of parental/carer mental illness on children through the use of practical activities and case scenarios. Consider their role in supporting and working in partnership with families and agencies to promote good outcomes for children living in families where parent /carer mental illness is present. Be able to identify factors associated with parent /carer mental illness that indicate a child or young person may be at risk of significant harm and know what procedures to follow.
 Learning lessons, taking action: Key messages from SCR’s Parental mental health problems were identified as a factor in over half of a sample of 33 serious case reviews in England from 2009 -2010 (Brandon, 2011) Mental illness was a feature in families with long standing concerns but also in the background of families where there were no current concerns Learning difficulties and/or disabilities were often linked with mental health issues for both parents and the children. Poor mental health affects 25% - 40% of adults with a learning disability Concerns about drug and alcohol misuse were identified in 17 reviews. Concerns about domestic violence featured in 15 serious case reviews. Some parents were receiving support from agencies in their own right, including from services for adult social care, adult mental health, substance misuse, housing and probation. These agencies were found to have held important information about the family circumstances, but too often this was not shared early enough.
Learning lessons, taking action: Key messages from SCR’s Parental mental health problems were identified as a factor in over half of a sample of 33 serious case reviews in England from 2009 -2010 (Brandon, 2011) Mental illness was a feature in families with long standing concerns but also in the background of families where there were no current concerns Learning difficulties and/or disabilities were often linked with mental health issues for both parents and the children. Poor mental health affects 25% - 40% of adults with a learning disability Concerns about drug and alcohol misuse were identified in 17 reviews. Concerns about domestic violence featured in 15 serious case reviews. Some parents were receiving support from agencies in their own right, including from services for adult social care, adult mental health, substance misuse, housing and probation. These agencies were found to have held important information about the family circumstances, but too often this was not shared early enough.
 What is Mental Illness ? ‘Mental illness is a mental physical, social, existential experience in which the individual is making sense of and working out how to survive’ (Seedhouse , 2002) ‘. . . mental health is not simply the absence of disease’ (WHO, 2006) any of various disorders in which a person's thoughts, emotions, or behaviour are so abnormal as to cause suffering to himself, herself, or other people (collins english dictionary) ‘ those whose symptoms are ‘sub-threshold’ are often viewed as having poor prognosis’ (Middleton and Shaw, 2000)
What is Mental Illness ? ‘Mental illness is a mental physical, social, existential experience in which the individual is making sense of and working out how to survive’ (Seedhouse , 2002) ‘. . . mental health is not simply the absence of disease’ (WHO, 2006) any of various disorders in which a person's thoughts, emotions, or behaviour are so abnormal as to cause suffering to himself, herself, or other people (collins english dictionary) ‘ those whose symptoms are ‘sub-threshold’ are often viewed as having poor prognosis’ (Middleton and Shaw, 2000)
 Prevalance About a quarter of the population will experience some kind of mental health problem in the course of a year, with mixed anxiety and depression the most common mental disorder in Britain Women are more likely to have been treated for a mental health problem than men and about ten percent of children have a mental health problem at any one time Depression affects 1 in 5 older people
Prevalance About a quarter of the population will experience some kind of mental health problem in the course of a year, with mixed anxiety and depression the most common mental disorder in Britain Women are more likely to have been treated for a mental health problem than men and about ten percent of children have a mental health problem at any one time Depression affects 1 in 5 older people
 Suicides rates show that British men are three times as likely to die by suicide than British women and selfharm statistics for the UK show one of the highest rates in Europe: 400 per 100, 000 population Only 1 in 10 prisoners has no mental disorder. Anxiety is one of the most prevalent mental health problems in the UK and elsewhere, yet it is still underreported, under-diagnosed and under-treated. (source: Mental Health Foundation)
Suicides rates show that British men are three times as likely to die by suicide than British women and selfharm statistics for the UK show one of the highest rates in Europe: 400 per 100, 000 population Only 1 in 10 prisoners has no mental disorder. Anxiety is one of the most prevalent mental health problems in the UK and elsewhere, yet it is still underreported, under-diagnosed and under-treated. (source: Mental Health Foundation)
 Types of Mental Health difficulties that people face
Types of Mental Health difficulties that people face
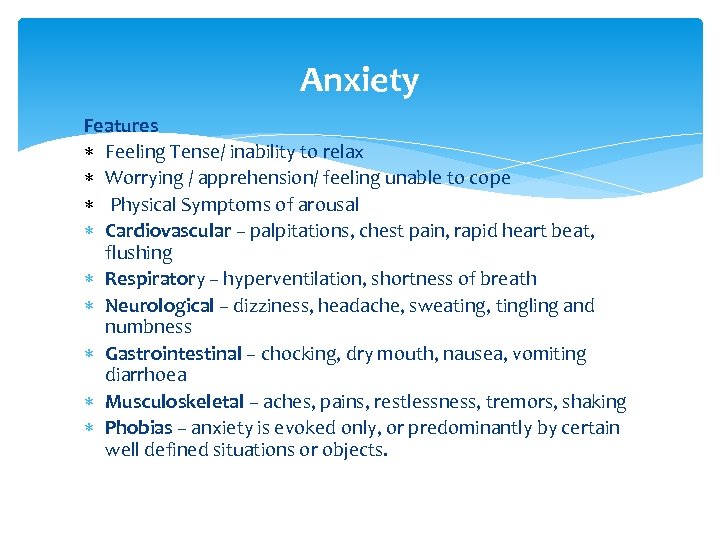 Anxiety Features Feeling Tense/ inability to relax Worrying / apprehension/ feeling unable to cope Physical Symptoms of arousal Cardiovascular – palpitations, chest pain, rapid heart beat, flushing Respiratory – hyperventilation, shortness of breath Neurological – dizziness, headache, sweating, tingling and numbness Gastrointestinal – chocking, dry mouth, nausea, vomiting diarrhoea Musculoskeletal – aches, pains, restlessness, tremors, shaking Phobias – anxiety is evoked only, or predominantly by certain well defined situations or objects.
Anxiety Features Feeling Tense/ inability to relax Worrying / apprehension/ feeling unable to cope Physical Symptoms of arousal Cardiovascular – palpitations, chest pain, rapid heart beat, flushing Respiratory – hyperventilation, shortness of breath Neurological – dizziness, headache, sweating, tingling and numbness Gastrointestinal – chocking, dry mouth, nausea, vomiting diarrhoea Musculoskeletal – aches, pains, restlessness, tremors, shaking Phobias – anxiety is evoked only, or predominantly by certain well defined situations or objects.
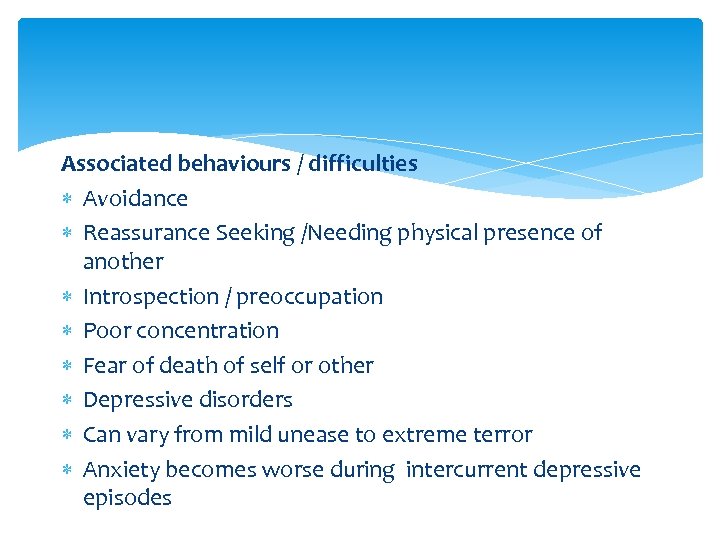 Associated behaviours / difficulties Avoidance Reassurance Seeking /Needing physical presence of another Introspection / preoccupation Poor concentration Fear of death of self or other Depressive disorders Can vary from mild unease to extreme terror Anxiety becomes worse during intercurrent depressive episodes
Associated behaviours / difficulties Avoidance Reassurance Seeking /Needing physical presence of another Introspection / preoccupation Poor concentration Fear of death of self or other Depressive disorders Can vary from mild unease to extreme terror Anxiety becomes worse during intercurrent depressive episodes
