ebd2e9839f9c0687ec0ac6016355a331.ppt
- Количество слайдов: 32

Painful neck in vertebral osteochondrosis. Treatment from Emergency till SCENAR-center. R. Kuzmova, E. Khatisova, T. Forostyan, I. Yakushev, A. V. Tarakanov (Bulgaria, Ukraine, Russia)

Parties to Research Coordinator: Acute Care and Emergency Department, Rostov State Medical University (A. V. Tarakanov) Bulgaria: (SCENAR-Center) R. Kuzmova Ukraine: (SCENAR-Center) T. Forostyan Russia: - St. Petersburg (Emergency Station) I. Yakushev - Bataisk (Emergency Station) E. Khatisova - Maikop (Emergency Station)
Painful process in cervical osteochondrosis can be considered a separate nosological form of musculoskeletal affections. This pathology involves all tissues of the vertebral segment, many of which may cause chronic pain. The pain syndromes that never develop in other regions of the spine are observed in the cervical spine.
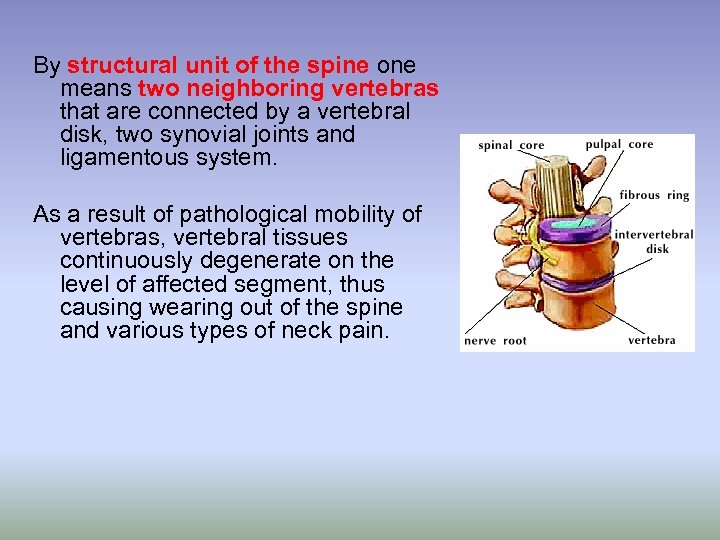
By structural unit of the spine one means two neighboring vertebras that are connected by a vertebral disk, two synovial joints and ligamentous system. As a result of pathological mobility of vertebras, vertebral tissues continuously degenerate on the level of affected segment, thus causing wearing out of the spine and various types of neck pain.
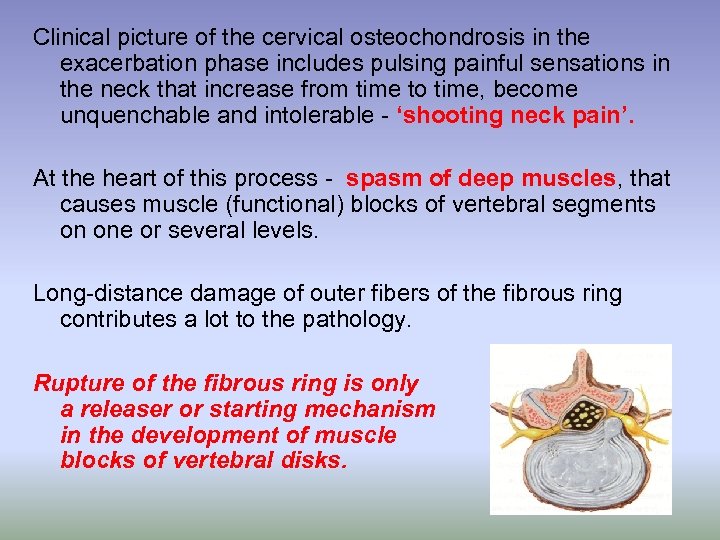
Clinical picture of the cervical osteochondrosis in the exacerbation phase includes pulsing painful sensations in the neck that increase from time to time, become unquenchable and intolerable - ‘shooting neck pain’. At the heart of this process - spasm of deep muscles, that causes muscle (functional) blocks of vertebral segments on one or several levels. Long-distance damage of outer fibers of the fibrous ring contributes a lot to the pathology. Rupture of the fibrous ring is only a releaser or starting mechanism in the development of muscle blocks of vertebral disks.
