b6166f8732f0eae7e76b8c195f14f76e.ppt
- Количество слайдов: 27
 Pain Management Communicating with Chronic Pain Patients Learning Session 1 Drs. Wesley Buch & David Hunt Presenter’s name here Location here Date here www. pspbc. ca
Pain Management Communicating with Chronic Pain Patients Learning Session 1 Drs. Wesley Buch & David Hunt Presenter’s name here Location here Date here www. pspbc. ca
 Faculty/Presenter Disclosure Speaker’s Name: Speaker’s Name Relationships with commercial interests: - Grants/Research Support: Pharma. Corp ABC - Speakers Bureau/Honoraria: XYZ Biopharmaceuticals Ltd - Consulting Fees: Med. X Group Inc. - Other: Employee of XYZ Hospital Group 2
Faculty/Presenter Disclosure Speaker’s Name: Speaker’s Name Relationships with commercial interests: - Grants/Research Support: Pharma. Corp ABC - Speakers Bureau/Honoraria: XYZ Biopharmaceuticals Ltd - Consulting Fees: Med. X Group Inc. - Other: Employee of XYZ Hospital Group 2
![Disclosure of Commercial Support This program has received financial support from [organization name] in Disclosure of Commercial Support This program has received financial support from [organization name] in](https://present5.com/presentation/b6166f8732f0eae7e76b8c195f14f76e/image-3.jpg) Disclosure of Commercial Support This program has received financial support from [organization name] in the form of [describe support here – e. g. educational grant]. This program has received in-kind support from [organization name] in the form of [describe the support here – e. g. logistical support]. Potential for conflict(s) of interest: - [Speaker/Faculty name] has received [payment/funding, etc. ] from [organization supporting this program AND/OR organization whose product(s) are being discussed in this program]. - [Supporting organization name] [developed/licenses/distributes/benefits from the sale of, etc. ] a product that will be discussed in this program: [enter generic and brand name here]. 3
Disclosure of Commercial Support This program has received financial support from [organization name] in the form of [describe support here – e. g. educational grant]. This program has received in-kind support from [organization name] in the form of [describe the support here – e. g. logistical support]. Potential for conflict(s) of interest: - [Speaker/Faculty name] has received [payment/funding, etc. ] from [organization supporting this program AND/OR organization whose product(s) are being discussed in this program]. - [Supporting organization name] [developed/licenses/distributes/benefits from the sale of, etc. ] a product that will be discussed in this program: [enter generic and brand name here]. 3
 Mitigating Potential Bias [Explain how potential sources of bias identified in slides 1 and 2 have been mitigated]. Refer to “Quick Tips” document 4
Mitigating Potential Bias [Explain how potential sources of bias identified in slides 1 and 2 have been mitigated]. Refer to “Quick Tips” document 4
 Certification § Up to 21 Mainpro+ Certified credits for GPs awarded upon completion of: › All 3 Learning Sessions (NOTE: Credits and payment will be based on the exact number of hours in session) › At least 1 Action Period › The Post-Activity Reflective Questionnaire (2 months after LS 3) § Up to 10. 5 Section 1 credits for Specialists › All 3 Learning Sessions (NOTE: Credits and payment will be based on the exact number of hours in session) › The Post-Activity Reflective Questionnaire (2 months after LS 3) 5