 Anxiety Treatment CBT Psychological therapies Psychosocial interventions Exposure Therapy Exercise Medication
Anxiety Treatment CBT Psychological therapies Psychosocial interventions Exposure Therapy Exercise Medication
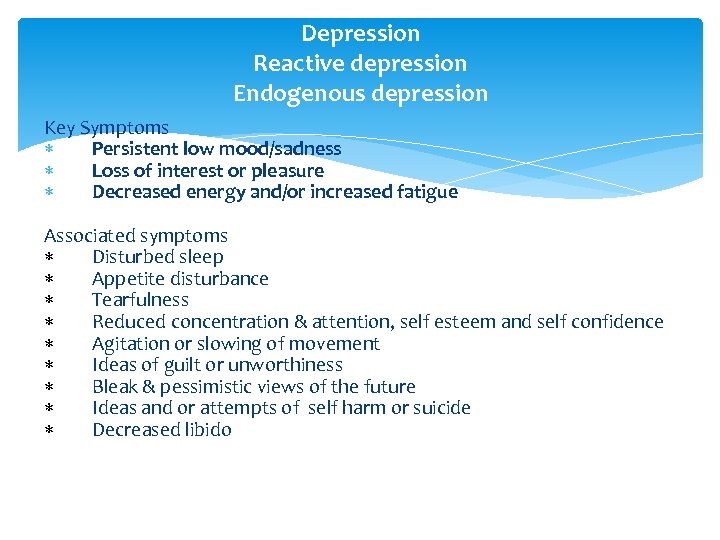 Depression Reactive depression Endogenous depression Key Symptoms Persistent low mood/sadness Loss of interest or pleasure Decreased energy and/or increased fatigue Associated symptoms Disturbed sleep Appetite disturbance Tearfulness Reduced concentration & attention, self esteem and self confidence Agitation or slowing of movement Ideas of guilt or unworthiness Bleak & pessimistic views of the future Ideas and or attempts of self harm or suicide Decreased libido
Depression Reactive depression Endogenous depression Key Symptoms Persistent low mood/sadness Loss of interest or pleasure Decreased energy and/or increased fatigue Associated symptoms Disturbed sleep Appetite disturbance Tearfulness Reduced concentration & attention, self esteem and self confidence Agitation or slowing of movement Ideas of guilt or unworthiness Bleak & pessimistic views of the future Ideas and or attempts of self harm or suicide Decreased libido
 Depression Treatment Talking therapies Counselling Psychosocial interventions Medications
Depression Treatment Talking therapies Counselling Psychosocial interventions Medications
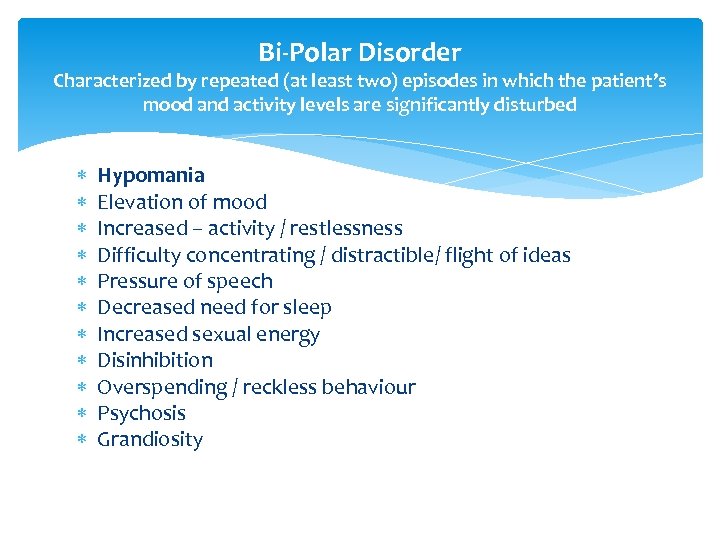 Bi-Polar Disorder Characterized by repeated (at least two) episodes in which the patient’s mood and activity levels are significantly disturbed Hypomania Elevation of mood Increased – activity / restlessness Difficulty concentrating / distractible/ flight of ideas Pressure of speech Decreased need for sleep Increased sexual energy Disinhibition Overspending / reckless behaviour Psychosis Grandiosity
Bi-Polar Disorder Characterized by repeated (at least two) episodes in which the patient’s mood and activity levels are significantly disturbed Hypomania Elevation of mood Increased – activity / restlessness Difficulty concentrating / distractible/ flight of ideas Pressure of speech Decreased need for sleep Increased sexual energy Disinhibition Overspending / reckless behaviour Psychosis Grandiosity
 Depression Often unresponsive to circumstances Exacerbation or pre-existing phobic or obsessional symptoms Irritability / agitation Lowering of mood Decreased energy Loss of interest / enjoyment Decreased energy Fatigue Diminished activity Marked tiredness after only slight activity Ideas of self harm and / or suicide
Depression Often unresponsive to circumstances Exacerbation or pre-existing phobic or obsessional symptoms Irritability / agitation Lowering of mood Decreased energy Loss of interest / enjoyment Decreased energy Fatigue Diminished activity Marked tiredness after only slight activity Ideas of self harm and / or suicide
 Bi-polar disorder Treatment Psychosocial Interventions Counselling Medications Mood stabilisers
Bi-polar disorder Treatment Psychosocial Interventions Counselling Medications Mood stabilisers
 Obsessive Compulsive Disorder. Recurrent obsessional thoughts or compulsive acts Ideas, images of impulses that enter the individuals mind over again. Recognised as the individuals own thoughts Almost invariably distressing Originate from within the mind of the client Repetitive and unpleasant Client tries to resist but is unsuccessful No pleasure derived from obsession / carrying out ritual Obsession causes distress/ interferes with functioning Anxiety symptoms often present Depression often present
Obsessive Compulsive Disorder. Recurrent obsessional thoughts or compulsive acts Ideas, images of impulses that enter the individuals mind over again. Recognised as the individuals own thoughts Almost invariably distressing Originate from within the mind of the client Repetitive and unpleasant Client tries to resist but is unsuccessful No pleasure derived from obsession / carrying out ritual Obsession causes distress/ interferes with functioning Anxiety symptoms often present Depression often present
 OCD Treatment CBT Medication Support mechanisms Specialist placements
OCD Treatment CBT Medication Support mechanisms Specialist placements
 Personality Disorder Deeply ingrained and enduring behaviour patterns, manifesting as inflexible responses to a broad range of personal and social situations Pervasive and persistent Associated with personal and social disruption Extreme or significant deviations from the way the average individual in a given culture perceives, thinks feels and particularly relates to others. Developmental condition Appear in childhood or early adolescents and continue to manifest in adulthood. Not secondary to other mental disorder or brain disease / injury
Personality Disorder Deeply ingrained and enduring behaviour patterns, manifesting as inflexible responses to a broad range of personal and social situations Pervasive and persistent Associated with personal and social disruption Extreme or significant deviations from the way the average individual in a given culture perceives, thinks feels and particularly relates to others. Developmental condition Appear in childhood or early adolescents and continue to manifest in adulthood. Not secondary to other mental disorder or brain disease / injury
 Personality Disorder Additionally • Deviation is pervasive • Personal distress and /or adverse impact • Of long duration (onset late childhood / adolescence) • Unexplained by another disorder • No organic cause • Falkov (1996) reported that 28% of the parents in his sample of fatal child abuse had identifiable personality disorder.
Personality Disorder Additionally • Deviation is pervasive • Personal distress and /or adverse impact • Of long duration (onset late childhood / adolescence) • Unexplained by another disorder • No organic cause • Falkov (1996) reported that 28% of the parents in his sample of fatal child abuse had identifiable personality disorder.
 Personality Disorder Abnormal behaviour pattern is enduring, not limited to episodes of mental illness. Poor regulation of emotions / poor impulse control Negative coping strategies / self harm / substance misuse / constant reassurance seeking Can lead to considerable personal distress Cluster A: Paranoid Personality Disorder Schizotypal Personality Disorder
Personality Disorder Abnormal behaviour pattern is enduring, not limited to episodes of mental illness. Poor regulation of emotions / poor impulse control Negative coping strategies / self harm / substance misuse / constant reassurance seeking Can lead to considerable personal distress Cluster A: Paranoid Personality Disorder Schizotypal Personality Disorder
 Cluster B: Antisocial Personality Disorder Borderline Personality Disorder Histrionic Personality Disorder Narcissistic Personality Disorder Cluster C: Avoidant Personality Disorder Dependent Personality Disorder Obsessive Compulsive Personality Disorder