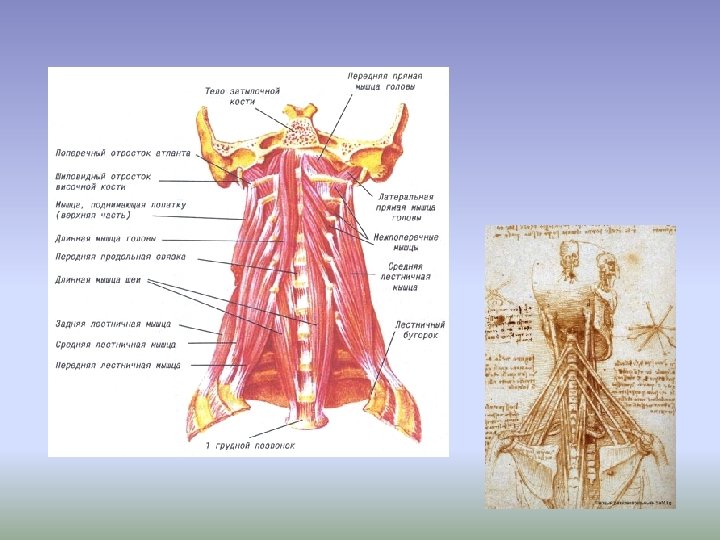
The anatomic substrate of the pain syndrome in cervical diskalgia on the level of С 2 -С 5 vertebras includes mainly multipartite muscles and short rotators. In case of protruded or herniated disk on the level of С 5 Тh 1 segments, the anterior and middle scalene muscles are additionally involved in developing of muscle blocks. This type of muscle blocks is known as the scalenusanticus syndrome. As a result of spasm and the following cicatrical degeneration of the scalene muscles, subclavian vessels and brachial plexus roots (traumatic radiculitis, neuritis, and arteritis) are continuously irritated.
Cervical osteochondrosis syndromes in intervertebral foramen narrowing The syndromes are caused by mechanical factors – narrowing of intervertebral foramen and of nerve root compression, which shows itself as neurodystrophic syndromes (shoulder-hand syndrome, epicondylitis, humeroscapular periarthrosis or visceral syndromes). Simultaneous affection of several roots is typical for the cervical spine. This usually occurs in the lower cervical spine, where the spinal mobility is the highest.
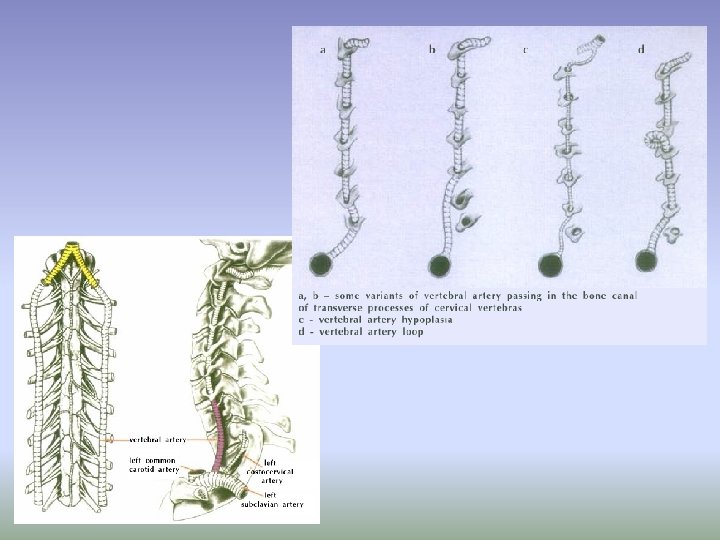
Craniocerebral Signs of Osteochondrosis The vertebral artery and the vegetative nerve plexus are located in the bone canaliculus of transverse processes of five lower cervical vertebras. Such anatomical determination makes the verterbal artery dependent on spondylosis presentations. Osteophytes may originate from the tissue of transverse processes but much more often they are caused by uncovertebral joints located near the vertebral artery. Their arthrosis leads to the development of massive uncovertebral exostosis. Two starting mechanisms underlie the vertebral artery syndrome: 1) irritation of vertebral plexus (a. vertebralis), and 2) artery compression by osteochondromas
Secondary (additional) sources of neck pain in vertebral osteochondrosis Myogenic trigger points make their contribution to the development of painful neck in osteochondrosis. They are painful indurations (hardening) in muscles, mainly in those that are usually involved in myotonic reactions. There are 2 stages: 1) functional stage characterized by reversible abnormalities in muscles; 2) dystrophic stage when functional disorders in the muscular tissue turn to the scarry changes that are irreversible.
Major tasks of management of patients in the acute period of pain 1. Pain relief 2. Restore normal biomechanics of the spine. 3. Create conditions for providing a full course of rehabilitation.