Certification § Up to 21 Mainpro+ Certified credits for GPs awarded upon completion of: › All 3 Learning Sessions (NOTE: Credits and payment will be based on the exact number of hours in session) › At least 1 Action Period › The Post-Activity Reflective Questionnaire (2 months after LS 3) § Up to 10. 5 Section 1 credits for Specialists › All 3 Learning Sessions (NOTE: Credits and payment will be based on the exact number of hours in session) › The Post-Activity Reflective Questionnaire (2 months after LS 3) 5
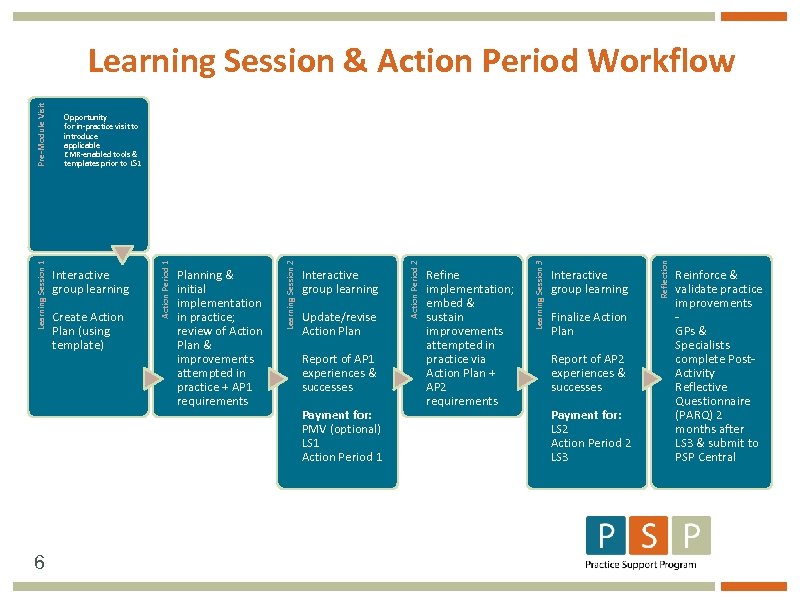 6 Update/revise Action Plan Report of AP 1 experiences & successes Payment for: PMV (optional) LS 1 Action Period 1 Refine implementation; embed & sustain improvements attempted in practice via Action Plan + AP 2 requirements Interactive group learning Finalize Action Plan Report of AP 2 experiences & successes Payment for: LS 2 Action Period 2 LS 3 Reflection Interactive group learning Learning Session 3 Create Action Plan (using template) Planning & initial implementation in practice; review of Action Plan & improvements attempted in practice + AP 1 requirements Action Period 2 Interactive group learning Learning Session 2 Opportunity for in-practice visit to introduce applicable EMR-enabled tools & templates prior to LS 1 Action Period 1 Learning Session 1 Pre-Module Visit Learning Session & Action Period Workflow Reinforce & validate practice improvements GPs & Specialists complete Post. Activity Reflective Questionnaire (PARQ) 2 months after LS 3 & submit to PSP Central
6 Update/revise Action Plan Report of AP 1 experiences & successes Payment for: PMV (optional) LS 1 Action Period 1 Refine implementation; embed & sustain improvements attempted in practice via Action Plan + AP 2 requirements Interactive group learning Finalize Action Plan Report of AP 2 experiences & successes Payment for: LS 2 Action Period 2 LS 3 Reflection Interactive group learning Learning Session 3 Create Action Plan (using template) Planning & initial implementation in practice; review of Action Plan & improvements attempted in practice + AP 1 requirements Action Period 2 Interactive group learning Learning Session 2 Opportunity for in-practice visit to introduce applicable EMR-enabled tools & templates prior to LS 1 Action Period 1 Learning Session 1 Pre-Module Visit Learning Session & Action Period Workflow Reinforce & validate practice improvements GPs & Specialists complete Post. Activity Reflective Questionnaire (PARQ) 2 months after LS 3 & submit to PSP Central
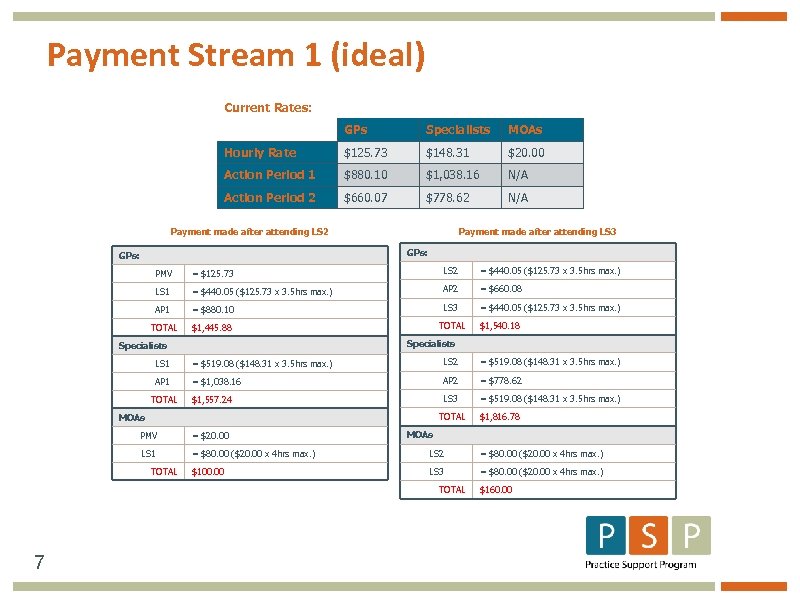 Payment Stream 1 (ideal) Current Rates: GPs Specialists MOAs Hourly Rate $125. 73 $148. 31 $20. 00 Action Period 1 $880. 10 $1, 038. 16 N/A Action Period 2 $660. 07 $778. 62 N/A Payment made after attending LS 2 Payment made after attending LS 3 GPs: PMV = $125. 73 LS 2 = $440. 05 ($125. 73 x 3. 5 hrs max. ) LS 1 = $440. 05 ($125. 73 x 3. 5 hrs max. ) AP 2 = $660. 08 AP 1 = $880. 10 LS 3 = $440. 05 ($125. 73 x 3. 5 hrs max. ) TOTAL $1, 445. 88 TOTAL $1, 540. 18 Specialists LS 1 = $519. 08 ($148. 31 x 3. 5 hrs max. ) LS 2 = $519. 08 ($148. 31 x 3. 5 hrs max. ) AP 1 = $1, 038. 16 AP 2 = $778. 62 $1, 557. 24 LS 3 = $519. 08 ($148. 31 x 3. 5 hrs max. ) TOTAL MOAs $1, 816. 78 MOAs PMV = $20. 00 LS 1 = $80. 00 ($20. 00 x 4 hrs max. ) LS 2 = $80. 00 ($20. 00 x 4 hrs max. ) $100. 00 LS 3 = $80. 00 ($20. 00 x 4 hrs max. ) TOTAL 7 $160. 00