Cluster B: Antisocial Personality Disorder Borderline Personality Disorder Histrionic Personality Disorder Narcissistic Personality Disorder Cluster C: Avoidant Personality Disorder Dependent Personality Disorder Obsessive Compulsive Personality Disorder
 Personality Disorder Treatment/ Management Talking therapies DBT –Dialectical Behaviour Therapy Mindfulness Specialist placements
Personality Disorder Treatment/ Management Talking therapies DBT –Dialectical Behaviour Therapy Mindfulness Specialist placements
 Schizophrenia Characterized in general by fundamental and characteristic distortions of thinking and perception Positive Symptoms: • Psychosis – a lack of contact with reality • Perception disturbed • Hallucinations – auditory • Colours or sounds may seem unduly vivid or altered • Thought insertion or withdrawal • Delusions may develop to make sense of these experiences. • Thought Disorder / Breaks in the train of thought, resulting in incoherence or irrelevant speech Negative Symptoms: • Blunting of emotions • Social withdrawal • Lowering of social performance • Loss of interest / aimlessness
Schizophrenia Characterized in general by fundamental and characteristic distortions of thinking and perception Positive Symptoms: • Psychosis – a lack of contact with reality • Perception disturbed • Hallucinations – auditory • Colours or sounds may seem unduly vivid or altered • Thought insertion or withdrawal • Delusions may develop to make sense of these experiences. • Thought Disorder / Breaks in the train of thought, resulting in incoherence or irrelevant speech Negative Symptoms: • Blunting of emotions • Social withdrawal • Lowering of social performance • Loss of interest / aimlessness
 Schizophrenia Treatment Medication Psychosocial interventions Insight work (Assessing insight) Family Therapy Exercise Physical health promotion Early Intervention in Psychosis
Schizophrenia Treatment Medication Psychosocial interventions Insight work (Assessing insight) Family Therapy Exercise Physical health promotion Early Intervention in Psychosis
 Maternal Mental Health Post Natal Depression Post Partum Psychosis Perinatal mental health covers the period from conception to 1 year as studies note the impact on the foetus of anxiety and depression 11. 8% women probably depressed (EPDS > 13) at 18 weeks pregnancy ( Evans et al 2001) 10%-15% women suffer from postnatal depression ( Cox et al 1996, Wisner 2012) 33% of women continue to suffer from postnatal depression into their second year 10% continue into their third year
Maternal Mental Health Post Natal Depression Post Partum Psychosis Perinatal mental health covers the period from conception to 1 year as studies note the impact on the foetus of anxiety and depression 11. 8% women probably depressed (EPDS > 13) at 18 weeks pregnancy ( Evans et al 2001) 10%-15% women suffer from postnatal depression ( Cox et al 1996, Wisner 2012) 33% of women continue to suffer from postnatal depression into their second year 10% continue into their third year
 Maternal Mental Health Suicide leading cause of maternal morbidity in developed countries(Oates 2003) Nearly all these were an early abrupt onset of psychotic illness. 85% were receiving treatment and had psychiatric problem identified. Previous history of a serious mental illness, post partum psychosis or family history poses a risk of reoccurrence following child birth of between 1 in 4 to as high as 1 in 2 (RCP 2014)
Maternal Mental Health Suicide leading cause of maternal morbidity in developed countries(Oates 2003) Nearly all these were an early abrupt onset of psychotic illness. 85% were receiving treatment and had psychiatric problem identified. Previous history of a serious mental illness, post partum psychosis or family history poses a risk of reoccurrence following child birth of between 1 in 4 to as high as 1 in 2 (RCP 2014)
 Maternal mental health Post partum Psychosis (suicide risk) Post partum Psychosis can result in confusion, hallucinations, irrational behaviour. Sudden in onset, usually within the first 2 weeks post delivery 7 in 10 women will attempt to hide their symptoms of PND or underplay their significant impact Prolonged symptoms of PND can lead to poor outcomes for children
Maternal mental health Post partum Psychosis (suicide risk) Post partum Psychosis can result in confusion, hallucinations, irrational behaviour. Sudden in onset, usually within the first 2 weeks post delivery 7 in 10 women will attempt to hide their symptoms of PND or underplay their significant impact Prolonged symptoms of PND can lead to poor outcomes for children
 Maternal mental health Treatment For psychosis, hospital admission usually required Medication CBT/ counselling Extended support due to major changes of having had a child and dealing with these difficulties Exercise therapy
Maternal mental health Treatment For psychosis, hospital admission usually required Medication CBT/ counselling Extended support due to major changes of having had a child and dealing with these difficulties Exercise therapy
 MENTAL ILLNESS, PARENTING AND INDIVIDUALISED ASSESSMENT Illness Pattern Severity Chronicity Specificity Individual Insight Treatment Concordance Violence / aggression/ offending history Coexisting substance misuse Family / Social Support Domestic abuse Child Resilience Vulnerability
MENTAL ILLNESS, PARENTING AND INDIVIDUALISED ASSESSMENT Illness Pattern Severity Chronicity Specificity Individual Insight Treatment Concordance Violence / aggression/ offending history Coexisting substance misuse Family / Social Support Domestic abuse Child Resilience Vulnerability
 Stress and resilience factors in parents with mental health problems and their children: Over one third of all UK adults with mental health problems are parents. (With most parents with MH problems parenting their children effectively). Children’s resilience is enhanced by a secure and reliable family base in which relationships promote self esteem, self efficacy and a sense of self control. A parent’s resilience is enhanced by family (particularly children’s) understanding, satisfactory employment, good physical health, community and personal support.
Stress and resilience factors in parents with mental health problems and their children: Over one third of all UK adults with mental health problems are parents. (With most parents with MH problems parenting their children effectively). Children’s resilience is enhanced by a secure and reliable family base in which relationships promote self esteem, self efficacy and a sense of self control. A parent’s resilience is enhanced by family (particularly children’s) understanding, satisfactory employment, good physical health, community and personal support.
 Potential Stressors: Lack of money Breakdowns in valued relationships Bereavement Loss of control at work and long working hours. Age of Child
Potential Stressors: Lack of money Breakdowns in valued relationships Bereavement Loss of control at work and long working hours. Age of Child