Emergency 2 treatment methods
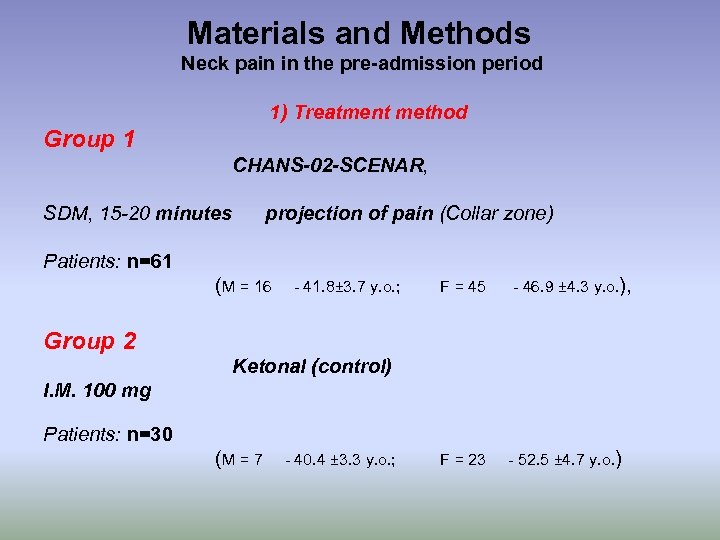
Materials and Methods Neck pain in the pre-admission period 1) Treatment method Group 1 CHANS-02 -SCENAR, SDM, 15 -20 minutes projection of pain (Collar zone) Patients: n=61 (M = 16 - 41. 8± 3. 7 y. o. ; F = 45 - 46. 9 ± 4. 3 y. o. ), F = 23 - 52. 5 ± 4. 7 y. o. ) Group 2 Ketonal (control) I. M. 100 mg Patients: n=30 (M = 7 - 40. 4 ± 3. 3 y. o. ;
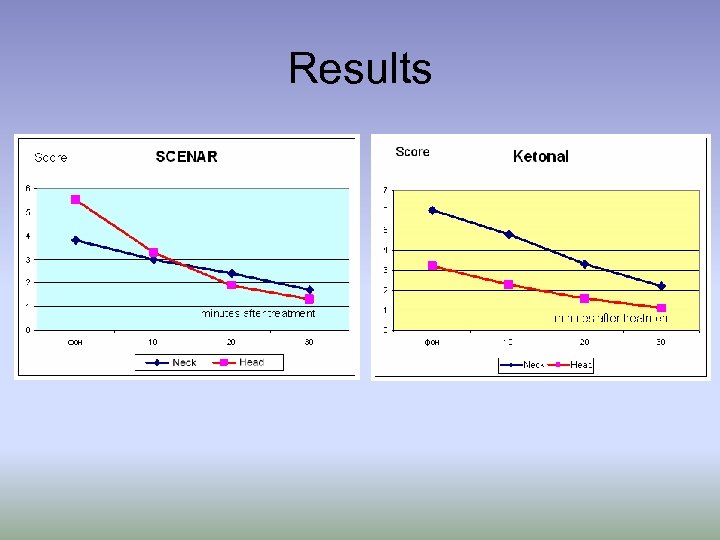
Results
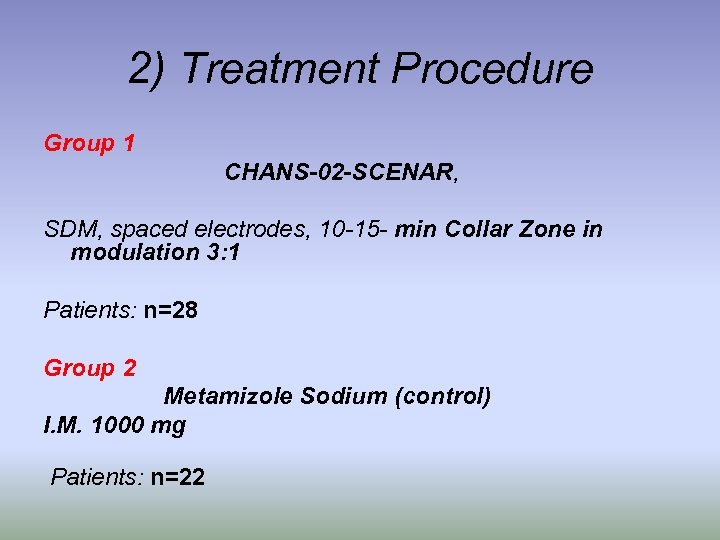
2) Treatment Procedure Group 1 CHANS-02 -SCENAR, SDM, spaced electrodes, 10 -15 - min Collar Zone in modulation 3: 1 Patients: n=28 Group 2 Metamizole Sodium (control) I. M. 1000 mg Patients: n=22