Payment Stream 1 (ideal) Current Rates: GPs Specialists MOAs Hourly Rate $125. 73 $148. 31 $20. 00 Action Period 1 $880. 10 $1, 038. 16 N/A Action Period 2 $660. 07 $778. 62 N/A Payment made after attending LS 2 Payment made after attending LS 3 GPs: PMV = $125. 73 LS 2 = $440. 05 ($125. 73 x 3. 5 hrs max. ) LS 1 = $440. 05 ($125. 73 x 3. 5 hrs max. ) AP 2 = $660. 08 AP 1 = $880. 10 LS 3 = $440. 05 ($125. 73 x 3. 5 hrs max. ) TOTAL $1, 445. 88 TOTAL $1, 540. 18 Specialists LS 1 = $519. 08 ($148. 31 x 3. 5 hrs max. ) LS 2 = $519. 08 ($148. 31 x 3. 5 hrs max. ) AP 1 = $1, 038. 16 AP 2 = $778. 62 $1, 557. 24 LS 3 = $519. 08 ($148. 31 x 3. 5 hrs max. ) TOTAL MOAs $1, 816. 78 MOAs PMV = $20. 00 LS 1 = $80. 00 ($20. 00 x 4 hrs max. ) LS 2 = $80. 00 ($20. 00 x 4 hrs max. ) $100. 00 LS 3 = $80. 00 ($20. 00 x 4 hrs max. ) TOTAL 7 $160. 00
 Format § Interactive Format § Four Scenarios § Three Repeating Questions › What’s Wrong Here? w Patient Feels? w Physician Feels? › What Would You Do Differently? › What Do We Suggest? 8
Format § Interactive Format § Four Scenarios § Three Repeating Questions › What’s Wrong Here? w Patient Feels? w Physician Feels? › What Would You Do Differently? › What Do We Suggest? 8
 What’s wrong here Scenario 1 9
What’s wrong here Scenario 1 9
 What would you do differently? Scenario 1: The Wound Up - Gobbledygook Physician 10
What would you do differently? Scenario 1: The Wound Up - Gobbledygook Physician 10
 What do we suggest? § Prepare yourself for patient in minute before entering office › “wind up” is contagious › “wind down” starts with physician § Look at the patient. § Talk slowly. Move slowly. § Focus on one or two major problems › make arrangements to see again for other problems. The Wound Up - Gobbledygook Physician 11
What do we suggest? § Prepare yourself for patient in minute before entering office › “wind up” is contagious › “wind down” starts with physician § Look at the patient. § Talk slowly. Move slowly. § Focus on one or two major problems › make arrangements to see again for other problems. The Wound Up - Gobbledygook Physician 11
 What do we suggest? § Speak slowly in ordinary language at patient’s level of understanding § Teach back technique (patient) § Invite a family member or friend to attend § Refer to Patient Self-Management & Health Literacy Module The Wound Up - Gobbledygook Physician 12
What do we suggest? § Speak slowly in ordinary language at patient’s level of understanding § Teach back technique (patient) § Invite a family member or friend to attend § Refer to Patient Self-Management & Health Literacy Module The Wound Up - Gobbledygook Physician 12
 What’s wrong here Scenario 2 13
What’s wrong here Scenario 2 13
 What would you do differently? Scenario 2: The Frustrated – Stuck Physician 14
What would you do differently? Scenario 2: The Frustrated – Stuck Physician 14
 What do we suggest? § Look for cues in yourself of feeling angry § Check & drop your biases at door § Deliberately choose an empathic approach § Consult – you’re not alone. § Sample script The Frustrated - Stuck Physician 15
What do we suggest? § Look for cues in yourself of feeling angry § Check & drop your biases at door § Deliberately choose an empathic approach § Consult – you’re not alone. § Sample script The Frustrated - Stuck Physician 15