 Psychiatric disorder: The level of ‘dangerousness’ that stems from psychiatric disorders relates to history and mental state. Previous violence Substance misuse Domestic Violence. Poor compliance (recent discontinuation of psychiatric treatments) Recent severe stress Unstable Lifestyle 70% of parents who seriously harm their children were themselves abused as children (Dale & Fellows 1999 ; Oliver 1993).
Psychiatric disorder: The level of ‘dangerousness’ that stems from psychiatric disorders relates to history and mental state. Previous violence Substance misuse Domestic Violence. Poor compliance (recent discontinuation of psychiatric treatments) Recent severe stress Unstable Lifestyle 70% of parents who seriously harm their children were themselves abused as children (Dale & Fellows 1999 ; Oliver 1993).
 Risk in relation to Mental State: Agitation Hostile and / or suspicious behaviour Angry mood Thought disturbances (such as delusions of persecution / jealousy) Impulsive and Aggressive behaviours.
Risk in relation to Mental State: Agitation Hostile and / or suspicious behaviour Angry mood Thought disturbances (such as delusions of persecution / jealousy) Impulsive and Aggressive behaviours.
 Group Activity Consider mental disorder and possible impacts for dependant children
Group Activity Consider mental disorder and possible impacts for dependant children
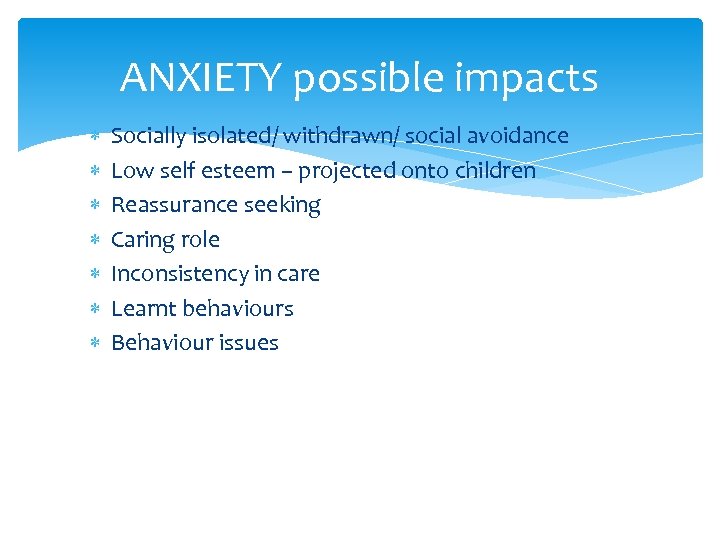 ANXIETY possible impacts Socially isolated/ withdrawn/ social avoidance Low self esteem – projected onto children Reassurance seeking Caring role Inconsistency in care Learnt behaviours Behaviour issues
ANXIETY possible impacts Socially isolated/ withdrawn/ social avoidance Low self esteem – projected onto children Reassurance seeking Caring role Inconsistency in care Learnt behaviours Behaviour issues
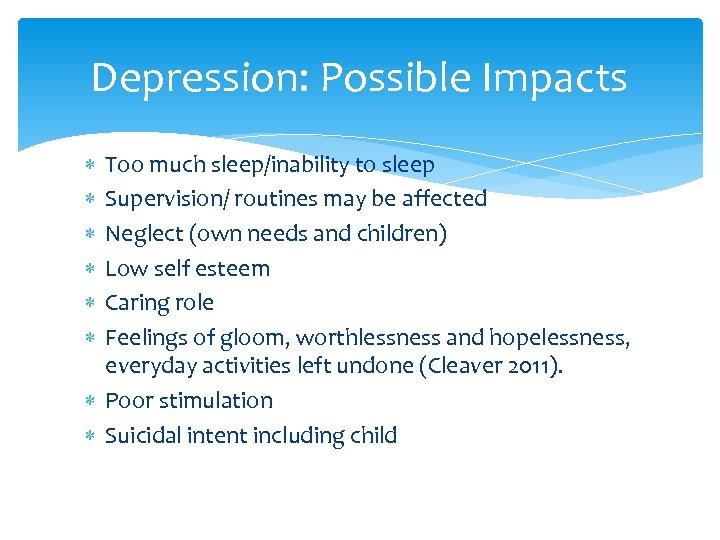 Depression: Possible Impacts Too much sleep/inability to sleep Supervision/ routines may be affected Neglect (own needs and children) Low self esteem Caring role Feelings of gloom, worthlessness and hopelessness, everyday activities left undone (Cleaver 2011). Poor stimulation Suicidal intent including child
Depression: Possible Impacts Too much sleep/inability to sleep Supervision/ routines may be affected Neglect (own needs and children) Low self esteem Caring role Feelings of gloom, worthlessness and hopelessness, everyday activities left undone (Cleaver 2011). Poor stimulation Suicidal intent including child
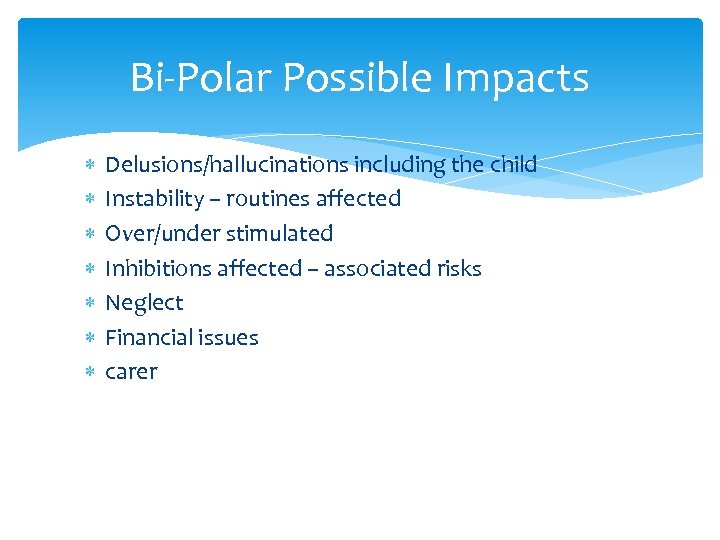 Bi-Polar Possible Impacts Delusions/hallucinations including the child Instability – routines affected Over/under stimulated Inhibitions affected – associated risks Neglect Financial issues carer
Bi-Polar Possible Impacts Delusions/hallucinations including the child Instability – routines affected Over/under stimulated Inhibitions affected – associated risks Neglect Financial issues carer
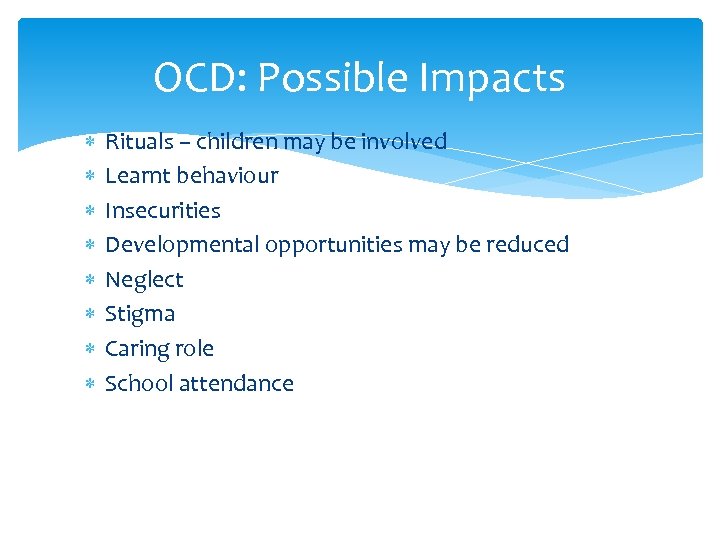 OCD: Possible Impacts Rituals – children may be involved Learnt behaviour Insecurities Developmental opportunities may be reduced Neglect Stigma Caring role School attendance
OCD: Possible Impacts Rituals – children may be involved Learnt behaviour Insecurities Developmental opportunities may be reduced Neglect Stigma Caring role School attendance
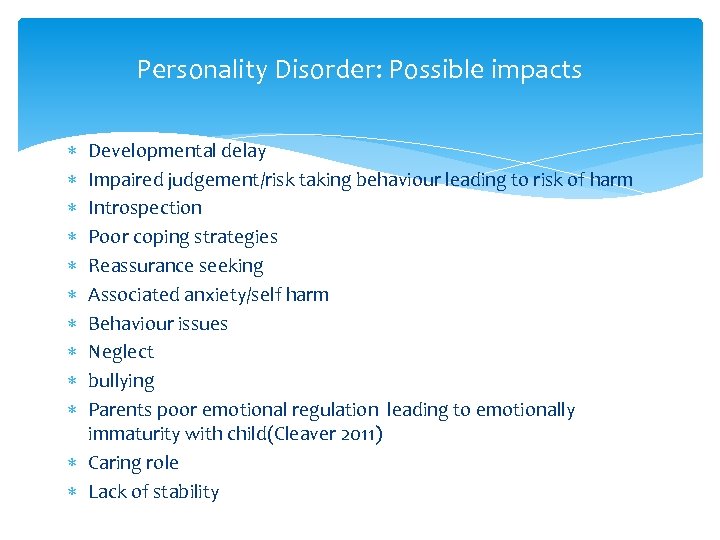 Personality Disorder: Possible impacts Developmental delay Impaired judgement/risk taking behaviour leading to risk of harm Introspection Poor coping strategies Reassurance seeking Associated anxiety/self harm Behaviour issues Neglect bullying Parents poor emotional regulation leading to emotionally immaturity with child(Cleaver 2011) Caring role Lack of stability
Personality Disorder: Possible impacts Developmental delay Impaired judgement/risk taking behaviour leading to risk of harm Introspection Poor coping strategies Reassurance seeking Associated anxiety/self harm Behaviour issues Neglect bullying Parents poor emotional regulation leading to emotionally immaturity with child(Cleaver 2011) Caring role Lack of stability
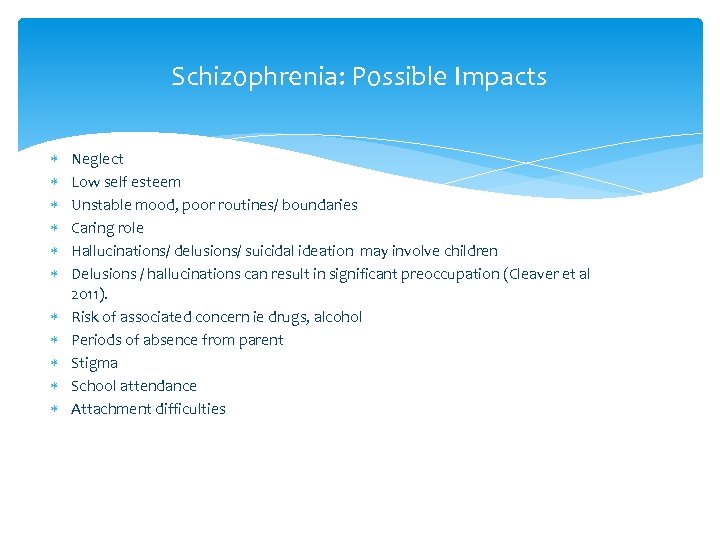 Schizophrenia: Possible Impacts Neglect Low self esteem Unstable mood, poor routines/ boundaries Caring role Hallucinations/ delusions/ suicidal ideation may involve children Delusions / hallucinations can result in significant preoccupation (Cleaver et al 2011). Risk of associated concern ie drugs, alcohol Periods of absence from parent Stigma School attendance Attachment difficulties
Schizophrenia: Possible Impacts Neglect Low self esteem Unstable mood, poor routines/ boundaries Caring role Hallucinations/ delusions/ suicidal ideation may involve children Delusions / hallucinations can result in significant preoccupation (Cleaver et al 2011). Risk of associated concern ie drugs, alcohol Periods of absence from parent Stigma School attendance Attachment difficulties
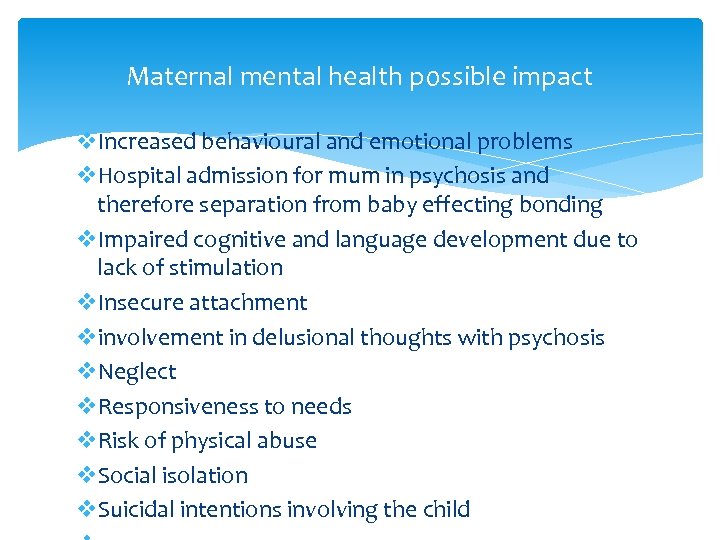 Maternal mental health possible impact v. Increased behavioural and emotional problems v. Hospital admission for mum in psychosis and therefore separation from baby effecting bonding v. Impaired cognitive and language development due to lack of stimulation v. Insecure attachment vinvolvement in delusional thoughts with psychosis v. Neglect v. Responsiveness to needs v. Risk of physical abuse v. Social isolation v. Suicidal intentions involving the child
Maternal mental health possible impact v. Increased behavioural and emotional problems v. Hospital admission for mum in psychosis and therefore separation from baby effecting bonding v. Impaired cognitive and language development due to lack of stimulation v. Insecure attachment vinvolvement in delusional thoughts with psychosis v. Neglect v. Responsiveness to needs v. Risk of physical abuse v. Social isolation v. Suicidal intentions involving the child
 Break time
Break time
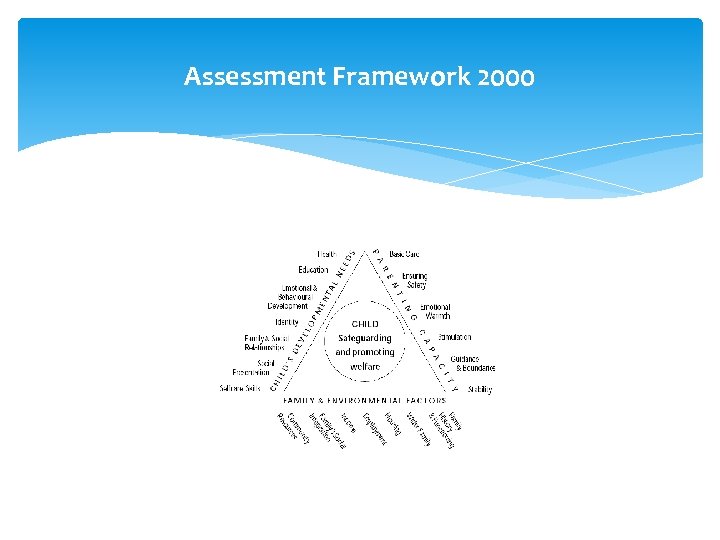 Assessment Framework 2000
Assessment Framework 2000
 Basic Care Parenting Capacity providing for physical needs, medical , dental , hygiene, food warmth etc Ensuring Safety from harm or danger in and out of home; from unsafe adults, other children and self etc Emotional Warmth sense of being specially valued, of racial and cultural identity , comfort , cuddles, praise etc Stimulation promoting learning via cognitive stimulation, social opportunities, ensuring school attendance, communication, responding to questions and joining in play etc
Basic Care Parenting Capacity providing for physical needs, medical , dental , hygiene, food warmth etc Ensuring Safety from harm or danger in and out of home; from unsafe adults, other children and self etc Emotional Warmth sense of being specially valued, of racial and cultural identity , comfort , cuddles, praise etc Stimulation promoting learning via cognitive stimulation, social opportunities, ensuring school attendance, communication, responding to questions and joining in play etc