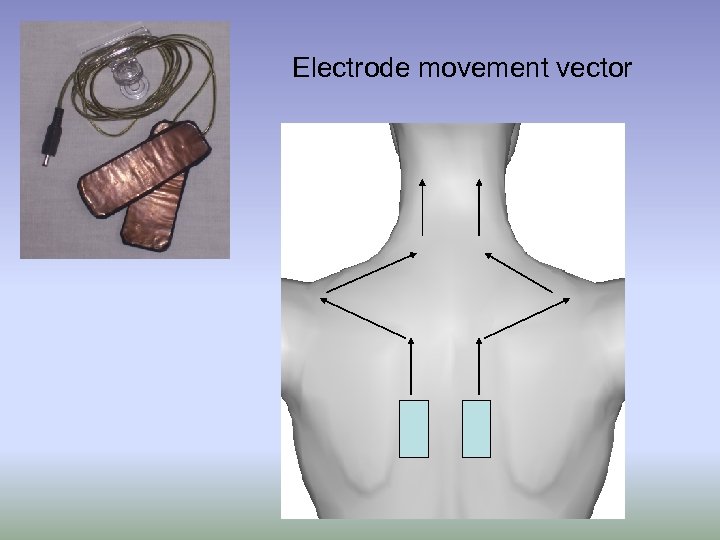
Electrode movement vector
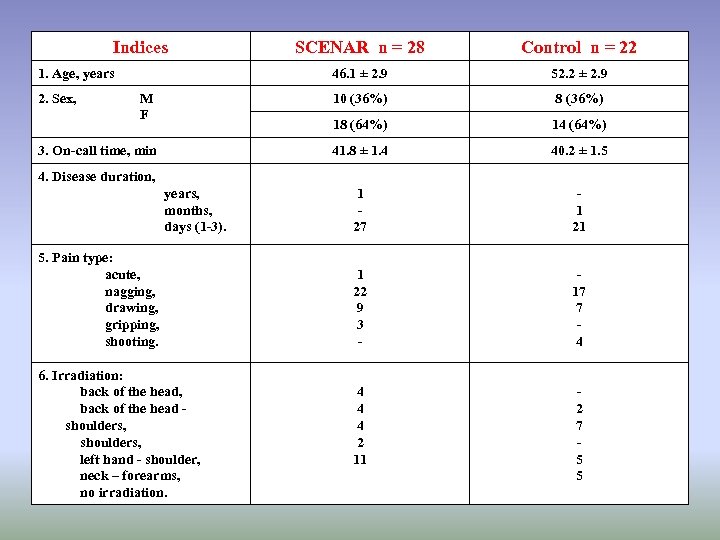
Indices SCENAR n = 28 Control n = 22 46. 1 ± 2. 9 52. 2 ± 2. 9 M F 10 (36%) 8 (36%) 18 (64%) 14 (64%) 3. On-call time, min 41. 8 ± 1. 4 40. 2 ± 1. 5 1 27 1 21 1 22 9 3 - 17 7 4 4 2 11 2 7 5 5 1. Age, years 2. Sex, 4. Disease duration, years, months, days (1 -3). 5. Pain type: acute, nagging, drawing, gripping, shooting. 6. Irradiation: back of the head, back of the head shoulders, left hand - shoulder, neck – forearms, no irradiation.