 Empathic script for frustrated physician § “I can see you’re still in a lot of pain. That must be so frustrating for you. It’s frustrating for me too & I don’t have your pain. I think we’re both feeling stuck. ” (joining) § “Trying new strategies takes time and small steps. As I’ve explained, when you engage in paced activity you will strengthen your body so that you can do more than you’re doing now without pain flare-ups. ” § “You might already know what to do but you worry about moving more because of pain or even re-injury. ” (fears, catastrophizing) § “So let’s look at what part of our plan isn’t working yet. ” (problem-solving) The Frustrated - Stuck Physician 16
Empathic script for frustrated physician § “I can see you’re still in a lot of pain. That must be so frustrating for you. It’s frustrating for me too & I don’t have your pain. I think we’re both feeling stuck. ” (joining) § “Trying new strategies takes time and small steps. As I’ve explained, when you engage in paced activity you will strengthen your body so that you can do more than you’re doing now without pain flare-ups. ” § “You might already know what to do but you worry about moving more because of pain or even re-injury. ” (fears, catastrophizing) § “So let’s look at what part of our plan isn’t working yet. ” (problem-solving) The Frustrated - Stuck Physician 16
 What’s wrong here Scenario 3 17
What’s wrong here Scenario 3 17
 What would you do differently? Scenario 3: The Argumentative Patient 18
What would you do differently? Scenario 3: The Argumentative Patient 18
 What do we suggest? § Do not personalize or become defensive. § Is your manner or approach off-putting? § Set boundaries & limits. Time to let go? § Do you wonder about unspoken agendas? § Sample script The Argumentative Patient 19
What do we suggest? § Do not personalize or become defensive. § Is your manner or approach off-putting? § Set boundaries & limits. Time to let go? § Do you wonder about unspoken agendas? § Sample script The Argumentative Patient 19
 Script for argumentative patient § “You still have pain. ” § “My treatment suggestions do not appear to be working for you. ” § “You seem more interested in trying these otherapies. ” § “You can always return. ” The Argumentative Patient 20
Script for argumentative patient § “You still have pain. ” § “My treatment suggestions do not appear to be working for you. ” § “You seem more interested in trying these otherapies. ” § “You can always return. ” The Argumentative Patient 20
 What’s wrong here Scenario 4 21
What’s wrong here Scenario 4 21
 What would you do differently? Scenario 4: The Rescuing – Discouraged Physician 22
What would you do differently? Scenario 4: The Rescuing – Discouraged Physician 22
 What do we suggest for the Rescuing Physician? § What cues your urge to rescue? § Self-coaching: “What does this patient really need or want? ” “Will I really help this patient by giving another round of Oxys? ” § Script that is empathic & firm. The Rescuing – Discouraged Physician 23
What do we suggest for the Rescuing Physician? § What cues your urge to rescue? § Self-coaching: “What does this patient really need or want? ” “Will I really help this patient by giving another round of Oxys? ” § Script that is empathic & firm. The Rescuing – Discouraged Physician 23
 Script for Rescuing Physician § “The research & my experience with this medication tells me that higher levels of these Oxys are bad for patients. This is because they lead to complications that are harmful. ” § “For example, you start to notice that you have to take increased doses just to get the same effect. But soon you get less relief and then more pain. ” § “If these medications allow you to move more, it makes sense to use them. Otherwise, we need to find a different plan. ” The Rescuing – Discouraged Physician 24