 Parenting Capacity cont. . . Guidance and Boundaries enabling the child to regulate own emotions and behaviour by demonstrating emotional and behavioural control in emotions and interactions with others e. g. social problem solving, anger management. Setting boundaries which enable the child to internalise pro social behaviour as opposed to being rule dependant. Stability providing a stable family environment which enables secure attachments with consistency of warmth over time, maintaining appropriate and similar responses to similar behaviour according to child's development. Enabling positive family contact
Parenting Capacity cont. . . Guidance and Boundaries enabling the child to regulate own emotions and behaviour by demonstrating emotional and behavioural control in emotions and interactions with others e. g. social problem solving, anger management. Setting boundaries which enable the child to internalise pro social behaviour as opposed to being rule dependant. Stability providing a stable family environment which enables secure attachments with consistency of warmth over time, maintaining appropriate and similar responses to similar behaviour according to child's development. Enabling positive family contact
 Early Help Providing early help is more effective in promoting the welfare of children than reacting later Effective early help relies upon local agencies working together to: • identify children and families who would benefit from early help; • undertake an assessment of the need for early help; and • provide targeted early help services to address the assessed needs of a child and their family which focuses on activity to significantly improve the outcomes for the child. Professionals should, in particular, be alert to the potential need for early help for a child who: is in a family circumstance presenting challenges for the child, such as substance abuse, adult mental health problems and domestic violence
Early Help Providing early help is more effective in promoting the welfare of children than reacting later Effective early help relies upon local agencies working together to: • identify children and families who would benefit from early help; • undertake an assessment of the need for early help; and • provide targeted early help services to address the assessed needs of a child and their family which focuses on activity to significantly improve the outcomes for the child. Professionals should, in particular, be alert to the potential need for early help for a child who: is in a family circumstance presenting challenges for the child, such as substance abuse, adult mental health problems and domestic violence
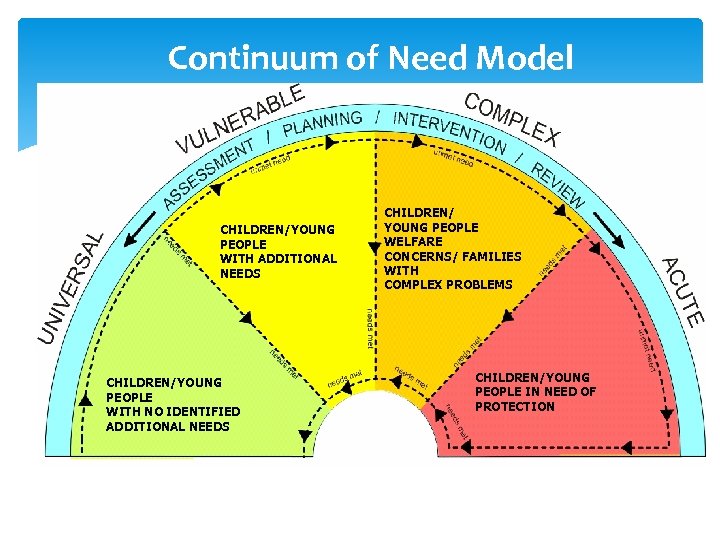 Continuum of Need Model CHILDREN/YOUNG PEOPLE WITH ADDITIONAL NEEDS CHILDREN/YOUNG PEOPLE WITH NO IDENTIFIED ADDITIONAL NEEDS CHILDREN/ YOUNG PEOPLE WELFARE CONCERNS/ FAMILIES WITH COMPLEX PROBLEMS CHILDREN/YOUNG PEOPLE IN NEED OF PROTECTION
Continuum of Need Model CHILDREN/YOUNG PEOPLE WITH ADDITIONAL NEEDS CHILDREN/YOUNG PEOPLE WITH NO IDENTIFIED ADDITIONAL NEEDS CHILDREN/ YOUNG PEOPLE WELFARE CONCERNS/ FAMILIES WITH COMPLEX PROBLEMS CHILDREN/YOUNG PEOPLE IN NEED OF PROTECTION
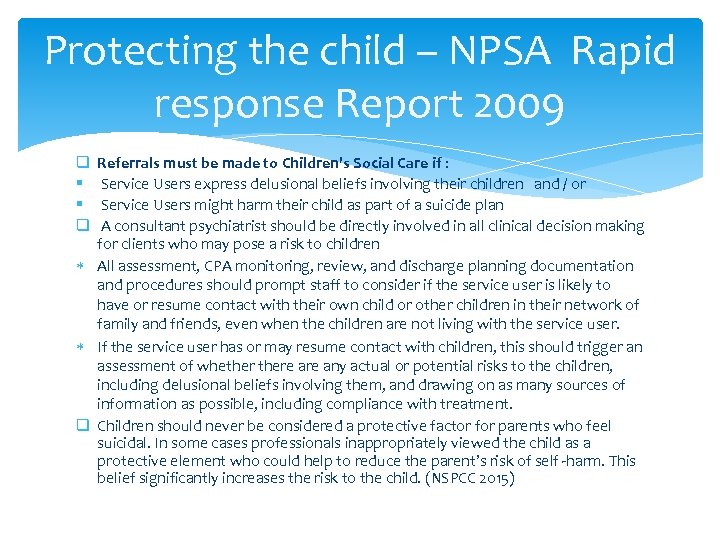 Protecting the child – NPSA Rapid response Report 2009 Referrals must be made to Children's Social Care if : Service Users express delusional beliefs involving their children and / or Service Users might harm their child as part of a suicide plan A consultant psychiatrist should be directly involved in all clinical decision making for clients who may pose a risk to children All assessment, CPA monitoring, review, and discharge planning documentation and procedures should prompt staff to consider if the service user is likely to have or resume contact with their own child or other children in their network of family and friends, even when the children are not living with the service user. If the service user has or may resume contact with children, this should trigger an assessment of whethere any actual or potential risks to the children, including delusional beliefs involving them, and drawing on as many sources of information as possible, including compliance with treatment. q Children should never be considered a protective factor for parents who feel suicidal. In some cases professionals inappropriately viewed the child as a protective element who could help to reduce the parent’s risk of self -harm. This belief significantly increases the risk to the child. (NSPCC 2015) q § § q
Protecting the child – NPSA Rapid response Report 2009 Referrals must be made to Children's Social Care if : Service Users express delusional beliefs involving their children and / or Service Users might harm their child as part of a suicide plan A consultant psychiatrist should be directly involved in all clinical decision making for clients who may pose a risk to children All assessment, CPA monitoring, review, and discharge planning documentation and procedures should prompt staff to consider if the service user is likely to have or resume contact with their own child or other children in their network of family and friends, even when the children are not living with the service user. If the service user has or may resume contact with children, this should trigger an assessment of whethere any actual or potential risks to the children, including delusional beliefs involving them, and drawing on as many sources of information as possible, including compliance with treatment. q Children should never be considered a protective factor for parents who feel suicidal. In some cases professionals inappropriately viewed the child as a protective element who could help to reduce the parent’s risk of self -harm. This belief significantly increases the risk to the child. (NSPCC 2015) q § § q
 Self Harm Majority of self harm occurs between 11 -25 yrs old. Also known to occur in very young and adults. Why? ? controlling mood a way of expressing themselves control/punishment - a form of trauma reenactment
Self Harm Majority of self harm occurs between 11 -25 yrs old. Also known to occur in very young and adults. Why? ? controlling mood a way of expressing themselves control/punishment - a form of trauma reenactment
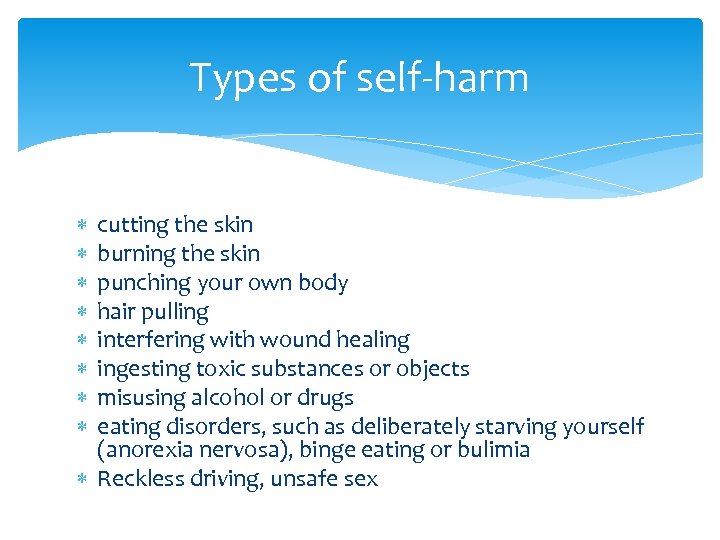 Types of self-harm cutting the skin burning the skin punching your own body hair pulling interfering with wound healing ingesting toxic substances or objects misusing alcohol or drugs eating disorders, such as deliberately starving yourself (anorexia nervosa), binge eating or bulimia Reckless driving, unsafe sex
Types of self-harm cutting the skin burning the skin punching your own body hair pulling interfering with wound healing ingesting toxic substances or objects misusing alcohol or drugs eating disorders, such as deliberately starving yourself (anorexia nervosa), binge eating or bulimia Reckless driving, unsafe sex
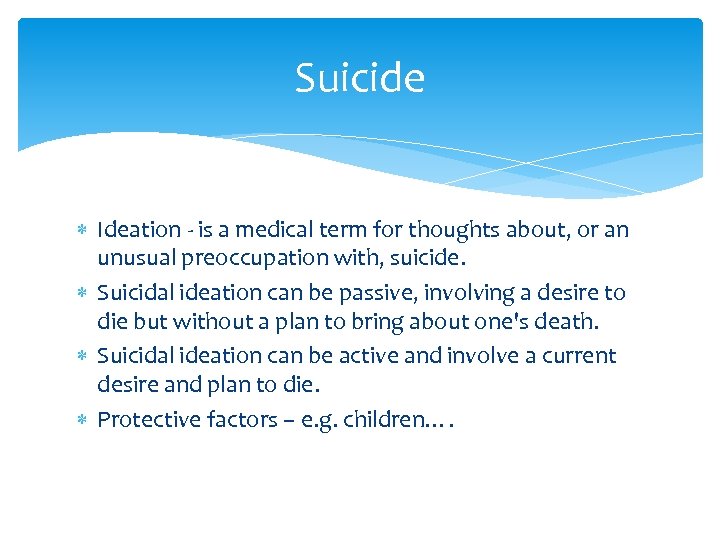 Suicide Ideation - is a medical term for thoughts about, or an unusual preoccupation with, suicide. Suicidal ideation can be passive, involving a desire to die but without a plan to bring about one's death. Suicidal ideation can be active and involve a current desire and plan to die. Protective factors – e. g. children….