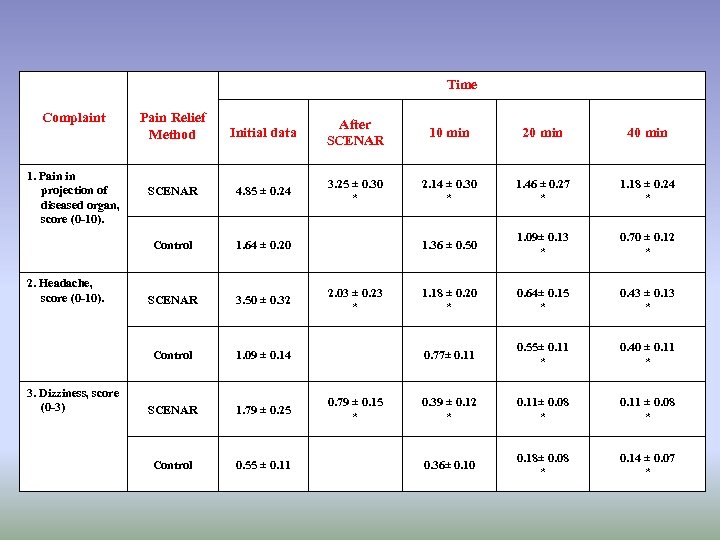
Time Complaint 3. Dizziness, score (0 -3) After SCENAR 10 min 20 min 40 min SCENAR 4. 85 ± 0. 24 3. 25 ± 0. 30 * 2. 14 ± 0. 30 * 1. 46 ± 0. 27 * 1. 18 ± 0. 24 * 1. 64 ± 0. 20 1. 36 ± 0. 50 1. 09± 0. 13 * 0. 70 ± 0. 12 * SCENAR 3. 50 ± 0. 32 1. 18 ± 0. 20 * 0. 64± 0. 15 * 0. 43 ± 0. 13 * Control 2. Headache, score (0 -10). Initial data Control 1. Pain in projection of diseased organ, score (0 -10). Pain Relief Method 1. 09 ± 0. 14 0. 77± 0. 11 0. 55± 0. 11 * 0. 40 ± 0. 11 * SCENAR 1. 79 ± 0. 25 0. 39 ± 0. 12 * 0. 11± 0. 08 * 0. 11 ± 0. 08 * Control 0. 55 ± 0. 11 0. 36± 0. 10 0. 18± 0. 08 * 0. 14 ± 0. 07 * 2. 03 ± 0. 23 * 0. 79 ± 0. 15 *
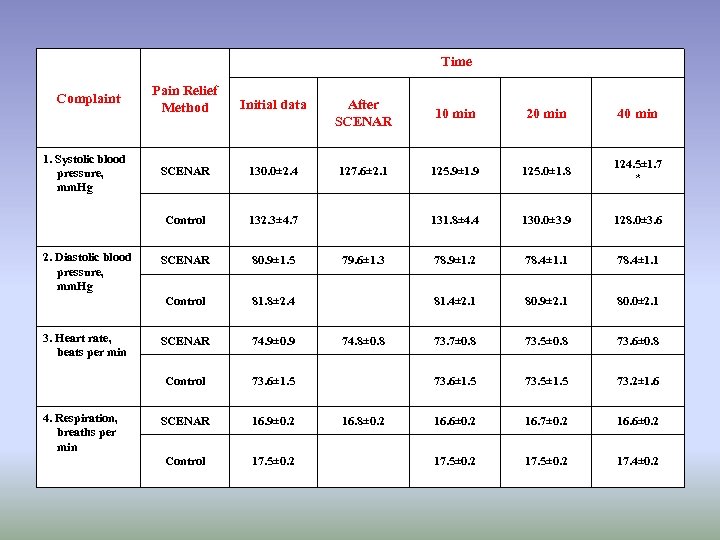
Time 3. Heart rate, beats per min 4. Respiration, breaths per min After SCENAR 10 min 20 min 40 min SCENAR 130. 0± 2. 4 127. 6± 2. 1 125. 9± 1. 9 125. 0± 1. 8 124. 5± 1. 7 * 132. 3± 4. 7 131. 8± 4. 4 130. 0± 3. 9 128. 0± 3. 6 SCENAR 80. 9± 1. 5 78. 9± 1. 2 78. 4± 1. 1 81. 8± 2. 4 81. 4± 2. 1 80. 9± 2. 1 80. 0± 2. 1 SCENAR 74. 9± 0. 9 73. 7± 0. 8 73. 5± 0. 8 73. 6± 0. 