Script for Rescuing Physician § “The research & my experience with this medication tells me that higher levels of these Oxys are bad for patients. This is because they lead to complications that are harmful. ” § “For example, you start to notice that you have to take increased doses just to get the same effect. But soon you get less relief and then more pain. ” § “If these medications allow you to move more, it makes sense to use them. Otherwise, we need to find a different plan. ” The Rescuing – Discouraged Physician 24
 What do we suggest for discouraged physician? § Are you aware of feeling discouraged about this patient? § Self-coaching: “I’m feeling discouraged about this patient. How can I proceed in a more hopeful manner? ” § Sample script The Rescuing - Discouraged Physician 25
What do we suggest for discouraged physician? § Are you aware of feeling discouraged about this patient? § Self-coaching: “I’m feeling discouraged about this patient. How can I proceed in a more hopeful manner? ” § Sample script The Rescuing - Discouraged Physician 25
 Script for Discouraged Physician § “Although there’s no specific diagnosis, I do believe that you have real pain. ” § “All the consults and tests support your experience of chronic pain. And there are some good ways to manage that pain. ” § “The best pain management will come from us working together to find the right combination of pain self-management and other treatments to support you in this. ” § “For example, I doubt that you will harm yourself if you do more around the house in a paced way. And this will help you both mentally & physically to prepare for work. ” The Rescuing - Discouraged Physician 26
Script for Discouraged Physician § “Although there’s no specific diagnosis, I do believe that you have real pain. ” § “All the consults and tests support your experience of chronic pain. And there are some good ways to manage that pain. ” § “The best pain management will come from us working together to find the right combination of pain self-management and other treatments to support you in this. ” § “For example, I doubt that you will harm yourself if you do more around the house in a paced way. And this will help you both mentally & physically to prepare for work. ” The Rescuing - Discouraged Physician 26
 Where to learn more § F. Daniel Duffy et al (2004), “Assessing competence in communication and interpersonal skills, ” Academic Medicine, 79(6), 495 -507. § Patricia L. B. Lockyear, Dec. 9, 2004, “Physician-patient communication: enhancing skills to improve patient satisfaction. ” www. medscape. com § Peter Tate (2010), The Doctor’s Communication Handbook, 6 th Ed. Abingdon Oxon, Radcliffe Publishers. § L. Wen & J. Kosowsky (2012), When doctors don’t listen. NY: St. Martin’s Press. Doctor – Patient Communication 27
Where to learn more § F. Daniel Duffy et al (2004), “Assessing competence in communication and interpersonal skills, ” Academic Medicine, 79(6), 495 -507. § Patricia L. B. Lockyear, Dec. 9, 2004, “Physician-patient communication: enhancing skills to improve patient satisfaction. ” www. medscape. com § Peter Tate (2010), The Doctor’s Communication Handbook, 6 th Ed. Abingdon Oxon, Radcliffe Publishers. § L. Wen & J. Kosowsky (2012), When doctors don’t listen. NY: St. Martin’s Press. Doctor – Patient Communication 27