Suicide Ideation - is a medical term for thoughts about, or an unusual preoccupation with, suicide. Suicidal ideation can be passive, involving a desire to die but without a plan to bring about one's death. Suicidal ideation can be active and involve a current desire and plan to die. Protective factors – e. g. children….
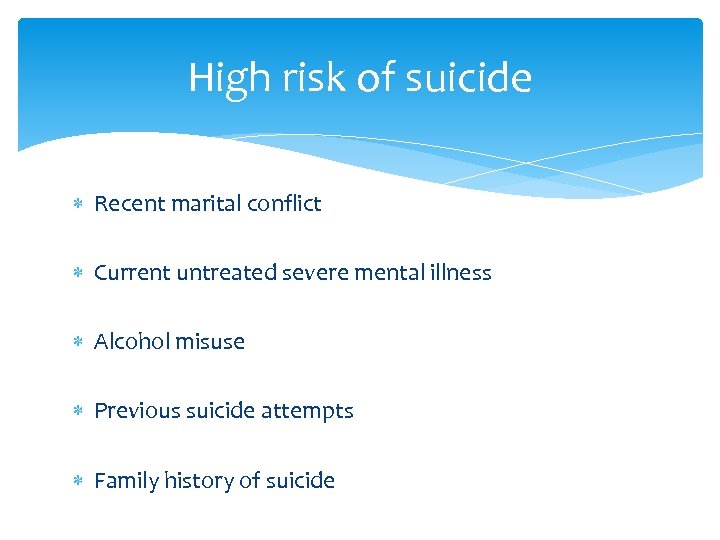 High risk of suicide Recent marital conflict Current untreated severe mental illness Alcohol misuse Previous suicide attempts Family history of suicide
High risk of suicide Recent marital conflict Current untreated severe mental illness Alcohol misuse Previous suicide attempts Family history of suicide
 Group Activity q. Using : § The Assessment Framework and § The Continuum of Need § Consider the scenarios and what actions you may need to take?
Group Activity q. Using : § The Assessment Framework and § The Continuum of Need § Consider the scenarios and what actions you may need to take?
 Case Scenario A Dawn is a 37 year old single mum who lives with her 14 year old daughter Jane and her 2 ½ year old son Tom. Jane has problematic school attendance and the education welfare officer has told Dawn she feels she is not assertive enough as a parent. Jane see’s a Connexion’s Worker in School and Tom is currently having assessments for visual difficulties and a squint. Dawn had a ‘panic attack’ 3 months ago and is currently experiencing physical symptoms of anxiety, palpitations, sweating and nausea with an accompanying fear that she will pass out. As a result, Dawn always takes Tom out in his ‘buggy’ as a coping mechanism and only shops locally. She only goes to town if she is accompanied by her daughter as she feels unable to get on the bus alone. Her son has recently missed an optical appointment which she claims is due to her fear of lifts at the hospital and because Jane refused to come with her.
Case Scenario A Dawn is a 37 year old single mum who lives with her 14 year old daughter Jane and her 2 ½ year old son Tom. Jane has problematic school attendance and the education welfare officer has told Dawn she feels she is not assertive enough as a parent. Jane see’s a Connexion’s Worker in School and Tom is currently having assessments for visual difficulties and a squint. Dawn had a ‘panic attack’ 3 months ago and is currently experiencing physical symptoms of anxiety, palpitations, sweating and nausea with an accompanying fear that she will pass out. As a result, Dawn always takes Tom out in his ‘buggy’ as a coping mechanism and only shops locally. She only goes to town if she is accompanied by her daughter as she feels unable to get on the bus alone. Her son has recently missed an optical appointment which she claims is due to her fear of lifts at the hospital and because Jane refused to come with her.
 Case Scenario B Helen lives with her 6 year old daughter, Abigail and her husband John. They have been married for 10 years and Helen was diagnosed with Schizophrenia 8 years ago during the final year of her teacher training. Helen has been detained under the mental health act twice, the last time was shortly after Abigail's birth when she began hearing voices telling her Abigail had leukaemia and she must develop a cure. Helen takes regular medication and sees a Psychiatrist 3 monthly. Helen has recently begun a college course and working a few hours in a local shop now Abigail has started school. John works away from home regularly. School have noticed that Helen has been muttering to herself in the playground appears preoccupied and that Abigail has seemed a little withdrawn recently and has refused to eat her lunch for the last 2 days. When asked why she is not eating Abigail becomes distressed and states that her mummy has told her that people are trying to poison them while daddy is away and she can’t eat or she will die.
Case Scenario B Helen lives with her 6 year old daughter, Abigail and her husband John. They have been married for 10 years and Helen was diagnosed with Schizophrenia 8 years ago during the final year of her teacher training. Helen has been detained under the mental health act twice, the last time was shortly after Abigail's birth when she began hearing voices telling her Abigail had leukaemia and she must develop a cure. Helen takes regular medication and sees a Psychiatrist 3 monthly. Helen has recently begun a college course and working a few hours in a local shop now Abigail has started school. John works away from home regularly. School have noticed that Helen has been muttering to herself in the playground appears preoccupied and that Abigail has seemed a little withdrawn recently and has refused to eat her lunch for the last 2 days. When asked why she is not eating Abigail becomes distressed and states that her mummy has told her that people are trying to poison them while daddy is away and she can’t eat or she will die.
 Case Scenario C Sarah is 23 years old, is unemployed and in debt. She has a 3 month old baby, Luke, and lives alone in a private rented flat which is in a poor state of repair. Luke’s father has intermittent contact with Luke and little is known about their relationship. Sarah has recently been feeling very low and is finding it difficult to motivate herself to get up and dressed or to prepare meals. The health visitor has noticed a decline in the home conditions, and has noticed that Sarah wasn’t responding when Luke was crying. Sarah has lost all her pregnancy weight. She says that she is upset easily spends some time most days crying and isn’t sure why. Sarah admits that she is unsure what Luke wants when he is crying and feels overwhelmed by the demands of looking after him.
Case Scenario C Sarah is 23 years old, is unemployed and in debt. She has a 3 month old baby, Luke, and lives alone in a private rented flat which is in a poor state of repair. Luke’s father has intermittent contact with Luke and little is known about their relationship. Sarah has recently been feeling very low and is finding it difficult to motivate herself to get up and dressed or to prepare meals. The health visitor has noticed a decline in the home conditions, and has noticed that Sarah wasn’t responding when Luke was crying. Sarah has lost all her pregnancy weight. She says that she is upset easily spends some time most days crying and isn’t sure why. Sarah admits that she is unsure what Luke wants when he is crying and feels overwhelmed by the demands of looking after him.