8 Control 2. Diastolic blood pressure, mm. Hg Initial data Control 1. Systolic blood pressure, mm. Hg Pain Relief Method Control Complaint 73. 6± 1. 5 73. 5± 1. 5 73. 2± 1. 6 SCENAR 16. 9± 0. 2 16. 6± 0. 2 16. 7± 0. 2 16. 6± 0. 2 Control 17. 5± 0. 2 17. 4± 0. 2 79. 6± 1. 3 74. 8± 0. 8 16. 8± 0. 2
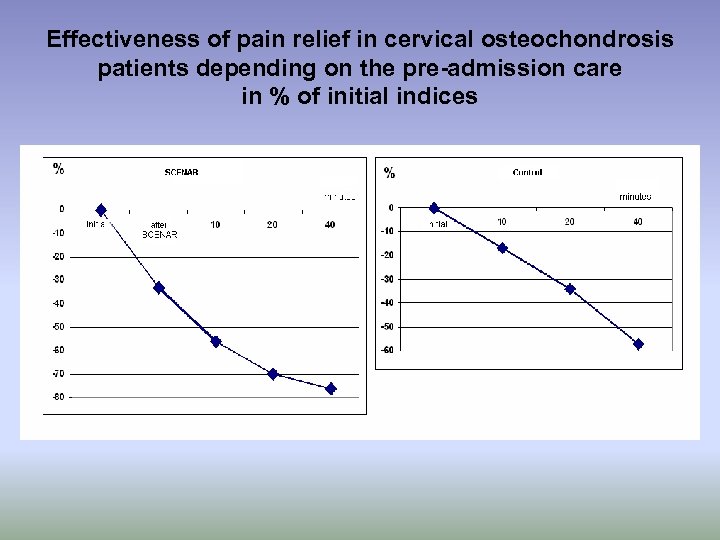
Effectiveness of pain relief in cervical osteochondrosis patients depending on the pre-admission care in % of initial indices
Rehabilitation in SCENAR-Center
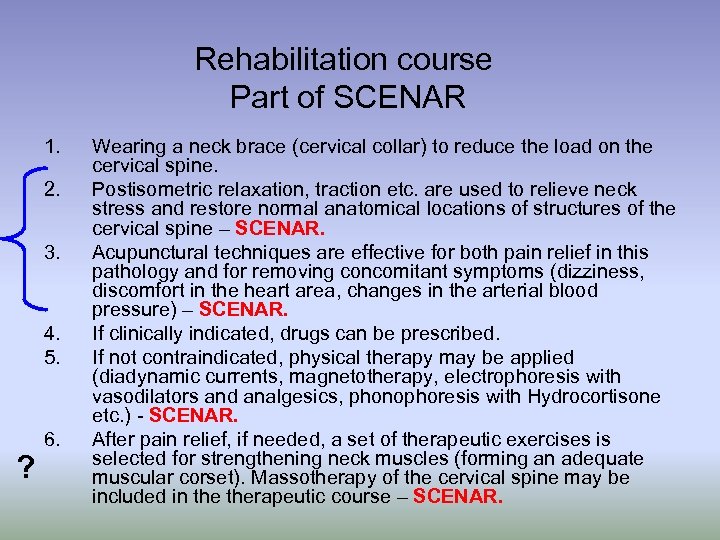
Rehabilitation course Part of SCENAR 1. 2. 3. 4. 5. ? 6. Wearing a neck brace (cervical collar) to reduce the load on the cervical spine. Postisometric relaxation, traction etc. are used to relieve neck stress and restore normal anatomical locations of structures of the cervical spine – SCENAR. Acupunctural techniques are effective for both pain relief in this pathology and for removing concomitant symptoms (dizziness, discomfort in the heart area, changes in the arterial blood pressure) – SCENAR. If clinically indicated, drugs can be prescribed. If not contraindicated, physical therapy may be applied (diadynamic currents, magnetotherapy, electrophoresis with vasodilators and analgesics, phonophoresis with Hydrocortisone etc. ) - SCENAR. After pain relief, if needed, a set of therapeutic exercises is selected for strengthening neck muscles (forming an adequate muscular corset). Massotherapy of the cervical spine may be included in therapeutic course – SCENAR.
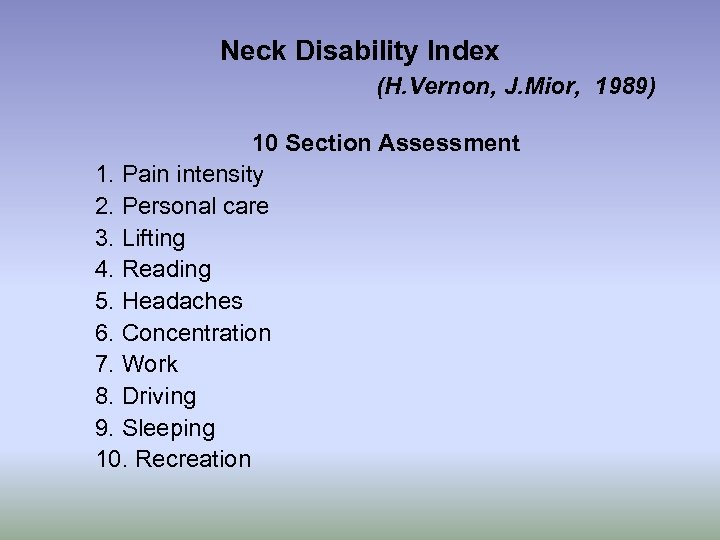
Neck Disability Index (H. Vernon, J. Mior, 1989) 10 Section Assessment 1. Pain intensity 2. Personal care 3. Lifting 4. Reading 5. Headaches 6. Concentration 7. Work 8. Driving 9. Sleeping 10. Recreation
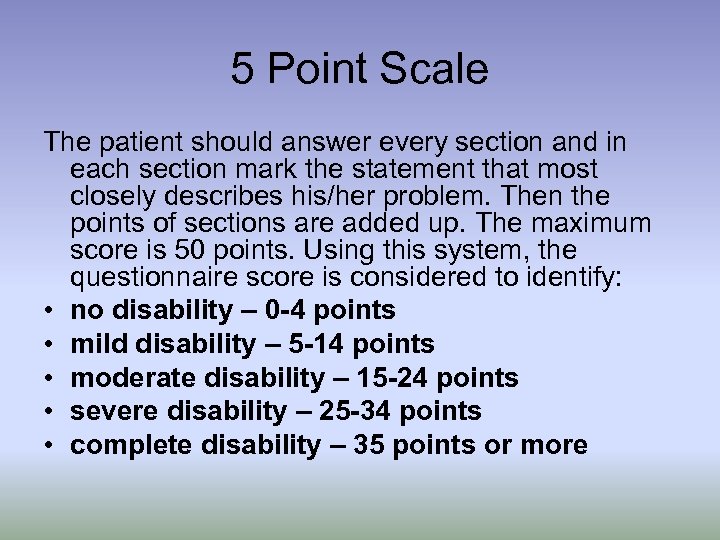
5 Point Scale The patient should answer every section and in each section mark the statement that most closely describes his/her problem. Then the points of sections are added up. The maximum score is 50 points. Using this system, the questionnaire score is considered to identify: • no disability – 0 -4 points • mild disability – 5 -14 points • moderate disability – 15 -24 points • severe disability – 25 -34 points • complete disability – 35 points or more
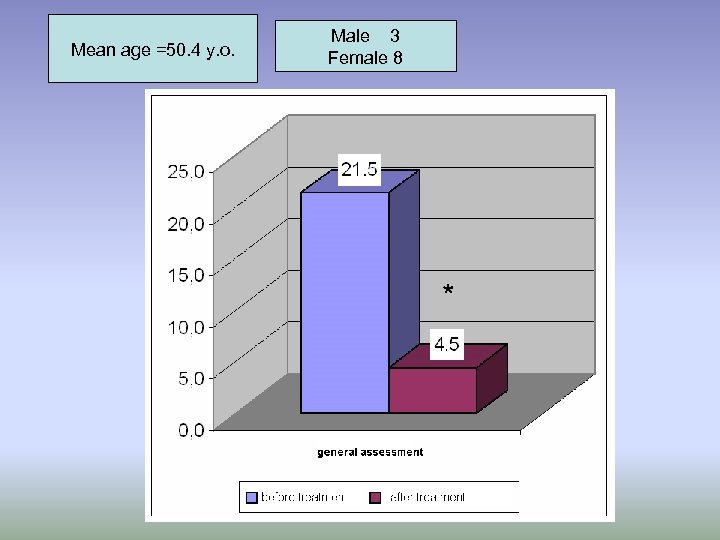
Mean age =50. 4 y. o. Male 3 Female 8 *