 Case Scenario D Paula is 23 years old and has been living with her boyfriend Simon for 3 months. Paula has a daughter Jessie who is 7 years old. Paula believes that Jessie should not have contact with her birth father Jake stating that he used to smoke cannabis when they were together however he is pursuing contact and sees Jessie every other weekend at a contact centre. Paula has been ordered by the court to maintain this contact and she is making a complaint against the CAFCASS worker who she feels is siding with Jake and often turns up late to limit the contact. Paula has a tense relationship with her mother Louise because she does not believe that Paula’s step father who died 9 years ago sexually abused her. Paula often phones the mental health crisis team distressed and threatening to kill herself after having had arguments with her mother and has a history of superficial self harm by cutting her thighs and wrists and also of taking small overdoses of paracetamol. She refuses any ‘talking therapies’ that have been offered. Jessie called an ambulance at 11. 45 pm yesterday after Paula cut her wrists whilst intoxicated following an argument with Simon.
Case Scenario D Paula is 23 years old and has been living with her boyfriend Simon for 3 months. Paula has a daughter Jessie who is 7 years old. Paula believes that Jessie should not have contact with her birth father Jake stating that he used to smoke cannabis when they were together however he is pursuing contact and sees Jessie every other weekend at a contact centre. Paula has been ordered by the court to maintain this contact and she is making a complaint against the CAFCASS worker who she feels is siding with Jake and often turns up late to limit the contact. Paula has a tense relationship with her mother Louise because she does not believe that Paula’s step father who died 9 years ago sexually abused her. Paula often phones the mental health crisis team distressed and threatening to kill herself after having had arguments with her mother and has a history of superficial self harm by cutting her thighs and wrists and also of taking small overdoses of paracetamol. She refuses any ‘talking therapies’ that have been offered. Jessie called an ambulance at 11. 45 pm yesterday after Paula cut her wrists whilst intoxicated following an argument with Simon.
 Case Scenario E Rebecca and Tom are in their 40’s, they both have mild learning disability, and Tom suffers with depression. They both have alcohol problems. They have a 4 year old son, Robert who has “query” Foetal Alcohol Spectrum Disorder, he has significant learning disability and behaviour challenges, he attends a special school. On a routine visit, Tom’s support worker finds Robert hanging upside down from the banister over the stairs, Rebecca and Tom appear unable to control his behaviour and maintain his safety. Robert has a social worker, there is a CAF and he has regular child in need meetings. Robert has regular contact with Tom’s sister in another city, he spends his weekends and school holidays with them. The sister’s children are both drug users, on Methadone programmes. Tom’s sister is very critical of Tom and Rebecca’s parenting of Robert, this causes frequent arguments. These arguments are usually in front of Robert on contact changeover at weekends. The police have been called on several occasions.
Case Scenario E Rebecca and Tom are in their 40’s, they both have mild learning disability, and Tom suffers with depression. They both have alcohol problems. They have a 4 year old son, Robert who has “query” Foetal Alcohol Spectrum Disorder, he has significant learning disability and behaviour challenges, he attends a special school. On a routine visit, Tom’s support worker finds Robert hanging upside down from the banister over the stairs, Rebecca and Tom appear unable to control his behaviour and maintain his safety. Robert has a social worker, there is a CAF and he has regular child in need meetings. Robert has regular contact with Tom’s sister in another city, he spends his weekends and school holidays with them. The sister’s children are both drug users, on Methadone programmes. Tom’s sister is very critical of Tom and Rebecca’s parenting of Robert, this causes frequent arguments. These arguments are usually in front of Robert on contact changeover at weekends. The police have been called on several occasions.
 Case Scenario F Jayne is 45 yrs, she has been a victim of domestic violence and her ex husband was also a drug user and had a diagnosis of schizophrenia. Her oldest son Dean is 17 yrs, has mild learning disability, ADHD, he regularly smokes Cannabis and takes MCAT. Dean has symptoms of psychosis, a psychiatrist visits him at home. Dean should take Risperidone for psychotic symptoms and to stabilize his mood. He is not engaging and refusing to take the medication. Dean can be aggressive, and has also been involved in burglaries and fights in the neighbourhood. Jayne has refused to give Dean money, when he has spent his own money. In a rage he has attacked her hitting her around the head with a shovel. There is a younger child in the house. Mitchell, who is 8 years old. Jayne feels that there is no risk to Mitchell and that she can keep him safe.
Case Scenario F Jayne is 45 yrs, she has been a victim of domestic violence and her ex husband was also a drug user and had a diagnosis of schizophrenia. Her oldest son Dean is 17 yrs, has mild learning disability, ADHD, he regularly smokes Cannabis and takes MCAT. Dean has symptoms of psychosis, a psychiatrist visits him at home. Dean should take Risperidone for psychotic symptoms and to stabilize his mood. He is not engaging and refusing to take the medication. Dean can be aggressive, and has also been involved in burglaries and fights in the neighbourhood. Jayne has refused to give Dean money, when he has spent his own money. In a rage he has attacked her hitting her around the head with a shovel. There is a younger child in the house. Mitchell, who is 8 years old. Jayne feels that there is no risk to Mitchell and that she can keep him safe.
 Case Scenario G Paula is 36 yrs, her husband Lee has Bi Polar disorder and uses amphetamines. Lee has support through adult mental health, and drug and alcohol services. They have 8 children, aged between 12 yrs and 7 months, Paula is 6 months pregnant and has attempted to conceal the pregnancy. One of the children Wayne, has severe learning disability, ADHD, epilepsy and severe challenging behaviour displayed as self harm, stripping and smearing faeces. Wayne often appears anxious and distressed in the family home. The children are all subject to a child protection plan under the category of physical abuse, following an incident of domestic violence in the home where the police were called. Lee had put a plastic bag over Paula’s head to suffocate her, believing she was having an affair. Professionals report that the family home is chaotic, untidy and dirty. Paula and Lee will only engage with certain professionals that they trust. They do not attend core group, but are making attempts to work with the child protection plan. The other son attends A & E with a burn to his foot, having climbed on the cooker to get to sweets in the cupboard.
Case Scenario G Paula is 36 yrs, her husband Lee has Bi Polar disorder and uses amphetamines. Lee has support through adult mental health, and drug and alcohol services. They have 8 children, aged between 12 yrs and 7 months, Paula is 6 months pregnant and has attempted to conceal the pregnancy. One of the children Wayne, has severe learning disability, ADHD, epilepsy and severe challenging behaviour displayed as self harm, stripping and smearing faeces. Wayne often appears anxious and distressed in the family home. The children are all subject to a child protection plan under the category of physical abuse, following an incident of domestic violence in the home where the police were called. Lee had put a plastic bag over Paula’s head to suffocate her, believing she was having an affair. Professionals report that the family home is chaotic, untidy and dirty. Paula and Lee will only engage with certain professionals that they trust. They do not attend core group, but are making attempts to work with the child protection plan. The other son attends A & E with a burn to his foot, having climbed on the cooker to get to sweets in the cupboard.
 Case Scenario H Razia is 36 yrs, she lives with her husband 3 children. Razia has a learning disability and receives support through her local advocacy service. The two youngest children have learning disability, one having ADHD also, the other has significant health needs. Razia is having difficulty managing the children’s behaviour. There have been A & E attendances where the children have sustained injuries through risky behaviour, including running into the road in front of cars. Razia’s family and her husband’s family are very critical of her parenting. Her husband does help with parenting, and will not engage with professionals, after the children were removed by social care in the past. Currently, the middle child has fractures to both legs, after coming down the stairs on a sledge. He is sleeping with Dad in the downstairs room.
Case Scenario H Razia is 36 yrs, she lives with her husband 3 children. Razia has a learning disability and receives support through her local advocacy service. The two youngest children have learning disability, one having ADHD also, the other has significant health needs. Razia is having difficulty managing the children’s behaviour. There have been A & E attendances where the children have sustained injuries through risky behaviour, including running into the road in front of cars. Razia’s family and her husband’s family are very critical of her parenting. Her husband does help with parenting, and will not engage with professionals, after the children were removed by social care in the past. Currently, the middle child has fractures to both legs, after coming down the stairs on a sledge. He is sleeping with Dad in the downstairs room.
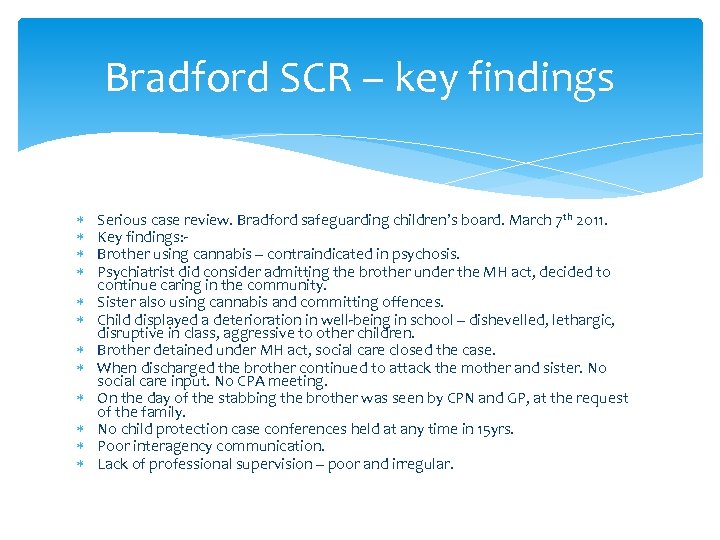 Bradford SCR – key findings Serious case review. Bradford safeguarding children’s board. March 7 th 2011. Key findings: Brother using cannabis – contraindicated in psychosis. Psychiatrist did consider admitting the brother under the MH act, decided to continue caring in the community. Sister also using cannabis and committing offences. Child displayed a deterioration in well-being in school – dishevelled, lethargic, disruptive in class, aggressive to other children. Brother detained under MH act, social care closed the case. When discharged the brother continued to attack the mother and sister. No social care input. No CPA meeting. On the day of the stabbing the brother was seen by CPN and GP, at the request of the family. No child protection case conferences held at any time in 15 yrs. Poor interagency communication. Lack of professional supervision – poor and irregular.
Bradford SCR – key findings Serious case review. Bradford safeguarding children’s board. March 7 th 2011. Key findings: Brother using cannabis – contraindicated in psychosis. Psychiatrist did consider admitting the brother under the MH act, decided to continue caring in the community. Sister also using cannabis and committing offences. Child displayed a deterioration in well-being in school – dishevelled, lethargic, disruptive in class, aggressive to other children. Brother detained under MH act, social care closed the case. When discharged the brother continued to attack the mother and sister. No social care input. No CPA meeting. On the day of the stabbing the brother was seen by CPN and GP, at the request of the family. No child protection case conferences held at any time in 15 yrs. Poor interagency communication. Lack of professional supervision – poor and irregular.
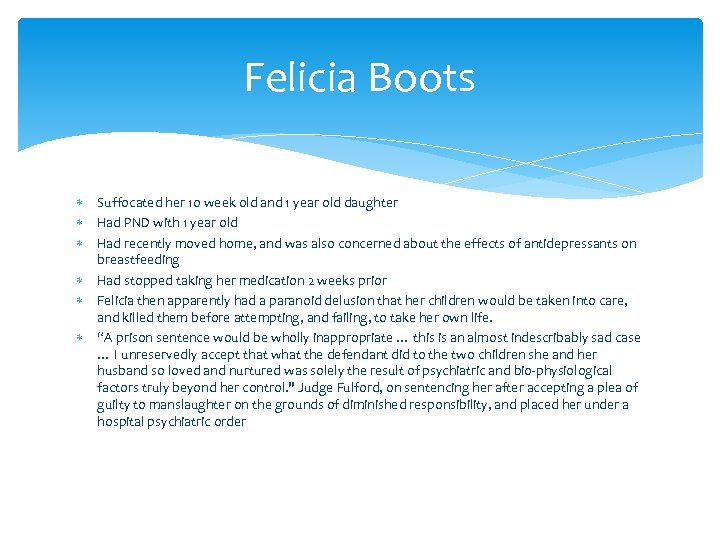 Felicia Boots Suffocated her 10 week old and 1 year old daughter Had PND with 1 year old Had recently moved home, and was also concerned about the effects of antidepressants on breastfeeding Had stopped taking her medication 2 weeks prior Felicia then apparently had a paranoid delusion that her children would be taken into care, and killed them before attempting, and failing, to take her own life. “A prison sentence would be wholly inappropriate … this is an almost indescribably sad case … I unreservedly accept that what the defendant did to the two children she and her husband so loved and nurtured was solely the result of psychiatric and bio-physiological factors truly beyond her control. " Judge Fulford, on sentencing her after accepting a plea of guilty to manslaughter on the grounds of diminished responsibility, and placed her under a hospital psychiatric order
Felicia Boots Suffocated her 10 week old and 1 year old daughter Had PND with 1 year old Had recently moved home, and was also concerned about the effects of antidepressants on breastfeeding Had stopped taking her medication 2 weeks prior Felicia then apparently had a paranoid delusion that her children would be taken into care, and killed them before attempting, and failing, to take her own life. “A prison sentence would be wholly inappropriate … this is an almost indescribably sad case … I unreservedly accept that what the defendant did to the two children she and her husband so loved and nurtured was solely the result of psychiatric and bio-physiological factors truly beyond her control. " Judge Fulford, on sentencing her after accepting a plea of guilty to manslaughter on the grounds of diminished responsibility, and placed her under a hospital psychiatric order
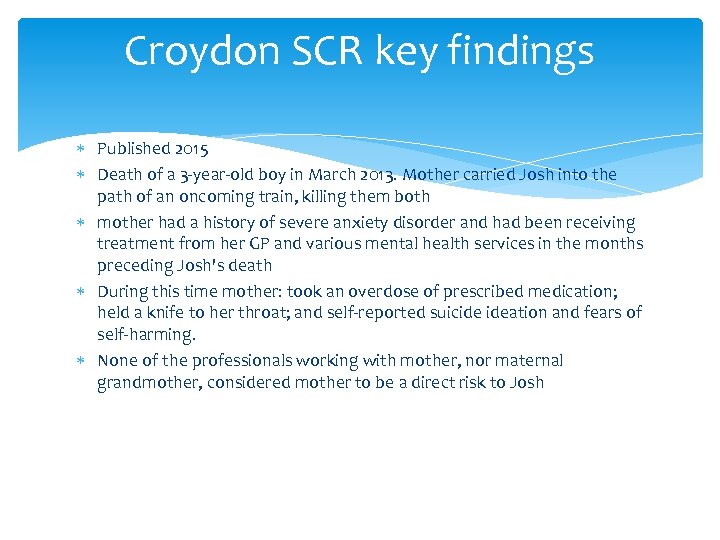 Croydon SCR key findings Published 2015 Death of a 3 -year-old boy in March 2013. Mother carried Josh into the path of an oncoming train, killing them both mother had a history of severe anxiety disorder and had been receiving treatment from her GP and various mental health services in the months preceding Josh's death During this time mother: took an overdose of prescribed medication; held a knife to her throat; and self-reported suicide ideation and fears of self-harming. None of the professionals working with mother, nor maternal grandmother, considered mother to be a direct risk to Josh
Croydon SCR key findings Published 2015 Death of a 3 -year-old boy in March 2013. Mother carried Josh into the path of an oncoming train, killing them both mother had a history of severe anxiety disorder and had been receiving treatment from her GP and various mental health services in the months preceding Josh's death During this time mother: took an overdose of prescribed medication; held a knife to her throat; and self-reported suicide ideation and fears of self-harming. None of the professionals working with mother, nor maternal grandmother, considered mother to be a direct risk to Josh
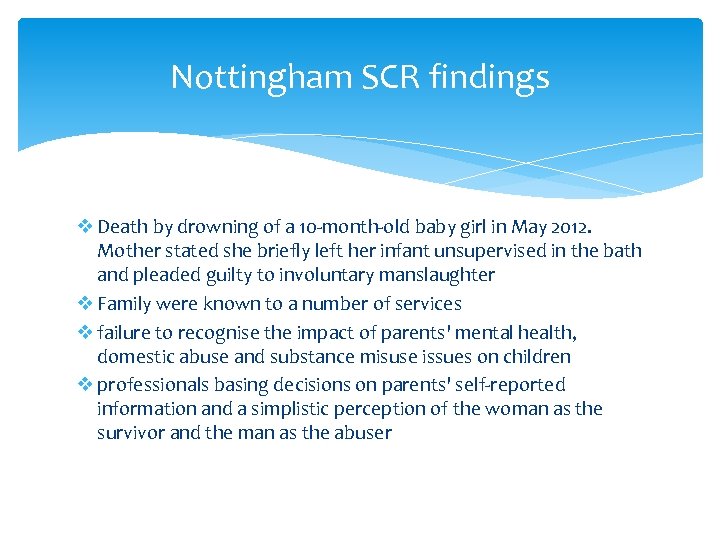 Nottingham SCR findings v Death by drowning of a 10 -month-old baby girl in May 2012. Mother stated she briefly left her infant unsupervised in the bath and pleaded guilty to involuntary manslaughter v Family were known to a number of services v failure to recognise the impact of parents' mental health, domestic abuse and substance misuse issues on children v professionals basing decisions on parents' self-reported information and a simplistic perception of the woman as the survivor and the man as the abuser
Nottingham SCR findings v Death by drowning of a 10 -month-old baby girl in May 2012. Mother stated she briefly left her infant unsupervised in the bath and pleaded guilty to involuntary manslaughter v Family were known to a number of services v failure to recognise the impact of parents' mental health, domestic abuse and substance misuse issues on children v professionals basing decisions on parents' self-reported information and a simplistic perception of the woman as the survivor and the man as the abuser
 The family as a whole…… Professionals must respond to the needs of the “whole family” in the context of “threshold” http: //www. bradford-scb. org. uk/scr. htm
The family as a whole…… Professionals must respond to the needs of the “whole family” in the context of “threshold” http: //www. bradford-scb. org. uk/scr. htm

 http: //www. rdash. nhs. uk/services/our-services/adult-mental-health-services/ Improving Access to Psychological Therapies (IAPT) Doncaster – The Talking Shop 63 Hall Gate, Doncaster DN 1 3 PB Phone: 01302 565650 If someone you know has concerns about their immediate health and you or they are already registered with one of our services then please use the following contact methods to get the help you need: During office hours Phone your GP Phone your care coordinator / lead professional or other mental health worker Phone Mental Health Access Team/Single Point of Contact – 01302 566999 Outside of office hours Doncaster – 01302 566999
http: //www. rdash. nhs. uk/services/our-services/adult-mental-health-services/ Improving Access to Psychological Therapies (IAPT) Doncaster – The Talking Shop 63 Hall Gate, Doncaster DN 1 3 PB Phone: 01302 565650 If someone you know has concerns about their immediate health and you or they are already registered with one of our services then please use the following contact methods to get the help you need: During office hours Phone your GP Phone your care coordinator / lead professional or other mental health worker Phone Mental Health Access Team/Single Point of Contact – 01302 566999 Outside of office hours Doncaster – 01302 566999
 Thankyou for attending Any questions?
Thankyou for attending Any questions?