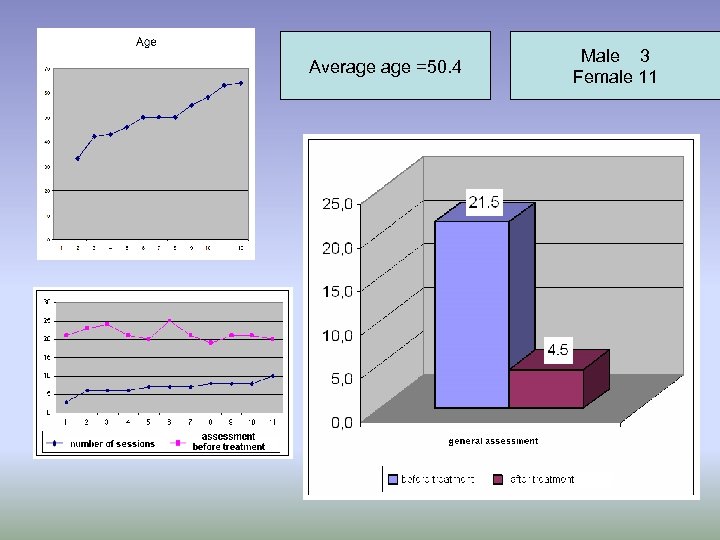
Average =50. 4 Male 3 Female 11
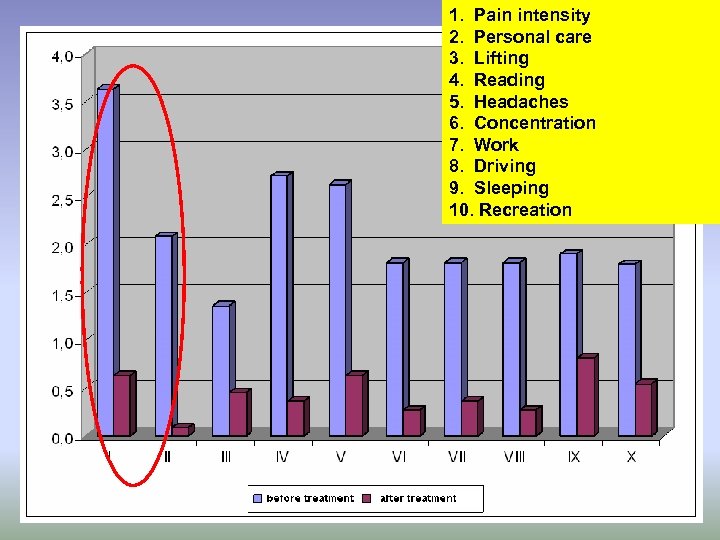
1. Pain intensity 2. Personal care 3. Lifting 4. Reading 5. Headaches 6. Concentration 7. Work 8. Driving 9. Sleeping 10. Recreation
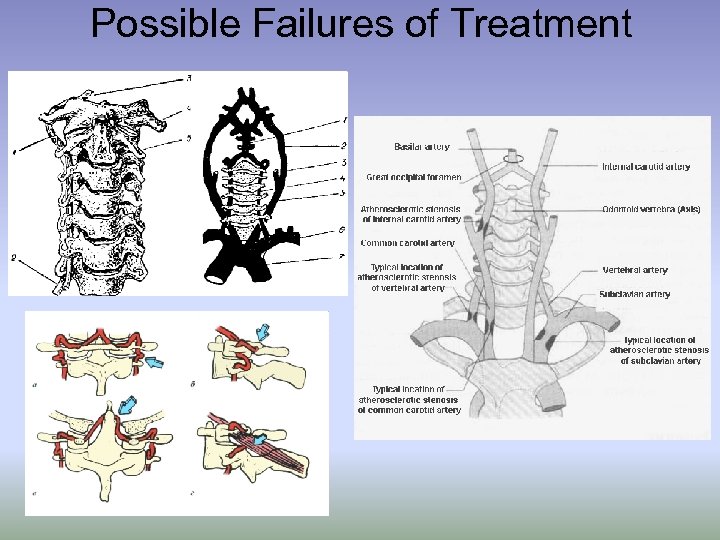
Possible Failures of Treatment
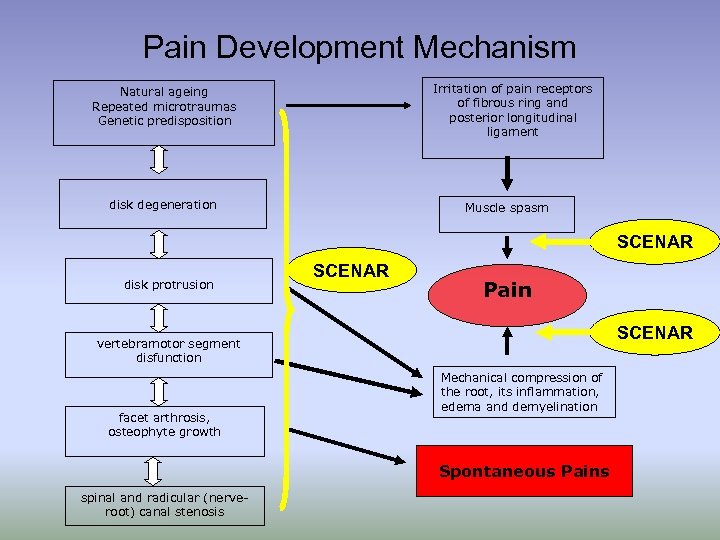
Pain Development Mechanism Irritation of pain receptors of fibrous ring and posterior longitudinal ligament Natural ageing Repeated microtraumas Genetic predisposition disk degeneration Muscle spasm SCENAR disk protrusion SCENAR Pain SCENAR vertebramotor segment disfunction facet arthrosis, osteophyte growth Mechanical compression of the root, its inflammation, edema and demyelination Spontaneous Pains spinal and radicular (nerveroot) canal stenosis
Conclusion SCENAR-therapy is an effective method for treating degenerative diseases of the spine on all levels of providing care. Basic effects pain relief better quality of life less drugs
Investigations to Be Done ! 1. Morphological investigations. 2. Ultrasound of blood circulation. 3. Biochemical investigations.
ebd2e9839f9c0687ec0ac6016355a331.ppt